Antibacterial and Antiviral Effects of Ag, Cu and Zn Metals, Respective Nanoparticles and Filter Materials Thereof against Coronavirus SARS-CoV-2 and Influenza A Virus
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials and Chemicals
2.2. Viruses and Cells
2.3. Dispersion Analysis for Polymer Solvent Systems with Metal Nanoparticles
2.4. Electrospinning of Filter Materials
2.4.1. Analysis of Morphology of Electrospun Filter Material
2.4.2. Air Permeability Testing of Electrospun Filter Materials
2.4.3. Testing of Aerosol Filtration Efficiency of Electrospun Filter Materials
2.4.4. Hydrophobicity/Hydrophilicity Determining
2.4.5. Quantification of Metal Content and the Released Metal Content of the Fiber Materials
2.5. Cytotoxicity Assay
2.6. Antibacterial Assay
2.7. Assessment of Antiviral Activity of Nanomaterials and Corresponding Salts in Suspensions
2.8. Deactivation of Viruses by Fiber Materials
2.9. Statistical Analysis
3. Results
3.1. Antiviral Efficacy of Nanoparticles in Suspensions
3.2. Development and Characterization of Filter Materials
3.2.1. Compatibility of NPs with Solvent Systems for Preparation of the Filter Materials
3.2.2. Development of Filter Materials
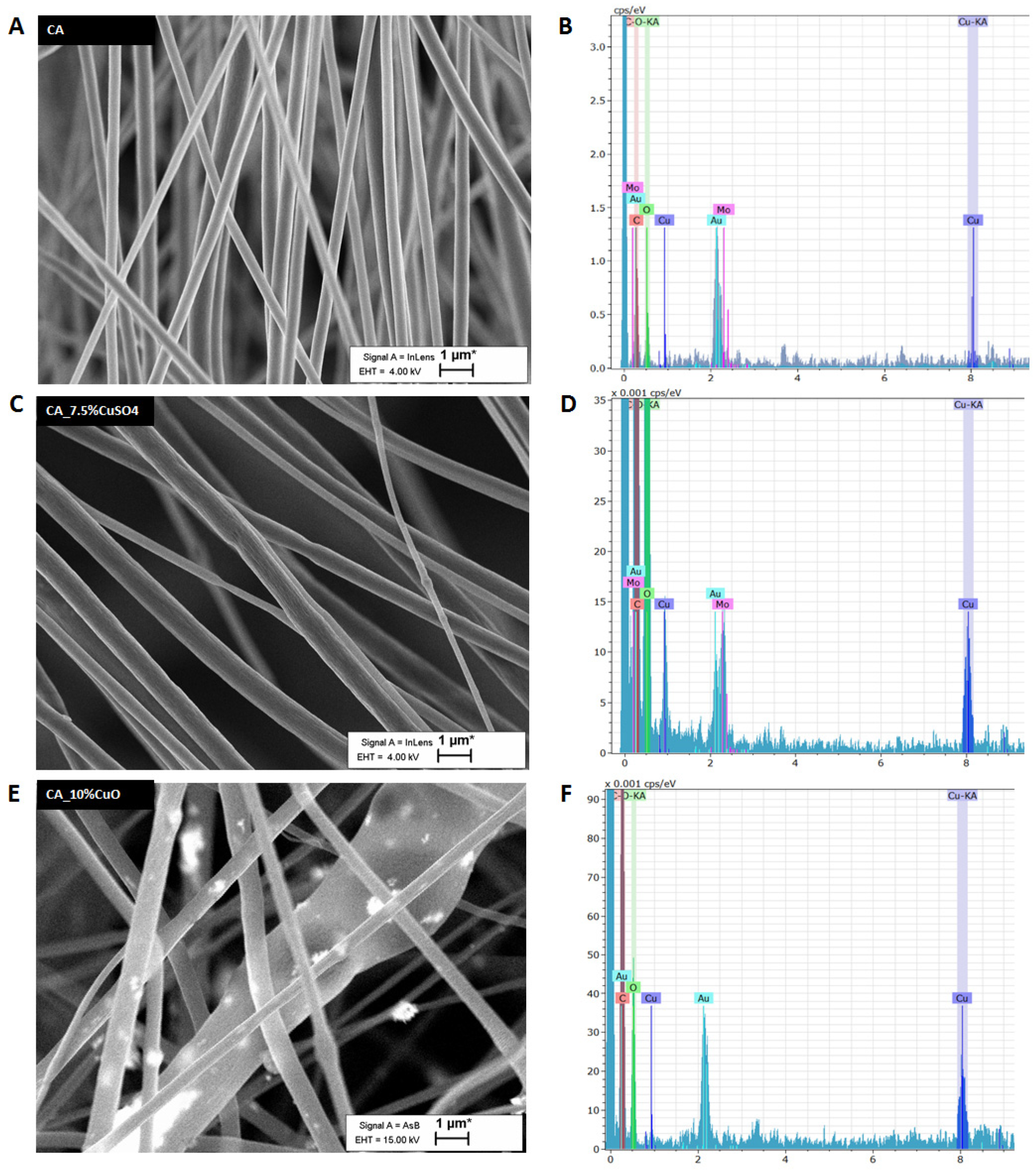
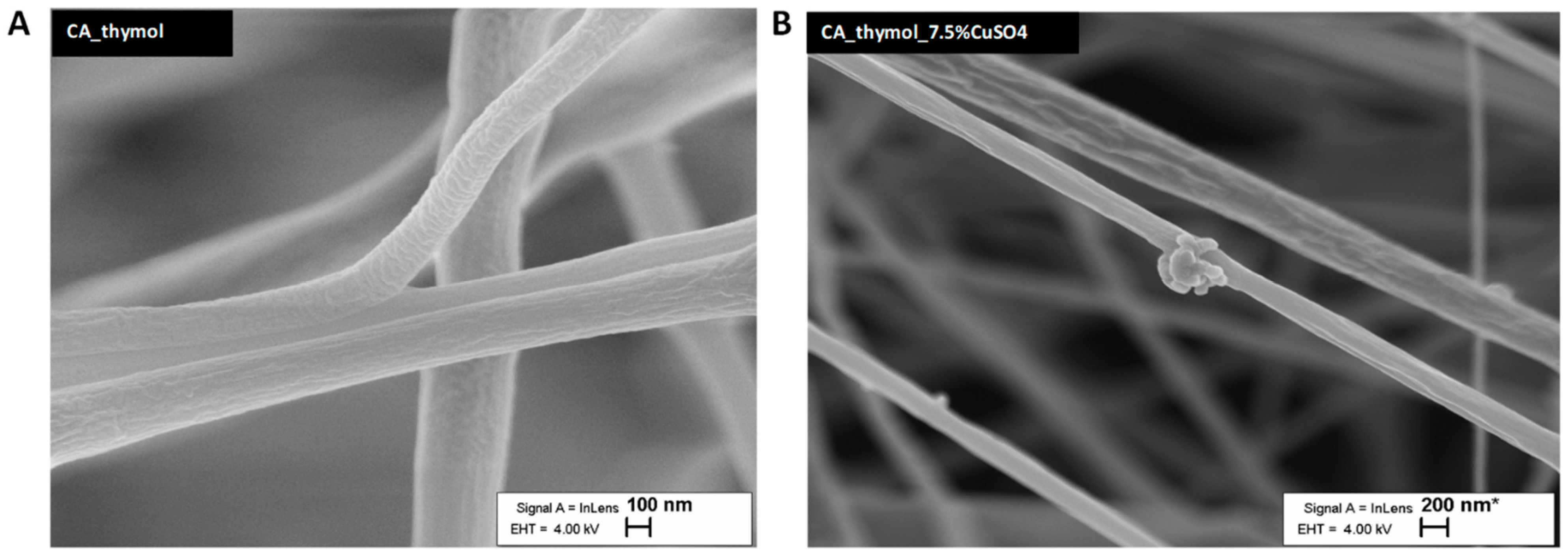
3.2.3. Morphology of Filter Materials
3.2.4. Thickness, Hydrophilicity, and Air Filtration Parameters of Filter Materials
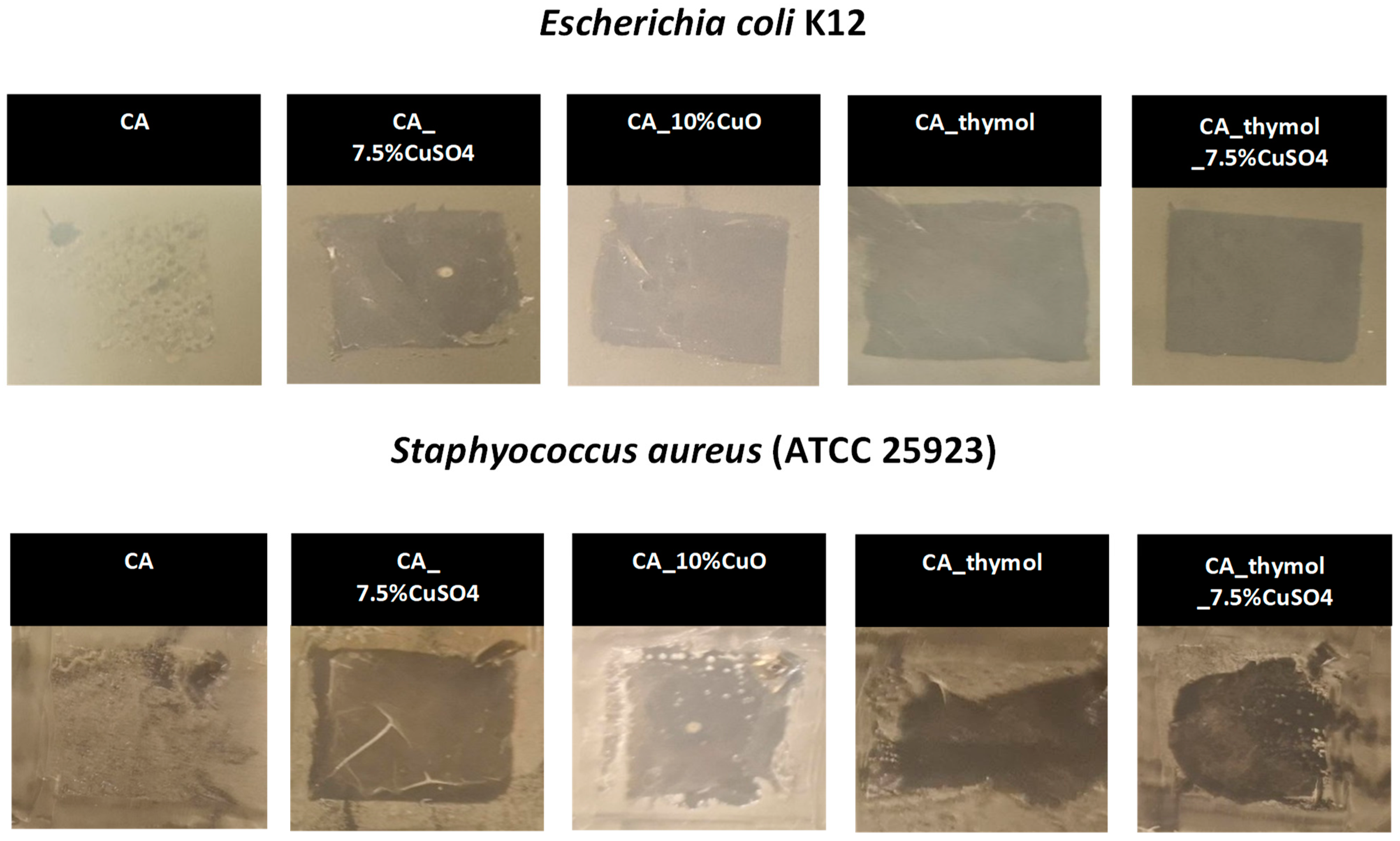
3.3. Antibacterial Efficacy of Filter Materials Comprising Copper NPs and Copper Salt
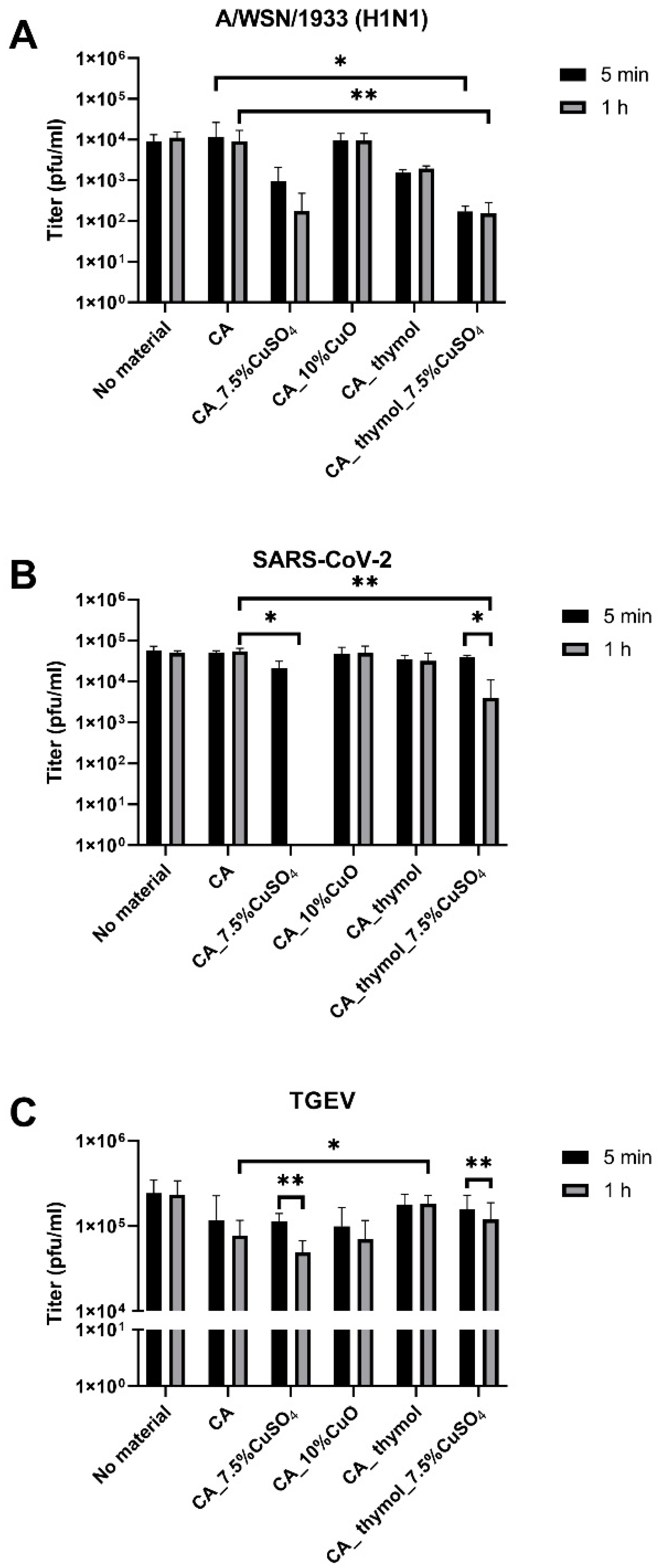
3.4. Antiviral Efficacy of Fiber Materials Comprising Antimicrobial Metals
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Menachery, V.D.; Yount, B.L.; Debbink, K.; Agnihothram, S.; Gralinski, L.E.; Plante, J.A.; Graham, R.L.; Scobey, T.; Ge, X.Y.; Donaldson, E.F.; et al. A SARS-like Cluster of Circulating Bat Coronaviruses Shows Potential for Human Emergence. Nat. Med. 2015, 21, 1508–1513. [Google Scholar] [CrossRef] [PubMed]
- Xia, X. Domains and Functions of Spike Protein in SARS-CoV-2 in the Context of Vaccine Design. Viruses 2021, 13, 109. [Google Scholar] [CrossRef] [PubMed]
- Sternberg, A.; Naujokat, C. Structural Features of Coronavirus SARS-CoV-2 Spike Protein: Targets for Vaccination. Life Sci. 2020, 257, 118056. [Google Scholar] [CrossRef] [PubMed]
- Wan, Y.; Shang, J.; Graham, R.; Baric, R.S.; Li, F. Receptor Recognition by the Novel Coronavirus from Wuhan: An Analysis Based on Decade-Long Structural Studies of SARS Coronavirus. J. Virol. 2020, 94, e00127-20. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Pei, S.; Chen, B.; Song, Y.; Zhang, T.; Yang, W.; Shaman, J. Substantial Undocumented Infection Facilitates the Rapid Dissemination of Novel Coronavirus (SARS-CoV-2). Science 2020, 368, 489–493. [Google Scholar] [CrossRef]
- Ochani, R.K.; Yasmin, F.; Jatoi, N.N. Epidemic Amidst the Coronavirus Disease-19 Pandemic. J. Glob. Health 2021, 11, 03056. [Google Scholar] [CrossRef]
- Hasöksüz, M.; Kiliç, S.; Saraç, F. Coronaviruses and SARS-CoV-2. Turkish J. Med. Sci. 2020, 50, 549–556. [Google Scholar] [CrossRef]
- Khan, M.; Syed, F.A.; Hamad, Z.A.; Muhammad, N.T.; Saif, S.; KHan, M.; Khan, S.T. Epidemiology and Progress So Far. Moléculas 2021, 26, 39. [Google Scholar] [CrossRef]
- WHO. Mask Use in the Context of COVID-19. Available online: https://extranet.who.int/iris/restricted/handle/10665/331789 (accessed on 3 May 2022).
- CDC. Coronavirus Disease 2019 Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant. Available online: https://stacks.cdc.gov/view/cdc/86440 (accessed on 3 May 2022).
- Gholamreza, F.; Nadaraja, A.V.; Milani, A.S.; Golovin, K. Enhanced Protection Face Masks Do Not Adversely Impact Thermophysiological Comfort. PLoS ONE 2022, 17, e0265126. [Google Scholar] [CrossRef]
- Neuman, B.W.; Adair, B.D.; Yoshioka, C.; Quispe, J.D.; Orca, G.; Kuhn, P.; Milligan, R.A.; Yeager, M.; Buchmeier, M.J. Supramolecular Architecture of Severe Acute Respiratory Syndrome Coronavirus Revealed by Electron Cryomicroscopy. J. Virol. 2006, 80, 7918–7928. [Google Scholar] [CrossRef]
- Siddharta, A.; Pfaender, S.; Vielle, N.J.; Dijkman, R.; Friesland, M.; Becker, B.; Yang, J.; Engelmann, M.; Todt, D.; Windisch, M.P.; et al. Virucidal Activity of World Health Organization-Recommended Formulations Against Enveloped Viruses, Including Zika, Ebola, and Emerging Coronaviruses. J. Infect. Dis. 2017, 215, 902–906. [Google Scholar] [CrossRef]
- Rai, M.; Deshmukh, S.D.; Ingle, A.P.; Gupta, I.R.; Galdiero, M.; Galdiero, S. Metal Nanoparticles: The Protective Nanoshield against Virus Infection. Crit. Rev. Microbiol. 2016, 42, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Jarach, N.; Dodiuk, H.; Kenig, S. Polymers in the Medical Antiviral Front-Line. Polymers 2020, 12, 1727. [Google Scholar] [CrossRef] [PubMed]
- Chakravarty, M.; Vora, A. Nanotechnology-Based Antiviral Therapeutics. Drug Deliv. Transl. Res. 2021, 11, 748–787. [Google Scholar] [CrossRef] [PubMed]
- Nasri, N.; Rusli, A.; Teramoto, N.; Jaafar, M.; Ishak, K.M.K.; Shafiq, M.D.; Hamid, Z.A.A. Past and Current Progress in the Development of Antiviral/ Antimicrobial Polymer Coating towards COVID-19 Prevention: A Review. Polymers 2021, 13, 4234. [Google Scholar] [CrossRef]
- Chua, M.H.; Cheng, W.; Goh, S.S.; Kong, J.; Li, B.; Lim, J.Y.C.; Mao, L.; Wang, S.; Xue, K.; Yang, L.; et al. Face Masks in the New COVID-19 Normal: Materials, Testing, and Perspectives. Research 2020, 2020, 1–40. [Google Scholar] [CrossRef] [PubMed]
- Bondarenko, O.; Juganson, K.; Ivask, A.; Kasemets, K.; Mortimer, M.; Kahru, A. Toxicity of Ag, CuO and ZnO Nanoparticles to Selected Environmentally Relevant Test Organisms and Mammalian Cells in Vitro: A Critical Review. Arch. Toxicol. 2013, 87, 1181–1200. [Google Scholar] [CrossRef]
- Ivask, A.; Juganson, K.; Bondarenko, O.; Mortimer, M.; Aruoja, V.; Kasemets, K.; Blinova, I.; Heinlaan, M.; Slaveykova, V.; Kahru, A. Mechanisms of Toxic Action of Ag, ZnO and CuO Nanoparticles to Selected Ecotoxicological Test Organisms and Mammalian Cells in Vitro: A Comparative Review. Nanotoxicology 2014, 8, 57–71. [Google Scholar] [CrossRef]
- Bahrami, A.; Arabestani, M.R.; Taheri, M.; Farmany, A.; Norozzadeh, F.; Hosseini, S.M.; Nozari, H.; Nouri, F. Exploring the Role of Heavy Metals and Their Derivatives on the Pathophysiology of COVID-19. Biol. Trace Elem. Res. 2022, 200, 2639–2650. [Google Scholar] [CrossRef]
- Jeremiah, S.S.; Miyakawa, K.; Morita, T.; Yamaoka, Y.; Akihide, R. Potent Antiviral Effect of Silver Nanoparticles on SARS-CoV-2. Biochem. Biophys. Res. Commun. 2020, 533, 195–200. [Google Scholar] [CrossRef]
- Fujimori, Y.; Sato, T.; Hayata, T.; Nagao, T.; Nakayam, M.; Nakayam, T.; Sugamat, R.; Suzuki, K. Novel Antiviral Characteristics of Nanosized Copper(i) Iodide Particles Showing Inactivation Activity against 2009 Pandemic H1N1 Influenza Virus. Appl. Environ. Microbiol. 2011, 78, 951–955. [Google Scholar] [CrossRef] [PubMed]
- Xiang, D.X.; Chen, Q.; Pang, L.; Zheng, C. long Inhibitory Effects of Silver Nanoparticles on H1N1 Influenza A Virus in Vitro. J. Virol. Methods 2011, 178, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Maduray, K.; Parboosing, R. Metal Nanoparticles: A Promising Treatment for Viral and Arboviral Infections. Biol. Trace Elem. Res. 2020, 199, 3159–3176. [Google Scholar] [CrossRef] [PubMed]
- De Toledo, G.G.; Toledo, V.H.; Lanfredi, A.J.C.; Escote, M.; Champi, A.; DA SILVA, M.C.C.; Nantes-Cardoso, I.L. Promising Nanostructured Materials against Enveloped Virus. An. Acad. Bras. Cienc. 2020, 92, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Aallaei, M.; Molaakbari, E.; Mostafavi, P.; Salarizadeh, N.; Malaksah, R.E.; Afzali, D. Investigation of Cu Metal Nanoparticles with Different Morphologies to Inhibit SARS-CoV-2 Main Protease and Spike Glycoprotein Using Molecular Docking and Dynamics Simulation. J. Mol. Struct. 2022, 1253, 132301. [Google Scholar] [CrossRef] [PubMed]
- Rani, I.; Goyal, A.; Bhatnagar, M.; Manhas, S.; Goel, P.; Pal, A.; Prasad, R. Potential Molecular Mechanisms of Zinc- and Copper-Mediated Antiviral Activity on COVID-19. Nutr. Res. 2021, 92, 109–128. [Google Scholar] [CrossRef]
- Karlsson, H.; Toprak, M.S.; Fadeel, B. Toxicity of Metal and Metal Oxide Nanoparticles. In Handbook on the Toxicology of Metals; Elsevier: Amsterdam, The Netherlands, 2015; pp. 75–112. ISBN 9780444594532. [Google Scholar]
- Cronholm, P.; Karlsson, H.L.; Hedberg, J.; Lowe, T.A.; Winnberg, L.; Elihn, K.; Wallinder, I.O.; Möller, L. Intracellular Uptake and Toxicity of Ag and CuO Nanoparticles: A Comparison between Nanoparticles and Their Corresponding Metal Ions. Small 2013, 9, 970–982. [Google Scholar] [CrossRef]
- Kubo, A.L.; Capjak, I.; Vrček, I.V.; Bondarenko, O.M.; Kurvet, I.; Vija, H.; Ivask, A.; Kasemets, K.; Kahru, A. Antimicrobial Potency of Differently Coated 10 and 50 nm Silver Nanoparticles against Clinically Relevant Bacteria Escherichia Coli and Staphylococcus Aureus. Colloids Surf. B Biointerfaces 2018, 170, 401–410. [Google Scholar] [CrossRef]
- Gupta, A.; Mumtaz, S.; Li, C.; Hussain, I.; Vincent, M.R. Combatting Antibiotic-Resistant Bacteria Using Nanomaterials. Chem. Soc. Rev. 2020, 48, 415–427. [Google Scholar] [CrossRef]
- Hodek, J.; Zajícová, V.; Lovetinská-Šlamborová, I.; Stibor, I.; Müllerová, J.; Weber, J. Protective Hybrid Coating Containing Silver, Copper and Zinc Cations Effective against Human Immunodeficiency Virus and Other Enveloped Viruses. BMC Microbiol. 2016, 16, 56. [Google Scholar] [CrossRef]
- Warnes, S.L.; Little, Z.R.; Keevil, C.W. Human Coronavirus 229E Remains Infectious on Common Touch Surface Materials. MBio 2015, 6, e01697-15. [Google Scholar] [CrossRef] [PubMed]
- Michels, H.T.; Keevil, C.W.; Salgado, C.D.; Schmidt, M.G. From Laboratory Research to a Clinical Trial: Copper Alloy Surfaces Kill Bacteria and Reduce Hospital-Acquired Infections. Health Environ. Res. Des. J. 2015, 9, 64–79. [Google Scholar] [CrossRef] [PubMed]
- Balasubramaniam, B.; Prateek; Ranjan, S.; Saraf, M.; Kar, P.; Singh, S.P.; Thakur, V.K.; Singh, A.; Gupta, R.K. Antibacterial and Antiviral Functional Materials: Chemistry and Biological Activity toward Tackling COVID-19-like Pandemics. ACS Pharmacol. Transl. Sci. 2021, 4, 8–54. [Google Scholar] [CrossRef] [PubMed]
- Palza, H. Antimicrobial Polymers with Metal Nanoparticles. Int. J. Mol. Sci. 2015, 16, 2099–2116. [Google Scholar] [CrossRef]
- Aragaw, T.A. Surgical Face Masks as a Potential Source for Microplastic Pollution in the COVID-19 Scenario. Mar. Pollut. Bull. 2020, 159, 111517. [Google Scholar] [CrossRef]
- The University of British Columbia What Size Particle Is Important to Transmission of COVID-19? Available online: https://www.aerosol.mech.ubc.ca/what-size-particle-is-important-to-transmission (accessed on 22 June 2022).
- Mills, K. 4—Measurement and Estimation of Physical Properties of Metals at High Temperatures. Fundam. Metall. 2005, 109–177. [Google Scholar] [CrossRef]
- Kubo, A.L.; Vasiliev, G.; Vija, H.; Krishtal, J.; Tõugu, V.; Visnapuu, M.; Kisand, V.; Kahru, A.; Bondarenko, O.M. Surface Carboxylation or PEGylation Decreases CuO Nanoparticles’ Cytotoxicity to Human Cells in Vitro without Compromising Their Antibacterial Properties. Arch. Toxicol. 2020, 94, 1561–1573. [Google Scholar] [CrossRef]
- Ivask, A.; Bondarenko, O.; Jepihhina, N.; Kahru, A. Profiling of the Reactive Oxygen Species-Related Ecotoxicity of CuO, ZnO, TiO2, Silver and Fullerene Nanoparticles Using a Set of Recombinant Luminescent Escherichia Coli Strains: Differentiating the Impact of Particles and Solubilised Metals. Anal. Bioanal. Chem. 2010, 398, 701–716. [Google Scholar] [CrossRef]
- Zhao, Z.; Cui, H.; Song, W.; Ru, X.; Zhou, W.; Yu, X. A Simple Magnetic Nanoparticles-Based Viral RNA Extraction Method for Efficient Detection of SARS-CoV-2. bioRxiv 2020, 518055. [Google Scholar] [CrossRef]
- Chen, Y.; Qiu, Y.; Chen, W.; Wei, Q. Electrospun Thymol-Loaded Porous Cellulose Acetate Fibers with Potential Biomedical Applications. Mater. Sci. Eng. C 2020, 109, 110536. [Google Scholar] [CrossRef]
- Pu, Y.; Zheng, J.; Chen, F.; Long, Y.; Wu, H.; Li, Q.; Yu, S.; Wang, X.; Ning, X. Preparation of Polypropylene Micro and Nanofibers by Electrostatic-Assisted Melt Blown and Their Application. Polymers 2018, 10, 959. [Google Scholar] [CrossRef] [PubMed]
- Lishchynskyi, O.; Shymborska, Y.; Stetsyshyn, Y.; Raczkowska, J.; Skirtach, A.G.; Peretiatko, T.; Budkowski, A. Passive Antifouling and Active Self-Disinfecting Antiviral Surfaces. Chem. Eng. J. 2022, 446, 137048. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, M.; Beyrer, C.; Goosby, E. Masks Do More Than Protect Others During COVID-19: Reducing the Inoculum of SARS-CoV-2 to Protect the Wearer. J. Gen. Intern. Med. 2020, 35, 3063–3066. [Google Scholar] [CrossRef] [PubMed]
- Roberts, K.L.; Shelton, H.; Stilwell, P.; Barclay, W.S. Transmission of a 2009 H1N1 Pandemic Influenza Virus Occurs before Fever Is Detected, in the Ferret Model. PLoS ONE 2012, 7, e43303. [Google Scholar] [CrossRef]
- Selvaranjan, K.; Navaratnam, S.; Rajeev, P.; Ravintherakumaran, N. Environmental Challenges Induced by Extensive Use of Face Masks during COVID-19: A Review and Potential Solutions. Environ. Chall. 2021, 3, 100039. [Google Scholar] [CrossRef]
- Suetens, C.; Hopkins, S.; Kolman, J.; Högberg, L.D. European Centre for Disease Prevention and Control. Point Prevalence Survey of Healthcare- Associated Infections and Antimicrobial Use in European Acute Care Hospitals; ECDC: Stockholm, Swden, 2013. [Google Scholar]
- Kampf, G.; Todt, D.; Pfaender, S.; Steinmann, E. Persistence of Coronaviruses on Inanimate Surfaces and Their Inactivation with Biocidal Agents. J. Hosp. Infect. 2020, 104, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Oxford, J.; Berezin, E.N.; Courvalin, P.; Dwyer, D.E.; Exner, M.; Jana, L.A.; Kaku, M.; Lee, C.; Letlape, K.; Low, D.E.; et al. The Survival of Influenza A(H1N1)Pdm09 Virus on 4 Household Surfaces. Am. J. Infect. Control. 2014, 42, 423–425. [Google Scholar] [CrossRef]
- Merkl, P.; Long, S.; McInerney, G.M.; Sotiriou, G.A. Antiviral Activity of Silver, Copper Oxide and Zinc Oxide Nanoparticle Coatings against SARS-CoV-2. Nanomaterials 2021, 11, 1312. [Google Scholar] [CrossRef]
- Meister, T.L.; Fortmann, J.; Breisch, M.; Sengstock, C.; Steinmann, E.; Köller, M.; Pfaender, S.; Ludwig, A. Nanoscale Copper and Silver Thin Film Systems Display Differences in Antiviral and Antibacterial Properties. Sci. Rep. 2022, 12, 1–10. [Google Scholar] [CrossRef]
- Balkrishna, A.; Arya, V.; Rohela, A.; Kumar, A.; Verma, R.; Kumar, D.; Nepovimova, E.; Kuca, K.; Thakur, N.; Thakur, N.; et al. Nanotechnology Interventions in the Management of COVID-19: Prevention, Diagnosis and Virus-Like Particle Vaccines. Vaccines 2021, 9, 1129. [Google Scholar] [CrossRef]
- Lemire, J.A.; Harrison, J.J.; Turner, R.J. Antimicrobial Activity of Metals: Mechanisms, Molecular Targets and Applications. Nat. Rev. Microbiol. 2013, 11, 371–384. [Google Scholar] [CrossRef]
- Ghaffari, H.; Tavakoli, A.; Moradi, A.; Tabarraei, A.; Bokharaei-Salim, F.; Zahmatkeshan, M.; Farahmand, M.; Javanmard, D.; Kiani, S.J.; Esghaei, M.; et al. Inhibition of H1N1 Influenza Virus Infection by Zinc Oxide Nanoparticles: Another Emerging Application of Nanomedicine. J. Biomed. Sci. 2019, 26, 70. [Google Scholar] [CrossRef] [PubMed]
- Borkow, G.; Zhou, S.S.; Page, T.; Gabbay, J. A Novel Anti-Influenza Copper Oxide Containing Respiratory Face Mask. PLoS ONE 2010, 5, e11295. [Google Scholar] [CrossRef] [PubMed]
- Imai, K.; Ogawa, H.; Bui, V.N.; Inoue, H.; Fukuda, J.; Ohba, M.; Yamamoto, Y.; Nakamura, K. Inactivation of High and Low Pathogenic Avian Influenza Virus H5 Subtypes by Copper Ions Incorporated in Zeolite-Textile Materials. Antivir. Res. 2012, 93, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Ito, A.; Tsuneki, A.; Yoshida, Y.; Ryoke, K.; Kaidoh, T.; Kageyama, S. In Vitro Inhibition of Cytopathic Effect of Influenza Virus and Human Immunodeficiency Virus by Bamboo Leaf Extract Solution and Sodium Copper Chlorophyllin. Yonago Acta Med. 2016, 59, 61–65. [Google Scholar]
- Minoshima, M.; Lu, Y.; Kimura, T.; Nakano, R.; Ishiguro, H.; Kubota, Y.; Hashimoto, K.; Sunada, K. Comparison of the Antiviral Effect of Solid-State Copper and Silver Compounds. J. Hazard. Mater. 2016, 312, 1–7. [Google Scholar] [CrossRef]
- Cortes, A.A.; Zuñiga, J.M. The Use of Copper to Help Prevent Transmission of SARS-Coronavirus and Influenza Viruses. A General Review. Diagn. Microbiol. Infect. Dis. 2020, 98, 115176. [Google Scholar] [CrossRef]
- Zerbib, S.; Vallet, L.; Muggeo, A.; De Champs, C.; Lefebvre, A.; Jolly, D.; Kanagaratnam, L. Copper for the Prevention of Outbreaks of Healthcare-Associated Infections in a Long-Term Care Facility for Elders. J. Post Acute Long Term Care Med. 2020, 21, 68–71.e1. [Google Scholar] [CrossRef]
- Shionoiri, N.; Sato, T.; Fujimori, Y.; Nakayama, T.; Nemoto, M.; Matsunaga, T.; Tanaka, T. Investigation of the Antiviral Properties of Copper Iodide Nanoparticles against Feline Calicivirus. J. Biosci. Bioeng. 2012, 113, 580–586. [Google Scholar] [CrossRef]
- Govind, V.; Bharadwaj, S.; Sai Ganesh, M.R.; Vishnu, J.; Shankar, K.V.; Shankar, B.; Rajesh, R. Antiviral Properties of Copper and Its Alloys to Inactivate COVID-19 Virus: A Review. BioMetals 2021, 34, 1217–1235. [Google Scholar] [CrossRef]
- Konai, M.M.; Bhattacharjee, B.; Ghosh, S.; Haldar, J. Recent Progress in Polymer Research to Tackle Infections and Antimicrobial Resistance. Biomacromolecules 2018, 19, 1888–1917. [Google Scholar] [CrossRef]
- Kamaruzzaman, N.F.; Tan, L.P.; Hamdan, R.H.; Choong, S.S.; Wong, W.K.; Gibson, A.J.; Chivu, A.; De Fatima Pina, M. Antimicrobial Polymers: The Potential Replacement of Existing Antibiotics? Int. J. Mol. Sci. 2019, 20, 2747. [Google Scholar] [CrossRef]
- Fischer, S.; Thümmler, K.; Volkert, B.; Hettrich, K.; Schmidt, I.; Fischer, K. Properties and Applications of Cellulose Acetate. Macromol. Symp. 2008, 262, 89–96. [Google Scholar] [CrossRef]
- Cheng, H.N.; Dowd, M.K.; Selling, G.W.; Biswas, A. Synthesis of Cellulose Acetate from Cotton Byproducts. Carbohydr. Polym. 2010, 80, 449–452. [Google Scholar] [CrossRef]
- Hansen, G.H.; Delmas, B.; Besnardeau, L.; Vogel, L.K.; Laude, H.; Sjöström, H.; Norén, O. The Coronavirus Transmissible Gastroenteritis Virus Causes Infection after Receptor-Mediated Endocytosis and Acid-Dependent Fusion with an Intracellular Compartment. J. Virol. 1998, 72, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Marchese, A.; Orhan, I.E.; Daglia, M.; Barbieri, R.; Di Lorenzo, A.; Nabavi, S.F.; Gortzi, O.; Izadi, M.; Nabavi, S.M. Antibacterial and Antifungal Activities of Thymol: A Brief Review of the Literature. Food Chem. 2016, 210, 402–414. [Google Scholar] [CrossRef]
- Kuroda, K.; Caputo, G.A.; DeGrado, W.F. The Role of Hydrophobicity in the Antimicrobial and Hemolytic Activities of Polymethacrylate Derivatives. Chem. A Eur. J. 2009, 15, 1123–1133. [Google Scholar] [CrossRef]
- Ahmed, F.; Ayoub Arbab, A.; Jatoi, A.W.; Khatri, M.; Memon, N.; Khatri, Z.; Kim, I.S. Ultrasonic-Assisted Deacetylation of Cellulose Acetate Nanofibers: A Rapid Method to Produce Cellulose Nanofibers. Ultrason. Sonochem. 2017, 36, 319–325. [Google Scholar] [CrossRef]
- Mikaeili, F.; Gouma, P.I. Super Water-Repellent Cellulose Acetate Mats. Sci. Rep. 2018, 8, 12472. [Google Scholar] [CrossRef]
- Pham, P.; Oliver, S.; Wong, E.H.H.; Boyer, C. Effect of Hydrophilic Groups on the Bioactivity of Antimicrobial Polymers. Polym. Chem. 2021, 12, 5689–5703. [Google Scholar] [CrossRef]
- Kumar, S.; Karmacharya, M.; Joshi, S.R.; Gulenko, O.; Park, J.; Kim, G.H.; Cho, Y.K. Photoactive Antiviral Face Mask with Self-Sterilization and Reusability. Nano Lett. 2021, 21, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, M.A.; Shuvho, M.B.A.; Shahid, A.; Haque, M.M.; Kashem, A.M.; Shiung, L.S.; Ong, H.C.; Uddin, A.; Mofijur, M. Prospect of Biobased Antiviral Face Mask to Limit the Coronavirus Outbreak. Environ. Res. 2021, 192, 110294. [Google Scholar] [CrossRef]
- Jung, S.; Byeon, E.Y.; Kim, D.G.; Lee, D.G.; Ryoo, S.; Lee, S.; Shin, C.W.; Jang, H.W.; Yang, J.Y.; Kim, H.J.; et al. Copper-Coated Polypropylene Filter Face Mask with SARS-CoV-2 Antiviral Ability. Polymers 2021, 13, 1367. [Google Scholar] [CrossRef] [PubMed]
- Selwyn, G.S.; Ye, C.; Bradfute, S.B. Anti-SARS-CoV-2 Activity of Surgical Masks Infused with Quaternary Ammonium Salts. Viruses 2021, 13, 960. [Google Scholar] [CrossRef] [PubMed]
- Blinova, I.; Niskanen, J.; Kajankari, P.; Kanarbik, L.; Käkinen, A.; Tenhu, H.; Kahru, A. Toxicity of two types of silver nanoparticles to aquatic crustaceans Daphnia magna and Thamnocephalus platyurus. Environ. Sci. Pollut. Res. 2013, 20, 3456–3463. [Google Scholar] [CrossRef] [PubMed]
| Substance | IC50 (mg/L) | ||
|---|---|---|---|
| Influenza A Virus | SARS-CoV-2 | TGEV | |
| CuSO4 | 1.40 | 0.45 | 4.44 |
| CuO | 49.25 | >100 | 383.4 |
| CuO-NH2 | 1.88 | 149.1 | 8.8 |
| CuO-COOH | 0.57 | 79.68 | 13.75 |
| ZnSO4 | 3.39 | 35.65 | ND |
| ZnO | 134.8 | ND | ND |
| AgNO3 | >100 | NA | >100 |
| Ag NP | >1000 | NA | NA |
| Samples | Mat Thickness | SEM Diameter | Air Permeability | Aerosol Filtration Efficiency, % | Aerosol Filtration Efficiency, % | Hydrophobic/ Hydrophilic Measuring | Contact Angle Measuring |
|---|---|---|---|---|---|---|---|
| mm | nm | Pa/cm2 | whole range 11.8–429.4 nm | 300 nm | ° | ||
| CA | 0.051 | 750 | 125.0 | 99.3 | 99.6 | hydrophobic | 104 |
| CA_7.5% CuSO4 | 0.062 | 972 | 54.1 | 84.3 | 85.5 | hydrophobic | 107 |
| CA_10% CuO | 0.163 | 759 | 47.4 | 78.4 | 81.6 | hydrophobic | 99 |
| CA_thymol | 0.036 | 545 | 45.4 | ND * | ND | hydrophilic | 82 |
| CA_thymol_7.5% CuSO4 | ND | 431 | 55.9 | ND | ND | hydrophilic | 86 |
| Fiber Material | Cu Content, % | Released Cu Content, 1 h, % |
|---|---|---|
| CA | 0 | ND |
| CA_7.5%CuSO4 | 4.68 ± 1.1 | 46 |
| CA_10%CuO | 8.01 ± 0.39 | 0 |
| CA_thymol | 0 | ND |
| CA_thymol_7.5%CuSO4 | 7.38 ± 0.61 | 78 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kubo, A.-L.; Rausalu, K.; Savest, N.; Žusinaite, E.; Vasiliev, G.; Viirsalu, M.; Plamus, T.; Krumme, A.; Merits, A.; Bondarenko, O. Antibacterial and Antiviral Effects of Ag, Cu and Zn Metals, Respective Nanoparticles and Filter Materials Thereof against Coronavirus SARS-CoV-2 and Influenza A Virus. Pharmaceutics 2022, 14, 2549. https://doi.org/10.3390/pharmaceutics14122549
Kubo A-L, Rausalu K, Savest N, Žusinaite E, Vasiliev G, Viirsalu M, Plamus T, Krumme A, Merits A, Bondarenko O. Antibacterial and Antiviral Effects of Ag, Cu and Zn Metals, Respective Nanoparticles and Filter Materials Thereof against Coronavirus SARS-CoV-2 and Influenza A Virus. Pharmaceutics. 2022; 14(12):2549. https://doi.org/10.3390/pharmaceutics14122549
Chicago/Turabian StyleKubo, Anna-Liisa, Kai Rausalu, Natalja Savest, Eva Žusinaite, Grigory Vasiliev, Mihkel Viirsalu, Tiia Plamus, Andres Krumme, Andres Merits, and Olesja Bondarenko. 2022. "Antibacterial and Antiviral Effects of Ag, Cu and Zn Metals, Respective Nanoparticles and Filter Materials Thereof against Coronavirus SARS-CoV-2 and Influenza A Virus" Pharmaceutics 14, no. 12: 2549. https://doi.org/10.3390/pharmaceutics14122549
APA StyleKubo, A.-L., Rausalu, K., Savest, N., Žusinaite, E., Vasiliev, G., Viirsalu, M., Plamus, T., Krumme, A., Merits, A., & Bondarenko, O. (2022). Antibacterial and Antiviral Effects of Ag, Cu and Zn Metals, Respective Nanoparticles and Filter Materials Thereof against Coronavirus SARS-CoV-2 and Influenza A Virus. Pharmaceutics, 14(12), 2549. https://doi.org/10.3390/pharmaceutics14122549






