Hyaluronic Acid Coating Reduces the Leakage of Melittin Encapsulated in Liposomes and Increases Targeted Delivery to Melanoma Cells
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials and Regents
2.2. Cell Line
2.3. Melittin Detection
2.4. Preparation and Optimization of Melittin-Loaded Liposomes (Mel-Lip)
2.4.1. Preparation of Mel-Lip
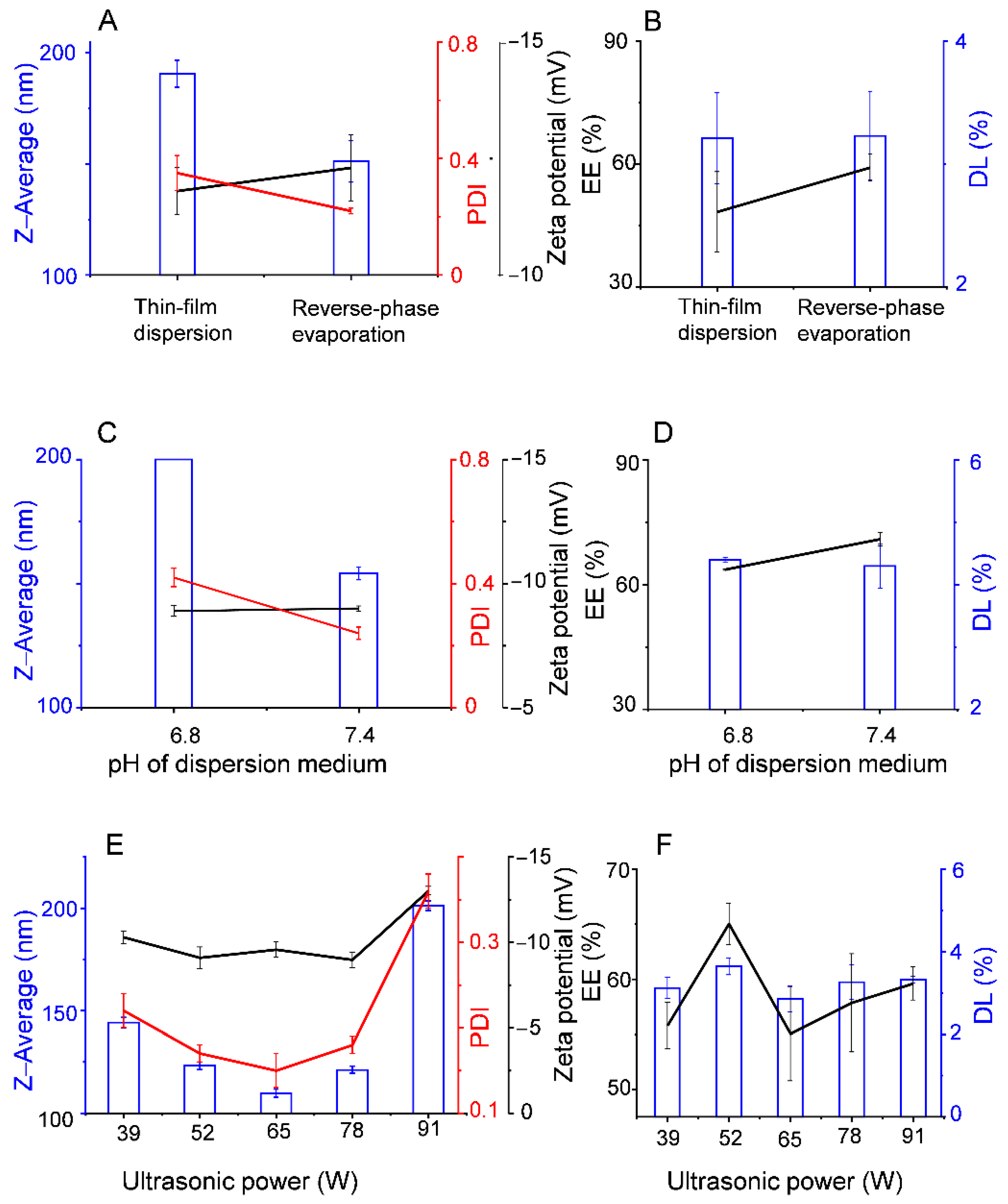
2.4.2. Optimization of Mel-Lip
2.5. Synthesis of HA-DOPE
2.6. Preparation of Mel-HA-Lip
2.7. Particle Size Distribution and Zeta Potential of Liposomes
2.8. DL and EE of Liposomes
2.9. Transmission Electron Microscopy (TEM)
2.10. Drug Release In Vitro
2.11. Cellular Uptake
2.12. Cellular Cytotoxicity
2.13. Statistical Analysis
3. Results
3.1. Preparation of Mel-Lip
3.2. Preparation of HA-Mel-Lip
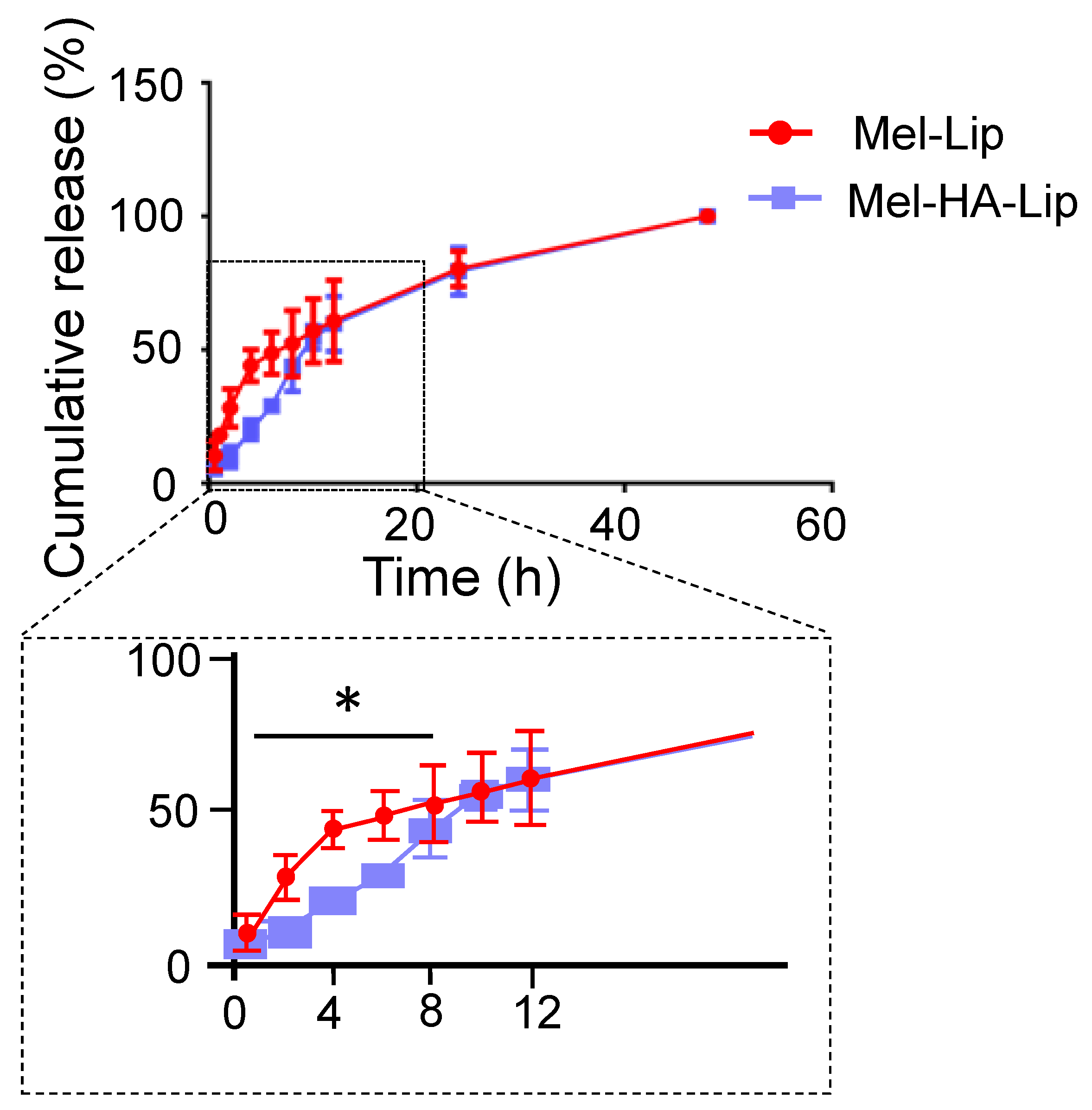
3.3. Drug Release In Vitro
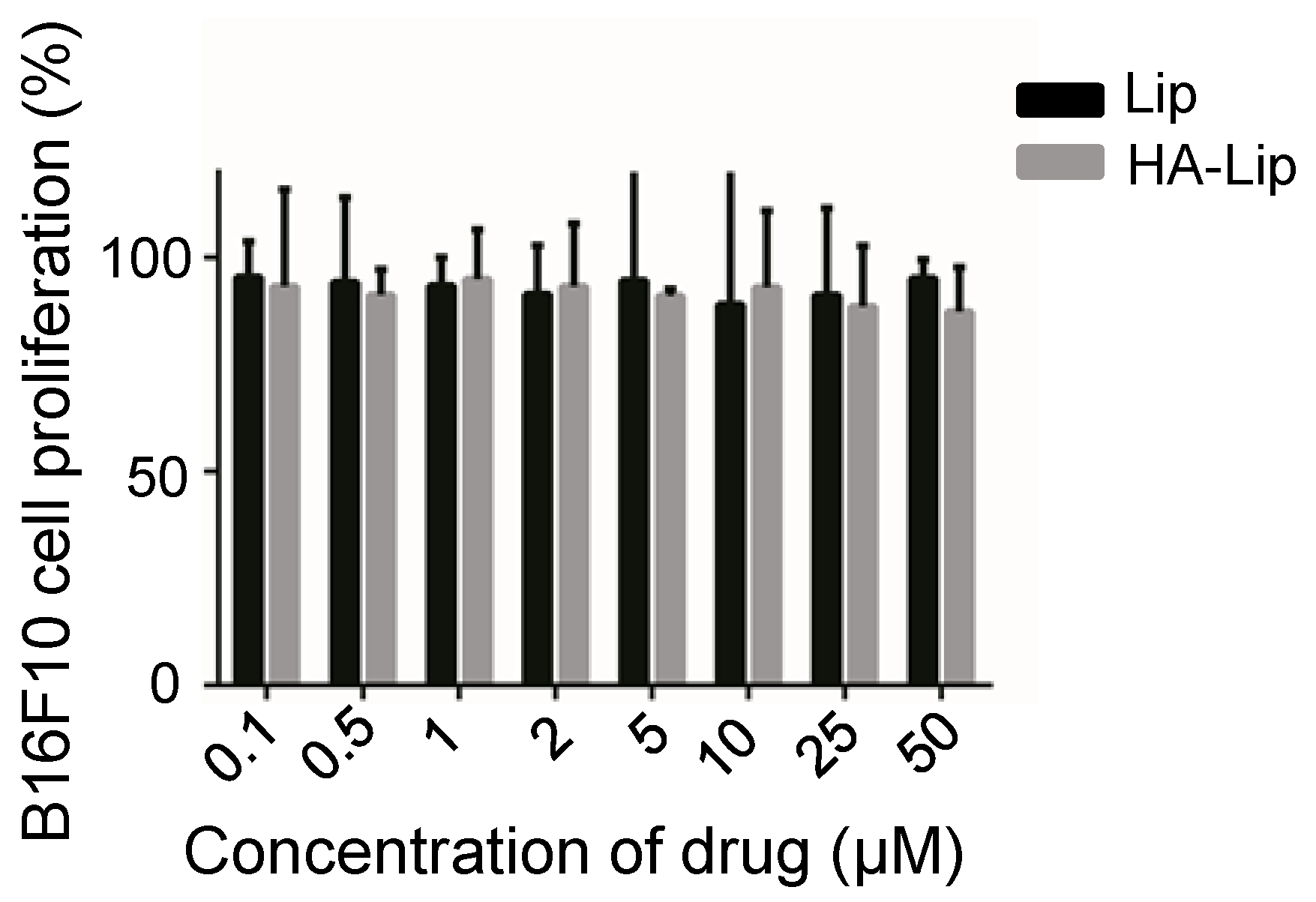
3.4. In Vitro Evaluation of Anti-Tumor Activity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, W.; Zheng, R.; Baade, P.; Zhang, S.; Zeng, H.; Bray, F.; Jemal, A.; Yu, X.Q.; He, J. Cancer statistics in China, 2015. CA A Cancer J. Clin. 2016, 66, 115–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Li, Q.; Zhang, J.; Huang, L.; Qi, C.; Xu, L.; Liu, X.; Wang, G.; Wang, L.; Wang, Z. Safe and Effective Reversal of Cancer Multidrug Resistance Using Sericin-Coated Mesoporous Silica Nanoparticles for Lysosome-Targeting Delivery in Mice. Small 2017, 13, 1602567. [Google Scholar] [CrossRef]
- Chen, H.; Chen, W.-Q.; Que, H.-Q.; Li, W.; Ma, Z.-J.; Lin, S. Research progress on drugs for treatment of nasopharyngeal carcinoma. Drugs Clinic. 2017, 32, 747–751. [Google Scholar]
- Tang, Z.H.; Lu, J.J. Osimertinib resistance in non-small cell lung cancer: Mechanisms and therapeutic strategies. Cancer Lett. 2018, 420, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Rady, I.; Siddiqui, I.A.; Rady, M.; Mukhtar, H. Melittin, a major peptide component of bee venom, and its conjugates in cancer therapy. Cancer Lett. 2017, 402, 16–31. [Google Scholar] [CrossRef] [Green Version]
- Son, D.J.; Lee, J.W.; Lee, Y.H.; Song, H.S.; Lee, C.K.; Hong, J.T. Therapeutic application of anti-arthritis, pain-releasing, and anti-cancer effects of bee venom and its constituent compounds. Pharmacol. Ther. 2007, 115, 246–270. [Google Scholar] [CrossRef]
- Liu, C.-C.; Hao, D.; Zhang, Q.; An, J.; Zhao, J.-J.; Chen, B.; Zhang, L.-L.; Yang, H. Application of bee venom and its main constituent melittin for cancer treatment. Cancer Chemother. Pharmacol. 2016, 78, 1113–1130. [Google Scholar] [CrossRef]
- Habermann, E. Bee and wasp venoms. Science 1972, 177, 314–322. [Google Scholar] [CrossRef]
- Lv, C.; Zhang, Z.; Zhao, T.; Han, M.-F.; Jia, D.-P.; Su, L.-Z.; Huang, F.; Wang, F.-Z.; Fang, F.-F.; Li, B. The anti-tumour effect of Mel and its role in autophagy in human hepatocellular carcinoma cells. Am. J. Transl. Res. 2019, 11, 931–941. [Google Scholar]
- Lyu, C.; Fang, F.; Li, B. Anti-Tumor Effects of Melittin and Its Potential Applications in Clinic. Curr. Protein Pept. Sci. 2019, 20, 240–250. [Google Scholar] [CrossRef] [PubMed]
- Oršolić, N. Possible Molecular Targets of Bee Venom in the Treatment of Cancer: Application and Perspectives. Forum Immunopathol. Dis. Ther. 2013, 4, 275–315. [Google Scholar] [CrossRef]
- Glattli, A.; Chandrasekhar, I.; van Gunsteren, W.F. A molecular dynamics study of the bee venom melittin in aqueous solution, in methanol, and inserted in a phospholipid bilayer. Eur. Biophys. J. 2006, 35, 255–267. [Google Scholar] [CrossRef] [Green Version]
- Kohno, M.; Horibe, T.; Ohara, K.; Ito, S.; Kawakami, K. The membrane-lytic peptides K8L9 and melittin enter cancer cells via receptor endocytosis following subcytotoxic exposure. Chem. Biol. 2014, 21, 1522–1532. [Google Scholar] [CrossRef] [Green Version]
- Kong, G.-M.; Tao, W.-H.; Diao, Y.-L.; Fang, P.-H.; Wang, J.-J.; Bo, P.; Qian, F. Melittin induces human gastric cancer cell apoptosis via activation of mitochondrial pathway. World J. Gastroenterol. 2016, 22, 3186–3195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jamasbi, E.; Batinovic, S.; Sharples, R.A.; Sani, M.-A.; Robins-Browne, R.; Wade, J.; Separovic, F.; Hossain, M.A. Melittin peptides exhibit different activity on different cells and model membranes. Amino Acids. 2014, 46, 2759–2766. [Google Scholar] [CrossRef] [PubMed]
- Mao, J.; Liu, S.; Ai, M.; Wang, Z.; Wang, D.; Li, X.; Hu, K.; Gao, X.; Yang, Y. A novel melittin nano-liposome exerted excellent anti-hepatocellular carcinoma efficacy with better biological safety. J. Hematol. Oncol. 2017, 10, 71. [Google Scholar] [CrossRef] [Green Version]
- Koide, H.; Suzuki, H.; Ochiai, H.; Egami, H.; Hamashima, Y.; Oku, N.; Asai, T. Enhancement of target toxin neutralization effect in vivo by PEGylation of multifunctionalized lipid nanoparticles. Biochem. Biophys. Res. Commun. 2021, 555, 32–39. [Google Scholar] [CrossRef]
- Gu, Z.; Da Silva, C.G.; Van der Maaden, K.; Ossendorp, F.; Cruz, L.J. Liposome-Based Drug Delivery Systems in Cancer Immunotherapy. Pharmaceutics 2020, 12, 1054. [Google Scholar] [CrossRef]
- Raghuraman, H.; Chattopadhyay, A. Interaction of melittin with membrane cholesterol: A fluorescence approach. Biophys. J. 2004, 87, 2419–2432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dosio, F.; Arpicco, S.; Stella, B.; Fattal, E. Hyaluronic acid for anticancer drug and nucleic acid delivery. Adv. Drug Deliv. Rev. 2016, 97, 204–236. [Google Scholar] [CrossRef]
- Bellei, B.; Caputo, S.; Migliano, E.; Lopez, G.; Marcaccini, V.; Cota, C.; Picardo, M. Simultaneous Targeting Tumor Cells and Cancer-Associated Fibroblasts with a Paclitaxel-Hyaluronan Bioconjugate: In Vitro Evaluation in Non-Melanoma Skin Cancer. Biomedicines 2021, 9, 597. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Yang, H.; Khan, A.R.; Yang, X.; Xu, J.; Ji, J.; Zhai, G. Redox-responsive hyaluronic acid-based nanoparticles for targeted photodynamic therapy/chemotherapy against breast cancer. J. Colloid Interface Sci. 2021, 598, 213–228. [Google Scholar] [CrossRef]
- Park, K.; Lee, M.Y.; Kim, K.S.; Hahn, S.K. Target specific tumor treatment by VEGF siRNA complexed with reducible polyethyleneimine-hyaluronic acid conjugate. Biomaterials 2010, 31, 5258–5265. [Google Scholar] [CrossRef]
- Naor, D.; Wallach-Dayan, S.B.; Zahalka, M.A.; Sionov, R.V. Involvement of CD44, a molecule with a thousand faces, in cancer dissemination. Semin. Cancer Biol. 2008, 18, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Koltai, T.; Reshkin, S.J.; Carvalho, T.M.A.; Cardone, R.A. Targeting the Stromal Pro-Tumoral Hyaluronan-CD44 Pathway in Pancreatic Cancer. Int. J. Mol. Sci. 2021, 22, 3953. [Google Scholar] [CrossRef]
- Surace, C.; Arpicco, S.; Dufaÿ-Wojcicki, A.; Marsaud, V.; Bouclier, C.; Clay, D.; Cattel, L.; Renoir, J.-M.; Fattal, E. Lipoplexes Targeting the CD44 Hyaluronic Acid Receptor for Efficient Transfection of Breast Cancer Cells. Mol. Pharm. 2009, 6, 1062–1073. [Google Scholar] [CrossRef] [PubMed]
- Eliaz, R.E.; Szoka, F.C. Liposome-encapsulated doxorubicin targeted to CD44: A strategy to kill CD44-overexpressing tumor cells. Cancer Res. 2001, 61, 2592–2601. [Google Scholar] [CrossRef]
- Cai, W.; Liu, J.; Zheng, L.; Xud, Z.; Chena, J.; Zhonga, J.; Songa, Z.; Xua, X.; Chena, S.; Jiaoa, C.; et al. Study on the anti-infection ability of vancomycin cationic liposome combined with polylactide fracture internal fixator. Int. J. Biol. Macromol. 2021, 167, 834–844. [Google Scholar] [CrossRef]
- Jing, W.; Li, G.; Yong, G.; Jingping, L. Preparation and characterization of hyaluronic acid-modified dexamethasone core-shell liponanoparticles. J. China Pharm. Univ. 2013, 44, 117–123. [Google Scholar]
- Zhang, Y.; Xia, Q.; Li, Y.; He, Z.; Li, Z.; Guo, T.; Wu, Z.; Feng, N. CD44 Assists the Topical Anti-Psoriatic Efficacy of Curcumin-Loaded Hyaluronan-Modified Ethosomes: A New Strategy for Clustering Drug in Inflammatory Skin. Theranostics 2019, 9, 48–64. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Liu, S.; Wan, J.; Yang, Q.; Xiang, Y.; Ni, L.; Long, Y.; Cui, M.; Ci, Z.; Tang, D.; et al. Preparation, Characterization and in vivo Study of Borneol-Baicalin-Liposomes for Treatment of Cerebral Ischemia-Reperfusion Injury. Int. J. Nanomed. 2020, 15, 5977–5989. [Google Scholar] [CrossRef]
- Wang, D.; Wang, Y.; Zhao, G.; Zhuang, J.; Wu, W. Improving systemic circulation of paclitaxel nanocrystals by surface hybridization of DSPE-PEG2000. Colloids Surf. B Biointerfaces 2019, 182, 110337. [Google Scholar] [CrossRef] [PubMed]
- Ravar, F.; Saadat, E.; Gholami, M.; Dehghankelishadi, P.; Mahdavi, M.; Azami, S.; Dorkoosh, F.A. Hyaluronic acid-coated liposomes for targeted delivery of paclitaxel, in-vitro characterization and in-vivo evaluation. J Control. Release 2016, 229, 10–22. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Cho, H.-J.; Yoon, H.Y.; Yoon, I.-S.; Ko, S.-H.; Shim, J.-S.; Cho, J.-H.; Park, J.H.; Kim, K.; Kwon, I.C.; et al. Hyaluronic acid derivative-coated nanohybrid liposomes for cancer imaging and drug delivery. J. Control. Release 2014, 174, 98–108. [Google Scholar] [CrossRef]
- Li, W.H.; Yi, X.L.; Liu, X.; Zhang, Z.R.; Fu, Y.; Gong, T. Hyaluronic acid ion-pairing nanoparticles for targeted tumor therapy. J. Control. Release 2016, 225, 170–182. [Google Scholar] [CrossRef]
- Liu, G.X.; Fang, G.Q.; Xu, W. Dual Targeting Biomimetic Liposomes for Paclitaxel/DNA Combination Cancer Treatment. Int. J. Mol. Sci. 2014, 15, 15287–15303. [Google Scholar] [CrossRef] [Green Version]
- Sangboonruang, S.; Kitidee, K.; Chantawannakul, P.; Tragoolpua, K.; Tragoolpua, Y. Melittin from Apis florea Venom as a Promising Therapeutic Agent for Skin Cancer Treatment. Antibiotics 2020, 9, 517. [Google Scholar] [CrossRef]






| Run | Factor | Mean Size (nm) | PDI | EE (%) | DL (%) | |
|---|---|---|---|---|---|---|
| x1 (mg/mL) | x2 (w/w) | |||||
| 1 | 0.5 | 1:15 | 126.2 | 0.19 | 86.01 | 4.11 |
| 2 | 1 | 1:25 | 136.4 | 0.21 | 91.86 | 2.00 |
| 3 | 1.5 | 1:10 | 125.4 | 0.21 | 77.89 | 4.62 |
| 4 | 2 | 1:20 | 135.9 | 0.21 | 92.18 | 2.64 |
| 5 | 2.5 | 1:30 | 152.8 | 0.22 | 96.92 | 1.70 |
| Formulation | Mean Size (nm) | PDI | Zeta Potential (mV) | EE (%) | DL (%) |
|---|---|---|---|---|---|
| Mel-Lip | 132.7 ± 1.55 | 0.23 ± 0.01 | −11.5 ± 1.51 | 86.25 ± 1.28 | 3.91 ± 0.49 |
| Mel-HA-Lip | 124.3 ± 8.93 | 0.19 ± 0.02 * | −12.4 ± 1.08 | 90.43 ± 0.41 ** | 4.46 ± 0.10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Ruan, S.; Wang, Z.; Feng, N.; Zhang, Y. Hyaluronic Acid Coating Reduces the Leakage of Melittin Encapsulated in Liposomes and Increases Targeted Delivery to Melanoma Cells. Pharmaceutics 2021, 13, 1235. https://doi.org/10.3390/pharmaceutics13081235
Li Y, Ruan S, Wang Z, Feng N, Zhang Y. Hyaluronic Acid Coating Reduces the Leakage of Melittin Encapsulated in Liposomes and Increases Targeted Delivery to Melanoma Cells. Pharmaceutics. 2021; 13(8):1235. https://doi.org/10.3390/pharmaceutics13081235
Chicago/Turabian StyleLi, Yanyan, Shuyao Ruan, Zhi Wang, Nianping Feng, and Yongtai Zhang. 2021. "Hyaluronic Acid Coating Reduces the Leakage of Melittin Encapsulated in Liposomes and Increases Targeted Delivery to Melanoma Cells" Pharmaceutics 13, no. 8: 1235. https://doi.org/10.3390/pharmaceutics13081235
APA StyleLi, Y., Ruan, S., Wang, Z., Feng, N., & Zhang, Y. (2021). Hyaluronic Acid Coating Reduces the Leakage of Melittin Encapsulated in Liposomes and Increases Targeted Delivery to Melanoma Cells. Pharmaceutics, 13(8), 1235. https://doi.org/10.3390/pharmaceutics13081235






