Defining a Regulatory Strategy for ATMP/Aerosol Delivery Device Combinations in the Treatment of Respiratory Disease
Abstract
1. Introduction
2. Cellular Therapy
2.1. Mesenchymal Stromal Cells
2.2. The Secretome
2.3. Extracellular Vesicles
3. Respiratory Diseases
3.1. Acute Respiratory Distress Syndrome
3.2. Chronic Obstructive Pulmonary Disease (COPD)
3.3. Asthma
3.4. Sepsis
3.5. COVID-19
4. Routes of Administration for the Treatment of Respiratory Diseases
4.1. Combination Product Development—Selecting the Delivery Device
4.2. The Feasibility of Aerosol-Mediated ATMP Delivery
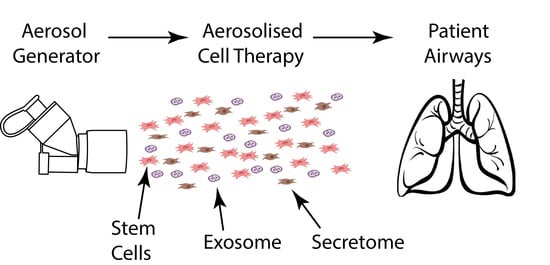
5. Rationale for Aerosol-Mediated Delivery of Cellular Therapies
6. Regulatory Framework for ATMP/Device Combination
6.1. EU Requirements
6.2. US Requirements
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Scavone, C.; di Mauro, G.; Mascolo, A.; Berrino, L.; Rossi, F.; Capuano, A. The new paradigms in clinical research: From early access programs to the novel therapeutic approaches for unmet medical needs. Front. Pharmacol. 2019, 10, 111. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.T.; Gupta, P.; Ronfard, V.; Vertès, A.A.; Bayon, Y. Recent progress in European advanced therapy medicinal products and beyond. Front. Bioeng. Biotechnol. 2018, 6, 130. [Google Scholar] [CrossRef] [PubMed]
- Regulation, E. No. 1394/2007 of the European Parliament and of the Council of 13 November 2007 on advanced therapy medicinal products and amending directive 2001/83/EC and regulation (EC) no 726/2004. J. Eur. Union 2007, 324, 121–137. [Google Scholar]
- Flory, E.; Reinhardt, J. European regulatory tools for advanced therapy medicinal products. Transfus. Med. Hemother. 2013, 40, 409–412. [Google Scholar] [CrossRef] [PubMed]
- Commission, E. Editor Commission Directive 2009/120/EC of 14 September 2009 amending Directive 2001/83/EC of the European Parliament and of the Council on the Community code relating to medicinal products for human use as regards advanced therapy medicinal products. Off. J. Eur. Union 2009, 159, L242/3–12. [Google Scholar]
- Zakrzewski, W.; Dobrzyński, M.; Szymonowicz, M.; Rybak, Z. Stem cells: Past, present, and future. Stem Cell Res. Ther. 2019, 10, 22. [Google Scholar] [CrossRef]
- Nelson, T.J.; Behfar, A.; Terzic, A. Strategies for therapeutic repair: The “R3” regenerative medicine paradigm. Clin. Transl. Sci. 2008, 1, 168–171. [Google Scholar] [CrossRef]
- Cuende, N.; Rasko, J.E.; Koh, M.B.; Dominici, M.; Ikonomou, L. Cell, tissue and gene products with marketing authorization in 2018 worldwide. Cytotherapy 2018, 20, 1401–1413. [Google Scholar] [CrossRef]
- Trounson, A. Why Stem Cell Research? Advances in the Field. Essentials of Stem Cell Biology; Elsevier: Amsterdam, The Netherlands, 2014; pp. 3–6. [Google Scholar]
- U.S. Food and Drug Administration. Regenerative Medicine Advanced Therapy Designation 2019. Available online: https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/regenerative-medicine-advanced-therapy-designation (accessed on 24 September 2020).
- Aurora, A.B.; Olson, E.N. Immune modulation of stem cells and regeneration. Cell Stem Cell 2014, 15, 14–25. [Google Scholar] [CrossRef]
- Till, J.E.; McCulloch, E.A. Hemopoietic stem cell differentiation. Biochim. Biophys. Acta BBA Rev. Cancer 1980, 605, 431–459. [Google Scholar] [CrossRef]
- Weissman, I.L. Stem cells: Units of development, units of regeneration, and units in evolution. Cell 2000, 100, 157–168. [Google Scholar] [PubMed]
- Caplan, A. Why are MSCs therapeutic? New data: New insight. J. Pathol. Soc. G. B. Irel. 2009, 217, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, J.R.; Teixeira, G.Q.; Santos, S.G.; Barbosa, M.A.; Almeida-Porada, G.; Gonçalves, R.M. Mesenchymal stromal cell secretome: Influencing therapeutic potential by cellular pre-conditioning. Front. Immun. 2018, 9, 2837. [Google Scholar] [CrossRef]
- Ayala-Cuellar, A.P.; Kang, J.-H.; Jeung, E.-B.; Choi, K.-C. Roles of mesenchymal stem cells in tissue regeneration and immunomodulation. Biomol. Ther. 2019, 27, 25. [Google Scholar] [CrossRef]
- Castro, L.L.; Kitoko, J.Z.; Xisto, D.G.; Olsen, P.C.; Guedes, H.L.; Morales, M.M.; Lopes-Pacheco, M.; Cruz, F.F.; Rocco, P.R. Multiple doses of adipose tissue-derived mesenchymal stromal cells induce immunosuppression in experimental asthma. Stem Cells Transl. Med. 2020, 9, 250–260. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.W.; Park, K.S.; Bae, J.Y. Effects of Wharton’s jelly-derived mesenchymal stem cells on chronic obstructive pulmonary disease. Regen. Ther. 2019, 11, 207–211. [Google Scholar] [CrossRef]
- Vizoso, F.J.; Eiro, N.; Cid, S.; Schneider, J.; Perez-Fernandez, R. Mesenchymal stem cell secretome: Toward cell-free therapeutic strategies in regenerative medicine. Int. J. Mol. Sci. 2017, 18, 1852. [Google Scholar] [CrossRef]
- Caplan, A.I. Mesenchymal stem cells: Time to change the name! Stem Cells Transl. Med. 2017, 6, 1445–1451. [Google Scholar] [CrossRef]
- Harrell, C.R.; Fellabaum, C.; Jovicic, N.; Djonov, V.; Arsenijevic, N.; Volarevic, V. Molecular mechanisms responsible for therapeutic potential of mesenchymal stem cell-derived secretome. Cells 2019, 8, 467. [Google Scholar] [CrossRef]
- Fierabracci, A.; Fattore, A.D.; Muraca, M. The immunoregulatory activity of mesenchymal stem cells:‘state of art’and ‘future avenues’. Curr. Med. Chem. 2016, 23, 3014–3024. [Google Scholar]
- Bari, E.; Ferrarotti, I.; Torre, M.L.; Corsico, A.G.; Perteghella, S. Mesenchymal stem/stromal cell secretome for lung regeneration: The long way through “pharmaceuticalization” for the best formulation. J. Control. Release 2019, 309, 11–24. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Jin, S.; Zhang, Y. Ischemic preconditioning potentiates the protective effect of mesenchymal stem cells on endotoxin-induced acute lung injury in mice through secretion of exosome. Int. J. Clin. Exp. Med. 2015, 8, 3825. [Google Scholar] [PubMed]
- Teixeira, F.G.; Salgado, A.J. Mesenchymal stem cells secretome: Current trends and future challenges. Neural Regen. Res. 2020, 15, 75. [Google Scholar] [CrossRef] [PubMed]
- Najar, M.; Krayem, M.; Merimi, M.; Burny, A.; Meuleman, N.; Bron, D.; Raicevic, L. Insights into inflammatory priming of mesenchymal stromal cells: Functional biological impacts. Inflamm. Res. 2018, 67, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.; Li, L. Preconditioning influences mesenchymal stem cell properties in vitro and in vivo. J. Cell. Mol. Med. 2018, 22, 1428–1442. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Tsai, T.-L.; Li, W.-J. Strategies to retain properties of bone marrow-derived mesenchymal stem cells ex vivo. Ann. N. Y. Acad. Sci. 2017, 1409, 3. [Google Scholar] [CrossRef]
- De Cássia Noronha, N.; Mizukami, A.; Caliári-Oliveira, C.; Cominal, J.G.; Rocha, J.L.M.; Covas, D.T.; Swiech, K.; Malmegrim, K.C.R. Priming approaches to improve the efficacy of mesenchymal stromal cell-based therapies. Stem Cell Res. Ther. 2019, 10, 131. [Google Scholar]
- Abbasi-Malati, Z.; Roushandeh, A.M.; Kuwahara, Y.; Roudkenar, M.H. Mesenchymal stem cells on horizon: A new arsenal of therapeutic agents. Stem Cell Rev. Rep. 2018, 14, 484–499. [Google Scholar] [CrossRef]
- Bermudez, M.A.; Sendon-Lago, J.; Seoane, S.; Eiro, N.; Gonzalez, F.; Saa, J.; Vizoso, F.; Perez-Fernandez, R. Anti-inflammatory effect of conditioned medium from human uterine cervical stem cells in uveitis. Exp. Eye Res. 2016, 149, 84–92. [Google Scholar] [CrossRef]
- Bermudez, M.A.; Sendon-Lago, J.; Eiro, N.; Trevino, M.; Gonzalez, F.; Yebra–Pimentel, E.; Trevino, M.; Giraldez, M.J.; Macia, M. Corneal epithelial wound healing and bactericidal effect of conditioned medium from human uterine cervical stem cells. Investig. Ophthalmol. Vis. Sci. 2015, 56, 983–992. [Google Scholar] [CrossRef]
- Gnecchi, M.; Danieli, P.; Malpasso, G.; Ciuffreda, M.C. Paracrine mechanisms of mesenchymal stem cells in tissue repair. In Mesenchymal Stem Cells; Springer: Berlin/Heidelberg, Germany, 2016; pp. 123–146. [Google Scholar]
- Barreca, M.M.; Cancemi, P.; Geraci, F. Mesenchymal and Induced Pluripotent Stem Cells-Derived Extracellular Vesicles: The New Frontier for Regenerative Medicine? Cells 2020, 9, 1163. [Google Scholar] [CrossRef] [PubMed]
- Van der Meel, R.; Fens, M.H.; Vader, P.; Van Solinge, W.W.; Eniola-Adefeso, O.; Schiffelers, R.M. Extracellular vesicles as drug delivery systems: Lessons from the liposome field. J. Control. Release 2014, 195, 72–85. [Google Scholar] [CrossRef] [PubMed]
- Simons, M.; Raposo, G. Exosomes–vesicular carriers for intercellular communication. Curr. Opin. Cell Biol. 2009, 21, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Yáñez-Mó, M.; Siljander, P.R.-M.; Andreu, Z.; Bedina Zavec, A.; Borràs, F.E.; Buzas, E.I.; Buzas, K.; Casal, E.; Cappello, F.; Carvalho, J. Biological properties of extracellular vesicles and their physiological functions. J. Extracell. Vesicles 2015, 4, 27066. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, D.; Kiselev, M.A.; Caccamo, M.T. Smart nanoparticles for drug delivery application: Development of versatile nanocarrier platforms in biotechnology and nanomedicine. J. Nanomater. 2019, 2019, 3702518. [Google Scholar] [CrossRef]
- Gangadaran, P.; Ahn, B.-C. Extracellular Vesicle-and Extracellular Vesicle Mimetics-Based Drug Delivery Systems: New Perspectives, Challenges, and Clinical Developments. Pharmaceutics 2020, 12, 442. [Google Scholar] [CrossRef]
- Gangadaran, P.; Hong, C.M.; Ahn, B.-C. An update on in vivo imaging of extracellular vesicles as drug delivery vehicles. Front. Pharmacol. 2018, 9, 169. [Google Scholar] [CrossRef]
- Han, C.; Sun, X.; Liu, L.; Jiang, H.; Shen, Y.; Xu, X.; Lie, J.; Zhang, G.; Huang, J.; Lin, Z. Exosomes and Their Therapeutic Potentials of Stem Cells. Stem Cells Int. 2016, 2016, 7653489. [Google Scholar] [CrossRef]
- Mousavinejad, M.; Andrews, P.W.; Shoraki, E.K. Current biosafety considerations in stem cell therapy. Cell, J. (Yakhteh) 2016, 18, 281. [Google Scholar]
- Doyle, L.M.; Wang, M.Z. Overview of extracellular vesicles, their origin, composition, purpose, and methods for exosome isolation and analysis. Cells 2019, 8, 727. [Google Scholar] [CrossRef]
- Seo, Y.; Kim, H.-S.; Hong, I.-S. Stem cell-derived extracellular vesicles as immunomodulatory therapeutics. Stem Cells Int. 2019, 2019. [Google Scholar] [CrossRef] [PubMed]
- Lai, R.C.; Yeo, R.W.Y.; Lim, S.K. (Eds.) Mesenchymal stem cell exosomes. In Seminars in Cell & Developmental Biology; Elsevier: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Hu, P.; Yang, Q.; Wang, Q.; Shi, C.; Wang, D.; Armato, U.; Prà, I.D.; Chiarini, A. Mesenchymal stromal cells-exosomes: A promising cell-free therapeutic tool for wound healing and cutaneous regeneration. Burns Trauma 2019, 7, s41038-019-0178-8. [Google Scholar] [CrossRef] [PubMed]
- Mendt, M.; Rezvani, K.; Shpall, E. Mesenchymal stem cell-derived exosomes for clinical use. Bone Marrow Transplant. 2019, 54, 789–792. [Google Scholar] [CrossRef] [PubMed]
- Abreu, S.C.; Weiss, D.J.; Rocco, P.R. Extracellular vesicles derived from mesenchymal stromal cells: A therapeutic option in respiratory diseases? Stem Cell Res. Ther. 2016, 7, 53. [Google Scholar] [CrossRef]
- Cruz, F.F.; Rocco, P.R. Stem-cell extracellular vesicles and lung repair. Stem Cell Investig. 2017, 4. [Google Scholar] [CrossRef]
- Vader, P.; Breakefield, X.O.; Wood, M.J. Extracellular vesicles: Emerging targets for cancer therapy. Trends Mol. Med. 2014, 20, 385–393. [Google Scholar] [CrossRef]
- WHO. The Global Impact of Respiratory Disease; World Health Organization: Sheffield, UK, 2017. [Google Scholar]
- Force, A.D.T.; Ranieri, V.; Rubenfeld, G.; Thompson, B.; Ferguson, N.; Caldwell, E. Acute respiratory distress syndrome. JAMA 2012, 307, 2526–2533. [Google Scholar]
- Tomashefski, J.J. Pulmonary pathology of the adult respiratory distress syndrome. Clin. Chest Med. 1990, 11, 593–619. [Google Scholar]
- Cukic, V.; Hadzic, A. The most common detected bacteria in sputum of patients with community acquired pneumonia (CAP) treated in hospital. Med. Arch. 2016, 70, 354. [Google Scholar] [CrossRef]
- Silversides, J.A.; Ferguson, N.D. Clinical review: Acute respiratory distress syndrome-clinical ventilator management and adjunct therapy. Crit. Care 2013, 17, 225. [Google Scholar] [CrossRef]
- Papazian, L.; Forel, J.-M.; Gacouin, A.; Penot-Ragon, C.; Perrin, G.; Loundou, A.; Jaber, S.; Arnal, J.M.; Perez, D.; Seghboyan, J.M. Neuromuscular blockers in early acute respiratory distress syndrome. N. Engl. J. Med. 2010, 363, 1107–1116. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Murphy, S.; Kochanek, K.; Arias, E. Mortality in the United States, 2015. NCHS Data Brief, No 267; US Department of Health and Human Services, CDC, National Center for Health Statistics: Hyattsville, MD, USA, 2016.
- Barnes, P.J. Small airways in COPD. N. Engl. J. Med. 2004, 350, 2635–2636. [Google Scholar] [CrossRef] [PubMed]
- Devine, J.F. Chronic obstructive pulmonary disease: An overview. Am. Health Drug Benefits. 2008, 1, 34. [Google Scholar] [PubMed]
- Subbarao, P.; Mandhane, P.J.; Sears, M.R. Asthma: Epidemiology, etiology and risk factors. Cmaj 2009, 181, E181–E90. [Google Scholar] [CrossRef] [PubMed]
- Global Asthma Network. The Global Asthma Report 2018. Available online: http://www.globalasthmareport.org/ (accessed on 24 September 2020).
- Quirt, J.; Hildebrand, K.J.; Mazza, J.; Noya, F.; Kim, H. Asthma. Allergy Asthma Clin. Immunol. 2018, 14, 50. [Google Scholar] [CrossRef] [PubMed]
- Win, P.H.; Hussain, I. Asthma Triggers: What Really Matters? Clin. Asthma 2008, 149–156. [Google Scholar] [CrossRef]
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. Available online: https://ginasthma.org/gina-reports/ (accessed on 24 September 2020).
- O’Byrne, P.; Fabbri, L.M.; Pavord, I.D.; Papi, A.; Petruzzelli, S.; Lange, P. Asthma progression and mortality: The role of inhaled corticosteroids. Eur. Respir. J. 2019, 54, 1900491. [Google Scholar] [CrossRef]
- Angus, D.C.; Linde-Zwirble, W.T.; Lidicker, J.; Clermont, G.; Carcillo, J.; Pinsky, M.R. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit. Care Med. 2001, 29, 1303–1310. [Google Scholar] [CrossRef]
- Delano, M.J.; Ward, P.A. The immune system’s role in sepsis progression, resolution, and long-term outcome. Immunol. Rev. 2016, 274, 330–353. [Google Scholar] [CrossRef]
- Chen, X.-H.; Yin, Y.-J.; Zhang, J.-X. Sepsis and immune response. World J. Emerg. Med. 2011, 2, 88. [Google Scholar] [CrossRef]
- Martin, G.S.; Bernard, G.R. Airway and lung in sepsis. Intensiv. Care Med. 2001, 27, S63. [Google Scholar]
- Denstaedt, S.J.; Singer, B.H.; Standiford, T.J. Sepsis and nosocomial infection: Patient characteristics, mechanisms, and modulation. Front. Immunol. 2018, 9, 2446. [Google Scholar] [PubMed]
- Evans, T. Diagnosis and management of sepsis. Clin. Med. 2018, 18, 146. [Google Scholar]
- Sohrabi, C.; Alsafi, Z.; O’Neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [PubMed]
- Xia, W.; Shao, J.; Guo, Y.; Peng, X.; Li, Z.; Hu, D. Clinical and CT features in pediatric patients with COVID-19 infection: Different points from adults. Pediatric Pulmonol. 2020, 55, 1169–1174. [Google Scholar]
- Yuki, K.; Fujiogi, M.; Koutsogiannaki, S. COVID-19 pathophysiology: A review. Clin. Immunol. 2020, 108427. [Google Scholar]
- Eiro, N.; Cabrera, J.R.; Fraile, M.; Costa, L.A.; Vizoso, F.J. The Coronavirus Pandemic (SARS-CoV-2): New Problems Demand New Solutions, the Alternative of Mesenchymal (Stem) Stromal Cells. Front. Cell Dev. Biol. 2020, 8, 645. [Google Scholar]
- Liu, Y.; Du, X.; Chen, J.; Jin, Y.; Peng, L.; Wang, H.H.; Lou, M.; Chen, L.; Zhao, Y. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J. Infect. 2020, 81, e6–e12. [Google Scholar]
- Ye, Q.; Wang, B.; Mao, J. Cytokine storm in COVID-19 and treatment. J. Infect. 2020, 80, 607–613. [Google Scholar]
- Centers for Disease Control Prevention. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/therapeutic-options.html (accessed on 24 September 2020).
- Sengupta, V.; Sengupta, S.; Lazo, A.; Woods, P.; Nolan, A.; Bremer, N. Exosomes derived from bone marrow mesenchymal stem cells as treatment for severe COVID-19. Stem Cells Dev. 2020. [Google Scholar] [CrossRef]
- Raza, S.S.; Khan, M.A. Mesenchymal Stem Cells: A new front emerge in COVID19 treatment: Mesenchymal Stem Cells therapy for SARS-CoV2 viral infection. Cytotherapy 2020. [Google Scholar] [CrossRef]
- Patil, J.; Sarasija, S. Pulmonary drug delivery strategies: A concise, systematic review. Lung India Off. Organ. Ind. Chest Soc. 2012, 29, 44. [Google Scholar]
- Borghardt, J.M.; Kloft, C.; Sharma, A. Inhaled therapy in respiratory disease: The complex interplay of pulmonary kinetic processes. Can. Respir. J. 2018, 2018, 2732017. [Google Scholar] [CrossRef] [PubMed]
- Dolovich, M.B.; Ahrens, R.C.; Hess, D.R.; Anderson, P.; Dhand, R.; Rau, J.L.; Smaldone, G.C.; Guyatt, G. Device selection and outcomes of aerosol therapy: Evidence-based guidelines: American College of Chest Physicians/American College of Asthma, Allergy, and Immunology. Chest 2005, 127, 335–371. [Google Scholar] [PubMed]
- Jin, J.-F.; Zhu, L.-L.; Chen, M.; Xu, H.-M.; Wang, H.-F.; Feng, X.-Q.; Zhu, X.-P.; Zhou, Q. The optimal choice of medication administration route regarding intravenous, intramuscular, and subcutaneous injection. Patient Prefer. Adherence 2015, 9, 923. [Google Scholar]
- Clinical trials.gov. A Pilot Clinical Study on Inhalation of Mesenchymal Stem Cells Exosomes Treating Severe Novel Coronavirus Pneumonia 2020. Available online: https://clinicaltrials.gov/ct2/show/NCT04276987?term=exosome%2C+aersol&cond=Covid19&cntry=CN&draw=2&rank=1 (accessed on 24 September 2020).
- Tekade, R.K. Drug Delivery Systems; Elsevier Science: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Bennett, G.; Joyce, M.; Sweeney, L.; MacLoughlin, R. In vitro study of the effect of breathing pattern on aerosol delivery during high-flow nasal therapy. Pulm. Ther. 2019, 5, 43–54. [Google Scholar] [CrossRef]
- Réminiac, F.; Vecellio, L.; Heuzé-Vourc’h, N.; Petitcollin, A.; Respaud, R.; Cabrera, M.; Pennec, D.L.; Diot, P.; Ehrmann, S. Aerosol therapy in adults receiving high flow nasal cannula oxygen therapy. J. Aerosol Med. Pulm. Drug Deliv. 2016, 29, 134–141. [Google Scholar] [CrossRef]
- MacLoughlin, R.; Telfer, C.; Clark, A.; Fink, J. Aerosol: A novel vehicle for pharmacotherapy in neonates. Curr. Pharm. Des. 2017, 23, 5928–5934. [Google Scholar] [CrossRef]
- Usmani, O.S.; Biddiscombe, M.F.; Barnes, P.J. Regional lung deposition and bronchodilator response as a function of β2-agonist particle size. Am. J. Respir. Crit. Care Med. 2005, 172, 1497–1504. [Google Scholar] [CrossRef]
- Bennett, G.; Joyce, M.; Fernández, E.F.; MacLoughlin, R. Comparison of aerosol delivery across combinations of drug delivery interfaces with and without concurrent high-flow nasal therapy. Intensive Care Med. Exp. 2019, 7, 20. [Google Scholar] [CrossRef]
- Baskin, M.I.; Abd, A.G.; Ilowite, J.S. Regional deposition of aerosolized pentamidine: Effects of body position and breathing pattern. Ann. Intern. Med. 1990, 113, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Darquenne, C. Aerosol deposition in health and disease. J. Aerosol Med. Pulm. Drug Deliv. 2012, 25, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Averyanov, A.; Konoplyannikov, A.; Zabozlaev, F.; Danilevskaya, O.; Konoplyannikov, M.; Kuzovlev, O.; Kulagina, N.; Koroleva, I. Comparative effects of inhaled and intravenous mesenchymal stem cells in bleomycin-induced pulmonary fibrosis in rabbits. Eur. Respir. Soc. 2013, 42, 226. [Google Scholar]
- Bari, E.; Perteghella, S.; Di Silvestre, D.; Sorlini, M.; Catenacci, L.; Sorrenti, M.; Marrubini, G.; Rossi, R.; Tripodo, G.; Mauri, P. Pilot production of mesenchymal stem/stromal freeze-dried secretome for cell-free regenerative nanomedicine: A validated GMP-compliant process. Cells 2018, 7, 190. [Google Scholar] [CrossRef] [PubMed]
- Bahr, M.M.; Amer, M.S.; Abo-El-Sooud, K.; Abdallah, A.N.; El-Tookhy, O.S. Preservation techniques of stem cells extracellular vesicles: A gate for manufacturing of clinical grade therapeutic extracellular vesicles and long-term clinical trials. Int. J. Vet. Sci. Med. 2020, 8, 1–8. [Google Scholar] [CrossRef]
- Halim, N.; Ch’ng, E.; Kardia, E.; Ali, S.; Radzi, R.; Yahaya, B. Aerosolised mesenchymal stem cells expressing angiopoietin-1 enhances airway repair. Stem Cell Rev. Rep. 2019, 15, 112–125. [Google Scholar] [CrossRef]
- Dinh, P.-U.C.; Paudel, D.; Brochu, H.; Popowski, K.D.; Gracieux, M.C.; Cores, J.; Huang, K.; Hensley, M.T.; Harrell, E.; Vandergriff, A.C. Inhalation of lung spheroid cell secretome and exosomes promotes lung repair in pulmonary fibrosis. Nat. Commun. 2020, 11, 1–14. [Google Scholar] [CrossRef]
- Kim, S.Y.; Burgess, J.K.; Wang, Y.; Kable, E.P.; Weiss, D.J.; Chan, H.-K.; Chrzanowski, W. Atomized human amniotic mesenchymal stromal cells for direct delivery to the airway for treatment of lung injury. J. Aerosol Med. Pulm. Drug Deliv. 2016, 29, 514–524. [Google Scholar] [CrossRef]
- McCarthy, S.D.; Horgan, E.; Ali, A.; Masterson, C.; Laffey, J.G.; MacLoughlin, R.; O’Toole, D. Nebulized Mesenchymal Stem Cell Derived Conditioned Medium Retains Antibacterial Properties Against Clinical Pathogen Isolates. J. Aerosol Med. Pulm. Drug Deliv. 2019, 33, 140–152. [Google Scholar] [CrossRef]
- Devaney, J.; Chao, J.; Elliman, S.; O’Toole, D.; Laffey, J.G.; MacLoughlin, R. Human Mesenchymal Stromal Cell Derived Exosomes and Conditioned Medium are Nebulisable by Aerogen Vibronic Micropump and Retain Anti-Inflammatory Properties; A34 ARDS AND LUNG INJURY; American Thoracic Society: New York, NY, USA, 2016; p. A1360-A. [Google Scholar]
- Seoane-Vazquez, E.; Shukla, V.; Rodriguez-Monguio, R. Innovation and competition in advanced therapy medicinal products. EMBO Mol. Med. 2019, 11, e9992. [Google Scholar] [CrossRef]
- Dugernier, J.; Hesse, M.; Vanbever, R.; Depoortere, V.; Roeseler, J.; Michotte, J.-B.; Laterre, P.-F.; Jamar, F.; Reychler, G. SPECT-CT comparison of lung deposition using a system combining a vibrating-mesh nebulizer with a valved holding chamber and a conventional jet nebulizer: A randomized cross-over study. Pharm. Res. 2017, 34, 290–300. [Google Scholar] [CrossRef] [PubMed]
- Reisner, C.; Katial, R.K.; Bartelson, B.B.; Buchmeir, A.; Rosenwasser, L.J.; Nelson, H.S. Characterization of aerosol output from various nebulizer/compressor combinations. Ann. Allergy Asthma Immunol. 2001, 86, 566–574. [Google Scholar] [CrossRef]
- Dugernier, J.; Reychler, G.; Wittebole, X.; Roeseler, J.; Depoortere, V.; Sottiaux, T.; Michotte, J.B.; Vanbever, R.; Dugernier, T.; Goffette, P. Aerosol delivery with two ventilation modes during mechanical ventilation: A randomized study. Ann. Intensive Care 2016, 6, 73. [Google Scholar] [CrossRef] [PubMed]
- McGrath, J.A.; O’Sullivan, A.; Bennett, G.; O’Toole, C.; Joyce, M.; Byrne, M.A.; MacLoughlin, R. Investigation of the quantity of exhaled aerosols released into the environment during nebulisation. Pharmaceutics 2019, 11, 75. [Google Scholar] [CrossRef] [PubMed]
- McGrath, J.A.; O’Toole, C.; Bennett, G.; Joyce, M.; Byrne, M.A.; MacLoughlin, R. Investigation of fugitive aerosols released into the environment during high-flow therapy. Pharmaceutics 2019, 11, 254. [Google Scholar] [CrossRef]
- O’Toole, C.; Joyce, M.; McGrath, J.A.; O’Sullivan, A.; Byrne, M.A.; MacLoughlin, R. Fugitive aerosols in the intensive care unit: A narrative review. Ann. Transl. Med. 2020. [Google Scholar] [CrossRef]
- Frank, E.; Ishau, S.; Maier, A.; Reutman, S.; Reichard, J.F. An occupational exposure limit (OEL) approach to protect home healthcare workers exposed to common nebulized drugs. Regul. Toxicol. Pharmacol. 2019, 106, 251–261. [Google Scholar] [CrossRef]
- Fink, J.B.; Ehrmann, S.; Li, J.; Dailey, P.; McKiernan, P.; Darquenne, C.; Martin, A.R.; Rothen-Rutishauser, B.; Kuehl, P.J.; Häussermann, S. Reducing Aerosol-Related Risk of Transmission in the Era of COVID-19: An Interim Guidance Endorsed by the International Society of Aerosols in Medicine. J. Aerosol Med. Pulm. Drug Deliv. 2020. [Google Scholar] [CrossRef]
- Wilson, J.G.; Liu, K.D.; Zhuo, H.; Caballero, L.; McMillan, M.; Fang, X.; Cosgrove, K.; Vojnik, R.; Calfee, C.S.; Lee, J.-W. Mesenchymal stem (stromal) cells for treatment of ARDS: A phase 1 clinical trial. Lancet Respir. Med. 2015, 3, 24–32. [Google Scholar] [CrossRef]
- Matthay, M.A.; Calfee, C.S.; Zhuo, H.; Thompson, B.T.; Wilson, J.G.; Levitt, J.E.; Rogers, A.J.; Gotts, J.E.; Wiener-Kronish, J.P.; Bajwa, E.K. Treatment with allogeneic mesenchymal stromal cells for moderate to severe acute respiratory distress syndrome (START study): A randomised phase 2a safety trial. Lancet Respir. Med. 2019, 7, 154–162. [Google Scholar] [CrossRef]
- Aver’yanov, A.; Konoplyannikov, A.; Antonov, N.; Osipova, G.; Vasil’eva, O.; Sakharova, M.; Tatarskii, A.R.; Kobylyansky, V.I. Survival of Mesenchymal Stem Cells in Different Methods of Nebulization. Bull. Exp. Biol. Med. 2018, 164, 576–578. [Google Scholar] [CrossRef] [PubMed]
- Brave, H.; MacLoughlin, R. State of the Art Review of Cell Therapy in the Treatment of Lung Disease, and the Potential for Aerosol Delivery. Int. J. Mol. Sci. 2020, 21, 6435. [Google Scholar] [CrossRef] [PubMed]
- Mason, R.J.; Broaddus, V.C.; Martin, T.R.; King, T.E.; Schraufnagel, D.; Murray, J.F.; Nadel, J.A. Murray and Nadel’s Textbook of Respiratory Medicine E-Book: 2-Volume Set; Elsevier Health Sciences: Amsterdam, The Netherlands, 2010. [Google Scholar]
- Cukic, V.; Lovre, V.; Dragisic, D.; Ustamujic, A. Asthma and chronic obstructive pulmonary disease (COPD)–differences and similarities. Mater. Soc. Med. 2012, 24, 100. [Google Scholar] [CrossRef] [PubMed]
- Duong, T.N.; Zeki, A.A.; Louie, S. Medical Management of Hospitalized Patients with Asthma or Chronic Obstructive Pulmonary Disease. Hosp. Med. Clin. 2017, 6, 437. [Google Scholar] [CrossRef] [PubMed]
- Behnke, J.; Kremer, S.; Shahzad, T.; Chao, C.-M.; Böttcher-Friebertshäuser, E.; Morty, R.E.; Bellusci, S.; Ehrhardt, H. MSC Based Therapies—New Perspectives for the Injured Lung. J. Clin. Med. 2020, 9, 682. [Google Scholar] [CrossRef]
- Mohammadipoor, A.; Antebi, B.; Batchinsky, A.I.; Cancio, L.C. Therapeutic potential of products derived from mesenchymal stem/stromal cells in pulmonary disease. Resp. Res. 2018, 19, 218. [Google Scholar] [CrossRef]
- Cagliani, J.; Grande, D.; Molmenti, E.P.; Miller, E.J.; Rilo, H.L. Immunomodulation by mesenchymal stromal cells and their clinical applications. J. Stem Cell Regen. Biol. 2017, 3. [Google Scholar] [CrossRef]
- Danchuk, S.; Ylostalo, J.H.; Hossain, F.; Sorge, R.; Ramsey, A.; Bonvillain, R.W.; Lasky, J.A.; Bunnel, B.A.; Welsh, D.A.; Prockop, D.J. Human multipotent stromal cells attenuate lipopolysaccharide-induced acute lung injury in mice via secretion of tumor necrosis factor-α-induced protein 6. Stem Cell Res. Ther. 2011, 2, 27. [Google Scholar] [CrossRef]
- Wong, A.P.; Keating, A.; Lu, W.-Y.; Duchesneau, P.; Wang, X.; Sacher, A.; Hu, J.; Waddel, T.K. Identification of a bone marrow–derived epithelial-like population capable of repopulating injured mouse airway epithelium. J. Clin. Investig. 2009, 119, 336–348. [Google Scholar] [CrossRef][Green Version]
- Prockop, D.J.; Brenner, M.; Fibbe, W.E.; Horwitz, E.; Le Blanc, K.; Phinney, D.G.; Simmons, P.J.; Sensebe, L.; Keating, A. Defining the risks of mesenchymal stromal cell therapy. Cytotherapy 2010, 12, 576–578. [Google Scholar] [CrossRef]
- Ehrmann, S. Vibrating mesh nebulisers–can greater drug delivery to the airways and lungs improve respiratory outcomes. Eur. Respir. Pulmon. Dis. 2018, 4. [Google Scholar] [CrossRef]
- McCarthy, S.D.; González, H.E.; Higgins, B.D. Future Trends in Nebulized Therapies for Pulmonary Disease. J. Personal. Med. 2020, 10, 37. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Dennis, J.E.; Muzic, R.F.; Lundberg, M.; Caplan, A.I. The dynamic in vivo distribution of bone marrow-derived mesenchymal stem cells after infusion. Cells Tissues Organs 2001, 169, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Iglesias-Lopez, C.; Agustí, A.; Obach, M.; Vallano, A. Regulatory Framework for Advanced Therapy Medicinal Products in Europe and United States. Front. Pharmacol. 2019, 10, 766. [Google Scholar] [CrossRef] [PubMed]
- Detela, G.; Lodge, A. EU regulatory pathways for ATMPs: Standard, accelerated and adaptive pathways to marketing authorisation. Mol. Ther. Methods Clin. Dev. 2019, 13, 205. [Google Scholar] [CrossRef] [PubMed]
- Ten Ham, R.M.; Hoekman, J.; Hövels, A.M.; Broekmans, A.W.; Leufkens, H.G.; Klungel, O.H. Challenges in advanced therapy medicinal product development: A survey among companies in Europe. Mol. Ther. Methods Clin. Dev. 2018, 11, 121–130. [Google Scholar] [CrossRef]
- European Medicines Agency. Committee for advanced therapies (CAT). Available online: https://www.ema.europa.eu/en/committees/committee-advanced-therapies-cat (accessed on 24 September 2020).
- European Medicines Agency. Guidance on good manufacturing practice and good distribution practice: Questions and answers 2020. Available online: https://www.ema.europa.eu/en/human-regulatory/research-development/compliance/good-manufacturing-practice/guidance-good-manufacturing-practice-good-distribution-practice-questions-answers (accessed on 24 September 2020).
- Phillips, L.D. Benefit-Risk Methodology Project. Work Package 1 Report: Description of the Current Practice of Benefit-Risk Assessment for Centralized Procedure Products in the EU Regulatory Network. 2009. Available online: http://eprints.lse.ac.uk/64593/1/Benefit%20risk%20methodology%20project.pdf (accessed on 24 September 2020).
- French-Mowat, E.; Burnett, J. How are medical devices regulated in the European Union? J. R. Soc. Med. 2012, 105, 22–28. [Google Scholar] [CrossRef]
- Behan, R.; Watson, M.; Pandit, A. New EU medical device regulations: Impact on the MedTech sector. Med. Writ. 2017, 26, 20–24. [Google Scholar]
- Purnama, A.; Drago, D. Fundamentals of the European Devices Regulatory Framework. 2019. Available online: https://www.topra.org/TOPRA/TOPRA_MEMBER/PDFs/TOPRA-RR-OCT19-CPD-Supplement.pdf (accessed on 24 September 2020).
- Directive, C. 93/42/EEC of 14 June 1993 Concerning Medical Devices; OJL Ltd.: Barnsley, UK, 1993.
- European Commission. Notified Bodies. Available online: https://ec.europa.eu/growth/single-market/goods/building-blocks/notified-bodies_en (accessed on 24 September 2020).
- Gupta, S.K. Medical Device Regulations: A Current Perspective. J. Young Pharm. 2016, 8. [Google Scholar] [CrossRef]
- Eurpoean Commission. Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on Medical Devices, Amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and Repealing Council Directives 90/385/EEC and 93/42/EEC; Eurpoean Commission: Makati, Philippines.
- UL, EB. Europe Medical Devices Regulation (MDR) CE Marking Regulatory Process 2019. Available online: https://www.emergobyul.com/resources/europe-medical-devices-regulation-mdr-ce-marking-regulatory-process (accessed on 24 September 2020).
- Mendicino, M.; Fan, Y.; Griffin, D.; Gunter, K.C.; Nichols, K. Current state of US Food and Drug Administration regulation for cellular and gene therapy products: Potential cures on the horizon. Cytotherapy 2019, 21, 699–724. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. Center for Biologics Evaluation and Research (CBER) 2017. Available online: https://www.fda.gov/about-fda/office-medical-products-and-tobacco/about-center-biologics-evaluation-andresearch-cber (accessed on 24 September 2020).
- U.S. Food and Drug Administration. 21st Century Cures Act; U.S. Food and Drug Administration: Silver Spring, MD, USA, 2018.
- U.S. Food and Drug Administration. Evaluation of Devices Used With Regenerative Medicine Advanced Therapies: Guidance for Industry; U.S. Food and Drug Administration: Silver Spring, MD, USA, 2019.
- Premarket Notification 510 (k). Special Considerations 2020. Available online: https://www.fda.gov/medical-devices/premarket-notification-510k/special-considerations (accessed on 24 September 2020).
- U.S. Food and Drug Administration. CFR—Code of Federal Regulations Title 21. 2017. Available online: Ecfr.gov/cgi-bin/text-idx (accessed on 24 September 2020).
- Meyer, R.J. Bringing new nebulizer technologies to market: Regulatory issues. Respir. Care 2002, 47, 1334–1336. [Google Scholar] [PubMed]
- De Pablo, E.; Fernández-García, R.; Ballesteros, M.P.; Torrado, J.J.; Serrano, D.R. Nebulised antibiotherapy: Conventional versus nanotechnology-based approaches, is targeting at a nano scale a difficult subject? Ann. Transl. Med. 2017, 5, 448. [Google Scholar] [CrossRef] [PubMed]
| ATMP and Its Formulation Characteristics | |||||
|---|---|---|---|---|---|
| Stem Cell | Secretome | Exosome | |||
| Micro suspension of cells | Mixture of suspended exosomes and solubilized proteins and peptides | Nano suspension of exosomes | |||
| Aerosol Generator | Typical Dose | Potential ATMP Compatibility with Aerosol Generator | Supporting References | ||
| Dry Powder Inhaler (DPI) | 8–40 mg | No | Yes | Yes | [95,96] |
| Pressurized Metered Dose Inhaler (pMDI) | 25 to 100 μL | No | Yes | Yes | [85] |
| Soft Mist Inhaler | 15 μL | Yes | Yes | Yes | [97] |
| Jet Nebulizer (JN) | 2 to 6 mL | Yes | Yes | Yes | [94,98] |
| Vibrating Mesh Nebulizer (VMN) | 0.1 to 50 mL | Yes | Yes | Yes | [99,100,101] |
| NCT No. | Title | Enrolled | Intervention | Dose | Phase | Status |
|---|---|---|---|---|---|---|
| NCT04276987 | A Pilot Clinical Study on Aerosol Inhalation of the Exosomes Derived From Allogenic Adipose Mesenchymal Stem Cells in the Treatment of Severe Patients With Novel Coronavirus Pneumonia | 30 | Single-group assignment | MSC derived exosomes 5 Times aerosol inhalations of MSCs-derived exosomes (2.0 × 108 nano vesicles/3 mL at Days 1, 2, 3, 4 and 5 | Phase 1 | Not yet recruiting |
| NCT04389385 | Aerosol Inhalation of the Exosomes Derived From Allogenic COVID-19 T Cell in the Treatment of Early Stage Novel Coronavirus Pneumonia | 60 | Single-group assignment | Specific T cell-derived exosomes (CSTC-Exo) Aerosol inhalation of CSTC-Exo (2.0 × 108 nanovesicles/3 mL at Day 1,2,3,4 and 5, 5 times daily | Phase 1 | Active, not recruiting |
| NCT04473170 | Study Evaluating the Safety and Efficacy of Autologous Non-Hematopoietic Peripheral Blood Stem Cells in COVID-19 (SENTAD-COVID) | 146 | Parallel assessment | Autologous Non-Hematopoietic Peripheral Blood Stem Cells (NHPBSC) therapy as add-on COVID-19 standard care | Phase 1 Phase 2 | Completed |
| Class | Risk | Description | Route |
|---|---|---|---|
| I | Low risk | Non-invasive, does not interact with body | Self-declaration route outlines in Annex VII Module. An EU Declaration of Conformity—manufacturer must declare the device satisfies the provisions of the directive. |
| IIa | Medium | Generally invasive Therapeutic transfer of energy to patient or used for the diagnosis or monitoring of medical condition | Carry out conformity assessment carried out by NB using Annex II, IV, V, or VI. Can declare conformity with the provisions of directives and regulations (Annex VII). |
| IIb | Medium | Invasive—surgical or implantation Potential to modify body fluid | Full quality assurance (Annex II)—with assessment by NB of technical documents in one sample in accordance with the directive (Annex II, Section 7). |
| III | High | Invasive—used to sustain human life, essential to maintain human health Devices connected to CNS or CCS | Full quality assurance system audit (Annex II)—full examination of device by a Notified Body (NB) |
| Class | Description |
|---|---|
| I | Devices are subject to a comprehensive set of regulatory authorities called general controls that are applicable to all classes of devices. |
| II | Devices for which general controls, by themselves, are insufficient to provide reasonable assurance of the safety and effectiveness of the device, and for which there is sufficient information to establish special controls to provide such assurance. |
| III | Devices for which general controls, by themselves, are insufficient and for which there is insufficient information to establish special controls to provide reasonable assurance of the safety and effectiveness of the device. Class III devices typically require premarket approval. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Woods, N.; MacLoughlin, R. Defining a Regulatory Strategy for ATMP/Aerosol Delivery Device Combinations in the Treatment of Respiratory Disease. Pharmaceutics 2020, 12, 922. https://doi.org/10.3390/pharmaceutics12100922
Woods N, MacLoughlin R. Defining a Regulatory Strategy for ATMP/Aerosol Delivery Device Combinations in the Treatment of Respiratory Disease. Pharmaceutics. 2020; 12(10):922. https://doi.org/10.3390/pharmaceutics12100922
Chicago/Turabian StyleWoods, Niamh, and Ronan MacLoughlin. 2020. "Defining a Regulatory Strategy for ATMP/Aerosol Delivery Device Combinations in the Treatment of Respiratory Disease" Pharmaceutics 12, no. 10: 922. https://doi.org/10.3390/pharmaceutics12100922
APA StyleWoods, N., & MacLoughlin, R. (2020). Defining a Regulatory Strategy for ATMP/Aerosol Delivery Device Combinations in the Treatment of Respiratory Disease. Pharmaceutics, 12(10), 922. https://doi.org/10.3390/pharmaceutics12100922