Remission of HPV-Related Diseases by Antivirals for Herpesvirus: Clinical Cases and a Literature Review
Abstract
1. Background
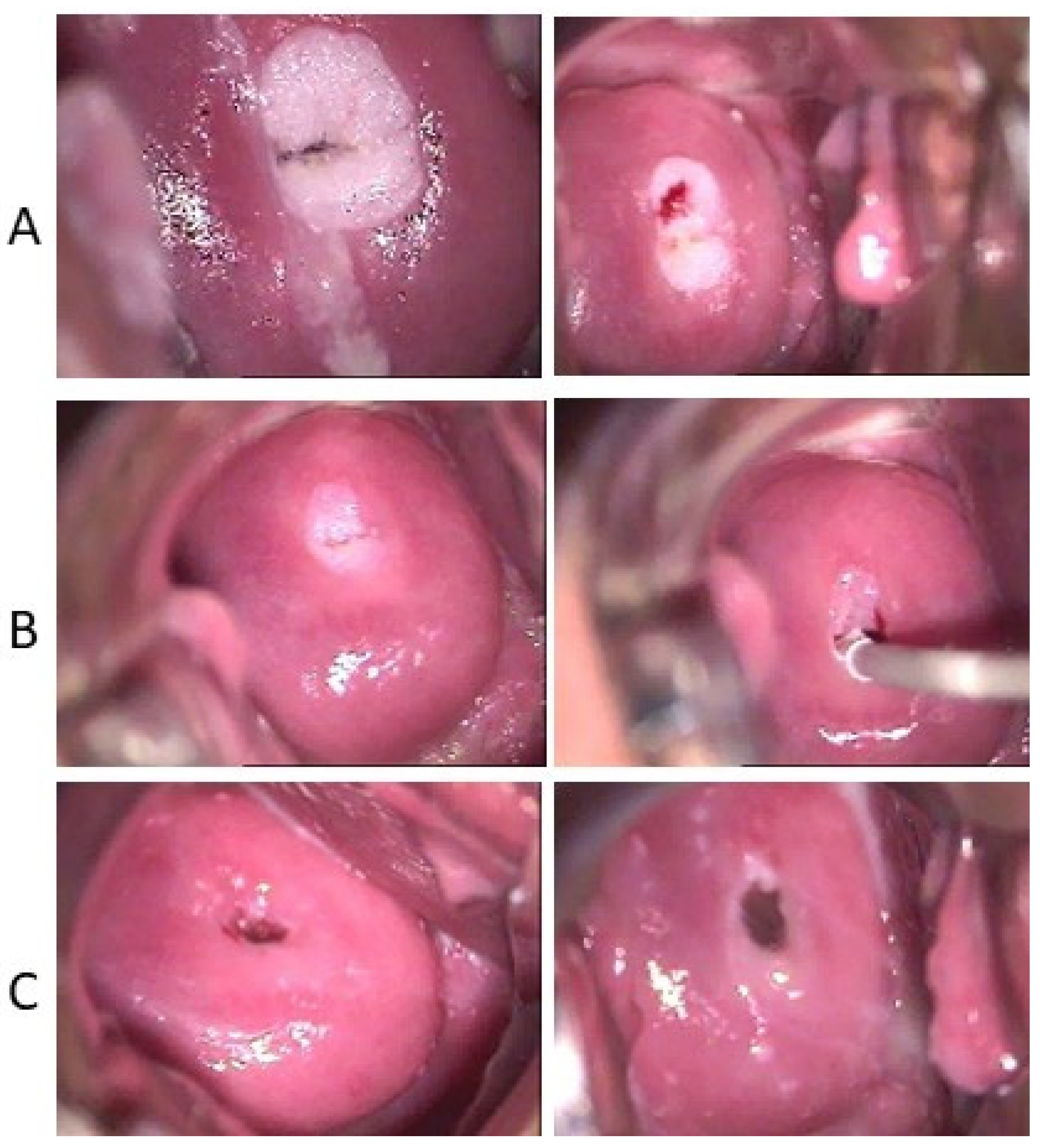
2. Acyclovir Treatment of Condyloma and Giant Condyloma Acuminate of Buschke and Lowenstein Clinical Cases
3. Acyclovir Treatment of Cutaneous Warts (Verrucas)
4. Acyclovir Treatment of Laryngeal Papillomatosis
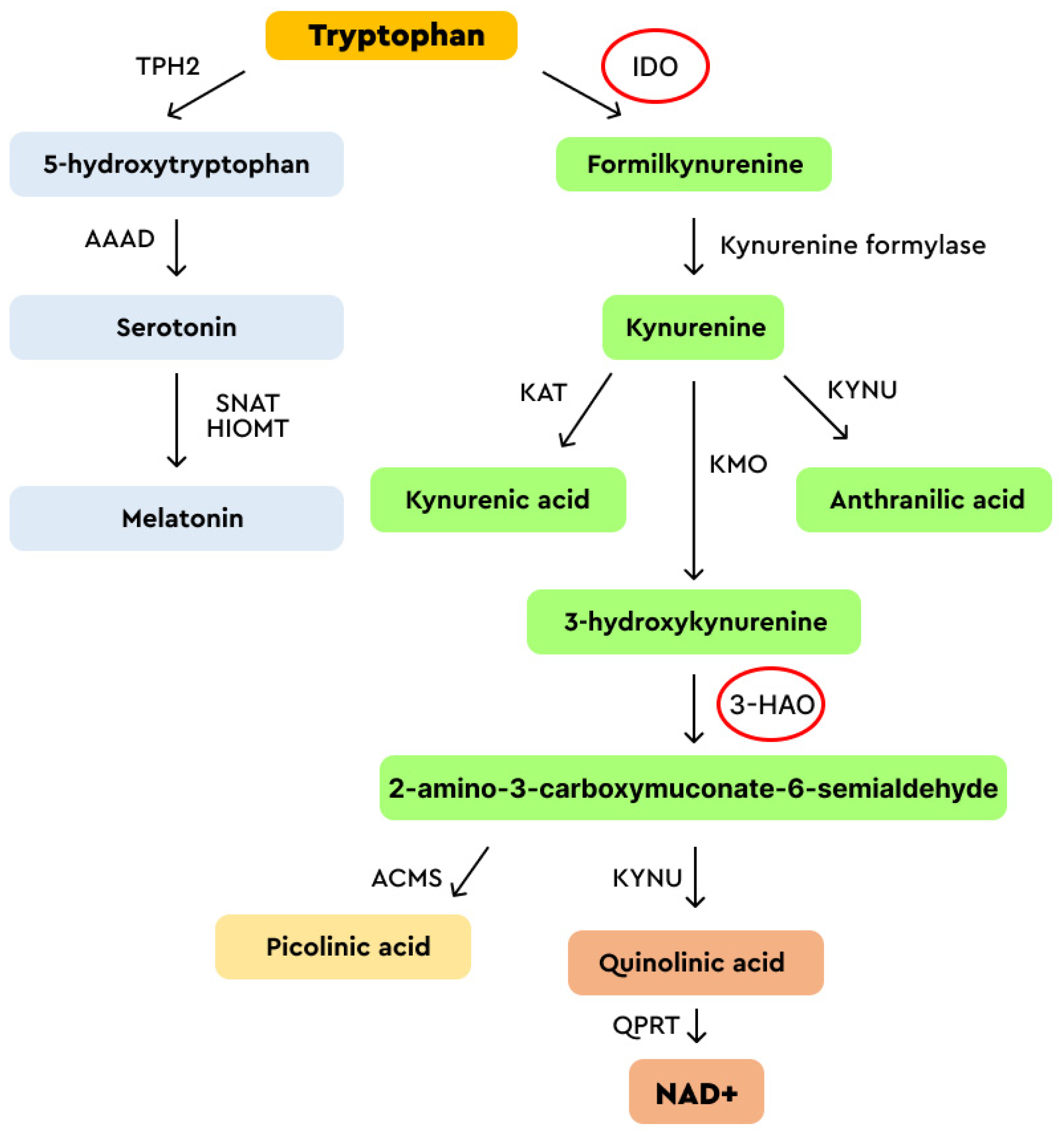
5. Acyclovir and Valaciclovir: Mechanism of Action
6. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclaimer
References
- Ault, K.A. Epidemiology and Natural History of Human Papillomavirus Infections in the Female Genital Tract. Infect. Dis. Obstet. Gynecol. 2006, 2006, 040470. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Giuliano, A.R.; Tortolero-Luna, G.; Ferrer, E.; Burchell, A.N.; de Sanjose, S.; Kjaer, S.K.; Muñoz, N.; Schiffman, M.; Bosch, F.X. Epidemiology of Human Papillomavirus Infection in Men, Cancers Other than Cervical and Benign Conditions. Vaccine 2008, 26 (Suppl. S10), K17–K28. [Google Scholar] [CrossRef]
- Deutsch, F.; Regina Bullen, I.; Nguyen, K.; Tran, N.H.; Elliott, M.; Tran, N. Current State of Play for HPV-Positive Oropharyngeal Cancers. Cancer Treat. Rev. 2022, 110, 102439. [Google Scholar] [CrossRef]
- Muñoz, N.; Bosch, F.X.; de Sanjosé, S.; Herrero, R.; Castellsagué, X.; Shah, K.V.; Snijders, P.J.F.; Meijer, C.J.L.M. Epidemiologic Classification of Human Papillomavirus Types Associated with Cervical Cancer. New Engl. J. Med. 2003, 348, 518–527. [Google Scholar] [CrossRef] [PubMed]
- Ball, S.L.R.; Winder, D.M.; Vaughan, K.; Hanna, N.; Levy, J.; Sterling, J.C.; Stanley, M.A.; Goon, P.K.C. Analyses of Human Papillomavirus Genotypes and Viral Loads in Anogenital Warts. J. Med. Virol. 2011, 83, 1345–1350. [Google Scholar] [CrossRef] [PubMed]
- Al-Awadhi, R.; Al-Mutairi, N.; Albatineh, A.N.; Chehadeh, W. Association of HPV Genotypes with External Anogenital Warts: A Cross Sectional Study. BMC Infect. Dis. 2019, 19, 375. [Google Scholar] [CrossRef] [PubMed]
- Rivera, G.A.; Morell, F. Laryngeal Papillomas; StatPearls: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK562327/ (accessed on 8 August 2023).
- Welschmeyer, A.; Berke, G.S. An Updated Review of the Epidemiological Factors Associated with Recurrent Respiratory Papillomatosis. Laryngoscope Investig. Otolaryngol. 2021, 6, 226–233. [Google Scholar] [CrossRef]
- Derkay, C.S.; Wiatrak, B. Recurrent Respiratory Papillomatosis: A Review. Laryngoscope 2008, 118, 1236–1247. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Sharma, M.; Tan, N.; Barnabas, R.V. HIV-Positive Women Have Higher Risk of Human Papilloma Virus Infection, Precancerous Lesions, and Cervical Cancer. Aids 2018, 32, 795–808. [Google Scholar] [CrossRef]
- Bogale, A.L.; Belay, N.B.; Medhin, G.; Ali, J.H. Molecular Epidemiology of Human Papillomavirus among HIV Infected Women in Developing Countries: Systematic Review and Meta-Analysis. Virol. J. 2020, 17, 179. [Google Scholar] [CrossRef]
- Khawar, L.; McManus, H.; Vickers, T.; Chow, E.P.F.; Fairley, C.K.; Donovan, B.; Machalek, D.A.; Regan, D.G.; Grulich, A.E.; Guy, R.J.; et al. Genital Warts Trends in Australian and Overseas-Born People in Australia: A Cross-Sectional Trend Analysis to Measure Progress towards Control and Elimination. Lancet Reg. Health-West. Pac. 2021, 16, 100251. [Google Scholar] [CrossRef]
- Drolet, M.; Bénard, É.; Pérez, N.; Brisson, M.; Ali, H.; Boily, M.C.; Baldo, V.; Brassard, P.; Brotherton, J.M.L.; Callander, D.; et al. Population-Level Impact and Herd Effects Following the Introduction of Human Papillomavirus Vaccination Programmes: Updated Systematic Review and Meta-Analysis. Lancet 2019, 394, 497–509. [Google Scholar] [CrossRef]
- Vlahovic, T.C.; Khan, M.T. The Human Papillomavirus and Its Role in Plantar Warts: A Comprehensive Review of Diagnosis and Management. Clin. Podiatr. Med. Surg. 2016, 33, 337–353. [Google Scholar] [CrossRef]
- Van Haalen, F.M.; Bruggink, S.C.; Gussekloo, J.; Assendelft, W.J.J.; Eekhof, J.A.H. Warts in Primary Schoolchildren: Prevalence and Relation with Environmental Factors. Br. J. Dermatol. 2009, 161, 148–152. [Google Scholar] [CrossRef]
- Bruggink, S.C.; Eekhof, J.A.H.; Egberts, P.F.; Van Blijswijk, S.C.E.; Assendelft, W.J.J.; Gussekloo, J. Warts Transmitted in Families and Schools: A Prospective Cohort. Pediatrics 2013, 131, 928–934. [Google Scholar] [CrossRef]
- Dambrogio, A.; Yerly, S.; Sahli, R.; Bouzourene, H.; Demartines, N.; Cotton, M.; Givel, J.C. Human Papilloma Virus Type and Recurrence Rate after Surgical Clearance of Anal Condylomata Acuminata. Sex. Transm. Dis. 2009, 36, 536–540. [Google Scholar] [CrossRef]
- Giuliano, A.R.; Sirak, B.; Abrahamsen, M.; Silva, R.J.C.; Baggio, M.L.; Galan, L.; Cintra, R.C.; Lazcano-Ponce, E.; Villa, L.L. Genital Wart Recurrence among Men Residing in Brazil, Mexico, and the United States. J. Infect. Dis. 2019, 219, 703–710. [Google Scholar] [CrossRef]
- Davis, K.G.; Barton, J.S.; Orangio, G.; Bivin, W.; Krane, S. Buschke-Lowenstein Tumors: A Review and Proposed Classification System. Sex. Transm. Dis. 2021, 48, e263–e268. [Google Scholar] [CrossRef]
- Testi, I.; Aggarwal, K.; Jaiswal, N.; Dahiya, N.; Thng, Z.X.; Agarwal, A.; Ahuja, A.; Duggal, M.; Kankaria, A.; Ling Ho, S.; et al. Antiviral Therapy for Varicella Zoster Virus (VZV) and Herpes Simplex Virus (HSV)-Induced Anterior Uveitis: A Systematic Review and Meta-Analysis. Front. Med. 2021, 8, 6427. [Google Scholar] [CrossRef]
- Balestrieri, M.; Carnovale-Scalzo, C.; Garbuglia, A.R.; Chiantore, M.V.; Accardi, L.; Di Bonito, P. Conventional Therapy for Genital Herpesvirus and Remission of HPV-Related Lesions: A Case Series. Infect. Agent. Cancer 2023, 18, 36. [Google Scholar] [CrossRef]
- Bauer, D.J. Treatment of Plantar Warts with Acyclovir. Am. J. Med. 1982, 73, 313–314. [Google Scholar] [CrossRef]
- Pechman, K.J. Does Acyclovir Have an Adjunctive Role in Plantar Wart Therapy? Cleve. Clin. Q. 1983, 50, 213. [Google Scholar] [CrossRef]
- Hurwitz, R.M. Verrucae Vulgares and Acyclovir Ointment. Cutis 1984, 34, 84–86. [Google Scholar]
- Gibson, J.R.; Harvey, S.G.; Barth, J.; Darley, C.R.; Reshad, H.; Burke, C.A. A Comparison of Acyclovir Cream versus Placebo Cream versus Liquid Nitrogen in the Treatment of Viral Plantar Warts. Dermatologica 1984, 168, 178–181. [Google Scholar] [CrossRef]
- Di Rosa, S.; Affronti, M.; Malta, R.; Scardavi, M.; Vassallo, L.; Renda, M.; Rotolo, G.; Maggio, A.M.; Rini, G.B. Verruca Plana Juvenilis (Plane Wart) Treated with Topical Application of Acyclovir. J. Chemother. 1989, 1, 1122. [Google Scholar]
- Bagwell, A.; Loy, A.; McFarland, M.S.; Tessmer-Neubauer, A. Oral Acyclovir in the Treatment of Verruca. J. Drugs Dermatol. 2016, 15, 237–238. [Google Scholar]
- Tandeter, H.; Tandeter, E.R. Treatment of Plantar Warts with Oral Valacyclovir. Am. J. Med. 2005, 118, 689–690. [Google Scholar] [CrossRef]
- Elsayed, A.; Nassar, A.; Marei, A.; Hoseiny, H.A.M.; Alakad, R. Intralesional Acyclovir: A Potential Therapeutic Option for Cutaneous Warts. J. Cutan. Med. Surg. 2022, 26, 25–30. [Google Scholar] [CrossRef]
- Shaheen, M.A.; Salem, S.A.M.; Fouad, D.A.; El-Fatah, A.A.A. Intralesional Tuberculin (PPD) versus Measles, Mumps, Rubella (MMR) Vaccine in Treatment of Multiple Warts: A Comparative Clinical and Immunological Study. Dermatol. Ther. 2015, 28, 194–200. [Google Scholar] [CrossRef]
- Meghana Reddy, E.; Rajashekar, T.S.; Suresh Kumar, K. A Comparative Study of Intralesional Acyclovir vs Immunotherapy for Treatment of Viral Warts. Cureus 2023, 15, e38781. [Google Scholar] [CrossRef]
- Aguado, D.L.; Piñero, B.P.; Betancor, L.; Mendez, A.; Bañales, E.C. Acyclovir in the Treatment of Laryngeal Papillomatosis. Int. J. Pediatr. Otorhinolaryngol. 1991, 21, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Kiroǧlu, M.; Çetik, F.; Soylu, L.; Abedi, A.; Aydogan, B.; Akçali, C.; Kiroǧlu, F.; Ozsahinoǧlu, C. Acyclovir in the Treatment of Recurrent Respiratory Papillomatosis: A Preliminary Report. Am. J. Otolaryngol. 1994, 15, 212–214. [Google Scholar] [CrossRef] [PubMed]
- Endres, D.R.; Burke, D.; Bauman, N.M.; Smith, R.J.H. Acyclovir in the Treatment of Recurrent Respiratory Papillomatosis: A Pilot Study. Ann. Otol. Rhinol. Laryngol. 1994, 103, 301–305. [Google Scholar] [CrossRef] [PubMed]
- Chaturvedi, J.; Sreenivas, V.; Hemanth, V.; Nandakumar, R. Management of Adult Recurrent Respiratory Papillomatosis with Oral Acyclovir Following Micro Laryngeal Surgery: A Case Series. Indian J. Otolaryngol. Head Neck Surg. 2014, 66, 359–363. [Google Scholar] [CrossRef] [PubMed]
- Mitra, S.; Das, A.; Ghosh, D.; Sengupta, A. Postoperative Systemic Acyclovir in Juvenile-Onset Recurrent Respiratory Papillomatosis: The Outcome. Ear Nose Throat J. 2019, 98, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Wright, G.E.; Brown, N.C. Deoxyribonucleotide Analogs as Inhibitors and Substrates of DNA Polymerases. Pharmacol. Ther. 1990, 47, 447–497. [Google Scholar] [CrossRef]
- Bitter, E.E.; Townsend, M.H.; Erickson, R.; Allen, C.; O’Neill, K.L. Thymidine Kinase 1 through the Ages: A Comprehensive Review. Cell Biosci. 2020, 10, 138. [Google Scholar] [CrossRef]
- Elion, G.B. Acyclovir: Discovery, Mechanism of Action, and Selectivity. J. Med. Virol. 1993, 41, 2–6. [Google Scholar] [CrossRef]
- Alibek, K.; Bekmurzayeva, A.; Mussabekova, A.; Sultankulov, B. Using Antimicrobial Adjuvant Therapy in Cancer Treatment: A Review. Infect. Agents Cancer 2012, 7, 33. [Google Scholar] [CrossRef]
- Shaimerdenova, M.; Karapina, O.; Mektepbayeva, D.; Alibek, K.; Akilbekova, D. The Effects of Antiviral Treatment on Breast Cancer Cell Line. Infect. Agents Cancer 2017, 12, 18. [Google Scholar] [CrossRef] [PubMed]
- Jagetia, G.C.; Aruna, R. Effect of Various Concentrations of Acyclovir on Cell Survival and Micronuclei Induction on Cultured HeLa Cells. Mutat. Res.-Genet. Toxicol. Environ. Mutagen. 1999, 446, 155–165. [Google Scholar] [CrossRef] [PubMed]
- Shafique, S.; Rashid, S. Antiviral Drug Acyclovir Exhibits Antitumor Activity via Targeting ΒTrCP1: Molecular Docking and Dynamics Simulation Study. J. Mol. Graph. Model. 2017, 72, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Spardy, N.; Covella, K.; Cha, E.; Hoskins, E.E.; Wells, S.I.; Duensing, A.; Duensing, S. Human Papillomavirus 16 E7 Oncoprotein Attenuates DNA Damage Checkpoint Control by Increasing the Proteolytic Turnover of Claspin. Cancer Res. 2009, 69, 7022–7029. [Google Scholar] [CrossRef] [PubMed]
- Lebeau, A.; Bruyere, D.; Roncarati, P.; Peixoto, P.; Hervouet, E.; Cobraiville, G.; Taminiau, B.; Masson, M.; Gallego, C.; Mazzucchelli, G.; et al. HPV Infection Alters Vaginal Microbiome through Down-Regulating Host Mucosal Innate Peptides Used by Lactobacilli as Amino Acid Sources. Nat. Commun. 2022, 13, 1076. [Google Scholar] [CrossRef] [PubMed]
- Müller, A.C.; Dairam, A.; Limson, J.L.; Daya, S. Mechanisms by Which Acyclovir Reduces the Oxidative Neurotoxicity and Biosynthesis of Quinolinic Acid. Life Sci. 2007, 80, 918–925. [Google Scholar] [CrossRef] [PubMed]
- Bodaghi, B.; Goureau, O.; Zipeto, D.; Laurent, L.; Virelizier, J.L.; Michelson, S. Role of IFN-g-Induced Indoleamine 2,3 Dioxygenase and Inducible Nitric Oxide Synthase in the Replication of Human Cytomegalovirus in Retinal Pigment Epithelial Cells. J. Immunol. 1999, 162, 957–964. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, S.V.; Schultze, J.L. New Insights into IDO Biology in Bacterial and Viral Infections. Front. Immunol. 2014, 5, 103079. [Google Scholar] [CrossRef] [PubMed]
- Xie, Z.; Zhang, M.; Xiong, W.; Wan, H.Y.; Zhao, X.C.; Xie, T.; Lei, H.; Lin, Z.C.; Luo, D.S.; Liang, X.L.; et al. Immunotolerant Indoleamine-2,3-Dioxygenase Is Increased in Condyloma Acuminata. Br. J. Dermatol. 2017, 177, 809–817. [Google Scholar] [CrossRef]
- Modoux, M.; Rolhion, N.; Mani, S.; Sokol, H. Tryptophan Metabolism as a Pharmacological Target. Trends Pharmacol. Sci. 2021, 42, 60–73. [Google Scholar] [CrossRef]
- Jamshed, L.; Debnath, A.; Jamshed, S.; Wish, J.V.; Raine, J.C.; Tomy, G.T.; Thomas, P.J.; Holloway, A.C. An Emerging Cross-Species Marker for Organismal Health: Tryptophan-Kynurenine Pathway. Int. J. Mol. Sci. 2022, 23, 6300. [Google Scholar] [CrossRef]
- Ferns, D.M.; Kema, I.P.; Buist, M.R.; Nijman, H.W.; Kenter, G.G.; Jordanova, E.S. Indoleamine-2,3-Dioxygenase (IDO) Metabolic Activity Is Detrimental for Cervical Cancer Patient Survival. Oncoimmunology 2015, 4, e981457. [Google Scholar] [CrossRef] [PubMed]
- Venancio, P.A.; Consolaro, M.E.L.; Derchain, S.F.; Boccardo, E.; Villa, L.L.; Maria-Engler, S.S.; Campa, A.; Discacciati, M.G. Indoleamine 2,3-dioxygenase and tryptophan 2,3-dioxygenase expression in HPV infection, SILs, and cervical cancer. Cancer Cytopathol. 2019, 127, 586–597. [Google Scholar] [CrossRef] [PubMed]
- Godin-Ethier, J.; Hanafi, L.A.; Piccirillo, C.A.; Lapointe, R. Indoleamine 2,3-Dioxygenase Expression in Human Cancers: Clinical and Immunologic Perspectives. Clin. Cancer Res. 2011, 17, 6985–6991. [Google Scholar] [CrossRef]
- Mittal, D.; Kassianos, A.J.; Tran, L.S.; Bergot, A.S.; Gosmann, C.; Hofmann, J.; Blumenthal, A.; Leggatt, G.R.; Frazer, I.H. Indoleamine 2,3-Dioxygenase Activity Contributes to Local Immune Suppression in the Skin Expressing Human Papillomavirus Oncoprotein E7. J. Investig. Dermatol. 2013, 133, 2686–2694. [Google Scholar] [CrossRef]
- Gouasmi, R.; Ferraro-Peyret, C.; Nancey, S.; Coste, I.; Renno, T.; Chaveroux, C.; Aznar, N.; Ansieau, S. The Kynurenine Pathway and Cancer: Why Keep It Simple When You Can Make It Complicated. Cancers 2022, 14, 2793. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; Si, Q.; Qi, R.; Liu, W.; Li, M.; Guo, M.; Wei, L.; Yao, Z. Indoleamine 2,3-Dioxygenase 1: A Promising Therapeutic Target in Malignant Tumor. Front. Immunol. 2021, 12, 630. [Google Scholar] [CrossRef]
- Turel, I.; Anderson, B.; Sletten, E.; White, A.J.P.; Williams, D.J. New Studies in the Copper(II) Acyclovir (Acv) System. NMR Relaxation Studies and the X-ray Crystal Structure of [Cu(Acv)2(H2O)2](NO3)2. Polyhedron 1998, 17, 4195–4201. [Google Scholar] [CrossRef]
- Herrero, L.A.; Cerro-Garrido, J.C.; Terrón-Homar, À. A Calorimetric Study of 3d Metal Ions-Acyclovir Interactions. The 2-Hydroxyethoxymethyl Group of Acyclovir Mimics the Role of Ribose in Deoxy-Guanosine and Guanosine Promoting the Coordination through N(7). J. Inorg. Biochem. 2001, 86, 677–680. [Google Scholar] [CrossRef]
- Pérez-Toro, I.; Domínguez-Martín, A.; Choquesillo-Lazarte, D.; Vílchez-Rodríguez, E.; González-Pérez, J.M.; Castiñeiras, A.; Niclós-Gutiérrez, J. Lights and Shadows in the Challenge of Binding Acyclovir, a Synthetic Purine-like Nucleoside with Antiviral Activity, at an Apical-Distal Coordination Site in Copper(II)-Polyamine Chelates. J. Inorg. Biochem. 2015, 148, 84–92. [Google Scholar] [CrossRef]
- Mehraj, V.; Routy, J.P. Tryptophan Catabolism in Chronic Viral Infections: Handling Uninvited Guests. Int. J. Tryptophan Res. 2015, 8, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Barnes, T.M.; Mijaljica, D.; Townley, J.P.; Spada, F.; Harrison, I.P. Vehicles for Drug Delivery and Cosmetic Moisturizers: Review and Comparison. Pharmaceutics 2021, 13, 2012. [Google Scholar] [CrossRef] [PubMed]
- Hogendoorn, G.K.; Bruggink, S.C.; de Koning, M.N.C.; Eekhof, J.A.H.; Hermans, K.E.; Rissmann, R.; Burggraaf, J.; Wolterbeek, R.; Quint, K.D.; Kouwenhoven, S.T.P.; et al. Morphological Characteristics and Human Papillomavirus Genotype Predict the Treatment Response in Cutaneous Warts. Br. J. Dermatol. 2018, 178, 253–260. [Google Scholar] [CrossRef]
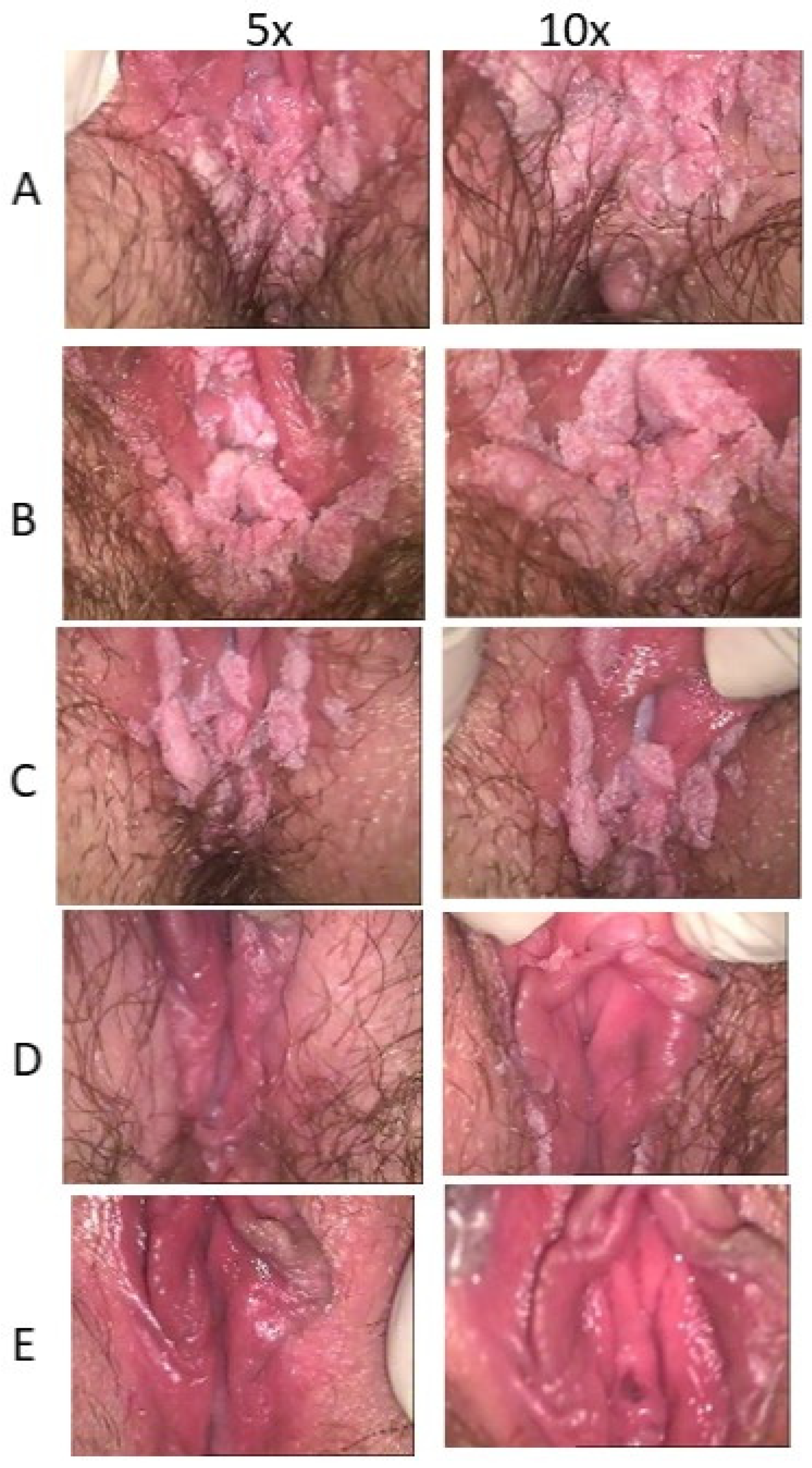

| ID | Age | HPV Lesion Type | Oral ACV Dosage | Topical ACV | Treatment Time (d,m) | Colposcopy Image |
|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G |
| 11 | 30 | Frenulum penile condylomatosis | ACV 1600 mg/20 d | 5% ACV (20 d) | 20 d |  |
| 30 | 32 | Penile condylomatosis (recurrence at cryoscopic treatment) | ACV 1600 mg/20 d | 5% ACV (2 × 30 d) | 2 m |  |
| 36 | 41 | Penile condylomatosis (recurrence at laser treatment) | _ | 8% ACV Transcutol (2 × 45 d) | 4 m |  |
| 39 | 29 | Penile micro-condylomatosis | _ | 7% ACV Pentravan (2 × 45 d) | 3 m |  |
| 41 | 37 | Penile micro-condylomatosis | _ | 8% ACV Transcutol (2 × 45 d) | 1 m |  |
| ID | Age | Cervical Lesions | HPV Lesion | Oral Dosage (mg/d) | Topical Dosage | Treatment Time (Month) |
|---|---|---|---|---|---|---|
| A | B | C | G | H | I | |
| 5 | 27 | Condyloma acuminate LR-HPV | Vulvar GCBL | ACV 2.4 g/30 d, VCV 2 g mg/40 d | 5% ACV (2 × 60 d) | 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balestrieri, M.; Chiantore, M.V.; Garbuglia, A.R.; Carnovale-Scalzo, C.; Falcucci, S.; Di Bonito, P. Remission of HPV-Related Diseases by Antivirals for Herpesvirus: Clinical Cases and a Literature Review. Viruses 2024, 16, 756. https://doi.org/10.3390/v16050756
Balestrieri M, Chiantore MV, Garbuglia AR, Carnovale-Scalzo C, Falcucci S, Di Bonito P. Remission of HPV-Related Diseases by Antivirals for Herpesvirus: Clinical Cases and a Literature Review. Viruses. 2024; 16(5):756. https://doi.org/10.3390/v16050756
Chicago/Turabian StyleBalestrieri, Maria, Maria Vincenza Chiantore, Anna Rosa Garbuglia, Caterina Carnovale-Scalzo, Susanna Falcucci, and Paola Di Bonito. 2024. "Remission of HPV-Related Diseases by Antivirals for Herpesvirus: Clinical Cases and a Literature Review" Viruses 16, no. 5: 756. https://doi.org/10.3390/v16050756
APA StyleBalestrieri, M., Chiantore, M. V., Garbuglia, A. R., Carnovale-Scalzo, C., Falcucci, S., & Di Bonito, P. (2024). Remission of HPV-Related Diseases by Antivirals for Herpesvirus: Clinical Cases and a Literature Review. Viruses, 16(5), 756. https://doi.org/10.3390/v16050756







