Clinical, Psychosocial, and Structural Factors Associated with the Detection of HIV Drug Resistance in Children Living with HIV in Kisumu, Kenya: Secondary Analysis of Data from the Opt4Kids Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
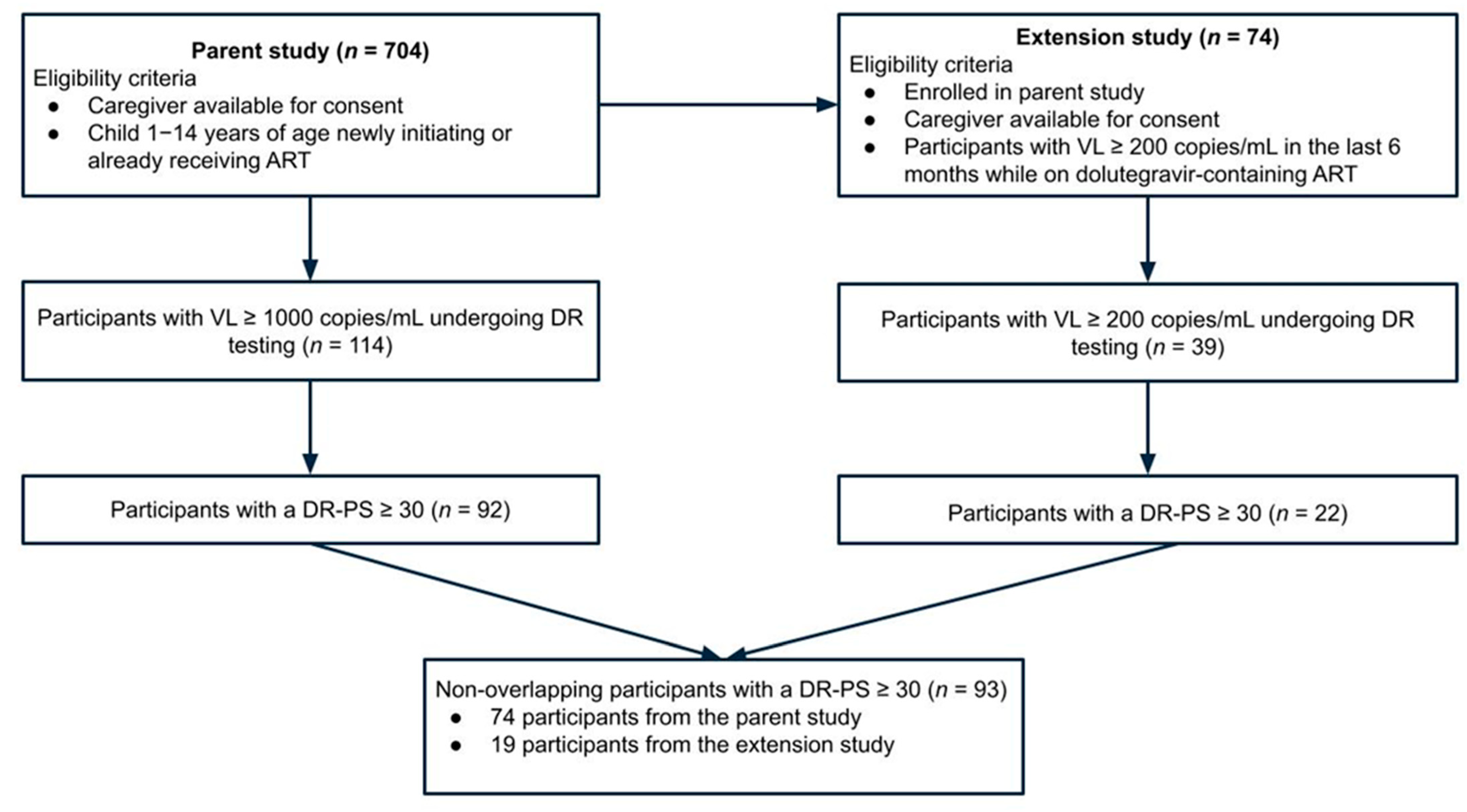
2.2. Participants and Sample Size
2.3. Variables
2.3.1. Primary Analytic Outcome
2.3.2. Associated Risk Factors
2.3.3. Child and Caregiver Clinical Characteristics
2.3.4. Child Psychosocial Characteristics
2.3.5. Caregiver Psychosocial Characteristics
2.3.6. Household Psychosocial Characteristics
2.3.7. Structural Characteristics
2.4. Data Sources and Management
2.5. Statistical Methods
3. Results
3.1. Individual, Household, and Structural Characteristics of Participants
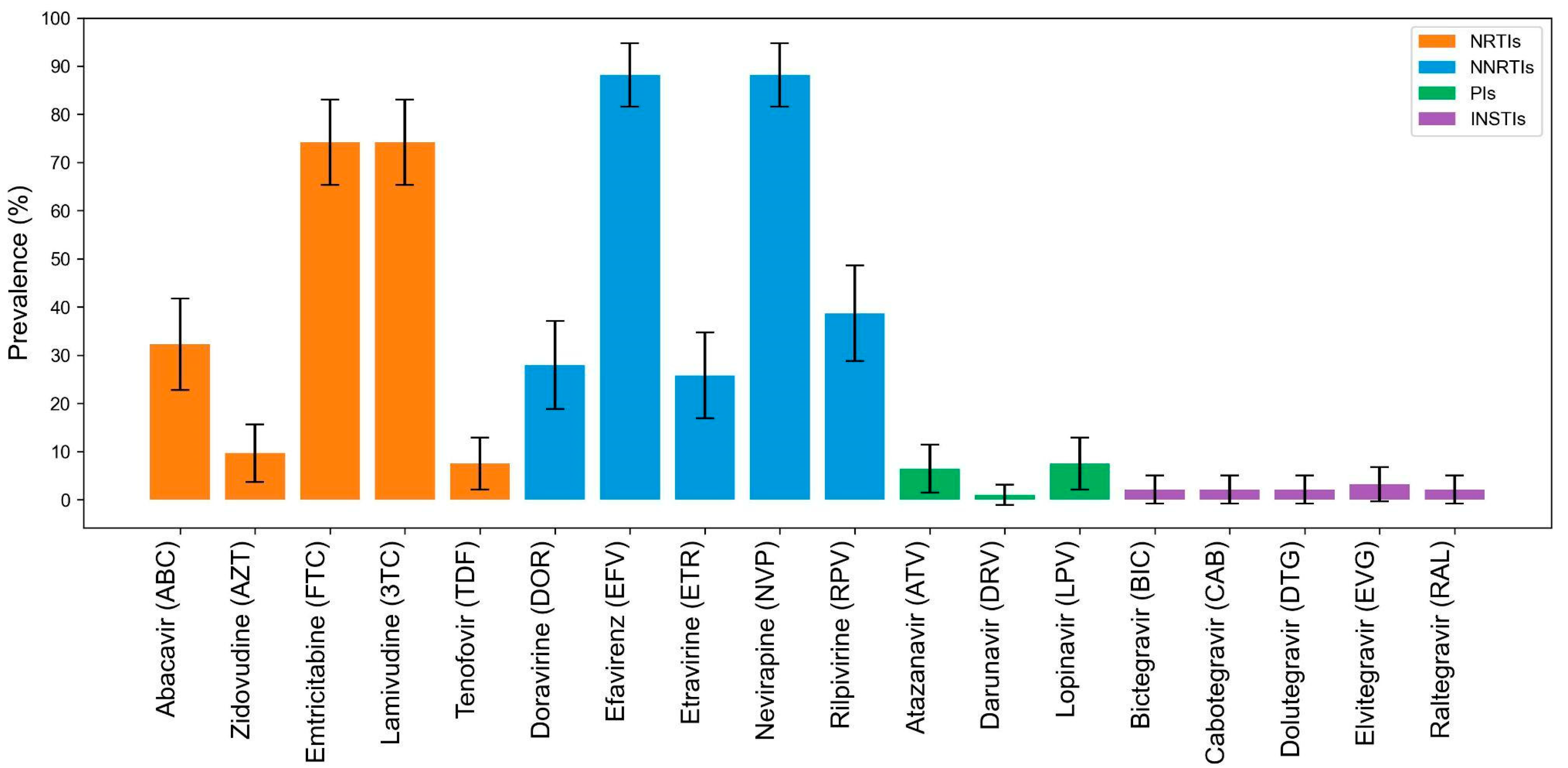
3.2. HIV Drug Resistance (DR) Testing and DR Penalty Scores (DR-PS) ≥ 30
3.3. Associations with DR-PS ≥ 30
Individual, Household, and Structural Characteristics
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- UNICEF. Global and Regional Trends. Updated July 2025. Available online: https://data.unicef.org/topic/hivaids/global-regional-trends/ (accessed on 18 August 2025).
- Han, W.M.; Law, M.G.; Egger, M.; Wools-Kaloustian, K.; Moore, R.; McGowan, C.; Kumarasamy, N.; Desmonde, S.; Edmonds, A.; Davies, M.-A.; et al. Global estimates of viral suppression in children and adolescents and adults on antiretroviral therapy adjusted for missing viral load measurements: A multiregional, retrospective cohort study in 31 countries. Lancet HIV 2021, 8, e766–e775. [Google Scholar] [CrossRef] [PubMed]
- UNAIDS. Kenya HIV and AIDS Estimates. Available online: https://www.unaids.org/en/regionscountries/countries/kenya (accessed on 18 August 2025).
- Mulinge, M.M.; Kibui, N.K.; Kimani, H.; Wainaina, J.; Bwana, P.; Omondi, M.; Wafula, K.; Wamalwa, D.C.; Omondi, E.O.; Nduati, R.W.; et al. Factors associated with viral load non-suppression among treatment-experienced pre-teenage children living with HIV in Kenya: A nationwide population-based cohort study, 2015–2021. eClinicalMedicine 2024, 68, 102454. [Google Scholar] [CrossRef]
- UNAIDS. New High-Quality Antiretroviral Therapy to be Launched in South Africa, Kenya and over 90 Low-and Middle-Income Countries at Reduced Price. Published 21 September 2017. Available online: https://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2017/September/20170921_TLD#:~:text=“Research%20has%20shown20%that%20dolutegravir,in%20the%20National%20ART%20Pro-gram.%E@%80%9D (accessed on 20 July 2025).
- The Lancet HIV. Declaration commits to ending AIDS in children. Lancet HIV 2023, 10, e209. [Google Scholar] [CrossRef]
- Inzaule, S.C.; Osi, S.J.; Akinbiyi, G.; Emeka, A.; Khamofu, H.; Mpazanje, R.; Ilesanmi, O.; Ndembi, N.; Odafe, S.; Sigaloff, K.C.E.; et al. High Prevalence of HIV Drug Resistance Among Newly Diagnosed Infants Aged <18 Months: Results From a Nationwide Surveillance in Nigeria. JAIDS J. Acquir. Immune Defic. Syndr. 2018, 77, e1–e7. [Google Scholar] [PubMed]
- Tsikhutsu, I.; Bii, M.; Dear, N.; Ganesan, K.; Kasembeli, A.; Sing’oEi, V.; Rombosia, K.; Ochieng, C.; Desai, P.; Wolfman, V.; et al. Prevalence and Correlates of Viral Load Suppression and Human Immunodeficiency Virus (HIV) Drug Resistance Among Children and Adolescents in South Rift Valley and Kisumu, Kenya. Clin. Infect. Dis. 2022, 75, 936–944. [Google Scholar] [CrossRef]
- Djiyou, A.B.D.; I Penda, C.; Madec, Y.; Ngondi, G.D.; Moukoko, A.; E Eboumbou, C.; Aghokeng, A.F. Prevalence of HIV drug resistance among adolescents receiving ART in Cameroon with low- or high-level viraemia. J. Antimicrob. Chemother. 2023, 78, 2938–2942. [Google Scholar] [CrossRef]
- Abuogi, L.; Oyaro, P.; Wakjira, G.; Thomas, K.K.; Scallon, A.J.; Mukui, I.; Chohan, B.H.; Brown, E.; Karauki, E.; Yongo, N.; et al. HIV Drug Resistance Patterns and Characteristics Associated with Clinically Significant Drug Resistance among Children with Virologic Failure on Antiretroviral Treatment in Kenya: Findings from the Opt4Kids Randomized Controlled Trial. Viruses 2023, 15, 2083. [Google Scholar] [CrossRef]
- Makoni, M. The promise of paediatric dolutegravir in Zimbabwe. Lancet HIV 2022, 9, e603–e604. [Google Scholar] [CrossRef]
- Bacha, J.M.; Dlamini, S.B.; Anabwani, F.; Gwimile, J.; Kanywa, J.B.; Farirai, J.; Bvumbwe, M.; Tsotako, M.; Steffy, T.; Nguyen, D.; et al. Realizing the Promise of Dolutegravir in Effectively Treating Children and Adolescents Living With HIV in Real-world Settings in 6 Countries in Eastern and Southern Africa. Pediatr. Infect. Dis. J. 2023, 42, 576–581. [Google Scholar] [CrossRef]
- Frange, P.; Avettand-Fenoel, V.; Veber, F.; Blanche, S. Similar efficacy and safety of dolutegravir between age groups of HIV-1-infected paediatric and young adult patients aged 5 years and older. HIV Med. 2019, 20, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Viani, R.M.; Ruel, T.; Alvero, C.; Fenton, T.; Acosta, E.P.; Hazra, R.; Townley, E.; Palumbo, P.; Buchanan, A.M.; Vavro, C.; et al. Long-Term Safety and Efficacy of Dolutegravir in Treatment-Experienced Adolescents With Human Immunodeficiency Virus Infection: Results of the IMPAACT P1093 Study. J. Pediatr. Infect. Dis. Soc. 2020, 9, 159–165. [Google Scholar] [CrossRef]
- Kamori, D.; Barabona, G.; Rugemalila, J.; Maokola, W.; Masoud, S.S.; Mizinduko, M.; Sabasaba, A.; Ruhago, G.; Sambu, V.; Mushi, J.; et al. Emerging integrase strand transfer inhibitor drug resistance mutations among children and adults on ART in Tanzania: Findings from a national representative HIV drug resistance survey. J. Antimicrob. Chemother. 2023, 78, 779–787. [Google Scholar] [CrossRef]
- World Health Organization. HIV Drug Resistance: Brief Report 2024. Published 2024. Available online: https://www.who.int/publications/i/item/9789240086319 (accessed on 20 July 2025).
- Malinga, S.; Khan, A.; Archary, M. Breaking the unbreakable: A paediatric case of dolutegravir resistance from KwaZulu-Natal. S. Afr. J. HIV Med. 2023, 24, 1458. [Google Scholar] [CrossRef]
- Brenner, B.G.; Wainberg, M.A. Clinical benefit of dolutegravir in HIV-1 management related to the high genetic barrier to drug resistance. Virus Res. 2017, 239, 1–9. [Google Scholar] [CrossRef]
- Boerma, R.S.; Boender, T.S.; van Hensbroek, M.B.; Rinke de Wit, T.F.; Sigaloff, K.C.E. Sequencing paediatric antiretroviral therapy in the context of a public health approach. J. Int. AIDS Soc. 2015, 18 (Suppl. S6), 20265. [Google Scholar] [CrossRef] [PubMed]
- Scallon, A.J.; Hassan, S.A.; Qian, S.R.; Gao, Y.; Oyaro, P.; Brown, E.; Wagude, J.; Mukui, I.; Kinywa, E.; Oluoch, F.; et al. “I feel drug resistance testing allowed us to make an informed decision”: Qualitative insights on the role of HIV drug resistance mutation testing among children and pregnant women living with HIV in western Kenya. BMC Health Serv. Res. 2023, 23, 908. [Google Scholar] [CrossRef] [PubMed]
- Kiekens, A.; de Casterlé, B.D.; Pellizzer, G.; Mosha, I.H.; Mosha, F.; de Wit, T.F.R.; Sangeda, R.Z.; Surian, A.; Vandaele, N.; Vranken, L.; et al. Exploring the mechanisms behind HIV drug resistance in sub-Saharan Africa: Conceptual mapping of a complex adaptive system based on multi-disciplinary expert insights. BMC Public Health 2022, 22, 455. [Google Scholar] [CrossRef]
- Bertagnolio, S.; De Luca, A.; Vitoria, M.; Essajee, S.; Penazzato, M.; Hong, S.Y.; McClure, C.; Duncombe, C.; Jordan, M.R. Determinants of HIV Drug Resistance and Public Health Implications in Low- and Middle-Income Countries. Antivir. Ther. 2012, 17, 941–953. [Google Scholar] [CrossRef] [PubMed]
- Bernheimer, J.M.; Patten, G.; Makeleni, T.; Mantangana, N.; Dumile, N.; Goemaere, E.; Cox, V. Paediatric HIV treatment failure: A silent epidemic. J. Int. AIDS Soc. 2015, 18, 20090. [Google Scholar] [CrossRef]
- Patel, R.C.; Oyaro, P.; Odeny, B.; Mukui, I.; Thomas, K.K.; Sharma, M.; Wagude, J.; Kinywa, E.; Oluoch, F.; Odhiambo, F.; et al. Optimizing viral load suppression in Kenyan children on antiretroviral therapy (Opt4Kids). Contemp. Clin. Trials Commun. 2020, 20, 100673. [Google Scholar] [CrossRef]
- Patel, R.C.; Oyaro, P.; Thomas, K.K.; Wagude, J.; Mukui, I.; Brown, E.; A Hassan, S.; Kinywa, E.; Oluoch, F.; Odhiambo, F.; et al. Point-of-care HIV viral load and targeted drug resistance mutation testing versus standard care for Kenyan children on antiretroviral therapy (Opt4Kids): An open-label, randomised controlled trial. Lancet Child Adolesc. Health 2022, 6, 681–691. [Google Scholar] [CrossRef]
- National AIDS and STI Control Programme (NASCOP). Preliminary KENPHIA 2018 Report. Published Online 2020. Available online: https://phia.icap.columbia.edu/wp-content/uploads/2020/04/KENPHIA-2018_Preliminary-Report_final-web.pdf (accessed on 20 July 2025).
- National AIDS and STI Control Programme (NASCOP). Kenya HIV Estimates 2015. Published online October 2016. Available online: https://nsdcc.go.ke/wp-content/uploads/2021/08/Kenya-HIV-Estimates-2015.pdf (accessed on 20 July 2025).
- Beck, I.A.; Boyce, C.L.; Bishop, M.D.; Oldroyd, A.R.; du Toit, L.; Saimen, A.; Ramarope, K.M.; Hitchcock, S.; du Plessis, N.M.; Mbogo, L.; et al. HIV resistance to dolutegravir varies with co-administered agents. Clin Infect Dis. 2025; in press. [Google Scholar] [CrossRef]
- Ministry of Health, National AIDS and STI Control Program (NASCOP). Guidelines on Use of Antiretroviral Drugs for Treating and Preventing HIV in Kenya, 2018 Edition. Published Online August 2018. Available online: https://cquin.icap.columbia.edu/wp-content/uploads/2017/04/ICAP_CQUIN_Kenya-ARV-Guidelines-2018-Final_20thAug2018.pdf (accessed on 21 July 2025).
- The Lancet HIV. End resistance to dolutegravir roll-out. Lancet HIV 2020, 7, e593. [Google Scholar] [CrossRef]
- Ministry of Health, National AIDS and STI Control Programme (NASCOP). Kenya HIV Prevention and Treatment Guidelines, 2022 Edition. Published Online August 2022. Available online: https://www.differentiatedservicedelivery.org/wp-content/uploads/Kenya-ARV-Guidelines-2022-Final-1.pdf (accessed on 10 July 2025).
- Tang, M.W.; Liu, T.F.; Shafer, R.W. The HIVdb system for HIV-1 genotypic resistance interpretation. Intervirology 2012, 55, 98–101. [Google Scholar] [CrossRef]
- World Health Organization. List of WHO-Designated Laboratories for HIV Drug Resistance Surveillance, November 2022. Published Online November 2022. Available online: https://cdn.who.int/media/docs/default-source/hq-hiv-hepatitis-and-stis-library/list_of_who-designated_hiv_drug_resistance_laboratories_november_2022.pdf?sfvrsn=c2b253ac_8 (accessed on 20 July 2025).
- National Public Health Institute. National HIV Reference Lab. Kenya National Public Health Institute. Available online: https://www.nphi.go.ke/national-hiv-reference-lab (accessed on 4 August 2025).
- Ahluwalia, A.K.; Inzaule, S.; Baggaley, R.C.; Vitoria, M.; Schaefer, R.; Schmidt, H.-M.A.; Rodolph, M.; Giron, A.; Jordan, M.R. Characterization of dolutegravir drug resistance in persons diagnosed with HIV after exposure to long-acting injectable cabotegravir for preexposure prophylaxis. AIDS 2022, 36, 1897–1898. [Google Scholar] [CrossRef] [PubMed]
- Rhee, S.-Y.; Jordan, M.R.; Raizes, E.; Chua, A.; Parkin, N.; Kantor, R.; Van Zyl, G.U.; Mukui, I.; Hosseinipour, M.C.; Frenkel, L.M.; et al. HIV-1 Drug Resistance Mutations: Potential Applications for Point-of-Care Genotypic Resistance Testing. PLoS ONE 2015, 10, e0145772. [Google Scholar] [CrossRef] [PubMed]
- Wensing, A.M.; Calvez, V.; Ceccherini-Silberstein, F.; Charpentier, C.; Gunthard, H.F.; Jacobsen, D.M.; Paredes, R.; Shafer, R.W.; Richman, D.D. 2025 update of the drug resistance mutations in HIV-1. Top. Antivir. Med. 2025, 33, 457–473. [Google Scholar]
- Vizzotto, A.D.B.; de Oliveira, A.M.; Elkis, H.; Cordeiro, Q.; Buchain, P.C. Psychosocial Characteristics. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 1578–1580. [Google Scholar] [CrossRef]
- Friedland, B.A.; Gottert, A.; Hows, J.; Baral, S.D.; Sprague, L.; Nyblade, L.; McClair, T.L.; Anam, F.; Geibel, S.; Kentutsi, S.; et al. The People Living with HIV Stigma Index 2.0: Generating critical evidence for change worldwide. AIDS 2020, 34 (Suppl. S1), S5–S18. [Google Scholar] [CrossRef]
- Monahan, P.O.; Shacham, E.; Reece, M.; Kroenke, K.; Ong’oR, W.O.; Omollo, O.; Yebei, V.N.; Ojwang, C. Validity/reliability of PHQ-9 and PHQ-2 depression scales among adults living with HIV/AIDS in western Kenya. J. Gen. Intern. Med. 2009, 24, 189–197. [Google Scholar] [CrossRef]
- Mazza, M.; Marano, G.; del Castillo, A.G.; Chieffo, D.; Monti, L.; Janiri, D.; Moccia, L.; Sani, G. Intimate partner violence: A loop of abuse, depression and victimization. World J. Psychiatry 2021, 11, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Moreno, C.; Jansen, H.A.F.M.; Ellsberg, M.; Heise, L.; Watts, C.H. Prevalence of intimate partner violence: Findings from the WHO multi-country study on women’s health and domestic violence. Lancet 2006, 368, 1260–1269. [Google Scholar] [CrossRef] [PubMed]
- Casimir, G.J.; Tobi, H. Defining and using the concept of household: A systematic review. Int. J. Consum. Stud. 2011, 35, 498–506. [Google Scholar] [CrossRef]
- Coates, J.; Swindale, A.; Bilinsky, P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Household Food Access: Indicator Guide (v. 3). Published Online August 2007. Available online: https://www.fantaproject.org/sites/default/files/resources/HFIAS_ENG_v3_Aug07.pdf (accessed on 20 June 2025).
- Heller, J.C.; Givens, M.L.; Johnson, S.P.; Kindig, D.A. Keeping It Political and Powerful: Defining the Structural Determinants of Health. Milbank Q. 2024, 102, 351–366. [Google Scholar] [CrossRef] [PubMed]
- Kantor, R. INSTI era resistance: Emerging concern or marginal issue? Lancet HIV 2023, 10, e696–e698. [Google Scholar] [CrossRef] [PubMed]
- Haberer, J.E.; Kiwanuka, J.; Nansera, D.; Ragland, K.; Mellins, C.; Bangsberg, D.R. Multiple Measures Reveal Antiretroviral Adherence Successes and Challenges in HIV-Infected Ugandan Children. PLoS ONE 2012, 7, e36737. [Google Scholar] [CrossRef]
- Bearden, D.R.; Sportiello, K.; Mweemba, M.; Lungu, F.; Mwanza-Kabaghe, S.; Birbeck, G. Adherence, Adverse Events and Viral Control among Children and Adolescents with HIV in Zambia Switched to an Integrase Inhibitor Regimen. medRxiv 2024, medRxiv:2024.09.17.24313837. [Google Scholar] [CrossRef]
- Muri, L.; Gamell, A.; Ntamatungiro, A.J.; Glass, T.R.; Luwanda, L.B.; Battegay, M.; Furrer, H.; Hatz, C.; Tanner, M.; Felger, I.; et al. Development of HIV drug resistance and therapeutic failure in children and adolescents in rural Tanzania: An emerging public health concern. AIDS 2017, 31, 61–70. [Google Scholar] [CrossRef]
- Khamadi, S.A.; Bahemana, E.; Dear, N.; Mavere, C.; George, F.; Kapene, R.; Papianus, G.; Willoughby, W.; Chambers, J.; Ganesan, K.; et al. Factors Associated With Viral Suppression and Drug Resistance in Children and Adolescents Living With HIV in Care and Treatment Programs in Southern Tanzania. J. Pediatr. Infect. Dis. Soc. 2023, 12, 353–363. [Google Scholar] [CrossRef]
- Sia, D.; Onadja, Y.; Nandi, A.; Foro, A.; Brewer, T. What lies behind gender inequalities in HIV/AIDS in sub-Saharan African countries: Evidence from Kenya, Lesotho and Tanzania. Health Policy Plan. 2014, 29, 938–949. [Google Scholar] [CrossRef]
- Nesamoney, S.N.; Mejía-Guevara, I.; Cislaghi, B.; Weber, A.M.; Mbizvo, M.T.; Darmstadt, G.L. Social normative origins of the taboo gap and implications for adolescent risk for HIV infection in Zambia. Soc. Sci. Med. 2022, 312, 115391. [Google Scholar] [CrossRef]
- Levy, J.K.; Darmstadt, G.L.; Ashby, C.; Quandt, M.; Halsey, E.; Nagar, A.; Greene, M.E. Characteristics of successful programmes targeting gender inequality and restrictive gender norms for the health and wellbeing of children, adolescents, and young adults: A systematic review. Lancet Glob. Health 2020, 8, e225–e236. [Google Scholar] [CrossRef] [PubMed]
- Embleton, L.; Logie, C.H.; Ngure, K.; Nelson, L.; Kimbo, L.; Ayuku, D.; Turan, J.M.; Braitstein, P. Intersectional Stigma and Implementation of HIV Prevention and Treatment Services for Adolescents Living with and at Risk for HIV: Opportunities for Improvement in the HIV Continuum in Sub-Saharan Africa. AIDS Behav. 2023, 27 (Suppl. S1), 162–184. [Google Scholar] [CrossRef]
- Campbell, C.; Cornish, F. Towards a “fourth generation” of approaches to HIV/AIDS management: Creating contexts for effective community mobilisation. AIDS Care 2010, 22 (Suppl. S2), 1569–1579. [Google Scholar] [CrossRef]
- Gupta, G.; Ogden, J.; Warner, A. Moving forward on women’s gender-related HIV vulnerability: The good news, the bad news and what to do about it. Glob. Public Health 2011, 6, S370–S382. [Google Scholar] [CrossRef] [PubMed]
- Shannon, K.; Leiter, K.; Phaladze, N.; Hlanze, Z.; Tsai, A.C.; Heisler, M.; Iacopino, V.; Weiser, S.D.; Kissinger, P. Gender inequity norms are associated with increased male-perpetrated rape and sexual risks for HIV infection in Botswana and Swaziland. PLoS ONE 2012, 7, e28739. [Google Scholar] [CrossRef] [PubMed]
- Subedar, H.; Barnett, S.; Chaka, T.; Dladla, S.; Hagerman, E.; Jenkins, S.; Matshimane, G.; Mangold, K.; Msimanga, B.; Pooe, R.; et al. Tackling HIV by empowering adolescent girls and young women: A multisectoral, government led campaign in South Africa. BMJ 2018, 363, k4585. [Google Scholar] [CrossRef]
- Gupta, G.R.; Parkhurst, J.O.; Ogden, J.A.; Aggleton, P.; Mahal, A. Structural approaches to HIV prevention. Lancet 2008, 372, 764–775. [Google Scholar] [CrossRef]
- Billioux, V.G.; Grabowski, M.K.; Ssekasanvu, J.; Reynolds, S.J.; Berman, A.; Bazaale, J.; Patel, E.U.; Bugos, E.; Ndyanabo, A.; Kisakye, A.; et al. HIV viral suppression and geospatial patterns of HIV antiretroviral therapy treatment facility use in Rakai, Uganda. AIDS 2018, 32, 819–824. [Google Scholar] [CrossRef]
- Mee, P.; Rice, B.; Kabudula, C.W.; Tollman, S.M.; Gómez-Olivé, F.X.; Reniers, G. The impact of HIV status on the distance traveled to health facilities and adherence to care. A record-linkage study from rural South Africa. J. Glob. Health 2020, 10, 020435. [Google Scholar] [CrossRef]
- Akullian, A.N.; Mukose, A.; Levine, G.A.; Babigumira, J.B. People living with HIV travel farther to access healthcare: A population-based geographic analysis from rural Uganda. J. Int. AIDS Soc. 2016, 19, 20171. [Google Scholar] [CrossRef]
- Kloos, H.; Assefa, Y.; Adugna, A.; Mulatu, M.S.; Mariam, D.H. Utilization of antiretroviral treatment in Ethiopia between February and December 2006: Spatial, temporal, and demographic patterns. Int. J. Health Geogr. 2007, 6, 45. [Google Scholar] [CrossRef] [PubMed]
- Adeneye, A.K.; Adewole, T.A.; Musa, A.Z.; Onwujekwe, D.; Odunukwe, N.N.; Araoyinbo, I.D.; Gbajabiamila, T.A.; Ezeobi, P.M.; Idigbe, E.O. Limitations to Access and Use of Antiretroviral Therapy (ART) Among HIV Positive Persons in Lagos, Nigeria. World Health Popul. 2006, 8, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Lankowski, A.J.; Siedner, M.J.; Bangsberg, D.R.; Tsai, A.C. Impact of geographic and transportation-related barriers on HIV outcomes in sub-Saharan Africa: A systematic review. AIDS Behav. 2014, 18, 1199–1223. [Google Scholar] [CrossRef] [PubMed]


| Total n = 704 | Children Without DR testing or DR-PS < 30 n = 611 | Children with DR-PS ≥ 30 n = 93 | |
|---|---|---|---|
| Characteristics | N (%) | N (%) | N (%) |
| Child Clinical Characteristics | |||
| Age, median (IQR) | 10 (7, 12) | 10 (7, 12) | 9 (5, 12) |
| Age category (years) | |||
| 1–5 | 79 (11.2) | 55 (9.0) | 24 (25.8) |
| 6–10 | 301 (42.8) | 269 (44.0) | 32 (34.4) |
| 11–15 | 324 (46.0) | 287 (47.0) | 37 (39.8) |
| Sex | |||
| Male | 360 (51.1) | 313 (51.2) | 49 (48.04) |
| Female | 344 (48.9) | 298 (48.8) | 53 (51.96) |
| History of VF within two years prior to enrolling in Opt4Kids | |||
| Yes | 144 (20.5) | 87 (14.2) | 57 (61.3) |
| No | 504 (71.6) | 476 (77.9) | 28 (30.1) |
| Missing | 56 (8.0) | 48 (7.9) | 8 (8.6) |
| Base drug in ART regimen at time of DR test analysis | |||
| NNRTI-containing | 363 (51.6) | 343 (56.1) | 20 (21.5) |
| PI-containing | 285 (40.5) | 240 (39.3) | 45 (48.4) |
| INSTI-containing | 55 (7.8) | 27 (4.4) | 28 (30.1) |
| Only NRTI-containing | 1 (0.1) | 1 (0.2) | 0 |
| Co-administered NRTIs at time of DR test analysis | |||
| ABC + 3TC | 479 (68.0) | 425 (69.6) | 54 (58.1) |
| AZT + 3TC | 135 (19.2) | 115 (18.8) | 20 (21.5) |
| TDF + 3TC | 90 (12.8) | 71 (11.6) | 19 (20.4) |
| Full ART regimen at the time of DR test analysis 1 | |||
| NNRTI-containing | |||
| ABC + 3TC + EFV | 203 (28.8) | 194 (31.8) | 9 (9.7) |
| ABC + 3TC + NVP | 47 (6.7) | 42 (6.9) | 5 (5.4) |
| AZT + 3TC + NVP | 41 (5.8) | 40 (6.5) | 1 (1.1) |
| AZT + 3TC + EFV | 12 (1.7) | 11 (1.8) | 1 (1.1) |
| TDF + 3TC + EFV | 60 (8.5) | 56 (9.2) | 4 (4.3) |
| PI-containing | |||
| ABC + 3TC + LPV/r | 198 (28.1) | 172 (28.2) | 26 (28.0) |
| AZT + 3TC + LPV/r | 72 (10.2) | 58 (9.5) | 14 (15.1) |
| AZT + 3TC + ATV/r | 6 (0.9) | 4 (0.7) | 2 (2.2) |
| TDF + 3TC + ATV/r | 4 (0.6) | 3 (0.5) | 1 (1.1) |
| TDF + 3TC + LPV/r | 4 (0.6) | ||
| INSTI-containing | 2 (0.3) | 2 (2.2) | |
| ABC + 3TC + DTG | 31 (4.4) | 17 (2.8) | 14 (15.1) |
| AZT + 3TC + DTG | 3 (0.4) | 1 (0.2) | 2 (2.2) |
| TDF + 3TC + DTG | 21 (3.0) | 9 (1.5) | 12 (12.9) |
| Other | |||
| TDF + 3TC + DTG + ATV/r | 1 (0.1) | 1 (0.2) | 0 |
| AZT + 3TC + ABC | 1 (0.1) | 1 (0.2) | 0 |
| Frequency of resistance to multiple drugs (DR-PS > 30) within an ART drug class 2 | |||
| NRTI—1 drug | - | - | 3 (3.2) |
| NRTI—>2 drugs | - | - | 69 (74.2) |
| NNRTI—1 drug | - | - | 0 |
| NNRTI—>2 drugs | - | - | 82 (88.2) |
| PI—1 drug | - | - | 1 (1.1) |
| PI—>2 drugs | - | - | 6 (6.5) |
| INSTI—1 drug | - | - | 0 |
| INSTI—>2 drugs | - | - | 3 (3.2) |
| Caregiver Clinical Characteristics | |||
| Age of caregiver | |||
| <24 years | 40 (5.7) | 31 (5.1) | 9 (9.7) |
| 24–35 years | 325 (46.2) | 272 (44.5) | 53 (57.0) |
| >35 years | 336 (47.7) | 305 (49.9) | 31 (33.3) |
| Missing | 3 (0.4) | 3 (0.5) | 0 |
| Caregiver viral suppression | |||
| Yes | 431 (61.2) | 379 (62.0) | 52 (55.9) |
| No | 39 (5.5) | 30 (4.9) | 9 (9.7) |
| Not applicable | 135 (19.2) | 116 (19.0) | 19 (20.4) |
| Unknown | 99 (14.1) | 86 (14.1) | 13 (14.0) |
| Child Psychosocial Characteristics | |||
| School level | |||
| Nursery | 124 (17.6) | 107 (17.5) | 17 (18.3) |
| Primary | 512 (72.7) | 454 (74.3) | 58 (62.4) |
| Secondary | 4 (0.6) | 4 (0.7) | 0 |
| Missing | 64 (9.1) | 46 (7.5) | 18 (19.4) |
| School type | |||
| Day school | 631 (89.6) | 557 (91.2) | 74 (79.6) |
| Boarding | 4 (0.6) | 4 (0.7) | 0 |
| Mix of day and boarding | 7 (1.0) | 6 (1.0) | 1 (1.1) |
| Missing | 62 (8.8) | 44 (7.2) | 18 (19.4) |
| ART adherence | |||
| Good | 558 (79.3) | 499 (81.7) | 59 (63.4) |
| Poor | 146 (20.7) | 112 (18.3) | 34 (36.6) |
| Adolescence awareness of status | |||
| No | 408 (58.0) | 352 (57.6) | 56 (60.2) |
| Yes | 296 (42.0) | 259 (42.4) | 37 (39.8) |
| Caregiver Psychosocial Characteristics | |||
| Caregiver marital status | |||
| Married | 442 (62.8) | 380 (62.2) | 62 (66.7) |
| Unmarried | 261 (97.1) | 230 (37.6) | 31 (33.3) |
| Unknown | 1 (0.1) | 1 (0.2) | 0 |
| Educational attainment of caregiver | |||
| No Education | 29 (4.1) | 27 (4.4) | 2 (2.2) |
| Primary | 398 (56.5) | 344 (56.3) | 54 (58.1) |
| Secondary & above | 277 (39.3) | 240 (39.3) | 37 (39.8) |
| Caregiver depression | |||
| Yes | 252 (35.8) | 205 (34.75) | 40 (43.0) |
| No | 451 (64.1) | 398 (65.1) | 53 (57.0) |
| Missing | 1 (0.14) | 1 (0.2) | 0 |
| Caregiver stigma | |||
| Yes | 105 (14.9) | 93 (15.2) | 12 (12.9) |
| No | 505 (71.7) | 436 (71.4) | 69 (74.2) |
| Missing | 94 (13.4) | 82 (13.4) | 12 (12.9) |
| HIV literacy | |||
| Yes | 331 (47.0) | 287 (47.0) | 49 (52.7) |
| No | 373 (53.0) | 324 (53.0) | 44 (47.3) |
| Medicine administration confidence | |||
| Yes | 665 (94.5) | 582 (95.3) | 83 (89.2) |
| No | 39 (5.5) | 29 (4.7) | 10 (10.8) |
| Caregiver intimate partner violence | |||
| Yes | 163 (23.2) | 140 (22.9) | 23 (24.7) |
| No | 540 (76.7) | 470 (76.9) | 70 (75.3) |
| Missing | 1 (0.1) | 1 (0.2) | 0 |
| Household Psychosocial Characteristics | |||
| Food insecurity | |||
| No | 16 (2.3) | 15 (2.5) | 1 (1.1) |
| Yes | 687 (97.6) | 595 (97.4) | 92 (98.9) |
| Missing | 1 (0.1) | 1 (0.2) | 0 |
| Other children in the home | |||
| Yes | 630 (89.5) | 544 (89.0) | 86 (92.5) |
| No | 71 (10.1) | 64 (10.5) | 7 (7.5) |
| Missing | 3 (0.4) | 3 (0.5) | 0 |
| Other CLHIV in the home | |||
| Yes | 107 (15.2) | 96 (15.7) | 11 (11.8) |
| No | 593 (84.2) | 512 (83.8) | 81 (87.1) |
| Missing | 4 (0.6) | 3 (0.5) | 1 (1.1) |
| Structural Characteristics | |||
| Travel time to facility | |||
| <30 min | 231 (32.8) | 188 (30.8) | 43 (46.2) |
| 30 min to 1 h | 309 (43.9) | 278 (45.5) | 31 (33.3) |
| >1 h | 164 (23.3) | 145 (23.7) | 19 (20.4) |
| Clinic location | |||
| Urban | 421 (59.8) | 367 (60.1) | 54 (58.1) |
| Semi-urban | 158 (22.4) | 132 (21.6) | 26 (28.0) |
| Rural | 125 (17.8) | 106 (17.97) | 13 (14.0) |
| Clinic population volume | |||
| Heavy | 203 (28.8) | 180 (29.5) | 23 (24.7) |
| Medium | 439 (62.4) | 383 (62.7) | 56 (60.2) |
| Light | 62 (8.8) | 48 (7.9) | 14 (15.1) |
| Unadjusted RR 1 | p-Value | Adjusted RR 1 | p-Value | |
|---|---|---|---|---|
| Child Clinical Characteristics | ||||
| Age category (years) | ||||
| 1–5 | 2.66 (1.69, 4.18) | <0.001 | 1.84 (1.07, 3.14) | 0.026 |
| 6–10 | 0.93 (0.60, 1.45) | 0.753 | 0.77 (0.51, 1.16) | 0.211 |
| 11–15 (Ref) | 1.0 | |||
| Sex | ||||
| Male (Ref) | 1.0 | |||
| Female | 1.02 (0.70, 1.5) | 0.901 | ||
| History of VF within two years prior to enrolling in Opt4Kids | ||||
| Yes | 7.13 (4.72, 10.76) | <0.001 | 4.18 (2.77, 6.31) | <0.001 |
| No (Ref) | 1.0 | |||
| Base drug in ART regimen at time of DR test analysis | ||||
| NNRTI-containing (Ref) | 1.0 | |||
| PI-containing | 2.87 (1.73, 4.74) | <0.001 | 6.05 (3.43, 10.68) | <0.001 |
| INSTI-containing | 9.24 (5.61, 15.22) | <0.001 | 1.83 (1.08, 3.11) | 0.026 |
| Only NRTI-containing 2 | - | - | ||
| Co-administered NRTIs at time of DR test analysis 3 | ||||
| ABC + 3TC (Ref) | 1.0 | |||
| AZT + 3TC | 1.31 (0.82, 2.12) | 0.260 | ||
| TDF + 3TC | 1.87 (1.17, 3.0) | 0.009 | ||
| Caregiver Clinical Characteristics | ||||
| Age of caregiver | ||||
| <24 years | 2.44 (1.25, 4.75) | 0.009 | 1.10 (0.64, 1.87) | 0.738 |
| 24–35 years | 1.77 (1.17, 2.68) | 0.007 | 1.28 (0.86, 1.91) | 0.226 |
| >35 years (Ref) | 1.0 | |||
| Caregiver viral suppression | ||||
| Yes (Ref) | 1.0 | |||
| No | 1.91 (1.02, 3.58) | 0.043 | 1.37 (0.74, 2.54) | 0.321 |
| Not applicable | 1.17 (0.72, 1.90) | 0.537 | 1.21 (0.80, 1.83) | 0.356 |
| Unknown | 1.09 (0.62, 1.92) | 0.769 | 1.42 (0.83, 2.45) | 0.202 |
| Child Psychosocial Characteristics | ||||
| School level | ||||
| Nursery (Ref) | 1.0 | |||
| Primary | 0.83 (0.50, 1.37) | 0.458 | ||
| Secondary 2 | - | |||
| School type | 0.832 | |||
| Day school | 0.82 (0.13, 5.1) | |||
| Boarding 2 | - | |||
| Mix of day and boarding (Ref) | 1.0 | |||
| ART adherence | ||||
| Good (Ref) | 1.0 | |||
| Poor | 2.2 (1.51, 3.22) | <0.001 | 1.91 (1.32, 2.76) | 0.001 |
| Adolescence awareness of status | ||||
| No | 1.1 (0.75, 1.62) | |||
| Yes (Ref) | 1.0 | 0.636 | ||
| Caregiver Psychosocial Characteristics | ||||
| Caregiver marital status | 0.419 | |||
| Married | 1.18 (0.79, 1.77) | |||
| Unmarried (Ref) | 1.0 | |||
| Unknown 2 | - | |||
| Caregiver educational attainment | ||||
| No Education | 0.52 (0.13, 2.03) | 0.345 | ||
| Primary | 1.02 (0.69, 1.5) | 0.937 | ||
| Secondary & above (Ref) | 1.0 | |||
| Caregiver depression | 0.122 | 1.02 (0.70, 1.49) | 0.916 | |
| Yes | 1.35 (0.92, 1.98) | |||
| No (Ref) | 1.0 | |||
| Caregiver stigma | 0.543 | |||
| Yes | 0.84 (0.47, 1.49) | |||
| No (Ref) | 1.0 | |||
| Caregiver HIV literacy | 0.951 | |||
| Yes | 0.99 (0.68, 1.44) | |||
| No (Ref) | 1.0 | |||
| Caregiver medicine administration confidence | ||||
| Yes (Ref) | 1.0 | |||
| No | 2.05 (1.16, 3.64) | 0.014 | 1.89 (1.11, 3.22) | 0.019 |
| Caregiver intimate partner violence | ||||
| Yes | 1.09 (0.7, 1.69) | 0.704 | ||
| No (Ref) | 1.0 | |||
| Household Psychosocial Characteristics | ||||
| Household food insecurity | ||||
| No (Ref) | 1.0 | |||
| Yes | 2.14 (0.32, 14.43) | 0.434 | ||
| Other children in the household | 0.382 | |||
| Yes | 1.38 (0.67, 2.87) | |||
| No (Ref) | 1.0 | |||
| Other CLHIV in the household | ||||
| Yes (Ref) | 1.0 | |||
| No | 1.33 (0.73, 2.41) | 0.349 | ||
| Structural Characteristics | ||||
| Time to facility | ||||
| <30 min (Ref) | 1.0 | |||
| 30 min to 1 h | 0.54 (0.35, 0.83) | 0.004 | 0.72 (0.47, 1.12) | 0.144 |
| >1 h | 0.62 (0.38, 1.03) | 0.064 | 0.71 (0.44, 1.14) | 0.156 |
| Clinic location | ||||
| Rural | 0.81 (0.46, 1.44) | 0.472 | ||
| Semi-urban | 1.28 (0.83, 1.97) | 0.257 | ||
| Urban (Ref) | 1.0 | |||
| Clinic volume | ||||
| Light (Ref) | 1.0 | |||
| Medium | 0.56 (0.34, 0.95) | 0.024 | 0.55 (0.33, 0.92) | 0.023 |
| Heavy | 0.5 (0.28, 0.91) | 0.032 | 0.76 (0.41, 1.39) | 0.371 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scallon, A.J.; Maheria, P.; Oyaro, P.; Thomas, K.K.; Chohan, B.H.; Odhiambo, F.; Brown, E.; Ochomo, E.; Karauki, E.; Yongo, N.; et al. Clinical, Psychosocial, and Structural Factors Associated with the Detection of HIV Drug Resistance in Children Living with HIV in Kisumu, Kenya: Secondary Analysis of Data from the Opt4Kids Study. Viruses 2025, 17, 1246. https://doi.org/10.3390/v17091246
Scallon AJ, Maheria P, Oyaro P, Thomas KK, Chohan BH, Odhiambo F, Brown E, Ochomo E, Karauki E, Yongo N, et al. Clinical, Psychosocial, and Structural Factors Associated with the Detection of HIV Drug Resistance in Children Living with HIV in Kisumu, Kenya: Secondary Analysis of Data from the Opt4Kids Study. Viruses. 2025; 17(9):1246. https://doi.org/10.3390/v17091246
Chicago/Turabian StyleScallon, Andrea J., Pooja Maheria, Patrick Oyaro, Katherine K. Thomas, Bhavna H. Chohan, Francesca Odhiambo, Evelyn Brown, Edwin Ochomo, Enericah Karauki, Nashon Yongo, and et al. 2025. "Clinical, Psychosocial, and Structural Factors Associated with the Detection of HIV Drug Resistance in Children Living with HIV in Kisumu, Kenya: Secondary Analysis of Data from the Opt4Kids Study" Viruses 17, no. 9: 1246. https://doi.org/10.3390/v17091246
APA StyleScallon, A. J., Maheria, P., Oyaro, P., Thomas, K. K., Chohan, B. H., Odhiambo, F., Brown, E., Ochomo, E., Karauki, E., Yongo, N., Hassan, S. A., Bishop, M. D., Beck, I. A., Boyce, C., Frenkel, L. M., Abuogi, L., & Patel, R. C. (2025). Clinical, Psychosocial, and Structural Factors Associated with the Detection of HIV Drug Resistance in Children Living with HIV in Kisumu, Kenya: Secondary Analysis of Data from the Opt4Kids Study. Viruses, 17(9), 1246. https://doi.org/10.3390/v17091246







