V4020 Venezuelan Equine Encephalitis Vaccine: Mitigating Neuroinvasion and Reversion Through Rational Design
Abstract
1. Introduction
2. Materials and Methods
2.1. Vaccine Viruses
2.2. Neuroinvasion Animal Model
2.3. In-Life Monitoring
2.4. Blood Cell Count
2.5. Brain Tissue Harvest, Fixation, and Histopathology
2.6. Tissue Homogenization
2.7. Detection of Virus by Plaque Assay
2.8. Detection of Virus by RNA/Scope Assay
2.9. Viral Genome Sequence Analysis
2.10. Statistical Analysis
3. Results
3.1. Study Design
3.2. V4020 Showed Lower Degree Adverse Effects than Tc-83
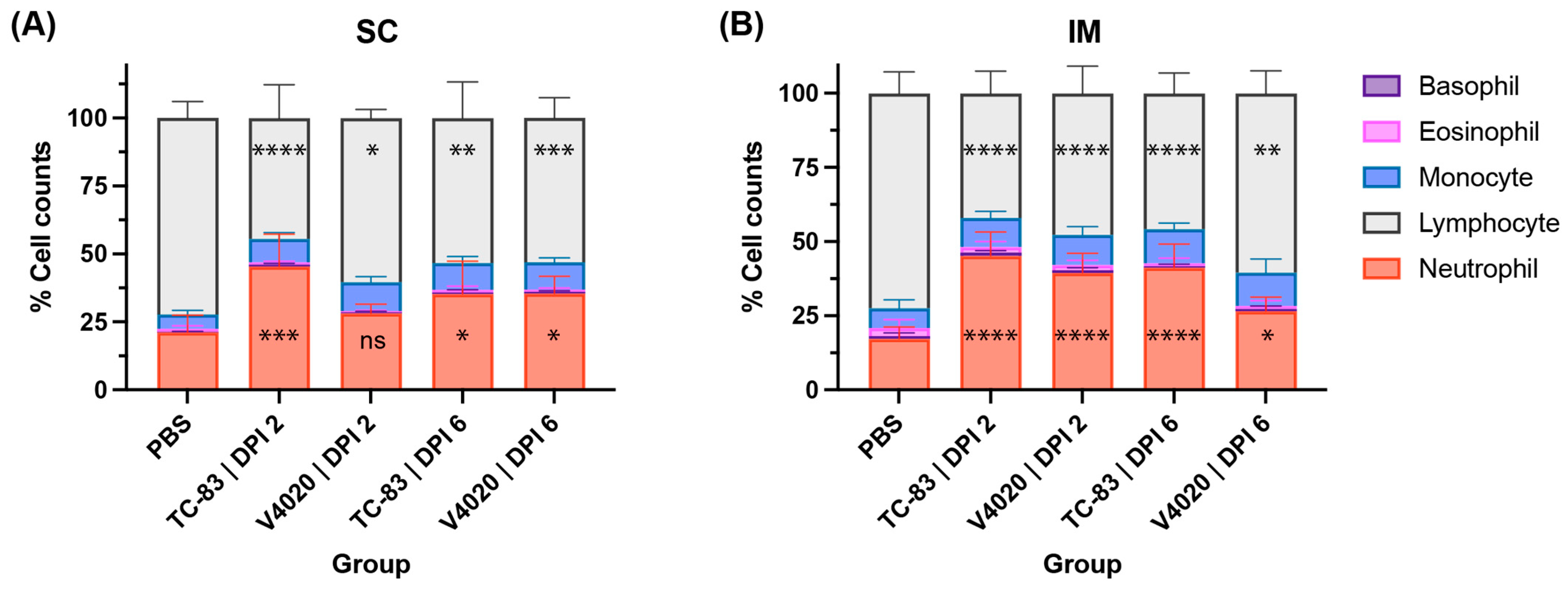
3.3. V4020 and TC-83 Induced a Low Degree of Changes in the Blood Cell Composition After Administration
3.4. Detection of Neuroinvasion in TC-83 Infected Mice
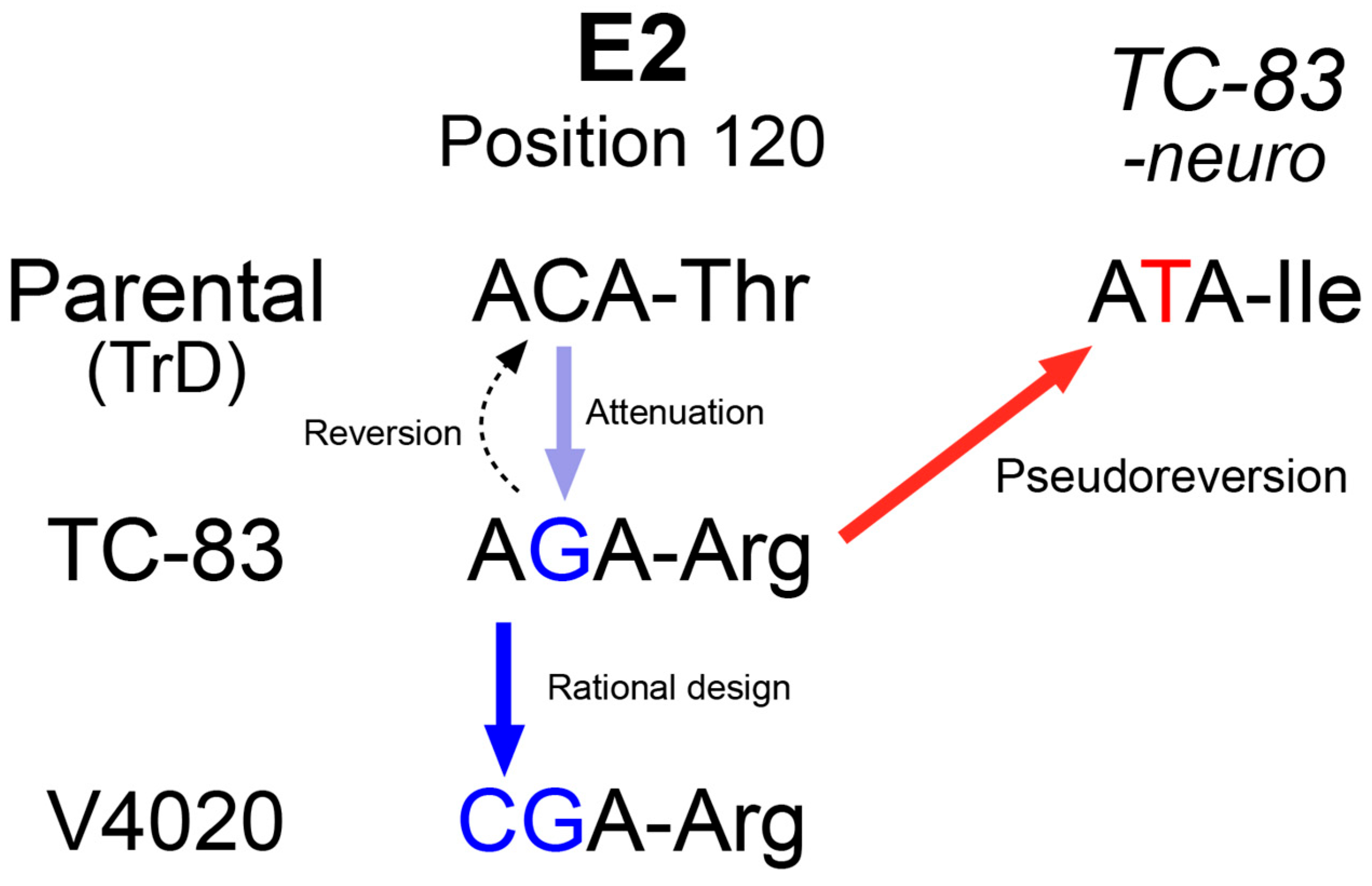
3.5. Pseudoreversion of the Neuroinvasive Tc-83 Population
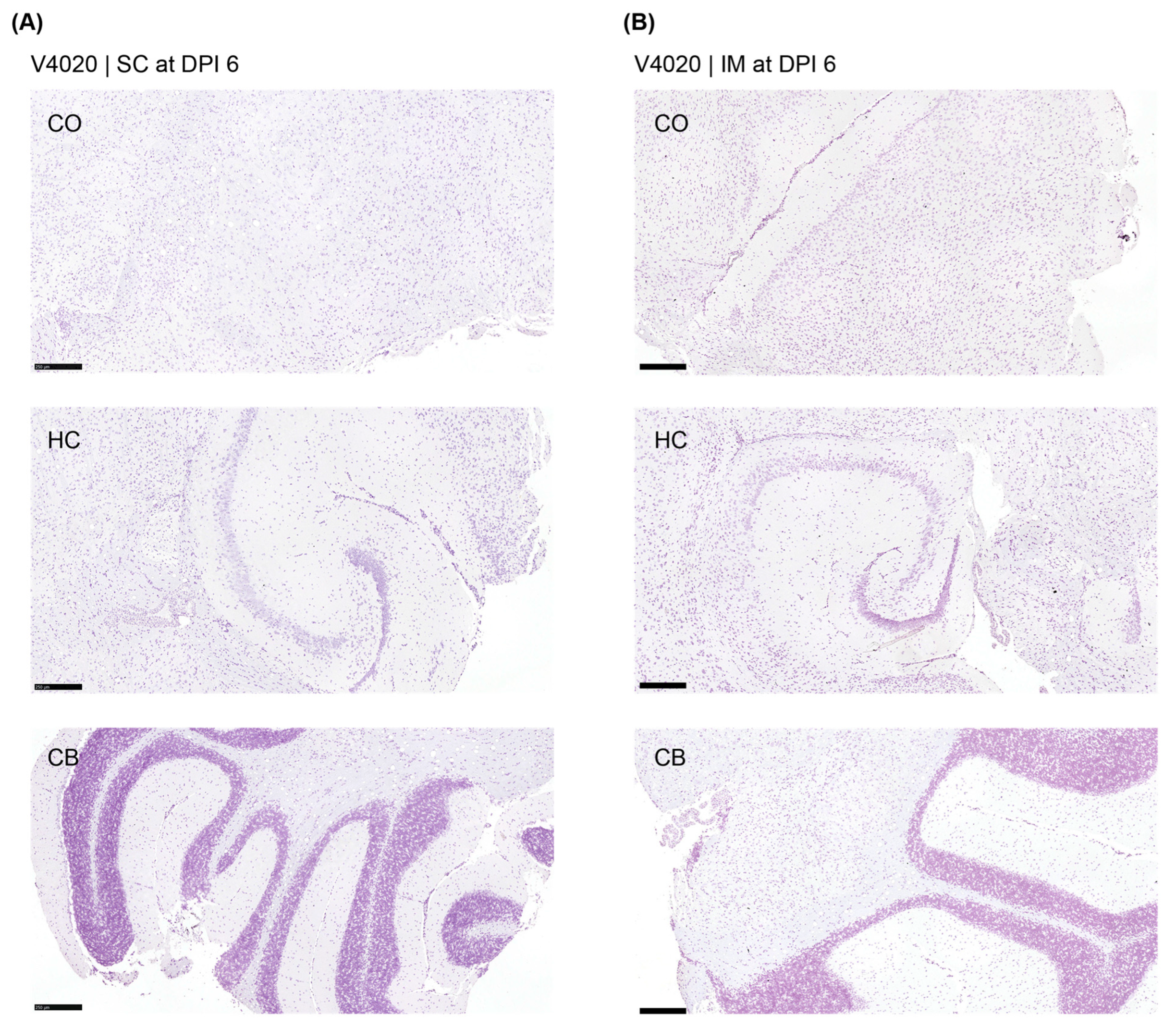
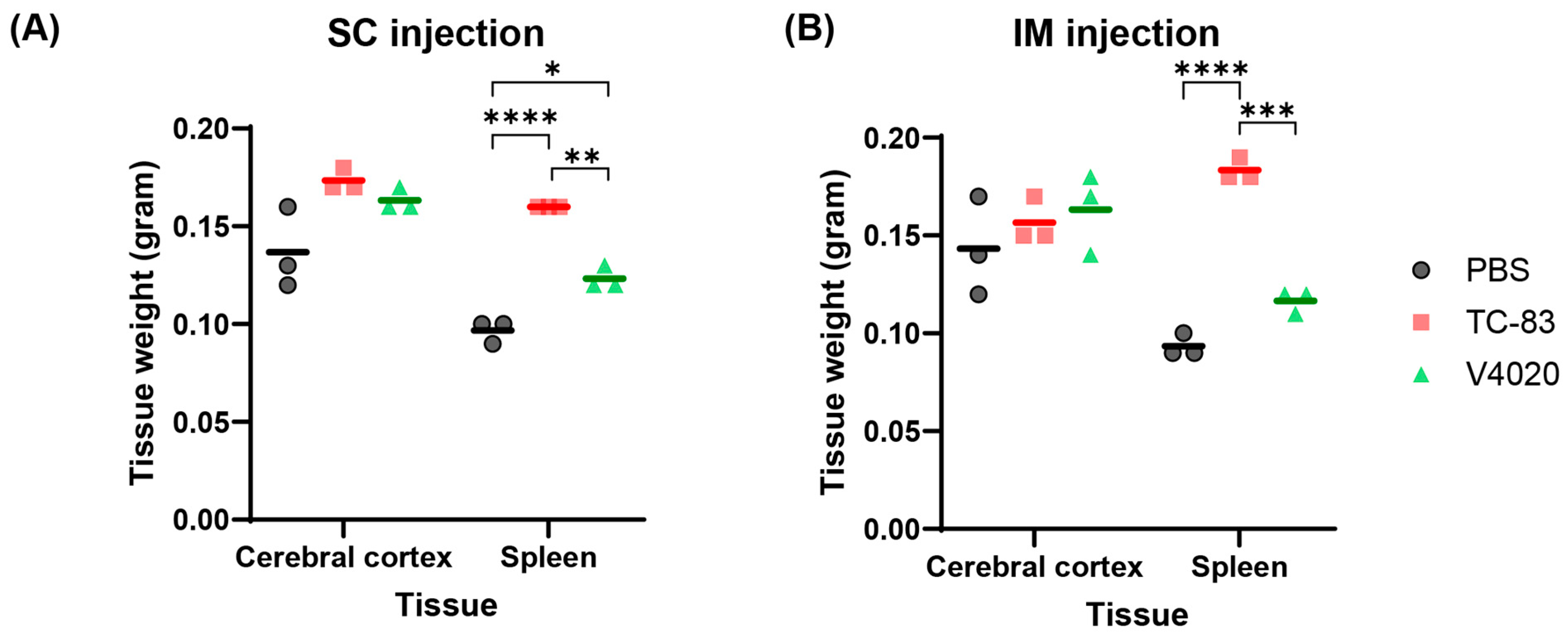
3.6. TC-83 and V4020 Did Not Induce Pathological Changes in the Brains and Other Organs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| VEEV | Venezuelan equine encephalitis virus |
| CNS | central nervous system |
| IM | intramuscular |
| SC | subcutaneous |
| IN | intranasal |
References
- Paessler, S.; Weaver, S.C. Vaccines for Venezuelan equine encephalitis. Vaccine 2009, 27 (Suppl. S4), D80–D85. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zacks, M.A.; Paessler, S. Encephalitic alphaviruses. Vet. Microbiol. 2010, 140, 281–286. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aguilar, P.V.; Estrada-Franco, J.G.; Navarro-Lopez, R.; Ferro, C.; Haddow, A.D.; Weaver, S.C. Endemic Venezuelan equine encephalitis in the Americas: Hidden under the dengue umbrella. Future Virol. 2011, 6, 721–740. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Samy, A.M.; Elaagip, A.H.; Kenawy, M.A.; Ayres, C.F.; Peterson, A.T.; Soliman, D.E. Climate Change Influences on the Global Potential Distribution of the Mosquito Culex quinquefasciatus, Vector of West Nile Virus and Lymphatic Filariasis. PLoS ONE 2016, 11, e0163863. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dietz, W.H.; Jr Peralta, P.H.; Johnson, K.M. Ten clinical cases of human infection with venezuelan equine encephalomyelitis virus, subtype I-D. Am. J. Trop. Med. Hyg. 1979, 28, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Rusnak, J.M.; Dupuy, L.C.; Niemuth, N.A.; Glenn, A.M.; Ward, L.A. Comparison of Aerosol- and Percutaneous-acquired Venezuelan Equine Encephalitis in Humans and Nonhuman Primates for Suitability in Predicting Clinical Efficacy under the Animal Rule. Comp. Med. 2018, 68, 380–395. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sulkin, S.E. Laboratory-acquired infections. Bacteriol. Rev. 1961, 25, 203–209. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pittman, P.R.; Makuch, R.S.; Mangiafico, J.A.; Cannon, T.L.; Gibbs, P.H.; Peters, C.J. Long-term duration of detectable neutralizing antibodies after administration of live-attenuated VEE vaccine and following booster vaccination with inactivated VEE vaccine. Vaccine 1996, 14, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.S.; Bakken, R.R.; Lind, C.M.; Garcia, P.; Jenkins, E.; Glass, P.J.; Parker, M.D.; Hart, M.K.; Fine, D.L. Evaluation of formalin inactivated V3526 virus with adjuvant as a next generation vaccine candidate for Venezuelan equine encephalitis virus. Vaccine 2010, 28, 3143–3151. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tretyakova, I.; Lukashevich, I.S.; Glass, P.; Wang, E.; Weaver, S.; Pushko, P. Novel vaccine against Venezuelan equine encephalitis combines advantages of DNA immunization and a live attenuated vaccine. Vaccine 2013, 31, 1019–1025. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Edelman, R.; Ascher, M.S.; Oster, C.N.; Ramsburg, H.H.; Cole, F.E.; Eddy, G.A. Evaluation in humans of a new, inactivated vaccine for Venezuelan equine encephalitis virus (C-84). J. Infect. Dis. 1979, 140, 708–715. [Google Scholar] [CrossRef] [PubMed]
- Grieder, F.B.; Davis, N.L.; Aronson, J.F.; Charles, P.C.; Sellon, D.C.; Suzuki, K.; Johnston, R.E. Specific restrictions in the progression of Venezuelan equine encephalitis virus-induced disease resulting from single amino acid changes in the glycoproteins. Virology 1995, 206, 994–1006. [Google Scholar] [CrossRef] [PubMed]
- Alejandro, B.; Kim, E.J.; Hwang, J.Y.; Park, J.W.; Smith, M.; Chung, D. Genetic and phenotypic changes to Venezuelan equine encephalitis virus following treatment with beta-D-N4-hydroxycytidine, an RNA mutagen. Sci. Rep. 2024, 14, 25265. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tretyakova, I.; Plante, K.S.; Rossi, S.L.; Lawrence, W.S.; Peel, J.E.; Gudjohnsen, S.; Wang, E.; Mirchandani, D.; Tibbens, A.; Lamichhane, T.N.; et al. Venezuelan equine encephalitis vaccine with rearranged genome resists reversion and protects non-human primates from viremia after aerosol challenge. Vaccine 2020, 38, 3378–3386. [Google Scholar] [CrossRef] [PubMed]
- Tretyakova, I.; Tibbens, A.; Jokinen, J.D.; Johnson, D.M.; Lukashevich, I.S.; Pushko, P. Novel DNA-launched Venezuelan equine encephalitis virus vaccine with rearranged genome. Vaccine 2019, 37, 3317–3325. [Google Scholar] [CrossRef] [PubMed]
- Tretyakova, I.; Tomai, M.; Vasilakos, J.; Pushko, P. Live-Attenuated VEEV Vaccine Delivered by iDNA Using Microneedles Is Immunogenic in Rabbits. Front Trop Dis. 2022, 3, 813671. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pushko, P.; Lukashevich, I.S.; Johnson, D.M.; Tretyakova, I. Single-Dose Immunogenic DNA Vaccines Coding for Live-Attenuated Alpha- and Flaviviruses. Viruses 2024, 16, 428. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pushko, P.; Lukashevich, I.S.; Weaver, S.C.; Tretyakova, I. DNA-launched live-attenuated vaccines for biodefense applications. Expert. Rev. Vaccines 2016, 15, 1223–1234. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Julander, J.G.; Bowen, R.A.; Rao, J.R.; Day, C.; Shafer, K.; Smee, D.F.; Morrey, J.D.; Chu, C.K. Treatment of Venezuelan equine encephalitis virus infection with (-)-carbodine. Antivir. Res. 2008, 80, 309–315. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, H. Minimap2: Pairwise alignment for nucleotide sequences. Bioinformatics 2018, 34, 3094–3100. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, H.; Handsaker, B.; Wysoker, A.; Fennell, T.; Ruan, J.; Homer, N.; Marth, G.; Abecasis, G.; Durbin, R.; 1000 Genome Project Data Processing Subgroup. The Sequence Alignment/Map format and SAMtools. Bioinformatics 2009, 25, 2078–2079. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Charles, P.C.; Walters, E.; Margolis, F.; Johnston, R.E. Mechanism of neuroinvasion of Venezuelan equine encephalitis virus in the mouse. Virology 1995, 208, 662–671. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.M.; Sokoloski, K.J.; Jokinen, J.D.; Pfeffer, T.L.; Chu, Y.K.; Adcock, R.S.; Chung, D.; Tretyakova, I.; Pushko, P.; Lukashevich, L.S. Advanced Safety and Genetic Stability in Mice of a Novel DNA-Launched Venezuelan Equine Encephalitis Virus Vaccine with Rearranged Structural Genes. Vaccines 2020, 8, 114. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cao, X.; Yang, D.; Parvathareddy, J.; Chu, Y.K.; Kim, E.J.; Fitz-Henley, J.N.; Li, X.; Lukka, P.B.; Parmar, K.R.; Temrikar, Z.H.; et al. Efficacy of a brain-penetrant antiviral in lethal Venezuelan and eastern equine encephalitis mouse models. Sci. Transl. Med. 2023, 15, eabl9344. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kinney, R.M.; Chang, G.J.; Tsuchiya, K.R.; Sneider, J.M.; Roehrig, J.T.; Woodward, T.M.; Trent, D.W. Attenuation of Venezuelan equine encephalitis virus strain TC-83 is encoded by the 5’-noncoding region and the E2 envelope glycoprotein. J. Virol. 1993, 67, 1269–1277. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Klimstra, W.B.; Ryman, K.D.; Johnston, R.E. Adaptation of Sindbis virus to BHK cells selects for use of heparan sulfate as an attachment receptor. J. Virol. 1998, 72, 7357–7366. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Byrnes, A.P.; Griffin, D.E. Large-plaque mutants of Sindbis virus show reduced binding to heparan sulfate, heightened viremia, and slower clearance from the circulation. J. Virol. 2000, 74, 644–651. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, R.; Hryc, C.F.; Cong, Y.; Liu, X.; Jakana, J.; Gorchakov, R.; Baker, M.L.; Weaver, S.C.; Chiu, W. 4.4 A cryo-EM structure of an enveloped alphavirus Venezuelan equine encephalitis virus. EMBO J. 2011, 30, 3854–3863. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jennings, A.D.; Gibson, C.A.; Miller, B.R.; Mathews, J.H.; Mitchell, C.J.; Roehrig, J.T.; Wood, D.J.; Taffs, F.; Sil, B.K.; Whitby, S.N.; et al. Analysis of a yellow fever virus isolated from a fatal case of vaccine-associated human encephalitis. J. Infect. Dis. 1994, 169, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Bakoa, F.; Prehaud, C.; Beauclair, G.; Chazal, M.; Mantel, N.; Lafon, M.; Jouvenet, N. Genomic diversity contributes to the neuroinvasiveness of the Yellow fever French neurotropic vaccine. NPJ Vaccines 2021, 6, 64. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hidajat, R.; Nickols, B.; Forrester, N.; Tretyakova, I.; Weaver, S.; Pushko, P. Next generation sequencing of DNA-launched Chikungunya vaccine virus. Virology 2016, 490, 83–90. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hallengard, D.; Kakoulidou, M.; Lulla, A.; Kummerer, B.M.; Johansson, D.X.; Mutso, M.; Lulla, V.; Fazakerley, J.K.; Roques, P.; Le Grand, R.; et al. Novel attenuated Chikungunya vaccine candidates elicit protective immunity in C57BL/6 mice. J. Virol. 2014, 88, 2858–2866. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]


| Goal/Purpose | Mouse Strain | Inoculum | Infection Route | Sacrifice Day (DPI) | No. of Animals | |
|---|---|---|---|---|---|---|
| Group 1 | Negative control | Balb/C | PBS | IM | 5 | 5 males and 5 females |
| Group 2 | IM route, comparator | Balb/C | TC-83, 2 × 106 PFU/ms | IM | 2 | 5 males and 5 females |
| 6 | 5 males and 5 females | |||||
| Group 3 | IM route, test article | Balb/C | V4020, 2 × 106 PFU/ms | IM | 2 | 5 males and 5 females |
| 6 | 5 males and 5 females | |||||
| Group 4 | SC route, comparator | Balb/C | TC-83, 2 × 106 PFU/ms | SC | 2 | 5 males and 5 females |
| 6 | 5 males and 5 females | |||||
| Group 5 | SC route, test article | Balb/C | V4020, 2 × 106 PFU/ms | SC | 2 | 5 males and 5 females |
| 6 | 5 males and 5 females |
| Inoculum | Animal ID | Sex | DPI 6 | |||
|---|---|---|---|---|---|---|
| OB | CO | CB | SP | |||
| TC-83 | 1 | Female | N.D. | 2.3 × 106 | 1.6 × 103 | N.D. |
| 2 | Female | N.D. | 2.2 × 103 | N.D. | N.D. | |
| 3 | Female | N.D. | N.D. | N.D. | N.D. | |
| 4 | Male | N.D. | N.D. | N.D. | N.D. | |
| 5 | Male | N.D. | N.D. | N.D. | 7.5 × 102 | |
| 6 | Male | N.D. | N.D. | N.D. | N.D. | |
| V4020 | 1 | Female | N.D. | N.D. | N.D. | N.D. |
| 2 | Female | N.D. | N.D. | N.D. | N.D. | |
| 3 | Female | N.D. | N.D. | N.D. | N.D. | |
| 4 | Male | N.D. | N.D. | N.D. | N.D. | |
| 5 | Male | N.D. | N.D. | N.D. | N.D. | |
| 6 | Male | N.D. | N.D. | N.D. | N.D. | |
| Inoculum | Animal ID | Sex | DPI 6 | |||
|---|---|---|---|---|---|---|
| OB | CO | CB | SP | |||
| TC-83 | 1 | Female | N.D. | N.D. | N.D. | N.D. |
| 2 | Female | N.D. | N.D. | N.D. | N.D. | |
| 3 | Female | N.D. | N.D. | N.D. | 9.0 × 102 | |
| 4 | Male | N.D. | N.D. | N.D. | N.D. | |
| 5 | Male | N.D. | N.D. | N.D. | 1.5 × 103 | |
| 6 | Male | N.D. | N.D. | N.D. | N.D. | |
| V4020 | 1 | Female | N.D. | N.D. | N.D. | N.D. |
| 2 | Female | N.D. | N.D. | N.D. | N.D. | |
| 3 | Female | N.D. | N.D. | N.D. | N.D. | |
| 4 | Male | N.D. | N.D. | N.D. | N.D. | |
| 5 | Male | N.D. | N.D. | N.D. | N.D. | |
| 6 | Male | N.D. | N.D. | N.D. | N.D. | |
| Gene/a.a, Position | TrD Reference | TC-83 Inoculum | V4020 Inoculum | Isolate 1 */Animal 1 CB | Isolate 2 */Animal 1 CO | Isolate 3 */Animal 2 CO |
|---|---|---|---|---|---|---|
| E2/120 | ACA/Thr | AGA/Arg | CGA/Arg | ATA/Ile | ATA/Ile | ATA/Ile |
| E1/80 | GTC/Val | GTC/Val | GTC/Val | GCC/Ala | GCC/Ala | GCC/Ala |
| Injection route | Inoculum | DPI | Pathological Findings |
|---|---|---|---|
| IN | PBS | 5 | No microscopic lesions in the brains (n = 10). |
| TC-83 | 6 | Minimal to moderate lesions in the meninges and cerebrum in all brains (n = 10). | |
| SC | PBS | 6 | No microscopic lesions in the brain (n = 6). |
| TC-83 | 2 | No microscopic lesions in the brain (n = 6). | |
| 6 | No microscopic lesions in the brain (n = 6). | ||
| V4020 | 2 | No microscopic lesions in the brain (n = 6). | |
| 6 | No microscopic lesions in the brain (n = 6). | ||
| IM | PBS | 5 | No microscopic lesions in the brain (n = 6). |
| TC-83 | 2 | No microscopic lesions in the brain (n = 6). | |
| 6 | No microscopic lesions in the brain (n = 6). | ||
| V4020 | 2 | No microscopic lesions in the brain (n = 6). | |
| 6 | No microscopic lesions in the brain (n = 6). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Centers, A.; Barnaby, K.; Goedeker, S.; Pignataro, A.; Tretyakova, I.; Lukashevich, I.; Pushko, P.; Chung, D. V4020 Venezuelan Equine Encephalitis Vaccine: Mitigating Neuroinvasion and Reversion Through Rational Design. Viruses 2025, 17, 1136. https://doi.org/10.3390/v17081136
Centers A, Barnaby K, Goedeker S, Pignataro A, Tretyakova I, Lukashevich I, Pushko P, Chung D. V4020 Venezuelan Equine Encephalitis Vaccine: Mitigating Neuroinvasion and Reversion Through Rational Design. Viruses. 2025; 17(8):1136. https://doi.org/10.3390/v17081136
Chicago/Turabian StyleCenters, Adrian, Koji Barnaby, Sidney Goedeker, Ava Pignataro, Irina Tretyakova, Igor Lukashevich, Peter Pushko, and Donghoon Chung. 2025. "V4020 Venezuelan Equine Encephalitis Vaccine: Mitigating Neuroinvasion and Reversion Through Rational Design" Viruses 17, no. 8: 1136. https://doi.org/10.3390/v17081136
APA StyleCenters, A., Barnaby, K., Goedeker, S., Pignataro, A., Tretyakova, I., Lukashevich, I., Pushko, P., & Chung, D. (2025). V4020 Venezuelan Equine Encephalitis Vaccine: Mitigating Neuroinvasion and Reversion Through Rational Design. Viruses, 17(8), 1136. https://doi.org/10.3390/v17081136






