Construction of Minigenome Replicon of Nipah Virus and Investigation of Biological Activity
Abstract
1. Introduction
2. Materials and Methods
2.1. Plasmid Constructions
2.2. Cell Culture
2.3. Plasmid Transfection and Measurement of Reporter Gene Expression
2.4. Luciferase Assay
2.5. RNA Isolation, RT-PCR, and RNA Quantification
2.6. Gene Silencing with siRNAs
2.7. Interferon Treatment
2.8. Drug Treatment
2.9. Confocal Fluorescence Microscope
2.10. Fluorescence Recovery After Photobleaching
2.11. Live Cell Imaging
2.12. Sensitivity of IBs to 1,6-Hexanediol Treatment
2.13. Statistical Analysis
3. Results
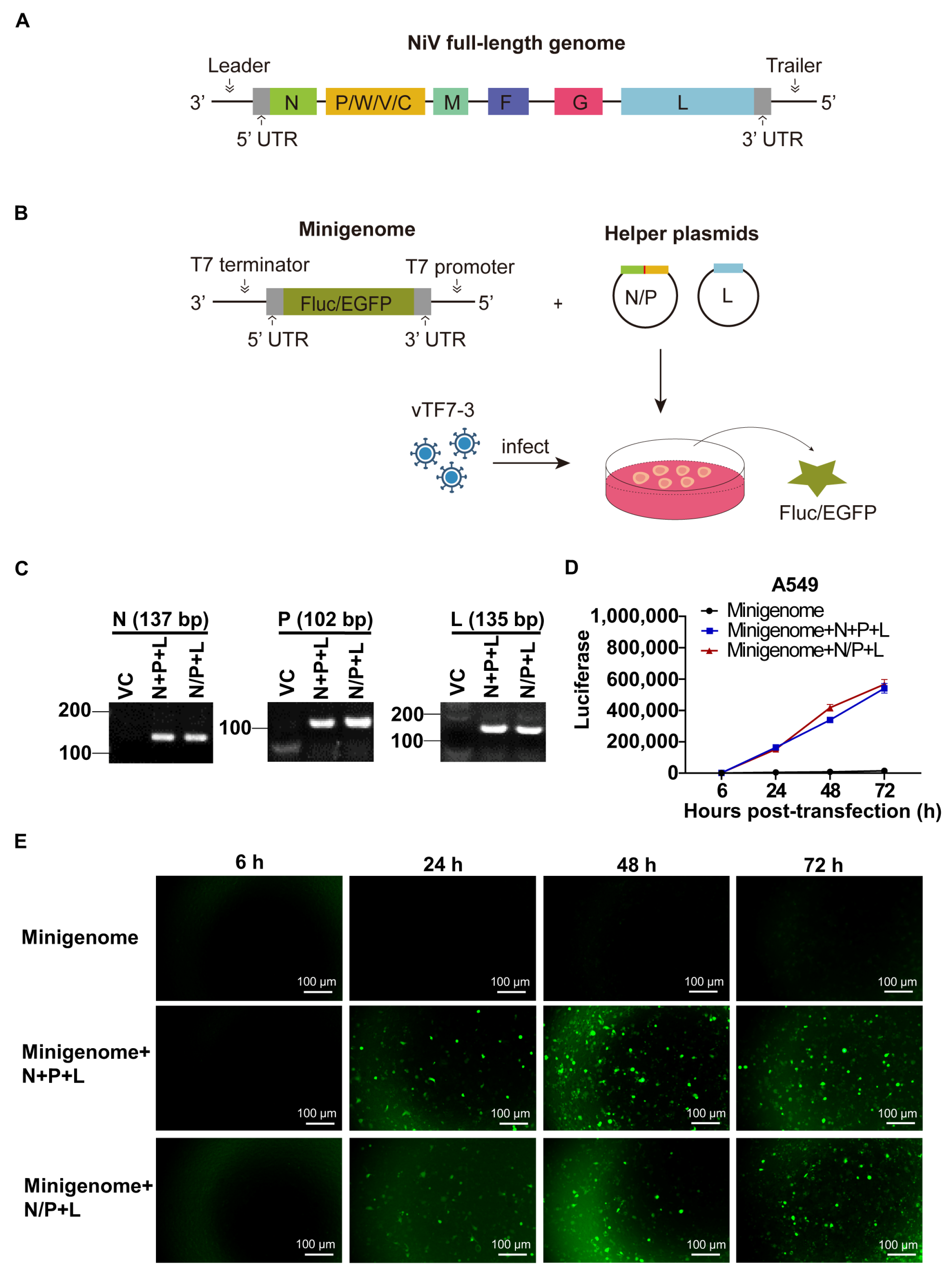
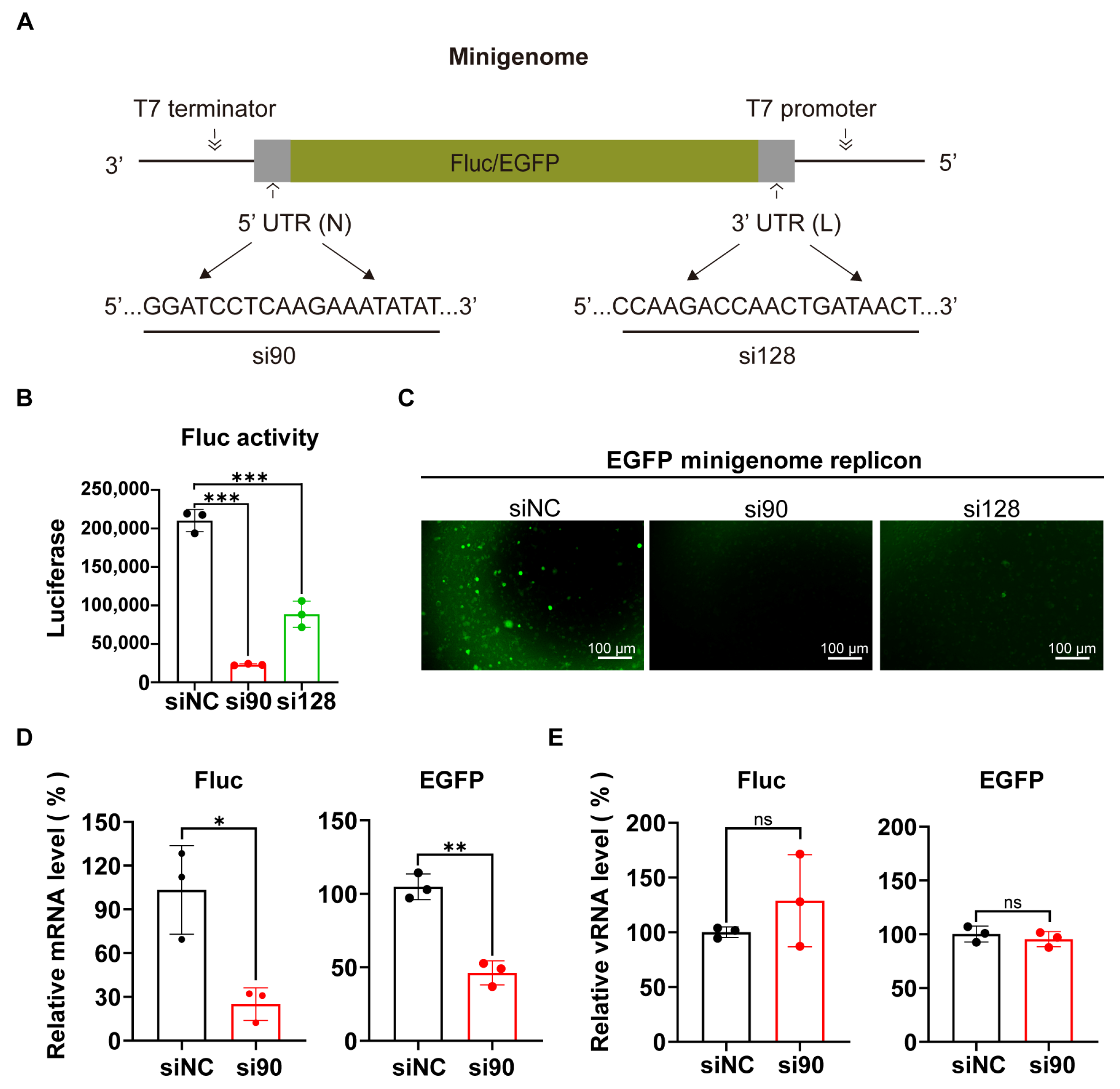
3.1. Generation of the NiV Minigenome Replicon
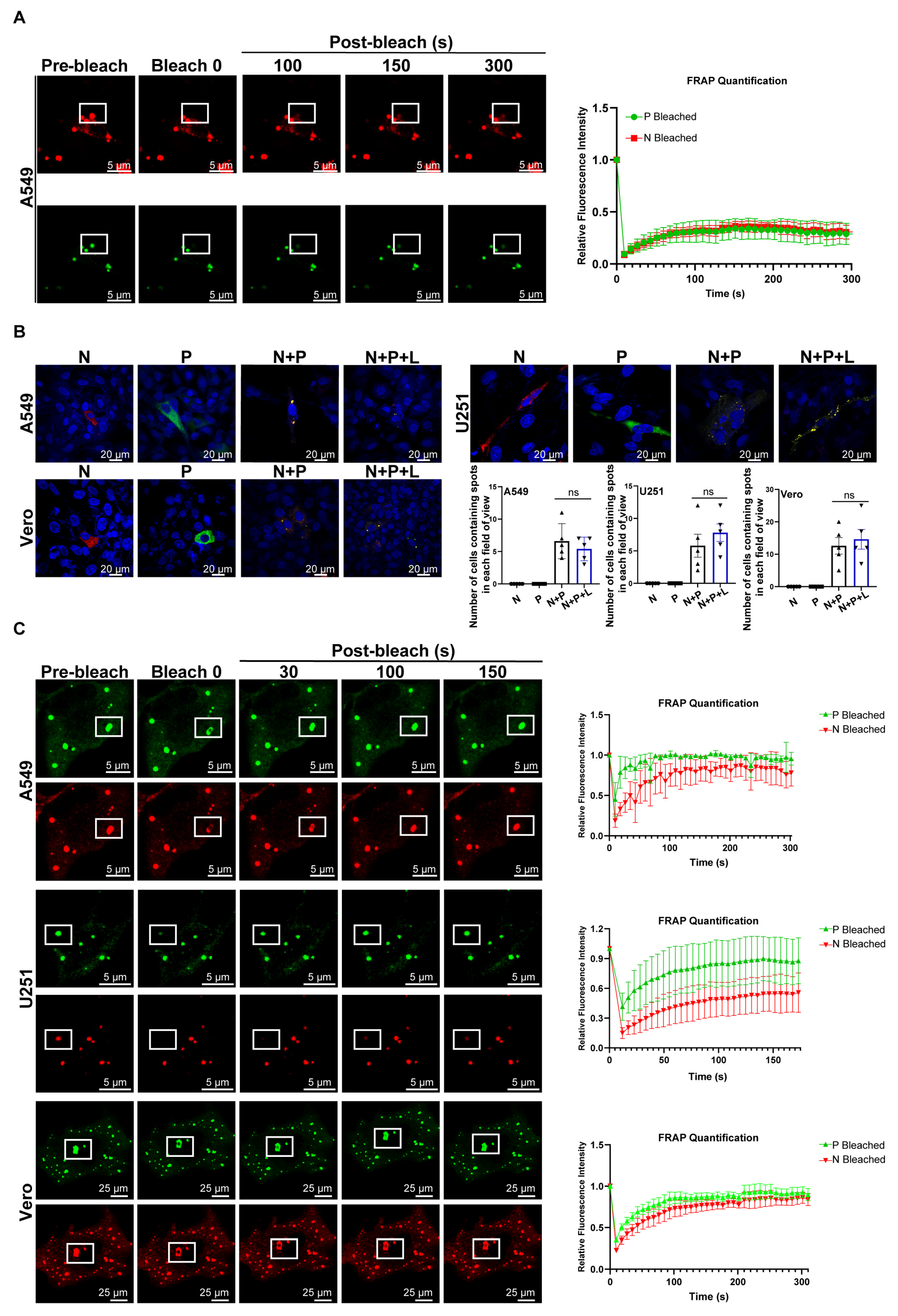
3.2. LLPS Drives the Formation of NiV IB-like Structures
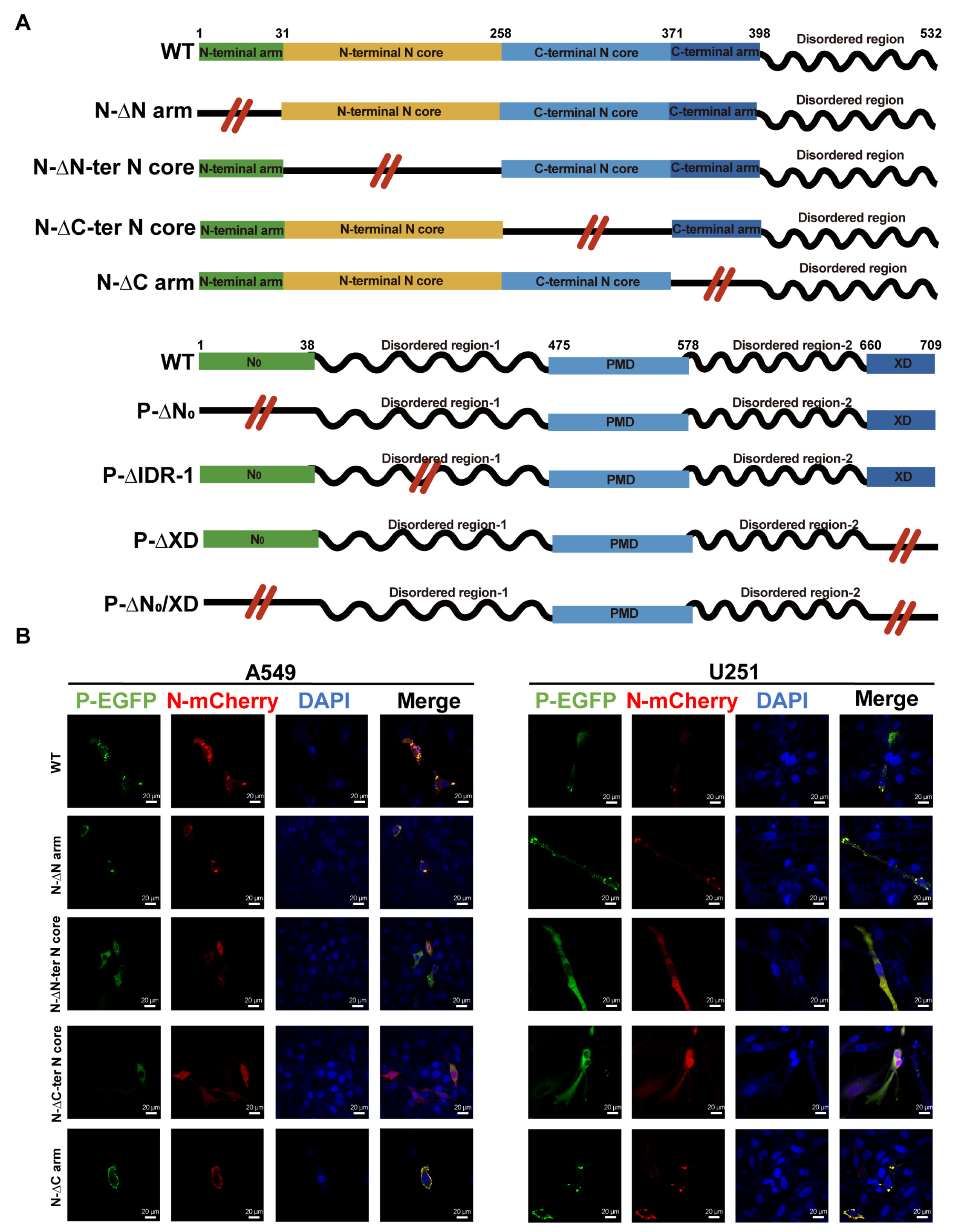
3.3. Identification of the Domains of P and N Required for the Morphogenesis of IBs
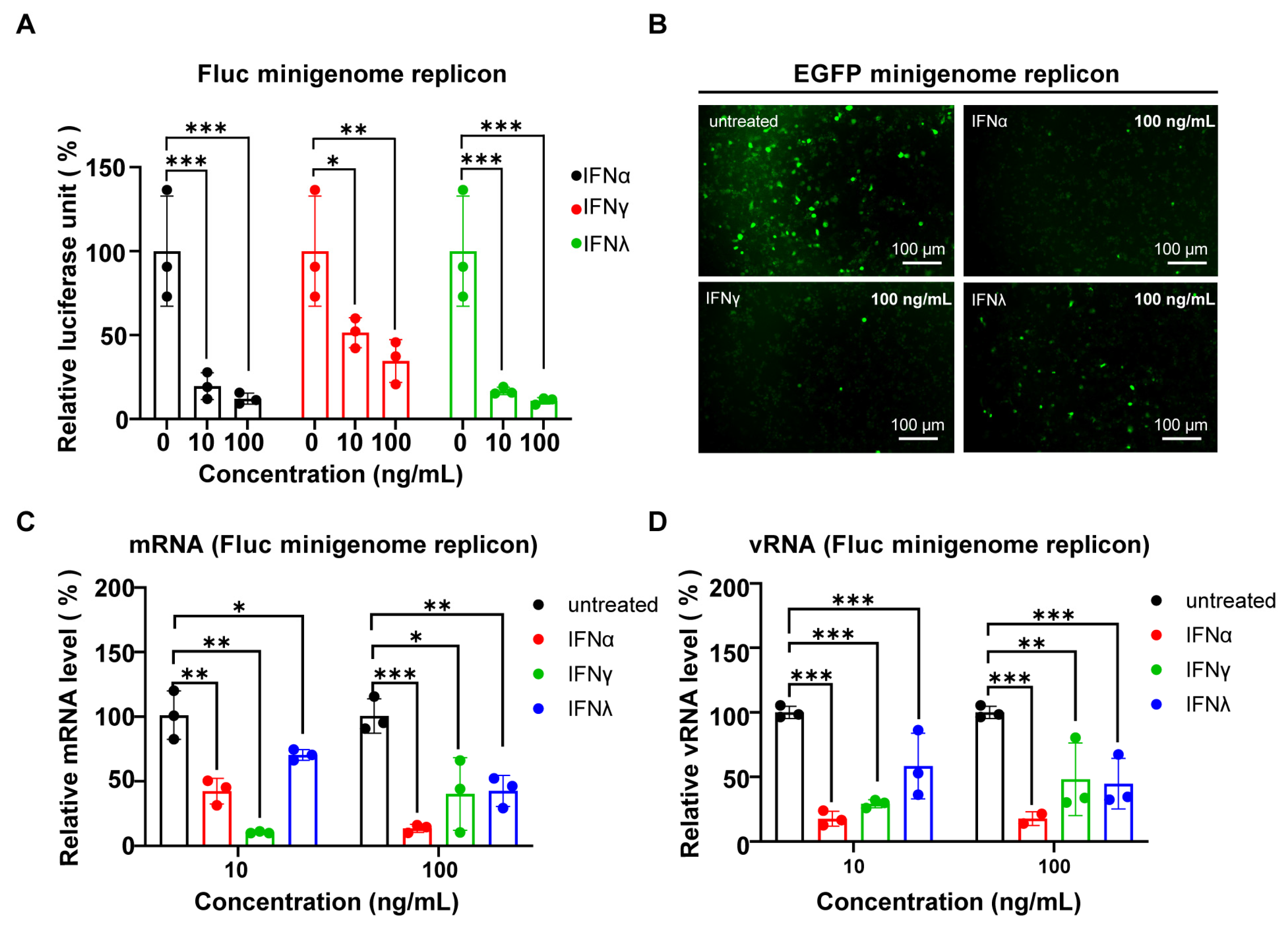
3.4. The NiV Minigenome Replicon Is Sensitive to RNA Interference and Interferons
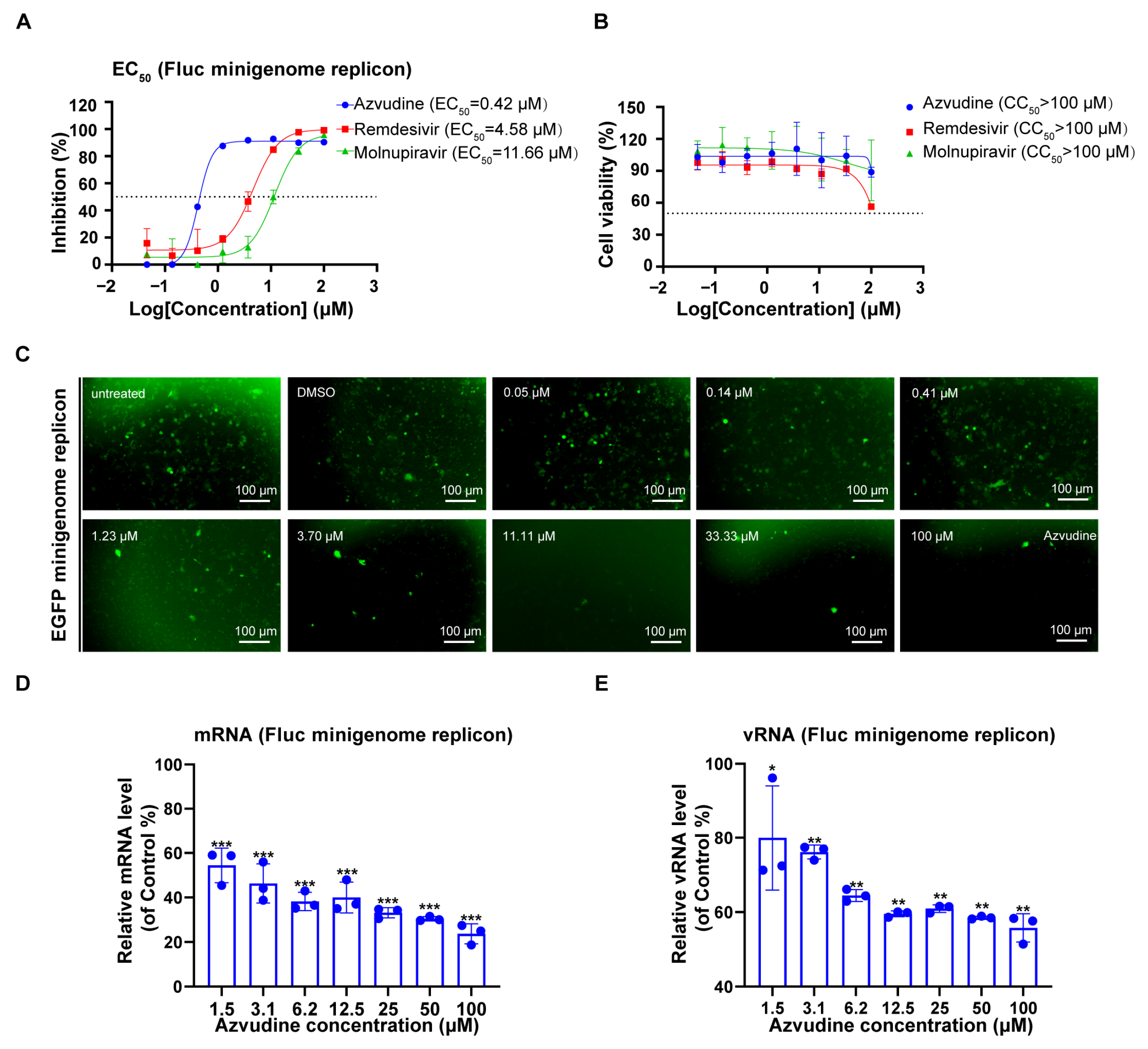
3.5. Evaluation of Antiviral Drugs Using NiV Minigenome Replicon
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NiV | Nipah virus |
| RSV | Respiratory syncytial virus |
| EBOV | Ebola virus |
| MARV | Marburg virus |
| MeV | Measles virus |
| vTF7-3 | Recombinant vaccinia virus expressing bacteriophage T7 polymerase |
| BSL-4 | Biosafety level 4 |
| BSL-2 | Biosafety level 2 |
| Fluc | Firefly luciferase |
| EGFP | Enhanced green fluorescent protein |
| IDR | Intrinsically disordered region |
| LLPS | Liquid–liquid phase separation |
| UTR | Untranslated region |
| CAT | Chloramphenicol acetyltransferase |
| CV-1 | African green monkey kidney fibroblast cells |
| IBs | Inclusion bodies |
| vRNPs | Viral ribonucleoproteins |
| RNP | Ribonucleoprotein |
| RdRp | RNA-dependent RNA polymerase |
| P2A | Porcine teschovirus-1 2A peptide |
| RT-qPCR | Reverse transcription quantitative polymerase chain reaction |
| FRAP | Fluorescence recovery after photobleaching |
| 1,6-HD | 1,6-hexanediol |
| IFN | Interferon |
| RNAi | RNA interference |
| EC50 | Half-maximal effective concentration |
| CC50 | Half-maximal cytotoxic concentration |
| ANOVA | Analysis of variance |
References
- Moore, K.A.; Mehr, A.J.; Ostrowsky, J.T.; Ulrich, A.K.; Moua, N.M.; Fay, P.C.; Hart, P.J.; Golding, J.P.; Benassi, V.; Preziosi, M.P.; et al. Measures to prevent and treat Nipah virus disease: Research priorities for 2024-29. Lancet Infect. Dis. 2024, 24, e707–e717. [Google Scholar] [CrossRef]
- Chua, K.B.; Goh, K.J.; Wong, K.T.; Kamarulzaman, A.; Tan, P.S.; Ksiazek, T.G.; Zaki, S.R.; Paul, G.; Lam, S.K.; Tan, C.T. Fatal encephalitis due to Nipah virus among pig-farmers in Malaysia. Lancet 1999, 354, 1257–1259. [Google Scholar] [CrossRef]
- Angeletti, S.; Lo Presti, A.; Cella, E.; Ciccozzi, M. Molecular epidemiology and phylogeny of Nipah virus infection: A mini review. Asian Pac. J. Trop. Med. 2016, 9, 630–634. [Google Scholar] [CrossRef]
- Wang, Y.; Fan, L.; Ye, P.; Wang, Z.; Liang, C.; Liu, Q.; Yang, X.; Long, Z.; Shi, W.; Zhou, Y.; et al. Novel transcription and replication-competent virus-like particles system modelling the Nipah virus life cycle. Emerg. Microbes Infect. 2024, 13, 2368217. [Google Scholar] [CrossRef]
- Peng, Q.; Dong, Y.; Jia, M.; Liu, Q.; Bi, Y.; Qi, J.; Shi, Y. Cryo-EM structure of Nipah virus L-P polymerase complex. Nat. Commun. 2024, 15, 10524. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, L.; Zhang, Y.; Wang, Y.; Tang, J.; Liu, S.; Gao, H.; Zhang, X.; Zinzula, L.; Kornberg, R.D.; et al. Cryo-EM structure of Nipah virus RNA polymerase complex. Sci. Adv. 2024, 10, eadr7116. [Google Scholar] [CrossRef]
- Hu, S.; Kim, H.; Yang, P.; Yu, Z.; Ludeke, B.; Mobilia, S.; Pan, J.; Stratton, M.; Bian, Y.; Fearns, R.; et al. Structural and functional analysis of the Nipah virus polymerase complex. Cell 2025, 188, 688–703.e618. [Google Scholar] [CrossRef]
- Ang, L.T.; Nguyen, A.T.; Liu, K.J.; Chen, A.; Xiong, X.; Curtis, M.; Martin, R.M.; Raftry, B.C.; Ng, C.Y.; Vogel, U.; et al. Generating human artery and vein cells from pluripotent stem cells highlights the arterial tropism of Nipah and Hendra viruses. Cell 2022, 185, 2523–2541.e2530. [Google Scholar] [CrossRef]
- Vallbracht, M.; Bodmer, B.S.; Fischer, K.; Makroczyova, J.; Winter, S.L.; Wendt, L.; Wachsmuth-Melm, M.; Hoenen, T.; Chlanda, P. Nucleocapsid assembly drives Ebola viral factory maturation and dispersion. Cell 2025, 188, 704–720.e717. [Google Scholar] [CrossRef]
- Kortepeter, M.G.; Dierberg, K.; Shenoy, E.S.; Cieslak, T.J. Marburg virus disease: A summary for clinicians. Int. J. Infect. Dis. 2020, 99, 233–242. [Google Scholar] [CrossRef]
- Ke, X.; Ye, C.; Liu, R.; Liu, F.; Chen, Q. Establishment of a novel minigenome system for the identification of drugs targeting Nipah virus replication. J. Gen. Virol. 2024, 105, 001944. [Google Scholar] [CrossRef]
- Tao, W.; Gan, T.; Guo, M.; Xu, Y.; Zhong, J. Novel Stable Ebola Virus Minigenome Replicon Reveals Remarkable Stability of the Viral Genome. J. Virol. 2017, 91, 10-1128. [Google Scholar] [CrossRef]
- Su, J.; Dou, Y.; You, Y.; Cai, X. Application of minigenome technology in virology research of the Paramyxoviridae family. J. Microbiol. Immunol. Infect. 2015, 48, 123–129. [Google Scholar] [CrossRef]
- Halpin, K.; Bankamp, B.; Harcourt, B.H.; Bellini, W.J.; Rota, P.A. Nipah virus conforms to the rule of six in a minigenome replication assay. J. Gen. Virol. 2004, 85, 701–707. [Google Scholar] [CrossRef]
- Netherton, C.L.; Wileman, T. Virus factories, double membrane vesicles and viroplasm generated in animal cells. Curr. Opin. Virol. 2011, 1, 381–387. [Google Scholar] [CrossRef]
- Novoa, R.R.; Calderita, G.; Arranz, R.; Fontana, J.; Granzow, H.; Risco, C. Virus factories: Associations of cell organelles for viral replication and morphogenesis. Biol. Cell 2005, 97, 147–172. [Google Scholar] [CrossRef]
- Nikolic, J.; Le Bars, R.; Lama, Z.; Scrima, N.; Lagaudrière-Gesbert, C.; Gaudin, Y.; Blondel, D. Negri bodies are viral factories with properties of liquid organelles. Nat. Commun. 2017, 8, 58. [Google Scholar] [CrossRef]
- Dolnik, O.; Stevermann, L.; Kolesnikova, L.; Becker, S. Marburg virus inclusions: A virus-induced microcompartment and interface to multivesicular bodies and the late endosomal compartment. Eur. J. Cell Biol. 2015, 94, 323–331. [Google Scholar] [CrossRef]
- Risso-Ballester, J.; Rameix-Welti, M.A. Spatial resolution of virus replication: RSV and cytoplasmic inclusion bodies. Adv. Virus Res. 2023, 116, 1–43. [Google Scholar] [CrossRef]
- Risso-Ballester, J.; Galloux, M.; Cao, J.; Le Goffic, R.; Hontonnou, F.; Jobart-Malfait, A.; Desquesnes, A.; Sake, S.M.; Haid, S.; Du, M.; et al. A condensate-hardening drug blocks RSV replication in vivo. Nature 2021, 595, 596–599. [Google Scholar] [CrossRef]
- Zhou, Y.; Su, J.M.; Samuel, C.E.; Ma, D. Measles Virus Forms Inclusion Bodies with Properties of Liquid Organelles. J. Virol. 2019, 93, 10-1128. [Google Scholar] [CrossRef]
- Wu, C.; Wagner, N.D.; Moyle, A.B.; Feng, A.; Sharma, N.; Stubbs, S.H.; Donahue, C.; Davey, R.A.; Gross, M.L.; Leung, D.W.; et al. Disruption of Ebola NP(0)VP35 Inclusion Body-like Structures reduce Viral Infection. J. Mol. Biol. 2023, 435, 168241. [Google Scholar] [CrossRef]
- Ringel, M.; Heiner, A.; Behner, L.; Halwe, S.; Sauerhering, L.; Becker, N.; Dietzel, E.; Sawatsky, B.; Kolesnikova, L.; Maisner, A. Nipah virus induces two inclusion body populations: Identification of novel inclusions at the plasma membrane. PLoS Pathog. 2019, 15, e1007733. [Google Scholar] [CrossRef]
- Uebelhoer, L.S.; Albariño, C.G.; McMullan, L.K.; Chakrabarti, A.K.; Vincent, J.P.; Nichol, S.T.; Towner, J.S. High-throughput, luciferase-based reverse genetics systems for identifying inhibitors of Marburg and Ebola viruses. Antiviral Res. 2014, 106, 86–94. [Google Scholar] [CrossRef]
- Ker, D.S.; Jenkins, H.T.; Greive, S.J.; Antson, A.A. CryoEM structure of the Nipah virus nucleocapsid assembly. PLoS Pathog. 2021, 17, e1009740. [Google Scholar] [CrossRef]
- Bruhn, J.F.; Hotard, A.L.; Spiropoulou, C.F.; Lo, M.K.; Saphire, E.O. A Conserved Basic Patch and Central Kink in the Nipah Virus Phosphoprotein Multimerization Domain Are Essential for Polymerase Function. Structure 2019, 27, 660–668.e664. [Google Scholar] [CrossRef]
- Hannemann, H. Viral replicons as valuable tools for drug discovery. Drug Discov. Today 2020, 25, 1026–1033. [Google Scholar] [CrossRef]
- Fearns, R.; Peeples, M.E.; Collins, P.L. Increased expression of the N protein of respiratory syncytial virus stimulates minigenome replication but does not alter the balance between the synthesis of mRNA and antigenome. Virology 1997, 236, 188–201. [Google Scholar] [CrossRef]
- Sleeman, K.; Bankamp, B.; Hummel, K.B.; Lo, M.K.; Bellini, W.J.; Rota, P.A. The C, V and W proteins of Nipah virus inhibit minigenome replication. J. Gen. Virol. 2008, 89, 1300–1308. [Google Scholar] [CrossRef]
- Ali Syeda, Z.; Langden, S.S.S.; Munkhzul, C.; Lee, M.; Song, S.J. Regulatory Mechanism of MicroRNA Expression in Cancer. Int. J. Mol. Sci. 2020, 21, 1723. [Google Scholar] [CrossRef]
- Hino, K.; Sato, H.; Sugai, A.; Kato, M.; Yoneda, M.; Kai, C. Downregulation of Nipah virus N mRNA occurs through interaction between its 3’ untranslated region and hnRNP D. J. Virol. 2013, 87, 6582–6588. [Google Scholar] [CrossRef]
- Uchida, S.; Sato, H.; Yoneda, M.; Kai, C. Eukaryotic elongation factor 1-beta interacts with the 5’ untranslated region of the M gene of Nipah virus to promote mRNA translation. Arch. Virol. 2016, 161, 2361–2368. [Google Scholar] [CrossRef]
- Bitko, V.; Barik, S. Phenotypic silencing of cytoplasmic genes using sequence-specific double-stranded short interfering RNA and its application in the reverse genetics of wild type negative-strand RNA viruses. BMC Microbiol. 2001, 1, 34. [Google Scholar] [CrossRef]
- Cullen, B.R. RNA Interference in Mammals: The Virus Strikes Back. Immunity 2017, 46, 970–972. [Google Scholar] [CrossRef]
- Dhondt, K.P.; Mathieu, C.; Chalons, M.; Reynaud, J.M.; Vallve, A.; Raoul, H.; Horvat, B. Type I interferon signaling protects mice from lethal henipavirus infection. J. Infect. Dis. 2013, 207, 142–151. [Google Scholar] [CrossRef]
- Sauerhering, L.; Müller, H.; Behner, L.; Elvert, M.; Fehling, S.K.; Strecker, T.; Maisner, A. Variability of interferon-λ induction and antiviral activity in Nipah virus infected differentiated human bronchial epithelial cells of two human donors. J. Gen. Virol. 2017, 98, 2447–2453. [Google Scholar] [CrossRef]
- Aleem, A.; Kothadia, J.P. Remdesivir. In StatPearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2025. [Google Scholar]
- Su, J.M.; Wilson, M.Z.; Samuel, C.E.; Ma, D. Formation and Function of Liquid-Like Viral Factories in Negative-Sense Single-Stranded RNA Virus Infections. Viruses 2021, 13, 126. [Google Scholar] [CrossRef]
- Brangwynne, C.P.; Eckmann, C.R.; Courson, D.S.; Rybarska, A.; Hoege, C.; Gharakhani, J.; Jülicher, F.; Hyman, A.A. Germline P granules are liquid droplets that localize by controlled dissolution/condensation. Science 2009, 324, 1729–1732. [Google Scholar] [CrossRef]
- Dolnik, O.; Gerresheim, G.K.; Biedenkopf, N. New Perspectives on the Biogenesis of Viral Inclusion Bodies in Negative-Sense RNA Virus Infections. Cells 2021, 10, 1460. [Google Scholar] [CrossRef]
- Jalihal, A.P.; Pitchiaya, S.; Xiao, L.; Bawa, P.; Jiang, X.; Bedi, K.; Parolia, A.; Cieslik, M.; Ljungman, M.; Chinnaiyan, A.M.; et al. Multivalent Proteins Rapidly and Reversibly Phase-Separate upon Osmotic Cell Volume Change. Mol. Cell 2020, 79, 978–990.e975. [Google Scholar] [CrossRef]
- Jalihal, A.P.; Schmidt, A.; Gao, G.; Little, S.R.; Pitchiaya, S.; Walter, N.G. Hyperosmotic phase separation: Condensates beyond inclusions, granules and organelles. J. Biol. Chem. 2021, 296, 100044. [Google Scholar] [CrossRef] [PubMed]
- Tan, X.; Cai, K.; Li, J.; Yuan, Z.; Chen, R.; Xiao, H.; Xu, C.; Hu, B.; Qin, Y.; Ding, B. Coronavirus subverts ER-phagy by hijacking FAM134B and ATL3 into p62 condensates to facilitate viral replication. Cell Rep. 2023, 42, 112286. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Pan, T.; Zhou, M.; Chen, T.; Wu, S.; Lv, X.; Liu, J.; Yu, F.; Guan, Y.; Liu, B.; et al. CBX4 contributes to HIV-1 latency by forming phase-separated nuclear bodies and SUMOylating EZH2. EMBO Rep. 2022, 23, e53855. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Sridharan, S.; Zagoriy, I.; Eugster Oegema, C.; Ching, C.; Pflaesterer, T.; Fung, H.K.H.; Becher, I.; Poser, I.; Müller, C.W.; et al. Molecular mechanisms of stress-induced reactivation in mumps virus condensates. Cell 2023, 186, 1877–1894.e1827. [Google Scholar] [CrossRef]

| Primer | Sequence (5′-3′) |
|---|---|
| N-mCherry-F | GGCCGACGTGGGAAGCGGAAGCGGAAGCATGGTGAGCAAGGGCGAGG |
| N-mCherry-R | TTACTTATCGTCGTCATCCTTGTAATCCTTGTACAGCTCGTCCATGCC |
| P-EGFP-F | CGGTAACATCGGAAGCGGAAGCGGAAGCATGGTGAGCAAGGGCGAG |
| P-EGFP-R | GGCATGGACGAGCTGTACAAGGATTACAAGGATGACGACGATAAGTAA |
| N-N-arm-del-F | ACCACCAAGATCCGGATCT |
| N-N-arm-del-R | AATTCTTTGCCAAAATGATGAGACAGCAC |
| N-N-Core-del-F | GTGGAGGAGACCGGCAT |
| N-N-Core-del-R | CGCCACCGCCACCCTG |
| N-C-Core-del-F | GGGGGGATTGACCAGAACATGG |
| N-C-Core-del-R | GGGGGGATTGACCAGAACATGG |
| N-C-arm-del-F | ACCAGCGCCGGGAGACAGG |
| N-C-arm-del-R | GTGATGCCTGGCGCTCTTCT |
| P-N0-del-F | AAGGACCAGACCAAGGCTTGG |
| P-N0-del-R | TGCTGTCTCATCATTTTGGCAAAGAATT |
| P-IDR1-del-F | TGCTGTCTCATCATTTTGGCAAAGAATT |
| P-IDR1-del-R | ATCCATCCAGCAGCCAAGCATC |
| P-XD-del-F | GGAAGCGGAAGCGGAAGC |
| P-XD-del-R | GGAAGCGGAAGCGGAAGC |
| Target | Primer | Sequence (5′-3′) |
|---|---|---|
| N | N-qPCR-F | GACATCTTCGAGGAGGCCGCCTCCT |
| N-qPCR-R | TCCCACCTCAGCTCGGGGCTATTGGT | |
| P | P-qPCR-F | GCTGGTGAACGACGGTCTGAAC |
| P-qPCR-R | TTGATGCTTGGCTGCTGGATGG | |
| L | L-qPCR-F | ACCACAAGTACCGCCGCATTG |
| L-qPCR-R | GCATCATGGAGCCACTACCTTCAC |
| Primer | Sequence (5′-3′) |
|---|---|
| vRNA-F | GGCCGTCATGGTGGCGAAT |
| vRNA-EGFP-tag | GGCCGTCATGGTGGCGAATACGTAAACGGCCACAAGTTC |
| vRNA-Fluc-tag | GGCCGTCATGGTGGCGAATGACAAGGATGGATGGCTACATTCTG |
| EGFP-R | AAGTCGTGCTGCTTCATGTG |
| vFluc-R | GGGTGTTGGAGCAAGATGGATTC |
| mRNA-tag | CCAGATCGTTCGAGTCGT |
| mRNA-R | CCAGATCGTTCGAGTCGT |
| mFluc-F | CCCACAACCTCGTTCTACCTAAG |
| mEGFP-F | TTCAGCACGACGAAGTACAC |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, F.; Chen, R.; Zhong, J.; Zhou, A.; Peng, R.; Xue, B.; Zhou, Y.; Tang, J.; Chen, X.; Yang, Q. Construction of Minigenome Replicon of Nipah Virus and Investigation of Biological Activity. Viruses 2025, 17, 707. https://doi.org/10.3390/v17050707
Wang F, Chen R, Zhong J, Zhou A, Peng R, Xue B, Zhou Y, Tang J, Chen X, Yang Q. Construction of Minigenome Replicon of Nipah Virus and Investigation of Biological Activity. Viruses. 2025; 17(5):707. https://doi.org/10.3390/v17050707
Chicago/Turabian StyleWang, Fan, Ruyi Chen, Jiayi Zhong, Anqi Zhou, Ran Peng, Bao Xue, Yuan Zhou, Jielin Tang, Xinwen Chen, and Qi Yang. 2025. "Construction of Minigenome Replicon of Nipah Virus and Investigation of Biological Activity" Viruses 17, no. 5: 707. https://doi.org/10.3390/v17050707
APA StyleWang, F., Chen, R., Zhong, J., Zhou, A., Peng, R., Xue, B., Zhou, Y., Tang, J., Chen, X., & Yang, Q. (2025). Construction of Minigenome Replicon of Nipah Virus and Investigation of Biological Activity. Viruses, 17(5), 707. https://doi.org/10.3390/v17050707






