Multi-Analytical Framework to Assess the In Vitro Swallowability of Solid Oral Dosage Forms Targeting Patient Acceptability and Adherence
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Preparation of Tablet
2.2.2. Preparation and Characterization of Artificial Saliva
2.2.3. Film Coating Apparatus
2.2.4. Coating Solution Preparations
2.2.5. Multi-Analytical Framework to Assess In Vitro Swallowability
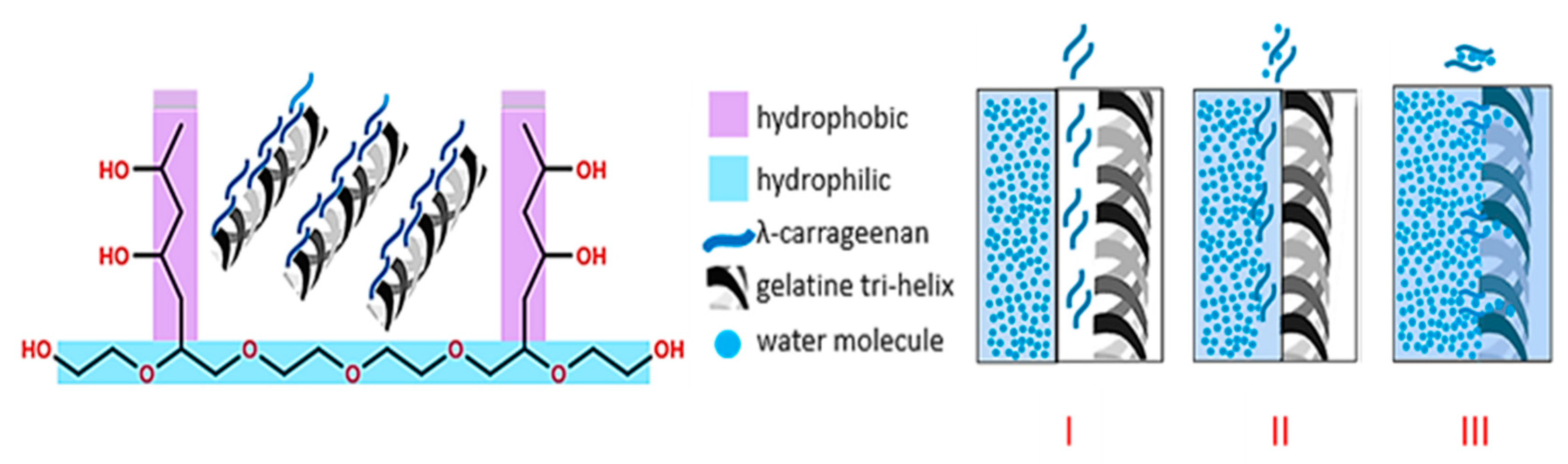
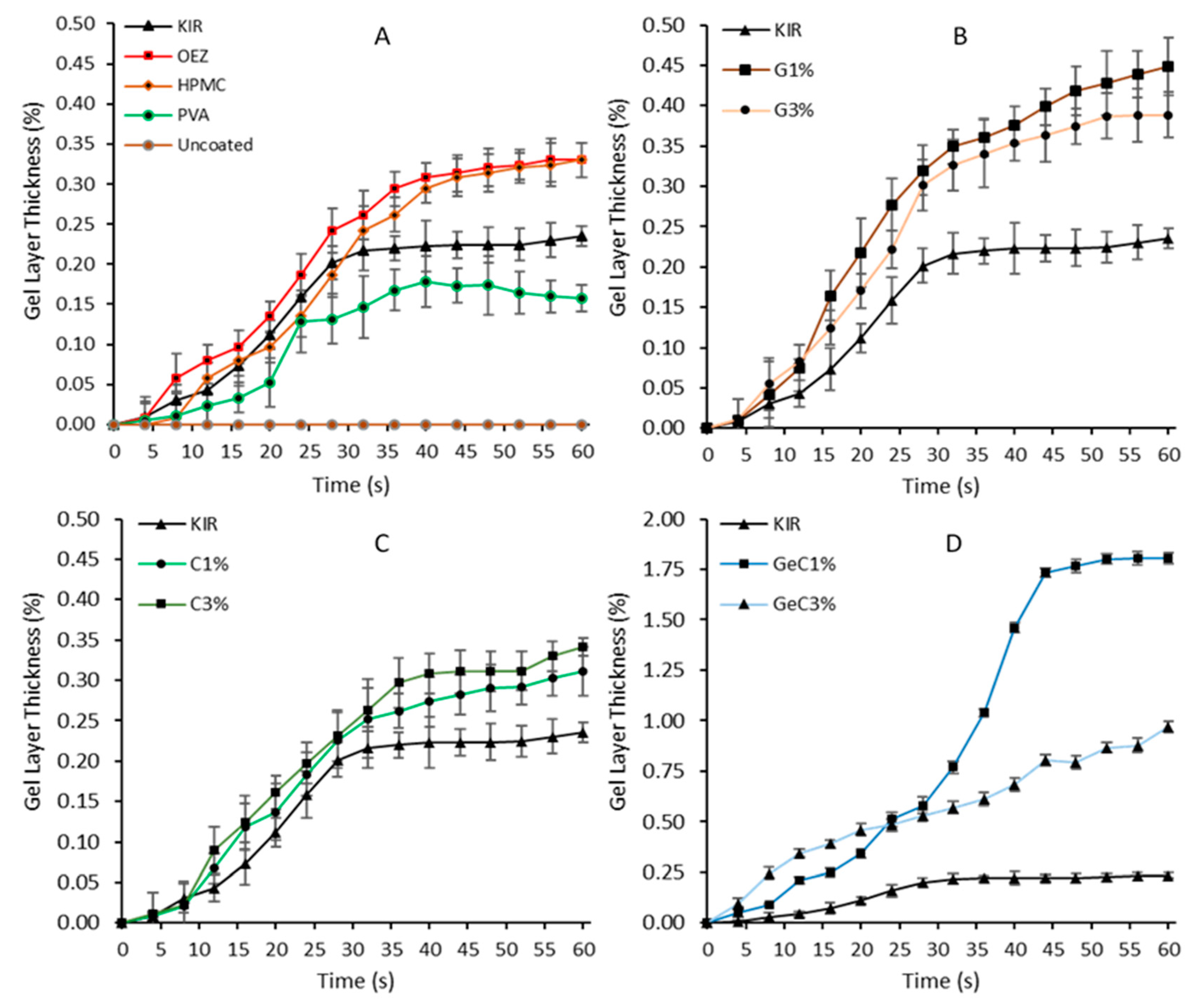
Change in Hydrated Film Coat Layer Thickness
In Vitro Wettability
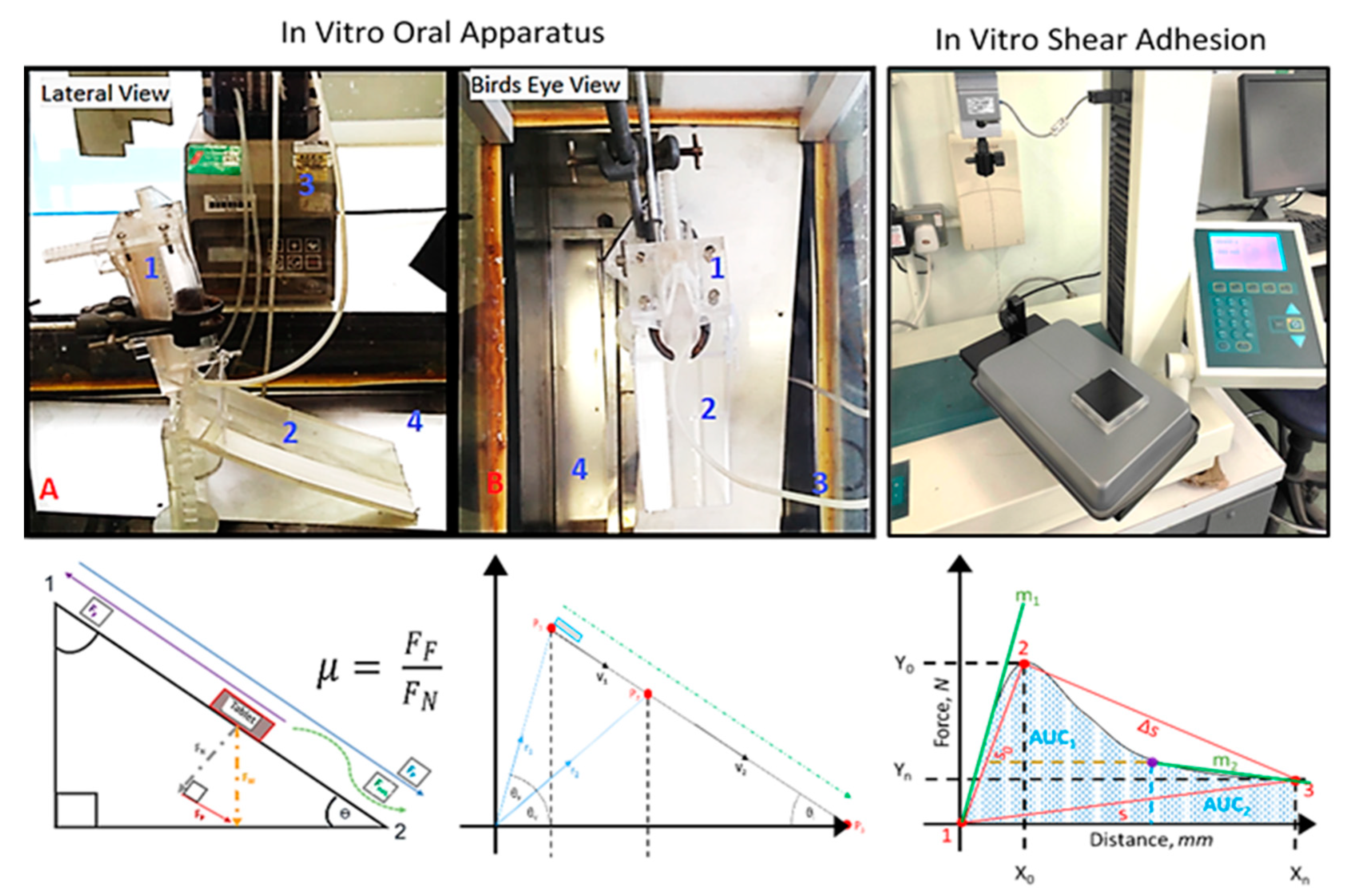
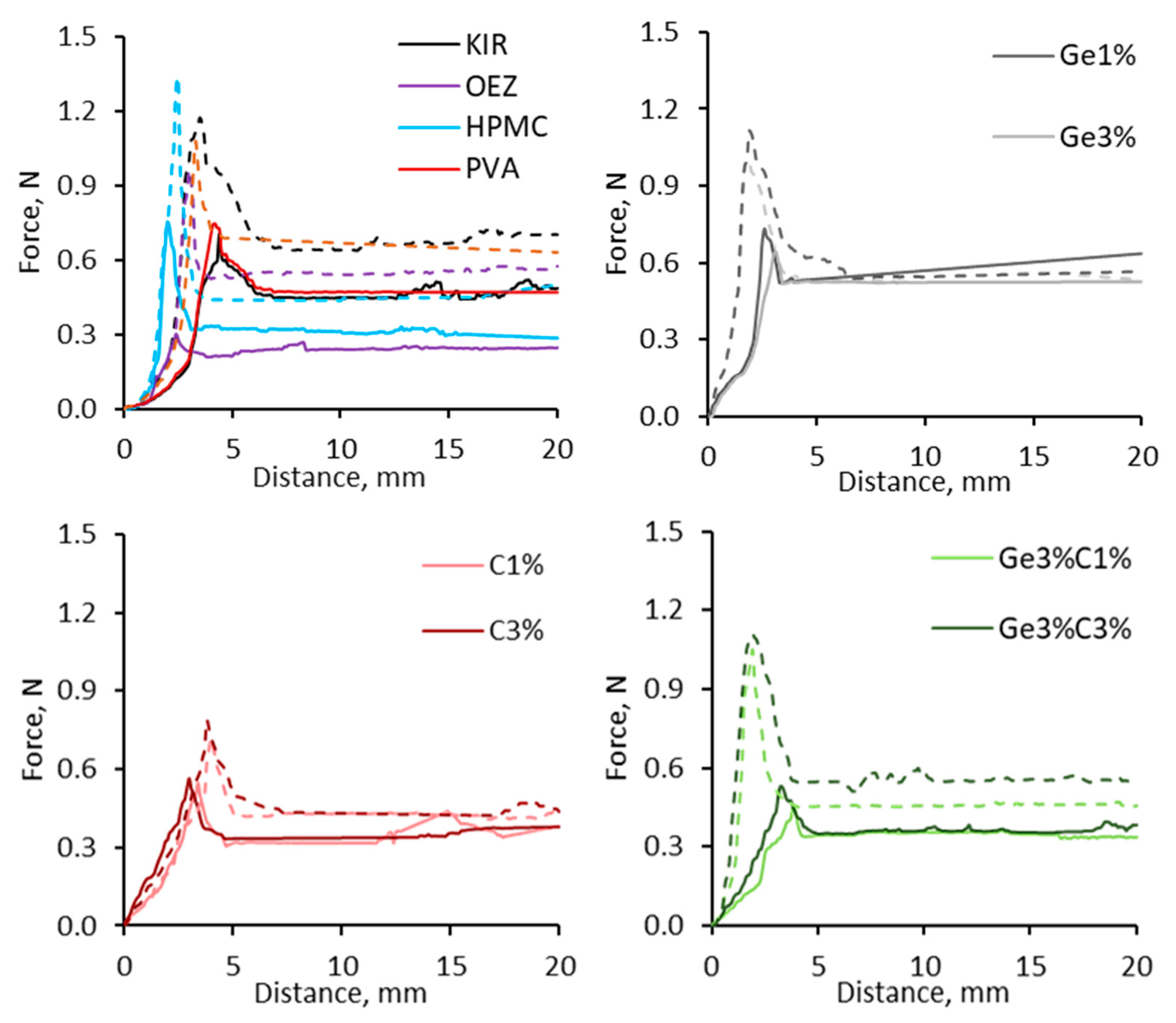
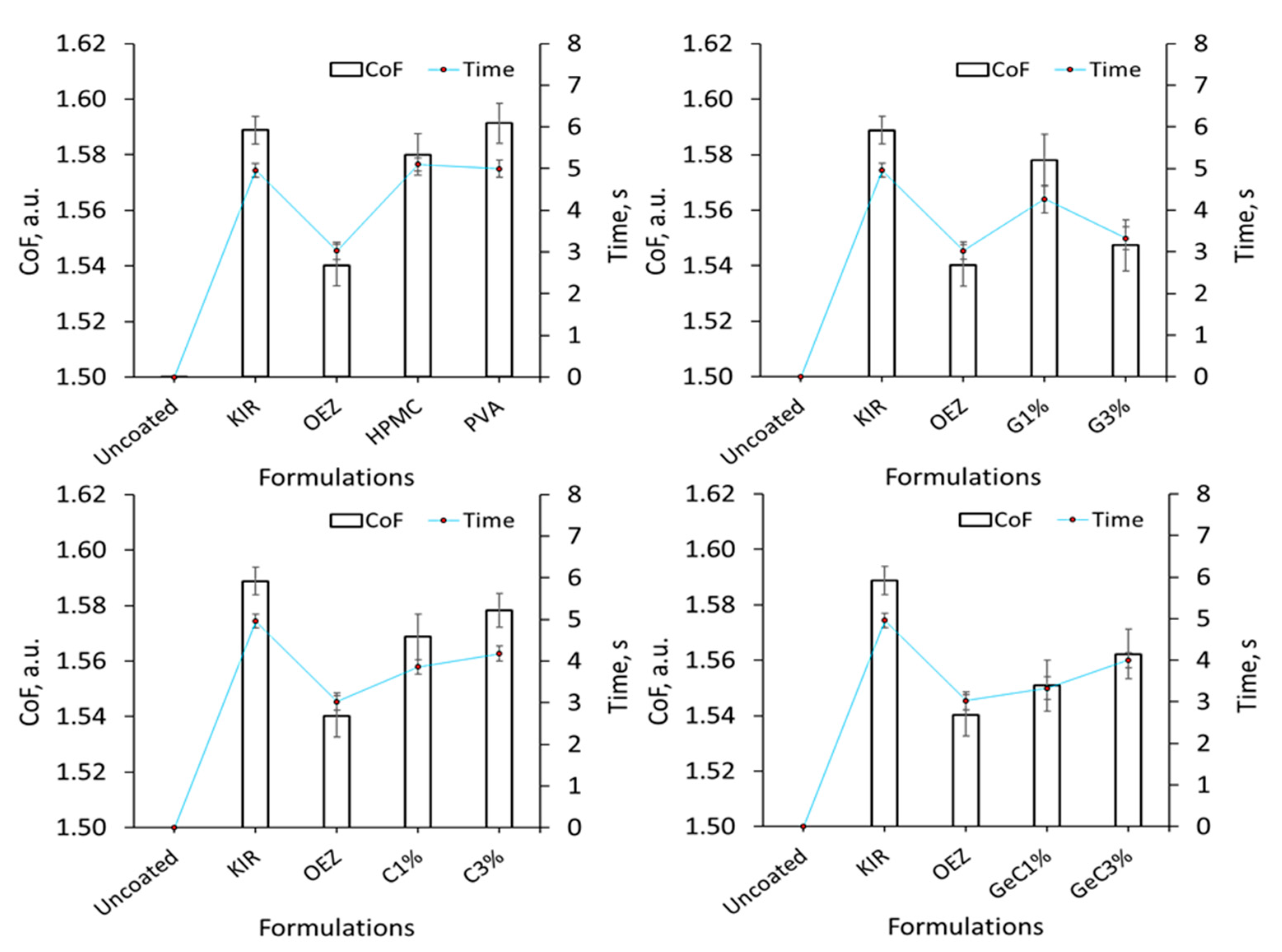
In Vitro Coefficient of Sliding Friction
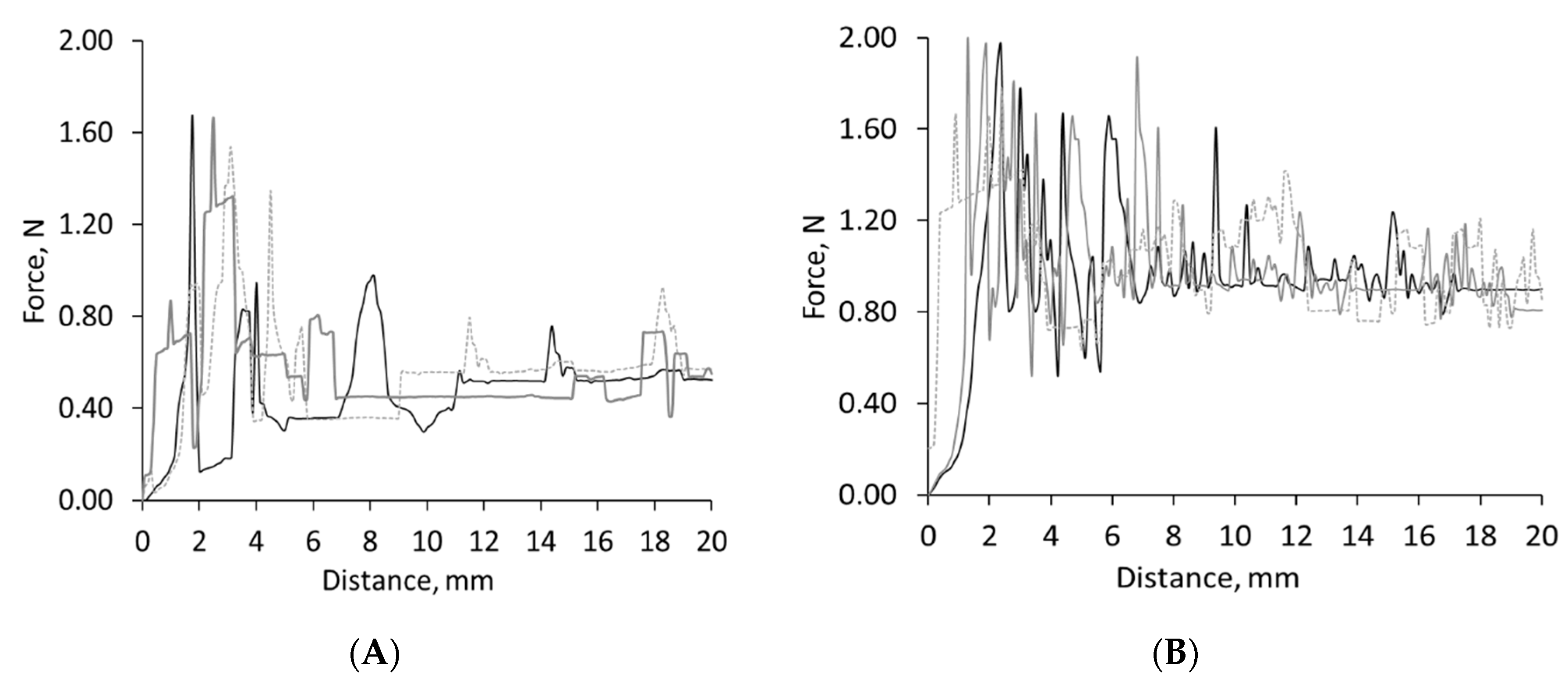
In Vitro Shear Adhesion
2.3. Statistical Analysis
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B
| Formulation | r2 |
|---|---|
| Uncoated | N/A |
| Kollicoat® IR | 0.99993 |
| Opadry® EZ | 0.97955 |
| PVA | 0.92344 |
| HPMC | 0.98178 |
| C 1% w/w | 0.92883 |
| C 3% w/w | 0.99932 |
| Ge 1% w/w | 0.99507 |
| Ge 3% w/w | 0.99842 |
| Ge 3%: C1% w/w | 0.99383 |
| Ge 3%: C3% w/w | 0.99089 |
Appendix C
References
- Cichero, J.A.Y. Age-Related Changes to Eating and Swallowing Impact Frailty: Aspiration, Choking Risk, Modified Food Texture and Autonomy of Choice. Geriatrics 2018, 3, 69. [Google Scholar] [CrossRef] [Green Version]
- Castell, D.O.; Donner, M.W. Evaluation of dysphagia: A careful history is crucial. Dysphagia 1987, 2, 65–71. [Google Scholar] [CrossRef]
- Harris Interactive Inc. Pill-Swallowing Problems in America: A National Survey of Adults; Harris Interactive Inc. for Schwarz Pharma: New York, NY, USA, 2003; Available online: http://healthymoments.com/downloads/40percent.doc (accessed on 17 March 2021).
- U.S. Food and Drug Administration (FDA). Guidance Document: Size, Shape, and Other Physical Attributes of Generic Tablets and Capsules, Center for Drug Evaluation and Research. 2015. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents (accessed on 18 January 2020).
- Badgujar, B.; Mundada, A. The technologies used for developing orally disintegrating tablets: A review. Acta Pharm. 2011, 61, 117–139. [Google Scholar] [CrossRef]
- Smithard, D. Dysphagia: Prevalence, Management and Side Effects, Nursing in Practice. 2015. Available online: https://www.nursinginpractice.com/article/dysphagia-prevalence-management-and-side-effects (accessed on 8 June 2018).
- Roden, D.F.; Altman, K.W. Causes of Dysphagia Among Different Age Groups: A Systematic Review of the Literature. Otolaryngol. Clin. N. Am. 2013, 46, 965–987. [Google Scholar] [CrossRef] [PubMed]
- Tho, I. Orally disintegrating tablets—Advantages and drawbacks. J. Nor. Med. Assoc. 2012, 132, 424–425. [Google Scholar] [CrossRef] [Green Version]
- Nagashree, K. Solid dosage forms: Tablets, Research & Reviews. J. Pharm. Anal. 2015, 4, 60–71. [Google Scholar]
- Pramod, K.; Abu Tahir, M.; Charoo, N.A.; Ansari, S.H.; Ali, J. Pharmaceutical product development: A quality by design approach. Int. J. Pharm. Investig. 2016, 6, 129–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shariff, Z.B.; Dahmash, D.T.; Kirby, D.J.; Missaghi, S.; Rajabi-Siahboomi, A.; Maidment, I.D. Does the Formulation of Oral Solid Dosage Forms Affect Acceptance and Adherence in Older Patients? A Mixed Methods Systematic Review. J. Am. Med Dir. Assoc. 2020, 21, 1015–1023.e8. [Google Scholar] [CrossRef] [Green Version]
- Shariff, Z.; Kirby, D.; Missaghi, S.; Rajabi-Siahboomi, A.; Maidment, I. Patient-Centric Medicine Design: Key Characteristics of Oral Solid Dosage Forms that Improve Adherence and Acceptance in Older People. Pharmaceutics 2020, 12, 905. [Google Scholar] [CrossRef]
- Perkins, A.C.; Wilson, C.G.; Frier, M.; Blackshaw, P.; Dansereau, R.J.; Vincent, R.M.; Wenderoth, D.; Hathaway, S.; Li, Z.; Spiller, R.C. The use of scintigraphy to demonstrate the rapid esophageal transit of the oval film-coated placebo risedronate tablet compared to a round uncoated placebo tablet when administered with minimal volumes of water. Int. J. Pharm. 2001, 222, 295–303. [Google Scholar] [CrossRef]
- Channer, K.S.; Virjee, J.P. The Effect of Size and Shape of Tablets on Their Esophageal Transit. J. Clin. Pharmacol. 1986, 26, 141–146. [Google Scholar] [CrossRef]
- Osmanoglou, E.; Van Der Voort, I.R.; Fach, K.; Kosch, O.; Bach, D.; Hartmann, V.; Strenzke, A.; Weitschies, W.; Wiedenmann, B.; Trahms, L.; et al. Oesophageal transport of solid dosage forms depends on body position, swallowing volume and pharyngeal propulsion velocity. Neurogastroenterol. Motil. 2004, 16, 547–556. [Google Scholar] [CrossRef]
- Overgaard, A.; Møller-Sonnergaard, J.; Christrup, L.; Højsted, J.; Hansen, R. Patients’ evaluation of shape, size and colour of solid dosage forms. Pharm. World Sci. 2001, 23, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Ankit, G.; Bilandi, A.; Kumar, K.M.; Neetu, K. Tablet Coating techniques: Concepts and recent trends. Int. Res. J. Pharm. 2012, 3, 50–58. [Google Scholar]
- Lopez, F.L.; Ernest, T.B.; Tuleu, C.; Gul, M.O. Formulation approaches to pediatric oral drug delivery: Benefits and limitations of current platforms. Expert Opin. Drug Deliv. 2015, 12, 1727–1740. [Google Scholar] [CrossRef] [PubMed]
- Wallingford, L.; Labuza, T.P. Evaluation of the Water Binding Properties of Food Hydrocolloids by Physical/Chemical Methods and in a Low Fat Meat Emulsion. J. Food Sci. 1983, 48, 1–5. [Google Scholar] [CrossRef]
- Doelker, E. Swelling Behavior of Water-Soluble Cellulose Derivatives. Stud. Polym. Sci. 1990, 8, 125–145. [Google Scholar] [CrossRef]
- Nguyen, P.T.; Kravchuk, O.; Bhandari, B.; Prakash, S. Effect of different hydrocolloids on texture, rheology, tribology and sensory perception of texture and mouthfeel of low-fat pot-set yoghurt. Food Hydrocoll. 2017, 72, 90–104. [Google Scholar] [CrossRef] [Green Version]
- Hofmanová, J.K.; Rajabi-Siahboomi, A.; Haque, S.; Mason, J.; Teckoe, J.; To, D.; Batchelor, H.K. Developing methodology to evaluate the oral sensory features of pharmaceutical tablet coatings. Int. J. Pharm. 2019, 562, 212–217. [Google Scholar] [CrossRef]
- Chen, J.; Lolivret, L. The determining role of bolus rheology in triggering a swallowing. Food Hydrocoll. 2011, 25, 325–332. [Google Scholar] [CrossRef]
- Yamamoto, S.; Taniguchi, H.; Hayashi, H.; Hori, K.; Tsujimura, T.; Nakamura, Y.; Sato, H.; Inoue, M. How do tablet properties influence swallowing behaviours? J. Pharm. Pharmacol. 2013, 66, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Peladeau-Pigeon, M.; Steele, C.M. Age-Related Variability in Tongue Pressure Patterns for Maximum Isometric and Saliva Swallowing Tasks. J. Speech Lang. Hear. Res. 2017, 60, 3177–3184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qazi, W.M.; Stading, M. In Vitro Models for Simulating Swallowing. In Radiation Oncology; Ekberg, O., Ed.; Springer: Cham, Switzerland, 2017; pp. 549–562. [Google Scholar]
- Cichero, J.A.Y.; Steele, C.M.; Duivestein, J.; Clavé, P.; Chen, J.; Kayashita, J.; Dantas, R.D.O.; Lecko, C.; Speyer, R.; Lam, P.; et al. The Need for International Terminology and Definitions for Texture-Modified Foods and Thickened Liquids Used in Dysphagia Management: Foundations of a Global Initiative. Curr. Phys. Med. Rehabil. Rep. 2013, 1, 280–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, F.; Ranmal, S.; Batchelor, H.K.; Orlu-Gul, M.; Ernest, T.B.; Thomas, I.W.; Flanagan, T.; Tuleu, C. Patient-Centered Pharmaceutical Design to Improve Acceptability of Medicines: Similarities and Differences in Paediatric and Geriatric Populations. Drugs 2014, 74, 1871–1889. [Google Scholar] [CrossRef] [Green Version]
- McCrickerd, K.; Forde, C.G. Sensory influences on food intake control: Moving beyond palatability. Obes. Rev. 2016, 17, 18–29. [Google Scholar] [CrossRef] [Green Version]
- Chojnicka-Paszun, A.; Doussinault, S.; De Jongh, H. Sensorial analysis of polysaccharide–gelled protein particle dispersions in relation to lubrication and viscosity properties. Food Res. Int. 2014, 56, 199–210. [Google Scholar] [CrossRef]
- Liu, F.; Ghaffur, A.; Bains, J.; Hamdy, S. Acceptability of oral solid medicines in older adults with and without dysphagia: A nested pilot validation questionnaire based observational study. Int. J. Pharm. 2016, 512, 374–381. [Google Scholar] [CrossRef] [Green Version]
- Pradal, C.; Stokes, J.R. Oral tribology: Bridging the gap between physical measurements and sensory experience. Curr. Opin. Food Sci. 2016, 9, 34–41. [Google Scholar] [CrossRef] [Green Version]
- Cook, S.L.; Bull, S.P.; Methven, L.; Parker, J.K.; Khutoryanskiy, V.V. Mucoadhesion: A food perspective. Food Hydrocoll. 2017, 72, 281–296. [Google Scholar] [CrossRef]
- Hofmanová, J.; Mason, J.; Batchelor, H. Tribology provides an in vitro tool that correlated to in vivo sensory data on the mouthfeel of coated tablets. Int. J. Pharm. 2021, 597, 120323. [Google Scholar] [CrossRef]
- Tuleu, C. Challenges of Sensory Evaluation (Palatability/Acceptability) of Pharmaceutical Products for Adults and Children. In Proceedings of the IFTS Science Sensory Group, London, UK, 16 June 2016. [Google Scholar]
- Batista, G.R.; Torres, C.R.G.; Sener, B.; Attin, T.; Wiegand, A. Artificial Saliva Formulations versus Human Saliva Pretreatment in Dental Erosion Experiments. Caries Res. 2016, 50, 78–86. [Google Scholar] [CrossRef] [Green Version]
- Williams, D.L.; Kuhn, A.T.; Amann, M.A.; Hausinger, M.B.; Konarik, M.M.; Nesselrode, E.I. Computerised Measurement of Contact Angles. Galvanotechnik 2010, 101, 2502–2512. [Google Scholar]
- Hotaling, N.A.; Bharti, K.; Kriel, H.; Simon, C.G., Jr. DiameterJ: A validated open source nanofiber diameter measurement tool. Biomaterials 2015, 61, 327–338. [Google Scholar] [CrossRef] [Green Version]
- Yoon, J.Y.; Trumper, D.L. Friction modeling, identification, and compensation based on friction hysteresis and Dahl resonance. Mechatronics 2014, 24, 734–741. [Google Scholar] [CrossRef]
- Mowlavi, S.; Engmann, J.; Burbidge, A.; Lloyd, R.; Hayoun, P.; Le Reverend, B.; Ramaioli, M. In vivo observations and in vitro experiments on the oral phase of swallowing of Newtonian and shear-thinning liquids. J. Biomech. 2016, 49, 3788–3795. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marconati, M.; Raut, S.; Burbidge, A.; Engmann, J.; Ramaioli, M. An in vitro experiment to simulate how easy tablets are to swallow. Int. J. Pharm. 2018, 535, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, A.; Andablo-Reyes, E.; Bryant, M.; Dowson, D.; Neville, A. Lubrication of soft oral surfaces. Curr. Opin. Colloid Interface Sci. 2019, 39, 61–75. [Google Scholar] [CrossRef]
- Fouad, E.A.; El-Badry, M.; Neau, S.H.; Alanazi, F.K.; Alsarra, I.A. Technology evaluation: Kollicoat IR. Expert Opin. Drug Deliv. 2011, 8, 693–703. [Google Scholar] [CrossRef]
- Kato, A.; Nakai, S. Hydrophobicity determined by a fluorescence probe method and its correlation with surface properties of proteins. Biochim. Biophys. Acta 1980, 624, 13–20. [Google Scholar] [CrossRef]
- Gonzalez, L.G.; Wess, T.J. The effects of hydration on the collagen and gelatine phases within parchment artefacts. Heritage Sci. 2013, 1, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Du, L.; Brenner, T.; Xie, J.; Matsukawa, S. A study on phase separation behavior in kappa/iota carrageenan mixtures by micro DSC, rheological measurements and simulating water and cations migration between phases. Food Hydrocoll. 2016, 55, 81–88. [Google Scholar] [CrossRef]
- Saha, D.; Bhattacharya, S. Hydrocolloids as thickening and gelling agents in food: A critical review. J. Food Sci. Technol. 2010, 47, 587–597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Necas, J.; Bartosikova, L. Carrageenan: A review. Vet. Med. 2013, 58, 187–205. [Google Scholar] [CrossRef] [Green Version]
- Joshi, S.; Petereit, H.-U. Film coatings for taste masking and moisture protection. Int. J. Pharm. 2013, 457, 395–406. [Google Scholar] [CrossRef]
- Siepmann, F.; Muschert, S.; Zach, S.; Leclercq, B.; Carlin, B.; Siepmann, J. Carrageenan as an Efficient Drug Release Modifier for Ethylcellulose-Coated Pharmaceutical Dosage Forms. Biomacromolecules 2007, 8, 3984–3991. [Google Scholar] [CrossRef]
- Rosiaux, Y.; Muschert, S.; Chokshi, R.; Leclercq, B.; Siepmann, F.; Siepmann, J. Ethanol-resistant polymeric film coatings for controlled drug delivery. J. Control. Release 2013, 169, 1–9. [Google Scholar] [CrossRef]
- Rosiaux, Y.; Velghe, C.; Muschert, S.; Chokshi, R.; Leclercq, B.; Siepmann, F.; Siepmann, J. Ethanol-resistant ethylcellulose/guar gum coatings—Importance of formulation parameters. Eur. J. Pharm. Biopharm. 2013, 85, 1250–1258. [Google Scholar] [CrossRef]
- Reddy, P.C.; Chaitanya, K.S.C.; Rao, Y.M. A review on bioadhesive buccal drug delivery systems: Current status of formulation and evaluation methods. DARU J. Pharm. Sci. 2011, 19, 385–403. [Google Scholar]
- Rao, M.R.P.; Ranpise, A.A.; Thanki, K.C.; Borate, S.G.; Parikh, G.N. Effect of processing and sintering on controlled release wax matrix tablets of ketorolac tromethamine. Indian J. Pharm. Sci. 2009, 71, 538–544. [Google Scholar] [CrossRef] [Green Version]
- Down, G.R.B. The etiology of pinhole and bubble defects in enteric and controlled-release film coatings. Drug Dev. Ind. Pharm. 1991, 17, 309–315. [Google Scholar] [CrossRef]
- Ho, L.; Müller, R.; Römer, M.; Gordon, K.; Heinämäki, J.; Kleinebudde, P.; Pepper, M.; Rades, T.; Shen, Y.; Strachan, C.; et al. Analysis of sustained-release tablet film coats using terahertz pulsed imaging. J. Control. Release 2007, 119, 253–261. [Google Scholar] [CrossRef]
- Kolter, K.; Dashevsky, A.; Irfan, M.; Bodmeier, R. Polyvinyl acetate-based film coatings. Int. J. Pharm. 2013, 457, 470–479. [Google Scholar] [CrossRef]
- Kariduraganavar, M.Y.; Kittur, A.A.; Kamble, R.R. Polymer Synthesis and Processing. In Natural and Synthetic Biomedical Polymers, 1st ed.; Elsevier: Amsterdam, The Netherlands, 2014; pp. 1–31. [Google Scholar] [CrossRef]
- Dos Santos, M.A.; Grenha, A. Polysaccharide Nanoparticles for Protein and Peptide Delivery. In Advances in Protein Chemistry and Structural Biology; Academic Press: Cambridge, MA, USA, 2015; Volume 98, pp. 223–261. [Google Scholar] [CrossRef]
- Ramesh, G.; Prabhu, K.N. Effect of Polymer Concentration on Wetting and Cooling Performance During Immersion Quenching. Met. Mater. Trans. B 2016, 47, 859–881. [Google Scholar] [CrossRef]
- Van Gorcum, M.; Karpitschka, S.; Andreotti, B.; Snoeijer, J.H. Spreading on viscoelastic solids: Are contact angles selected by Neumann’s law? Soft Matter 2020, 16, 1306–1322. [Google Scholar] [CrossRef] [Green Version]
- Shultz, M.J.; Bisson, P.; Vu, T.H. Insights into hydrogen bonding via ice interfaces and isolated water. J. Chem. Phys. 2014, 141, 18C521. [Google Scholar] [CrossRef]
- Liu, M.; Guo, T. Preparation and swelling properties of crosslinked sodium polyacrylate. J. Appl. Polym. Sci. 2001, 82, 1515–1520. [Google Scholar] [CrossRef]
- Choi, H.; Mitchell, J.R.; Gaddipati, S.R.; Hill, S.E.; Wolf, B. Shear rheology and filament stretching behaviour of xanthan gum and carboxymethyl cellulose solution in presence of saliva. Food Hydrocoll. 2014, 40, 71–75. [Google Scholar] [CrossRef] [Green Version]
- Hamilton, I.; Norton, I. Modification to the lubrication properties of xanthan gum fluid gels as a result of sunflower oil and triglyceride stabilised water in oil emulsion addition. Food Hydrocoll. 2016, 55, 220–227. [Google Scholar] [CrossRef]
- Liu, L.; Eriten, M. Frictional Energy Dissipation in Wavy Surfaces. J. Appl. Mech. 2016, 83, 121001. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.; Ding, J.; Zhou, L.; Chen, S. Mechanical properties, water-swelling behavior, and morphology of water-swellable rubber prepared using crosslinked sodium polyacrylate. J. Appl. Polym. Sci. 2006, 102, 1489–1496. [Google Scholar] [CrossRef]
| Formulation | Kollicoat® IR, % w/w | λ-Carrageenan, % w/w | Gelatin Type A, % w/w |
|---|---|---|---|
| Control | 10 | 0 | 0 |
| Binary Composition | 10 | 1 | 0 |
| 10 | 3 | 0 | |
| 10 | 0 | 1 | |
| 10 | 0 | 3 | |
| Ternary Composition | 10 | 1 | 3 |
| 10 | 3 | 3 |
| Formulation | Immediate * | 10 s | 20 s | |||
|---|---|---|---|---|---|---|
| Mean | Std | Mean | Std | Mean | Std | |
| Uncoated | 0 | 0 | 0 | 0 | 0 | 0 |
| Kollicoat® IR | 97.17 | 1.46 | 89.92 | 1.59 | 83.32 | 1.33 |
| Opadry® EZ | 91.64 | 1.83 | 87.43 | 1.34 | 81.03 | 1.37 |
| PVA | 96.24 | 1.46 | 90.53 | 1.49 | 88.62 | 1.23 |
| HPMC | 94.28 | 1.21 | 89.24 | 1.36 | 86.13 | 1.16 |
| C 1% w/w | 93.06 | 1.92 | 88.73 | 1.21 | 75.77 | 1.31 |
| C 3% w/w | 88.67 | 1.24 | 81.97 | 1.25 | 73.03 | 1.83 |
| Ge 1% w/w | 98.37 | 1.37 | 93.07 | 1.15 | 80.87 | 1.31 |
| Ge 3% w/w | 104.17 | 1.55 | 91.17 | 1.04 | 82.87 | 1.82 |
| Ge 3%: C1% w/w | 93.23 | 1.53 | 86.07 | 1.54 | 76.33 | 1.22 |
| Ge 3%: C3% w/w | 89.57 | 1.64 | 81.87 | 1.42 | 71.08 | 1.36 |
| In-Vitro Oral Transit Time, s | |||||
|---|---|---|---|---|---|
| 4 | 8 | 12 | 16 | 20 | |
| Unc. | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| PVA | 0.11 | 0.17 | 0.37 | 0.54 | 0.82 |
| HPMC | 0.23 | 0.76 | 1.05 | 1.35 | 1.86 |
| KIR | 0.14 | 0.61 | 0.82 | 1.10 | 1.83 |
| OEZ | 1.19 | 4.82 | 5.42 | 6.78 | 7.99 |
| C1% | 0.51 | 1.19 | 3.46 | 6.20 | 6.64 |
| C3% | 0.60 | 1.40 | 4.49 | 6.18 | 7.41 |
| Ge1% | 0.36 | 1.56 | 2.61 | 3.97 | 6.10 |
| Ge3% | 0.29 | 1.41 | 2.22 | 3.19 | 4.36 |
| Ge3%C1% | 1.46 | 2.78 | 5.49 | 6.77 | 7.87 |
| Ge3%C3% | 1.42 | 2.34 | 5.65 | 6.93 | 9.47 |
| In-Vitro Oral Transit Time, s | |||||
|---|---|---|---|---|---|
| 4 | 8 | 12 | 16 | 20 | |
| Unc. | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| PVA | 0.11 | 0.17 | 0.37 | 0.54 | 0.82 |
| KIR | 0.14 | 0.61 | 0.82 | 1.10 | 1.83 |
| HPMC | 0.23 | 0.76 | 1.05 | 1.35 | 1.86 |
| Ge3% | 0.29 | 1.41 | 2.22 | 3.19 | 4.36 |
| Ge1% | 0.36 | 1.56 | 2.61 | 3.97 | 6.10 |
| C1% | 0.51 | 1.19 | 3.46 | 6.20 | 6.64 |
| C3% | 0.60 | 1.40 | 4.49 | 6.18 | 7.41 |
| Ge3%C1% | 1.46 | 2.78 | 5.49 | 6.77 | 7.87 |
| Ge3%C3% | 1.42 | 2.34 | 5.65 | 6.93 | 9.47 |
| OEZ | 1.19 | 4.82 | 5.42 | 6.78 | 7.99 |
| Swallowability Index | Swallowability Rank | Colour Map |
|---|---|---|
| 0 | Poor | |
| 0 < SI < 1 | Pass | |
| 1 < SI < 2 | Good | |
| 2 < SI < 4 | Very Good | |
| ≥ 4 | Excellent |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ershad, A.L.; Rajabi-Siahboomi, A.; Missaghi, S.; Kirby, D.; Mohammed, A.R. Multi-Analytical Framework to Assess the In Vitro Swallowability of Solid Oral Dosage Forms Targeting Patient Acceptability and Adherence. Pharmaceutics 2021, 13, 411. https://doi.org/10.3390/pharmaceutics13030411
Ershad AL, Rajabi-Siahboomi A, Missaghi S, Kirby D, Mohammed AR. Multi-Analytical Framework to Assess the In Vitro Swallowability of Solid Oral Dosage Forms Targeting Patient Acceptability and Adherence. Pharmaceutics. 2021; 13(3):411. https://doi.org/10.3390/pharmaceutics13030411
Chicago/Turabian StyleErshad, Abdul Latif, Ali Rajabi-Siahboomi, Shahrzad Missaghi, Daniel Kirby, and Afzal Rahman Mohammed. 2021. "Multi-Analytical Framework to Assess the In Vitro Swallowability of Solid Oral Dosage Forms Targeting Patient Acceptability and Adherence" Pharmaceutics 13, no. 3: 411. https://doi.org/10.3390/pharmaceutics13030411
APA StyleErshad, A. L., Rajabi-Siahboomi, A., Missaghi, S., Kirby, D., & Mohammed, A. R. (2021). Multi-Analytical Framework to Assess the In Vitro Swallowability of Solid Oral Dosage Forms Targeting Patient Acceptability and Adherence. Pharmaceutics, 13(3), 411. https://doi.org/10.3390/pharmaceutics13030411








