Consensus Sequences for Gag and Pol Introduced into HIV-1 Clade B Laboratory Strains Differentially Influence the Impact of Point Mutations Associated with Immune Escape and with Drug Resistance on Viral Replicative Capacity
Abstract
1. Introduction
2. Materials and Methods
2.1. Consensus Sequence
2.2. Variant NL4-3 and Consensus Constructs
2.3. Cells
2.4. Viral Stocks
2.5. ELISA
2.6. Viral Infectivity Assays
2.7. Flow Cytometry
2.8. Statistical Analysis
3. Results
3.1. HIV-1 Clones with Consensus Sequences in Gag and/or Pol Are Replication-Competent
3.2. The Impact of Immune Escape Variants on Replication Capacity in Gag Is Influenced by the Underlying Backbone
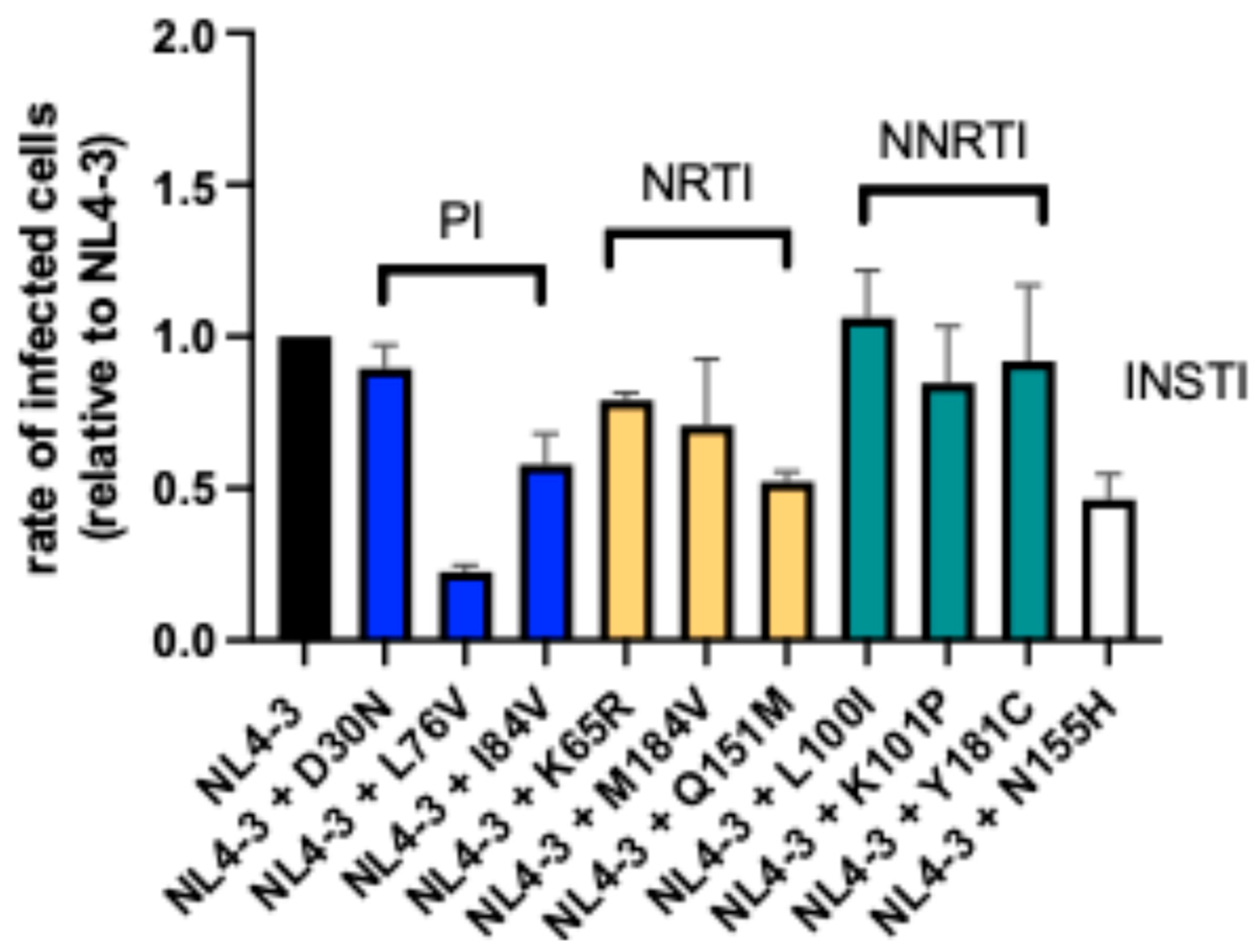
3.3. The Viral Backbone Differentially Influences the Impact of Drug Resistance Mutations on Replication Capacity
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Koup, R.A.; Safrit, J.T.; Cao, Y.; Andrews, C.A.; McLeod, G.; Borkowsky, W.; Farthing, C.; Ho, D.D. Temporal association of cellular immune responses with the initial control of viremia in primary human immunodeficiency virus type 1 syndrome. J. Virol. 1994, 68, 4650–4655. [Google Scholar] [CrossRef] [PubMed]
- Borrow, P.; Lewicki, H.; Hahn, B.H.; Shaw, G.M.; Oldstone, M.B. Virus-specific CD8+ cytotoxic T-lymphocyte activity associated with control of viremia in primary human immunodeficiency virus type 1 infection. J. Virol. 1994, 68, 6103–6110. [Google Scholar] [CrossRef] [PubMed]
- Brockman, M.A.; Brumme, Z.L.; Brumme, C.J.; Miura, T.; Sela, J.; Rosato, P.C.; Kadie, C.M.; Carlson, J.M.; Markle, T.J.; Streeck, H.; et al. Early selection in Gag by protective HLA alleles contributes to reduced HIV-1 replication capacity that may be largely compensated for in chronic infection. J. Virol. 2010, 84, 11937–11949. [Google Scholar] [CrossRef] [PubMed]
- Zaunders, J.; van Bockel, D. Innate and Adaptive Immunity in Long-Term Non-Progression in HIV Disease. Front. Immunol. 2013, 4, 95. [Google Scholar] [CrossRef]
- Borrow, P.; Lewicki, H.; Wei, X.; Horwitz, M.S.; Peffer, N.; Meyers, H.; Nelson, J.A.; Gairin, J.E.; Hahn, B.H.; Oldstone, M.B.; et al. Antiviral pressure exerted by HIV-1-specific cytotoxic T lymphocytes (CTLs) during primary infection demonstrated by rapid selection of CTL escape virus. Nat. Med. 1997, 3, 205–211. [Google Scholar] [CrossRef]
- Allen, T.M.; Altfeld, M.; Geer, S.C.; Kalife, E.T.; Moore, C.; O’Sullivan, K.M.; Desouza, I.; Feeney, M.E.; Eldridge, R.L.; Maier, E.L.; et al. Selective escape from CD8+ T-cell responses represents a major driving force of human immunodeficiency virus type 1 (HIV-1) sequence diversity and reveals constraints on HIV-1 evolution. J. Virol. 2005, 79, 13239–13249. [Google Scholar] [CrossRef]
- Altfeld, M.; Kalife, E.T.; Qi, Y.; Streeck, H.; Lichterfeld, M.; Johnston, M.N.; Burgett, N.; Swartz, M.E.; Yang, A.; Alter, G.; et al. HLA Alleles Associated with Delayed Progression to AIDS Contribute Strongly to the Initial CD8(+) T Cell Response against HIV-1. PLoS Med. 2006, 3, e403. [Google Scholar] [CrossRef]
- Kelleher, A.D.; Long, C.; Holmes, E.C.; Allen, R.L.; Wilson, J.; Conlon, C.; Workman, C.; Shaunak, S.; Olson, K.; Goulder, P.; et al. Clustered mutations in HIV-1 gag are consistently required for escape from HLA-B27-restricted cytotoxic T lymphocyte responses. J. Exp. Med. 2001, 193, 375–386. [Google Scholar] [CrossRef]
- Miura, T.; Brockman, M.A.; Schneidewind, A.; Lobritz, M.; Pereyra, F.; Rathod, A.; Block, B.L.; Brumme, Z.L.; Brumme, C.J.; Baker, B.; et al. HLA-B57/B*5801 human immunodeficiency virus type 1 elite controllers select for rare gag variants associated with reduced viral replication capacity and strong cytotoxic T-lymphocyte [corrected] recognition. J. Virol. 2009, 83, 2743–2755. [Google Scholar] [CrossRef]
- den Uyl, D.; van der Horst-Bruinsma, I.E.; van Agtmael, M. Progression of HIV to AIDS: A protective role for HLA-B27? AIDS Rev. 2004, 6, 89–96. [Google Scholar]
- Altfeld, M.; Addo, M.M.; Rosenberg, E.S.; Hecht, F.M.; Lee, P.K.; Vogel, M.; Yu, X.G.; Draenert, R.; Johnston, M.N.; Strick, D.; et al. Influence of HLA-B57 on clinical presentation and viral control during acute HIV-1 infection. Aids 2003, 17, 2581–2591. [Google Scholar] [CrossRef] [PubMed]
- Navis, M.; Schellens, I.; van Baarle, D.; Borghans, J.; van Swieten, P.; Miedema, F.; Kootstra, N.; Schuitemaker, H. Viral replication capacity as a correlate of HLA B57/B5801-associated nonprogressive HIV-1 infection. J. Immunol. 2007, 179, 3133–3143. [Google Scholar] [CrossRef] [PubMed]
- Kaslow, R.A.; Carrington, M.; Apple, R.; Park, L.; Munoz, A.; Saah, A.J.; Goedert, J.J.; Winkler, C.; O’Brien, S.J.; Rinaldo, C.; et al. Influence of combinations of human major histocompatibility complex genes on the course of HIV-1 infection. Nat. Med. 1996, 2, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Pereyra, F.; Jia, X.; McLaren, P.J.; Telenti, A.; de Bakker, P.I.; Walker, B.D.; Ripke, S.; Brumme, C.J.; Pulit, S.L.; Carrington, M.; et al. The major genetic determinants of HIV-1 control affect HLA class I peptide presentation. Science 2010, 330, 1551–1557. [Google Scholar]
- Boutwell, C.L.; Carlson, J.M.; Lin, T.H.; Seese, A.; Power, K.A.; Peng, J.; Tang, Y.; Brumme, Z.L.; Heckerman, D.; Schneidewind, A.; et al. Frequent and variable cytotoxic-T-lymphocyte escape-associated fitness costs in the human immunodeficiency virus type 1 subtype B Gag proteins. J. Virol. 2013, 87, 3952–3965. [Google Scholar] [CrossRef]
- Schneidewind, A.; Brockman, M.A.; Yang, R.; Adam, R.I.; Li, B.; Le Gall, S.; Rinaldo, C.R.; Craggs, S.L.; Allgaier, R.L.; Power, K.A.; et al. Escape from the dominant HLA-B27-restricted cytotoxic T-lymphocyte response in Gag is associated with a dramatic reduction in human immunodeficiency virus type 1 replication. J. Virol. 2007, 81, 12382–12393. [Google Scholar] [CrossRef]
- Gijsbers, E.F.; Feenstra, K.A.; van Nuenen, A.C.; Navis, M.; Heringa, J.; Schuitemaker, H.; Kootstra, N.A. HIV-1 replication fitness of HLA-B*57/58:01 CTL escape variants is restored by the accumulation of compensatory mutations in gag. PLoS ONE 2013, 8, e81235. [Google Scholar] [CrossRef]
- Du, Y.; Zhang, T.H.; Dai, L.; Zheng, X.; Gorin, A.M.; Oishi, J.; Wu, T.T.; Yoshizawa, J.M.; Li, X.; Yang, O.O.; et al. Effects of Mutations on Replicative Fitness and Major Histocompatibility Complex Class I Binding Affinity Are Among the Determinants Underlying Cytotoxic-T-Lymphocyte Escape of HIV-1 Gag Epitopes. mBio 2017, 8. [Google Scholar] [CrossRef]
- Ammaranond, P.; van Bockel, D.J.; Petoumenos, K.; McMurchie, M.; Finlayson, R.; Middleton, M.G.; Davenport, M.P.; Venturi, V.; Suzuki, K.; Gelgor, L.; et al. HIV immune escape at an immunodominant epitope in HLA-B*27-positive individuals predicts viral load outcome. J. Immunol. 2011, 186, 479–488. [Google Scholar] [CrossRef]
- Havlir, D.V.; Hellmann, N.S.; Petropoulos, C.J.; Whitcomb, J.M.; Collier, A.C.; Hirsch, M.S.; Tebas, P.; Sommadossi, J.P.; Richman, D.D. Drug susceptibility in HIV infection after viral rebound in patients receiving indinavir-containing regimens. Jama 2000, 283, 229–234. [Google Scholar] [CrossRef]
- Ledergerber, B.; Egger, M.; Opravil, M.; Telenti, A.; Hirschel, B.; Battegay, M.; Vernazza, P.; Sudre, P.; Flepp, M.; Furrer, H.; et al. Clinical progression and virological failure on highly active antiretroviral therapy in HIV-1 patients: A prospective cohort study. Swiss HIV Cohort Study. Lancet 1999, 353, 863–868. [Google Scholar] [CrossRef] [PubMed]
- Deeks, S.G.; Barbour, J.D.; Martin, J.N.; Swanson, M.S.; Grant, R.M. Sustained CD4+ T cell response after virologic failure of protease inhibitor-based regimens in patients with human immunodeficiency virus infection. J. Infect. Dis. 2000, 181, 946–953. [Google Scholar] [CrossRef] [PubMed]
- Deeks, S.G.; Wrin, T.; Liegler, T.; Hoh, R.; Hayden, M.; Barbour, J.D.; Hellmann, N.S.; Petropoulos, C.J.; McCune, J.M.; Hellerstein, M.K.; et al. Virologic and immunologic consequences of discontinuing combination antiretroviral-drug therapy in HIV-infected patients with detectable viremia. N. Engl. J. Med. 2001, 344, 472–480. [Google Scholar] [CrossRef]
- Martinez-Picado, J.; DePasquale, M.P.; Kartsonis, N.; Hanna, G.J.; Wong, J.; Finzi, D.; Rosenberg, E.; Gunthard, H.F.; Sutton, L.; Savara, A.; et al. Antiretroviral resistance during successful therapy of HIV type 1 infection. Proc. Natl. Acad. Sci. USA 2000, 97, 10948–10953. [Google Scholar] [CrossRef]
- Seyler, C.; Adjé-Touré, C.; Messou, E.; Dakoury-Dogbo, N.; Rouet, F.; Gabillard, D.; Nolan, M.; Toure, S.; Anglaret, X. Impact of genotypic drug resistance mutations on clinical and immunological outcomes in HIV-infected adults on HAART in West Africa. Aids 2007, 21, 1157–1164. [Google Scholar] [CrossRef]
- Martinez-Picado, J.; Savara, A.V.; Sutton, L.; D’Aquila, R.T. Replicative fitness of protease inhibitor-resistant mutants of human immunodeficiency virus type 1. J. Virol. 1999, 73, 3744–3752. [Google Scholar] [CrossRef]
- Zennou, V.; Mammano, F.; Paulous, S.; Mathez, D.; Clavel, F. Loss of viral fitness associated with multiple Gag and Gag-Pol processing defects in human immunodeficiency virus type 1 variants selected for resistance to protease inhibitors in vivo. J. Virol. 1998, 72, 3300–3306. [Google Scholar] [CrossRef]
- Croteau, G.; Doyon, L.; Thibeault, D.; McKercher, G.; Pilote, L.; Lamarre, D. Impaired fitness of human immunodeficiency virus type 1 variants with high-level resistance to protease inhibitors. J. Virol. 1997, 71, 1089–1096. [Google Scholar] [CrossRef]
- Harrigan, P.R.; Bloor, S.; Larder, B.A. Relative replicative fitness of zidovudine-resistant human immunodeficiency virus type 1 isolates in vitro. J. Virol. 1998, 72, 3773–3778. [Google Scholar] [CrossRef]
- Mammano, F.; Trouplin, V.; Zennou, V.; Clavel, F. Retracing the evolutionary pathways of human immunodeficiency virus type 1 resistance to protease inhibitors: Virus fitness in the absence and in the presence of drug. J. Virol. 2000, 74, 8524–8531. [Google Scholar] [CrossRef]
- Sharma, P.L.; Crumpacker, C.S. Attenuated replication of human immunodeficiency virus type 1 with a didanosine-selected reverse transcriptase mutation. J. Virol. 1997, 71, 8846–8851. [Google Scholar] [CrossRef] [PubMed]
- De Luca, A. Resistance to newly approved and investigational protease inhibitors. Curr. Opin. HIV AIDS 2007, 2, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Hicks, C.B.; Goswami, N.D.; Tafoya, E.; Ribeiro, R.M.; Cai, F.; Perelson, A.S.; Gao, F. Evolution of drug-resistant viral populations during interruption of antiretroviral therapy. J. Virol. 2011, 85, 6403–6415. [Google Scholar] [CrossRef]
- Deeks, S.G.; Hoh, R.; Neilands, T.B.; Liegler, T.; Aweeka, F.; Petropoulos, C.J.; Grant, R.M.; Martin, J.N. Interruption of treatment with individual therapeutic drug classes in adults with multidrug-resistant HIV-1 infection. J. Infect. Dis. 2005, 192, 1537–1544. [Google Scholar] [CrossRef]
- Devereux, H.L.; Youle, M.; Johnson, M.A.; Loveday, C. Rapid decline in detectability of HIV-1 drug resistance mutations after stopping therapy. Aids 1999, 13, 123–127. [Google Scholar] [CrossRef]
- Lawrence, J.; Mayers, D.L.; Hullsiek, K.H.; Collins, G.; Abrams, D.I.; Reisler, R.B.; Crane, L.R.; Schmetter, B.S.; Dionne, T.J.; Saldanha, J.M.; et al. Structured treatment interruption in patients with multidrug-resistant human immunodeficiency virus. N. Engl. J. Med. 2003, 349, 837–846. [Google Scholar] [CrossRef]
- Verhofstede, C.; Wanzeele, F.V.; Van Der Gucht, B.; De Cabooter, N.; Plum, J. Interruption of reverse transcriptase inhibitors or a switch from reverse transcriptase to protease inhibitors resulted in a fast reappearance of virus strains with a reverse transcriptase inhibitor-sensitive genotype. Aids 1999, 13, 2541–2546. [Google Scholar] [CrossRef]
- Goudsmit, J.; De Ronde, A.; Ho, D.D.; Perelson, A.S. Human immunodeficiency virus fitness in vivo: Calculations based on a single zidovudine resistance mutation at codon 215 of reverse transcriptase. J. Virol. 1996, 70, 5662–5664. [Google Scholar] [CrossRef]
- Pingen, M.; Nijhuis, M.; de Bruijn, J.A.; Boucher, C.A.; Wensing, A.M. Evolutionary pathways of transmitted drug-resistant HIV-1. J. Antimicrob. Chemother. 2011, 66, 1467–1480. [Google Scholar] [CrossRef]
- Machnowska, P.; Meixenberger, K.; Schmidt, D.; Jessen, H.; Hillenbrand, H.; Gunsenheimer-Bartmeyer, B.; Hamouda, O.; Kücherer, C.; Bannert, N. Prevalence and persistence of transmitted drug resistance mutations in the German HIV-1 Seroconverter Study Cohort. PLoS ONE 2019, 14, e0209605. [Google Scholar] [CrossRef]
- Crawford, H.; Prado, J.G.; Leslie, A.; Hué, S.; Honeyborne, I.; Reddy, S.; van der Stok, M.; Mncube, Z.; Brander, C.; Rousseau, C.; et al. Compensatory mutation partially restores fitness and delays reversion of escape mutation within the immunodominant HLA-B*5703-restricted Gag epitope in chronic human immunodeficiency virus type 1 infection. J. Virol. 2007, 81, 8346–8351. [Google Scholar] [CrossRef] [PubMed]
- Schneidewind, A.; Brockman, M.A.; Sidney, J.; Wang, Y.E.; Chen, H.; Suscovich, T.J.; Li, B.; Adam, R.I.; Allgaier, R.L.; Mothé, B.R.; et al. Structural and functional constraints limit options for cytotoxic T-lymphocyte escape in the immunodominant HLA-B27-restricted epitope in human immunodeficiency virus type 1 capsid. J. Virol. 2008, 82, 5594–5605. [Google Scholar] [CrossRef] [PubMed]
- Goulder, P.J.; Phillips, R.E.; Colbert, R.A.; McAdam, S.; Ogg, G.; Nowak, M.A.; Giangrande, P.; Luzzi, G.; Morgan, B.; Edwards, A.; et al. Late escape from an immunodominant cytotoxic T-lymphocyte response associated with progression to AIDS. Nat. Med. 1997, 3, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Brockman, M.A.; Schneidewind, A.; Lahaie, M.; Schmidt, A.; Miura, T.; Desouza, I.; Ryvkin, F.; Derdeyn, C.A.; Allen, S.; Hunter, E.; et al. Escape and compensation from early HLA-B57-mediated cytotoxic T-lymphocyte pressure on human immunodeficiency virus type 1 Gag alter capsid interactions with cyclophilin A. J. Virol. 2007, 81, 12608–12618. [Google Scholar] [CrossRef]
- Migueles, S.A.; Laborico, A.C.; Imamichi, H.; Shupert, W.L.; Royce, C.; McLaughlin, M.; Ehler, L.; Metcalf, J.; Liu, S.; Hallahan, C.W.; et al. The differential ability of HLA B*5701+ long-term nonprogressors and progressors to restrict human immunodeficiency virus replication is not caused by loss of recognition of autologous viral gag sequences. J. Virol. 2003, 77, 6889–6898. [Google Scholar] [CrossRef]
- Phillips, R.E.; Rowland-Jones, S.; Nixon, D.F.; Gotch, F.M.; Edwards, J.P.; Ogunlesi, A.O.; Elvin, J.G.; Rothbard, J.A.; Bangham, C.R.; Rizza, C.R.; et al. Human immunodeficiency virus genetic variation that can escape cytotoxic T cell recognition. Nature 1991, 354, 453–459. [Google Scholar] [CrossRef]
- Larder, B.A.; Darby, G.; Richman, D.D. HIV with reduced sensitivity to zidovudine (AZT) isolated during prolonged therapy. Science 1989, 243, 1731–1734. [Google Scholar] [CrossRef]
- Schuurman, R.; Nijhuis, M.; van Leeuwen, R.; Schipper, P.; de Jong, D.; Collis, P.; Danner, S.A.; Mulder, J.; Loveday, C.; Christopherson, C.; et al. Rapid changes in human immunodeficiency virus type 1 RNA load and appearance of drug-resistant virus populations in persons treated with lamivudine (3TC). J. Infect. Dis. 1995, 171, 1411–1419. [Google Scholar] [CrossRef]
- Rooke, R.; Tremblay, M.; Soudeyns, H.; DeStephano, L.; Yao, X.J.; Fanning, M.; Montaner, J.S.; O’Shaughnessy, M.; Gelmon, K.; Tsoukas, C.; et al. Isolation of drug-resistant variants of HIV-1 from patients on long-term zidovudine therapy. Canadian Zidovudine Multi-Centre Study Group. Aids 1989, 3, 411–415. [Google Scholar] [CrossRef]
- Condra, J.H.; Holder, D.J.; Schleif, W.A.; Blahy, O.M.; Danovich, R.M.; Gabryelski, L.J.; Graham, D.J.; Laird, D.; Quintero, J.C.; Rhodes, A.; et al. Genetic correlates of in vivo viral resistance to indinavir, a human immunodeficiency virus type 1 protease inhibitor. J. Virol. 1996, 70, 8270–8276. [Google Scholar] [CrossRef]
- Richman, D.D.; Havlir, D.; Corbeil, J.; Looney, D.; Ignacio, C.; Spector, S.A.; Sullivan, J.; Cheeseman, S.; Barringer, K.; Pauletti, D.; et al. Nevirapine resistance mutations of human immunodeficiency virus type 1 selected during therapy. J. Virol. 1994, 68, 1660–1666. [Google Scholar] [CrossRef] [PubMed]
- Richman, D.D.; Meng, T.C.; Spector, S.A.; Fischl, M.A.; Resnick, L.; Lai, S. Resistance to AZT and ddC during long-term combination therapy in patients with advanced infection with human immunodeficiency virus. J. Acquir. Immune Defic. Syndr. 1994, 7, 135–138. [Google Scholar] [PubMed]
- Havlir, D.V.; Marschner, I.C.; Hirsch, M.S.; Collier, A.C.; Tebas, P.; Bassett, R.L.; Ioannidis, J.P.; Holohan, M.K.; Leavitt, R.; Boone, G.; et al. Maintenance antiretroviral therapies in HIV-infected subjects with undetectable plasma HIV RNA after triple-drug therapy. AIDS Clinical Trials Group Study 343 Team. N. Engl. J. Med. 1998, 339, 1261–1268. [Google Scholar] [CrossRef]
- Soares, E.A.; Santos, A.F.; Sousa, T.M.; Sprinz, E.; Martinez, A.M.; Silveira, J.; Tanuri, A.; Soares, M.A. Differential drug resistance acquisition in HIV-1 of subtypes B and C. PLoS ONE 2007, 2, e730. [Google Scholar] [CrossRef]
- Dumans, A.T.; Barreto, C.C.; Santos, A.F.; Arruda, M.; Sousa, T.M.; Machado, E.S.; Sabino, E.C.; Brindeiro, R.M.; Tanuri, A.; Duarte, A.J.; et al. Distinct resistance mutation and polymorphism acquisition in HIV-1 protease of subtypes B and F1 from children and adult patients under virological failure. Infect. Genet. Evol. 2009, 9, 62–70. [Google Scholar] [CrossRef]
- Cunha, R.D.; Abreu, C.M.; Gonzalez, L.M.; Nijhuis, M.; de Jong, D.; Aguiar, R.S.; Afonso, A.O.; Brindeiro, R.M.; Tanuri, A. Differential in vitro kinetics of drug resistance mutation acquisition in HIV-1 RT of subtypes B and C. PLoS ONE 2012, 7, e46622. [Google Scholar] [CrossRef]
- Adachi, A.; Gendelman, H.E.; Koenig, S.; Folks, T.; Willey, R.; Rabson, A.; Martin, M.A. Production of acquired immunodeficiency syndrome-associated retrovirus in human and nonhuman cells transfected with an infectious molecular clone. J. Virol. 1986, 59, 284–291. [Google Scholar] [CrossRef]
- Ratner, L.; Fisher, A.; Jagodzinski, L.L.; Mitsuya, H.; Liou, R.S.; Gallo, R.C.; Wong-Staal, F. Complete nucleotide sequences of functional clones of the AIDS virus. AIDS Res. Hum. Retrovir. 1987, 3, 57–69. [Google Scholar] [CrossRef]
- Foley, B.; Leitner, T.; Apetrei, C.; Hahn, B.; Mizrachi, I.; Mullins, J.; Rambaut, A.; Wolinsky, S.; Korber, B. (Eds.) HIV Sequence Compendium 2018; Los Alamos National Laboratory: Los Alamos, NM, USA, 2018.
- Altfeld, M.; Allen, T.M.; Yu, X.G.; Johnston, M.N.; Agrawal, D.; Korber, B.T.; Montefiori, D.C.; O’Connor, D.H.; Davis, B.T.; Lee, P.K.; et al. HIV-1 superinfection despite broad CD8+ T-cell responses containing replication of the primary virus. Nature 2002, 420, 434–439. [Google Scholar] [CrossRef]
- Brockman, M.A.; Tanzi, G.O.; Walker, B.D.; Allen, T.M. Use of a novel GFP reporter cell line to examine replication capacity of CXCR4- and CCR5-tropic HIV-1 by flow cytometry. J. Virol. Methods 2006, 131, 134–142. [Google Scholar] [CrossRef]
- Gervaix, A.; West, D.; Leoni, L.M.; Richman, D.D.; Wong-Staal, F.; Corbeil, J. A new reporter cell line to monitor HIV infection and drug susceptibility in vitro. Proc. Natl. Acad. Sci. USA 1997, 94, 4653–4658. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, T.C.; Frye, C.A.; Yant, L.J.; O’Connor, D.H.; Kriewaldt, N.A.; Benson, M.; Vojnov, L.; Dodds, E.J.; Cullen, C.; Rudersdorf, R.; et al. Extraepitopic compensatory substitutions partially restore fitness to simian immunodeficiency virus variants that escape from an immunodominant cytotoxic-T-lymphocyte response. J. Virol. 2004, 78, 2581–2585. [Google Scholar] [CrossRef] [PubMed]
- Goulder, P.J.; Brander, C.; Tang, Y.; Tremblay, C.; Colbert, R.A.; Addo, M.M.; Rosenberg, E.S.; Nguyen, T.; Allen, R.; Trocha, A.; et al. Evolution and transmission of stable CTL escape mutations in HIV infection. Nature 2001, 412, 334–338. [Google Scholar] [CrossRef]
- Ammaranond, P.; Zaunders, J.; Satchell, C.; van Bockel, D.; Cooper, D.A.; Kelleher, A.D. A new variant cytotoxic T lymphocyte escape mutation in HLA-B27-positive individuals infected with HIV type 1. AIDS Res. Hum. Retrovir. 2005, 21, 395–397. [Google Scholar] [CrossRef]
- Das, K.; Martinez, S.E.; Arnold, E. Structural Insights into HIV Reverse Transcriptase Mutations Q151M and Q151M Complex That Confer Multinucleoside Drug Resistance. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef]
- Quiros-Roldan, E.; Bertelli, D.; Signorini, S.; Airoldi, M.; Torti, C.; Moretti, F.; Carosi, G. HIV-1 multi-dideoxynucleoside resistance mutation (Q151M): Prevalence, associated resistance mutations and response to antiretroviral salvage treatment. Microbios 2001, 106, 137–145. [Google Scholar]
- Brenner, B.G.; Coutsinos, D. The K65R mutation in HIV-1 reverse transcriptase: Genetic barriers, resistance profile and clinical implications. HIV Ther. 2009, 3, 583–594. [Google Scholar] [CrossRef]
- Parikh, U.M.; Koontz, D.L.; Chu, C.K.; Schinazi, R.F.; Mellors, J.W. In vitro activity of structurally diverse nucleoside analogs against human immunodeficiency virus type 1 with the K65R mutation in reverse transcriptase. Antimicrob. Agents Chemother. 2005, 49, 1139–1144. [Google Scholar] [CrossRef]
- Parkin, N.T.; Gupta, S.; Chappey, C.; Petropoulos, C.J. The K101P and K103R/V179D mutations in human immunodeficiency virus type 1 reverse transcriptase confer resistance to nonnucleoside reverse transcriptase inhibitors. Antimicrob. Agents Chemother. 2006, 50, 351–354. [Google Scholar] [CrossRef]
- Basson, A.E.; Rhee, S.Y.; Parry, C.M.; El-Khatib, Z.; Charalambous, S.; De Oliveira, T.; Pillay, D.; Hoffmann, C.; Katzenstein, D.; Shafer, R.W.; et al. Impact of drug resistance-associated amino acid changes in HIV-1 subtype C on susceptibility to newer nonnucleoside reverse transcriptase inhibitors. Antimicrob. Agents Chemother. 2015, 59, 960–971. [Google Scholar] [CrossRef]
- Anta, L.; Llibre, J.M.; Poveda, E.; Blanco, J.L.; Alvarez, M.; Pérez-Elías, M.J.; Aguilera, A.; Caballero, E.; Soriano, V.; de Mendoza, C. Rilpivirine resistance mutations in HIV patients failing non-nucleoside reverse transcriptase inhibitor-based therapies. Aids 2013, 27, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Wensing, A.M.; Calvez, V.; Ceccherini-Silberstein, F.; Charpentier, C.; Günthard, H.F.; Paredes, R.; Shafer, R.W.; Richman, D.D. 2019 update of the drug resistance mutations in HIV-1. Top. Antivir. Med. 2019, 27, 111–121. [Google Scholar] [PubMed]
- Clotet, B.; Ruiz, L.; Martinez-Picado, J.; Negredo, E.; Hill, A.; Popescu, M. Prevalence of HIV protease mutations on failure of nelfinavir-containing HAART: A retrospective analysis of four clinical studies and two observational cohorts. HIV Clin. Trials 2002, 3, 316–323. [Google Scholar] [PubMed]
- Tupinambás, U.; Aleixo, A.; Greco, D. HIV-1 genotypes related to failure of nelfinavir as the first protease inhibitor treatment. Braz. J. Infect. Dis. 2005, 9, 324–329. [Google Scholar] [CrossRef]
- Wainberg, M.A. The impact of the M184V substitution on drug resistance and viral fitness. Expert Rev. Anti-Infect. Ther. 2004, 2, 147–151. [Google Scholar] [CrossRef]
- Weber, J.; Chakraborty, B.; Weberova, J.; Miller, M.D.; Quiñones-Mateu, M.E. Diminished replicative fitness of primary human immunodeficiency virus type 1 isolates harboring the K65R mutation. J. Clin. Microbiol. 2005, 43, 1395–1400. [Google Scholar] [CrossRef]
- Hu, Z.; Kuritzkes, D.R. Altered viral fitness and drug susceptibility in HIV-1 carrying mutations that confer resistance to nonnucleoside reverse transcriptase and integrase strand transfer inhibitors. J. Virol. 2014, 88, 9268–9276. [Google Scholar] [CrossRef]
- Andreatta, K.N.; Goodman, D.D.; Miller, M.D.; White, K.L. Reduced viral fitness and lack of cross-class resistance with integrase strand transfer inhibitor and nucleoside reverse transcriptase inhibitor resistance mutations. Antimicrob. Agents Chemother. 2015, 59, 3441–3449. [Google Scholar] [CrossRef]
- Timm, J.; Lauer, G.M.; Kavanagh, D.G.; Sheridan, I.; Kim, A.Y.; Lucas, M.; Pillay, T.; Ouchi, K.; Reyor, L.L.; Schulze zur Wiesch, J.; et al. CD8 epitope escape and reversion in acute HCV infection. J. Exp. Med. 2004, 200, 1593–1604. [Google Scholar] [CrossRef]
- Kim, J.; De La Cruz, J.; Lam, K.; Ng, H.; Daar, E.S.; Balamurugan, A.; Yang, O.O. CD8(+) Cytotoxic T Lymphocyte Responses and Viral Epitope Escape in Acute HIV-1 Infection. Viral Immunol. 2018, 31, 525–536. [Google Scholar] [CrossRef]
- Price, D.A.; Goulder, P.J.; Klenerman, P.; Sewell, A.K.; Easterbrook, P.J.; Troop, M.; Bangham, C.R.; Phillips, R.E. Positive selection of HIV-1 cytotoxic T lymphocyte escape variants during primary infection. Proc. Natl. Acad. Sci. USA 1997, 94, 1890–1895. [Google Scholar] [CrossRef] [PubMed]
- Peyerl, F.W.; Bazick, H.S.; Newberg, M.H.; Barouch, D.H.; Sodroski, J.; Letvin, N.L. Fitness costs limit viral escape from cytotoxic T lymphocytes at a structurally constrained epitope. J. Virol. 2004, 78, 13901–13910. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shahid, A.; Olvera, A.; Anmole, G.; Kuang, X.T.; Cotton, L.A.; Plana, M.; Brander, C.; Brockman, M.A.; Brumme, Z.L. Consequences of HLA-B*13-Associated Escape Mutations on HIV-1 Replication and Nef Function. J. Virol. 2015, 89, 11557–11571. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.K.; Brumme, Z.L.; Carlson, J.M.; Heckerman, D.; Kadie, C.M.; Brumme, C.J.; Wang, B.; Losina, E.; Miura, T.; Chonco, F.; et al. Gag-protease-mediated replication capacity in HIV-1 subtype C chronic infection: Associations with HLA type and clinical parameters. J. Virol. 2010, 84, 10820–10831. [Google Scholar] [CrossRef]
- Wright, J.K.; Naidoo, V.L.; Brumme, Z.L.; Prince, J.L.; Claiborne, D.T.; Goulder, P.J.; Brockman, M.A.; Hunter, E.; Ndung’u, T. Impact of HLA-B*81-associated mutations in HIV-1 Gag on viral replication capacity. J. Virol. 2012, 86, 3193–3199. [Google Scholar] [CrossRef]
- Leslie, A.J.; Pfafferott, K.J.; Chetty, P.; Draenert, R.; Addo, M.M.; Feeney, M.; Tang, Y.; Holmes, E.C.; Allen, T.; Prado, J.G.; et al. HIV evolution: CTL escape mutation and reversion after transmission. Nat. Med. 2004, 10, 282–289. [Google Scholar] [CrossRef]
- Liu, D.; Zuo, T.; Hora, B.; Song, H.; Kong, W.; Yu, X.; Goonetilleke, N.; Bhattacharya, T.; Perelson, A.S.; Haynes, B.F.; et al. Preexisting compensatory amino acids compromise fitness costs of a HIV-1 T cell escape mutation. Retrovirology 2014, 11, 101. [Google Scholar] [CrossRef]
- Dam, E.; Quercia, R.; Glass, B.; Descamps, D.; Launay, O.; Duval, X.; Kräusslich, H.G.; Hance, A.J.; Clavel, F. Gag mutations strongly contribute to HIV-1 resistance to protease inhibitors in highly drug-experienced patients besides compensating for fitness loss. PLoS Pathog. 2009, 5, e1000345. [Google Scholar] [CrossRef]
- Nijhuis, M.; Schuurman, R.; de Jong, D.; Erickson, J.; Gustchina, E.; Albert, J.; Schipper, P.; Gulnik, S.; Boucher, C.A. Increased fitness of drug resistant HIV-1 protease as a result of acquisition of compensatory mutations during suboptimal therapy. Aids 1999, 13, 2349–2359. [Google Scholar] [CrossRef]
- Li, S.; Ouyang, J.; Zhao, B.; An, M.; Wang, L.; Ding, H.; Zhang, M.; Han, X. The S68G polymorphism is a compensatory mutation associated with the drug resistance mutation K65R in CRF01_AE strains. BMC Infect. Dis. 2020, 20, 123. [Google Scholar] [CrossRef]
- Brumme, Z.L.; Li, C.; Miura, T.; Sela, J.; Rosato, P.C.; Brumme, C.J.; Markle, T.J.; Martin, E.; Block, B.L.; Trocha, A.; et al. Reduced replication capacity of NL4-3 recombinant viruses encoding reverse transcriptase-integrase sequences from HIV-1 elite controllers. J. Acquir. Immune Defic. Syndr. 2011, 56, 100–108. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Murakoshi, H.; Koyanagi, M.; Chikata, T.; Rahman, M.A.; Kuse, N.; Sakai, K.; Gatanaga, H.; Oka, S.; Takiguchi, M. Accumulation of Pol Mutations Selected by HLA-B*52:01-C*12:02 Protective Haplotype-Restricted Cytotoxic T Lymphocytes Causes Low Plasma Viral Load Due to Low Viral Fitness of Mutant Viruses. J. Virol. 2017, 91. [Google Scholar] [CrossRef] [PubMed]
- Seki, S.; Matano, T. CTL Escape and Viral Fitness in HIV/SIV Infection. Front. Microbiol. 2011, 2, 267. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.T.; Asahchop, E.L.; Oliveira, M.; Quashie, P.K.; Quan, Y.; Brenner, B.G.; Wainberg, M.A. Compensation by the E138K mutation in HIV-1 reverse transcriptase for deficits in viral replication capacity and enzyme processivity associated with the M184I/V mutations. J. Virol. 2011, 85, 11300–11308. [Google Scholar] [CrossRef]
- Weber, J.; Henry, K.R.; Arts, E.J.; Quiñones-Mateu, M.E. Viral fitness: Relation to drug resistance mutations and mechanisms involved: Nucleoside reverse transcriptase inhibitor mutations. Curr. Opin. HIV AIDS 2007, 2, 81–87. [Google Scholar] [CrossRef]
- Cong, M.E.; Heneine, W.; García-Lerma, J.G. The fitness cost of mutations associated with human immunodeficiency virus type 1 drug resistance is modulated by mutational interactions. J. Virol. 2007, 81, 3037–3041. [Google Scholar] [CrossRef]
- Wei, X.; Liang, C.; Götte, M.; Wainberg, M.A. The M184V mutation in HIV-1 reverse transcriptase reduces the restoration of wild-type replication by attenuated viruses. Aids 2002, 16, 2391–2398. [Google Scholar] [CrossRef]
- Gonzalez, L.M.; Brindeiro, R.M.; Aguiar, R.S.; Pereira, H.S.; Abreu, C.M.; Soares, M.A.; Tanuri, A. Impact of nelfinavir resistance mutations on in vitro phenotype, fitness, and replication capacity of human immunodeficiency virus type 1 with subtype B and C proteases. Antimicrob. Agents Chemother. 2004, 48, 3552–3555. [Google Scholar] [CrossRef]
- Hsieh, S.M.; Pan, S.C.; Chang, S.Y.; Hung, C.C.; Sheng, W.H.; Chen, M.Y.; Chang, S.C. Differential impact of resistance-associated mutations to protease inhibitors and nonnucleoside reverse transcriptase inhibitors on HIV-1 replication capacity. AIDS Res. Hum. Retrovir. 2013, 29, 1117–1122. [Google Scholar] [CrossRef]
- Dykes, C.; Wu, H.; Sims, M.; Holden-Wiltse, J.; Demeter, L.M. Human immunodeficiency virus type 1 protease inhibitor drug-resistant mutants give discordant results when compared in single-cycle and multiple-cycle fitness assays. J. Clin. Microbiol. 2010, 48, 4035–4043. [Google Scholar] [CrossRef]
- Menéndez-Arias, L.; Martín-Alonso, S.; Frutos-Beltrán, E. An Update on Antiretroviral Therapy. Adv. Exp. Med. Biol. 2021, 1322, 31–61. [Google Scholar] [PubMed]
- Xu, H.T.; Martinez-Cajas, J.L.; Ntemgwa, M.L.; Coutsinos, D.; Frankel, F.A.; Brenner, B.G.; Wainberg, M.A. Effects of the K65R and K65R/M184V reverse transcriptase mutations in subtype C HIV on enzyme function and drug resistance. Retrovirology 2009, 6, 14. [Google Scholar] [CrossRef] [PubMed]
- Brenner, B.G.; Oliveira, M.; Doualla-Bell, F.; Moisi, D.D.; Ntemgwa, M.; Frankel, F.; Essex, M.; Wainberg, M.A. HIV-1 subtype C viruses rapidly develop K65R resistance to tenofovir in cell culture. Aids 2006, 20, F9–F13. [Google Scholar] [CrossRef] [PubMed]
- Deval, J.; Navarro, J.M.; Selmi, B.; Courcambeck, J.; Boretto, J.; Halfon, P.; Garrido-Urbani, S.; Sire, J.; Canard, B. A loss of viral replicative capacity correlates with altered DNA polymerization kinetics by the human immunodeficiency virus reverse transcriptase bearing the K65R and L74V dideoxynucleoside resistance substitutions. J. Biol. Chem. 2004, 279, 25489–25496. [Google Scholar] [CrossRef]
- Deval, J.; White, K.L.; Miller, M.D.; Parkin, N.T.; Courcambeck, J.; Halfon, P.; Selmi, B.; Boretto, J.; Canard, B. Mechanistic basis for reduced viral and enzymatic fitness of HIV-1 reverse transcriptase containing both K65R and M184V mutations. J. Biol. Chem. 2004, 279, 509–516. [Google Scholar] [CrossRef]
- Lloyd, S.B.; Lichtfuss, M.; Amarasena, T.H.; Alcantara, S.; De Rose, R.; Tachedjian, G.; Alinejad-Rokny, H.; Venturi, V.; Davenport, M.P.; Winnall, W.R.; et al. High fidelity simian immunodeficiency virus reverse transcriptase mutants have impaired replication in vitro and in vivo. Virology 2016, 492, 1–10. [Google Scholar] [CrossRef]
- Harrigan, P.R.; Stone, C.; Griffin, P.; Nájera, I.; Bloor, S.; Kemp, S.; Tisdale, M.; Larder, B. Resistance profile of the human immunodeficiency virus type 1 reverse transcriptase inhibitor abacavir (1592U89) after monotherapy and combination therapy. CNA2001 Investigative Group. J. Infect. Dis. 2000, 181, 912–920. [Google Scholar] [CrossRef]
- Paredes, R.; Sagar, M.; Marconi, V.C.; Hoh, R.; Martin, J.N.; Parkin, N.T.; Petropoulos, C.J.; Deeks, S.G.; Kuritzkes, D.R. In vivo fitness cost of the M184V mutation in multidrug-resistant human immunodeficiency virus type 1 in the absence of lamivudine. J. Virol. 2009, 83, 2038–2043. [Google Scholar] [CrossRef]
- Bleiber, G.; Munoz, M.; Ciuffi, A.; Meylan, P.; Telenti, A. Individual contributions of mutant protease and reverse transcriptase to viral infectivity, replication, and protein maturation of antiretroviral drug-resistant human immunodeficiency virus type 1. J. Virol. 2001, 75, 3291–3300. [Google Scholar] [CrossRef]
- Wagner, B.G.; Garcia-Lerma, J.G.; Blower, S. Factors limiting the transmission of HIV mutations conferring drug resistance: Fitness costs and genetic bottlenecks. Sci. Rep. 2012, 2, 320. [Google Scholar] [CrossRef]
- Frankel, F.A.; Invernizzi, C.F.; Oliveira, M.; Wainberg, M.A. Diminished efficiency of HIV-1 reverse transcriptase containing the K65R and M184V drug resistance mutations. AIDS 2007, 21, 665–675. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Breitschwerdt, S.; Grandel, B.; Asbach, B.; Winter, F.; Allen, T.; Wagner, R.; Salzberger, B.; Schneidewind, A. Consensus Sequences for Gag and Pol Introduced into HIV-1 Clade B Laboratory Strains Differentially Influence the Impact of Point Mutations Associated with Immune Escape and with Drug Resistance on Viral Replicative Capacity. Viruses 2025, 17, 842. https://doi.org/10.3390/v17060842
Breitschwerdt S, Grandel B, Asbach B, Winter F, Allen T, Wagner R, Salzberger B, Schneidewind A. Consensus Sequences for Gag and Pol Introduced into HIV-1 Clade B Laboratory Strains Differentially Influence the Impact of Point Mutations Associated with Immune Escape and with Drug Resistance on Viral Replicative Capacity. Viruses. 2025; 17(6):842. https://doi.org/10.3390/v17060842
Chicago/Turabian StyleBreitschwerdt, Sven, Benedikt Grandel, Benedikt Asbach, Franziska Winter, Todd Allen, Ralf Wagner, Bernd Salzberger, and Arne Schneidewind. 2025. "Consensus Sequences for Gag and Pol Introduced into HIV-1 Clade B Laboratory Strains Differentially Influence the Impact of Point Mutations Associated with Immune Escape and with Drug Resistance on Viral Replicative Capacity" Viruses 17, no. 6: 842. https://doi.org/10.3390/v17060842
APA StyleBreitschwerdt, S., Grandel, B., Asbach, B., Winter, F., Allen, T., Wagner, R., Salzberger, B., & Schneidewind, A. (2025). Consensus Sequences for Gag and Pol Introduced into HIV-1 Clade B Laboratory Strains Differentially Influence the Impact of Point Mutations Associated with Immune Escape and with Drug Resistance on Viral Replicative Capacity. Viruses, 17(6), 842. https://doi.org/10.3390/v17060842




