SARS-CoV-2 Infection and Adverse Maternal and Perinatal Outcomes: Time-to-Event Analysis of a Hospital-Based Cohort Study of Pregnant Women in Rio de Janeiro, Brazil
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Variables
2.3. Statistical Analysis
2.4. Sensitivity Analysis
3. Results
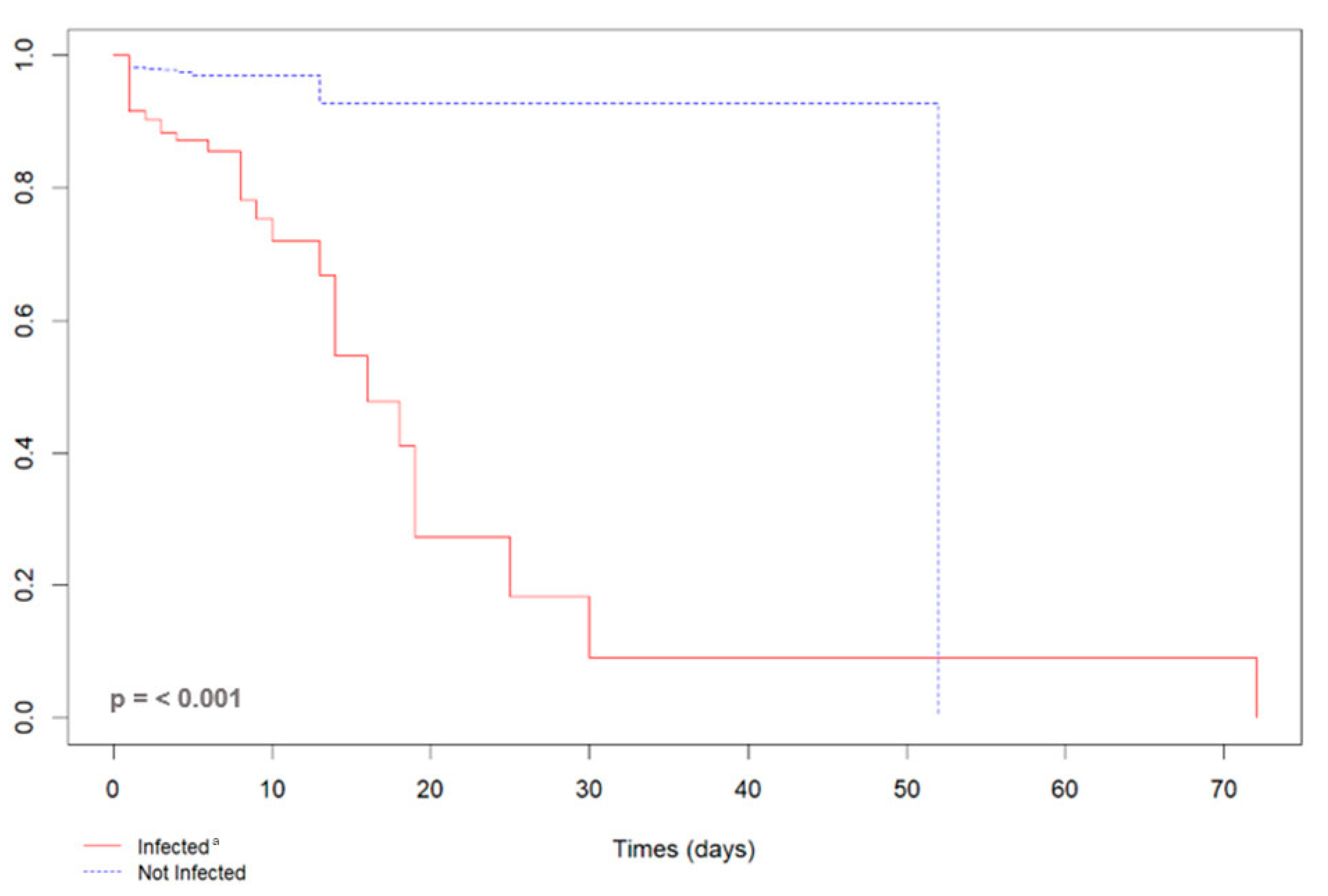
3.1. SARS-CoV-2 and Maternal Outcomes
3.2. SARS-CoV-2 and Perinatal Outcomes
3.3. SARS-CoV-2 and Vertical Transmission
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rasmussen, S.A.; Smulian, J.C.; Lednicky, J.A.; Wen, T.S.; Jamieson, D.J. Coronavirus Disease 2019 (COVID-19) and pregnancy: What obstetricians need to know. Am. J. Obstet. Gynecol. 2020, 222, 415–426. [Google Scholar] [CrossRef]
- Pan-American Health Organization. Director Urges Countries to Prioritize Pregnant and Lactating Women for COVID-19 Vaccinations 2021. Available online: https://www.paho.org/en/news/8-9-2021-paho-director-urges-countries-prioritize-pregnant-and-lactating-women-covid-19 (accessed on 26 January 2025).
- Kasehagen, L.; Byers, P.; Taylor, K.; Kittle, T.; Roberts, C.; Collier, C.; Rust, B.; Ricaldi, J.N.; Green, J.; Zapata, L.B.; et al. COVID-19-Associated Deaths After SARS-CoV-2 Infection During Pregnancy—Mississippi, March 1, 2020-October 6, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1646–1648. [Google Scholar] [CrossRef]
- Souza, A.S.R.; Amorim, M.M.R. Maternal mortality by COVID-19 in Brazil. Revista Brasileira de Saúde Materno Infantil 2021, 21, 253–256. [Google Scholar] [CrossRef]
- Orellana, J.; Jacques, N.; Leventhal, D.G.P.; Marrero, L.; Morón-Duarte, L.S. Excess maternal mortality in Brazil: Regional inequalities and trajectories during the COVID-19 epidemic. PLoS ONE. 2022, 17, e0275333. [Google Scholar] [CrossRef] [PubMed]
- Blakeway, H.; Prasad, S.; Kalafat, E.; Heath, P.T.; Ladhani, S.N.; Le Doare, K.; Magee, L.A.; O’brien, P.; Rezvani, A.; von Dadelszen, P.; et al. COVID-19 vaccination during pregnancy: Coverage and safety. Am. J. Obstet. Gynecol. 2022, 226, 236.e1–236.e14. [Google Scholar] [CrossRef]
- Pan-American Health Organization. Epidemiological Alert: COVID-19 During Pregnancy 2020. Available online: https://www.paho.org/en/documents/epidemiological-alert-covid-19-during-pregnancy-13-august-2020 (accessed on 26 January 2025).
- Swamy, G.K. Infectious diseases in pregnancy. Obstet. Gynecol. Clin. N. Am. 2014, 41, xi–xii. [Google Scholar] [CrossRef]
- Toglia, M.R.; Weg, J.G. Venous thromboembolism during pregnancy. N. Engl. J. Med. 1996, 335, 108–114. [Google Scholar] [CrossRef]
- Liu, H.; Wang, L.L.; Zhao, S.J.; Kwak-Kim, J.; Mor, G.; Liao, A.H. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J. Reprod. Immunol. 2020, 139, 103122. [Google Scholar] [CrossRef]
- Menezes, M.O.; Takemoto, M.L.S.; Nakamura-Pereira, M.; Katz, L.; Amorim, M.M.R.; Salgado, H.O.; Melo, A.; Diniz, C.S.G.; de Sousa, L.A.R.; Magalhaes, C.G.; et al. Risk factors for adverse outcomes among pregnant and postpartum women with acute respiratory distress syndrome due to COVID-19 in Brazil. Int. J. Gynaecol. Obstet. 2020, 151, 415–423. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Palacio, I.; Maldonado, L.; Malo, S.; Sánchez-Recio, R.; Marcos-Campos, I.; Magallón-Botaya, R.; Rabanaque, M.J. COVID-19 Inequalities: Individual and Area Socioeconomic Factors (Aragón, Spain). Int. J. Environ. Res. Public Health 2021, 18, 6607. [Google Scholar] [CrossRef]
- Amorim, M.M.R.; Soligo Takemoto, M.L.; Fonseca, E.B.D. Maternal deaths with coronavirus disease 2019: A different outcome from low- to middle-resource countries? Am J Obstet Gynecol. 2020, 223, 298–299. [Google Scholar] [CrossRef] [PubMed]
- Ministério da Saúde. Governo Recomenda Vacinação contra COVID-19 em Gestantes e Puérperas sem Comorbidades 2021. Available online: https://www.gov.br/pt-br/noticias/saude-e-vigilancia-sanitaria/2021/07/governo-recomenda-vacinacao-contra-covid-19-em-gestantes-e-puerperas-sem-comorbidades (accessed on 26 January 2025).
- Observatório Obstétrico Brasileiro. OOBr Vacinação COVID-19: Vacinação contra COVID-19 de Gestante e Puérperas 2021. Available online: https://observatorioobstetrico.shinyapps.io/vacinacao-covid19 (accessed on 26 January 2025).
- Borges, M.; Florentino, P.T.V.; Cerqueira-Silva, T.; de Carvalho, L.F.; de Araújo Oliveira, V.; Aguilar, G.M.O.; Prado, R.d.S.; Soranz, D.; Werneck, G.L.; Pescarini, J.M.; et al. Factors associated with COVID-19 vaccination among pregnant women in Rio De Janeiro City, Brazil. Sci. Rep. 2023, 13, 18235. [Google Scholar] [CrossRef] [PubMed]
- Razzaghi, H.; Meghani, M.; Pingali, C.; Crane, B.; Naleway, A.; Weintraub, E.; Kenigsberg, T.A.; Lamias, M.J.; Irving, S.A.; Kauffman, T.L.; et al. COVID-19 Vaccination Coverage Among Pregnant Women During Pregnancy—Eight Integrated Health Care Organizations, United States, December 14, 2020-May 8, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 895–899. [Google Scholar] [CrossRef] [PubMed]
- Secretaria Estadual de Saúde do Rio de Janeiro. Maternidades 2017. Available online: https://www.saude.rj.gov.br/humanizacao/maternidades/2017/05/hospital-estadual-adao-pereira-nunes (accessed on 26 January 2025).
- Instituto Brasileiro de Geografia e Estatística. Documentação do Censo 2022. Available online: https://cidades.ibge.gov.br/brasil/rj/duque-de-caxias/pesquisa/19/29765?tipo=ranking (accessed on 26 January 2025).
- Carvalho, M.S.; Bastos, L.S.; Fuller, T.; Cruz, O.G.; Damasceno, L.; Calvet, G.; Resende, P.C.; Smith, C.; Whitworth, J.; Siqueira, M.; et al. Incidence of SARS-CoV-2 over four epidemic waves in a low-resource community in Rio de Janeiro, Brazil: A prospective cohort study. Lancet Reg. Health Am. 2022, 12, 100283. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. COVID-19, Pregnancy, Childbirth, and Breastfeeding: Answers from Ob-Gyns 2024. Available online: www.acog.org/womens-health/faqs/coronavirus-covid-19-pregnancy-and-breastfeeding (accessed on 26 January 2025).
- US Centers for Disease Control and Prevention. COVID-19 Vaccines While Pregnant or Breastfeeding 2023. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/pregnancy.html (accessed on 26 January 2025).
- R Core Team. R: A Language and Environment for Statistical Computing 2020. Available online: https://www.r-project.org/ (accessed on 26 January 2025).
- de Wreede, L.C.; Fiocco, M.; Putter, H. mstate: An R Package for the Analysis of Competing Risks and Multi-State Models. J. Stat. Softw. 2011, 38, 1–30. [Google Scholar] [CrossRef]
- Brendolin, M.; Fuller, T.; Wakimoto, M.; Rangel, L.; Rodrigues, G.M.; Rohloff, R.D.; Guaraldo, L.; Nielsen-Saines, K.; Brasil, P. Severe maternal morbidity and mortality during the COVID-19 pandemic: A cohort study in Rio de Janeiro. IJID Reg. 2023, 6, 1–6. [Google Scholar] [CrossRef]
- Takemoto, M.L.S.; Menezes, M.O.; Andreucci, C.B.; Nakamura-Pereira, M.; Amorim, M.M.R.; Katz, L.; Knobel, R. The tragedy of COVID-19 in Brazil: 124 maternal deaths and counting. Int. J. Gynaecol. Obstet. 2020, 151, 154–156. [Google Scholar] [CrossRef] [PubMed]
- González-Vanegas, O.; Martinez-Perez, O. SARS-CoV-2 Infection and Preeclampsia—How an Infection Can Help Us to Know More about an Obstetric Condition. Viruses 2023, 15, 1564. [Google Scholar] [CrossRef] [PubMed]
- Mira, A.R.; De Pinho, A.; Calado-Araújo, M.; Ferreira, C.; David, D.; Enes, M.; Vaz-de-Macedo, C. COVID-19 and Hypertensive Disorders of Pregnancy (HDP): A Portuguese Multicentric Retrospective Cohort Study of HDP in SARS-CoV-2 Infected Patients. Cureus 2023, 15, e36483. [Google Scholar] [CrossRef] [PubMed]
- Aabakke, A.J.M.; Petersen, T.G.; Wøjdemann, K.; Ibsen, M.H.; Jonsdottir, F.; Rønneberg, E.; Hammer, A.; Clausen, T.D.; Milbak, J.; Burmester, L.; et al. Risk factors for and pregnancy outcomes after SARS-CoV-2 in pregnancy according to disease severity: A nationwide cohort study with validation of the SARS-CoV-2 diagnosis. Acta Obstet. Gynecol. Scand. 2023, 102, 282–293. [Google Scholar] [CrossRef] [PubMed]
- Qeadan, F.; Mensah, N.A.; Tingey, B.; Stanford, J.B. The risk of clinical complications and death among pregnant women with COVID-19 in the Cerner COVID-19 cohort: A retrospective analysis. BMC Pregnancy Childbirth 2021, 21, 305. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.M.; Ahmadi, H.; Huo, L.; Lix, L.M.; Maslin, K.; Latour, J.M.; Shawe, J. COVID-19 and pregnancy: A comprehensive study of comorbidities and outcomes. BMC Public Health 2024, 24, 3157. [Google Scholar] [CrossRef] [PubMed]
- Zambrano, L.D.; Ellington, S.; Strid, P.; Galang, R.R.; Oduyebo, T.; Tong, V.T.; Woodworth, K.R.; Nahabedian, J.F., 3rd; Azziz-Baumgartner, E.; Gilboa, S.M.; et al. Update: Characteristics of Symptomatic Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status—United States, January 22-October 3, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1641–1647. [Google Scholar] [CrossRef] [PubMed]
- Breslin, N.; Baptiste, C.; Gyamfi-Bannerman, C.; Miller, R.; Martinez, R.; Bernstein, K.; Ring, L.; Landau, R.; Purisch, S.; Friedman, A.M.; et al. Coronavirus disease 2019 infection among asymptomatic and symptomatic pregnant women: Two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am. J. Obstet. Gynecol. MFM 2020, 2, 100118. [Google Scholar] [CrossRef]
- Wali, A.S.; Ali, M.M.; Bibi, R.; Rahim, A. The clinical manifestations and pregnancy outcomes of COVID-19 infection at a tertiary care hospital. Pak. J. Med. Sci. 2024, 40, S15–S20. [Google Scholar] [CrossRef]
- Silasi, M.; Cardenas, I.; Kwon, J.Y.; Racicot, K.; Aldo, P.; Mor, G. Viral infections during pregnancy. Am. J. Reprod. Immunol. 2015, 73, 199–213. [Google Scholar] [CrossRef]
- Kourtis, A.P.; Read, J.S.; Jamieson, D.J. Pregnancy and infection. N. Engl. J. Med. 2014, 370, 2211–2218. [Google Scholar] [CrossRef] [PubMed]
- Chudnovets, A.; Liu, J.; Narasimhan, H.; Liu, Y.; Burd, I. Role of Inflammation in Virus Pathogenesis during Pregnancy. J. Virol. 2020, 95. [Google Scholar] [CrossRef]
- Martínez-Perez, O.; Vouga, M.; Cruz Melguizo, S.; Forcen Acebal, L.; Panchaud, A.; Muñoz-Chápuli, M.; Baud, D. Association Between Mode of Delivery Among Pregnant Women With COVID-19 and Maternal and Neonatal Outcomes in Spain. JAMA 2020, 324, 296–299. [Google Scholar] [CrossRef]
- Knight, M.; Bunch, K.; Vousden, N.; Morris, E.; Simpson, N.; Gale, C.; O’brien, P.; Quigley, M.; Brocklehurst, P.; Kurinczuk, J.J. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: National population based cohort study. BMJ 2020, 369, m2107. [Google Scholar] [CrossRef]
- Örtqvist, A.K.; Magnus, M.C.; Aabakke, A.J.M.; Urhoj, S.K.; Vinkel Hansen, A.; Nybo Andersen, A.M.; Krebs, L.; Pettersson, K.; Håberg, S.E.; Stephansson, O. Severe COVID-19 during pregnancy in Sweden, Norway, and Denmark. Acta Obstet. Gynecol. Scand. 2023, 102, 681–689. [Google Scholar] [CrossRef]
- Oncel, M.Y.; Akın, I.M.; Kanburoglu, M.K.; Tayman, C.; Coskun, S.; Narter, F.; Er, I.; Oncan, T.G.; Memisoglu, A.; Cetinkaya, M.; et al. A multicenter study on epidemiological and clinical characteristics of 125 newborns born to women infected with COVID-19 by Turkish Neonatal Society. Eur. J. Pediatr. 2021, 180, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Di Toro, F.; Gjoka, M.; Di Lorenzo, G.; De Santo, D.; De Seta, F.; Maso, G.; Risso, F.M.; Romano, F.; Wiesenfeld, U.; Levi-D’Ancona, R.; et al. Impact of COVID-19 on maternal and neonatal outcomes: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2021, 27, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Jafari, M.; Pormohammad, A.; Sheikh Neshin, S.A.; Ghorbani, S.; Bose, D.; Alimohammadi, S.; Basirjafari, S.; Mohammadi, M.; Rasmussen-Ivey, C.; Razizadeh, M.H.; et al. Clinical characteristics and outcomes of pregnant women with COVID-19 and comparison with control patients: A systematic review and meta-analysis. Rev. Med. Virol. 2021, 31, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Li, Q.; Zheng, D.; Jiang, H.; Wei, Y.; Zou, L.; Feng, L.; Xiong, G.; Sun, G.; Wang, H.; et al. Clinical Characteristics of Pregnant Women with Covid-19 in Wuhan, China. N. Engl. J. Med. 2020, 382, e100. [Google Scholar] [CrossRef] [PubMed]
- Morán Antolín, E.; Broullón Molanes, J.R.; de la Cruz Conty, M.L.; Encinas Pardilla, M.B.; Guadix Martín, M.D.P.; Sainz Bueno, J.A.; Acebal, L.F.; Recarte, P.P.; Bartolomé, A.Á.; Cendán, J.P.M.; et al. SARS-CoV-2 Infection and C-Section: A Prospective Observational Study. Viruses 2021, 13, 2330. [Google Scholar] [CrossRef]
- Narang, K.; Enninga, E.A.L.; Gunaratne, M.; Ibirogba, E.R.; Trad, A.T.A.; Elrefaei, A.; Theiler, R.N.; Ruano, R.; Szymanski, L.M.; Chakraborty, R.; et al. SARS-CoV-2 Infection and COVID-19 During Pregnancy: A Multidisciplinary Review. Mayo Clin. Proc. 2020, 95, 1750–1765. [Google Scholar] [CrossRef] [PubMed]
- Quaresima, P.; Saccone, G.; Pellegrino, R.; Vaccarisi, S.; Taranto, L.; Mazzulla, R.; Bernardo, S.; Venturella, R.; Di Carlo, C.; Morelli, M. Incidental diagnosis of a pancreatic adenocarcinoma in a woman affected by gestational diabetes mellitus: Case report and literature review. Am. J. Obstet. Gynecol. MFM. 2021, 3, 100471. [Google Scholar] [CrossRef]
- Allotey, J.; Kew, T.; Fernández-García, S.; Gaetano-Gil, A.; Yap, M.; Sheikh, J.; Littmoden, M.; Akande, O.; Khalil, H.; Kumaran, M.; et al. SARS-CoV-2 positivity in offspring and timing of mother-to-child transmission: Living systematic review and meta-analysis. BMJ 2022, 376, e067696. [Google Scholar] [CrossRef]
- Fenizia, C.; Biasin, M.; Cetin, I.; Vergani, P.; Mileto, D.; Spinillo, A.; Gismondo, M.R.; Perotti, F.; Callegari, C.; Mancon, A.; et al. Analysis of SARS-CoV-2 vertical transmission during pregnancy. Nat. Commun. 2020, 11, 5128. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, D.J.; Rasmussen, S.A. An update on COVID-19 and pregnancy. Am. J. Obstet. Gynecol. 2022, 226, 177–186. [Google Scholar] [CrossRef]
- Vivanti, A.J.; Vauloup-Fellous, C.; Prevot, S.; Zupan, V.; Suffee, C.; Do Cao, J.; Benachi, A.; De Luca, D. Transplacental transmission of SARS-CoV-2 infection. Nat. Commun. 2020, 11, 3572. [Google Scholar] [CrossRef]
- Carsetti, R.; Quintarelli, C.; Quinti, I.; Piano Mortari, E.; Zumla, A.; Ippolito, G.; Locatelli, F. The immune system of children: The key to understanding SARS-CoV-2 susceptibility? Lancet Child Adolesc Health. 2020, 4, 414–416. [Google Scholar] [CrossRef]
- Wang, X.; Yang, P.; Zheng, J.; Liu, P.; Wei, C.; Guo, J.; Zhang, Y.; Zhao, D. Dynamic changes of acquired maternal SARS-CoV-2 IgG in infants. Sci. Rep. 2021, 11, 8021. [Google Scholar] [CrossRef] [PubMed]
- Palmeira, P.; Quinello, C.; Silveira-Lessa, A.L.; Zago, C.A.; Carneiro-Sampaio, M. IgG placental transfer in healthy and pathological pregnancies. Clin. Dev. Immunol. 2012, 2012, 985646. [Google Scholar] [CrossRef] [PubMed]
- Zeng, H.; Xu, C.; Fan, J.; Tang, Y.; Deng, Q.; Zhang, W.; Long, X. Antibodies in Infants Born to Mothers With COVID-19 Pneumonia. JAMA 2020, 323, 1848–1849. [Google Scholar] [CrossRef] [PubMed]
- Cambou, M.C.; Liu, C.M.; Mok, T.; Fajardo-Martinez, V.; Paiola, S.G.; Ibarrondo, F.J.; Kerin, T.; Fuller, T.; Tobin, N.H.; Garcia, G.; et al. Longitudinal Evaluation of Antibody Persistence in Mother-Infant Dyads After Severe Acute Respiratory Syndrome Coronavirus 2 Infection in Pregnancy. J. Infect. Dis. 2023, 227, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Simbar, M.; Nazarpour, S.; Sheidaei, A. Evaluation of pregnancy outcomes in mothers with COVID-19 infection: A systematic review and meta-analysis. J. Obstet. Gynaecol. 2023, 43, 2162867. [Google Scholar] [CrossRef]
- Pierce-Williams, R.A.M.; Burd, J.; Felder, L.; Khoury, R.; Bernstein, P.S.; Avila, K.; Penfield, C.A.; Roman, A.S.; DeBolt, C.A.; Stone, J.L.; et al. Clinical course of severe and critical coronavirus disease 2019 in hospitalized pregnancies: A United States cohort study. Am. J. Obstet. Gynecol. MFM. 2020, 2, 100134. [Google Scholar] [CrossRef]
- Woodworth, K.R.; Olsen, E.O.; Neelam, V.; Lewis, E.L.; Galang, R.R.; Oduyebo, T.; Aveni, K.; Yazdy, M.M.; Harvey, E.; Longcore, N.D.; et al. Birth and Infant Outcomes Following Laboratory-Confirmed SARS-CoV-2 Infection in Pregnancy—SET-NET, 16 Jurisdictions, March 29-October 14, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1635–1640. [Google Scholar] [CrossRef]
- Engjom, H.; Aabakke, A.J.M.; Klungsøyr, K.; Svanvik, T.; Äyräs, O.; Jonasdottir, E.; Thurn, L.; Jones, E.; Pettersson, K.; Nyfløt, L.T.; et al. COVID-19 in pregnancy-characteristics and outcomes of pregnant women admitted to hospital because of SARS-CoV-2 infection in the Nordic countries. Acta Obstet. Gynecol. Scand. 2021, 100, 1611–1619. [Google Scholar] [CrossRef] [PubMed]
- Gurol-Urganci, I.; Jardine, J.E.; Carroll, F.; Draycott, T.; Dunn, G.; Fremeaux, A.; Harris, T.; Hawdon, J.; Morris, E.; Muller, P.; et al. Maternal and perinatal outcomes of pregnant women with SARS-CoV-2 infection at the time of birth in England: National cohort study. Am. J. Obstet. Gynecol. 2021, 225, 522.e1–522.e11. [Google Scholar] [CrossRef]
- Birol Ilter, P.; Prasad, S.; Berkkan, M.; Mutlu, M.A.; Tekin, A.B.; Celik, E.; Ata, B.; Turgal, M.; Yildiz, S.; Turkgeldi, E.; et al. Clinical severity of SARS-CoV-2 infection among vaccinated and unvaccinated pregnancies during the Omicron wave. Ultrasound Obstet. Gynecol. 2022, 59, 560–562. [Google Scholar] [CrossRef] [PubMed]
- Cambou, M.C.; David, H.; Moucheraud, C.; Nielsen-Saines, K.; Comulada, W.S.; Macinko, J. Time series analysis of comprehensive maternal deaths in Brazil during the COVID-19 pandemic. Sci. Rep. 2024, 14, 23960. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, M.R.; Silva, M.A.P.; Prates, L.F.L.; Oliveira, R.R.; Carvalho, M.D.B.; Pelloso, S.M. Factors associated with COVID-19 death in pregnant women hospitalized in Intensive Care Units. Rev. Bras. Enferm. 2024, 77, e20230172. [Google Scholar] [CrossRef] [PubMed]
- Battarbee, A.N.; Stockwell, M.S.; Varner, M.; Newes-Adeyi, G.; Daugherty, M.; Gyamfi-Bannerman, C.; Tita, A.T.; Vorwaller, K.; Vargas, C.; Subramaniam, A.; et al. Attitudes Toward COVID-19 Illness and COVID-19 Vaccination among Pregnant Women: A Cross-Sectional Multicenter Study during August-December 2020. Am. J. Perinatol. 2022, 39, 75–83. [Google Scholar] [CrossRef]

| Variables | All Pregnant Women n = 1185 | SARS-CoV-2 Infected | CI (95%) a | SARS-CoV-2 Not Infected | CI (95%) a | p-Value |
|---|---|---|---|---|---|---|
| n = 249 (%) | n = 936 (%) | |||||
| Age Range | ||||||
| 16–19 years old | 156 (13.2) | 25 (10.0) | 6–14 | 131 (14.0) | 11–16 | 0.070 |
| 20–34 years old | 867 (73.1) | 181 (72.7) | 66–78 | 686 (73.3) | 70–76 | |
| 35–47 years old | 162 (13.7) | 43 (17.3) | 12–22 | 119 (12.7) | 10–15 | |
| Race/ethnicity | ||||||
| Other b | 1020 (86.1) | 218 (87.5) | 82–91 | 802 (85.7) | 83–87 | 0.450 |
| White | 165 (13.9) | 31 (12.5) | 8–17 | 134 (14.3) | 12–16 | |
| Education | ||||||
| Complete/incomplete elementary education | 393 (33.1) | 70 (28.1) | 22–34 | 323 (34.5) | 31–37 | 0.073 |
| Complete/incomplete high school | 749 (63.2) | 166 (66.7) | 60–72 | 583 (62.3) | 59–65 | |
| Complete/incomplete higher education | 43 (3.7) | 13 (5.2) | 2–8 | 30 (3.2) | 2–4 | |
| Symptoms of COVID-19 | ||||||
| Cough | 159 (41.8) | 104 (41.8) | 35–48 | 55 (5.9) | 4–7 | <0.001 |
| Fever | 162 (39.0) | 97 (39.0) | 32–45 | 65 (6.9) | 5–8 | <0.001 |
| Dyspnea | 94 (22.0) | 55 (22.1) | 17–27 | 39 (4.2) | 2–5 | <0.001 |
| Myalgia | 76 (22.1) | 55 (22.1) | 17–27 | 21 (2.2) | 1–3 | <0.001 |
| COVID-19 Vaccination c | ||||||
| Complete (two doses) | 209 (21.8) | 54 (21.8) | 16–27 | 155 (16.6) | 14–19 | 0.001 |
| Incomplete (one dose) | 183 (8.5) | 21 (8.5) | 5–12 | 162 (17.3) | 15–20 | |
| Not vaccinated | 792 (69.7) | 173 (69.8) | 63–75 | 619 (66.1) | 62–69 | |
| Comorbidity | ||||||
| Anemia | 230 (19.4) | 47 (18.9) | 14–24 | 183(19.6) | 17–22 | 0.811 |
| Arterial hypertension | 138 (13.2) | 33 (13.3) | 9–18 | 105 (11.2) | 9–13 | 0.374 |
| Obesity | 66 (8.4) | 21 (8.4) | 5–12 | 45 (4.8) | 3–6 | 0.027 |
| Asthma | 52 (4.4) | 16 (6.4) | 3–10 | 36 (3.8) | 2–5 | 0.083 |
| Diabetes mellitus | 17 (1.4) | 5 (2.0) | 0.7–4 | 12 (1.3) | 0.6–2 | 0.375 |
| HIV | 12 (1.0) | 3 (1.2) | 0.3–3 | 9 (1.0) | 0.4–1.8 | 0.724 |
| Gestational Complication | ||||||
| Pre-eclampsia | 237 (18.5) | 46 (18.5) | 13–23 | 191 (20.4) | 17–23 | 0.498 |
| Gestational diabetes | 93 (8.0) | 20 (8.0) | 4–12 | 73 (7.8) | 6–9 | 0.903 |
| Placental abruption | 39 (4.0) | 10 (4.0) | 1–7 | 29 (3.1) | 2–4 | 0.471 |
| Prenatal consultations | ||||||
| 0–5 consultations (inappropriate) | 483 (41.4) | 103 (41.4) | 35–47 | 380 (40.6) | 37–43 | 0.827 |
| ≥ 6 consultations (suitable) | 702 (58.6) | 146 (58.6) | 52–64 | 556 (59.4) | 56–62 | |
| Gestational Trimester | ||||||
| 1° trimester (≤ 13 weeks) | 17 (2.0) | 5 (2.0) | 0.6–4 | 12 (1.3) | 0.6–2 | <0.001 |
| 2° trimester (14–27 weeks) | 107 (17.3) | 43 (17.3) | 12–22 | 64 (6.8) | 5–8 | |
| 3° trimester (28–42 weeks) | 1061 (80.7) | 201 (80.7) | 75–85 | 860 (91.9) | 89–93 | |
| Mode of delivery (N = 1151) d | ||||||
| Cesarean section | 526 (45.7) | 135 (57.0) | 50–63 | 391 (43.0) | 39–46 | <0.001 |
| Vaginal delivery | 625 (54.3) | 102(43.0) | 36–49 | 523 (57.0) | 53–60 |
| Outcomes | All Pregnant Women | SARS-CoV-2 Infected a | CI (95%) | SARS-CoV-2 Not Infected b | CI (95%) | p-Value c |
|---|---|---|---|---|---|---|
| N = 1211 (%) | N = 257 (%) | N = 954 (%) | ||||
| All Adverse Perinatal d | ||||||
| Yes | 422 (42.4) | 109 (42.4%) | 36–48 | 313 (32.8) | 29–35 | 0.004 |
| No | 789 (57.6) | 148 (57.6) | 51–63 | 641 (67.2) | 64–70 | |
| Prematurity | ||||||
| Yes | 304 (30.7) | 79 (30.7) | 25–36 | 225 (23.6) | 20–26 | 0.019 |
| No | 907 (69.3) | 178 (69.3) | 63–74 | 729 (76.4) | 73–79 | |
| Fetal distress | ||||||
| Yes | 101 (9.7) | 25 (9.7) | 6–14 | 76 (8.0) | 6–9 | 0.364 |
| No | 1110 (90.3) | 232 (90.3) | 85–93 | 878 (92.0) | 90–93 | |
| Stillbirths | ||||||
| Yes | 37 (4.7) | 12 (4.7) | 2–8 | 25 (2.6) | 1–3 | 0.090 |
| No | 1174 (95.3) | 245 (95.3) | 91–97 | 929 (97.4) | 96–98 | |
| Neonatal deaths | ||||||
| Yes | 26 (3.1) | 8 (3.2) | 1–6 | 18 (1.9) | 1–2 | 0.229 |
| No | 1185 (96.9) | 249 (96.9) | 93–98 | 936 (98.1) | 97–99 | |
| Birth weight (g)e | N = 1174 (%) | N = 245 (%) | N = 929 (%) | |||
| <2500 | 270 (23.0) | 57 (23.3) | 18–29 | 213 (23.0) | 20–25 | 0.911 |
| ≥2500 | 904 (77.0) | 188 (76.7) | 70–81 | 716 (77.0) | 74–79 |
| Perinatal Outcome | Crude HR (CI 95%) | Adjusted HR a *(CI 95%) |
|---|---|---|
| All Adverse Perinatalb | 0.96 (0.77–1.20) | 0.94 (0.75–1.19) |
| Neonatal death | 1.41 (0.63–3.14) | 0.96 (0.35–2.67) |
| Stillbirth | 1.51 (0.77–2.95) | 1.07 (0.48–2.38) |
| Fetal distress | 1.12 (0.71–1.75) | 1.29 (0.82–2.05) |
| Prematurity (< 37 weeks) | 1.05 (0.80–1.38) | 0.92 (0.68–1.23) |
| Assay | SARS-CoV-2 Positive+ Results | IC (95%) | SARS-CoV-2 Negative Results | IC (95%) |
|---|---|---|---|---|
| N (%) | N (%) | |||
| IgG Serum (n = 124) | 71 (57.2) | 49–66 | 53 (42.8) | 33–50 |
| RT-PCR nasopharyngeal swab (n = 81) | 3 (3.7%) | 7–10 | 78 (96.2) | 89–99 |
| SARS CoV-2 IgM Serum (n = 42) | 0 | 0 | 42 (100.0) | 91–100 |
| Sars CoV-2 IgA Serum (n = 90) | 3 (3.0) | 0.6–9 | 87 (97.0) | 90–99 |
| Case | Ballard a | Weight | APGAR b | Clinical signs | NICU | RT-PCR | IgA |
|---|---|---|---|---|---|---|---|
| 1 | 34s | 2265 | 5/6 | respiratory discomfort | yes | Positive | − |
| 2 (G1) | 34s | 2125 | 8/9 | respiratory discomfort | yes | Positive | − |
| 3 (G2) | 34s | 1800 | 4/8 | respiratory discomfort; bradycardia | yes | Positive | − |
| 4 | 30s | 1310 | 6/9 | sepsis | yes | Negative | Positive |
| 5 | 37s | 3190 | 4/8 | respiratory discomfort | no | − | Positive |
| 6 | 37s | 3100 | 7/8 | asymptomatic | no | − | Positive |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brendolin, M.; Wakimoto, M.D.; de Oliveira, R.d.V.C.; Mageste, L.R.; Nielsen-Saines, K.; Brasil, P. SARS-CoV-2 Infection and Adverse Maternal and Perinatal Outcomes: Time-to-Event Analysis of a Hospital-Based Cohort Study of Pregnant Women in Rio de Janeiro, Brazil. Viruses 2025, 17, 207. https://doi.org/10.3390/v17020207
Brendolin M, Wakimoto MD, de Oliveira RdVC, Mageste LR, Nielsen-Saines K, Brasil P. SARS-CoV-2 Infection and Adverse Maternal and Perinatal Outcomes: Time-to-Event Analysis of a Hospital-Based Cohort Study of Pregnant Women in Rio de Janeiro, Brazil. Viruses. 2025; 17(2):207. https://doi.org/10.3390/v17020207
Chicago/Turabian StyleBrendolin, Michelle, Mayumi Duarte Wakimoto, Raquel de Vasconcellos Carvalhaes de Oliveira, Larissa Rangel Mageste, Karin Nielsen-Saines, and Patricia Brasil. 2025. "SARS-CoV-2 Infection and Adverse Maternal and Perinatal Outcomes: Time-to-Event Analysis of a Hospital-Based Cohort Study of Pregnant Women in Rio de Janeiro, Brazil" Viruses 17, no. 2: 207. https://doi.org/10.3390/v17020207
APA StyleBrendolin, M., Wakimoto, M. D., de Oliveira, R. d. V. C., Mageste, L. R., Nielsen-Saines, K., & Brasil, P. (2025). SARS-CoV-2 Infection and Adverse Maternal and Perinatal Outcomes: Time-to-Event Analysis of a Hospital-Based Cohort Study of Pregnant Women in Rio de Janeiro, Brazil. Viruses, 17(2), 207. https://doi.org/10.3390/v17020207






