1. Introduction
The Nipah virus (NiV), a member of genus
Henipavirus within
Paramyxoviridae, is an emerging zoonotic pathogen capable of causing severe encephalitis and respiratory illness in humans. Since its initial outbreak in Malaysia in 1998, NiV has caused recurrent outbreaks in South and Southeast Asia, with fatality rates exceeding 70% in some regions. More recently, several significant NiV outbreaks have occurred in South Asia, including the devastating 2018 Kerala outbreak with 19 cases and 17 deaths, the 2023 Bangladesh outbreak resulting in 11 cases and 8 fatalities, and the ongoing 2025 Kerala outbreak with 4 confirmed cases and 2 deaths [
1,
2,
3]. These events demonstrate the persistent public health threat posed by NiV through sporadic zoonotic spillover from bat reservoirs and subsequent human-to-human transmission. Owing to its high pathogenicity, human-to-human transmission potential, and lack of licensed vaccines or therapeutics, NiV has been designated as a priority pathogen by the World Health Organization.
Effective vaccine development against NiV requires a reliable assessment of vaccine-induced neutralizing antibody responses and protective efficacy. However, direct evaluation using live NiV poses substantial challenges owing to BSL-4 containment requirements, limited accessibility to facilities, and biosafety risks. As a result, alternative approaches using pseudotyped viral systems have gained increasing attention as safe, scalable, and informative tools for the preclinical evaluation of vaccine candidates.
Recombinant vesicular stomatitis virus (rVSV)-based pseudoviruses represent a versatile platform for mimicking the entry of high-risk viruses. By incorporating the envelope glycoproteins of target pathogens along with a luciferase reporter gene, rVSV pseudoviruses allow for quantitative infectivity measurements under BSL-2 conditions. Moreover, when coupled with in vivo imaging, these pseudoviruses offer a non-lethal method for assessing real-time infection dynamics and vaccine-induced protection in animal models [
4,
5].
Although lentivirus-based pseudoviruses have been previously used to evaluate NiV vaccine candidates and monoclonal antibodies in vivo [
6], the use of VSV-based pseudoviruses for in vivo bioluminescent imaging of vaccine-induced protection in mice has not been well established.
In this study, we engineered an rVSV-based pseudovirus-expressing the NiV-F and NiV-G glycoproteins and evaluated its usefulness in both in vitro neutralization assays and in vivo protection studies. We optimized pseudovirus production, verified the co-expression of NiV-F/G on the viral surface, and demonstrated neutralization of the pseudovirus produced using both immunized mouse sera and commercial antibodies. Importantly, we established a mouse challenge model using this pseudovirus and successfully visualized the vaccine-mediated inhibition of infection in vivo through bioluminescent imaging. This novel, integrated pseudovirus system provides a safe and robust platform for the comprehensive preclinical evaluation of NiV vaccine candidates, encompassing both humoral immune responses and protective efficacy. Furthermore, this system may serve as a versatile model not only for NiV but also for other emerging BSL-4 pathogens, thereby allowing for ready preclinical evaluation under BSL-2 conditions.
2. Materials and Methods
2.1. Cells
Vero76 (Korean Cell Line Bank, Cat. No. KCLB-21587, Seoul, Korea) cells were maintained in Dulbecco’s modified eagle medium (DMEM, Gibco™, Cat. No.11995-065, Boston, MA, USA) supplemented with 10% fetal bovine serum (FBS, Gibco, Cat. No.26140-079, Boston, MA, USA) and 1× penicillin–streptomycin (100× P/S, Gibco™, Cat. No.15140-122, Boston, MA, USA) in a 5% CO2 environment at 37 °C. BHK-21 (WI2) (Kerafast, Cat. No. EH1011, Boston, MA, USA) cells were maintained at 37 °C in DMEM supplemented with 5% FBS and 1% P/S in an 8% CO2 environment.
2.2. Generation of NiV Fusion Glycoprotein-Specific Antisera in Mice
Five-week-old BALB/c mice were purchased from Orient Bio (Seongnam, Korea) and acclimated to the animal facility for 1 week prior to experimentation. All procedures were approved by the Institutional Animal Care and Use Committee (IACUC No. 2017–008). Mice were immunized intramuscularly at 2-week intervals for administration of four doses. Each dose consisted of 1 μg of recombinant Nipah virus fusion glycoprotein F (NiV-F, Recombinant Nipah Virus Glycoprotein F (UniProt Q9IH63; Fc Chimera, Abcam, Cat. No. Ab256443, Cambridge, UK)) mixed with an aluminum hydroxide-based adjuvant (Imject Alum, Thermo Fisher, Cat. No. 77161, Waltham, MA, USA) at 1/4 of the total volume, in a final volume of 50 μL per injection. The injections were alternated between the left and right hind limbs for each immunization. 1 week after the fourth immunization, blood samples were collected to obtain serum from immunized mice. The resulting serum (NiV F-immunized mouse serum) was used for Western blotting (WB) and neutralization assays.
2.3. Production of the Vesicular Stomatitis Virus (VSV)-Based Pseudovirus
The NiV-F and NiV-G genes of the Malaysian strain (GenBank accession no. AAK50544.1 and AAK50545.1, respectively), were codon-optimized, synthesized using GenScript (Piscataway, NJ, USA), and cloned into the mammalian expression vector pCAGGS-Kan (Kerafast, Cat. No. EH1017, Boston, MA, USA). Subsequently, BHK-21 (WI-2) cells were transfected with a total of 16 μg of DNA at various NiV F to NiV G ratios. For a ratio of F:G = 1:2, 5.33 μg of NiV-F and 10.66 μg of NiV-G were transfected per 100 mm dish using Lipofectamine 2000 (Invitrogen, Cat. No. 11668019, Frederick, MD, USA) according to manufacturer instructions. Then, at 24 h post-transfection, cells were infected with VSV-G*ΔG-Luciferase (Kerafast, Cat. No. EH1020-PM; Boston, MA, USA) at a multiplicity of infection (MOI) factor of 4 [
7]. This VSV-ΔG system harbors a deletion of the native VSV G glycoprotein, rendering a replication-incompetent virus that is dependent on heterologous envelope proteins for a single round of infection. During viral assembly, the codon-optimized NiV-F and NiV-G expressed in transfected cells were incorporated into budding virions, generating pseudotyped particles suitable for entry and neutralization assays under BSL-2 conditions. Pseudovirus production was performed as previously described, with minor modifications to optimize NiV-F/G incorporation. Our protocol closely followed that of Loomis et al. [
8] and Moon et al. [
9], who also used VSV-ΔG backbones and codon-optimized glycoprotein expression to generate high-titer henipavirus pseudotypes for neutralization assays. Then, after 1 h, the cells were washed and the medium was replaced with fresh DMEM containing 5% FBS and incubated at 37 °C in an 8% CO
2 environment for an additional 24 h. Culture supernatants containing the rVSV-NiV-F/G pseudovirus were harvested, filtered through a 0.45 μm filter (Nalgene, Cat. No. 165-0045, Frederick, MD, USA) and stored at −80 °C until further use. Images of the co-expression of both NiV-F and NiV-G during pseudovirus production were captured using a Nikon ECLIPSE Ts2 (Tokyo, Japan) with a 20× phase objective.
2.4. Verification of F/G Co-Expression on the Pseudovirus via Immunoprecipitation (IP) and Western Blotting for F/G Detection
The harvested rVSV-NiV-F/G supernatants were prepared and loaded onto 12% iodixanol cushion (OptiprepTM, Serumwerk Bernburg AG, Cat. No.1114542, Bernburg, Germany) in a polypropylene centrifuge tube (Beckman Coulter, Cat. No. 326819, Brea, CA, USA). Samples were ultracentrifuged at 154,000× g for 2 h at 10 °C using an Optima XE-100 (Beckman Coulter, Brea, CA, USA) equipped with SW55Ti rotor (Beckman Coulter, Brea, CA, USA). After ultracentrifugation, the fractions were divided into an upper, a middle, and a lower layer.
The lower fraction was incubated with rabbit anti-NiV glycoprotein antibody, IgG fraction (1:50, Alpha Diagnostic International, Cat. No. NIV11-S, San Antonio, Texas, USA), and protein A agarose beads (Millipore, Cat No. IP02-1.5MLCN, Boston, MA, USA). Normal rabbit IgG (Sino Biological, Cat. No. CR1, Beijing, China) was used as a negative control for immunoprecipitation (IP).
After washing, pellets were resolved by 4–20% gradient SDS-PAGE (Bio-Rad, Cat. No. 4561095; Brea, CA, USA) and transferred to a polyvinylidene fluoride membrane (Bio-Rad, Cat. No. 162-0239, Brea, CA, USA). Then, this membrane was incubated with NiV F-immunized mouse serum (1:500), anti-VSV-M (23H12) mouse IgG2a (1:2000; absolute antibody, Cat. No. Ab01404-2.0, Cleveland, UK). The blots were further incubated in blocking buffer containing horseradish peroxidase (HRP)-conjugated goat anti-mouse IgG (1:5000, Southern Biotech, Cat. No. 1030-05, Birmingham, AL), and detection was performed with ECL reagent using the Amersham Imager 680 (GE Healthcare, Chicago, IL, USA).
2.5. Pseudovirus-Based Neutralization Assay (PBNA)
Vero76 cells were seeded onto a black, flat-bottomed 96-well assay plate (Corning, Cat. No. 3916, Phoenix, Phoenix, AZ, USA) and incubated at 37 °C with 5% CO
2 for 24 h. Mouse and rabbit serum samples were serially diluted 2-fold starting from 1/10 to 1/1280 and incubated with rVSV-NiV-F/G diluted to 200 TCID
50 in DMEM containing 10% FBS and 1× P/S at room temperature (20–25 °C) for 1 h. The infectious titer of the pseudovirus (expressed as TCID
50) was determined as described in
Section 2.6. A rabbit anti-NiV glycoprotein antibody (Alpha Diagnostic International, Cat. No. NIV11-S, San Antonio, TX, USA), raised against recombinant full-length NiV G glycoprotein (UniProt Q9IH62), was used as the positive control and diluted 3-fold starting from 1/20 to 1/43740. Normal rabbit control IgG (Sino Biological Cat. No. CR1 HC13MA0602, Beijing, China) was used as a negative control.
After incubation, the cell culture medium was removed from the Vero76 cells, and the serum–pseudovirus mixture was added to the cells. The plates were then incubated at 37 °C with 5% CO
2 for 24 h, following which the mixture was removed, and the Vero76 cells were lysed with 50 μL of ONE-Glo™ EX Reagent (Promega, Cat. No. E8130, Madison, WI, USA) on a Microplate Shaker (Jeio Tech, Cat. No. CPS-350, Daejeon, Korea) at 600 rpm for 5 min. Bioluminescence was measured in relative light units (RLUs) at 570 nm using a SpectraMax L Microplate Reader (Molecular Devices, San Jose, CA, USA). Finally, the percentage of neutralization was calculated and the half-maximal inhibitory concentration (IC
50) was determined using the GraphPad Prism 10 software [
10].
2.6. Determination of Infectious Concentration of the Experimental Pseudovirus
Vero76 cells were seeded into 96-well assay plates and cultured at 37 °C in a 5% CO
2 atmosphere. Then, 24 h after seeding, the culture medium was removed. Purified rVSV-NiV-F/G was obtained from the lower fraction collected after ultracentrifugation under the conditions described in
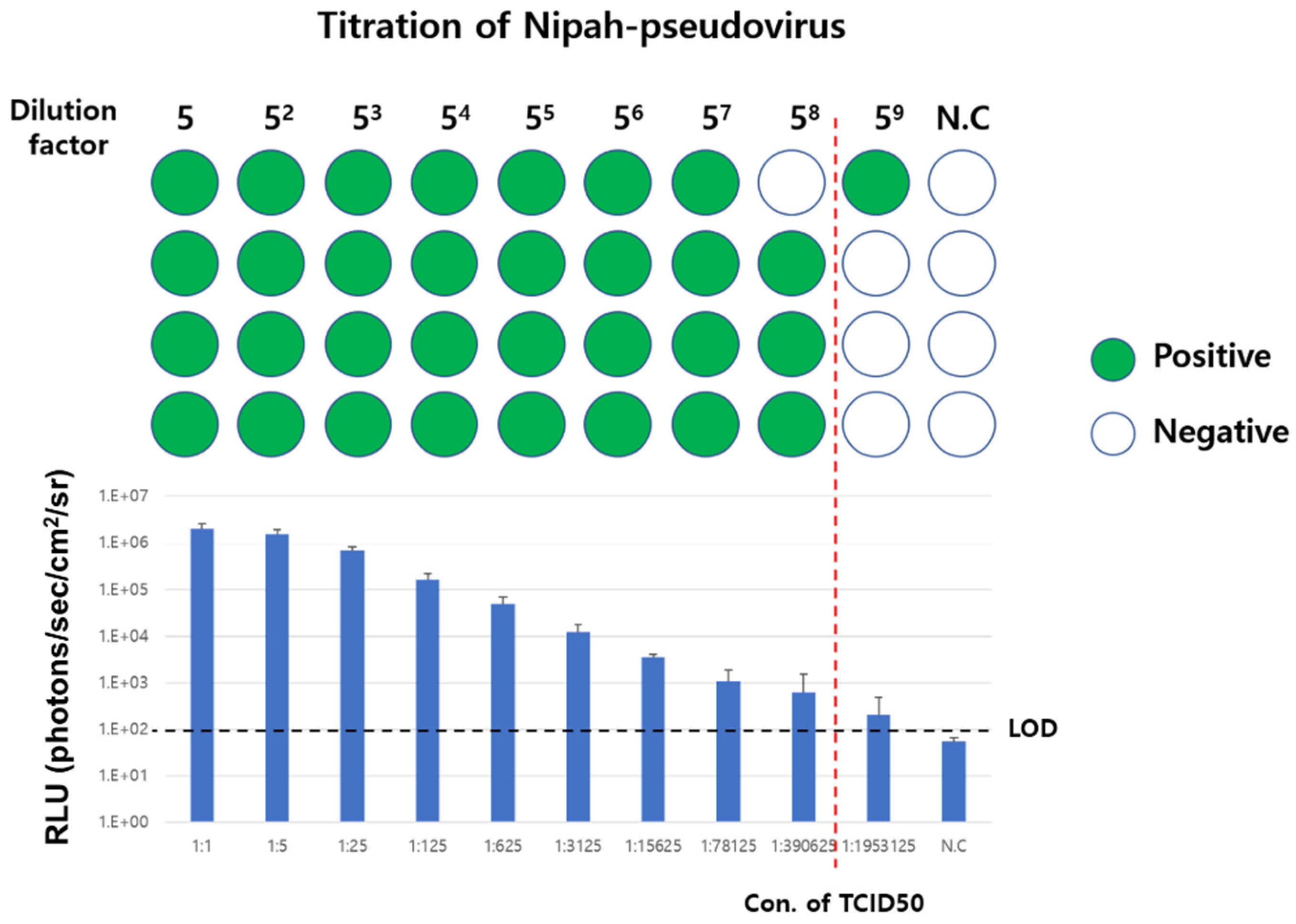
Section 2.4. The purified pseudovirus was diluted five-fold (four replicates for each concentration) in fresh culture medium and added to each well to induce pseudovirus infection. Lastly, 24 h after infection, the bioluminescence of each well was measured as described above.
To determine whether a well was infected, the average of the luminescence signal of cells to which no pseudovirus was added was used as a negative control, and wells in which the recorded luminescence signal was more than three times that of the “negative” control were determined as “positive” wells. Based on the “negative” and “positive” results of each well, the tissue culture infectious dose 50% (TCID
50) was calculated by the method of Reed and Muench [
11].
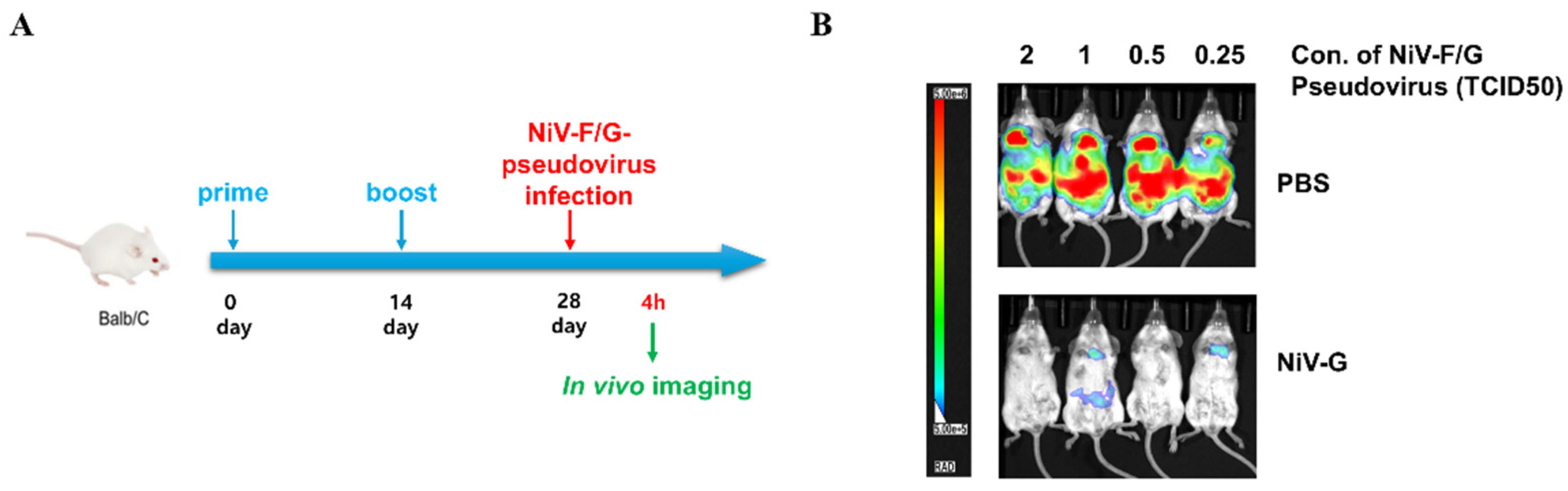
2.7. In Vivo Evaluation of Protective Efficacy for NiV Vaccine Candidates
Six-week-old BALB/c mice were purchased from Orient Bio (Seongnam, Korea) and acclimated to the animal facility for 1 week. After the acclimation period, the mice were randomly divided into two groups (four mice per group): PBS (control group) and NiV-G (vaccination group). Purified recombinant NiV-G protein (183-602 aa) was kindly provided from the laboratory of Dae Gwin Jeong at the Korea Research Institute of Bioscience and Biotechnology (KRIBB) and used for vaccination. Mice in each group received either the vaccine (10 μg/mouse) formulated with aluminum hydroxide (Alhydrogel adjuvant 2%; InvivoGen, Toulouse, France) or PBS (A total of eight mice were used, N = 1 for each concentration treatment for each of the two experimental groups). The vaccine was injected intramuscularly twice with a 2-week interval between injections. Two weeks after the 2nd vaccination, purified rVSV-NiV-F/G was intraperitoneally administered to each mouse at the indicated concentrations; 2, 1, 0.5, and 0.25 TCID50. The pseudovirus did not cause any suffering to the experimental subjects and no unexpected adverse events were observed.
According to a previous in vivo imaging study using VSV-based pseudoviruses [
5], four hours after NiV-F/G-pseudovirus infection, in vivo bioluminescence imaging was conducted using an in vivo imaging system (Spectral Instruments Imaging, Tucson, AZ, USA) at the Core Facility for Cell-to-In Vivo Imaging of the Lee Gil Ya Cancer and Diabetes Institute of Gachon University. Mice were administered an intraperitoneal injection of RediJect D-luciferin (150 μL/mouse; 150 mg/kg body weight; Perkin Elmer, Waltham, MD, USA). Then, the mice were anesthetized in an induction chamber with 3% isoflurane (Hana Pharm Co., Ltd., Hwaseong, Korea) at a flow rate of 0.5 L/min. Bioluminescent signals were detected 10 min later using the Aura Image Analysis Software (Version 2.2.1.1, Spectral Instruments Imaging, Tucson, AZ, USA). Relative bioluminescence signals were measured in photons per section per square centimeter per steradian (photons/sec/cm
2/sr) and are shown as RLU. In vivo experiments were performed using a minimal number of animals to demonstrate the feasibility of applying pseudoviruses to animal testing. No data were excluded from the dataset obtained from each experiment. Animal experiments were conducted with approval from the Center of Animal Care and Use of the Lee Gil Ya Cancer and Diabetes Institute of Gachon University (LCDI-2023-0144).
4. Discussion
In this study, we developed a replication-incompetent rVSV pseudotyped with the NiV F and G glycoproteins using a luciferase reporter gene. Our system enables both in vitro and in vivo evaluation of NiV-specific immune responses under BSL-2 conditions and offers a safer and scalable platform for preclinical vaccine assessment.
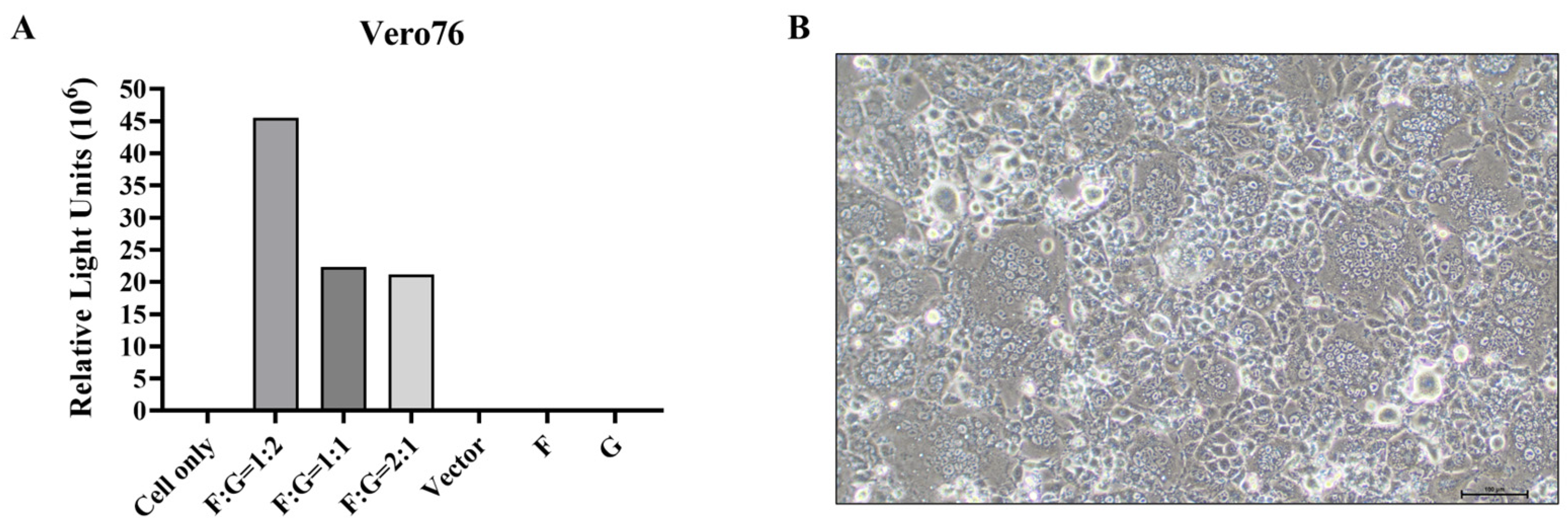
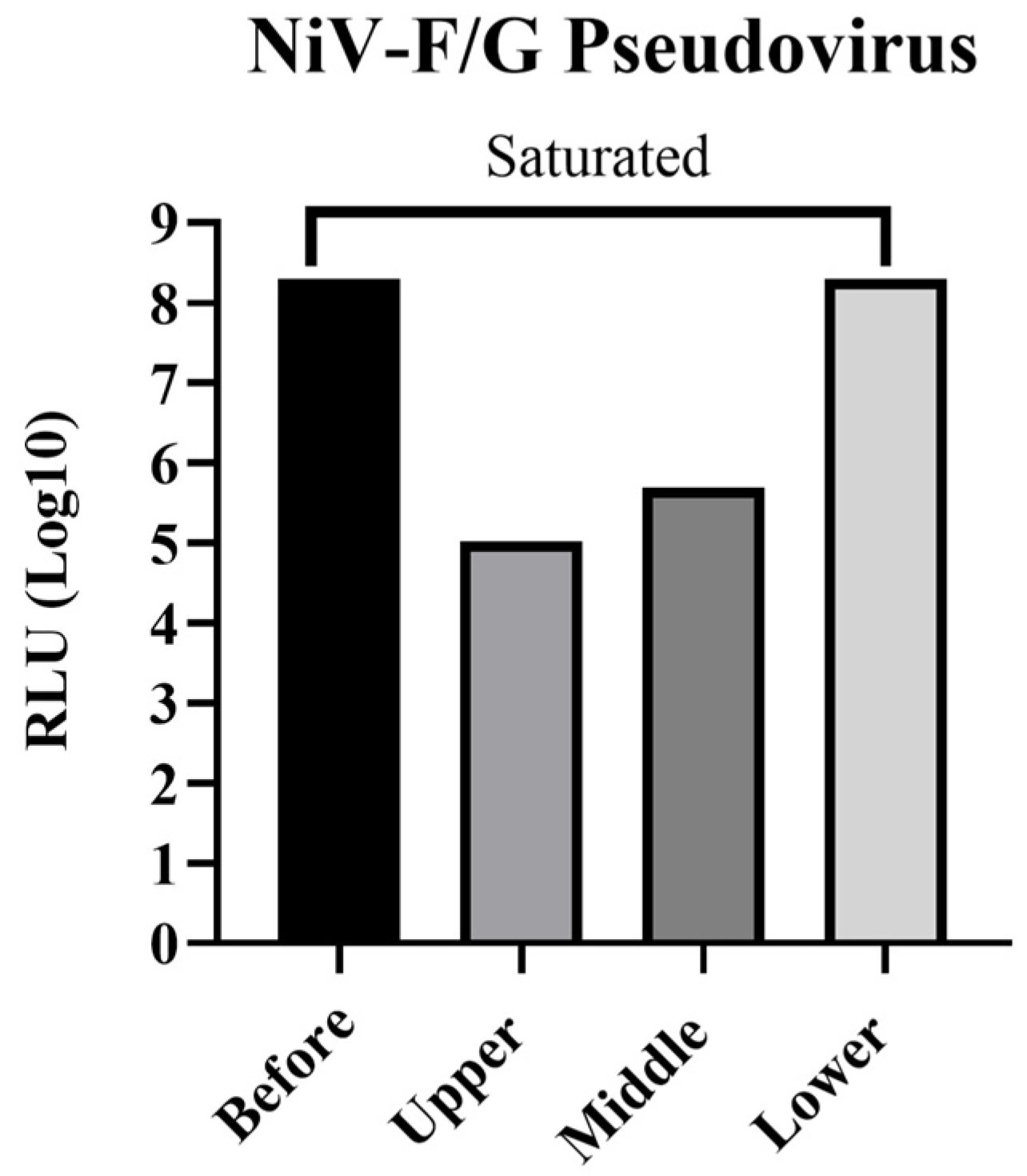
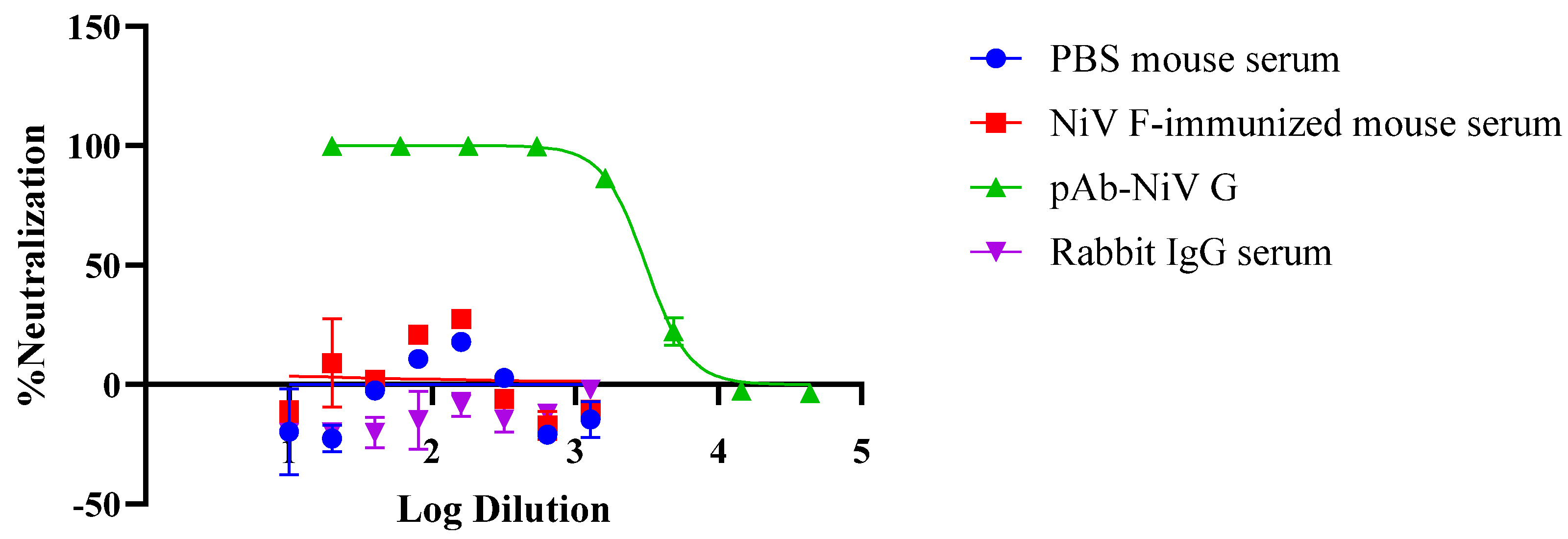
We determined the optimal F:G plasmid transfection ratio for the production of a pseudovirus and verified an enhancement of transduction efficiency using a luciferase assay. Further, ultracentrifugation and fractionation enabled the enrichment of high-titer pseudovirus fractions, hence providing an effective method for concentration and purification during the preparation of the experimental pseudovirus. Western blot and immunoprecipitation analyses confirmed the incorporation of both the precursor (F0) and cleaved (F1) forms of the NiV F glycoprotein, alongside NiV G, into pseudovirions. These findings indicate proper processing and membrane integration of envelope glycoproteins that are essential for accurately mimicking viral entry and performing robust and efficient neutralization assays [
12,
13].
Syncytia formation during the production of the pseudovirus was also observed. Co-transfection with NiV-F and NiV-G resulted in pronounced syncytia formation in pCAGGS-NiV-F/G-transfected cells, whereas the control groups (vector only, F only, and G only) did not exhibit any syncytia formation (
Figure 1B). These observations suggest that the co-expression of both NiV-F and NiV-G is required for effective production of the pseudovirus. This requirement is consistent with the well-characterized mechanism at play in henipaviruses, in which case, NiV-G binding to ephrin-B2/B3 triggers the conformational activation of NiV-F to mediate membrane fusion and syncytia formation, whereas the expression of either glycoprotein alone fails to produce CPE [
14,
15].
Importantly, our experiments served as a proof-of-principle for the applicability of this system in real-time in vivo imaging. Specifically, using a luciferase-based bioluminescence imaging platform, we established a mouse model in which NiV-F/G-pseudotyped rVSV was administered intraperitoneally to visualize infection. Strong luminescent signals were observed at the injection site and in the thoracic region of non-immunized mice, whereas vaccinated animals immunized with the recombinant NiV-G protein, which has been proposed as a promising target antigen for vaccines to prevent Nipah virus infection [
16,
17,
18], showed significantly reduced luminescence. And, although statistically limited, our study also demonstrated that NiV-G antigen effectively induced protective immunity (
Figure 6). These results confirm the applicability of our pseudovirus system for evaluating vaccine-mediated protection in vivo and are consistent with the potential protective efficacy of NiV-G suggested by previous studies [
19,
20]. This dual in vitro and in vivo evaluation strongly supports the usefulness of the G protein as a promising target for NiV vaccine design and justifies other pandemic-preparedness agendas using the systems reported herein.
The proposed rVSV-based model shows several advantages. The VSV genome replicates and is transcribed exclusively in the cytoplasm, with an mRNA half-life of only a few minutes, thus driving robust luciferase or fluorescent protein expression detectable as early as 2–6 h post-infection [
21,
22]. In turn, this enables rapid, single-day neutralization or entry-inhibition assays, in contrast to lentiviral pseudotypes, which typically require 48–72 h to reach assay endpoints [
6,
21,
23]. Additionally, it is known that Nipah virus infection primarily begins in respiratory and lung epithelial cells, and then, as the infection progresses, enters the bloodstream and spreads to various organs, including the brain [
24]. In our current study (
Figure 6), the observation of a strong signal in the thoracic region by intraperitoneally administered Nipah pseudovirus suggests that pseudovirus systems can mimic the physiological infection pattern of authentic Nipah virus. At the same time, the strong signal at the pseudovirus injection site suggests that the infection can be preferentially induced at the injection site, implying the possibility of establishing an organ-specific infection model using pseudovirus.
Furthermore, ΔG pseudotyped viruses are replication-defective, as they undergo only one round of infection because progeny virions lack envelope proteins. This feature allows studies involving high-risk viral glycoproteins, such as those from Ebola, Nipah, MERS-CoV, and SARS-CoV-2, to be performed under BSL-2 conditions, thereby overcoming infrastructure barriers and enabling broader collaborative research.
While ΔG-pseudotyped VSV particles have been explored for in vitro entry and neutralization assays, reports on their use for real-time in vivo imaging of protective efficacy in small animal models have remained limited. Our findings fill this gap by evaluating a non-replicating BSL-2-compatible pseudovirus-based infection model that enables visual monitoring of vaccine-induced protection in vivo.
Despite these strengths, this platform shows some limitations. Foremost, the use of recombinant VSV-expressed proteins NiV-F and NiV-G and antibodies raised against recombinant antigens is an important limitation of our study, as, despite sequence identity, such systems may not fully reproduce the post-translational modifications, conformational dynamics, and immunogenic properties of natural Nipah virus proteins or antibodies elicited by natural infections. Hence, future verification using authentic Nipah virus isolates and sera from convalescent patients would lend decisive support to the findings reported herein. In addition, as non-replicating viruses, pseudoviruses do not recapitulate systemic viral replication, dissemination, or pathogenesis. In addition, the platform primarily captures humoral immune responses and may not fully account for the contributions of T cell-mediated immunity, which is important in the context of NiV protection. Finally, although common, the use of Vero76 cells for neutralization assays may not reflect the full range of host-specific receptor interactions.
Nevertheless, the NiV F/G-pseudotyped rVSV system described herein provides a novel, robust, and versatile tool for evaluating neutralizing antibodies and vaccine candidates under accessible biosafety conditions. In particular, its ability to enable both in vitro analysis and in vivo bioluminescence imaging offers new opportunities for rapid and safe preclinical assessment of novel immunogens and may be readily adapted for other emerging high-containment pathogens.