Chimeric Vesicular Stomatitis Virus Bearing Western Equine Encephalitis Virus Envelope Proteins E2-E1 Is a Suitable Surrogate for Western Equine Encephalitis Virus in a Plaque Reduction Neutralization Test
Abstract
1. Introduction
2. Materials and Methods
2.1. Cells, Wildtype Viruses, and Immune Sera
2.2. Generation and Recovery of VSV Chimeras
2.3. Virus Stocks
2.4. Virus Purification
2.5. Immunoblotting
2.6. Morphological Plaque Assessment
2.7. Viral Kinetics
2.8. Plaque Reduction Neutralization Test (PRNT)
2.9. Neutralization Curves
2.10. Reporter Stability Assessment
3. Results
3.1. Generation and Characterization of Chimeric VSV/WEEV
3.2. Viral Growth Kinetics of Chimeric VSV/WEEV Are Intermediate Between VSV/VSV and WEEV
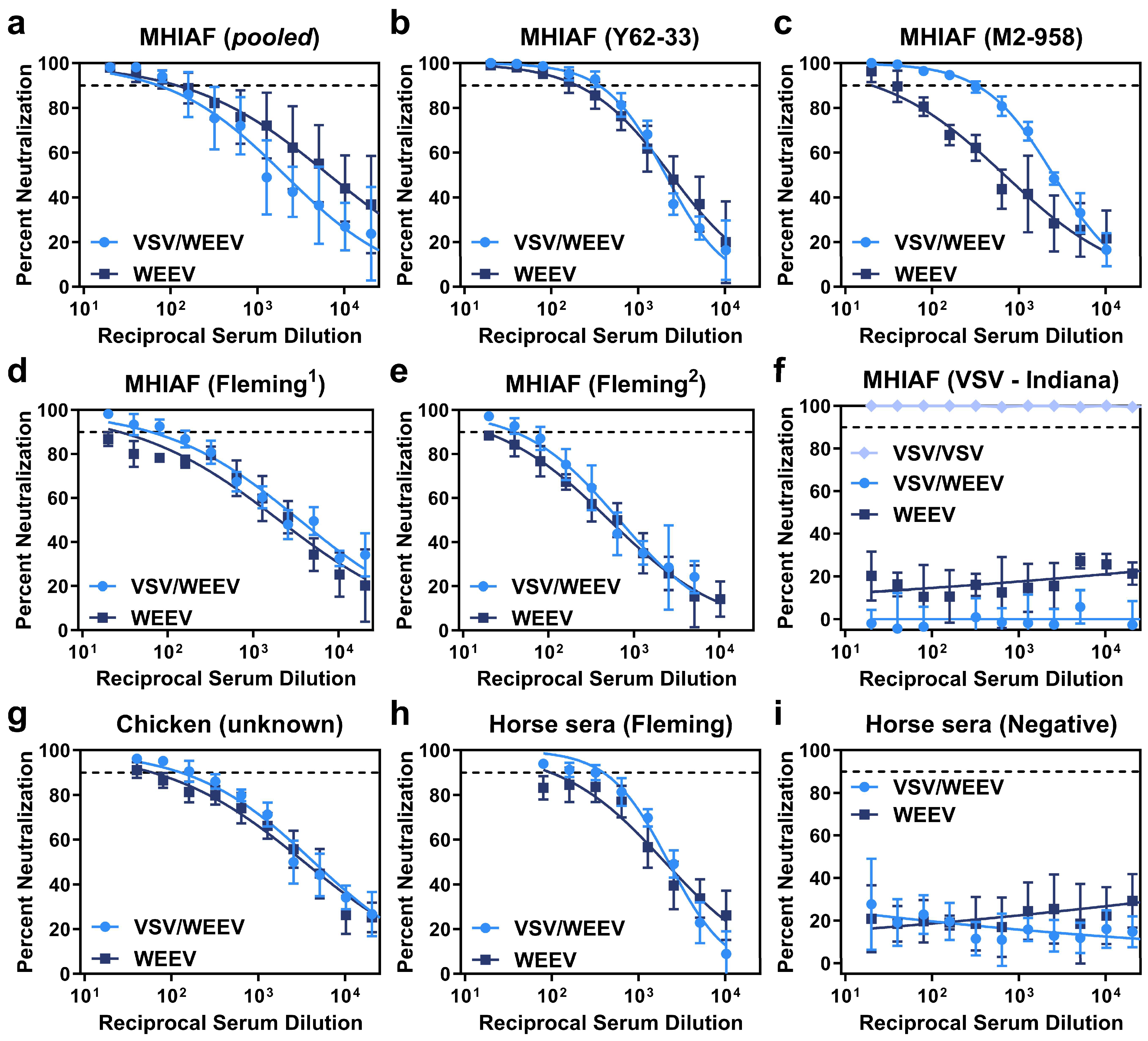
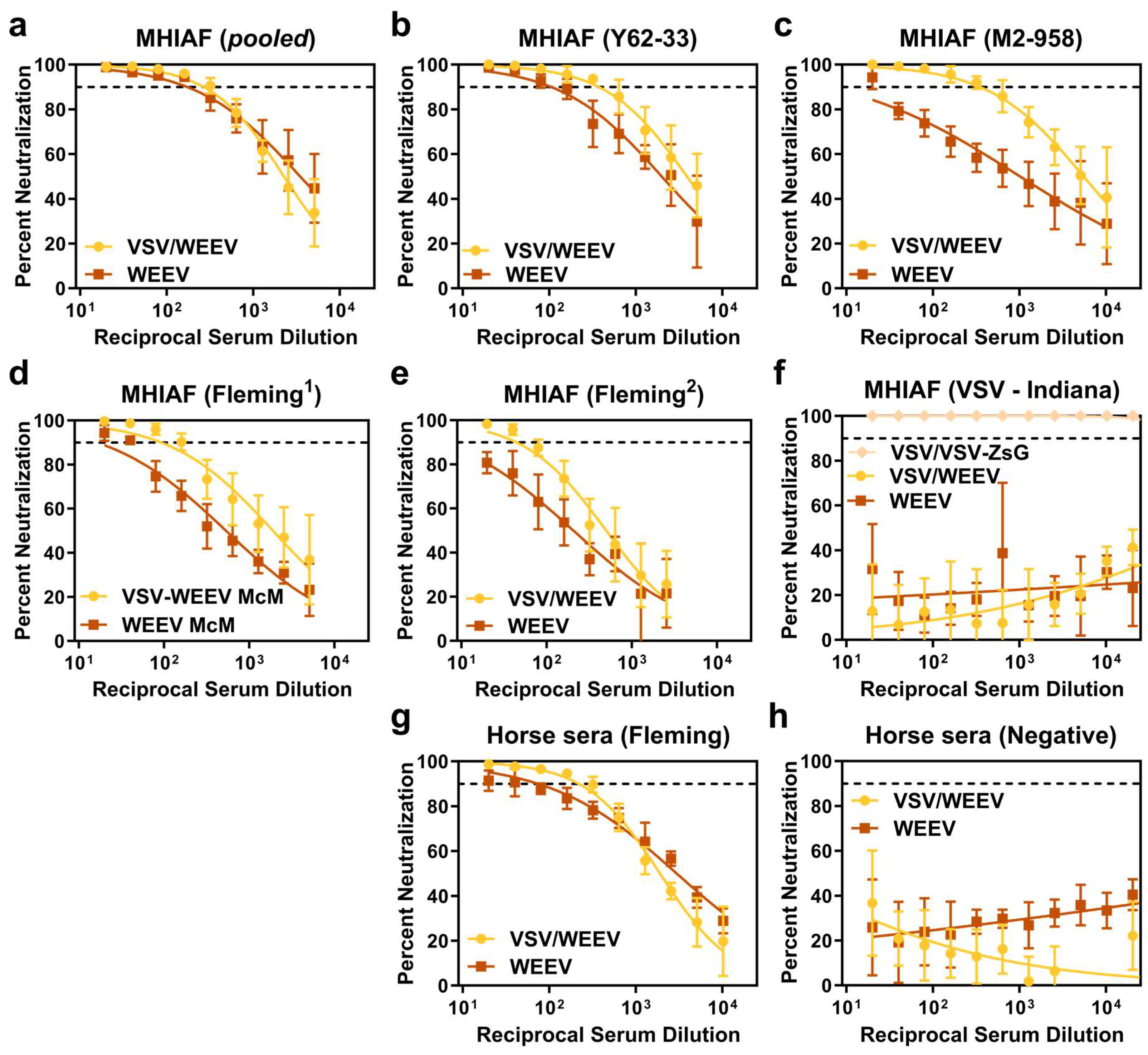
3.3. Chimeric VSV/WEEV Performs Equivalently to Authentic WEEV in Neutralization Assays
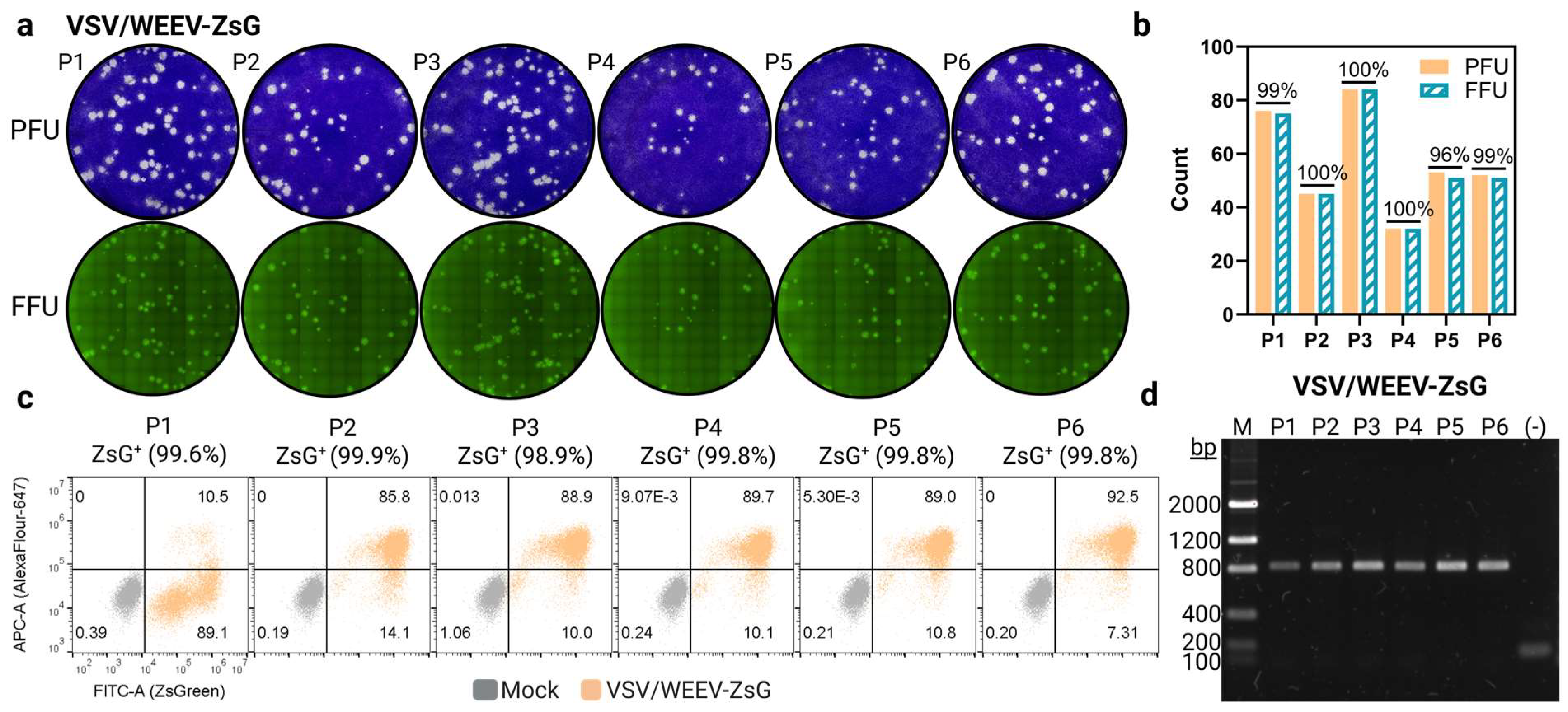
3.4. Reporter Gene, ZsGreen, Remains Stable with Repeated Chimeric rVSV Passaging in Tissue Culture
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclosure
Abbreviations
| WEE | Western equine encephalitis |
| WEEV | Western equine encephalitis virus |
| VSV | Vesicular stomatitis virus |
| WHO | World Health Organization |
| PAHO | Pan American Health Organization |
| PRNT | Plaque reduction neutralization test |
| MHIAF | Mouse hyperimmune ascites fluid |
| CDPH | California department of public health |
| CDC | Centers for disease control and prevention |
| DVBD | Division of vector-borne disease |
| ADB | Arboviral disease branch |
| DRT | Diagnostics and reference team |
| ZsG | ZsGreen |
Appendix A
| Application | Origin | Clonality | Specificity | Source | Catalog (Lot) |
|---|---|---|---|---|---|
| PRNT | Mouse | Polyclonal | WEEV (pooled) | DRT | (M29802) |
| PRNT | Mouse | Polyclonal | WEEV (Y62-33) | DRT | (M15559) |
| PRNT | Mouse | Polyclonal | WEEV (M2-958) | DRT | (M13583) |
| PRNT | Mouse | Polyclonal | WEEV (Flemming1) | DRT | VS0126 (88-0017) |
| PRNT | Mouse | Polyclonal | WEEV (Flemming2) | DRT | (M29686) |
| PRNT | Mouse | Polyclonal | VSV (Indiana) | DRT | PR76288 (1) |
| PRNT | Chicken | Polyclonal | WEEV (unknown) | CDPH | Not applicable |
| PRNT | Horse | Polyclonal | WEEV (Flemming) | DRT | (M29685) |
| PRNT | Horse | Polyclonal | Normal control | DRT | (M29687) |
| FACs/WB | Mouse | Monoclonal | VSV M (Indiana) | Douglas Lyles | [clone 23H12] |
| FACs | Goat | Monoclonal | AlexaFlour647-αM IgG | Invitrogen | A21236 (2552956) |
| WB | Mouse | Monoclonal | VSV G (Indiana) | Douglas Lyles | [clone 8G5F11] |
| WB | Goat | Monoclonal | HRP-αM IgG | Jackson Immuno | 115-035-003 |
References
- Frabasile, S.; Morel, N.; Pérez, R.; Marrero, L.M.; Burgueño, A.; Cortinas, M.N.; Bassetti, L.; Negro, R.; Rodríguez, S.; Bórmida, V.; et al. Equine Encephalomyelitis Outbreak, Uruguay, 2023-2024. Emerg. Infect. Dis. 2025, 31, 180–183. [Google Scholar] [CrossRef]
- Campos, A.S.; Franco, A.C.; Godinho, F.M.; Huff, R.; Candido, D.S.; da Cruz Cardoso, J.; Hua, X.; Claro, I.M.; Morais, P.; Franceschina, C.; et al. Molecular Epidemiology of Western Equine Encephalitis Virus, South America, 2023-2024. Emerg. Infect. Dis. 2024, 30, 1834–1840. [Google Scholar] [CrossRef]
- Vissani, M.A.; Alamos, F.; Tordoya, M.S.; Minatel, L.; Schammas, J.M.; Dus Santos, M.J.; Trono, K.; Barrandeguy, M.E.; Balasuriya, U.B.; Carossino, M. Outbreak of Western Equine Encephalitis Virus Infection Associated with Neurological Disease in Horses Following a Nearly 40-Year Intermission Period in Argentina. Viruses 2024, 16, 1594. [Google Scholar] [CrossRef] [PubMed]
- Public Health Risk Assessment Related to Western Equine Encephalitis (WEE) Virus in the Region of the Americas [Press Release]. Online, 23 February 2024. Public Health Risk Assessment Related to Western Equine Encephalitis (WEE) Virus in the Region of the Americas—23 February 2024—PAHO/WHO|Pan American Health Organization. Available online: https://reliefweb.int/report/argentina/public-health-risk-assessment-related-western-equine-encephalitis-wee-virus-region-americas-23-february-2024 (accessed on 1 March 2024).
- Laveck, G.D.; Winn, J.F.; Welch, S.F. Inapparent infection with western equine encephalitis virus: Epidemiologic observations. Am. J. Public Health Nations Health 1955, 45, 1409–1416. [Google Scholar] [CrossRef] [PubMed]
- Cohen, R.; O’Connor, R.E.; Townsend, T.E.; Webb, P.A.; McKey, R.W. Western equine encephalomyelitis; clinical observations in infants and children. J. Pediatr. 1953, 43, 26–34. [Google Scholar] [CrossRef]
- McGowan, J.E., Jr.; Bryan, J.A.; Gregg, M.B. Surveillance of arboviral encephalitis in the United States, 1955-1971. Am. J. Epidemiol. 1973, 97, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Saul, F.; Alessandrini, M.V.; Maggi, M.; Lombardi, F.; Martiren, M.S. Western equine encephalitis, a report of two cases in pediatric patients. Arch. Argent Pediatr. 2025, 123, e202410383. [Google Scholar] [CrossRef]
- Rozdilsky, B.; Robertson, H.E.; Chorney, J. Western encephalitis: Report of eight fatal cases. Saskatchewan epidemic, 1965. Can. Med. Assoc. J. 1968, 98, 79–86. [Google Scholar]
- Mulder, D.W.; Parrott, M.; Thaler, M. Sequelae of western equine encephalitis. Neurology 1951, 1, 318–327. [Google Scholar] [CrossRef]
- Earnest, M.P.; Goolishian, H.A.; Calverley, J.R.; Hayes, R.O.; Hill, H.R. Neurologic, intellectual, and psychologic sequelae following western encephalitis. A follow-up study of 35 cases. Neurology 1971, 21, 969–974. [Google Scholar] [CrossRef]
- Barba, M.; Fairbanks, E.L.; Daly, J.M. Equine viral encephalitis: Prevalence, impact, and management strategies. Vet. Med. 2019, 10, 99–110. [Google Scholar] [CrossRef]
- Weaver, S.C.; Kang, W.; Shirako, Y.; Rumenapf, T.; Strauss, E.G.; Strauss, J.H. Recombinational history and molecular evolution of western equine encephalomyelitis complex alphaviruses. J. Virol. 1997, 71, 613–623. [Google Scholar] [CrossRef]
- Zacks, M.A.; Paessler, S. Encephalitic alphaviruses. Vet. Microbiol. 2010, 140, 281–286. [Google Scholar] [CrossRef]
- Chen, R.; Mukhopadhyay, S.; Merits, A.; Bolling, B.; Nasar, F.; Coffey, L.L.; Powers, A.; Weaver, S.C.; ICTV Report Consortium. ICTV Virus Taxonomy Profile: Togaviridae. J. Gen. Virol. 2018, 99, 761–762. [Google Scholar] [CrossRef] [PubMed]
- Hahn, C.S.; Lustig, S.; Strauss, E.G.; Strauss, J.H. Western equine encephalitis virus is a recombinant virus. Proc. Natl. Acad. Sci. USA 1988, 85, 5997–6001. [Google Scholar] [CrossRef] [PubMed]
- Sherman, M.B.; Weaver, S.C. Structure of the recombinant alphavirus Western equine encephalitis virus revealed by cryoelectron microscopy. J. Virol. 2010, 84, 9775–9782. [Google Scholar] [CrossRef] [PubMed]
- Reisen, W.K.; Fang, Y.; Brault, A.C. Limited interdecadal variation in mosquito (Diptera: Culicidae) and avian host competence for Western equine encephalomyelitis virus (Togaviridae: Alphavirus). Am. J. Trop. Med. Hyg. 2008, 78, 681–686. [Google Scholar] [CrossRef]
- Reisen, W.K.; Lundstrom, J.O.; Scott, T.W.; Eldridge, B.F.; Chiles, R.E.; Cusack, R.; Martinez, V.M.; Lothrop, H.D.; Gutierrez, D.; Wright, S.E.; et al. Patterns of avian seroprevalence to western equine encephalomyelitis and Saint Louis encephalitis viruses in California, USA. J. Med. Entomol. 2000, 37, 507–527. [Google Scholar] [CrossRef]
- Meyer, K.F.; Haring, C.M.; Howitt, B. The Etiology of Epizootic Encephalomyelitis of Horses in the San Joaquin Valley, 1930. Science 1931, 74, 227–228. [Google Scholar] [CrossRef]
- Bergren, N.A.; Auguste, A.J.; Forrester, N.L.; Negi, S.S.; Braun, W.A.; Weaver, S.C. Western equine encephalitis virus: Evolutionary analysis of a declining alphavirus based on complete genome sequences. J. Virol. 2014, 88, 9260–9267. [Google Scholar] [CrossRef]
- Bergren, N.A.; Haller, S.; Rossi, S.L.; Seymour, R.L.; Huang, J.; Miller, A.L.; Bowen, R.A.; Hartman, D.A.; Brault, A.C.; Weaver, S.C. "Submergence" of Western equine encephalitis virus: Evidence of positive selection argues against genetic drift and fitness reductions. PLoS Pathog. 2020, 16, e1008102. [Google Scholar] [CrossRef]
- Li, W.; Plante, J.A.; Lin, C.; Basu, H.; Plung, J.S.; Fan, X.; Boeckers, J.M.; Oros, J.; Buck, T.K.; Anekal, P.V.; et al. Shifts in receptors during submergence of an encephalitic arbovirus. Nature 2024, 632, 614–621. [Google Scholar] [CrossRef]
- (NCEZID) NCZID. Data and Maps for Western Equine Encephalitis Centers for Disease and Control. Available online: https://www.cdc.gov/wee/data-maps/index.html (accessed on 1 April 2025).
- Atasheva, S.; Wang, E.; Adams, A.P.; Plante, K.S.; Ni, S.; Taylor, K.; Miller, M.E.; Frolov, I.; Weaver, S.C. Chimeric alphavirus vaccine candidates protect mice from intranasal challenge with western equine encephalitis virus. Vaccine 2009, 27, 4309–4319. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kenney, J.L.; Adams, A.P.; Weaver, S.C. Transmission potential of two chimeric western equine encephalitis vaccine candidates in Culex tarsalis. Am. J. Trop. Med. Hyg. 2010, 82, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Coates, E.E.; Edupuganti, S.; Chen, G.L.; Happe, M.; Strom, L.; Widge, A.; Florez, M.B.; Cox, J.H.; Gordon, I.; Plummer, S.; et al. Safety and immunogenicity of a trivalent virus-like particle vaccine against western, eastern, and Venezuelan equine encephalitis viruses: A phase 1, open-label, dose-escalation, randomised clinical trial. Lancet Infect. Dis. 2022, 22, 1210–1220. [Google Scholar] [CrossRef] [PubMed]
- Ko, S.Y.; Akahata, W.; Yang, E.S.; Kong, W.P.; Burke, C.W.; Honnold, S.P.; Nichols, D.K.; Huang, Y.S.; Schieber, G.L.; Carlton, K.; et al. A virus-like particle vaccine prevents equine encephalitis virus infection in nonhuman primates. Sci. Transl. Med. 2019, 11. [Google Scholar] [CrossRef]
- Smith, D.R.; Schmaljohn, C.S.; Badger, C.; Ostrowski, K.; Zeng, X.; Grimes, S.D.; Rayner, J.O. Comparative pathology study of Venezuelan, eastern, and western equine encephalitis viruses in non-human primates. Antiviral Res. 2020, 182, 104875. [Google Scholar] [CrossRef]
- Martin, D.A.; Muth, D.A.; Brown, T.; Johnson, A.J.; Karabatsos, N.; Roehrig, J.T. Standardization of immunoglobulin M capture enzyme-linked immunosorbent assays for routine diagnosis of arboviral infections. J. Clin. Microbiol. 2000, 38, 1823–1826. [Google Scholar] [CrossRef]
- Calisher, C.H.; Berardi, V.P.; Muth, D.J.; Buff, E.E. Specificity of immunoglobulin M and G antibody responses in humans infected with eastern and western equine encephalitis viruses: Application to rapid serodiagnosis. J. Clin. Microbiol. 1986, 23, 369–372. [Google Scholar] [CrossRef]
- Calisher, C.H.; Mahmud, M.I.; El-Kafrawi, A.O.; Emerson, J.K.; Muth, D.J. Rapid and specific serodiagnosis of western equine encephalitis virus infection in horses. Am. J. Vet. Res. 1986, 47, 1296–1299. [Google Scholar] [CrossRef]
- U.S. Centers for Disease Control and Prevention. Biosafety in Microbiological and Biomedical Laboratories, 6th ed.; U.S. Department of Health and Human Services: Washington, DC, USA, 2020.
- Johnson, B.W.; Kosoy, O.; Hunsperger, E.; Beltran, M.; Delorey, M.; Guirakhoo, F.; Monath, T. Evaluation of chimeric Japanese encephalitis and dengue viruses for use in diagnostic plaque reduction neutralization tests. Clin. Vaccine Immunol. 2009, 16, 1052–1059. [Google Scholar] [CrossRef]
- Johnson, B.W.; Kosoy, O.; Wang, E.; Delorey, M.; Russell, B.; Bowen, R.A.; Weaver, S.C. Use of sindbis/eastern equine encephalitis chimeric viruses in plaque reduction neutralization tests for arboviral disease diagnostics. Clin. Vaccine Immunol. 2011, 18, 1486–1491. [Google Scholar] [CrossRef]
- Ni, H.; Yun, N.E.; Zacks, M.A.; Weaver, S.C.; Tesh, R.B.; da Rosa, A.P.; Powers, A.M.; Frolov, I.; Paessler, S. Recombinant alphaviruses are safe and useful serological diagnostic tools. Am. J. Trop. Med. Hyg. 2007, 76, 774–781. [Google Scholar] [CrossRef] [PubMed]
- Simon, J.K.; Kennedy, S.B.; Mahon, B.E.; Dubey, S.A.; Grant-Klein, R.J.; Liu, K.; Hartzel, J.; Coller, B.G.; Welebob, C.; Hanson, M.E.; et al. Immunogenicity of rVSVDeltaG-ZEBOV-GP Ebola vaccine (ERVEBO(R)) in African clinical trial participants by age, sex, and baseline GP-ELISA titer: A post hoc analysis of three Phase 2/3 trials. Vaccine 2022, 40, 6599–6606. [Google Scholar] [CrossRef]
- Safronetz, D.; Mire, C.; Rosenke, K.; Feldmann, F.; Haddock, E.; Geisbert, T.; Feldmann, H. A recombinant vesicular stomatitis virus-based Lassa fever vaccine protects guinea pigs and macaques against challenge with geographically and genetically distinct Lassa viruses. PLoS Negl. Trop. Dis. 2015, 9, e0003736. [Google Scholar] [CrossRef]
- Foster, S.L.; Woolsey, C.; Borisevich, V.; Agans, K.N.; Prasad, A.N.; Deer, D.J.; Geisbert, J.B.; Dobias, N.S.; Fenton, K.A.; Cross, R.W.; et al. A recombinant VSV-vectored vaccine rapidly protects nonhuman primates against lethal Nipah virus disease. Proc. Natl. Acad. Sci. USA 2022, 119, e2200065119. [Google Scholar] [CrossRef]
- Jones, S.M.; Feldmann, H.; Stroher, U.; Geisbert, J.B.; Fernando, L.; Grolla, A.; Klenk, H.D.; Sullivan, N.J.; Volchkov, V.E.; Fritz, E.A.; et al. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat. Med. 2005, 11, 786–790. [Google Scholar] [CrossRef]
- Marzi, A.; Jankeel, A.; Menicucci, A.R.; Callison, J.; O’Donnell, K.L.; Feldmann, F.; Pinski, A.N.; Hanley, P.W.; Messaoudi, I. Single Dose of a VSV-Based Vaccine Rapidly Protects Macaques From Marburg Virus Disease. Front. Immunol. 2021, 12, 774026. [Google Scholar] [CrossRef]
- Nasar, F.; Matassov, D.; Seymour, R.L.; Latham, T.; Gorchakov, R.V.; Nowak, R.M.; Leal, G.; Hamm, S.; Eldridge, J.H.; Tesh, R.B.; et al. Recombinant Isfahan Virus and Vesicular Stomatitis Virus Vaccine Vectors Provide Durable, Multivalent, Single-Dose Protection against Lethal Alphavirus Challenge. J. Virol. 2017, 91. [Google Scholar] [CrossRef] [PubMed]
- Chattopadhyay, A.; Aguilar, P.V.; Bopp, N.E.; Yarovinsky, T.O.; Weaver, S.C.; Rose, J.K. A recombinant virus vaccine that protects against both Chikungunya and Zika virus infections. Vaccine 2018, 36, 3894–3900. [Google Scholar] [CrossRef] [PubMed]
- Chattopadhyay, A.; Wang, E.; Seymour, R.; Weaver, S.C.; Rose, J.K. A chimeric vesiculo/alphavirus is an effective alphavirus vaccine. J. Virol. 2013, 87, 395–402. [Google Scholar] [CrossRef]
- Buchholz, U.J.; Finke, S.; Conzelmann, K.K. Generation of bovine respiratory syncytial virus (BRSV) from cDNA: BRSV NS2 is not essential for virus replication in tissue culture, and the human RSV leader region acts as a functional BRSV genome promoter. J. Virol. 1999, 73, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Mossel, E.C.; Ledermann, J.P.; Phillips, A.T.; Borland, E.M.; Powers, A.M.; Olson, K.E. Molecular determinants of mouse neurovirulence and mosquito infection for Western equine encephalitis virus. PLoS ONE 2013, 8, e60427. [Google Scholar] [CrossRef]
- Calvert, A.E.; Bennett, S.L.; Hunt, A.R.; Fong, R.H.; Doranz, B.J.; Roehrig, J.T.; Blair, C.D. Exposing cryptic epitopes on the Venezuelan equine encephalitis virus E1 glycoprotein prior to treatment with alphavirus cross-reactive monoclonal antibody allows blockage of replication early in infection. Virology 2022, 565, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Baer, A.; Kehn-Hall, K. Viral concentration determination through plaque assays: Using traditional and novel overlay systems. J. Vis. Exp. 2014, e52065. [Google Scholar] [CrossRef]
- Goodman, C.; Powers, J.A.; Mikula, S.R.; Hughes, H.R.; Biggerstaff, B.J.; Fitzpatrick, K.; Panella, A.J.; Machain-Williams, C.; Lee, S.; Calvert, A.E. Development of a Diagnostic IgM Antibody Capture ELISA for Detection of Anti-Cache Valley Virus Human IgM. Am. J. Trop. Med. Hyg. 2025, 112, 386–395. [Google Scholar] [CrossRef] [PubMed]
- Obijeski, J.F.; Marchenko, A.T.; Bishop, D.H.; Cann, B.W.; Murphy, F.A. Comparative electrophoretic analysis of the virus proteins of four rhabdoviruses. J. Gen. Virol. 1974, 22, 21–33. [Google Scholar] [CrossRef]
- Mendoza, E.J.; Manguiat, K.; Wood, H.; Drebot, M. Two Detailed Plaque Assay Protocols for the Quantification of Infectious SARS-CoV-2. Curr. Protoc. Microbiol. 2020, 57, ecpmc105. [Google Scholar] [CrossRef]
- Wertz, G.W.; Moudy, R.; Ball, L.A. Adding genes to the RNA genome of vesicular stomatitis virus: Positional effects on stability of expression. J. Virol. 2002, 76, 7642–7650. [Google Scholar] [CrossRef]
- Ge, P.; Tsao, J.; Schein, S.; Green, T.J.; Luo, M.; Zhou, Z.H. Cryo-EM model of the bullet-shaped vesicular stomatitis virus. Science 2010, 327, 689–693. [Google Scholar] [CrossRef]
- Phelps, A.L.; O’Brien, L.M.; Ulaeto, D.O.; Holtsberg, F.W.; Liao, G.C.; Douglas, R.; Aman, M.J.; Glass, P.J.; Moyer, C.L.; Ennis, J.; et al. Cross-Strain Neutralizing and Protective Monoclonal Antibodies against EEEV or WEEV. Viruses 2021, 13, 2231. [Google Scholar] [CrossRef] [PubMed]
- Schmaljohn, A.L.; Johnson, E.D.; Dalrymple, J.M.; Cole, G.A. Non-neutralizing monoclonal antibodies can prevent lethal alphavirus encephalitis. Nature 1982, 297, 70–72. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.S.; Kafai, N.M.; Winkler, E.S.; Gilliland, T.C., Jr.; Cottle, E.L.; Earnest, J.T.; Jethva, P.N.; Kaplonek, P.; Shah, A.P.; Fong, R.H.; et al. Pan-protective anti-alphavirus human antibodies target a conserved E1 protein epitope. Cell 2021, 184, 4414–4429 e4419. [Google Scholar] [CrossRef]
- Sutton, M.S.; Pletnev, S.; Callahan, V.; Ko, S.; Tsybovsky, Y.; Bylund, T.; Casner, R.G.; Cerutti, G.; Gardner, C.L.; Guirguis, V.; et al. Vaccine elicitation and structural basis for antibody protection against alphaviruses. Cell 2023, 186, 2672–2689.e25. [Google Scholar] [CrossRef]
- Hanson, R.P.; Sulkin, S.E.; Beuscher, E.L.; Hammon, W.M.; McKinney, R.W.; Work, T.H. Arbovirus infections of laboratory workers. Extent of problem emphasizes the need for more effective measures to reduce hazards. Science 1967, 158, 1283–1286. [Google Scholar] [CrossRef]

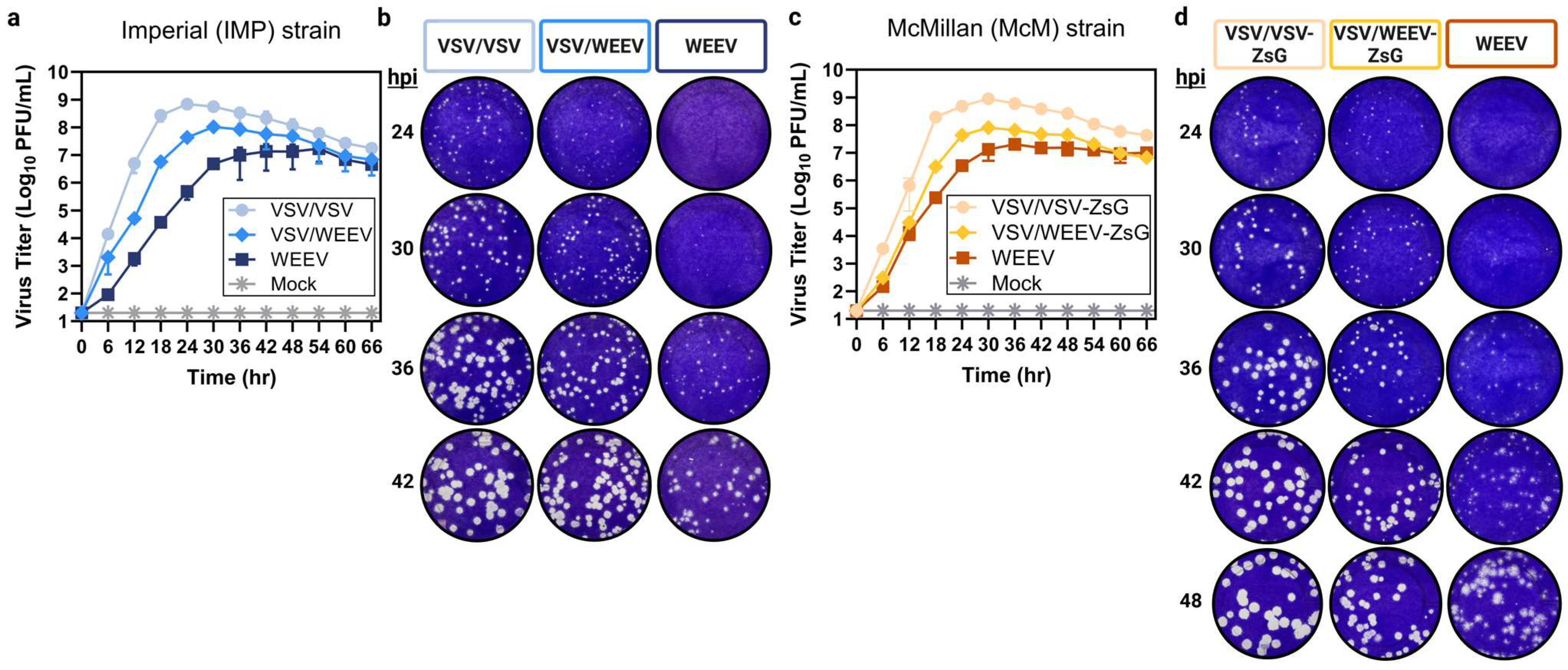
| Virus | Mean Plaque Diameter (Range) in mm | ||||
|---|---|---|---|---|---|
| 24 hpi | 30 hpi | 36 hpi | 42 hpi | 48 hpi | |
| VSV/VSV | 1 (<0.5–1.0) | 1.3 (<0.5–2.0) | 2.0 (0.5–2.5) | 2.5 (0.5–3.0) | --- |
| VSV/WEEV (IMP) | 0.5 (<0.5–1.0) | 1.0 (<0.5–1.3) | 1.5 (0.5–2.0) | 2.0 (1.0–2.5) | --- |
| WEEV (IMP) | Not detectable | <0.5 (<0.5–0.75) | 0.75 (<0.5–1.0) | 1.5 (<0.5–2.0) | --- |
| VSV/VSV-ZsG | 1.0 (<0.5–1.0) | 1.3 (<0.5–1.5) | 2.0 (0.5–2.5) | 2.5 (1.5–3.0) | 3.0 (2.0–3.5) |
| VSV/WEEV-ZsG (McM) | 0.5 (<0.5–1.0) | 1.0 (<0.5–1.3) | 1.5 (0.5–2.0) | 2.0 (1.0–2.0) | 2.5 (1.0–2.5) |
| WEEV (McM) | Not detectable | <0.5 (<0.50) | 1.0 (<0.5–1.3) | 1.5 (<0.5–2.0) | 2.0 (<0.5–3.0) |
| Antibody | IC90 1 | PRNT90 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| Specificity | Source | Isolate | VSV/WEEV | WEEV | VSV/WEEV | WEEV | ||
| Mean (95% CI) | Mean (95% CI) | Trial 1 | Trial 2 | Trial 1 | Trial 2 | |||
| WEEV | mouse | pooled 3 | 72 (40–130) | 118 (57–246) | 160 | 80 | 160 | 80 |
| WEEV | mouse | Y62-33 | 354 (289–433) | 198 (137–284) | 160 | 320 | 160 | 80 |
| WEEV | mouse | M2-958 | 328 (280–385) | 20 (12–35) | 160 | 320 | 20 | 40 |
| WEEV | mouse | Fleming1 | 62 (43–92) | 27 (15–48) | 20 | 80 | <20 | <20 |
| WEEV | mouse | Fleming2 | 40 (26–62) | <20 | 80 | 40 | <20 | <20 |
| WEEV | chicken | unknown | 128 (87–187) | 60 (40–91) | 80 | 160 | 40 | <40 |
| WEEV | horse | Fleming | 393 (313–494) | 97 (59–158) | 320 | 320 | 20 | 20 |
| VSV | mouse | Indiana | <20 | <20 | <20 | <20 | <20 | <20 |
| ------ | horse | ------- | <20 | <20 | <20 | <20 | <20 | <20 |
| Antibody | IC90 1 | PRNT90 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| Specificity | Source | Isolate | VSV/WEEV | WEEV | VSV/WEEV | WEEV | ||
| Mean (95% CI) | Mean (95% CI) | Trial 1 | Trial 2 | Trial 1 | Trial 2 | |||
| WEEV | mouse | pooled 3 | 267 (200–344) | 172 (109–258) | 320 | 160 | 160 | 160 |
| WEEV | mouse | Y62-33 | 372 (256–520) | 105 (63–165) | 640 | 320 | 160 | 80 |
| WEEV | mouse | M2-958 | 348 (224–517) | <20 | 320 | 160 | 20 | 20 |
| WEEV | mouse | Fleming1 | 93 (53–149) | <20 | 160 | 80 | 40 | 40 |
| WEEV | mouse | Fleming2 | 44 (27–67) | <20 | 40 | 40 | <20 | <20 |
| WEEV | horse | Fleming | 219 (173–272) | 74 (52–103) | 320 | 160 | 40 | <20 |
| VSV | mouse | Indiana | <20 | <20 | <20 | <20 | <20 | <20 |
| ------ | horse | ------- | <20 | <20 | <20 | <20 | <20 | <20 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miazgowicz, K.L.; Maloney, B.E.; Brindley, M.A.; Cassaday, M.; Petch, R.J.; Bates, P.; Brault, A.C.; Calvert, A.E. Chimeric Vesicular Stomatitis Virus Bearing Western Equine Encephalitis Virus Envelope Proteins E2-E1 Is a Suitable Surrogate for Western Equine Encephalitis Virus in a Plaque Reduction Neutralization Test. Viruses 2025, 17, 1067. https://doi.org/10.3390/v17081067
Miazgowicz KL, Maloney BE, Brindley MA, Cassaday M, Petch RJ, Bates P, Brault AC, Calvert AE. Chimeric Vesicular Stomatitis Virus Bearing Western Equine Encephalitis Virus Envelope Proteins E2-E1 Is a Suitable Surrogate for Western Equine Encephalitis Virus in a Plaque Reduction Neutralization Test. Viruses. 2025; 17(8):1067. https://doi.org/10.3390/v17081067
Chicago/Turabian StyleMiazgowicz, Kerri L., Bailey E. Maloney, Melinda A. Brindley, Mattie Cassaday, Raegan J. Petch, Paul Bates, Aaron C. Brault, and Amanda E. Calvert. 2025. "Chimeric Vesicular Stomatitis Virus Bearing Western Equine Encephalitis Virus Envelope Proteins E2-E1 Is a Suitable Surrogate for Western Equine Encephalitis Virus in a Plaque Reduction Neutralization Test" Viruses 17, no. 8: 1067. https://doi.org/10.3390/v17081067
APA StyleMiazgowicz, K. L., Maloney, B. E., Brindley, M. A., Cassaday, M., Petch, R. J., Bates, P., Brault, A. C., & Calvert, A. E. (2025). Chimeric Vesicular Stomatitis Virus Bearing Western Equine Encephalitis Virus Envelope Proteins E2-E1 Is a Suitable Surrogate for Western Equine Encephalitis Virus in a Plaque Reduction Neutralization Test. Viruses, 17(8), 1067. https://doi.org/10.3390/v17081067









