COVID-19 and HIV: Clinical Outcomes and Inflammatory Markers in a Cohort from a Reference Hospital in Rio de Janeiro, Brazil
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Enrollment and Study Design
2.2. Clinical Profiles at Presentation
2.3. HIV Diagnosis
2.4. Plasmatic Inflammatory Markers
2.5. Statistical Analysis
3. Results
3.1. Sociodemographic and Clinical Characteristics of the Cohort
3.2. Sociodemographic and Clinical Characteristics of the COVID/PLWH Group
3.3. Clinical Blood Parameters and Plasma Cytokines Among COVID-19 Individuals with Distinct Severity Profiles
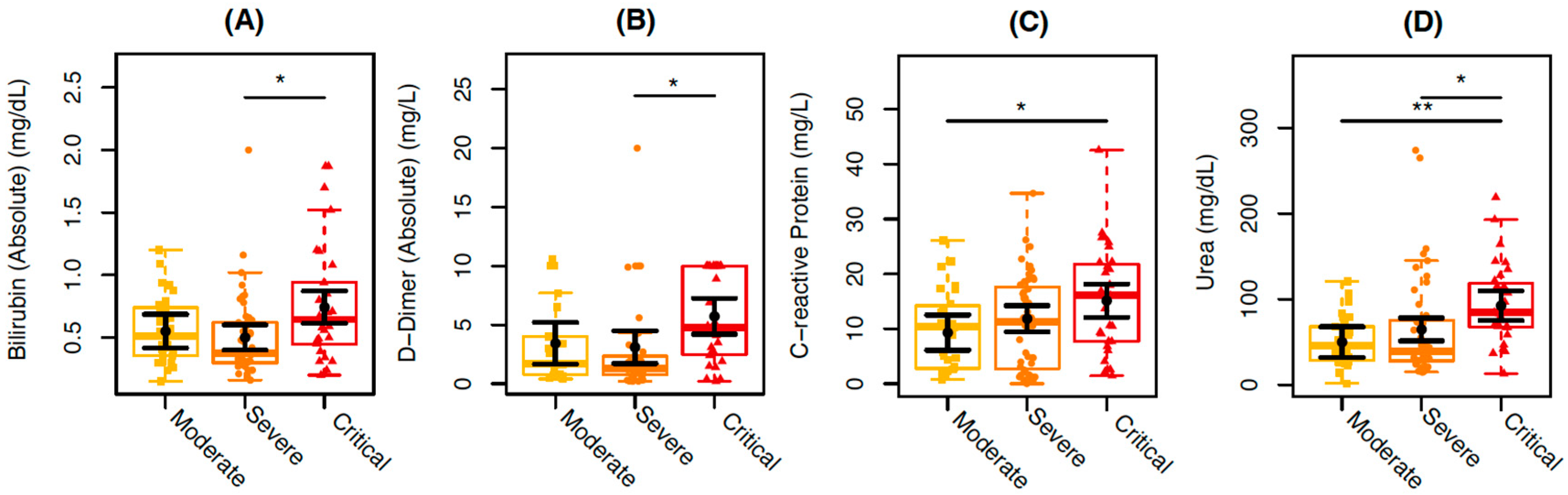
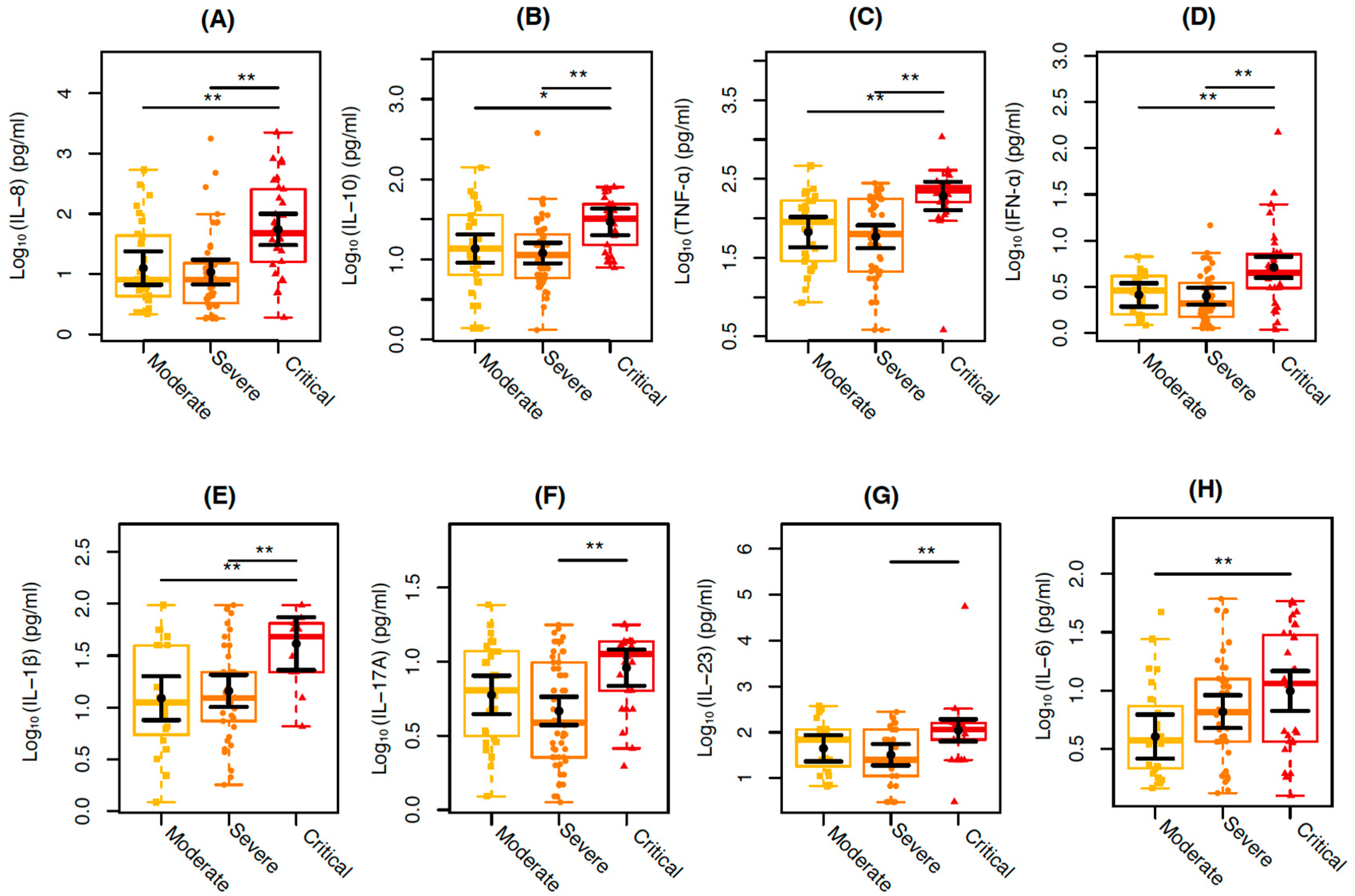
3.4. Clinical Blood Parameters and Cytokines Markers of COVID-19 and COVID/PLWH Individuals
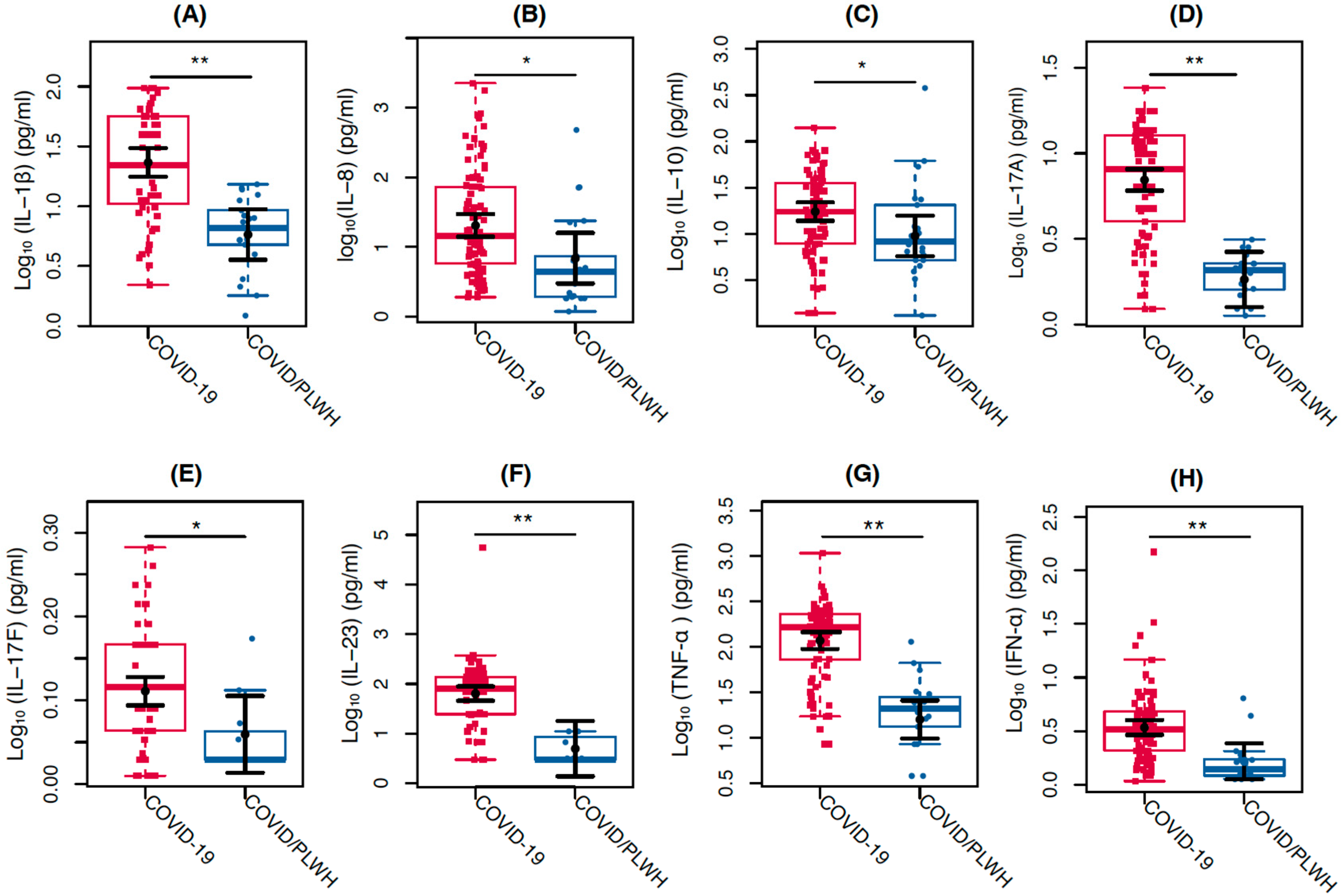
3.5. Correlations Between the Clinical Laboratory and Cytokines Markers
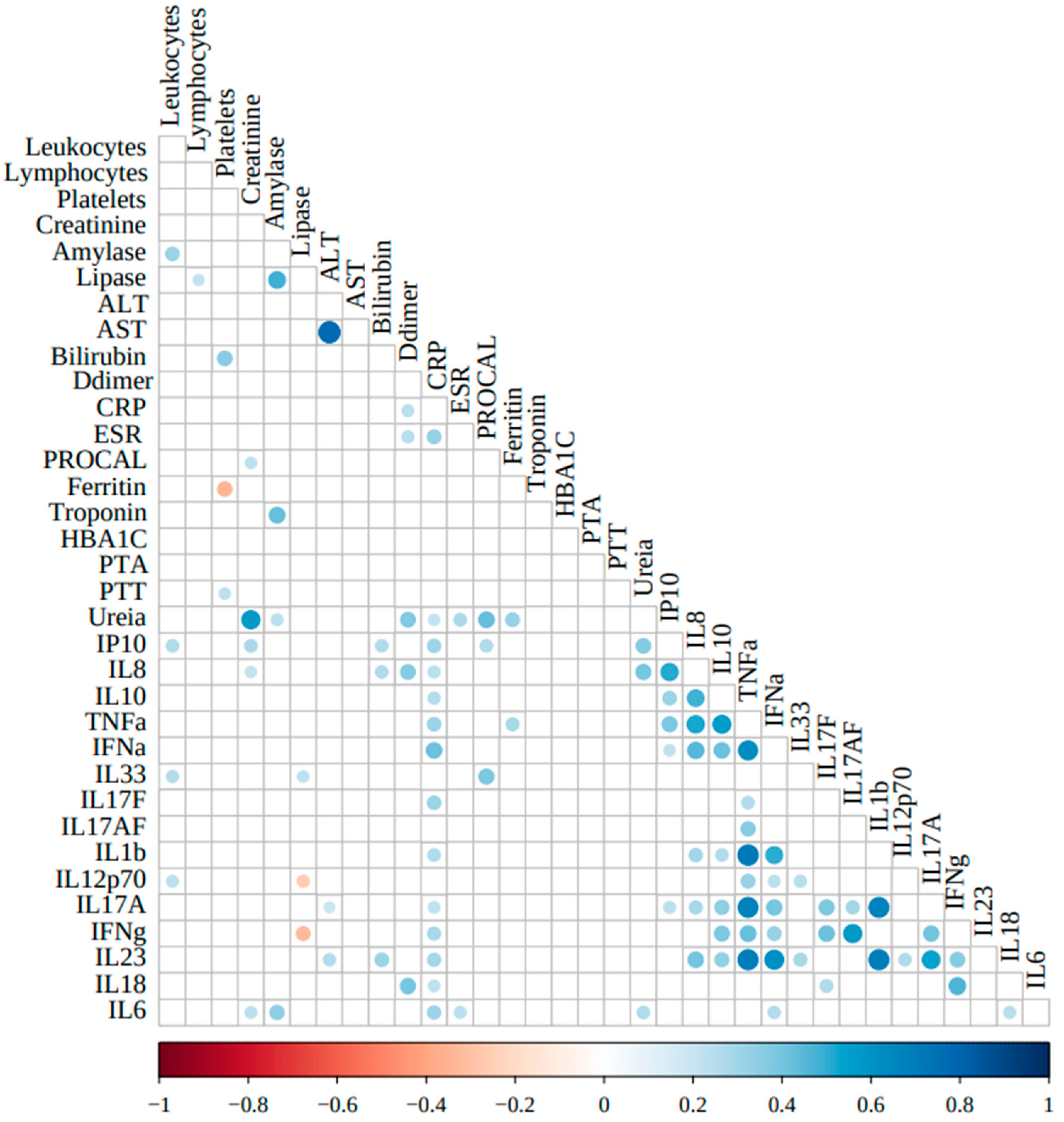
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gao, G.F. From “A”IV to “Z”IKV: Attacks from Emerging and Re-emerging Pathogens. Cell 2018, 172, 1157–1159. [Google Scholar] [CrossRef]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard|WHO Coronavirus (COVID-19) Dashboard with Vaccination Data 2022. Available online: https://covid19.who.int/ (accessed on 16 January 2022).
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Han, Y.; Zhang, H.; Mu, S.; Wei, W.; Jin, C.; Tong, C.; Song, Z.; Zha, Y.; Xue, Y.; Gu, G. Lactate dehydrogenase, an independent risk factor of severe COVID-19 patients: A retrospective and observational study. Aging (Albany N.Y.) 2020, 12, 11245–11258. [Google Scholar] [CrossRef] [PubMed]
- Chi, Y.; Ge, Y.; Wu, B.; Zhang, W.; Wu, T.; Wen, T.; Liu, J.; Guo, X.; Huang, C.; Jiao, Y.; et al. Serum Cytokine and Chemokine Profile in Relation to the Severity of Coronavirus Disease 2019 in China. J. Infect. Dis. 2020, 222, 746–754. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497. [Google Scholar] [CrossRef]
- Zhang, J.-J.; Dong, X.; Liu, G.-H.; Gao, Y.-D. Risk and Protective Factors for COVID-19 Morbidity, Severity, and Mortality. Clin. Rev. Allergy Immunol. 2022, 64, 90–107. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Chi, J.; Lv, W.; Wang, Y. Obesity and diabetes as high-risk factors for severe coronavirus disease 2019 (COVID-19). Diabetes Metab. Res. Rev. 2021, 37, e3377. [Google Scholar] [CrossRef]
- Bhaskaran, K.; Rentsch, C.T.; MacKenna, B.; Schultze, A.; Mehrkar, A.; Bates, C.J.; Eggo, R.M.; Morton, C.E.; Bacon, S.C.J.; Inglesby, P.; et al. HIV infection and COVID-19 death: A population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet HIV 2021, 8, e24. [Google Scholar] [CrossRef]
- Castel, A.D.; Wilbourn, B.; Magnus, M.; Greenberg, A.E. SARS-CoV-2 and HIV: Epidemiology, treatment, and lessons learned from HIV. AIDS Rev. 2020, 22, 133–142. [Google Scholar] [CrossRef]
- Ssentongo, P.; Heilbrunn, E.S.; Ssentongo, A.E.; Advani, S.; Chinchilli, V.M.; Nunez, J.J.; Du, P. Epidemiology and outcomes of COVID-19 in HIV-infected individuals: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 6283. [Google Scholar] [CrossRef] [PubMed]
- Shiau, S.; Krause, K.D.; Valera, P.; Swaminathan, S.; Halkitis, P.N. The Burden of COVID-19 in People Living with HIV: A Syndemic Perspective. AIDS Behav. 2020, 24, 2244. [Google Scholar] [CrossRef] [PubMed]
- Ambrosioni, J.; Blanco, J.L.; Reyes-Urueña, J.M.; Davies, M.A.; Sued, O.; Marcos, M.A.; Martínez, E.; Bertagnolio, S.; Alcamí, J.; Miro, J.M.; et al. Overview of SARS-CoV-2 infection in adults living with HIV. Lancet HIV 2021, 8, e294. [Google Scholar] [CrossRef]
- Prabhu, S.; Poongulali, S.; Kumarasamy, N. Impact of COVID-19 on people living with HIV: A review. J. Virus Erad. 2020, 6, 100019. [Google Scholar] [CrossRef] [PubMed]
- Perazzo, H.; Cardoso, S.W.; Ribeiro, M.P.D.; Moreira, R.; Coelho, L.E.; Jalil, E.M.; Japiassú, A.M.; Gouvêa, E.P.; Nunes, E.P.; Andrade, H.B.; et al. In-hospital mortality and severe outcomes after hospital discharge due to COVID-19: A prospective multicenter study from Brazil. Lancet Reg. Health Am. 2022, 11, 100244. [Google Scholar] [CrossRef] [PubMed]
- de Sá, N.B.R.; Neira-Goulart, M.; Ribeiro-Alves, M.; Perazzo, H.; Geraldo, K.M.; Ribeiro, M.P.D.; Cardoso, S.W.; Grinsztejn, B.; Veloso, V.G.; Capão, A.; et al. Inflammasome Genetic Variants Are Associated with Protection to Clinical Severity of COVID-19 among Patients from Rio de Janeiro, Brazil. Biomed. Res. Int. 2022, 2022, 9082455. [Google Scholar] [CrossRef]
- Neira-Goulart, M.; de Sá, N.B.R.; Ribeiro-Alves, M.; Perazzo, H.; Geraldo, K.M.; Ribeiro, M.P.D.; Cardoso, S.W.; Grinsztejn, B.; Veloso, V.G.; Gomes, L.R.; et al. Inflammasome genes polymorphisms are associated with progression to mechanical ventilation and death in a cohort of hospitalized COVID-19 patients in a reference hospital in Rio de Janeiro, Brazil. Gene 2023, 865, 147325. [Google Scholar] [CrossRef] [PubMed]
- Instituto Brasileiro de Geografia e Estatística. Características étnico—Raciais da população: Classificação e identidades. In Estudos e Análises: Informação Demográfica e Socioeconômica; Instituto Brasileiro de Geografia e Estatística: Rio de Janeiro, Brazil, 2013; pp. 83–99.
- WHO Working Group on the Clinical Characterisation and Management of COVID-19 Infection. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect. Dis. 2020, 20, e192–e197, Erratum in Lancet Infect. Dis. 2020, 20, e250. https://doi.org/10.1016/S1473-3099(20)30637-X. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hastak, P.; Cromer, D.; Malycha, J.; Andersen, C.R.; Raith, E.; Davenport, M.P.; Plummer, M.; Sasson, S.C. Defining the correlates of lymphopenia and independent predictors of poor clinical outcome in adults hospitalized with COVID-19 in Australia. Sci. Rep. 2024, 14, 11102. [Google Scholar] [CrossRef]
- Hottz, E.D.; Azevedo-Quintanilha, I.G.; Palhinha, L.; Teixeira, L.; Barreto, E.A.; Pão, C.R.R.; Righy, C.; Franco, S.; Souza, T.M.; Kurtz, P.; et al. Platelet activation and platelet-monocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19. Blood 2020, 136, 1330–1341. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Yan, X.; Fan, Q.; Liu, H.; Liu, X.; Liu, Z.; Zhang, Z. D-dimer levels on admission to predict in-hospital mortality in patients with COVID-19. J. Thromb. Haemost. 2020, 18, 1324. [Google Scholar] [CrossRef]
- Tang, N.; Li, D.; Wang, X.; Sun, Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020, 18, 844. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Wu, D.; Guo, W.; Cao, Y.; Huang, D.; Wang, H.; Wang, T.; Zhang, X.; Chen, H.; Yu, H.; et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J. Clin. Investig. 2020, 130, 2620–2629. [Google Scholar] [CrossRef]
- Smail, S.W.; Babaei, E.; Amin, K.; Abdulahad, W.H. Serum IL-23, IL-10, and TNF-α predict in-hospital mortality in COVID-19 patients. Front. Immunol. 2023, 14, 1145840. [Google Scholar] [CrossRef] [PubMed]
- Kong, B.; Lai, Y. IL-17 family cytokines in inflammatory or autoimmune skin diseases. Adv. Immunol. 2024, 163, 21–49. [Google Scholar] [PubMed]
- Navarro-Compán, V.; Puig, L.; Vidal, S.; Ramírez, J.; Llamas-Velasco, M.; Fernández-Carballido, C.; Almodóvar, R.; Pinto, J.A.; Galíndez-Aguirregoikoa, E.; Zarco, P.; et al. The paradigm of IL-23-independent production of IL-17F and IL-17A and their role in chronic inflammatory diseases. Front. Immunol. 2023, 14, 1191782. [Google Scholar]
- Shibabaw, T. Inflammatory Cytokine: IL-17A Signaling Pathway in Patients Present with COVID-19 and Current Treatment Strategy. J. Inflamm. Res. 2020, 13, 673. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Clinical Features and Prognostic Factors of COVID-19 in People Living with HIV Hospitalized with Suspected or Confirmed SARS-CoV-2 Infection; World Health Organization: Geneva, Switzerland, 2021.
- Favara, G.; Barchitta, M.; Maugeri, A.; Faro, G.; Agodi, A. HIV infection does not affect the risk of death of COVID-19 patients: A systematic review and meta-analysis of epidemiological studies. J. Glob. Health 2022, 12, 05036. [Google Scholar] [CrossRef] [PubMed]
- Anzurez, A.; Runtuwene, L.; Dang, T.T.T.; Nakayama-Hosoya, K.; Koga, M.; Yoshimura, Y.; Sasaki, H.; Miyata, N.; Miyazaki, K.; Takahashi, Y.; et al. Characterization of proinflammatory cytokines profile during acute SARS-CoV-2 infection in people with human immunodeficiency virus. Jpn J. Infect. Dis. 2024, 77, 301–310. [Google Scholar] [CrossRef]
| Features | Overall N = 134 | Moderate N = 30 | Severe N = 67 | Critical N = 32 | p-Value a | |
|---|---|---|---|---|---|---|
| Sociodemographic | ||||||
| Gender *; n (%) | Female | 60 (44.8%) | 15 (50%) | 29 (43.3%) | 13(40.6%) | 0.742 |
| Male | 74 (55.2%) | 15 (50%) | 38 (56.7%) | 19 (59.4%) | ||
| Skin Color; n (%) | White | 21 (15.7%) | 4 (13.3%) | 8 (11.9%) | 8 (25%) | NC |
| Brown | 91 (67.9%) | 21 (70%) | 46 (68.7%) | 22 (68.8%) | ||
| Black | 10 (7.5%) | 4 (13.3%) | 5 (7.5%) | 1 (3.1%) | ||
| Others | 2 (1.5%) | 0 (0%) | 2 (3%) | 0 (0%) | ||
| Age; n (IQR) | 58.22 (IQR = 21.3) | 60.27 (IQR = 18.61) | 55.49 (IQR = 19.8) | 65.85 (IQR = 25.61) | 0.104 | |
| (18–40] | 18 (13.8%) | 4 (13.8%) | 6 (9.1%) | 6 (19.4%) | 0.059 | |
| (40–60] | 49 (37.7%) | 9 (31%) | 33 (50%) | 6 (19.4%) | ||
| (60–80] | 57 (43.8%) | 13 (44.8%) | 26 (39.4%) | 17 (54.8%) | ||
| (80–90] | 6 (4.6%) | 3 (10.3%) | 1 (1.5%) | 2 (6.5%) | ||
| Schooling; n (%) | University education | 9 (8.8%) | 1 (4%) | 3 (6.4%) | 4 (16%) | 0.243 |
| High school | 44 (43.1%) | 9 (36%) | 20 (42.6%) | 13 (52%) | ||
| Low Education | 49 (48%) | 15 (60%) | 24 (51.1%) | 8 (32%) | ||
| Comorbidities | ||||||
| HAS; n (%) | No | 74 (55.2%) | 15 (50%) | 39 (58.2%) | 15 (46.9%) | 0.52 |
| Yes | 60 (44.8%) | 15 (50%) | 28 (41.8%) | 17 (53.1%) | ||
| Diabetes Mellitus (DM); n (%) | No | 94 (70.1%) | 23 (76.7%) | 41 (61.2%) | 26 (81.2%) | 0.082 |
| Yes | 40 (29.9%) | 7 (23.3%) | 26 (38.8%) | 6 (18.8%) | ||
| Cardiac Insufficiency; n (%) | No | 129 (96.3%) | 28 (93.3%) | 66 (98.5%) | 30 (93.8%) | 0.344 |
| Yes | 5 (3.7%) | 2 (6.7%) | 1 (1.5%) | 2 (6.2%) | ||
| COPD; n (%) | No | 124 (92.5%) | 29 (96.7%) | 64 (95.5%) | 27 (84.4%) | 0.084 |
| Yes | 10 (7.5%) | 1 (3.3%) | 3 (4.5%) | 5 (15.6%) | ||
| Coronary Artery Disease; n (%) | No | 133 (99.3%) | 29 (96.7%) | 67 (100%) | 32 (100%) | 0.19 |
| Yes | 1 (0.7%) | 1 (3.3%) | 0 (0%) | 0 (0%) | ||
| Obesity; n (%) | No | 113 (84.3%) | 24 (80%) | 58 (86.6%) | 27 (84.4%) | 0.711 |
| Yes | 21 (15.7%) | 6 (20%) | 9 (13.4%) | 5 (15.6%) | ||
| Active Tuberculosis; n (%) | No | 129 (96.3%) | 30 (100%) | 66 (98.5%) | 30 (93.8%) | 0.213 |
| Yes | 5 (3.7%) | 0 (0%) | 1 (1.5%) | 2 (6.2%) | ||
| HIV infection * | No | 112 (83.6%) | 29 (96.7%) | 51 (76.1%) | 31 (96.9%) | 0.003 |
| Yes | 22 (16.4%) | 1 (3.3%) | 16 (23.9%) | 1 (3.1%) | ||
| Symptoms | ||||||
| Fever; n (%) | No | 64 (47.8%) | 15 (50%) | 26 (38.8%) | 19 (59.4%) | 0.144 |
| Yes | 70 (52.2%) | 15 (50%) | 41 (61.2%) | 13 (40.6%) | ||
| Cough; n (%) | No | 49 (36.6%) | 8 (26.7%) | 21 (31.3%) | 18 (56.2%) | 0.025 |
| Yes | 85 (63.4%) | 22 (73.3%) | 46 (68.7%) | 14 (43.8%) | ||
| Chest Pain; n (%) | No | 116 (86.6%) | 27 (90%) | 55 (82.1%) | 30 (93.8%) | 0.232 |
| Yes | 18 (13.4%) | 3 (10%) | 12 (17.9%) | 2 (6.2%) | ||
| Coryza; n (%) | No | 125 (93.3%) | 28 (93.3%) | 63 (94%) | 30 (93.8%) | 0.991 |
| Yes | 9 (6.7%) | 2 (6.7%) | 4 (6%) | 2 (6.2%) | ||
| Dyspneia; n (%) | No | 29 (21.6%) | 4 (13.3%) | 14 (20.9%) | 8 (25%) | 0.507 |
| Yes | 105 (78.4%) | 26 (86.7%) | 53 (79.1%) | 24 (75%) | ||
| Odynophagy; n (%) | No | 132 (98.5%) | 29 (96.7%) | 66 (98.5%) | 32 (100%) | 0.568 |
| Yes | 2 (1.5%) | 1 (3.3%) | 1 (1.5%) | 0 (0%) | ||
| Anosmia; n (%) | No | 122 (91%) | 28 (93.3%) | 58 (86.6%) | 31 (96.9%) | 0.218 |
| Yes | 12 (9%) | 2 (6.7%) | 9 (13.4%) | 1 (3.1%) | ||
| Loss Of Taste; n (%) | No | 122 (91%) | 29 (96.7%) | 57 (85.1%) | 31 (96.9%) | 0.073 |
| Yes | 12 (9%) | 1 (3.3%) | 10 (14.9%) | 1 (3.1%) | ||
| Diarrhea; n (%) | No | 123 (91.8%) | 27 (90%) | 61 (91%) | 31 (96.9%) | 0.521 |
| Yes | 11 (8.2%) | 3 (10%) | 6 (9%) | 1 (3.1%) | ||
| Abdominal Pain; n (%) | No | 131 (97.8%) | 30 (100%) | 65 (97%) | 31 (96.9%) | 0.627 |
| Yes | 3 (2.2%) | 0 (0%) | 2 (3%) | 1 (3.1%) | ||
| Nausea; n (%) | No | 131 (97.8%) | 28 (93.3%) | 66 (98.5%) | 32 (100%) | 0.178 |
| Yes | 3 (2.2%) | 2 (6.7%) | 1 (1.5%) | 0 (0%) | ||
| Headache; n (%) | No | 120 (89.6%) | 28 (93.3%) | 57 (85.1%) | 30 (93.8%) | 0.302 |
| Yes | 14 (10.4%) | 2 (6.7%) | 10 (14.9%) | 2 (6.2%) | ||
| Myalgia; n (%) | No | 110 (82.1%) | 25 (83.3%) | 53 (79.1%) | 27 (84.4%) | 0.781 |
| Yes | 24 (17.9%) | 5 (16.7%) | 14 (20.9%) | 5 (15.6%) | ||
| Severity status | ||||||
| Oxygen supplementation or ventilatory support | No | 18 (13.4%) | 2 (6.7%) | 11 (16.4%) | 1 (3.1%) | 0.097 |
| Yes | 116 (86.6%) | 28 (93.3%) | 56 (83.6%) | 31 (96.9%) | ||
| WHO scale; n | 8 | 5 | 8 | 9 | NC | |
| Glasgow scale cat | (2.9,9] | 6 (5.6%) | 0 (0%) | 2 (3.4%) | 4 (21.1%) | 0.005 |
| (9,13] | 8 (7.5%) | 3 (12.5%) | 2 (3.4%) | 3 (15.8%) | ||
| (13,15.1] | 93 (86.9%) | 21 (87.5%) | 55 (93.2%) | 12 (63.2%) | ||
| SOFA cat | (0,10] | 127 (95.5%) | 30 (100%) | 64 (97%) | 28 (87.5%) | 0.044 |
| (10,12.1] | 6 (4.5%) | 0 (0%) | 2 (3%) | 4 (12.5%) | ||
| SAPS-III cat | (30.9,57] | 98 (73.7%) | 25 (83.3%) | 51 (77.3%) | 17 (53.1%) | 0.014 |
| (57,98.1] | 35 (26.3%) | 5 (16.7%) | 15 (22.7%) | 15 (46.9%) | ||
| Clinical Parameters of HIV-1 infection | ||||||
| CD4 counts, cells/mm3 (IQR) | 64 (IQR = 239) | 19 (IQR = 0) | 68.5 (IQR = 234) | 385 (IQR = 0) | 0.487 | |
| CD8 counts, cells/mm3 (IQR) | 514 (IQR = 351) | 520 (IQR = 0) | 467.5 (IQR = 488.75) | 719 (IQR = 0) | 0.74 | |
| Viral load, HIV RNA copies/mL (IQR) | 92,151 (IQR = 628,649.75) | 695 (IQR = 0) | 98,311 (IQR = 624,932.5) | 6938 (IQR = 0) | 0.187 | |
| Viral load Log10/mL | 4.96 (IQR = 1.94) | 2.84 (IQR = 0) | 4.99 (IQR = 1.4) | 3.84 (IQR = 0) | 0.187 | |
| Features | Overall N = 134 | COVID-19 N = 112 | COVID/PLWH N = 22 | p-Value a | |
|---|---|---|---|---|---|
| Sociodemographic | |||||
| Gender; n (%) | Female | 60 (44.8%) | 51 (45.5%) | 9 (40.9%) | 0.869 |
| Male | 74 (55.2%) | 61 (54.5%) | 13 (59.1%) | ||
| Skin Color; n (%) | White | 21 (15.7%) | 20 (17.9%) | 1 (4.5%) | NC |
| Brown | 91 (67.9%) | 74 (66.1%) | 17 (77.3%) | ||
| Black | 10 (7.5%) | 9 (8%) | 1 (4.5%) | ||
| Others | 2 (1.5%) | 2 (1.8%) | 0 (0%) | ||
| Age; n (IQR) | 58.22 (IQR = 21.3) | 62.61 (IQR = 19.37) | 44.37 (IQR = 17.84) | <0.001 | |
| (18–40] | 18 (13.8%) | 9 (8.2%) | 9 (45%) | <0.001 | |
| (40–60] | 49 (37.7%) | 41 (37.3%) | 8 (40%) | ||
| (60–80] | 57 (43.8%) | 54 (49.1%) | 3 (15%) | ||
| (80–90] | 6 (4.6%) | 6 (5.5%) | 0 (0%) | ||
| Schooling; n (%) | University education | 9 (8.8%) | 8 (9.1%) | 1 (7.1%) | 0.521 |
| High school | 44 (43.1%) | 36 (40.9%) | 8 (57.1%) | ||
| Low Education | 49 (48%) | 44 (50%) | 5 (35.7%) | ||
| Comorbidities | |||||
| HAS; n (%) | No | 74 (55.2%) | 56 (50%) | 18 (81.8%) | 0.012 |
| Yes | 60 (44.8%) | 56 (50%) | 4 (18.2%) | ||
| Diabetes Mellitus (DM); n (%) | No | 94 (70.1%) | 77 (68.8%) | 17 (77.3%) | 0.587 |
| Yes | 40 (29.9%) | 35 (31.2%) | 5 (22.7%) | ||
| Cardiac Insufficiency; n (%) | No | 129 (96.3%) | 107 (95.5%) | 22 (100%) | 0.693 |
| Yes | 5 (3.7%) | 5 (4.5%) | 0 (0%) | ||
| COPD; n (%) | No | 124 (92.5%) | 104 (92.9%) | 20 (90.9%) | 1 |
| Yes | 10 (7.5%) | 8 (7.1%) | 2 (9.1%) | ||
| Coronary Artery Disease; n (%) | No | 133 (99.3%) | 111 (99.1%) | 22 (100%) | 1 |
| Yes | 1 (0.7%) | 1 (0.9%) | 0 (0%) | ||
| Obesity; n (%) | No | 113 (84.3%) | 93 (83%) | 20 (90.9%) | 0.543 |
| Yes | 21 (15.7%) | 19 (17%) | 2 (9.1%) | ||
| Active Tuberculosis; n (%) | No | 129 (96.3%) | 111 (99.1%) | 18 (81.8%) | 0.001 |
| Yes | 5 (3.7%) | 1 (0.9%) | 4 (18.2%) | ||
| Symptoms | |||||
| Fever; n (%) | No | 64 (47.8%) | 55 (49.1%) | 9 (40.9%) | 0.638 |
| Yes | 70 (52.2%) | 57 (50.9%) | 13 (59.1%) | ||
| Cough; n (%) | No | 49 (36.6%) | 40 (35.7%) | 9 (40.9%) | 0.826 |
| Yes | 85 (63.4%) | 72 (64.3%) | 13 (59.1%) | ||
| Chest Pain; n (%) | No | 116 (86.6%) | 95 (84.8%) | 21 (95.5%) | 0.32 |
| Yes | 18 (13.4%) | 17 (15.2%) | 1 (4.5%) | ||
| Coryza; n (%) | No | 125 (93.3%) | 106 (94.6%) | 19 (86.4%) | 0.341 |
| Yes | 9 (6.7%) | 6 (5.4%) | 3 (13.6%) | ||
| Dyspnea; n (%) | No | 29 (21.6%) | 20 (17.9%) | 9 (40.9%) | 0.034 |
| Yes | 105 (78.4%) | 92 (82.1%) | 13 (59.1%) | ||
| Odynophagy; n (%) | No | 132 (98.5%) | 110 (98.2%) | 22 (100%) | 1 |
| Yes | 2 (1.5%) | 2 (1.8%) | 0 (0%) | ||
| Anosmia; n (%) | No | 122 (91%) | 100 (89.3%) | 22 (100%) | 0.23 |
| Yes | 12 (9%) | 12 (10.7%) | 0 (0%) | ||
| Loss Of Taste; n (%) | No | 122 (91%) | 100 (89.3%) | 22 (100%) | 0.23 |
| Yes | 12 (9%) | 12 (10.7%) | 0 (0%) | ||
| Diarrhea; n (%) | No | 123 (91.8%) | 103 (92%) | 20 (90.9%) | 1 |
| Yes | 11 (8.2%) | 9 (8%) | 2 (9.1%) | ||
| Abdominal Pain; n (%) | No | 131 (97.8%) | 109 (97.3%) | 22 (100%) | 1 |
| Yes | 3 (2.2%) | 3 (2.7%) | 0 (0%) | ||
| Nausea; n (%) | No | 131 (97.8%) | 109 (97.3%) | 22 (100%) | 1 |
| Yes | 3 (2.2%) | 3 (2.7%) | 0 (0%) | ||
| Headache; n (%) | No | 120 (89.6%) | 99 (88.4%) | 21 (95.5%) | 0.543 |
| Yes | 14 (10.4%) | 13 (11.6%) | 1 (4.5%) | ||
| Myalgia; n (%) | No | 110 (82.1%) | 93 (83%) | 17 (77.3%) | 0.734 |
| Yes | 24 (17.9%) | 19 (17%) | 5 (22.7%) | ||
| Severity status | |||||
| Oxygen supplementation or ventilatory support | No | 18 (13.4%) | 10 (8.9%) | 8 (36.4%) | 0.002 |
| Yes | 116 (86.6%) | 102 (91.1%) | 14 (63.6%) | ||
| WHO scale | 8 (IQR = 0) | 8 (IQR = 3.5) | 8 (IQR = 0) | 0.906 | |
| WHO scale cat | moderate | 30 (23.3%) | 29 (26.1%) | 1 (5.6%) | 0.106 |
| severe/critical | 99 (76.7%) | 82 (73.9%) | 17 (94.4%) | ||
| Glasgow scale cat | (2.9,9] | 6 (5.6%) | 5 (5.7%) | 1 (5%) | 0.361 |
| (9,13] | 8 (7.5%) | 8 (9.2%) | 0 (0%) | ||
| (13,15.1] | 93 (86.9%) | 74 (85.1%) | 19 (95%) | ||
| SOFA cat | (0,10] | 127 (95.5%) | 106 (95.5%) | 21 (95.5%) | 1 |
| (10,12.1] | 6 (4.5%) | 5 (4.5%) | 1 (4.5%) | ||
| SAPS-III cat | (30.9,57] | 98 (73.7%) | 81 (73%) | 17 (77.3%) | |
| (57,98.1] | 35 (26.3%) | 30 (27%) | 5 (22.7%) | ||
| Outcomes; n (%) | discharge | 80 (59.7%) | 66 (58.9%) | 14 (63.6%) | 0.862 |
| death | 54 (40.3%) | 46 (41.1%) | 8 (36.4%) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Sá, N.B.R.; Macieira, K.V.; Coelho, M.R.I.; Goulart, M.N.; Ribeiro-Alves, M.; Rosadas, L.A.d.S.; Geraldo, K.M.; Ribeiro, M.P.D.; Cardoso, S.W.; Grinsztejn, B.; et al. COVID-19 and HIV: Clinical Outcomes and Inflammatory Markers in a Cohort from a Reference Hospital in Rio de Janeiro, Brazil. Viruses 2025, 17, 91. https://doi.org/10.3390/v17010091
de Sá NBR, Macieira KV, Coelho MRI, Goulart MN, Ribeiro-Alves M, Rosadas LAdS, Geraldo KM, Ribeiro MPD, Cardoso SW, Grinsztejn B, et al. COVID-19 and HIV: Clinical Outcomes and Inflammatory Markers in a Cohort from a Reference Hospital in Rio de Janeiro, Brazil. Viruses. 2025; 17(1):91. https://doi.org/10.3390/v17010091
Chicago/Turabian Stylede Sá, Nathalia Beatriz Ramos, Karine Venegas Macieira, Mariana Rosa Inacio Coelho, Milena Neira Goulart, Marcelo Ribeiro-Alves, Leonardo Azevedo da Silva Rosadas, Kim Mattos Geraldo, Maria Pia Diniz Ribeiro, Sandra Wagner Cardoso, Beatriz Grinsztejn, and et al. 2025. "COVID-19 and HIV: Clinical Outcomes and Inflammatory Markers in a Cohort from a Reference Hospital in Rio de Janeiro, Brazil" Viruses 17, no. 1: 91. https://doi.org/10.3390/v17010091
APA Stylede Sá, N. B. R., Macieira, K. V., Coelho, M. R. I., Goulart, M. N., Ribeiro-Alves, M., Rosadas, L. A. d. S., Geraldo, K. M., Ribeiro, M. P. D., Cardoso, S. W., Grinsztejn, B., Veloso, V. G., Cazote, A. d. S., de Almeida, D. V., Giacoia-Gripp, C. B. W., Côrtes, F. H., & Morgado, M. G. (2025). COVID-19 and HIV: Clinical Outcomes and Inflammatory Markers in a Cohort from a Reference Hospital in Rio de Janeiro, Brazil. Viruses, 17(1), 91. https://doi.org/10.3390/v17010091








