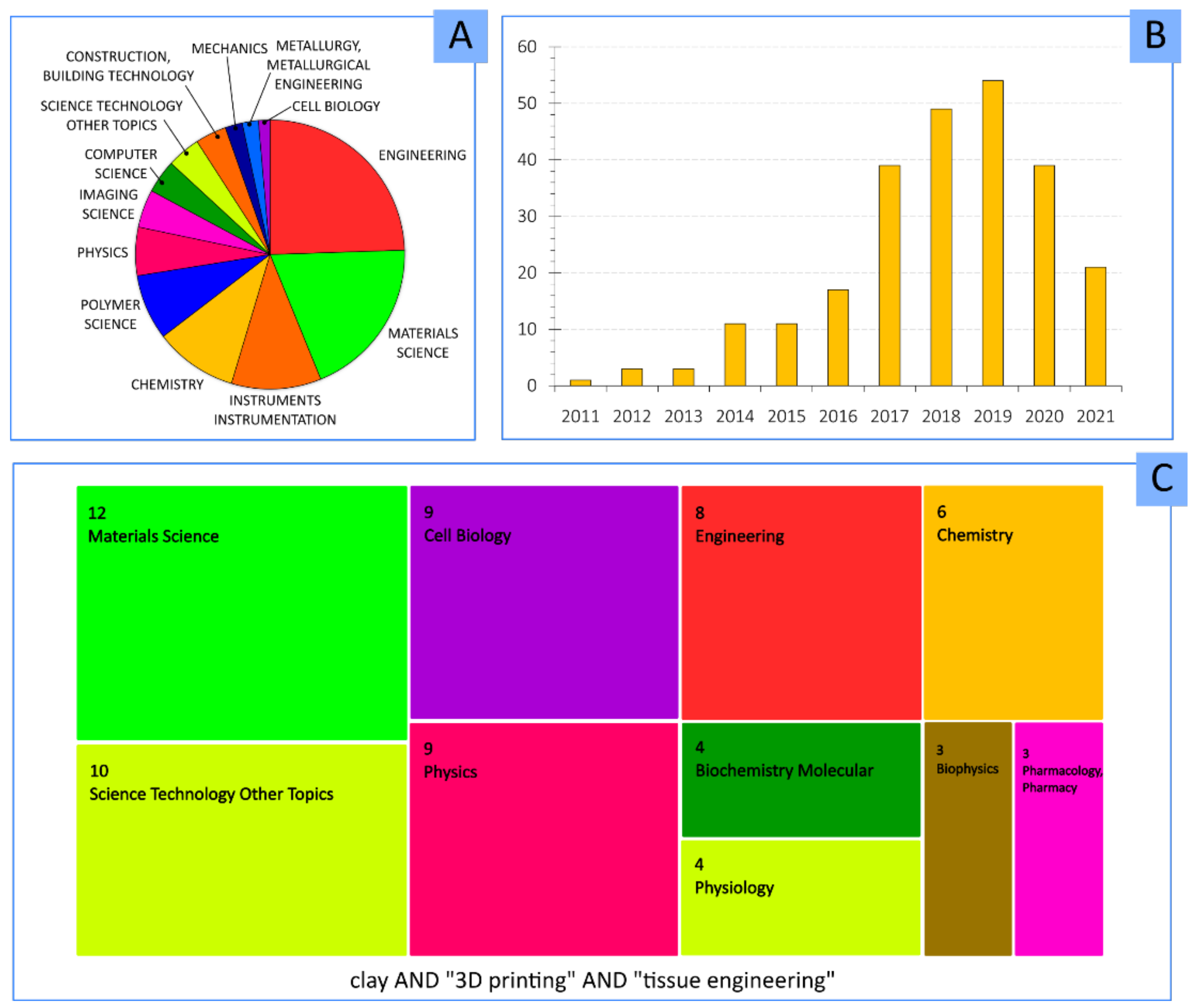
Clay Minerals as Bioink Ingredients for 3D Printing and 3D Bioprinting: Application in Tissue Engineering and Regenerative Medicine
Abstract
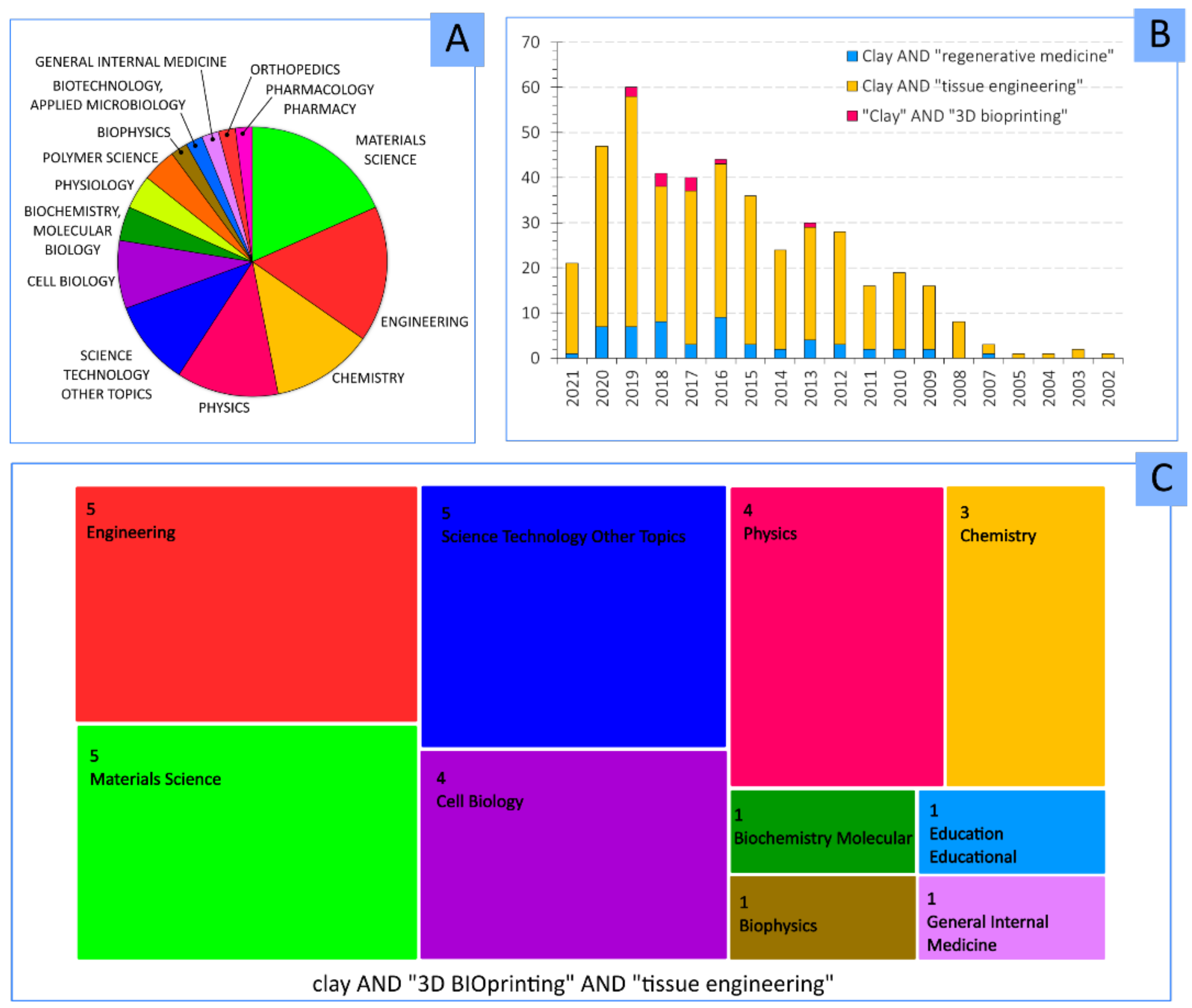
:1. Introduction
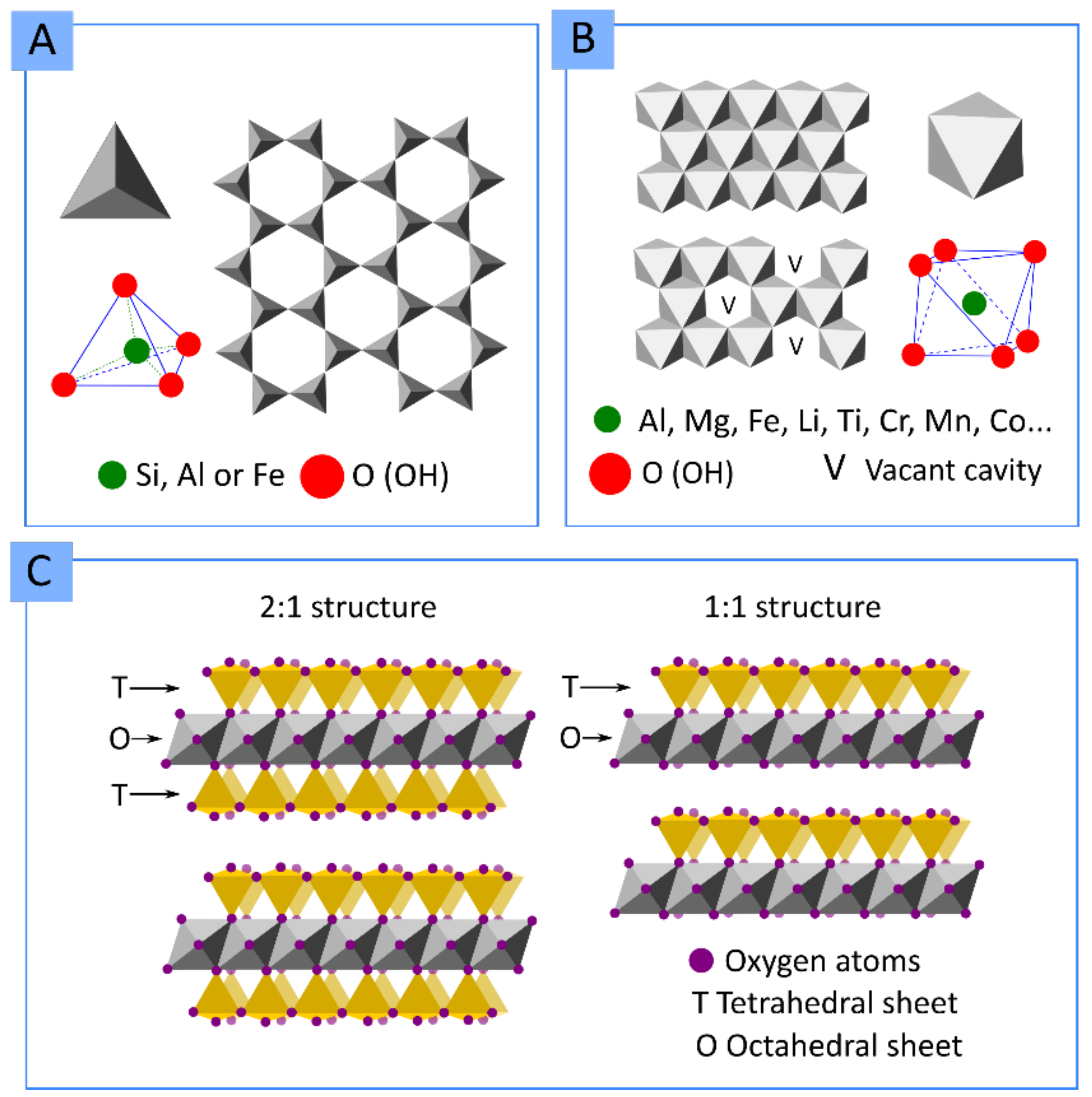
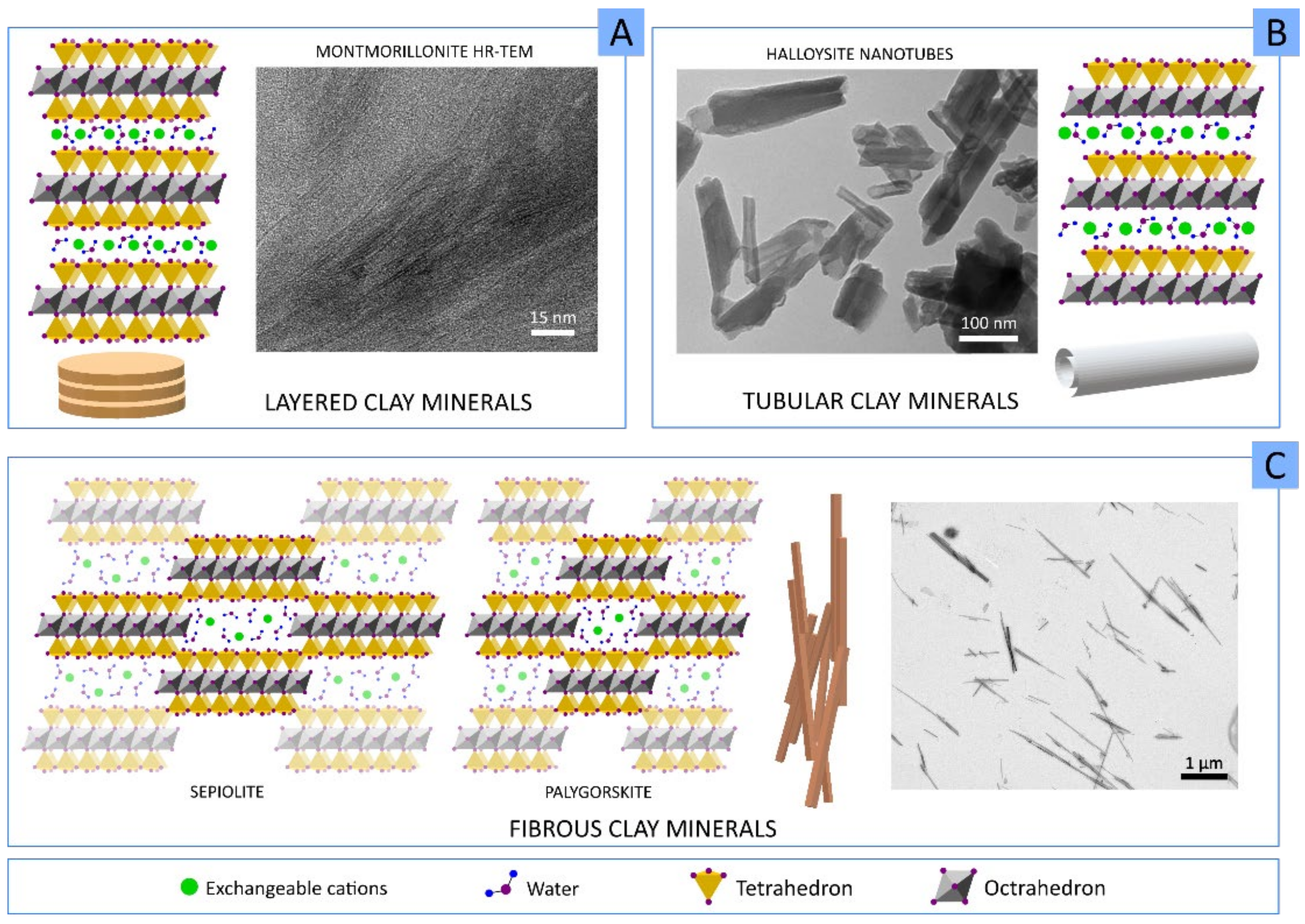
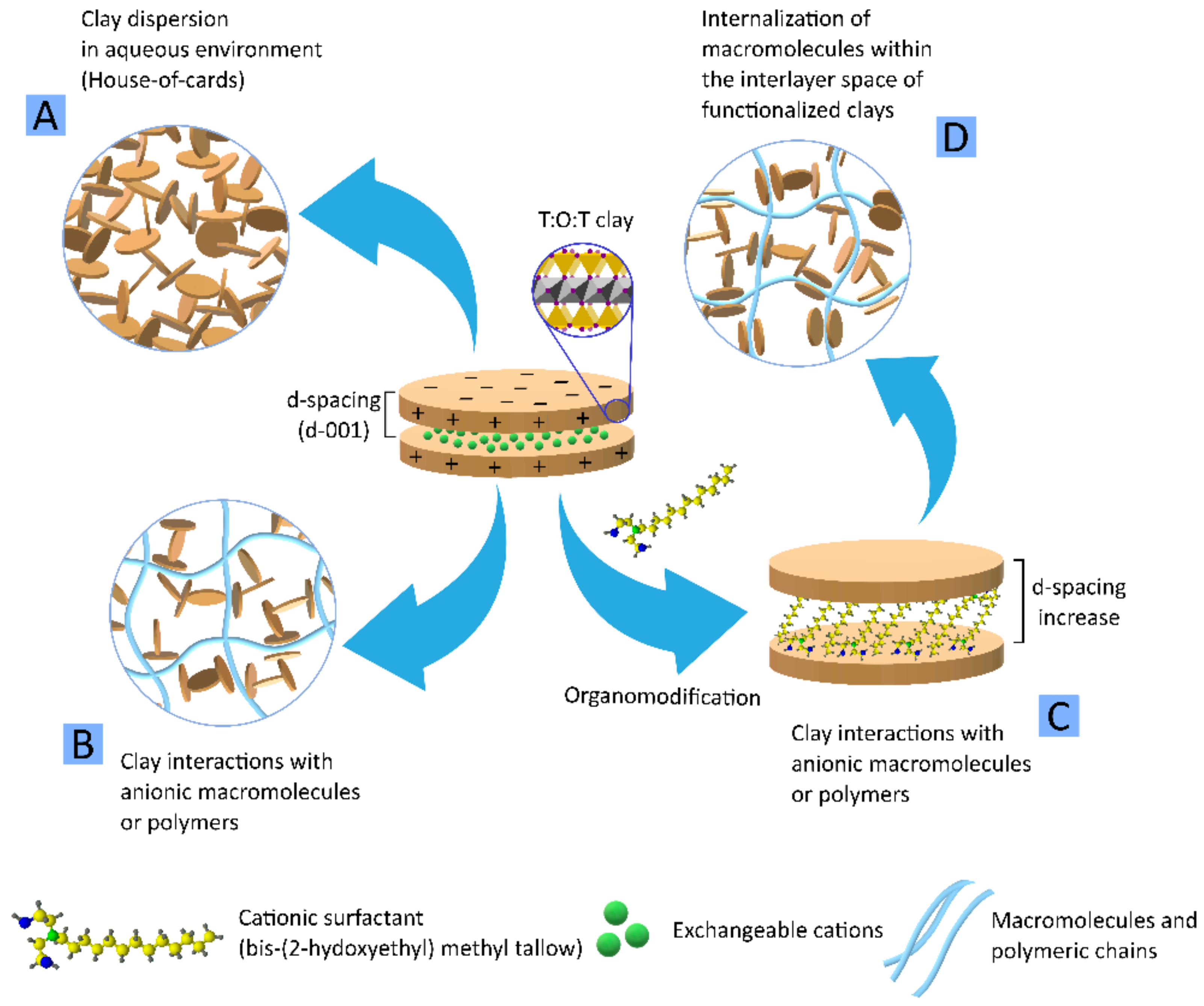
1.1. Clay Minerals
- Layered clay minerals such as montmorillonite (MMT), hectorite (HT), or laponite (LAP);
- Tubular clay minerals, where halloysite nanotubes (HNTs) are included;
- Fibrous clay minerals or “non-planar phyllosilicates”, a group formed by sepiolite (SEP) and palygorskite (PAL, also known as attapulgite).
1.2. Clay Minerals in 3D Printing
| Clay Mineral and Concentration | Other Ink Ingredients | Clay Role | 3DP Technique | Ref |
|---|---|---|---|---|
| MMT (Cloisite® 30B)—4% w/w | PLA | Increasing PLA crystallinity, melting temperature modifier and mechanical reinforcement | Fused deposition modelling | [21,22] |
| MMT (Cloisite® 5, Cloisite® 20, Na Cloisite®)—1, 5% w/w | PLA | Improved mechanical properties of PLA by organo-modified clay minerals due to increased d-spacing of organo-modified clay particles | Fused filament fabrication | [25] |
| MMT—0.5, 1, 2, 5% w/w | HDPE | MMT provided superior mechanical performance | Fused filament fabrication | [20] |
| MMT (Cloisite® SE300)—1, 3, 5% w/w | PETG | Mechanical reinforcement. Simplification of the 3D construct post-processing or post-treatment | Extrusion | [26] |
| SEP—1, 2, 3, 5, 7% w/w | PETG | Improvement of mechanical properties due to directional alignment of SEP particles within PETG filament | Fused deposition modelling | [27] |
| LAP—2.5% w/v | Silk fibroin | Formation of a print-bed (in combination with PEG) to support silk-fibroin BI 3D constructs | Submerged extrusion into LAP–PEG suspension | [28] |
| LAP—7% w/w | NIPAAM, PAAM | Rheological modifier for 3DP and mechanical reinforcement | Extrusion | [29] |
| LAP—12% w/v | Pluronic | Improvement of printability and mechanical properties of ink used as sacrificial material template (mold) for the production of microfluidic system | Extrusion | [30] |
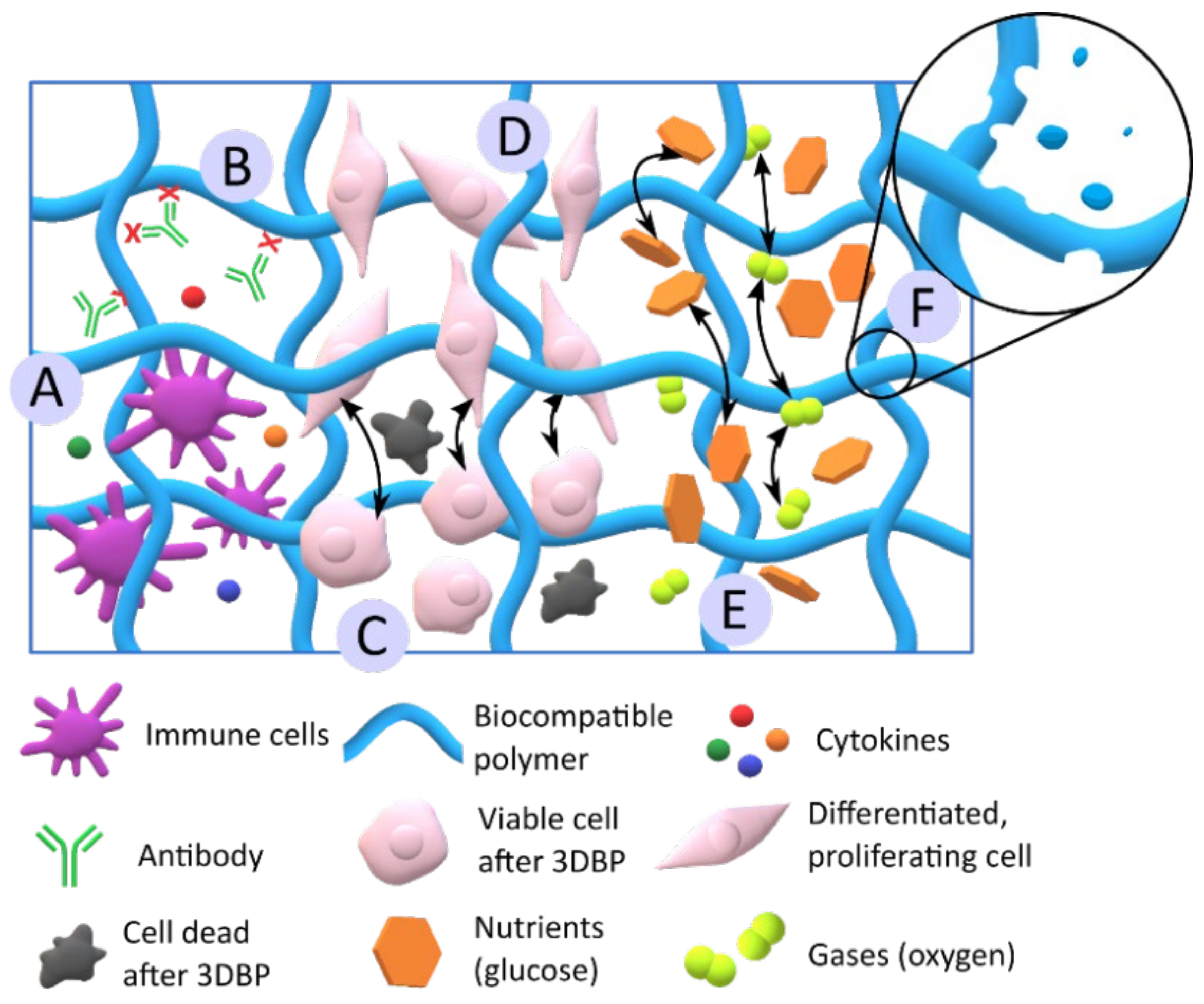
2. Clay Minerals in 3D Bioprinting
2.1. Desirable Bioink and Biomaterial Ink Properties
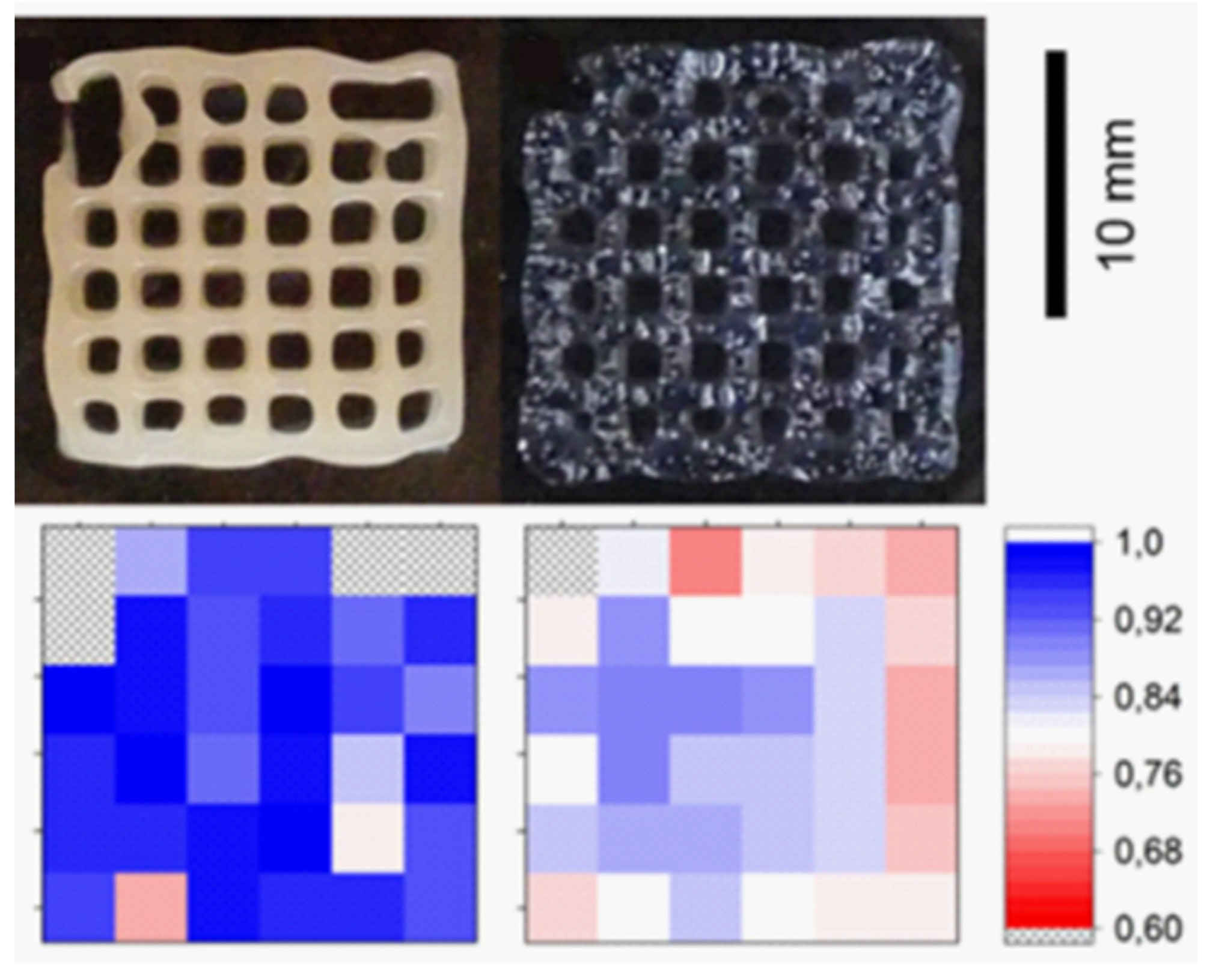
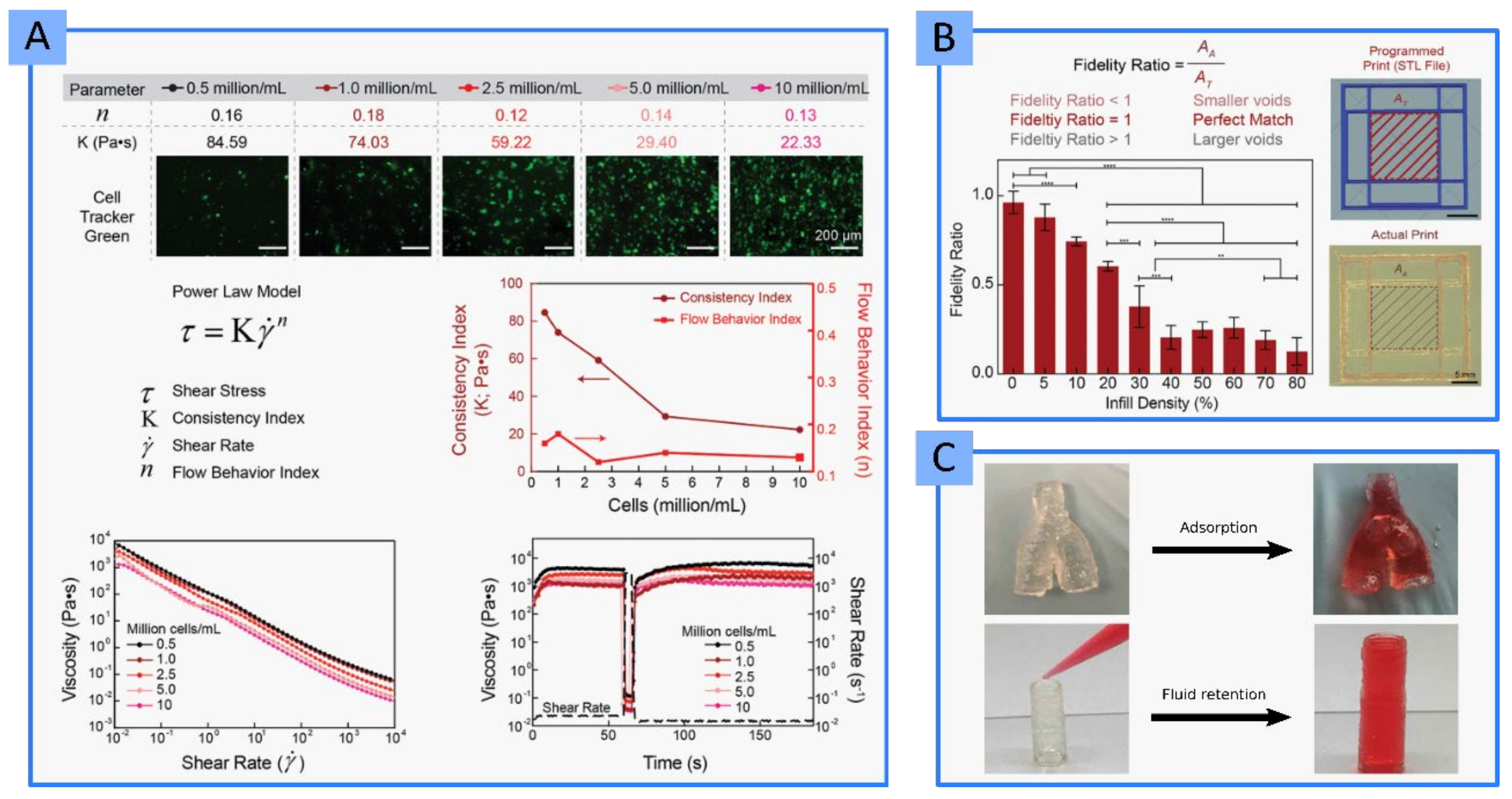
2.1.1. Printability and Shape Fidelity

2.1.2. Biocompatibility and Functionality
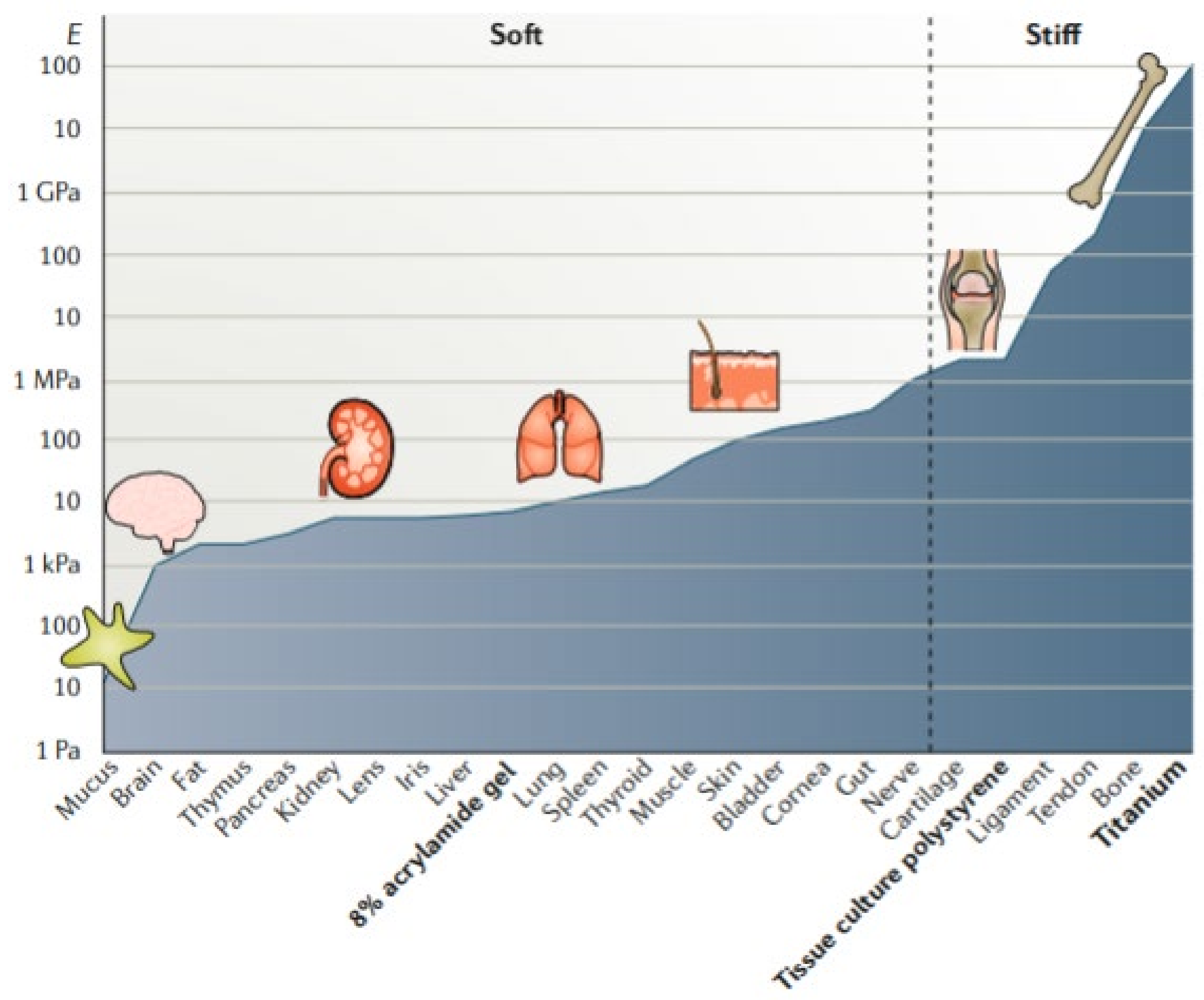
2.1.3. Mechanical Properties
| Clay Mineral | Clay Concentration | Other Biomaterial Ink Ingredients | Final Scope | Clay Role | Ref |
|---|---|---|---|---|---|
| LAP | 10–100 µg/mL | GelMA | 3D bone TE | Osteoinductive ingredient; controlled release of VEGF | [85] |
| 3, 4 and 5% w/v | GelMA | Printability studies of BMI for TE (target tissue undetermined) | Increase in porosity and printability | [96] | |
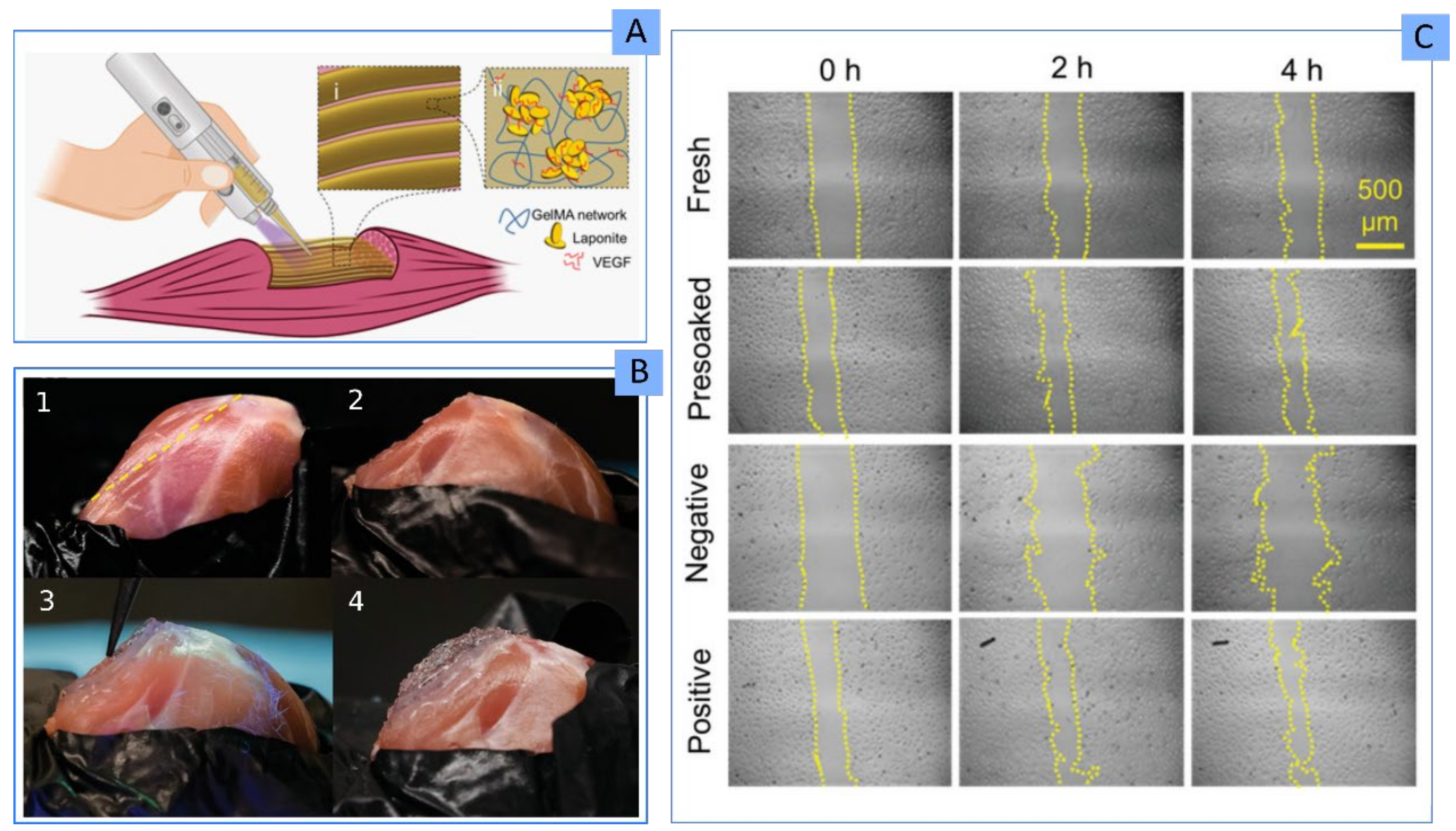
| Not specified | GelMA | 3D skeletal muscle TE | Carrier and control release of VEGF | [63] | |
| 5% w/w | PEGDA, ALG | 3D cartilage TE | Improved printability and shape retention | [97] | |
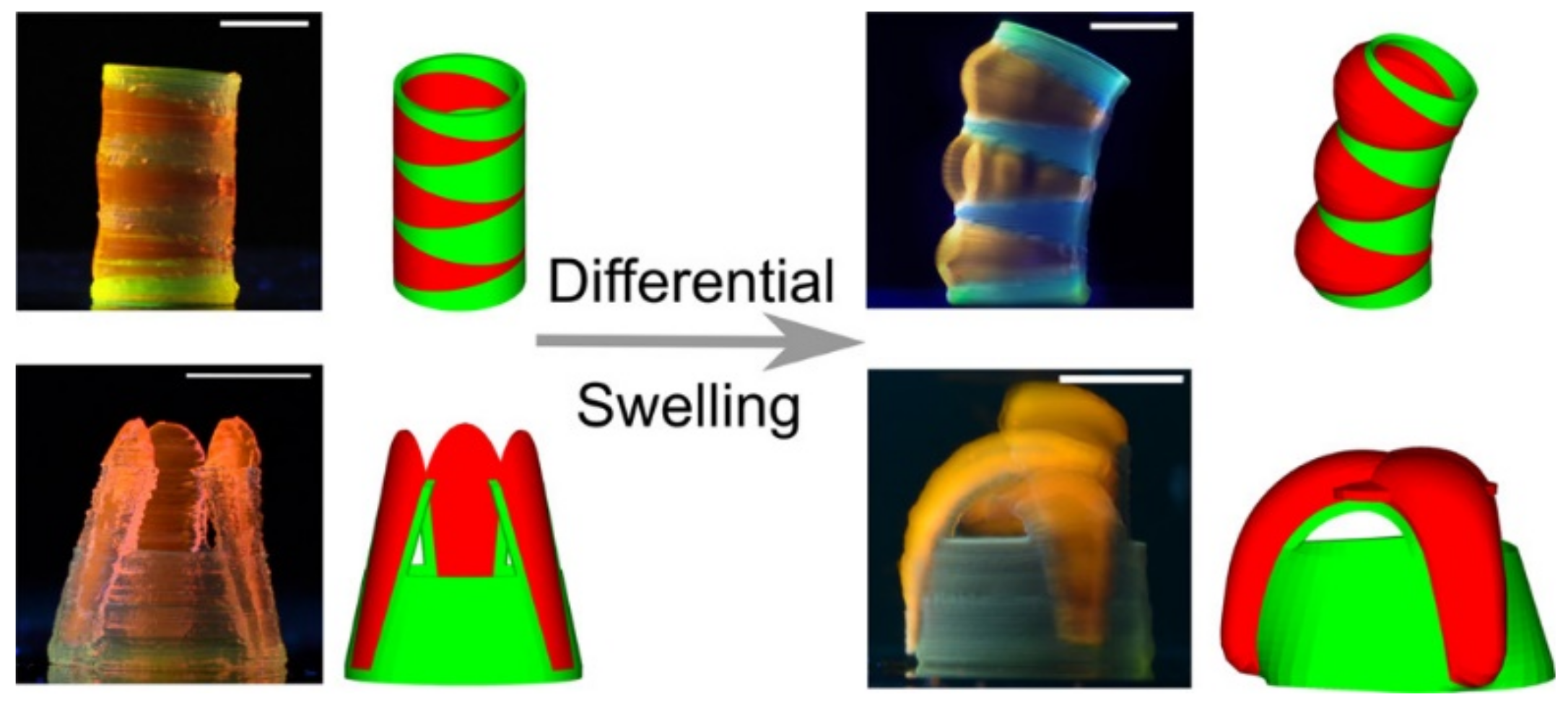
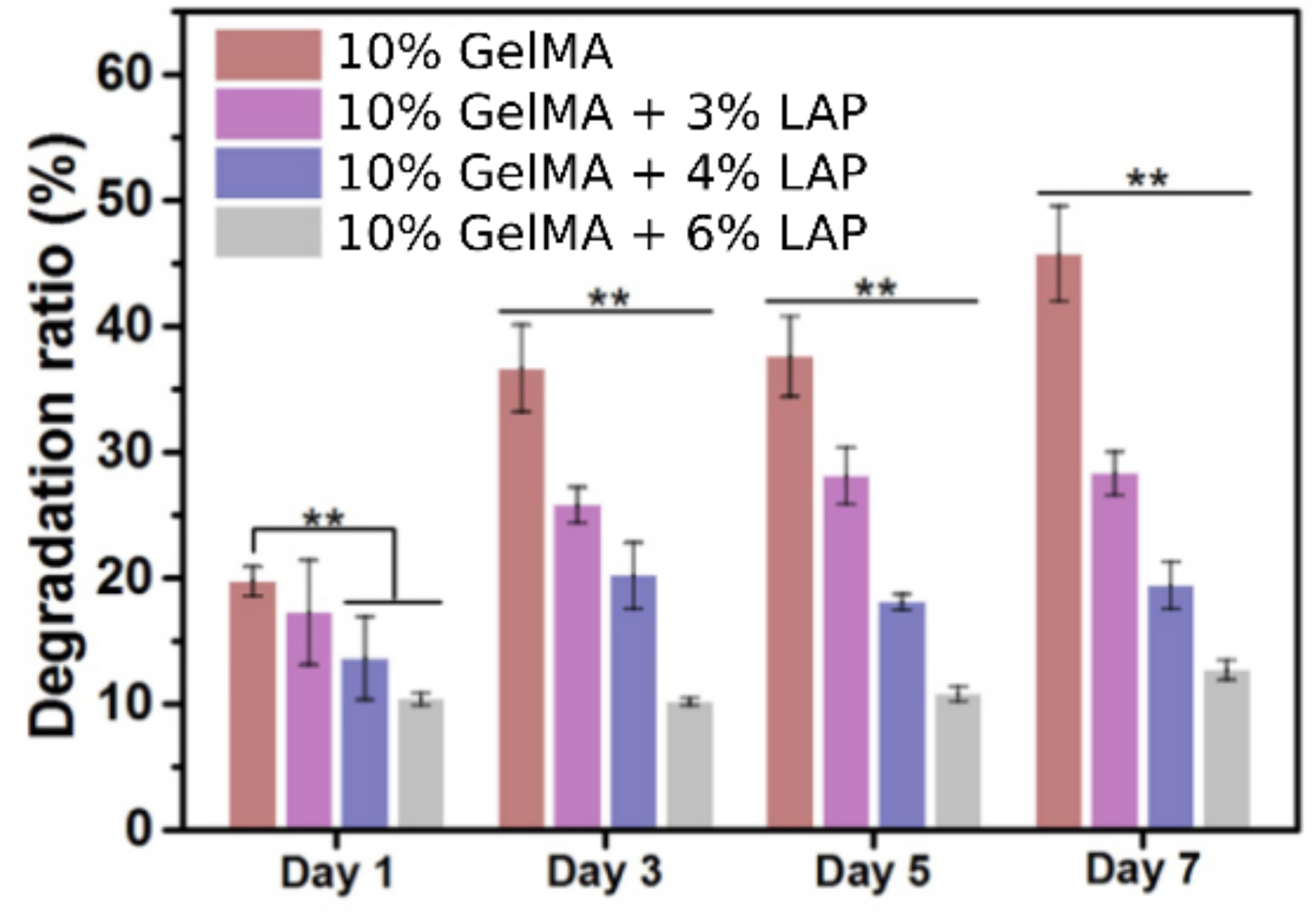
| 6% w/v | PEGDA, ALG, GEL | Development of self-supporting BMI for complex, in air, 3D structures | Printability and shape retention: self-supporting ingredient. Enabled “printing-then-crosslinking” process; Improved mechanical properties; Control of construct biodegradability | [40] | |
| 0.1, 0.5 and 1% w/v | ALG-GEL | 3D TE (target tissue undetermined) | Optimization of BI material printability | [98] | |
| 4.5% w/w | AGA, PAM | 3D TE (target tissue undetermined) | Mechanical reinforcement ingredient | [99] | |
| 6, 12, 18 and 22% w/w | NIPAM, CNT | Medical device for human motion monitoring | Mechanical reinforcement ingredient; Biocompatible to fibroblasts | [7] | |
| 10% w/w | PAAM, PEDOT | Medical device for neurological regeneration | Improved conductivity and mechanical properties | [100] | |
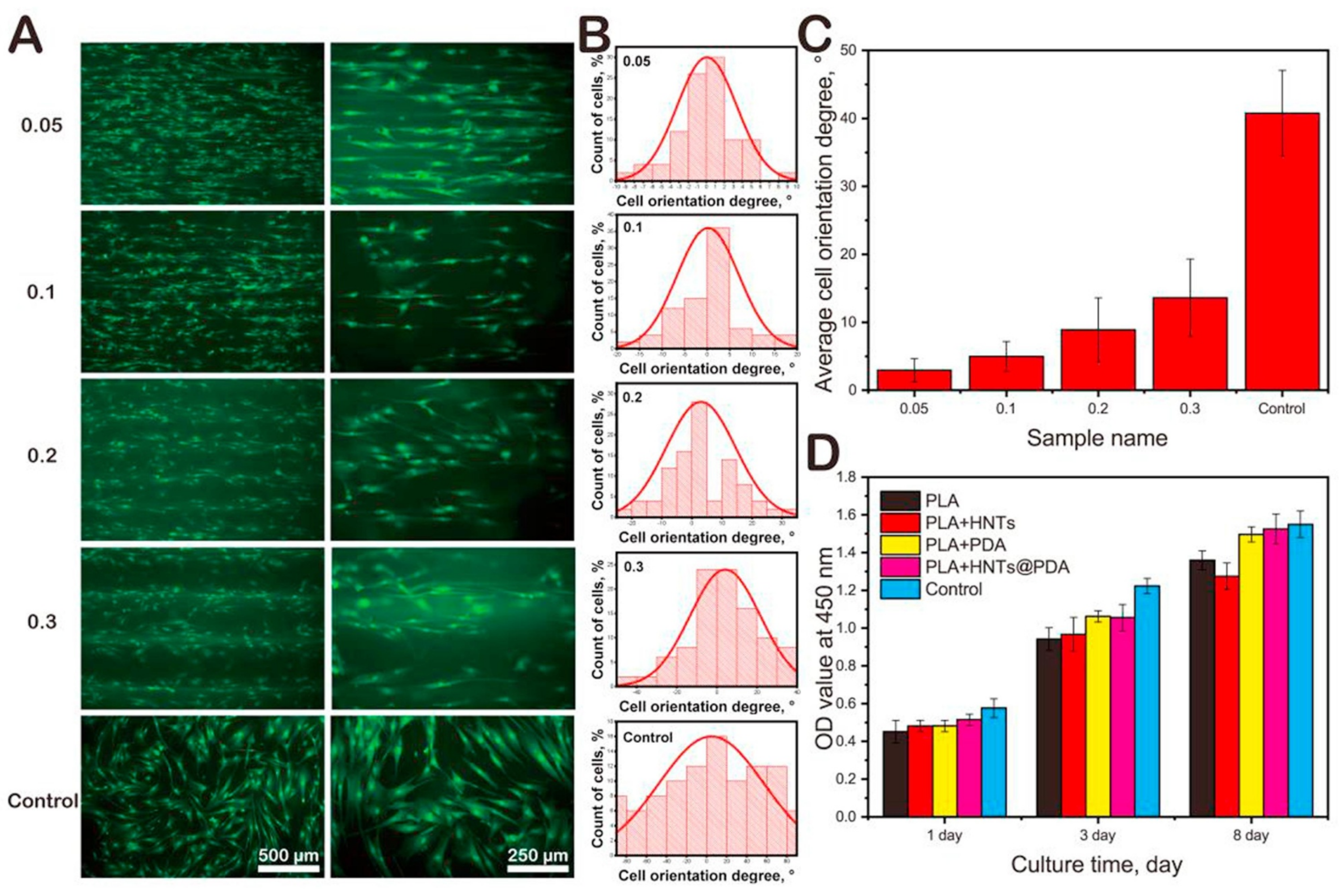
| 7–9% w/w | HEMA | 3D scaffolds able to direct cellular attachment, growth and differentiation | Improvement and modulation of cellular attachment and motility | [101] | |
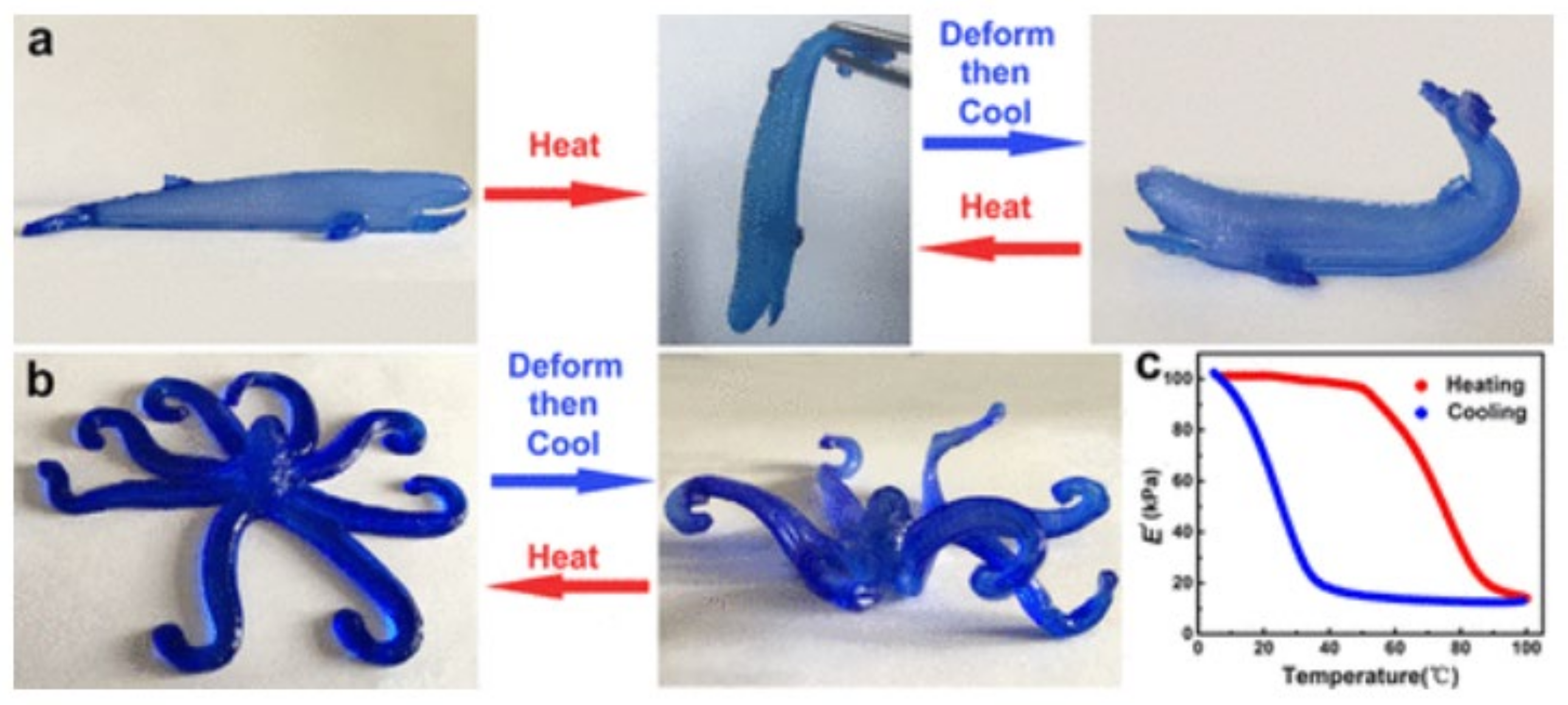
| 1.4–1.7% w/w | PMet-b-POxa | Stimuli-responsive BMI for TE (target tissue undetermined) | Modification of polymer gelling temperature, improvement of shape-fidelity | [102] | |
| 6 and 10% w/w | SPE | Medical device for lower limb prostheses adapted to movement | SPE crosslinker, rheological additive | [103] | |
| 0.1, 0.5 and 1% | TEMPO BC, ALG | 3D TE (target tissue undetermined) | Printability and shape-fidelity enhancer; control release of BSA | [104] | |
| HT and LAP | 0.5–7% w/v | PEGDA | Recyclable 3D construct for biocatalysis | Rheological additives: HT induced higher viscosities with lower shear-thinning profile with respect to LAP. HT performed higher printing fidelity and faster construct biodegradation | [81] |
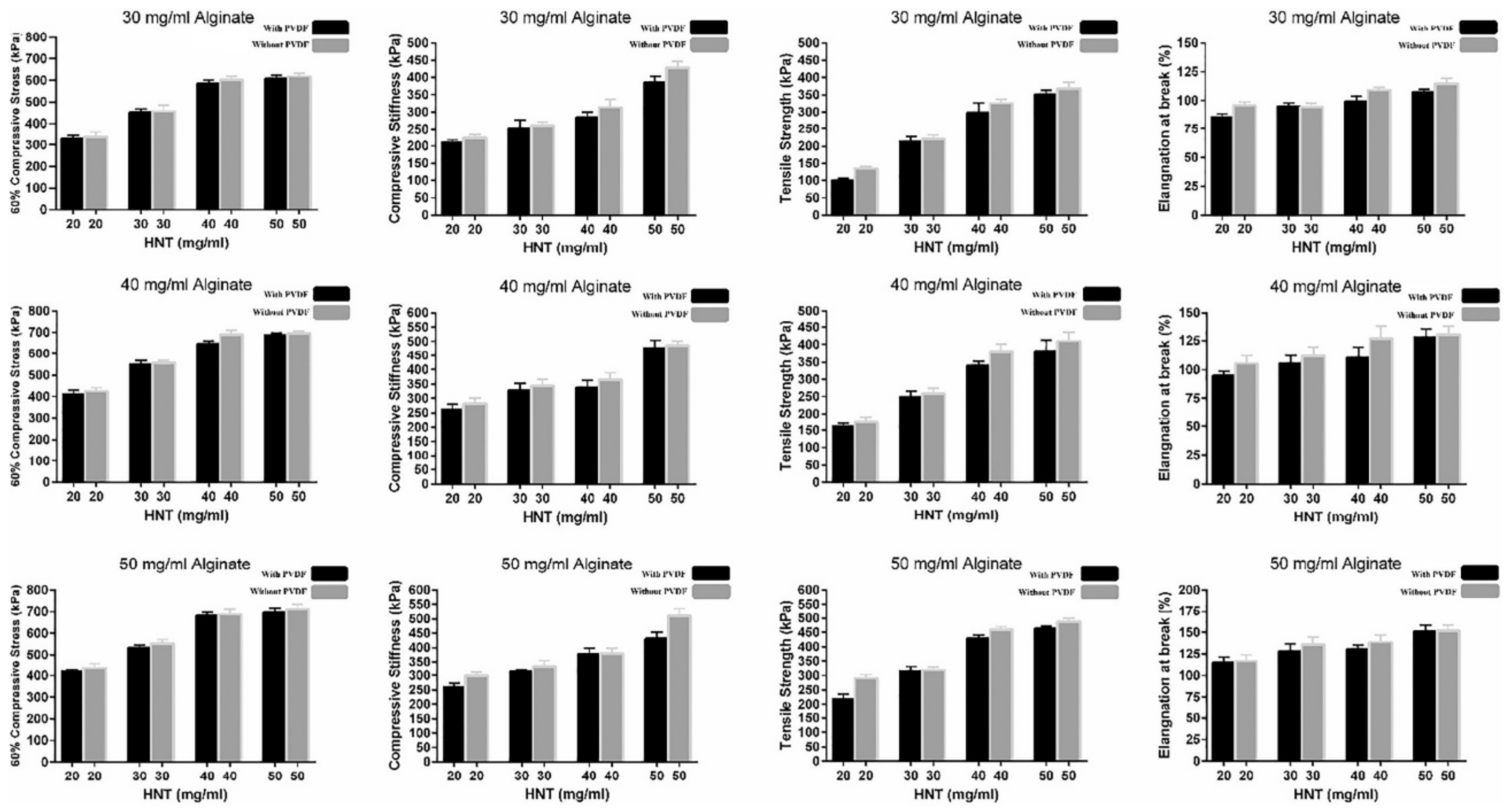
| HNTs | 2, 3, 4, 5% w/v | ALG, MC, PVDF | 3D cartilage TE | Improved mechanical properties | [91] |
| PAL | 50–90% w/w | PVA | 3D bone TE | Osteoinductive ingredient with significant mechanical resistance | [90] |
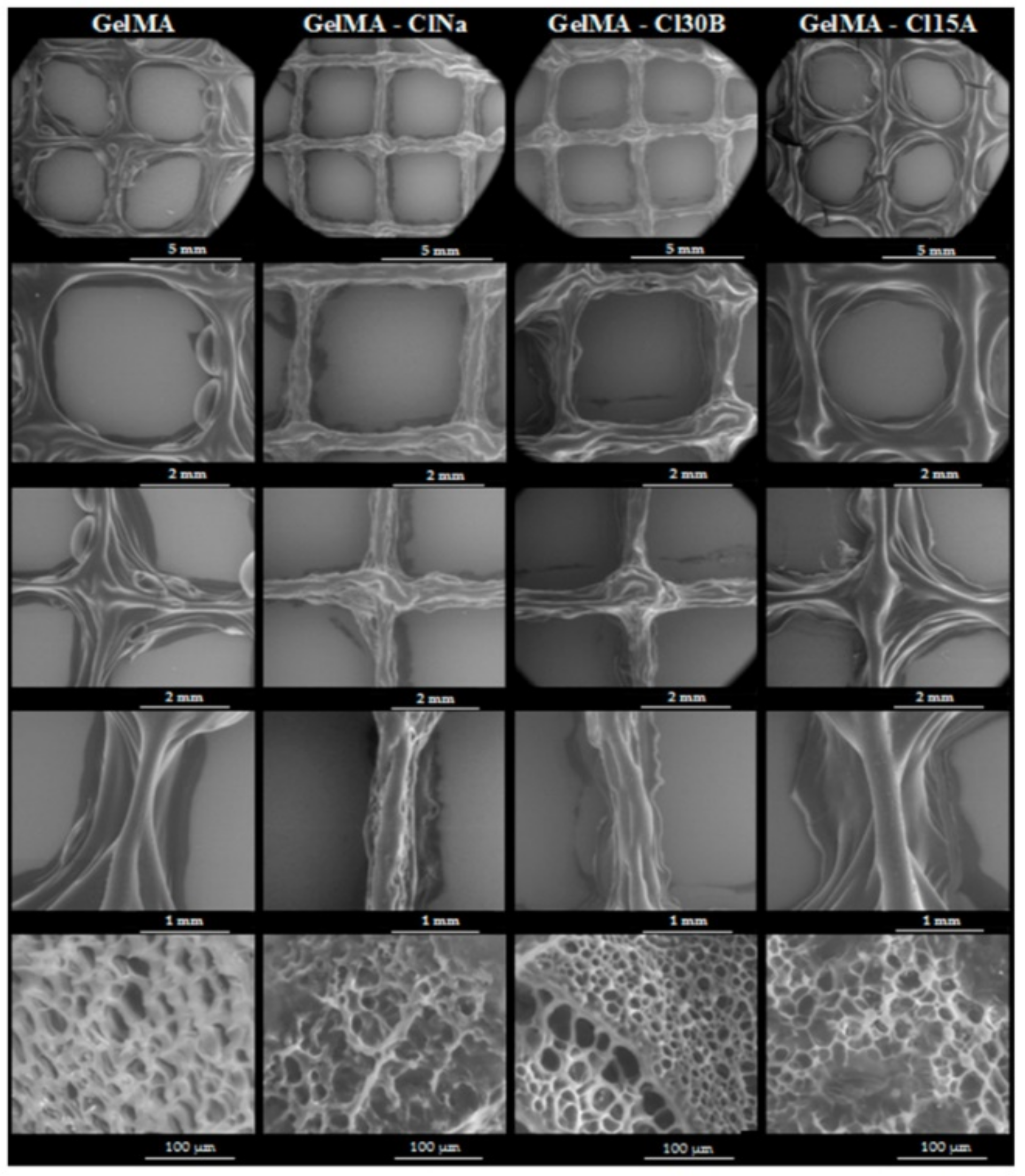
| Cloisite® Na, Cloisite® 30B, Cloisite® 15A | 3% w/w | GelMA | Production of 3D bioactive medical devices | Rheological additives; improved and controlled porosity. Mechanical reinforcement ingredients | [105] |
2.2. Use of Clay Minerals as Printability and Shape Fidelity Ingredients
| Clay | Clay Concentration | Rest of Bi Ingredients | Final Scope | Cell Type | Cellular Viability | Ref |
|---|---|---|---|---|---|---|
| LAP | 3% w/w | ALG, MC | 3D skeletal tissues engineering | Mesenchymal stem cells | 70–75% | [73] |
| 3% w/v | ALG, MC | 3D bone TE | Human bone marrow stromal cells | >90% from day 7 | [114] | |
| 0.5% and 1% w/v | GG | 3D bone TE | Myoblasts | 80% | [115] | |
| 2.3% w/w | dcECM, PEGDA | 3D cardiac TE | Human cardiac fibroblasts | >97% in 7 days | [92] | |
| 0.5, 0.75, 1 and 2% w/w | GelMA | 3D bone and vascular TE | Human bone marrow stromal cell | 85% in 21 days | [72] | |
| 1–5% w/w | GelMA/PEGDA | Production of multicellular, free-standing 3D vascular model | Endothelial cells and vascular smooth muscle cells | >85% post-extrusion on days 1, 3, and 7 | [69] | |
| 7% w/v | NAGA | 3D bone TE | Osteoblasts | Not mentioned | [89] | |
| >4% w/v | PEG | 3D TE (target tissue undetermined) | Pre-osteoblasts | >90% in 21 days | [74] | |
| 7% w/v | PEGDA, HA | 3D bone TE | Osteoblast | 95% after 1 day | [71] | |
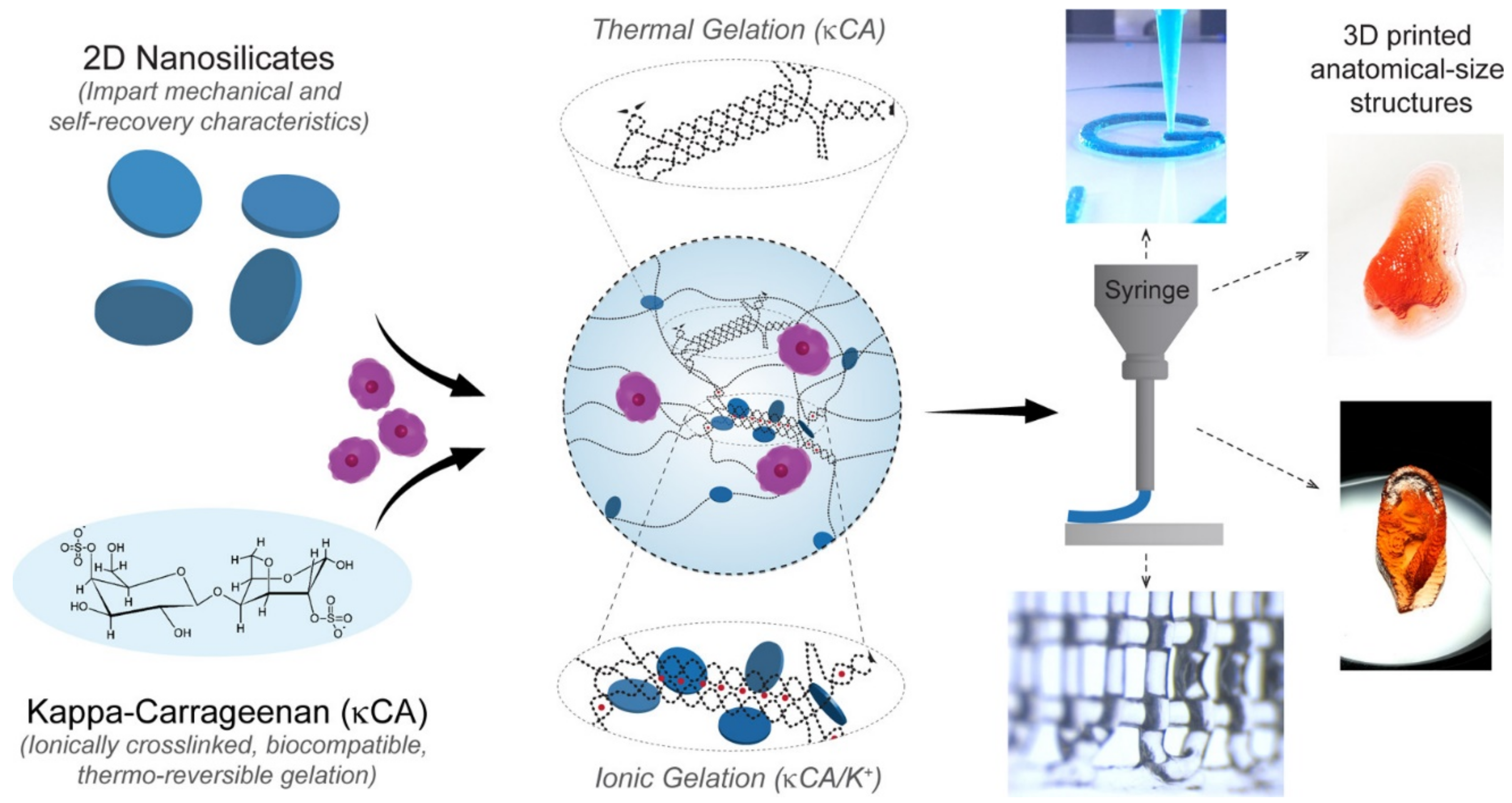
| 0–6% w/v | k-CA | 3D TE (target tissue undetermined) | Pre-osteoblasts | Not reported | [113] | |
| 4% w/v | PEG and PEGDTT | Control and direction of cell migration | HUVEC | 85% just after 3D bioprinting | [82] | |
| 0.1, 0.25, 0.5 and 1% w/v | AGA | Increase the bioactivity of AGA BI | NIH/3T3 fibroblasts | Analysis performed, quantitative data not specified | [112] | |
| MMT | 4% w/v | CMC, ALG | 3D soft-tissue engineering | Human pancreatic cancer cells | 84% after 7 days | [70] |
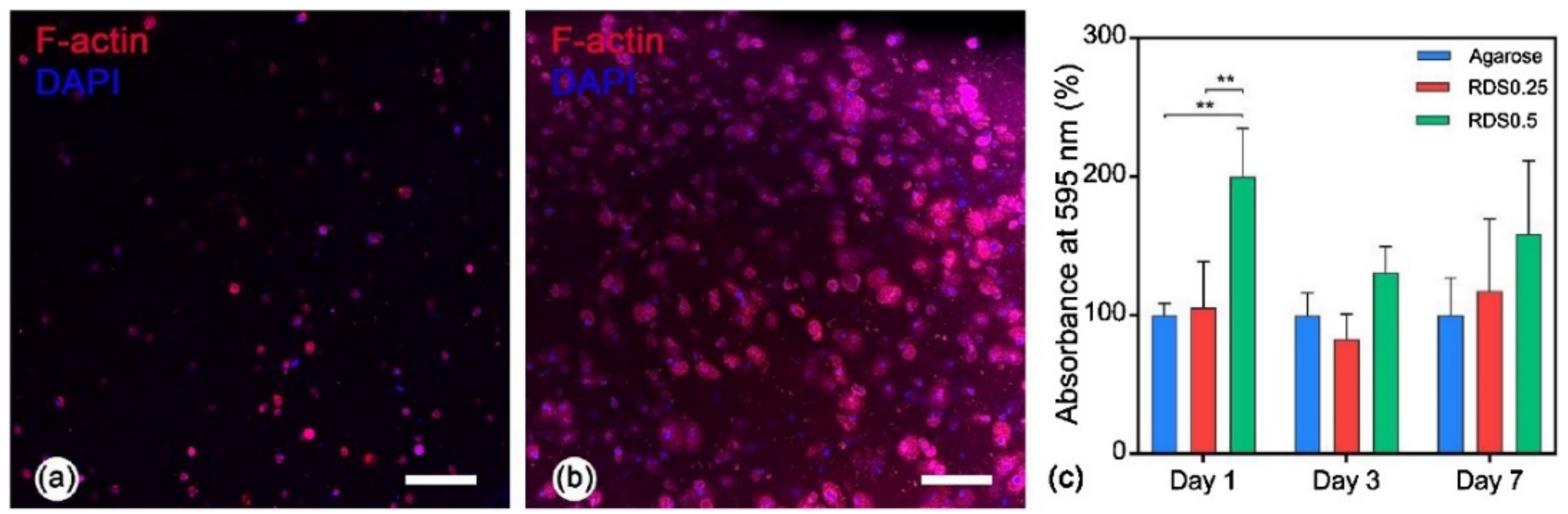
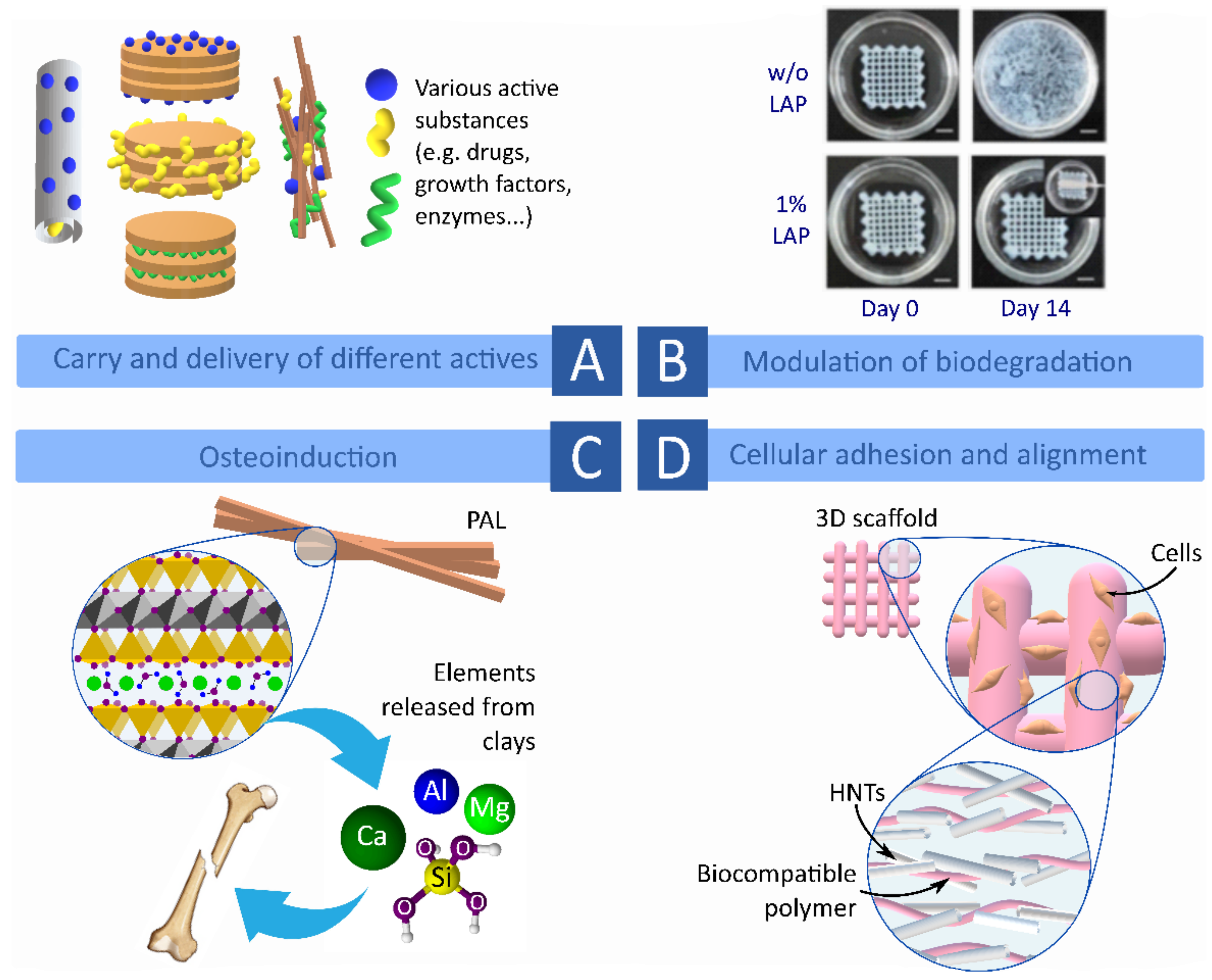
2.3. Clay Minerals as Biocompatible and Functional Ingredients of Bioinks and Biomaterial Inks
2.3.1. Biocompatibility, Cellular Adhesion and Proliferation
2.3.2. Biodegradation of 3D Printed Constructs
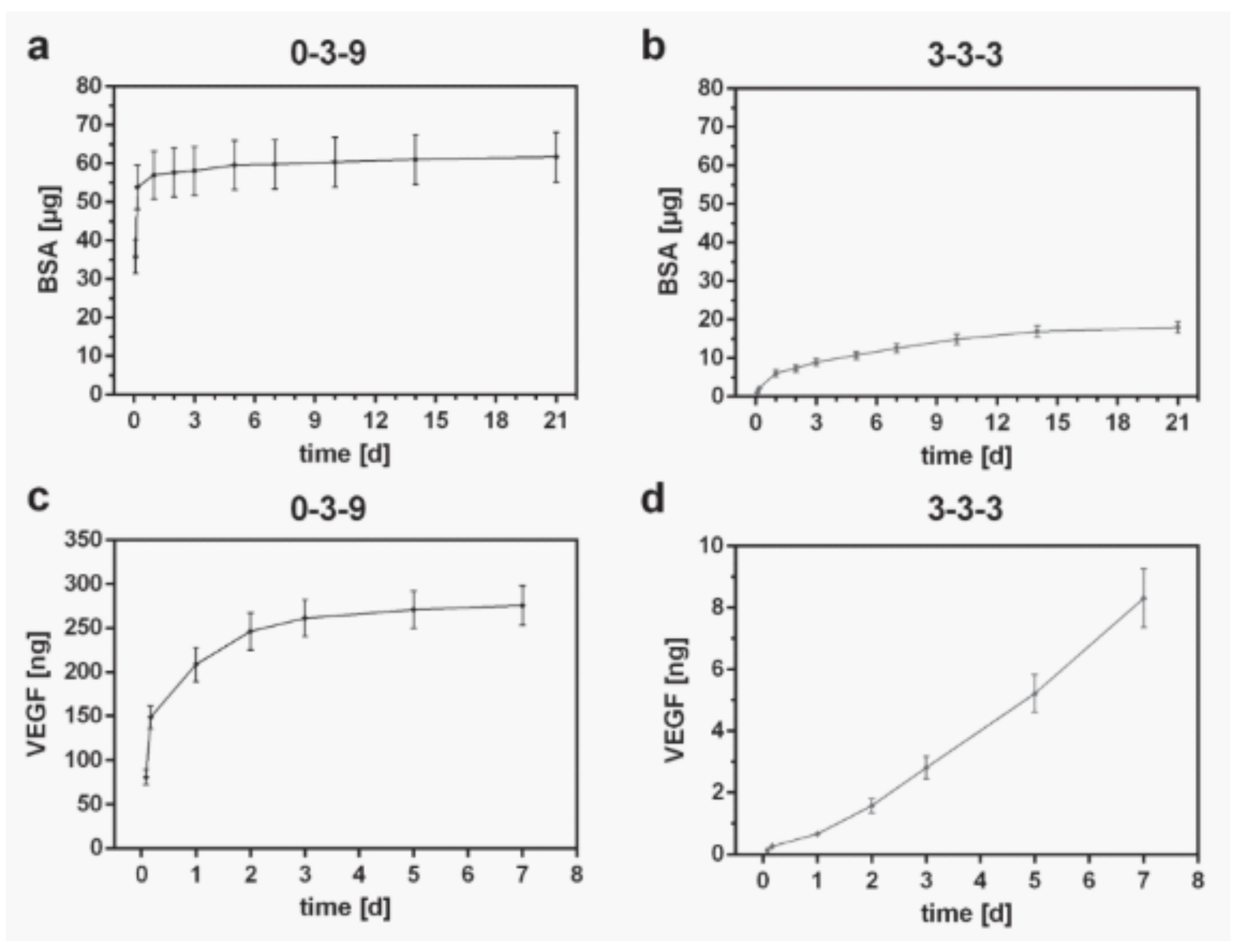
2.3.3. Carriers and Control Release of Functional Ingredients
2.3.4. Clay Minerals as Functional Ingredients of Bioinks and Biomaterial Inks
2.4. Mechanical Reinforcement of Bioinks and Biomaterial Inks
3. Future Prospects of Clay Minerals in 3D Bioprinting
4. Conclusions
- Functionalized or organo-modified layered phyllosilicates (montmorillonite or bentonite) are more prone to intercalate macromolecules within the interlayer space. This ability was proven to enhance the mechanical properties of macromolecules such as polymers;
- Fibrous (sepiolite and palygorskite) and tubular clay minerals (halloysite nanotubes) were also proven to enhance the mechanical properties of certain macromolecules by adjusting their orientation within the inkjet;
- Due to the chemical composition of clay minerals (aluminosilicates), they are promising materials for bone TE, with being able not only to provide mechanical resistance but also to trigger osteoinduction;
- Clay minerals were proven to induce cellular attachment, which is of great interest to add anchor points for cells when working with 3D constructs made of synthetic materials, for which cells usually do not show too much affinity;
- The high surface area of clay minerals makes them able to adsorb and carry a wide range of molecules. In fact, this feature was exploited throughout the years for the design and development of drug delivery systems. In the field of study at hand, clay minerals were proven to control the diffusion of growth factors within 3D constructs, something that could also be extended to the controlled release of other actives;
- Even if clay minerals are able to improve the viscosity of aqueous formulations, it is not possible to predict the final rheological behavior of the formulation. Rheological properties not only depend on the clay type and concentration but also on the preparation procedure and the different interactions between clay particles and the rest of the ingredients in the environment. Bearing in mind that BMIs and BI are usually complex mixtures, it is imperative to find the proper clay concentration for each formulation.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 3DBP | 3D bioprinting, bioprinting |
| 3DP | 3D printing |
| AGA | Agarose |
| ALG | Alginate |
| BI | Bioink |
| BMI | Biomaterial ink |
| BSA | Bovine serum albumin |
| CMC | Carboxymethylcellulose |
| CNT | Carbon nanotubes |
| CS | Chitosan |
| dcECM | De-cellularized cardiac extracellular matrix |
| dECM | De-cellularized extracellular matrix |
| GelMA | Gelatin methacryloyl |
| GG | Gellan gum |
| HA | Hyaluronic acid |
| HDPE | High-density polyethylene |
| HDPE | High-density polyethylene |
| HEK | Human embryonic kidney cells |
| HEMA | 2-hydroxyethyl methacrylate |
| HNTs | Halloysite nanotubes |
| HT | Hectorite, Bentone® MA |
| k-CA | kappa-carrageenan |
| LAP | Laponite |
| MC | Methylcellulose |
| MMT | Montmorillonite, bentonite, Veegum® HS |
| NAGA | N-acryloyl glycinamid |
| NIPAM | N-isopropyl acrylamide |
| PAAM | Polyacrylamide |
| PAL | Palygorskite or attapulgite |
| PEDOT | Poly(3,4-ethylenedioxythiophene) |
| PEG | Poly-ethylene glycol |
| PEGDA | Poly(ethylene glycol) di-acrylate |
| PEGDTT | poly(ethylene glycol)-dithiothreitol |
| PETG | Polyethylene glycol terephthalate |
| PLA | Polylactic acid |
| PMet-b-POxa | Poly(2-methyl-2-oxazoline)-b-poly(2-n-propyl-2-oxazine |
| PVA | Polyvinyl alcohol |
| PVDF | Polyvinylidene fluoride |
| SEM | Scanning Electron Microscopy |
| SEP | Sepiolite |
| SF | Silk fibroin |
| SPE | N-(3-Sulfopropyl)-N-methacroyloxyethyl-N,N-dimethylammonium betaine |
| TE | Tissue engineering |
| TEMPO BC | 2,2,6,6-tetramethyl-piperidinyl-1-oxyl-oxidized bacterial cellulose |
References
- Pedroza-González, S.C.; Rodriguez-Salvador, M.; Pérez-Benítez, B.; Alvarez, M.M.; Trujillo-de Santiago, G. Bioinks for 3D Bioprinting: A Scientometric Analysis of Two Decades of Progress. Int. J. Bioprint. 2021, 7, 68–91. [Google Scholar] [CrossRef]
- Groll, J.; Burdick, J.A.; Cho, D.W.; Derby, B.; Gelinsky, M.; Heilshorn, S.C.; Jüngst, T.; Malda, J.; Mironov, V.A.; Nakayama, K.; et al. A definition of bioinks and their distinction from biomaterial inks. Biofabrication 2019, 11, 13001. [Google Scholar] [CrossRef] [PubMed]
- Heid, S.; Boccaccini, A.R. Advancing bioinks for 3D bioprinting using reactive fillers: A review. Acta Biomater. 2020, 113, 1–22. [Google Scholar] [CrossRef]
- Schwab, A.; Levato, R.; D’Este, M.; Piluso, S.; Eglin, D.; Malda, J. Printability and Shape Fidelity of Bioinks in 3D Bioprinting. Chem. Rev. 2020, 120, 11028–11055. [Google Scholar] [CrossRef] [PubMed]
- Gu, Q.; Hao, J.; Lu, Y.J.; Wang, L.; Wallace, G.G.; Zhou, Q. Three-dimensional bio-printing. Sci. China Life Sci. 2015, 58, 411–419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manita, P.G.; Garcia-Orue, I.; Santos-Vizcaino, E.; Hernandez, R.-M.; Igartua, M. 3D Bioprinting of Functional Skin Substitutes: From Current Achievements to Future Goals. Pharmaceuticals 2021, 14, 362. [Google Scholar] [CrossRef] [PubMed]
- Deng, Z.; Hu, T.; Lei, Q.; He, J.; Ma, P.X.; Guo, B. Stimuli-Responsive Conductive Nanocomposite Hydrogels with High Stretchability, Self-Healing, Adhesiveness, and 3D Printability for Human Motion Sensing. ACS Appl. Mater. Interfaces 2019, 11, 6796–6808. [Google Scholar] [CrossRef]
- Papageorgiou, D.G.; Li, Z.; Liu, M.; Kinloch, I.A.; Young, R.J. Mechanisms of mechanical reinforcement by graphene and carbon nanotubes in polymer nanocomposites. Nanoscale 2020, 12, 2228–2267. [Google Scholar] [CrossRef] [Green Version]
- Chakraborty, A.; Roy, A.; Ravi, S.P.; Paul, A. Exploiting the role of nanoparticles for use in hydrogel-based bioprinting applications: Concept, design, and recent advances. Biomater. Sci. 2021, 9, 6337–6354. [Google Scholar] [CrossRef]
- Wang, S.; Li, R.; Qing, Y.; Wei, Y.; Wang, Q.; Zhang, T.; Sun, C.; Qin, Y.; Li, D.; Yu, J. Antibacterial activity of Ag-incorporated zincosilicate zeolite scaffolds fabricated by additive manufacturing. Inorg. Chem. Commun. 2019, 105, 31–35. [Google Scholar] [CrossRef]
- Guggenheim, S.; Martin, R.T. Definition of clay and clay mineral: Joint report of the AIPEA Nomenclature and CMS Nomenclature Committees. Clays Clay Miner. 1995, 43, 255–256. [Google Scholar] [CrossRef]
- Massaro, M.; Barone, G.; Barra, V.; Cancemi, P.; Di Leonardo, A.; Grossi, G.; Lo Celso, F.; Schenone, S.; Viseras Iborra, C.; Riela, S. Pyrazole[3,4-d]pyrimidine derivatives loaded into halloysite as potential CDK inhibitors. Int. J. Pharm. 2021, 599, 120281. [Google Scholar] [CrossRef]
- Bergaya, F.; Lagaly, G. General introduction: Clays, clay minerals and clay science. In Handbook of Clay Science; Bergaya, F., Theng, B.K., Lagaly, G., Eds.; Elsevier: Amsterdam, The Netherlands, 2006; pp. 1–18. ISBN 9780080441832. [Google Scholar]
- Christidis, G.E.; Aldana, C.; Chryssikos, G.D.; Gionis, V.; Kalo, H.; Stöter, M.; Breu, J.; Robert, J.-L. The Nature of Laponite: Pure Hectorite or a Mixture of Different Trioctahedral Phases? Minerals 2018, 8, 314. [Google Scholar] [CrossRef] [Green Version]
- Gaharwar, A.K.; Cross, L.M.; Peak, C.W.; Gold, K.; Carrow, J.K.; Brokesh, A.; Singh, K.A. 2D Nanoclay for Biomedical Applications: Regenerative Medicine, Therapeutic Delivery, and Additive Manufacturing. Adv. Mater. 2019, 31, 1900332. [Google Scholar] [CrossRef]
- Au, P.I.; Hassan, S.; Liu, J.; Leong, Y.K. Behaviour of laponite gels: Rheology, ageing, pH effect and phase state in the presence of dispersant. Chem. Eng. Res. Des. 2015, 101, 65–73. [Google Scholar] [CrossRef]
- Aguzzi, C.; Sánchez-Espejo, R.; Cerezo, P.; Machado, J.; Bonferoni, C.; Rossi, S.; Salcedo, I.; Viseras, C. Networking and rheology of concentrated clay suspensions “matured” in mineral medicinal water. Int. J. Pharm. 2013, 453, 473–479. [Google Scholar] [CrossRef]
- García-Villén, F.; Sánchez-Espejo, R.; López-Galindo, A.; Cerezo, P.; Viseras, C. Design and characterization of spring water hydrogels with natural inorganic excipients. Appl. Clay Sci. 2020, 197, 105772. [Google Scholar] [CrossRef]
- Lagaly, G. Colloid Clay Science. In Handbook of Clay Science; Bergaya, F., Theng, B., Lagaly, G., Eds.; Elsevier: Amsterdam, The Netherlands, 2006; pp. 141–245. ISBN 9780080441832. [Google Scholar]
- Beesetty, P.; Kale, A.; Patil, B.; Doddamani, M. Mechanical behavior of additively manufactured nanoclay/HDPE nanocomposites. Compos. Struct. 2020, 247, 112442. [Google Scholar] [CrossRef]
- Coppola, B.; Cappetti, N.; Di Maio, L.; Scarfato, P.; Incarnato, L. 3D printing of PLA/clay nanocomposites: Influence of printing temperature on printed samples properties. Materials 2018, 11, 1947. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coppola, B.; Cappetti, N.; Di Maio, L.; Scarfato, P.; Incarnato, L. Layered silicate reinforced polylactic acid filaments for 3D printing of polymer nanocomposites. In Proceedings of the RTSI 2017—IEEE 3rd International Forum on Research and Technologies for Society and Industry; IEEE: Piscataway, NJ, USA, 2017. [Google Scholar]
- Da Silva, D.; Kaduri, M.; Poley, M.; Adir, O.; Krinsky, N.; Shainsky-Roitman, J.; Schroeder, A. Biocompatibility, biodegradation and excretion of polylactic acid (PLA) in medical implants and theranostic systems. Chem. Eng. J. 2018, 340, 9–14. [Google Scholar] [CrossRef]
- Humayun, A.; Luo, Y.; Elumalai, A.; Mills, D.K. 3D printed antimicrobial PLA constructs functionalised with zinc- coated halloysite nanotubes-Ag-chitosan oligosaccharide lactate. Mater. Technol. 2020, 1–8. [Google Scholar] [CrossRef]
- Paspali, A.; Bao, Y.; Gawne, D.T.; Piestert, F.; Reinelt, S. The influence of nanostructure on the mechanical properties of 3D printed polylactide/nanoclay composites. Compos. Part B Eng. 2018, 152, 160–168. [Google Scholar] [CrossRef]
- Mahesh, V.; Joseph, A.S.; Mahesh, V.; Harursampath, D.; Chethan, V.N. Investigation on the mechanical properties of additively manufactured PETG composites reinforced with OMMT nanoclay and carbon fibers. Polym. Compos. 2021, 42, 2380–2395. [Google Scholar] [CrossRef]
- Kim, H.; Ryu, K.H.; Baek, D.; Khan, T.A.; Kim, H.J.; Shin, S.; Hyun, J.; Ahn, J.S.; Ahn, S.J.; Kim, H.J.; et al. 3D Printing of Polyethylene Terephthalate Glycol-Sepiolite Composites with Nanoscale Orientation. ACS Appl. Mater. Interfaces 2020, 12, 23453–23463. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, M.J.; Dixon, T.A.; Cohen, E.; Huang, W.; Omenetto, F.G.; Kaplan, D.L. 3D freeform printing of silk fibroin. Acta Biomater. 2018, 71, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Erol, O.; Pantula, A.; Liu, W.; Jiang, Z.; Kobayashi, K.; Chatterjee, D.; Hibino, N.; Romer, L.H.; Kang, S.H.; et al. Dual-Gel 4D Printing of Bioinspired Tubes. ACS Appl. Mater. Interfaces 2019, 11, 8492–8498. [Google Scholar] [CrossRef] [PubMed]
- Zhou, K.; Dey, M.; Ayan, B.; Zhang, Z.; Ozbolat, V.; Kim, M.H.; Khristov, V.; Ozbolat, I.T. Fabrication of PDMS microfluidic devices using nanoclay-reinforced Pluronic F-127 as a sacrificial ink. Biomed. Mater. 2021, 16, 45005. [Google Scholar] [CrossRef]
- Tarchitzky, J.; Chen, Y. Rheology of Sodium-montmorillonite suspensions. Soil Sci. Soc. Am. J. 2002, 66, 406–412. [Google Scholar]
- Pusch, R.; Zhang, L.; Adey, R.; Kasbohm, J. Rheology of an artificial smectitic clay. Appl. Clay Sci. 2010, 47, 120–126. [Google Scholar] [CrossRef]
- Abu-Jdayil, B. Rheology of sodium and calcium bentonite-water dispersions: Effect of electrolytes and aging time. Int. J. Miner. Process. 2011, 98, 208–213. [Google Scholar] [CrossRef]
- Khiari, I.; Sánchez-Espejo, R.; García-Villén, F.; Cerezo, P.; Aguzzi, C.; López-Galindo, A.; Jamoussi, F.; Viseras, C. Rheology and cation release of tunisian medina mud-packs intended for topical applications. Appl. Clay Sci. 2019, 171, 110–117. [Google Scholar] [CrossRef]
- Viseras, C.; Meeten, G.H.; Lopez-Galindo, A. Pharmaceutical grade phyllosilicate dispersions: The influence of shear history on floc structure. Int. J. Pharm. 1999, 182, 7–20. [Google Scholar] [CrossRef]
- Hernández, A.C.; Awad, M.E.; Meléndez, W.; González, G.; López-Galindo, A.; Sánchez-Espejo, R.; García-Villén, F.; Viseras, C. Colloidal and thermal behaviors of some venezuelan kaolin pastes for therapeutic applications. Minerals 2019, 9, 756. [Google Scholar] [CrossRef] [Green Version]
- Álvarez, A.; Santarén, J.; Esteban-Cubillo, A.; Aparicio, P. Current Industrial Applications of Palygorskite and Sepiolite. In Developments in Palygorskite-Sepiolite Research. A New Outlook of These Nanomaterials; Galán, E., Singer, A., Eds.; Elsevier B.V.: Oxford, UK, 2011; pp. 281–298. ISBN 978-0-444-53607-5. [Google Scholar]
- Okada, A.; Usuki, A. Twenty Years of Polymer-Clay Nanocomposites. Macromol. Mater. Eng. 2006, 291, 1449–1476. [Google Scholar] [CrossRef]
- Ruiz-Hitzky, E.; Aranda, P.; Darder, M.; Rytwo, G. Hybrid materials based on clays for environmental and biomedical applications. J. Mater. Chem. 2010, 20, 9306–9321. [Google Scholar] [CrossRef]
- Jin, Y.; Liu, C.; Chai, W.; Compaan, A.; Huang, Y. Self-supporting Nanoclay as Internal Scaffold Material for Direct Printing of Soft Hydrogel Composite Structures in Air. Appl. Mater. Interfaces 2017, 9, 17456–17465. [Google Scholar] [CrossRef]
- Mousa, M.; Evans, N.D.; Oreffo, R.O.C.; Dawson, J.I. Clay nanoparticles for regenerative medicine and biomaterial design: A review of clay bioactivity. Biomaterials 2018, 159, 204–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García-Villén, F.; Souza, I.M.S.; de Melo Barbosa, R.; Borrego-Sánchez, A.; Sánchez-Espejo, R.; Ojeda-Riascos, S.; Viseras, C. Natural inorganic ingredients in wound healing. Curr. Pharm. Des. 2020, 26, 621–641. [Google Scholar] [CrossRef]
- Sandri, G.; Bonferoni, M.C.; Rossi, S.; Ferrari, F.; Aguzzi, C.; Viseras, C.; Caramella, C. Clay minerals for tissue regeneration, repair, and engineering. In Wound Healing Biomaterials; Ågren, M.S., Ed.; Elsevier: Amsterdam, The Netherlands, 2016; pp. 385–402. ISBN 9781782424567. [Google Scholar]
- Pereira, I.; Saleh, M.; Nunes, C.; Reis, S.; Veiga, F.; Paiva-Santos, A.C. Preclinical developments of natural-occurring halloysite clay nanotubes in cancer therapeutics. Adv. Colloid Interface Sci. 2021, 291, 102406. [Google Scholar] [CrossRef] [PubMed]
- Srasra, E.; Bekri-Abbes, I. Bentonite Clays for Therapeutic Purposes and Biomaterial Design. Curr. Pharm. Des. 2020, 26, 642–649. [Google Scholar] [CrossRef]
- Santos, A.C.; Pereira, I.; Reis, S.; Veiga, F.; Saleh, M.; Lvov, Y. Biomedical potential of clay nanotube formulations and their toxicity assessment. Expert Opin. Drug Deliv. 2019, 16, 1169–1182. [Google Scholar] [CrossRef]
- Das, S.S.; Neelam; Hussain, K.S.; Singh, S.; Hussain, A.; Faruk, A.; Tebyetekerwa, M. Laponite-based nanomaterials for biomedical applications: A review. Curr. Pharm. Des. 2019, 25, 424–443. [Google Scholar] [CrossRef] [PubMed]
- Tomás, H.; Alves, C.S.; Rodrigues, J. Laponite®: A key nanoplatform for biomedical applications? Nanomed. Nanotechnol. Biol. Med. 2018, 14, 2407–2420. [Google Scholar] [CrossRef] [PubMed]
- Bakht Khosh Hagh, H.; Farshi Azhar, F. Reinforcing materials for polymeric tissue engineering scaffolds: A review. J. Biomed. Mater. Res. Part B Appl. Biomater. 2019, 107, 1560–1575. [Google Scholar] [CrossRef] [PubMed]
- Bertolino, V.; Cavallaro, G.; Milioto, S.; Lazzara, G. Polysaccharides/Halloysite nanotubes for smart bionanocomposite materials. Carbohydr. Polym. 2020, 245, 116502. [Google Scholar] [CrossRef]
- Naumenko, E.; Fakhrullin, R. Halloysite Nanoclay/Biopolymers Composite Materials in Tissue Engineering. Biotechnol. J. 2019, 14, e1900055. [Google Scholar] [CrossRef]
- Jamróz, E.; Kulawik, P.; Kopel, P. The effect of nanofillers on the functional properties of biopolymer-based films: A review. Polymers 2019, 11, 675. [Google Scholar] [CrossRef] [Green Version]
- Tenci, M.; Rossi, S.; Aguzzi, C.; Carazo, E.; Sandri, G.; Bonferoni, M.C.; Grisoli, P.; Viseras, C.; Caramella, C.M.; Ferrari, F. Carvacrol/clay hybrids loaded into in situ gelling films. Int. J. Pharm. 2017, 531, 676–688. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Zhang, Y.; Wu, C.; Xiong, S.; Zhou, C. Chitosan/halloysite nanotubes bionanocomposites: Structure, mechanical properties and biocompatibility. Int. J. Biol. Macromol. 2012, 51, 566–575. [Google Scholar] [CrossRef] [PubMed]
- Sirousazar, M.; Kokabi, M.; Hassan, Z.M. In vivo and cytotoxic assays of a poly(vinyl alcohol)/clay nanocomposite hydrogel wound dressing. J. Biomater. Sci. Polym. Ed. 2011, 22, 1023–1033. [Google Scholar] [CrossRef]
- Liu, M.; Jia, Z.; Jia, D.; Zhou, C. Recent advance in research on halloysite nanotubes-polymer nanocomposite. Prog. Polym. Sci. 2014, 39, 1498–1525. [Google Scholar] [CrossRef]
- Thakur, G.; Singh, A.; Singh, I. Formulation and evaluation of transdermal composite films of chitosan-montmorillonite for the delivery of curcumin. Int. J. Pharm. Investig. 2016, 6, 23–31. [Google Scholar]
- Gaharwar, A.K.; Schexnailder, P.J.; Kline, B.P.; Schmidt, G. Assessment of using Laponite® cross-linked poly(ethylene oxide) for controlled cell adhesion and mineralization. Acta Biomater. 2011, 7, 568–577. [Google Scholar] [CrossRef] [PubMed]
- Abduljauwad, S.N.; Ahmed, H. ur R. Enhancing cancer cell adhesion with clay nanoparticles for countering metastasis. Sci. Rep. 2019, 9, 5935. [Google Scholar] [CrossRef] [PubMed]
- Haraguchi, K. Development of soft nanocomposite materials and their applications in cell culture and tissue engineering. J. Stem Cells Regen. Med. 2012, 8, 2–11. [Google Scholar] [PubMed]
- García-Villén, F.; Carazo, E.; Borrego-Sánchez, A.; Sánchez-Espejo, R.; Cerezo, P.; Viseras, C.; Aguzzi, C. Clay minerals in drug delivery systems. In Modified Clay and Zeolite Nanocomposite Materials; Mercurio, M., Sarkar, B., Langella, A., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; ISBN 978-0-12-814617-0. [Google Scholar]
- Viseras, C.; Aguzzi, C.; Cerezo, P.; Bedmar, M.C. Biopolymer–clay nanocomposites for controlled drug delivery. Mater. Sci. Technol. 2008, 24, 1020–1026. [Google Scholar] [CrossRef]
- Quint, J.P.; Mostafavi, A.; Endo, Y.; Panayi, A.; Russell, C.S.; Nourmahnad, A.; Wiseman, C.; Abbasi, L.; Samandari, M.; Sheikhi, A.; et al. In Vivo Printing of Nanoenabled Scaffolds for the Treatment of Skeletal Muscle Injuries. Adv. Healthc. Mater. 2021, 10, 2002152. [Google Scholar] [CrossRef]
- Nerger, B.A.; Brun, P.T.; Nelson, C.M. Microextrusion printing cell-laden networks of type I collagen with patterned fiber alignment and geometry. Soft Matter 2019, 15, 5728–5738. [Google Scholar] [CrossRef]
- Hölzl, K.; Lin, S.; Tytgat, L.; Van Vlierberghe, S.; Gu, L.; Ovsianikov, A. Bioink properties before, during and after 3D bioprinting. Biofabrication 2016, 8, 032002. [Google Scholar] [CrossRef]
- Donderwinkel, I.; Van Hest, J.C.M.; Cameron, N.R. Bio-inks for 3D bioprinting: Recent advances and future prospects. Polym. Chem. 2017, 8, 4451–4471. [Google Scholar] [CrossRef] [Green Version]
- Abd-Elsatar, A.G.; Farag, M.M.; Youssef, H.F.; Salih, S.A.; Mounier, M.M.; El-Meliegy, E. Different zeolite systems for colon cancer therapy: Monitoring of ion release, cytotoxicity and drug release behavior. Prog. Biomater. 2019, 8, 101–113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cooke, M.E.; Rosenzweig, D.H. The rheology of direct and suspended extrusion bioprinting. APL Bioeng. 2020, 5, 1–20. [Google Scholar]
- Gold, K.A.; Saha, B.; Rajeeva Pandian, N.K.; Walther, B.K.; Palma, J.A.; Jo, J.; Cooke, J.P.; Jain, A.; Gaharwar, A.K. 3D Bioprinted Multicellular Vascular Models. Adv. Healthc. Mater. 2021, 2101141. [Google Scholar]
- Habib, M.A.; Khoda, B. Development of clay based novel bio-ink for 3D bio-printing process. Procedia Manuf. 2018, 26, 846–856. [Google Scholar] [CrossRef]
- Zhai, X.; Ruan, C.; Ma, Y.; Cheng, D.; Wu, M.; Liu, W.; Zhao, X.; Pan, H.; Lu, W.W. 3D-Bioprinted Osteoblast-Laden Nanocomposite Hydrogel Constructs with Induced Microenvironments Promote Cell Viability, Differentiation, and Osteogenesis both In Vitro and In Vivo. Adv. Sci. 2018, 5, 1700550. [Google Scholar] [CrossRef] [Green Version]
- Cidonio, G.; Alcala-Orozco, C.R.; Lim, K.S.; Glinka, M.; Mutreja, I.; Kim, Y.H.; Dawson, J.I.; Woodfield, T.B.F.; Oreffo, R.O.C. Osteogenic and angiogenic tissue formation in high fidelity nanocomposite Laponite-gelatin bioinks. Biofabrication 2019, 11, 35027. [Google Scholar] [CrossRef]
- Ahlfeld, T.; Cidonio, G.; Kilian, D.; Duin, S.; Akkineni, A.R.; Dawson, J.I.; Yang, S.; Lode, A.; Oreffo, R.O.C.; Gelinsky, M. Development of a clay based bioink for 3D cell printing for skeletal application. Biofabrication 2017, 9, 34103. [Google Scholar] [CrossRef]
- Peak, C.W.; Stein, J.; Gold, K.A.; Gaharwar, A.K. Nanoengineered Colloidal Inks for 3D Bioprinting. Langmuir 2018, 34, 917–925. [Google Scholar] [CrossRef]
- Stanco, D.; Boffito, M.; Bogni, A.; Puricelli, L.; Barrero, J.; Soldati, G.; Ciardelli, G. 3D bioprinting of human adipose-derived stem cells and their tenogenic differentiation in clinical-grade medium. Int. J. Mol. Sci. 2020, 21, 8694. [Google Scholar] [CrossRef]
- Hu, X.; Man, Y.; Li, W.; Li, L.; Xu, J.; Parungao, R.; Wang, Y.; Zheng, S.; Nie, Y.; Liu, T.; et al. 3D bio-printing of CS/Gel/HA/Gr hybrid osteochondral scaffolds. Polymers 2019, 11, 1601. [Google Scholar] [CrossRef] [Green Version]
- Bociaga, D.; Bartniak, M.; Grabarczyk, J.; Przybyszewska, K. Sodium alginate/gelatine hydrogels for direct bioprinting-the effect of composition selection and applied solvents on the bioink properties. Materials 2019, 12, 2669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lafuente-Merchan, M.; Ruiz-Alonso, S.; Espona-Noguera, A.; Galvez-Martin, P.; López-Ruiz, E.; Marchal, J.A.; López-Donaire, M.L.; Zabala, A.; Ciriza, J.; Saenz-del-Burgo, L.; et al. Development, characterization and sterilisation of Nanocellulose-alginate-(hyaluronic acid)- bioinks and 3D bioprinted scaffolds for tissue engineering. Mater. Sci. Eng. C 2021, 126, 112160. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, R.R.; Ullah, M.W.; Booth, P.; Pei, E.; Yang, G. The use of bacterial polysaccharides in bioprinting. Biotechnol. Adv. 2019, 37, 107448. [Google Scholar] [CrossRef] [PubMed]
- Morgan, H.; Tseng, S.Y.; Gallais, Y.; Leineweber, M.; Buchmann, P.; Riccardi, S.; Nabhan, M.; Lo, J.; Gani, Z.; Szely, N.; et al. Evaluation of in vitro assays to assess the modulation of dendritic cells functions by therapeutic antibodies and aggregates. Front. Immunol. 2019, 10, 601. [Google Scholar] [CrossRef]
- Schmieg, B.; Schimek, A.; Franzreb, M. Development and performance of a 3D-printable poly(ethylene glycol) diacrylate hydrogel suitable for enzyme entrapment and long-term biocatalytic applications. Eng. Life Sci. 2018, 18, 659–667. [Google Scholar] [CrossRef] [Green Version]
- Peak, C.W.; Singh, K.A.; Adlouni, M.; Chen, J.; Gaharwar, A.K. Printing Therapeutic Proteins in 3D using Nanoengineered Bioink to Control and Direct Cell Migration. Adv. Healthc. Mater. 2019, 8, 1801553. [Google Scholar] [CrossRef]
- Liu, M.; Zhang, T.; Long, L.; Zhang, R.; Ding, S. Efficient enzymatic degradation of poly (ɛ-caprolactone) by an engineered bifunctional lipase-cutinase. Polym. Degrad. Stab. 2019, 160, 120–125. [Google Scholar] [CrossRef]
- Yao, B.; Hu, T.; Cui, X.; Song, W.; Fu, X.; Huang, S. Enzymatically degradable alginate/gelatin bioink promotes cellular behavior and degradation in vitro and in vivo. Biofabrication 2019, 11, 45020. [Google Scholar] [CrossRef]
- Byambaa, B.; Annabi, N.; Yue, K.; Trujillo-de Santiago, G.; Alvarez, M.M.; Jia, W.; Kazemzadeh-Narbat, M.; Shin, S.R.; Tamayol, A.; Khademhosseini, A. Bioprinted Osteogenic and Vasculogenic Patterns for Engineering 3D Bone Tissue. Adv. Healthc. Mater. 2017, 6, 1700015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freeman, F.E.; Kelly, D.J. Tuning alginate bioink stiffness and composition for controlled growth factor delivery and to spatially direct MSC Fate within bioprinted tissues. Sci. Rep. 2017, 7, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, X.; Kim, G.J.; Kang, M.G.; Lee, J.K.; Seo, J.W.; Do, J.T.; Hong, K.; Cha, J.M.; Shin, S.R.; Bae, H. Marine biomaterial-Based bioinks for generating 3D printed tissue constructs. Mar. Drugs 2018, 16, 484. [Google Scholar] [CrossRef] [Green Version]
- Antich, C.; de Vicente, J.; Jiménez, G.; Chocarro, C.; Carrillo, E.; Montañez, E.; Gálvez-Martín, P.; Marchal, J.A. Bio-inspired hydrogel composed of hyaluronic acid and alginate as a potential bioink for 3D bioprinting of articular cartilage engineering constructs. Acta Biomater. 2020, 106, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Zhai, X.; Ma, Y.; Hou, C.; Gao, F.; Zhang, Y.; Ruan, C.; Pan, H.; Lu, W.W.; Liu, W. 3D-Printed High Strength Bioactive Supramolecular Polymer/Clay Nanocomposite Hydrogel Scaffold for Bone Regeneration. ACS Biomater. Sci. Eng. 2017, 3, 1109–1118. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Hui, A.; Zhao, H.; Ye, X.; Zhang, C.; Wang, A.; Zhang, C. A novel 3D-bioprinted porous nano attapulgite scaffolds with good performance for bone regeneration. Int. J. Nanomed. 2020, 15, 6945–6960. [Google Scholar] [CrossRef] [PubMed]
- Zineh, B.R.; Shabgard, M.R.; Roshangar, L. Mechanical and biological performance of printed alginate/methylcellulose/halloysite nanotube/polyvinylidene fluoride bio-scaffolds. Mater. Sci. Eng. C 2018, 92, 779–789. [Google Scholar] [CrossRef]
- Shin, Y.J.; Shafranek, R.T.; Tsui, J.H.; Walcott, J.; Nelson, A.; Kim, D.H. 3D bioprinting of mechanically tuned bioinks derived from cardiac decellularized extracellular matrix. Acta Biomater. 2021, 119, 75–88. [Google Scholar] [CrossRef]
- Liu, M.; Dai, L.; Shi, H.; Xiong, S.; Zhou, C. In vitro evaluation of alginate/halloysite nanotube composite scaffolds for tissue engineering. Mater. Sci. Eng. C 2015, 49, 700–712. [Google Scholar] [CrossRef] [PubMed]
- Pazarçeviren, E.; Erdemli, Ö.; Keskin, D.; Tezcaner, A. Clinoptilolite/PCL-PEG-PCL composite scaffolds for bone tissue engineering applications. J. Biomater. Appl. 2017, 31, 1148–1168. [Google Scholar] [CrossRef] [PubMed]
- Bonifacio, M.A.; Gentile, P.; Ferreira, A.M.; Cometa, S.; De Giglio, E. Insight into halloysite nanotubes-loaded gellan gum hydrogels for soft tissue engineering applications. Carbohydr. Polym. 2017, 163, 280–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, Q.; Niu, X.; Shao, L.; Zhou, L.; Lin, Z.; Sun, A.; Fu, J.; Chen, Z.; Hu, J.; Liu, Y.; et al. 3D printing of complex GelMA-based scaffolds with nanoclay. Biofabrication 2019, 11, 35006. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.; Sycks, D.; Chan, H.F.; Lin, S.; Lopez, G.P.; Guilak, F.; Leong, K.W.; Zhao, X. 3D Printing of Highly Stretchable and Tough Hydrogels into Complex, Cellularized Structures. Adv. Mater. 2015, 27, 4035–4040. [Google Scholar] [CrossRef] [Green Version]
- Cai, F.F.; Heid, S.; Boccaccini, A.R. Potential of laponite incorporated oxidized alginate–gelatin (ADA-GEL) composite hydrogels for extrusion-based 3D printing. J. Biomed. Mater. Res. Part B Appl. Biomater. 2020, 109, 1090–1104. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Zhang, R.; Zhang, L.; Cao, X. 4D printing of robust hydrogels consisted of agarose nanofibers and polyacrylamide. ACS Macro Lett. 2018, 7, 442–446. [Google Scholar] [CrossRef]
- Tondera, C.; Akbar, T.F.; Thomas, A.K.; Lin, W.; Werner, C.; Busskamp, V.; Zhang, Y.; Minev, I.R. Highly conductive, stretchable, and cell-adhesive hydrogel by nanoclay doping. Small 2019, 15, 1901406. [Google Scholar] [CrossRef] [PubMed]
- McCracken, J.M.; Rauzan, B.M.; Kjellman, J.C.E.; Kandel, M.E.; Liu, Y.H.; Badea, A.; Miller, L.A.; Rogers, S.A.; Popescu, G.; Nuzzo, R.G. 3D-Printed Hydrogel Composites for Predictive Temporal (4D) Cellular Organizations and Patterned Biogenic Mineralization. Adv. Healthc. Mater. 2019, 8, 1800788. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, C.; Hahn, L.; Yang, M.; Altmann, A.; Stahlhut, P.; Rgen Groll, J.; Luxenhofer, R. Improving printability of a thermoresponsive hydrogel biomaterial ink by nanoclay addition. J. Mater. Sci. 2020, 56, 691–705. [Google Scholar] [CrossRef]
- Sällström, N.; Capel, A.; Lewis, M.P.; Engstrøm, D.S.; Martin, S. 3D-printable zwitterionic nano-composite hydrogel system for biomedical applications. J. Tissue Eng. 2020, 11, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Wang, B.; Li, Z.; Wu, Z.; Zhang, M.; Sheng, N.; Liang, Q.; Wang, H.; Chen, S. A 3D-printable TEMPO-oxidized bacterial cellulose/alginate hydrogel with enhanced stability via nanoclay incorporation. Carbohydr. Polym. 2020, 238, 116207. [Google Scholar] [CrossRef] [PubMed]
- Alexa, R.L.; Iovu, H.; Trica, B.; Zaharia, C.; Serafim, A.; Alexandrescu, E.; Radu, I.C.; Vlasceanu, G.; Preda, S.; Ninciuleanu, C.M.; et al. Assessment of naturally sourced mineral clays for the 3D printing of biopolymer-based nanocomposite inks. Nanomaterials 2021, 11, 703. [Google Scholar] [CrossRef]
- Guimarães, C.F.; Gasperini, L.; Marques, A.P.; Reis, R.L. The stiffness of living tissues and its implications for tissue engineering. Nat. Rev. Mater. 2020, 5, 351–370. [Google Scholar] [CrossRef]
- Dávila, J.L.; d’Ávila, M.A. Laponite as a rheology modifier of alginate solutions: Physical gelation and aging evolution. Carbohydr. Polym. 2017, 157, 1–8. [Google Scholar] [CrossRef]
- Sears, C.; Mondragon, E.; Richards, Z.I.; Sears, N.; Chimene, D.; McNeill, E.P.; Gregory, C.A.; Gaharwar, A.K.; Kaunas, R. Conditioning of 3D Printed Nanoengineered Ionic–Covalent Entanglement Scaffolds with iP-hMSCs Derived Matrix. Adv. Healthc. Mater. 2020, 9, 1901580. [Google Scholar] [CrossRef]
- Jatav, S.; Joshi, Y.M. Chemical stability of Laponite in aqueous media. Appl. Clay Sci. 2014, 97–98, 72–77. [Google Scholar] [CrossRef] [Green Version]
- Sánchez, C.J.; Parras, J.; Carretero, M.I. The effect of maturation upon the mineralogical and physicochemical properties of illitic-smectitic clays for pelotherapy. Clay Miner. 2002, 37, 457–463. [Google Scholar] [CrossRef]
- Sánchez-Espejo, R.; Cerezo, P.; Aguzzi, C.; López-Galindo, A.; Machado, J.; Viseras, C. Physicochemical and in vitro cation release relevance of therapeutic muds “maturation”. Appl. Clay Sci. 2015, 116–117, 1–7. [Google Scholar] [CrossRef]
- Topuz, F.; Nadernezhad, A.; Caliskan, O.S.; Menceloglu, Y.Z.; Koc, B. Nanosilicate embedded agarose hydrogels with improved bioactivity. Carbohydr. Polym. 2018, 201, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.A.; Cross, L.M.; Peak, C.W.; Gaharwar, A.K. Shear-Thinning and Thermo-Reversible Nanoengineered Inks for 3D Bioprinting. ACS Appl. Mater. Interfaces 2017, 9, 43449–43458. [Google Scholar] [CrossRef] [PubMed]
- Cidonio, G.; Glinka, M.; Kim, Y.H.; Kanczler, J.M.; Lanham, S.A.; Ahlfeld, T.; Lode, A.; Dawson, J.I.; Gelinsky, M.; Oreffo, R.O.C. Nanoclay-based 3D printed scaffolds promote vascular ingrowth ex vivo and generate bone mineral tissue in vitro and in vivo. Biofabrication 2020, 12, 35010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cidonio, G.; Cooke, M.; Glinka, M.; Dawson, J.I.; Grover, L.; Oreffo, R.O.C. Printing bone in a gel: Using nanocomposite bioink to print functionalised bone scaffolds. Mater. Today Bio 2019, 4, 100028. [Google Scholar] [CrossRef] [PubMed]
- Carrow, J.K.; Cross, L.M.; Reese, R.W.; Jaiswal, M.K.; Gregory, C.A.; Kaunas, R.; Singh, I.; Gaharwar, A.K. Widespread changes in transcriptome profile of human mesenchymal stem cells induced by two-dimensional nanosilicates. Proc. Natl. Acad. Sci. USA 2018, 115, E3905–E3913. [Google Scholar] [CrossRef] [Green Version]
- Castro-Smirnov, F.A.; Ayache, J.; Bertrand, J.R.; Dardillac, E.; Le Cam, E.; Piétrement, O.; Aranda, P.; Ruiz-Hitzky, E.; Lopez, B.S. Cellular uptake pathways of sepiolite nanofibers and DNA transfection improvement. Sci. Rep. 2017, 7, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Long, Z.; Zhang, J.; Shen, Y.; Zhou, C.; Liu, M. Polyethyleneimine grafted short halloysite nanotubes for gene delivery. Mater. Sci. Eng. C 2017, 81, 224–235. [Google Scholar] [CrossRef]
- Salcedo, I.; Aguzzi, C.; Sandri, G.; Bonferoni, M.C.; Mori, M.; Cerezo, P.; Sánchez, R.; Viseras, C.; Caramella, C. In vitro biocompatibility and mucoadhesion of montmorillonite chitosan nanocomposite: A new drug delivery. Appl. Clay Sci. 2012, 55, 131–137. [Google Scholar] [CrossRef]
- Naumenko, E.A.; Guryanov, I.D.; Yendluri, R.; Lvov, Y.M.; Fakhrullin, R.F. Clay nanotube-biopolymer composite scaffolds for tissue engineering. Nanoscale 2016, 8, 7257–7271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García-Villén, F.; Carazo, E.; Borrego-Sánchez, A.; Sánchez-Espejo, R.; Cerezo, P.; Viseras, C.; Aguzzi, C. Clay minerals in drug delivery systems. In Modified Clay and Zeolite Nanocomposite Materials: Environmental and Pharmaceutical Applications; Elsevier: Amsterdam, The Netherlands, 2018; pp. 129–166. ISBN 9780128146187. [Google Scholar]
- Viseras, C.; Carazo, E.; Borrego-Sánchez, A.; García-Villén, F.; Sánchez-Espejo, R.; Cerezo, P.; Aguzzi, C. Clay minerals in skin drug delivery. Clays Clay Miner. 2019, 67, 59–71. [Google Scholar] [CrossRef]
- Carretero, M.I. Clay minerals and their beneficial effects upon human health. A review. Appl. Clay Sci. 2002, 21, 155–163. [Google Scholar] [CrossRef]
- Purwada, A.; Singh, A. Immuno-engineered organoids for regulating the kinetics of B-cell development and antibody production. Nat. Protoc. 2017, 12, 168–182. [Google Scholar] [CrossRef]
- Jurkić, L.M.; Cepanec, I.; Pavelić, S.K.; Pavelić, K. Biological and therapeutic effects of ortho-silicic acid and some ortho-silicic acid-releasing compounds: New perspectives for therapy. Nutr. Metab. 2013, 10, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Afewerki, S.; Magalhães, L.S.S.M.; Silva, A.D.R.; Stocco, T.D.; Silva Filho, E.C.; Marciano, F.R.; Lobo, A.O. Bioprinting a Synthetic Smectic Clay for Orthopedic Applications. Adv. Healthc. Mater. 2019, 8, 1900158. [Google Scholar] [CrossRef]
- Mieszawska, A.J.; Llamas, J.G.; Vaiana, C.A.; Kadakia, M.P.; Naik, R.R.; Kaplan, D.L. Clay enriched silk biomaterials for bone formation. Acta Biomater. 2011, 7, 3036–3041. [Google Scholar] [CrossRef] [Green Version]
- Gaharwar, A.K.; Mihaila, S.M.; Swami, A.; Patel, A.; Sant, S.; Reis, R.L.; Marques, A.P.; Gomes, M.E.; Khademhosseini, A. Bioactive silicate nanoplatelets for osteogenic differentiation of human mesenchymal stem cells. Adv. Mater. 2013, 25, 3329–3336. [Google Scholar] [CrossRef]
- Mihaila, S.M.; Gaharwar, A.K.; Reis, R.L.; Khademhosseini, A.; Marques, A.P.; Gomes, M.E. The osteogenic differentiation of SSEA-4 sub-population of human adipose derived stem cells using silicate nanoplatelets. Biomaterials 2014, 35, 9087–9099. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, T.; Liu, Z.L.; Xiao, M.; Yang, Z.Z.; Peng, M.Z.; Di Li, C.; Zhou, X.J.; Wang, J.W. Impact of bone marrow mesenchymal stem cell immunomodulation on the osteogenic effects of laponite. Stem Cell Res. Ther. 2018, 9, 100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freeman, F.E.; Pitacco, P.; van Dommelen, L.H.A.; Nulty, J.; Browe, D.C.; Shin, J.-Y.; Alsberg, E.; Kelly, D.J. 3D bioprinting spatiotemporally defined patterns of growth factors to tightly control tissue regeneration. Sci. Adv. 2020, 6, eabb5093. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Hitzky, E.; Meerbeek, A. Van Clay Mineral—And organoclay—Polymer nanocomposite. In Handbook of Clay Science; Bergaya, F., Theng, B.K.G., Lagaly, G., Eds.; Elsevier: Amsterdam, The Netherlands, 2006; pp. 583–621. [Google Scholar]
- Andrejkovičová, S.; Velosa, A.L.; Ferraz, E.; Rocha, F. Influence of clay minerals addition on mechanical properties of air lime-metakaolin mortars. Constr. Build. Mater. 2014, 65, 132–139. [Google Scholar] [CrossRef]
- Xu, J.; Wang, A. Electrokinetic and colloidal properties of homogenized and unhomogenized palygorskite in the presence of electrolytes. J. Chem. Eng. Data 2012, 57, 1586–1593. [Google Scholar] [CrossRef]
- Neaman, A.; Singer, A. Rheology of mixed palygorskite-montmorillonite suspensions. Clays Clay Miner. 2000, 48, 713–715. [Google Scholar] [CrossRef]
- Mironova, M.V.; Ilyin, S.O. Effect of silica and clay minerals on rheology of heavy crude oil emulsions. Fuel 2018, 232, 290–298. [Google Scholar] [CrossRef]
- Panda, B.; Ruan, S.; Unluer, C.; Tan, M.J. Improving the 3D printability of high volume fly ash mixtures via the use of nano attapulgite clay. Compos. Part B Eng. 2019, 165, 75–83. [Google Scholar] [CrossRef]
- Chougan, M.; Ghaffar, S.H.; Sikora, P.; Chung, S.Y.; Rucinska, T.; Stephan, D.; Albar, A.; Swash, M.R. Investigation of additive incorporation on rheological, microstructural and mechanical properties of 3D printable alkali-activated materials. Mater. Des. 2021, 202, 109574. [Google Scholar] [CrossRef]
- Aguzzi, C.; Sandri, G.; Cerezo, P.; Carazo, E.; Viseras, C. Health and medical applications of tubular clay minerals. In Developments in clay science; Elsevier: Amsterdam, The Netherlands, 2016; Volume 7, pp. 708–725. ISBN 9780081002933. [Google Scholar]
- Wu, F.; Zheng, J.; Li, Z.; Liu, M. Halloysite nanotubes coated 3D printed PLA pattern for guiding human mesenchymal stem cells (hMSCs) orientation. Chem. Eng. J. 2019, 359, 672–683. [Google Scholar] [CrossRef]
- Shahbazi, M.; Jäger, H.; Ahmadi, S.J.; Lacroix, M. Electron beam crosslinking of alginate/nanoclay ink to improve functional properties of 3D printed hydrogel for removing heavy metal ions. Carbohydr. Polym. 2020, 240, 116211. [Google Scholar] [CrossRef] [PubMed]
- Yadav, H.K.S.; Kasina, S.; Raizaday, A. Sunscreens. In Nanobiomaterials in Galenic Formulations and Cosmetics: Applications of Nanobiomaterials; Grumezescu, A.M., Ed.; Elsevier Inc.: Oxford, UK, 2016; pp. 201–230. ISBN 978-0-323-42868-2. [Google Scholar]
- Ghadiri, M.; Chrzanowski, W.; Rohanizadeh, R. Biomedical applications of cationic clay minerals. RSC Adv. 2015, 5, 29467–29481. [Google Scholar] [CrossRef]
- Moraes, J.D.D.; Bertolino, S.R.A.; Cuffini, S.L.; Ducart, D.F.; Bretzke, P.E.; Leonardi, G.R. Clay minerals: Properties and applications to dermocosmetic products and perspectives of natural raw materials for therapeutic purposes—A review. Int. J. Pharm. 2017, 534, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Francis, V.; Jain, P.K. Investigation on the effect of surface modification of 3D printed parts by nanoclay and dimethyl ketone. Mater. Manuf. Process. 2018, 33, 1080–1092. [Google Scholar] [CrossRef]




| Properties | 3DBP | 3DP |
|---|---|---|
| Nature, type and characteristics of the ink ingredients | Biological and biocompatible materials (BMI), sometimes laden with human or mammalian cells (BI). Liquid or semisolid, gel-like materials (aqueous-rich). Usually, post-processing steps are needed to improve the resistance and manageability of the construct (chemical or physical crosslinking methods such as light-based crosslinking, among many others). | Molten plastics, synthetic polymers, metal alloys, ceramics, concrete, etc. Solid, semisolid, biocompatible or non-biocompatible materials. Minimal/absent post-processing. |
| Printer features | The “bioprinters” require less robustness: they usually work at low temperatures, pressures, speeds, etc. These mild working conditions guarantee cellular viability. High precision is mandatory to reproduce native tissue structures. | Robust equipment, able to work in extreme conditions (high temperatures and/or pressures). No need to ensure cellular viability. Precision depends on the item and its final scope (i.e., less precision for building industry; higher for microchips or microfluidics). |
| Most frequently used techniques | Extrusion-based bioprinting, droplet (or inkjet) bioprinting and laser-based bioprinting. | Fused-deposition modelling, selective laser sintering, stereolithography, multi-jet fusion. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Villén, F.; Ruiz-Alonso, S.; Lafuente-Merchan, M.; Gallego, I.; Sainz-Ramos, M.; Saenz-del-Burgo, L.; Pedraz, J.L. Clay Minerals as Bioink Ingredients for 3D Printing and 3D Bioprinting: Application in Tissue Engineering and Regenerative Medicine. Pharmaceutics 2021, 13, 1806. https://doi.org/10.3390/pharmaceutics13111806
García-Villén F, Ruiz-Alonso S, Lafuente-Merchan M, Gallego I, Sainz-Ramos M, Saenz-del-Burgo L, Pedraz JL. Clay Minerals as Bioink Ingredients for 3D Printing and 3D Bioprinting: Application in Tissue Engineering and Regenerative Medicine. Pharmaceutics. 2021; 13(11):1806. https://doi.org/10.3390/pharmaceutics13111806
Chicago/Turabian StyleGarcía-Villén, Fátima, Sandra Ruiz-Alonso, Markel Lafuente-Merchan, Idoia Gallego, Myriam Sainz-Ramos, Laura Saenz-del-Burgo, and Jose Luis Pedraz. 2021. "Clay Minerals as Bioink Ingredients for 3D Printing and 3D Bioprinting: Application in Tissue Engineering and Regenerative Medicine" Pharmaceutics 13, no. 11: 1806. https://doi.org/10.3390/pharmaceutics13111806
APA StyleGarcía-Villén, F., Ruiz-Alonso, S., Lafuente-Merchan, M., Gallego, I., Sainz-Ramos, M., Saenz-del-Burgo, L., & Pedraz, J. L. (2021). Clay Minerals as Bioink Ingredients for 3D Printing and 3D Bioprinting: Application in Tissue Engineering and Regenerative Medicine. Pharmaceutics, 13(11), 1806. https://doi.org/10.3390/pharmaceutics13111806








