Influence of Seropositivity against Adenovirus-36 on the Risk of Obesity and Insulin Resistance in the Child Population of Southern Chile
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Clinical Evaluation, Anthropometric Measurements, and Nutritional Status
2.3. Biochemical Determinations, Definition of Insulin Resistance and Dyslipidemias
2.4. Seropositivity against HAdv-D36
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Haslam, D.W.; James, W.P. Obesity. Lancet 2005, 366, 1197–1209. [Google Scholar] [CrossRef] [PubMed]
- Bridger, T. Childhood obesity and cardiovascular disease. Paediatr. Child Health 2009, 14, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Lobstein, T.; Baur, L.; Uauy, R. Obesity in children and young people: A crisis in public health. Obes. Rev. 2004, 5 (Suppl. S1), 4–104. [Google Scholar] [CrossRef] [PubMed]
- JUNAEB Mapa Nutricional. 2018. Available online: https://www.junaeb.cl/wp-content/uploads/2023/03/Informe-Mapa-Nutricional-2018-1.pdf (accessed on 1 June 2024).
- Weinsier, R.L.; Hunter, G.R.; Heini, A.F.; Goran, M.I.; Sell, S.M. The etiology of obesity: Relative contribution of metabolic factors, diet, and physical activity. Am. J. Med. 1998, 105, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Dhurandhar, N.V. Infectobesity: Obesity of infectious origin. J. Nutr. 2001, 131, 2794S–2797S. [Google Scholar] [CrossRef] [PubMed]
- Akheruzzaman, M.; Hegde, V.; Dhurandhar, N.V. Twenty-five years of research about adipogenic adenoviruses: A systematic review. Obes. Rev. 2019, 20, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Cancelier, A.C.L.; Rezin, G.T.; Fernandes, J.; Silva, H.C.G.; Trevisol, D.J.; Atkinson, R.L.; Schuelter-Trevisol, F. Adenovirus-36 as one of the causes of obesity: The review of the pathophysiology. Nutr. Res. 2021, 86, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Lynch, J.P.; Fishbein, M.; Echavarria, M. Adenovirus. Semin. Respir. Crit. Care Med. 2011, 32, 494–511. [Google Scholar] [CrossRef] [PubMed]
- Marjani, A.; Khatami, A.; Saadati, H.; Asghari, M.; Razizadeh, M.H.; Abbasi, A.; Zarei, M.; Beikzadeh, L.; Soleimani, A. Association of adenovirus 36 infection and obesity; An updated meta-analysis of community-based studies. Rev. Med. Virol. 2022, 32, e2255. [Google Scholar] [CrossRef] [PubMed]
- Sapunar, J.; Fonseca, L.; Molina, V.; Ortiz, E.; Barra, M.I.; Reimer, C.; Charles, M.; Schneider, C.; Ortiz, M.; Brito, R.; et al. Adenovirus 36 seropositivity is related to obesity risk, glycemic control, and leptin levels in Chilean subjects. Int. J. Obes. 2020, 44, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Task Force on Blood Pressure Control in Children. Report of the Second Task Force on Blood Pressure Control in Children—1987. Pediatrics 1987, 79, 1–25. [Google Scholar] [CrossRef]
- Barja, S.; Arnaiz, P.; Domínguez, A.; Villarroel, L.; Cassis, B.; Castillo, O.; Salomó, G.; Farías, M.; Goycoolea, M.; Quiroga, T.; et al. Normal plasma insulin and HOMA values among Chilean children and adolescents. Rev. Med. Chil. 2011, 139, 1435–1443. [Google Scholar] [CrossRef] [PubMed]
- Sapunar, J.; Aguilar-Farías, N.; Navarro, J.; Araneda, G.; Chandía-Poblete, D.; Manríquez, V.; Brito, R.; Cerda, Á. High prevalence of dyslipidemia and high atherogenic index of plasma in children and adolescents. Rev. Med. Chil. 2018, 146, 1112–1122. [Google Scholar] [CrossRef] [PubMed]
- Cristancho, A.G.; Lazar, M.A. Forming functional fat: A growing understanding of adipocyte differentiation. Nat. Rev. Mol. Cell Biol. 2011, 12, 722–734. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.E.; Schmidt, H.; Lai, B.; Ge, K. Transcriptional and Epigenomic Regulation of Adipogenesis. Mol. Cell. Biol. 2019, 39, e00601-18. [Google Scholar] [CrossRef] [PubMed]
- Vangipuram, S.D.; Sheele, J.; Atkinson, R.L.; Holland, T.C.; Dhurandhar, N.V. A human adenovirus enhances preadipocyte differentiation. Obes. Res. 2004, 12, 770–777. [Google Scholar] [CrossRef] [PubMed]
- Karamese, M.; Altoparlak, U.; Turgut, A.; Aydogdu, S.; Karamese, S.A. The relationship between adenovirus-36 seropositivity, obesity and metabolic profile in Turkish children and adults. Epidemiol. Infect. 2015, 143, 3550–3556. [Google Scholar] [CrossRef] [PubMed]
- Na, H.N.; Hong, Y.M.; Kim, J.; Kim, H.K.; Jo, I.; Nam, J.H. Association between human adenovirus-36 and lipid disorders in Korean schoolchildren. Int. J. Obes. 2010, 34, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Almgren, M.; Atkinson, R.; He, J.; Hilding, A.; Hagman, E.; Wolk, A.; Thorell, A.; Marcus, C.; Näslund, E.; Östenson, C.-G.; et al. Adenovirus-36 is associated with obesity in children and adults in Sweden as determined by rapid ELISA. PLoS ONE 2012, 7, e41652. [Google Scholar] [CrossRef] [PubMed]
- Cancelier, A.C.L.; Dhurandhar, N.V.; Peddibhotla, S.; Atkinson, R.L.; Silva, H.C.G.; Trevisol, D.J.; Schuelter-Trevisol, F. Adenovirus 36 infection and daycare starting age are associated with adiposity in children and adolescents. J. Pediatr. 2021, 97, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Parra-Rojas, I.; Del Moral-Hernández, O.; Salgado-Bernabé, A.B.; Guzmán-Guzmán, I.P.; Salgado-Goytia, L.; Muñoz-Valle, J.F. Adenovirus-36 seropositivity and its relation with obesity and metabolic profile in children. Int. J. Endocrinol. 2013, 2013, 463194. [Google Scholar] [CrossRef] [PubMed]
- Broderick, M.P.; Hansen, C.J.; Irvine, M.; Metzgar, D.; Campbell, K.; Baker, C.; Russell, K.L. Adenovirus 36 seropositivity is strongly associated with race and gender, but not obesity, among US military personnel. Int. J. Obes. 2010, 34, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Na, H.N.; Kim, J.; Lee, H.S.; Shim, K.W.; Kimm, H.; Jee, S.H.; Jo, I.; Nam, J.H. Association of human adenovirus-36 in overweight Korean adults. Int. J. Obes. 2012, 36, 281–285. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Pan, Q.; Wang, X.; Zhang, L.; Xiao, F.; Guo, L. The relationship between human adenovirus 36 and obesity in Chinese Han population. Biosci. Rep. 2018, 38, BSR20180553. [Google Scholar] [CrossRef] [PubMed]
- Kocazeybek, B.; Dinc, H.O.; Ergin, S.; Saribas, S.; Ozcabi, B.T.; Cizmecigil, U.; Altan, E.; Atalik, K.; Yüksel, P.; Taner, Z.; et al. Evaluation of Adenovirus-36 (HAdv-D36) antibody seropositivity and adipokine levels in obese children. Microb. Pathog. 2017, 108, 27–31. [Google Scholar] [CrossRef] [PubMed]
- da Silva Fernandes, J.; Schuelter-Trevisol, F.; Cancelier, A.C.L.; Gonçalves ESilva, H.C.; de Sousa, D.G.; Atkinson, R.L.; Trevisol, D.J. Adenovirus 36 prevalence and association with human obesity: A systematic review. Int. J. Obes. 2021, 45, 1342–1356. [Google Scholar] [CrossRef] [PubMed]
- Al-Beltagi, M.; Bediwy, A.S.; Saeed, N.K. Insulin-resistance in paediatric age: Its magnitude and implications. World J. Diabetes 2022, 13, 282–307. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total Group (208) | Normal Weight Group (60) | Overweight Group (79) | Obese Group (69) | p-Value |
|---|---|---|---|---|---|
| Clinical and biodemographic data | |||||
| Age, years | 10.4 ± 1.0 | 10.3 ± 1.0 | 10.4 ± 1.0 | 10.4 ± 1.1 | 0.647 |
| Tanner Stage [1–2/3–5], % | 66.2 (137) /33.8 (70) | 60.0 (36) /40.0 (24) | 62.8 (49) /37.2 (29) | 75.0 (51) /25.0 (17) | 0.144 |
| Sex [M/F], % | 48.3/51.7 (101/107) | 35.0/65.0 (21/39) | 50.6/49.4 (40/39) | 58.0/42.0 (40/29) | 0.029 |
| Dyslipidemia % | 38.3 (78) | 24.6 (14) | 34.2 (27) | 54.4 (37) | 0.002 |
| Insulin Resistance, % | 19 (39) | 5 (3) | 15 (12) | 35 (24) | <0.001 |
| SBP, mmHg DBP, mmHg | 109.6 ± 18.6 61.5 ± 16.7 | 105.3 ± 18.4 a 63.9 ± 17.8 | 107.6 ± 18.3 57.8 ± 13.8 a.b | 115.7± 18.1 b 64.4 ± 18.3 | <0.001 0.190 |
| Hypertension % | 35.5 (55) | 28.8 (13) | 28.8 (17) | 49.0% (25) | 0.050 |
| Anthropometric Parameters | |||||
| BMI z-score | 1.50 ± 0.67 | 0.35 ± 0.55 a | 1.42 ± 0.28 b | 2.58 ± 0.40 c | <0.001 |
| Body fat, % | 28.4± 8.7 | 21.7± 6.8 a | 27.3 ± 5.7 b | 36.4 ± 7.1 c | <0.001 |
| Biochemical Parameters | |||||
| Total Cholesterol, mg/dL | 154 ± 29 | 150 ± 32 | 154 ± 27 | 157 ± 28 | 0.392 |
| Triglycerides, mg/dL | 99 ± 68 | 80 ± 31 a | 90 ± 37 a | 127 ± 102 b | <0.001 |
| LDL cholesterol, mg/dL | 82 ± 24 | 79 ± 25 | 85 ± 23 | 87 ± 24 | 0.171 |
| HDL cholesterol, mg/dL | 51 ± 13 | 54 ± 14 a | 52 ± 12 a | 46 ± 13 b | <0.001 |
| Non-HDL cholesterol, mg/dL | 103 ± 30 | 97 ± 27 a | 103 ± 25 a.b | 112 ± 30 b | 0.003 |
| VLDL cholesterol, mg/dL | 20 ± 14 | 16 ± 6 a | 18 ± 8 a | 26 ± 21 b | <0.001 |
| Glucose, mg/dL | 85 ± 7 | 85 ± 6 | 85 ± 6 | 86 ± 9 | 0.844 |
| Insulin, μU/Ml | 14.1 ± 9.4 | 10.1 ± 5.5 a | 13.5 ± 8.2 b | 18.0 ± 11.6 c | <0.001 |
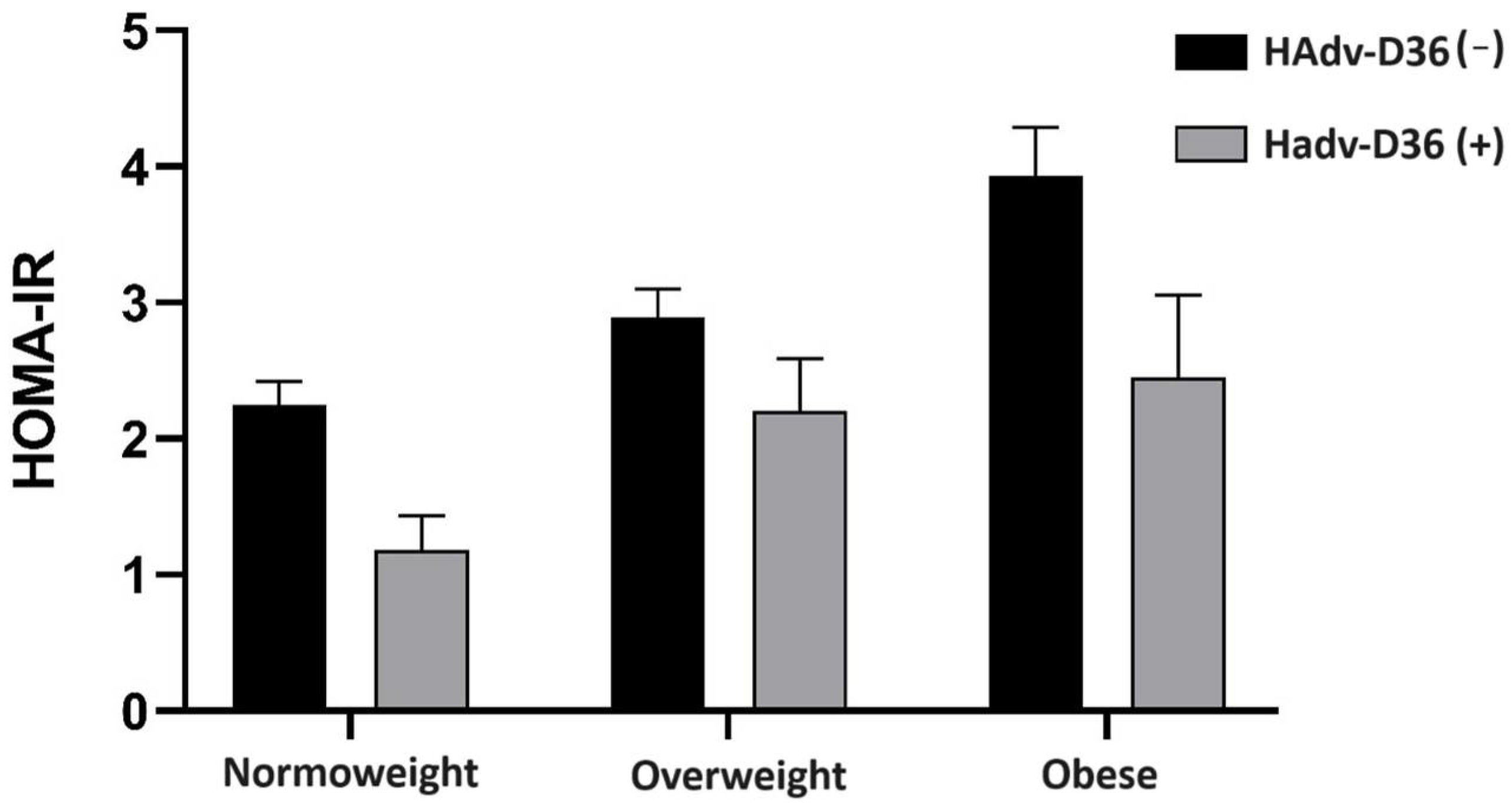
| HOMA-IR | 3.00 ± 2.58 | 2.15 ± 1.25 a | 2.86 ± 1.82 a | 3.86 ± 2.81 b | <0.001 |
| Serology | |||||
| Anti-HAdv-D36, % | 5.4% (11) | 8.8% (5) | 3.8% (3) | 4.4% (3) | 0.089 |
| Variables | HAdv-D36 (+) (11) | HAdv-D36 (−) (194) | p-Value |
|---|---|---|---|
| Clinical and biodemographic data | |||
| Age, years | 9.7 ± 1.01 | 10.4 ± 1.02 | 0.054 |
| Tanner Stage [1–2/3–5], % | 72.7 (8)/27.3 (3) | 66.2 (127)/33.9 (65) | 0.647 |
| Sex [M/F], % | 45.5 (5)/55.6 (6) | 49.5 (96)/50.5 (98) | 0.795 |
| Dyslipidemia % | 36.4 (4) | 38.2 (74) | 0.906 |
| SBP, mmHg | 107.7 ± 15.5 | 109.4 ± 18.7 | 0.864 |
| DBP, mmHg | 67.0 ± 18.4 | 61.2 ± 16.7 | 0.642 |
| Insulin Resistance, % | 0 (0) | 20.1 (39) | 0.029 |
| Anthropometric Parameters | |||
| BMI z-score | 1.12 ± 0.90 | 1.53 ± 0.97 | 0.174 |
| Body fat, % | 24.0 ± 7.5 | 28.8 ± 8.8 | 0.084 |
| Biochemical Parameters | |||
| Total cholesterol, mg/dL | 153.3 ± 17 | 154 ± 29 | 0.895 |
| Triglycerides, mg/dL | 99 ± 54 | 100 ± 69 | 0.953 |
| LDL Cholesterol, mg/dL | 88 ± 13 | 84 ± 24 | 0.346 |
| HDL Cholesterol, mg/dL | 46 ± 8 | 51 ± 14 | 0.063 |
| Non-HDL cholesterol, mg/Dl | 107 ± 13 | 103 ± 29 | 0.347 |
| VLDL cholesterol, mg/dL | 21 ± 12 | 20 ± 14 | 0.833 |
| Glucose, mg/dL | 83 ± 5 | 85 ± 7 | 0.134 |
| Insulin, μU/mL | 8.9 ± 4.7 | 14.4 ± 9.5 | 0.003 |
| HOMA-IR | 1.81 ± 0.86 | 3.07 ± 2.21 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brito, R.; Sapunar, J.; Aguilar-Farías, N.; Navarro-Riquelme, J.; Pavez, M.; Hirata, M.H.; Cerda, A. Influence of Seropositivity against Adenovirus-36 on the Risk of Obesity and Insulin Resistance in the Child Population of Southern Chile. Viruses 2024, 16, 995. https://doi.org/10.3390/v16060995
Brito R, Sapunar J, Aguilar-Farías N, Navarro-Riquelme J, Pavez M, Hirata MH, Cerda A. Influence of Seropositivity against Adenovirus-36 on the Risk of Obesity and Insulin Resistance in the Child Population of Southern Chile. Viruses. 2024; 16(6):995. https://doi.org/10.3390/v16060995
Chicago/Turabian StyleBrito, Roberto, Jorge Sapunar, Nicolás Aguilar-Farías, Juan Navarro-Riquelme, Monica Pavez, Mario Hiroyuki Hirata, and Alvaro Cerda. 2024. "Influence of Seropositivity against Adenovirus-36 on the Risk of Obesity and Insulin Resistance in the Child Population of Southern Chile" Viruses 16, no. 6: 995. https://doi.org/10.3390/v16060995
APA StyleBrito, R., Sapunar, J., Aguilar-Farías, N., Navarro-Riquelme, J., Pavez, M., Hirata, M. H., & Cerda, A. (2024). Influence of Seropositivity against Adenovirus-36 on the Risk of Obesity and Insulin Resistance in the Child Population of Southern Chile. Viruses, 16(6), 995. https://doi.org/10.3390/v16060995






