COVID-19 Disease Burden in the Omicron Variant-Dominated Endemic Phase: Insights from the ROUTINE-COV19 Study Using Real-World German Statutory Health Insurance Data
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
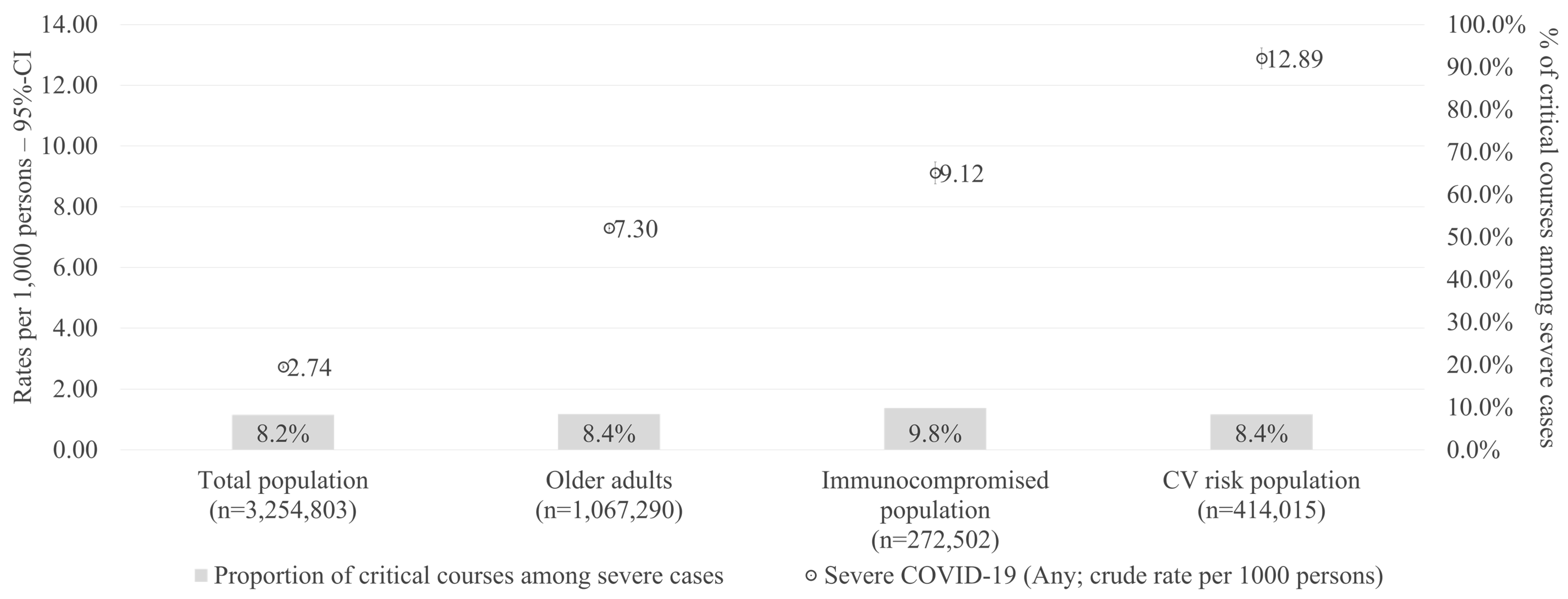
2.2. Study Population
- Older adults, defined as individuals aged 60 years or older.
- Cardiovascular (CV) risk population, defined as individuals with a CHA2DS2-VASc score ≥ 3 or those diagnosed with atrial fibrillation (ICD-10-GM: I48.0/1/2/9), coronary heart disease (ICD-10-GM: I20, I21-I22, I24, I25), or heart failure (ICD-10-GM: I50), identified by two confirmed outpatient diagnoses in two different quarters or one inpatient diagnosis using the respective ICD-10-GM codes in the 12-month pre-index period.
- Immunocompromised individuals as defined by the German Standing Committee on Vaccination (STIKO, see Supplemental Table S1 for specific conditions and code).
- Individuals suffering from other non-immunocompromising STIKO risk conditions (see Supplemental Table S1).
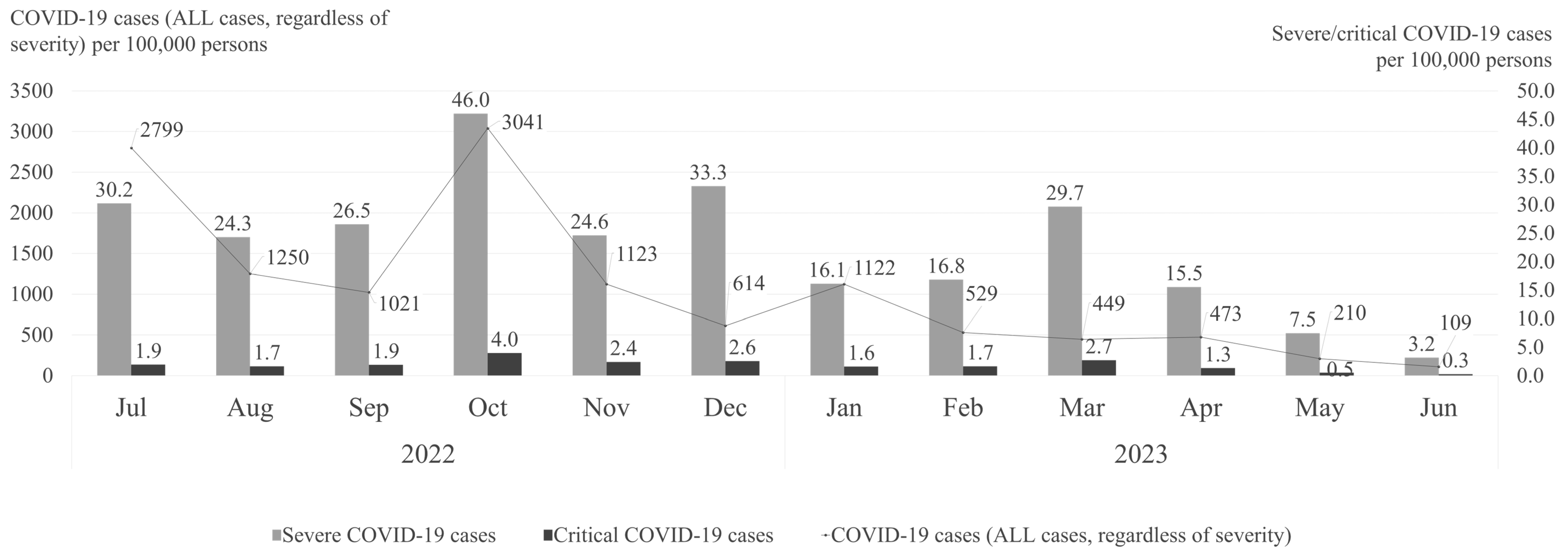
2.3. Outcomes
- Non-severe cases: COVID-19 cases that did not require hospitalization, i.e., individuals with a confirmed outpatient diagnosis of COVID-19 without subsequent hospital admission.
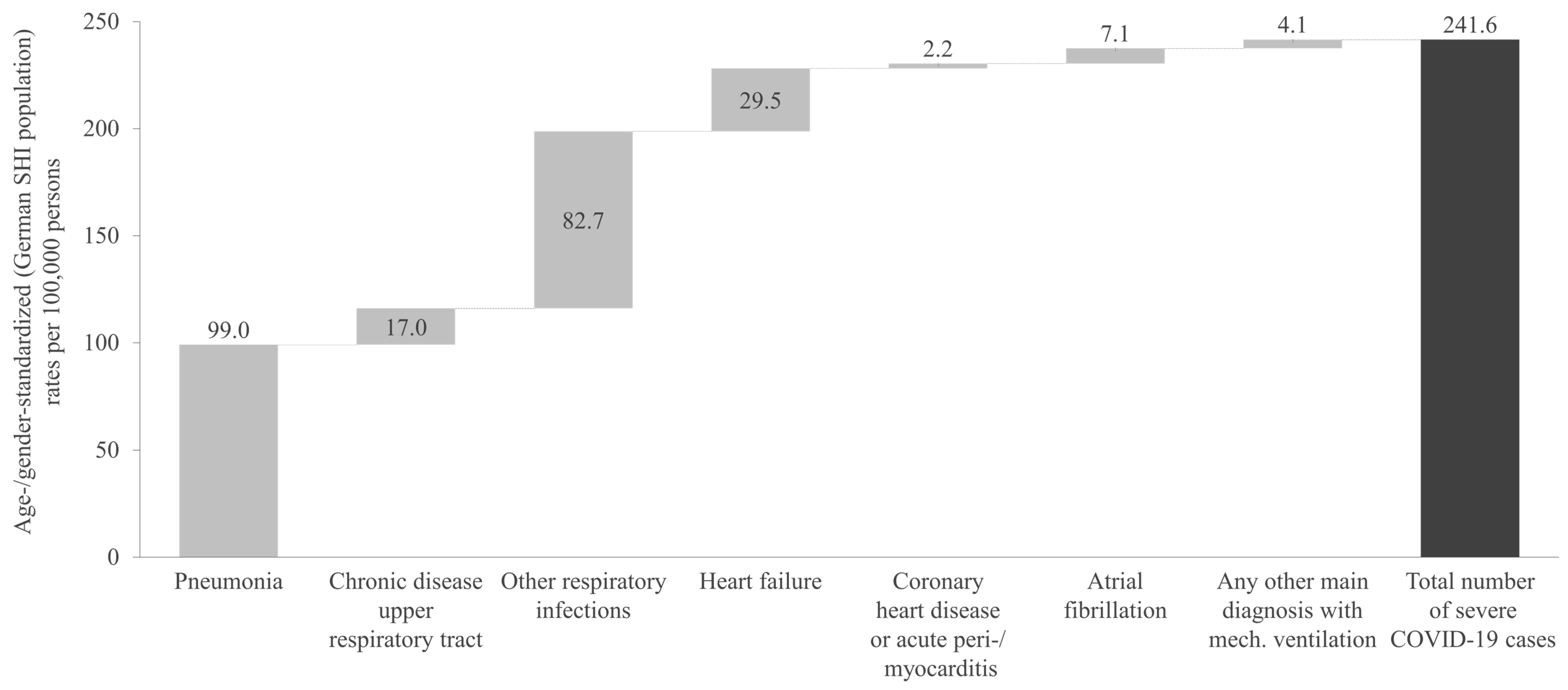
- Severe cases: Hospital admissions with a confirmed COVID-19 diagnosis (ICD-10-GM U07.1!) and at least one of the following conditions:
- ◦
- A predefined main diagnosis indicating severe disease (pneumonia, chronic disease of the lower respiratory tract, respiratory infections, heart failure, chronic heart disease, acute pericarditis/myocarditis, or atrial fibrillation; see Supplemental Table S1 for respective ICD-10-GM codes).
- ◦
- A requirement for mechanical ventilation, regardless of the main diagnosis (OPS codes 8-711, 8-712, 8-713, 8-714).
- Critical cases: A subset of severe cases that required intensive care (OPS codes 8-980, 8-97a, 8-97b, 8-98d, 8-98f, 8-712.0, 8-721.1, 8-721.2, 8-721.3).
2.4. Statistical Analysis
2.5. Regulatory Aspects
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AF | Atrial fibrillation |
| CCI | Charlson Comorbidity Index |
| CHD | Coronary heart disease |
| CI | Confidence interval |
| CNS | Central nervous system |
| COVID-19 | Coronavirus disease 2019 |
| CV | Cardiovascular |
| DRG | Diagnosis-related group |
| EBM | Einheitlicher Bewertungmaßstab (German uniform evaluation standard) |
| GP | General practitioner |
| HF | Heart failure |
| ICD-10-GM | International Classification of Disease and related health problems, 10th revision, German Modification |
| OPS | Operation and procedure classification system |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus type 2 |
| SD | Standard deviation |
| SHI | Statutory Health Insurance |
| STIKO | Ständige Impfkommission |
| WHO | World Health Organization |
| RKI | Robert Koch Institute |
| LOS | Length of stay |
| N/A | Not applicable |
References
- Farrokhi, M.; Khankeh, H.; Saatchi, M.; Hadinejad, Z.; Ahmadi-Mazhin, S.; Mohsenzadeh, Y.; Nazdik, Z.M.; Shojafard, J.; Pourvakhshoori, N.; Ahmadi, S. The Effect of the COVID-19 Pandemic on Environmental Health (Two Sides of the Same Coin): A Systematic Review. Disaster Med. Public Health Prep. 2023, 17, e499. [Google Scholar] [CrossRef] [PubMed]
- The COVID-19 Pandemic and Continuing Challenges to GLOBAL Health. Available online: https://www.who.int/about/funding/invest-in-who/investment-case-2.0/challenges (accessed on 14 October 2024).
- Pollard, C.A.; Morran, M.P.; Nestor-Kalinoski, A.L. The COVID-19 pandemic: A global health crisis. Physiol. Genom. 2020, 52, 549. [Google Scholar] [CrossRef] [PubMed]
- Machado, B.A.S.; Hodel, K.V.S.; Fonseca, L.M.D.S.; Pires, V.C.; Mascarenhas, L.A.B.; da Silva Andrade, L.P.C.; Moret, M.A.; Badaró, R. The Importance of Vaccination in the Context of the COVID-19 Pandemic: A Brief Update Regarding the Use of Vaccines. Vaccines 2022, 2022, 591. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Li, J.; Chen, Z.; Luo, Q.; Wu, X.; Ye, L.; Ni, H.; Fei, C. The global COVID-19 pandemic at a crossroads: Relevant countermeasures and ways ahead. J. Thorac. Dis. 2020, 12, 5739–5755. [Google Scholar] [CrossRef]
- Sohrabi, C.; Alsafi, Z.; O’neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef]
- Infektionsradar. Available online: https://infektionsradar.gesund.bund.de/de (accessed on 28 November 2024).
- Yang, J.; Rai, K.K.; Seif, M.; Volkman, H.R.; Ren, J.; Schmetz, A.; Gowman, H.; Massey, L.; Pather, S.; Nguyen, J.L. COVID-19-Related Work Absenteeism and Associated Lost Productivity Cost in Germany: A Population-Based Study. J. Occup. Environ. Med. 2024, 66, 514–522. [Google Scholar] [CrossRef]
- Gandjour, A. Long COVID: Costs for the German economy and health care and pension system. BMC Health Serv. Res. 2023, 23, 1–7. [Google Scholar] [CrossRef]
- Andre, M.; Lau, L.S.; Pokharel, M.D.; Ramelow, J.; Owens, F.; Souchak, J.; Akkaoui, J.; Ales, E.; Brown, H.; Shil, R.; et al. From Alpha to Omicron: How Different Variants of Concern of the SARS-Coronavirus-2 Impacted the World. Biology 2023, 12, 1267. [Google Scholar] [CrossRef]
- Karim, S.S.A.; Karim, Q.A. Omicron SARS-CoV-2 variant: A new chapter in the COVID-19 pandemic. Lancet 2021, 398, 2126–2128. [Google Scholar] [CrossRef]
- Hoffmann, M.; Krüger, N.; Schulz, S.; Cossmann, A.; Rocha, C.; Kempf, A.; Nehlmeier, I.; Graichen, L.; Moldenhauer, A.S.; Winkler, M.S.; et al. The Omicron variant is highly resistant against antibody-mediated neutralization: Implications for control of the COVID-19 pandemic. Cell 2022, 185, 447–456.e11. [Google Scholar] [CrossRef]
- Ingraham, N.E.; Ingbar, D.H. The omicron variant of SARS-CoV-2: Understanding the known and living with unknowns. Clin. Transl. Med. 2021, 11, e685. [Google Scholar] [CrossRef] [PubMed]
- Pather, S.; Madhi, S.A.; Cowling, B.J.; Moss, P.; Kamil, J.P.; Ciesek, S.; Muik, A.; Türeci, Ö. SARS-CoV-2 Omicron variants: Burden of disease, impact on vaccine effectiveness and need for variant-adapted vaccines. Front. Immunol. 2023, 14, 1130539. [Google Scholar] [CrossRef]
- Rzymski, P.; Pokorska-Śpiewak, M.; Jackowska, T.; Kuchar, E.; Nitsch-Osuch, A.; Pawłowska, M.; Babicki, M.; Jaroszewicz, J.; Szenborn, L.; Wysocki, J.; et al. Key Considerations during the Transition from the Acute Phase of the COVID-19 Pandemic: A Narrative Review. Vaccines 2023, 11, 1502. [Google Scholar] [CrossRef]
- Chatterjee, S.; Bhattacharya, M.; Nag, S.; Dhama, K.; Chakraborty, C. A Detailed Overview of SARS-CoV-2 Omicron: Its Sub-Variants, Mutations and Pathophysiology, Clinical Characteristics, Immunological Landscape, Immune Escape, and Therapies. Viruses 2023, 15, 167. [Google Scholar] [CrossRef]
- BfArM—OPS. Available online: https://www.bfarm.de/DE/Kodiersysteme/Klassifikationen/OPS-ICHI/OPS/_node.html (accessed on 1 October 2024).
- EBM—EBM-Ansicht. Available online: https://ebm.kbv.de/ (accessed on 1 October 2024).
- Chae, J.-W.; Song, C.S.; Kim, H.; Lee, K.-B.; Seo, B.-S.; Kim, D.-I. Prediction of Mortality in Patients Undergoing Maintenance Hemodialysis by Charlson Comorbidity Index Using ICD-10 Database. Nephron Clin. Pract. 2010, 117, 379–384. [Google Scholar] [CrossRef]
- Van Walraven, C.; Austin, P.C.; Jennings, A.; Quan, H.; Forster, A.J. A modification of the elixhauser comorbidity measures into a point system for hospital death using administrative data. Med. Care 2009, 47, 626–633. [Google Scholar] [CrossRef]
- van den Ham, H.A.; Klungel, O.H.; Singer, D.E.; Leufkens, H.G.; van Staa, T.P. Comparative Performance of ATRIA, CHADS2, and CHA2DS2-VASc Risk Scores Predicting Stroke in Patients With Atrial Fibrillation: Results From a National Primary Care Database. J. Am. Coll. Cardiol. 2015, 66, 1851–1859. [Google Scholar] [CrossRef]
- BAuA—Zahlen|Daten|Fakten—Volkswirtschaftliche Kosten durch Arbeitsunfähigkeit—Bundesanstalt für Arbeitsschutz und Arbeitsmedizin. Available online: https://www.baua.de/DE/Themen/Monitoring-Evaluation/Zahlen-Daten-Fakten/Kosten-der-Arbeitsunfaehigkeit (accessed on 1 October 2024).
- Townsend, J.P.; Hassler, H.B.; Lamb, A.D.; Sah, P.; Alvarez Nishio, A.; Nguyen, C.; Tew, A.D.; Galvani, A.P.; Dornburg, A. Seasonality of endemic COVID-19. mBio 2023, 14, e01426-23. [Google Scholar] [CrossRef]
- RKI. Wöchentlicher Lagebericht des RKI zur Coronavirus-Krankheit-2019 (COVID-19). Wöchentlicher Lagebericht des RKI, May 2023. Available online: https://influenza.rki.de/Wochenberichte.aspx (accessed on 15 October 2024).
- Sabatino, J.; De Rosa, S.; Di Salvo, G.; Indolfi, C. Impact of cardiovascular risk profile on COVID-19 outcome. A meta-analysis. PLoS ONE 2020, 15, e0237131. [Google Scholar] [CrossRef]
- Rezel-Potts, E.; Douiri, A.; Sun, X.; Chowienczyk, P.J.; Shah, A.M.; Gulliford, M.C. Cardiometabolic outcomes up to 12 months after COVID-19 infection. A matched cohort study in the UK. PLoS Med. 2022, 19, e1004052. [Google Scholar] [CrossRef]
- Cochrane Heart Group; Pellicori, P.; Doolub, G.; Wong, C.M.; Lee, K.S.; Mangion, K.; Ahmad, M.; Berry, C.; Squire, I.; Lambiase, P.D.; et al. COVID-19 and its cardiovascular effects: A systematic review of prevalence studies. Cochrane Database Syst. Rev. 2021. [Google Scholar] [CrossRef]
- Liu, F.; Liu, F.; Wang, L. COVID-19 and cardiovascular diseases. J. Mol. Cell Biol. 2021, 13, 161–167. [Google Scholar] [CrossRef]
- Bedekar, P.; Kearsley, A.J.; Patrone, P.N. Prevalence estimation and optimal classification methods to account for time dependence in antibody levels. J. Theor. Biol. 2023, 559, 111375. [Google Scholar] [CrossRef]
- Bedekar, P.; Luke, R.A.; Kearsley, A.J. Prevalence Estimation Methods for Time-Dependent Antibody Kinetics of Infected and Vaccinated Individuals: A Markov Chain Approach. Bull. Math. Biol. 2025, 87, 1–33. [Google Scholar] [CrossRef]
- Attaway, A.H.; Scheraga, R.G.; Bhimraj, A.; Biehl, M.; Hatipoğlu, U. Severe COVID-19 pneumonia: Pathogenesis and clinical management. BMJ 2021, 372. [Google Scholar] [CrossRef]
- Karagiannidis, C.; Mostert, C.; Hentschker, C.; Voshaar, T.; Malzahn, J.; Schillinger, G.; Klauber, J.; Janssens, U.; Marx, G.; Weber-Carstens, S.; et al. Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: An observational study. Lancet Respir. Med. 2020, 8, 853–862. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.D.; Ding, M.; Dong, X.; Zhang, J.J.; Kursat Azkur, A.; Azkur, D.; Gan, H.; Sun, Y.L.; Fu, W.; Li, W.; et al. Risk factors for severe and critically ill COVID-19 patients: A review. Allergy 2021, 76, 428–455. [Google Scholar] [CrossRef]
- Warren-Gash, C.; Davidson, J.A.; Strongman, H.; Herrett, E.; Smeeth, L.; Breuer, J.; Banerjee, A. Severe COVID-19 outcomes by cardiovascular risk profile in England in 2020: A population-based cohort study. Lancet Reg. Health—Eur. 2023, 27. [Google Scholar] [CrossRef]
- Guo, F.; Qin, Y.; Fu, H.; Xu, F. The impact of COVID-19 on Emergency Department length of stay for urgent and life-threatening patients. BMC Health Serv. Res. 2022, 22, 696. [Google Scholar] [CrossRef]
- Hobohm, L.; Sagoschen, I.; Barco, S.; Schmidtmann, I.; Espinola-Klein, C.; Konstantinides, S.; Muenzel, T.; Keller, K. Trends and Risk Factors of In-Hospital Mortality of Patients with COVID-19 in Germany: Results of a Large Nationwide Inpatient Sample. Viruses 2022, 14, 275. [Google Scholar] [CrossRef]
- Brandt, F.; Simone, G.; Loth, J.; Schilling, D. COVID-19-associated costs and mortality in Germany: An incidence-based analysis from a payer’s perspective. BMC Health Serv. Res. 2024, 24, 321. [Google Scholar] [CrossRef] [PubMed]
- Suwono, B.; Brandl, M.; Hecht, J.; Eckmanns, T.; Haller, S. Epidemiology of healthcare-associated SARS-CoV-2 outbreaks in Germany between March 2020 and May 2022. J. Hosp. Infect. 2023, 134, 108–120. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.; Meinicke, M.; Schenkel, A. Krankheitsbedingte Fehlzeiten in Der Deutschen Wirtschaft im Jahr 2022. In Fehlzeiten-Report 2023; Badura, B., Ducki, A., Baumgardt, J., Meyer, M., Schröder, H., Eds.; Springer: Berlin/Heidelberg, Germany, 2023; pp. 435–520. [Google Scholar] [CrossRef]
- Badura, B.; Ducki, A.; Baumgardt, J.; Meyer, M.; Schröder, H. Fehlzeiten-Report 2023: Zeitenwende—Arbeit Gesund Gestalten; Springer: Berlin/Heidelberg, Germany, 2023; Volume 02023, p. 499. [Google Scholar]
- Fehlzeiten-Report 2024|Pressemitteilungen|WIdO—Wissenschaftliches Institut der AOK. Available online: https://www.wido.de/news-presse/pressemitteilungen/2024/fehlzeiten-report-2024/ (accessed on 28 November 2024).
- COVID-19 Impfdashboard. Available online: https://impfdashboard.de/ (accessed on 21 February 2025).
- Viscusi, W.K. The global COVID-19 mortality cost report card: 2020, 2021, and 2022. PLoS ONE 2023, 18, e0284273. [Google Scholar] [CrossRef] [PubMed]

| Non-Severe COVID-19 Cases | Severe COVID-19 Cases | Critical COVID-19 Cases | |
|---|---|---|---|
| N | 362,786 | 7968 | 692 |
| Age in years [mean (SD)|median] | 46.4 (20.2)|46 | 73.6 (22.1)|81 | 73.1 (12.8)|75 |
| Female gender [n (%)] | 206,032 (56.8%) | 3724 (46.7%) | 253 (36.6%) |
| Employment status/”Type of insurance” [n (%)] | |||
| employee | 235,062 (64.8%) | 374 (4.7%) | 38 (5.5%) |
| unemployed | 13,296 (3.7%) | 169 (2.1%) | 23 (3.3%) |
| pensioner/retiree | 65,187 (18.0%) | 6698 (84.1%) | 603 (87.1%) |
| self-payer | 14,463 (4.0%) | 161 (2.0%) | 15 (2.2%) |
| rehabilitator | 576 (0.2%) | 3 (0.0%) | 0 (0.0%) |
| insured family member without an own income | 34,202 (9.4%) | 563 (7.1%) | 13 (1.9%) |
| Charlson Comorbidity Index [mean (SD)|median] | 1.0 (2.0)|0 | 4.3 (3.2)|4 | 4.6 (3.2)|4 |
| Elixhauser Comorbidity Index [mean (SD)|median] | 2.5 (6.6)|0 | 12.4 (10.9)|11 | 13.4 (11.1)|12 |
| CHA2DS2-VASc score [mean (SD)|Median] | 1.5 (1.6)|1 | 4.2 (2.0)|4 | 4.1 (1.9)|4 |
| Presence of a high-risk condition—immunocompromised [n (%)] | 30,816 (8.5%) | 2166 (27.2%) | 226 (32.7%) |
| Presence of a high-risk condition—others + [n (%)] | 224,442 (61.9%) | 7242 (90.9%) | 655 (94.7%) |
| Pre-index AF [n (%)] | 14,797 (4.1%) | 2282 (28.6%) | 191 (27.6%) |
| Pre-index HF [n (%)] | 19,713 (5.4%) | 2898 (36.4%) | 271 (39.2%) |
| Pre-index CHD [n (%)] | 24,332 (6.7%) | 2847 (35.7%) | 278 (40.2%) |
| Pre-index depression [n (%)] | 45,876 (12.6%) | 1442 (18.1%) | 116 (16.8%) |
| Pre-index anxiety disorder [n (%)] | 31,593 (8.7%) | 776 (9.7%) | 78 (11.3%) |
| COVID-19-Related Hospitalizations | COVID-19-Related Outpatient GP Visits | COVID-19-Related Outpatient Specialist Visits | COVID-19-Related Inpatient Rehabilitations | Days Absent from Work Due to COVID-19 (in the General Working Population) | ||
|---|---|---|---|---|---|---|
| Number of persons observed (N) | 3,254,803 | 1,917,317 | ||||
| Total observational time in years | 3,195,992 | 1,890,139 | ||||
| Total number of utilizations | 8912 | 1,237,879 | 407,006 | 530 | 3,415,635 | |
| Rate per person-year (95% CI) | 0.003 (0.003–0.003) | 0.387 (0.387–0.388) | 0.127 (0.127–0.128) | 0.000 (0.000–0.000) | 1.807 (1.805–1.809) | |
| Total number of inpatient days | 88,605 | N/A | N/A | 10,850 | N/A | |
| Associated COVID-19-related costs | EUR 64,929,586.51 | EUR 37,747,345.06 | EUR 10,983,757.24 | EUR 1,914,842.80 | EUR 454,279,455.00 | |
| % of COVID-19-related costs in all-cause costs | 1.5% | 5.5% | 1.0% | 1.0% | 7.5% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Müller, S.; Schmetz, A.; Knaul, J.K.; Wilke, T.; Yang, J.; Dornig, S.; Lehmann, C.; Spinner, C.D. COVID-19 Disease Burden in the Omicron Variant-Dominated Endemic Phase: Insights from the ROUTINE-COV19 Study Using Real-World German Statutory Health Insurance Data. Viruses 2025, 17, 424. https://doi.org/10.3390/v17030424
Müller S, Schmetz A, Knaul JK, Wilke T, Yang J, Dornig S, Lehmann C, Spinner CD. COVID-19 Disease Burden in the Omicron Variant-Dominated Endemic Phase: Insights from the ROUTINE-COV19 Study Using Real-World German Statutory Health Insurance Data. Viruses. 2025; 17(3):424. https://doi.org/10.3390/v17030424
Chicago/Turabian StyleMüller, Sabrina, Andrea Schmetz, Julia K. Knaul, Thomas Wilke, Jingyan Yang, Sabine Dornig, Clara Lehmann, and Christoph D. Spinner. 2025. "COVID-19 Disease Burden in the Omicron Variant-Dominated Endemic Phase: Insights from the ROUTINE-COV19 Study Using Real-World German Statutory Health Insurance Data" Viruses 17, no. 3: 424. https://doi.org/10.3390/v17030424
APA StyleMüller, S., Schmetz, A., Knaul, J. K., Wilke, T., Yang, J., Dornig, S., Lehmann, C., & Spinner, C. D. (2025). COVID-19 Disease Burden in the Omicron Variant-Dominated Endemic Phase: Insights from the ROUTINE-COV19 Study Using Real-World German Statutory Health Insurance Data. Viruses, 17(3), 424. https://doi.org/10.3390/v17030424






