Predicting COVID-19 Sepsis Outcomes: Roles of IL-6, Cardiac Biomarkers, Clinical Factors, and Vaccination Status and Exploratory Analysis of Tocilizumab Therapy in an Eastern European Cohort
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. General Characteristics of Study Population
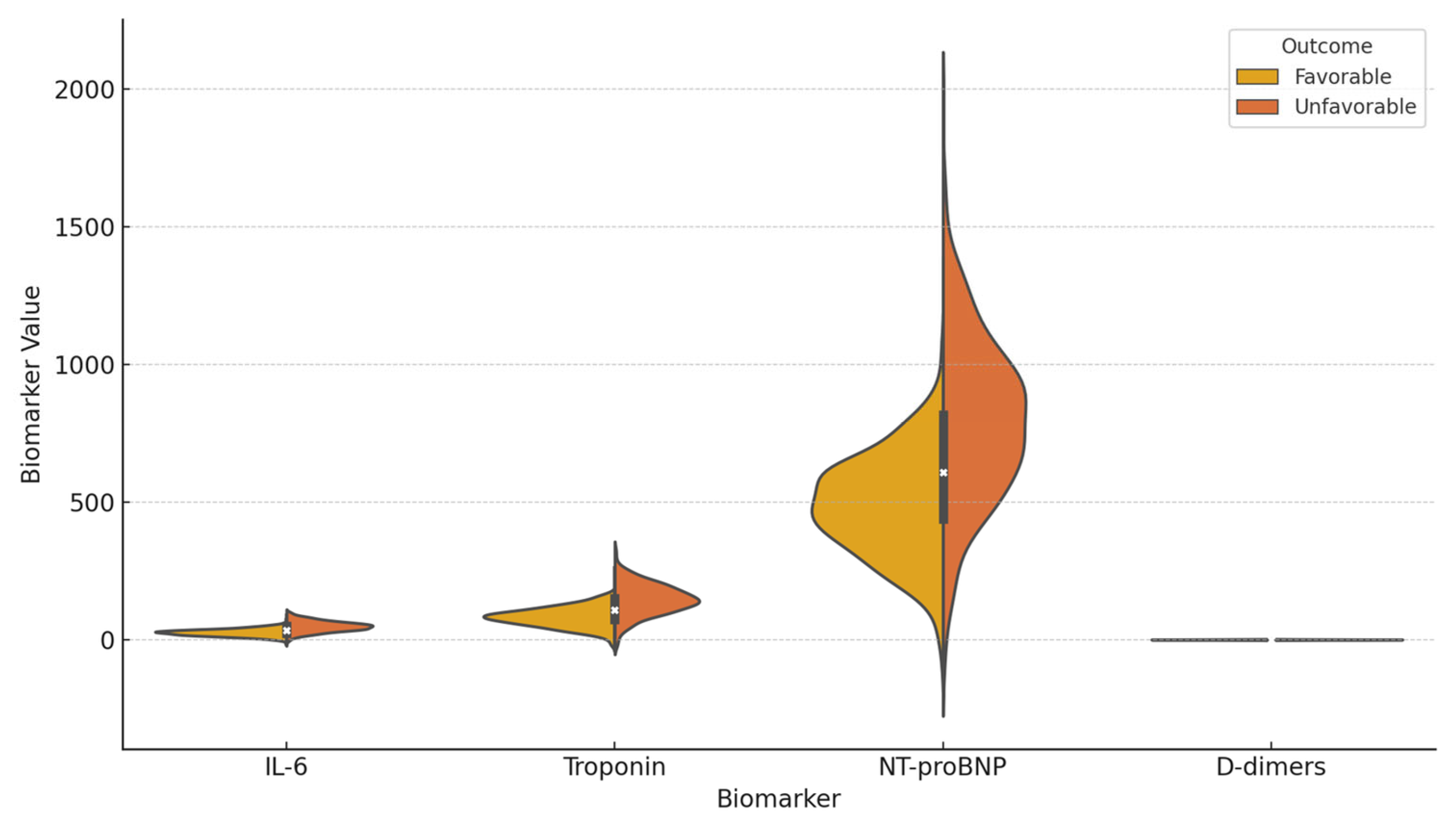
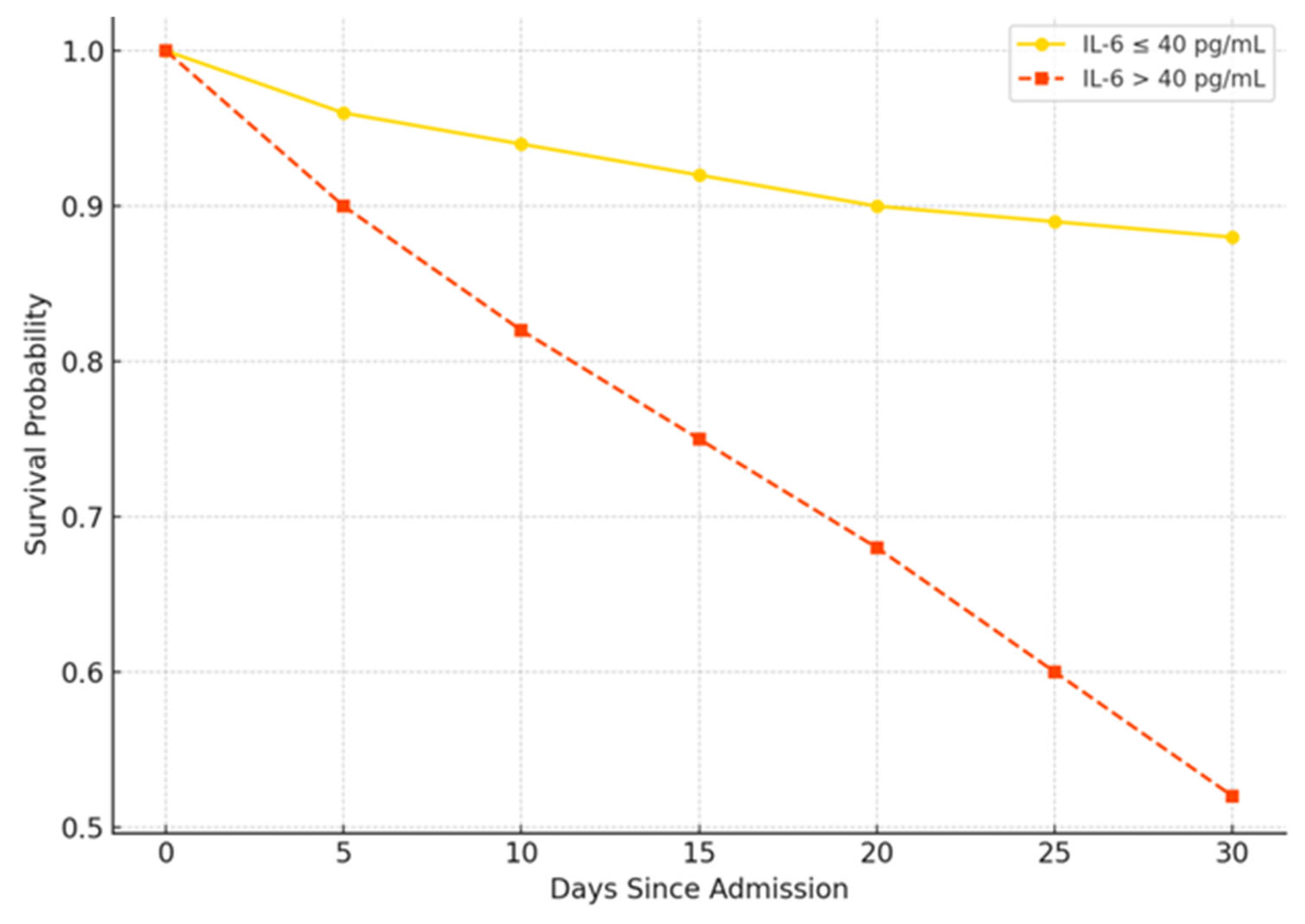
3.2. Univariate Analysis of Factors Associated with Unfavorable Outcomes
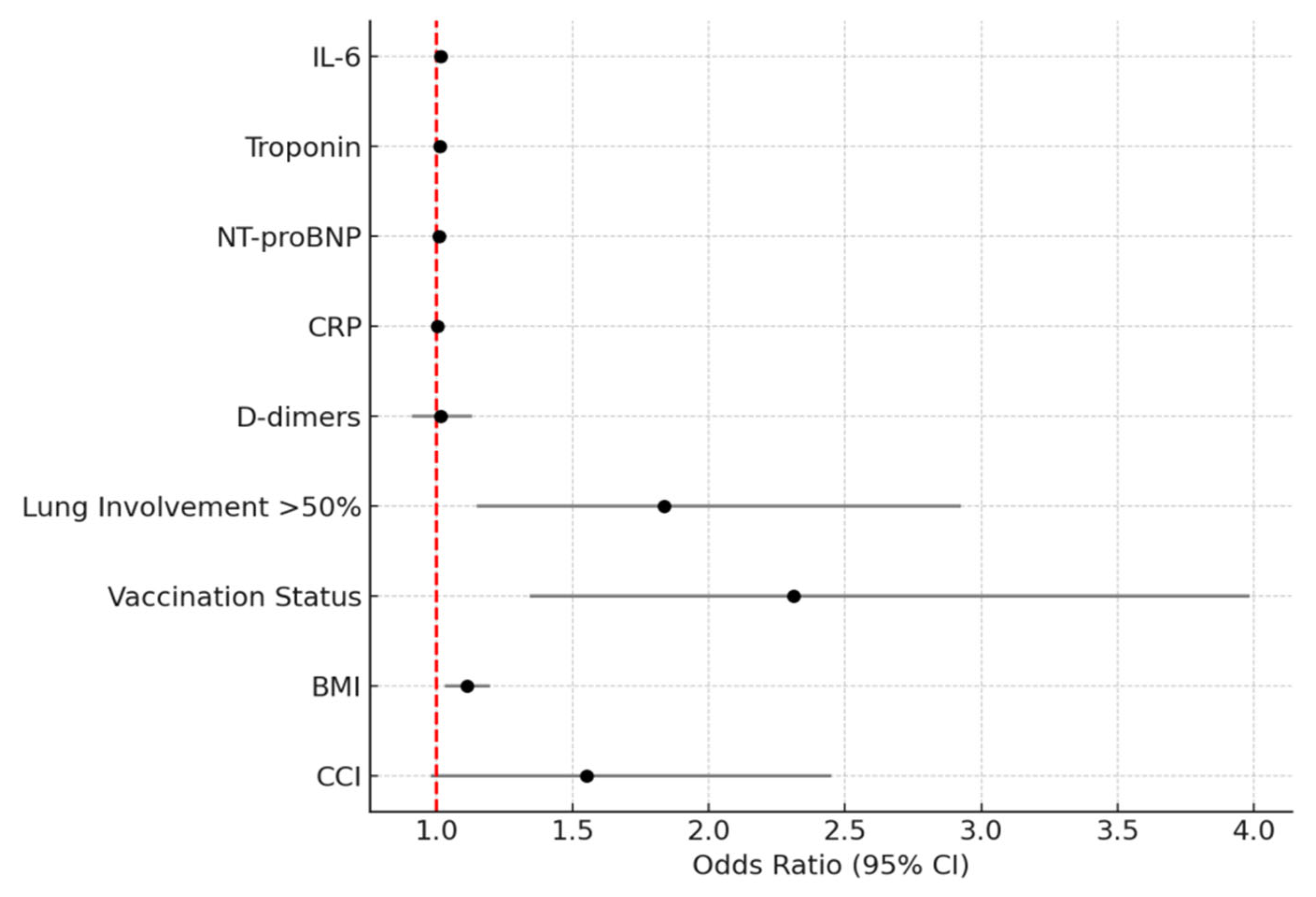
3.3. Multivariable Analysis of Predictors of Unfavorable Outcomes
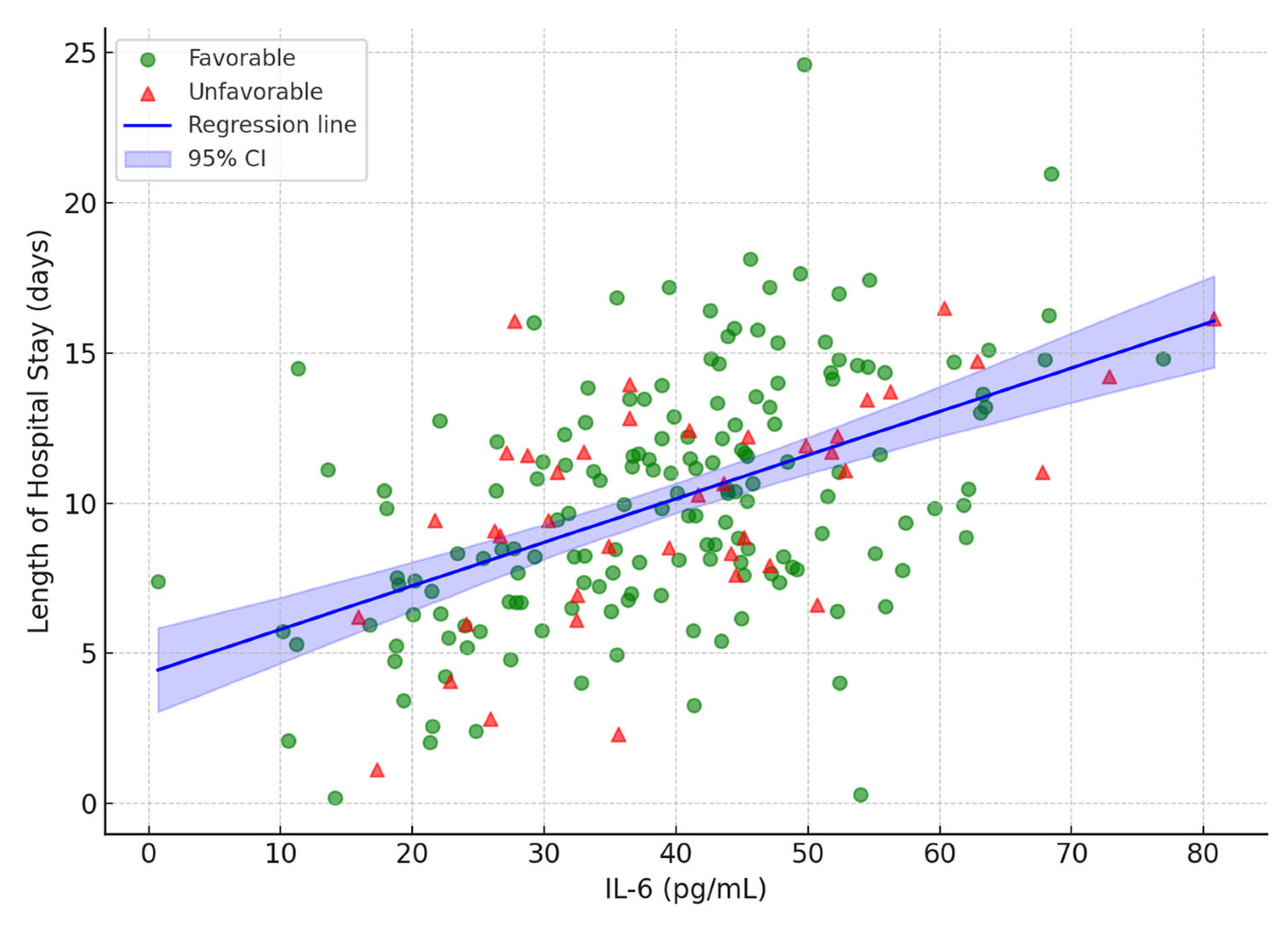
3.4. Linear Regression Analysis of Continuous Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NT-proBNP | N-Terminal Pro-B-Type Natriuretic Peptide |
| IL-6 | Interleukin-6 |
| CRP | C-Reactive Protein |
| PCT | Procalcitonin |
| SpO2 | Oxygen Saturation Measured by Pulse Oximetry |
| CT | Computed Tomography |
| ICU | Intensive Care Unit |
| LOS | Length of Stay |
| CCI | Charlson Comorbidity Index |
| BMI | Body Mass Index |
| AUC | Area Under the Curve (ROC) |
| ROC | Receiver Operating Characteristic curve |
| COVID-19 | Coronavirus Disease 2019 |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome Coronavirus 2 |
| MV | Mechanical Ventilation |
| SOFA | Sequential Organ Failure Assessment |
| AUROC | Area Under the Receiver Operating Characteristic Curve |
| OR | Odds Ratio |
| CI | Confidence Interval |
| SD | Standard Deviation |
| IQR | Interquartile Range |
| p | p-Value |
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- La Via, L.; Sangiorgio, G.; Stefani, S.; Marino, A.; Nunnari, G.; Cocuzza, S.; La Mantia, I.; Cacopardo, B.; Stracquadanio, S.; Spampinato, S.; et al. The global burden of sepsis and septic shock. Epidemiologia 2024, 5, 456–478. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.C. COVID-19 sepsis: Pathogenesis and endothelial molecular mechanisms based on “two-path unifying theory” of hemostasis and endotheliopathy-associated vascular microthrombotic disease, and proposed therapeutic approach with antimicrothrombotic therapy. Vasc. Health Risk Manag. 2021, 17, 273–298. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Chousterman, B.G.; Swirski, F.K.; Weber, G.F. Cytokine storm and sepsis disease pathogenesis. Semin. Immunopathol. 2017, 39, 517–528. [Google Scholar] [CrossRef]
- Chaudhry, H.; Zhou, J.; Zhong, Y.; Ali, M.M.; McGuire, F.; Nagarkatti, P.S.; Nagarkatti, M. Role of cytokines as a double-edged sword in sepsis. In Vivo 2013, 27, 669–684. [Google Scholar] [PubMed]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J.; on behalf of theHLH Across Speciality Collaboration, UK. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Herold, T.; Jurinovic, V.; Arnreich, C.; Lipworth, B.J.; Hellmuth, J.C.; von Bergwelt-Baildon, M.; Klein, M.; Weinberger, T. Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J. Allergy Clin. Immunol. 2020, 146, 128–136.e4. [Google Scholar] [CrossRef]
- Coomes, E.A.; Haghbayan, H. Interleukin-6 in COVID-19: A systematic review and meta-analysis. Rev. Med. Virol. 2020, 30, 1–9. [Google Scholar] [CrossRef]
- Varga, N.I.; Bagiu, I.C.; Vulcanescu, D.D.; Lazureanu, V.; Turaiche, M.; Rosca, O.; Bota, A.V.; Horhat, F.G. IL-6 baseline values and dynamic changes in predicting sepsis mortality: A systematic review and meta-analysis. Biomolecules 2025, 15, 407. [Google Scholar] [CrossRef]
- Zinellu, A.; Sotgia, S.; Carru, C.; Mangoni, A.A. B-type natriuretic peptide concentrations, COVID-19 severity, and mortality: A systematic review and meta-analysis with meta-regression. Front. Cardiovasc. Med. 2021, 8, 690790. [Google Scholar] [CrossRef]
- Chi, L.; Wang, S.; Wang, X.; Yang, C.; Luo, J. Predictive value of C-reactive protein for disease severity and survival in COVID-19 patients: A systematic review and meta-analysis. Clin. Exp. Med. 2023, 23, 2001–2008. [Google Scholar] [CrossRef] [PubMed]
- Huang, I.; Pranata, R.; Lim, M.A.; Oehadian, A.; Alisjahbana, B. C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: A meta-analysis. Ther. Adv. Respir. Dis. 2020, 14, 1753466620937175. [Google Scholar] [CrossRef] [PubMed]
- Nemec, H.M.; Ferenczy, A.; Christie, B.D., 3rd; Ashley, D.W.; Montgomery, A. Correlation of D-dimer and outcomes in COVID-19 patients. Am. Surg. 2022, 88, 2115–2118. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.; Su, Z.; Komissarov, A.A.; Liu, S.L.; Yi, G.; Idell, S.; Matthay, M.A.; Ji, H.-L. Associations of D-dimer on admission and clinical features of COVID-19 patients: A systematic review, meta-analysis, and meta-regression. Front. Immunol. 2021, 12, 691249. [Google Scholar] [CrossRef]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020, 5, 802–810. [Google Scholar] [CrossRef]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811–818. [Google Scholar] [CrossRef]
- Kim, C.W.; Aronow, W.S. COVID-19, cardiovascular diseases and cardiac troponins. Future Cardiol. 2022, 18, 135–142. [Google Scholar] [CrossRef]
- Vrsalovic, M.; VrsalovicPresecki, A. Cardiac troponins predict mortality in patients with COVID-19: A meta-analysis of adjusted risk estimates. J. Infect. 2020, 81, e99–e100. [Google Scholar] [CrossRef]
- Hochhegger, B.; Zanon, M.; Altmayer, S.; Mandelli, N.S.; Stüker, G.; Mohammed, T.L.; Verma, N.; Meirelles, G.S.P.; Marchiori, E. COVID-19 mimics on chest CT: A pictorial review and radiologic guide. Br. J. Radiol. 2021, 94, 20200703. [Google Scholar] [CrossRef] [PubMed]
- Al-Shudifat, A.E.; Al-Radaideh, A.; Hammad, S.; Hijjawi, N.; Abu-Baker, S.; Azab, M.; Tayyem, R. Association of lung CT findings in coronavirus disease 2019 (COVID-19) with patients’ age, body weight, vital signs, and medical regimen. Front. Med. 2022, 9, 912752. [Google Scholar] [CrossRef] [PubMed]
- Lanza, E.; Muglia, R.; Bolengo, I.; Santonocito, O.G.; Lisi, C.; Angelotti, G.; Morandini, P.; Savevski, V.; Politi, L.S.; Balzarini, L. Quantitative chest CT analysis in COVID-19 to predict the need for oxygenation support and intubation. Eur. Radiol. 2020, 30, 6770–6778. [Google Scholar] [CrossRef]
- Kumar, K.; Ratnakumar, R.; Collin, S.M.; Berrocal-Almanza, L.C.; Ricci, P.; Al-Zubaidy, M.; Coker, R.K.; Coleman, M.; Elkin, S.L.; Mallia, P.; et al. Chest CT features and functional correlates of COVID-19 at 3 months and 12 months follow-up. Clin. Med. 2023, 23, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Aziz, M.; Fatima, R.; Assaly, R.; Lee-Smith, W.; Nawras, Y.; Malik, R.; Hanrahan, J.; Assaly, E. Efficacy of tocilizumab in COVID-19: A systematic review and meta-analysis. J. Med. Virol. 2021, 93, 1620–1630. [Google Scholar] [CrossRef]
- Lombardi, C.M.; Carubelli, V.; Iorio, A.; Inciardi, R.M.; Bellasi, A.; Canale, C.; Camporotondo, R.; Catagnano, F.; Dalla Vecchia, L.A.; Giovinazzo, S.; et al. Association of Troponin Levels With Mortality in Italian Patients Hospitalized With Coronavirus Disease 2019: Results of a Multicenter Study. JAMA Cardiol. 2020, 5, 1274–1280. [Google Scholar] [CrossRef]
- Benhuri, B.; Aikawa, T.; Takagi, H.; Benhuri, D.; Kuno, T. Elevated natriuretic peptides in patients with severe or critical COVID-19: A meta-analysis. Tex. Heart Inst. J. 2022, 49, e207404. [Google Scholar] [CrossRef]
- Meslé, M.M.; Brown, K.E.; Mook, P.; Campbell, H.; WHO Working Group. Estimated number of lives saved and hospitalizations averted by COVID-19 vaccination in the WHO European Region between December 2020 and March 2023: A modelling study. Lancet Respir. Med. 2024, 12, 327–337. [Google Scholar] [CrossRef]
- Briciu, V.; Topan, A.; Calin, M.; Dobrota, R.; Leucuta, D.-C.; Lupse, M. Comparison of COVID-19 Severity in Vaccinated and Unvaccinated Patients during the Delta and Omicron Wave of the Pandemic in a Romanian Tertiary Infectious Diseases Hospital. Healthcare 2023, 11, 373. [Google Scholar] [CrossRef]
- Kompaniyets, L.; Goodman, A.B.; Belay, B.; Freedman, D.S.; Sucosky, M.S.; Lange, S.J.; Gundlapalli, A.V.; Boehmer, T.K.; Blanck, H.M. Body Mass Index and Risk for COVID-19-Related Hospitalization, Intensive Care Unit Admission, Invasive Mechanical Ventilation, and Death—United States, March–December 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 355–361. [Google Scholar] [CrossRef]
- Poly, T.N.; Islam, M.M.; Yang, H.C.; Lin, M.C.; Jian, W.-S.; Hsu, M.-H.; Jack Li, Y.-C. Obesity and mortality among patients diagnosed with COVID-19: A systematic review and meta-analysis. Front. Med. 2021, 8, 620044. [Google Scholar] [CrossRef]
- WHO; Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group; Shankar-Hari, M.; Vale, C.L.; Godolphin, P.J.; Fisher, D.; Higgins, J.P.T.; Spiga, F.; Savović, J.; Tierney, J.; et al. Association Between Administration of IL-6 Antagonists and Mortality Among Patients Hospitalized for COVID-19: A Meta-analysis. JAMA 2021, 326, 499–518. [Google Scholar] [CrossRef]
- Tleyjeh, I.M.; Kashour, Z.; Damlaj, M.; Riaz, M.; Tlayjeh, H.; Altannir, M.; Altannir, Y.; Al-Tannir, M.; Tleyjeh, R.; Hassett, L.; et al. Efficacy and safety of tocilizumab in COVID-19 patients: A living systematic review and meta-analysis. Clin. Microbiol. Infect. 2021, 27, 215–227. [Google Scholar] [CrossRef] [PubMed]
- Derde, L.P.G.; Gordon, A.C.; Mouncey, P.R.; Al-Beidh, F.; Rowan, K.M.; Nichol, A.D.; Arabi, Y.M.; Annane, D.; Beane, A.; Beasley, R.; et al. Effectiveness of tocilizumab, sarilumab, and anakinra in critically ill patients with COVID-19: A randomised, controlled, open-label, adaptive platform trial. Thorax 2025, 80, 267–275. [Google Scholar] [CrossRef]
- Li, Y.; Li, X.; Zheng, X. Effect of subcutaneous vs intravenous tocilizumab in patients with severe COVID-19: A systematic review. Eur. J. Clin. Pharmacol. 2024, 80, 1523–1530. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Value (n = 207) |
|---|---|
| Demographics | |
| Age (years), Median (IQR) | 69 (61–77) |
| Male Sex, n (%) | 112 (54.1%) |
| Vaccination Status | |
| Unvaccinated, n (%) | 176 (85.0%) |
| Vaccinated, n (%) | 31 (15.0%) |
| Clinical Characteristics | |
| Days to Admission, Mean (SD) | 4.2 (1.5) |
| Smoking, n (%) | 64 (30.9%) |
| Frequent Alcohol Consumption, n (%) | 78 (37.7%) |
| BMI, Median (IQR) | 28.5 (26–31) |
| Comorbidities | |
| CCI Score, Median (IQR) | 3 (2–4) |
| Hypertension, n (%) | 169 (81.6%) |
| Diabetes, n (%) | 72 (34.8%) |
| Coronary Artery Disease, n (%) | 42 (20.3%) |
| CT Severity Score | |
| <25% Lung Involvement, n (%) | 52 (25.1%) |
| 25–50% Lung Involvement, n (%) | 74 (35.7%) |
| >50% Lung Involvement, n (%) | 81 (39.1%) |
| Oxygenation and Severity | |
| Oxygen Saturation at Baseline, Mean (SD) | 90.1 (5.7) |
| Oxygen Flow >15 L/min, n (%) | 95 (45.9%) |
| SOFA Score, Median (IQR) | 6 (5–8) |
| Baseline Biomarkers, Median (IQR) | |
| IL-6 (pg/mL) | 30 (20–45) |
| Troponin (ng/L) | 95 (65–130) |
| NT-proBNP (pg/mL) | 550 (400–750) |
| CRP (mg/L) | 110 (80–140) |
| PCT (ng/mL) | 2.0 (1.5–3.0) |
| D-dimers (µg/mL) | 1.0 (0.6–1.5) |
| EKG Changes | |
| EKG Changes, n (%) | 55 (26.6%) |
| Treatment, n (%) | |
| Remdesivir | 189 (91.3%) |
| Antibiotics | 177 (85.5%) |
| Corticosteroids | 204 (98.6%) |
| Tocilizumab | 12 (5.8%) |
| Length of Stay | |
| Length of Stay (days), Mean (SD) | 14.3 (8.0) |
| Outcomes, n (%) | |
| ICU Admission | 42 (20.3%) |
| Mechanical Ventilation | 38 (18.4%) |
| Death | 28 (13.5%) |
| Characteristic | Favorable (n = 155) | Unfavorable (n = 52) | p-Value |
|---|---|---|---|
| Demographics | |||
| Age (years), Mean (SD); Median (IQR) | 66.3 (10.4); 66 (59–74) | 76.2 (9.8); 76 (69–83) | 0.0001 |
| Male Sex, n (%) | 83 (53.5%) | 29 (55.8%) | 0.763 |
| BMI, Mean (SD);Median (IQR) | 27.3 (3.4); 27 (25–30) | 30.5 (3.3); 30 (28–33) | 0.0003 |
| Vaccination Status, n (%) | 0.001 | ||
| Vaccinated | 31 (20.0%) | 0 (0.0%) | |
| Unvaccinated | 124 (80.0%) | 52 (100.0%) | |
| Comorbidities | |||
| CCI, Mean (SD); Median (IQR) | 2.8 (1.2); 3 (2–4) | 3.8 (1.3); 4 (3–5) | 0.0002 |
| CT Severity, n (%) | |||
| <25% | 44 (28.4%) | 8 (15.4%) | |
| 25–50% | 58 (37.4%) | 16 (30.8%) | |
| >50% | 53 (34.2%) | 28 (53.8%) | |
| Oxygenation and Severity | |||
| Oxygen Saturation, Mean (SD) | 90.2 (5.9) | 87.3 (8.1) | 0.194 |
| Oxygen Flow >15 L/min, n (%) | 98 (63.2%) | 43 (82.7%) | 0.072 |
| SOFA Score, Mean (SD); Median (IQR) | 5.8 (2.1); 6 (4–7) | 7.8 (2.5); 8 (6–10) | 0.025 |
| Baseline Biomarkers, Mean (SD), Median (IQR) | |||
| IL-6 (pg/mL) | 27.3(12.8);25(18–35) | 48.7 (19.4); 45 (35–60) | 0.012 |
| Troponin (ng/L) | 78.9(34.6);75(55–100) | 145.2(56.3);140(110–180) | 0.008 |
| NT-proBNP (pg/mL) | 489.3(189.7);480(350–600) | 789.4 (298.2); 750 (600–950) | 0.015 |
| CRP (mg/L) | 111.8(45.2);110(80–140) | 111.8 (45.2); 110 (80–140) | 0.950 |
| PCT (ng/mL) | 2.1 (1.1); 2.0 (1.4–2.8) | 2.7 (1.4); 2.5 (1.8–3.5) | 0.089 |
| D-dimers (µg/mL) | 1.1 (0.8); 1.0 (0.6–1.4) | 1.1 (0.8); 1.0 (0.6–1.5) | 0.920 |
| EKG Changes | |||
| EKG Changes, n (%) | 41 (26.5%) | 14 (26.9%) | 0.950 |
| Variable | OR | 95% CI | p-Value |
|---|---|---|---|
| CCI | 1.550 | 0.980–2.452 | 0.060 |
| IL-6 | 1.016 | 1.004–1.028 | 0.013 |
| Troponin | 1.013 | 1.003–1.023 | 0.017 |
| NT-proBNP | 1.009 | 1.000–1.018 | 0.049 |
| CRP | 1.002 | 0.992–1.012 | 0.910 |
| D-dimers | 1.015 | 0.910–1.132 | 0.930 |
| Lung Involvement (>50%) | 1.835 | 1.150–2.927 | 0.011 |
| Vaccination Status (Unvaccinated vs. Vaccinated) | 2.312 | 1.342–3.986 | 0.002 |
| BMI | 1.112 | 1.032–1.198 | 0.005 |
| Variable | β | 95% CI | p-Value |
|---|---|---|---|
| IL-6 (per pg/mL) | 0.120 | 0.078–0.162 | <0.001 |
| Troponin (per ng/L) | 0.080 | 0.065–0.095 | <0.001 |
| D-dimers (per µg/mL) | 0.150 | −0.650–0.950 | 0.850 |
| Lung Involvement (>50% vs. ≤50%) | 2.650 | 1.290–4.010 | <0.001 |
| Age (per year) | 0.045 | −0.015–0.105 | 0.140 |
| CCI | 0.430 | 0.110–0.750 | 0.010 |
| Vaccination Status (Unvaccinated vs. Vaccinated) | −2.500 | −4.082–−0.918 | 0.002 |
| BMI(per kg/m2) | 0.300 | 0.100–0.500 | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mateescu, D.-M.; Ilie, A.-C.; Cotet, I.; Muresan, C.-O.; Pah, A.-M.; Badalica-Petrescu, M.; Iurciuc, S.; Craciun, M.-L.; Cote, A.; Enache, A. Predicting COVID-19 Sepsis Outcomes: Roles of IL-6, Cardiac Biomarkers, Clinical Factors, and Vaccination Status and Exploratory Analysis of Tocilizumab Therapy in an Eastern European Cohort. Viruses 2025, 17, 1168. https://doi.org/10.3390/v17091168
Mateescu D-M, Ilie A-C, Cotet I, Muresan C-O, Pah A-M, Badalica-Petrescu M, Iurciuc S, Craciun M-L, Cote A, Enache A. Predicting COVID-19 Sepsis Outcomes: Roles of IL-6, Cardiac Biomarkers, Clinical Factors, and Vaccination Status and Exploratory Analysis of Tocilizumab Therapy in an Eastern European Cohort. Viruses. 2025; 17(9):1168. https://doi.org/10.3390/v17091168
Chicago/Turabian StyleMateescu, Diana-Maria, Adrian-Cosmin Ilie, Ioana Cotet, Camelia-Oana Muresan, Ana-Maria Pah, Marius Badalica-Petrescu, Stela Iurciuc, Maria-Laura Craciun, Adrian Cote, and Alexandra Enache. 2025. "Predicting COVID-19 Sepsis Outcomes: Roles of IL-6, Cardiac Biomarkers, Clinical Factors, and Vaccination Status and Exploratory Analysis of Tocilizumab Therapy in an Eastern European Cohort" Viruses 17, no. 9: 1168. https://doi.org/10.3390/v17091168
APA StyleMateescu, D.-M., Ilie, A.-C., Cotet, I., Muresan, C.-O., Pah, A.-M., Badalica-Petrescu, M., Iurciuc, S., Craciun, M.-L., Cote, A., & Enache, A. (2025). Predicting COVID-19 Sepsis Outcomes: Roles of IL-6, Cardiac Biomarkers, Clinical Factors, and Vaccination Status and Exploratory Analysis of Tocilizumab Therapy in an Eastern European Cohort. Viruses, 17(9), 1168. https://doi.org/10.3390/v17091168






