Rustrela Virus-Associated Encephalomyelitis (‘Staggering Disease’) in Cats from Eastern Austria, 1994–2016
Abstract
1. Introduction
2. Materials and Methods
2.1. Database Search
2.2. Selected Samples
2.3. Nucleic Acid Extraction
2.4. PCR Analysis
2.5. Hematoxylin-Eosin (H.E.) Staining of the FFPE Samples
2.6. Immunohistochemistry
2.7. In Situ Hybridization (ISH)
3. Results
3.1. PCR and Sequencing Results
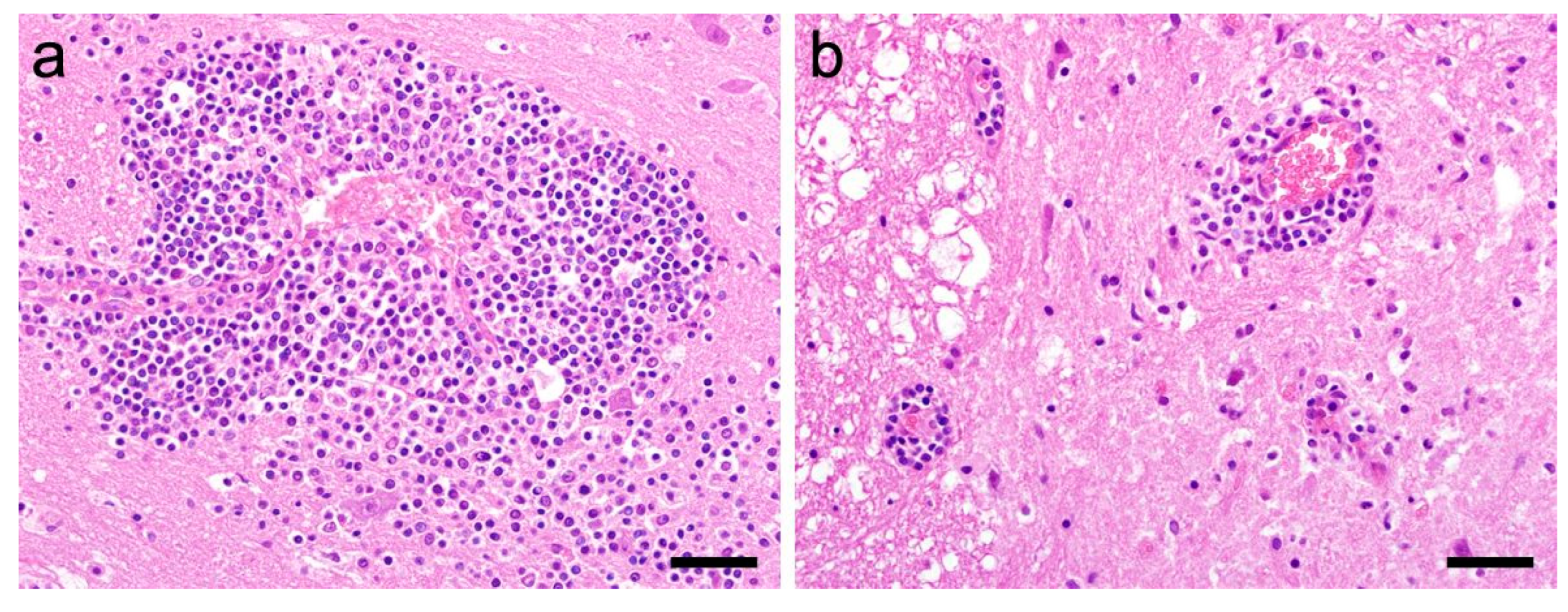
3.2. Histological Analysis and Immunohistochemistry
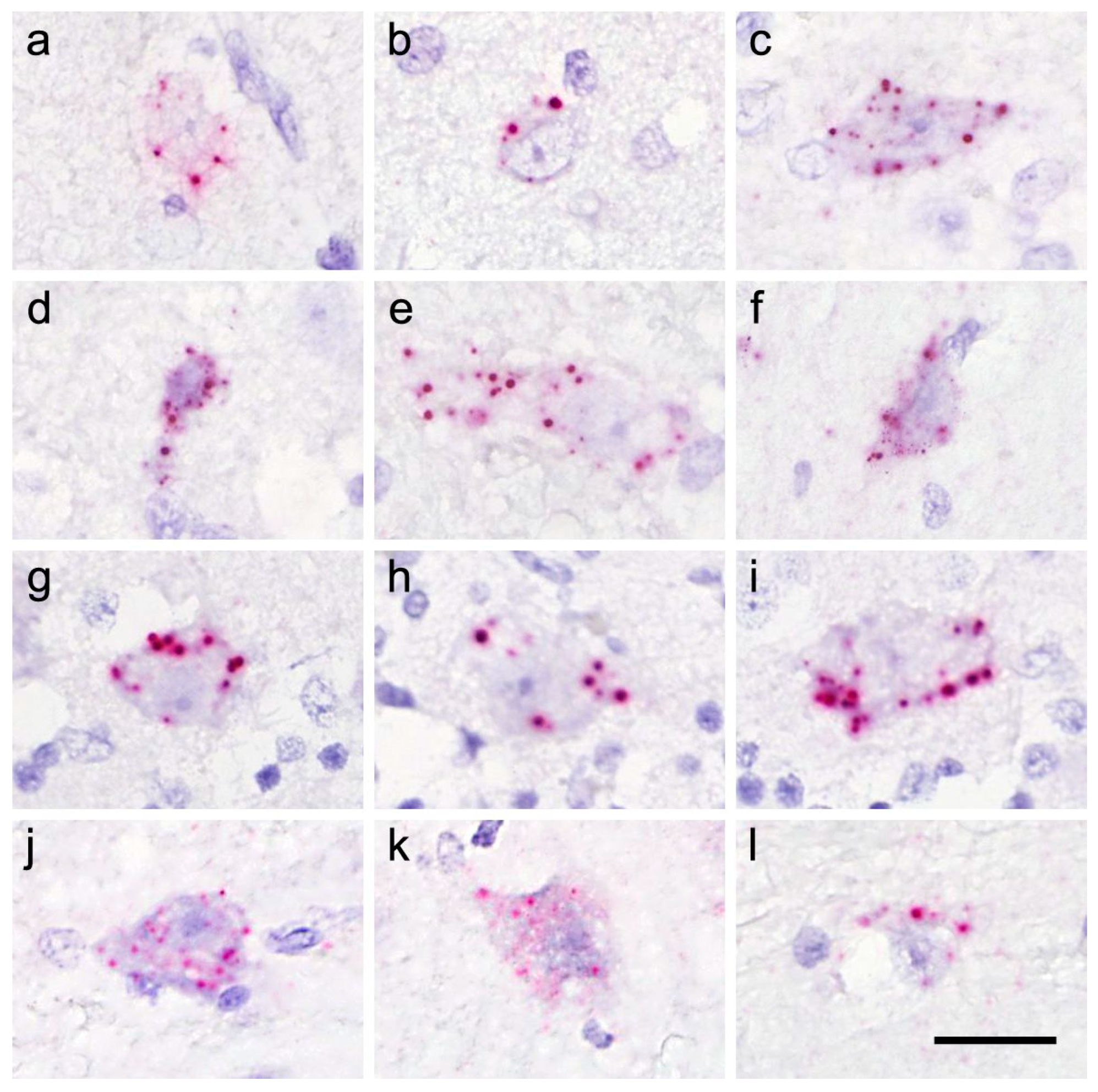
3.3. In Situ Hybridization (ISH)
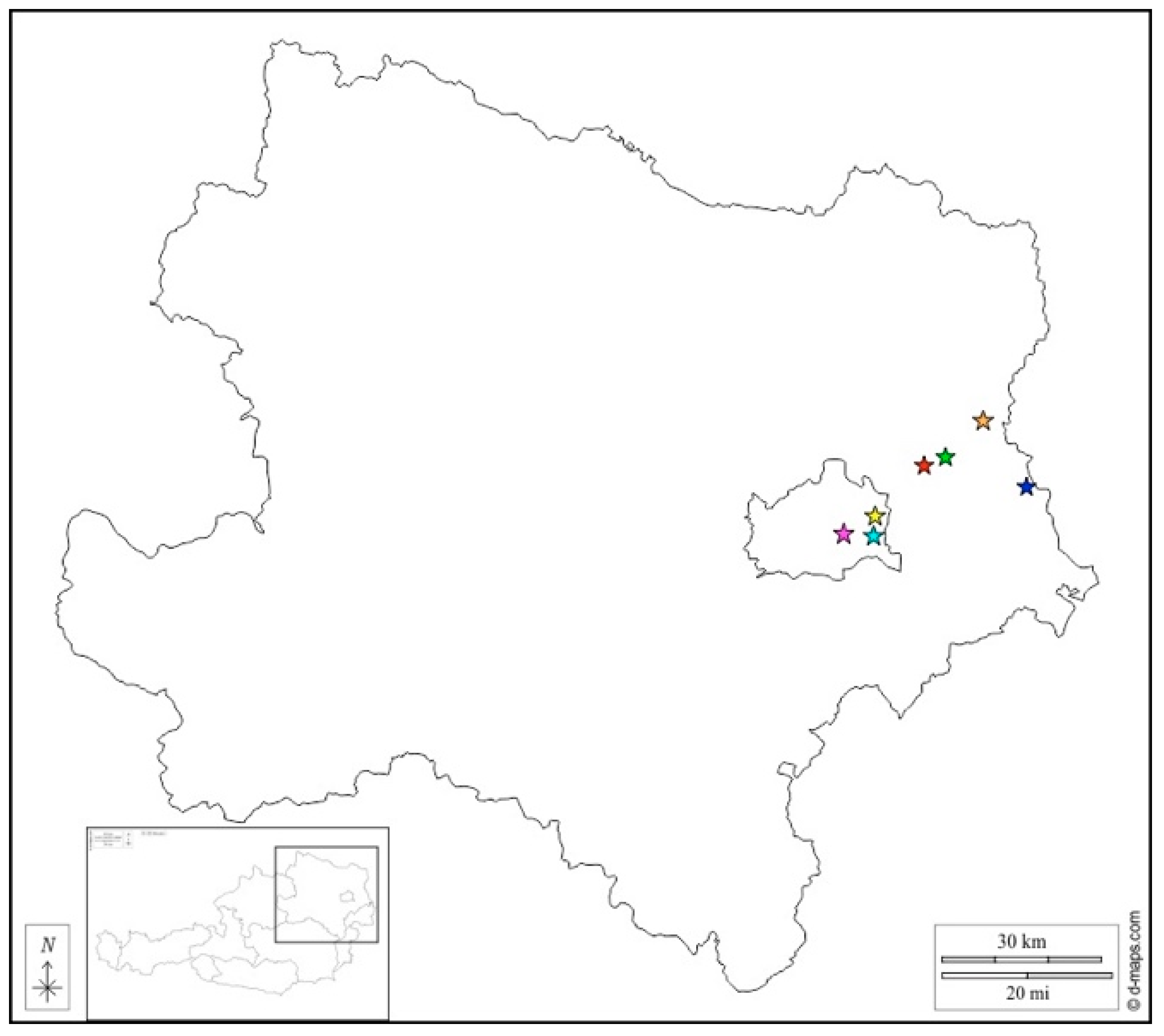
| Sample ID | Geographic Origin | Sex | Age | Month of Euthanasia/Death | Reported Anamnesis | Severity of Inflammation | RusV RT-qPCR (Ct) | RusV ISH Score |
|---|---|---|---|---|---|---|---|---|
| 826/94 | 1220 Wien | fn | adult | June 1994 | CNS signs, blindness, deterioration despite therapy; euthanasia | moderate | - | 1 |
| 1942/94 | 3920 Hopfenleiten | mn | adult | November 1994 | Aujeszky’s disease or toxicosis suspected | severe | - | - |
| 2003/94 | 2252 Ollersdorf | fn | 3 y | November 1994 | ‘staggering disease’ suspected | severe | 26.1–30.9 (frozen) 38.5–44.0 (PET) | 3 |
| 2250/94 | 1120 Wien | m | juvenile | December 1994 | ataxia, weak hind extremities; euthanasia | moderate | - | - |
| 2272/94 | 1040 Wien | m | 1 y | December 1994 | seizures with salivation, tonic–clonic convulsions for 3 days, brief improvement after administration of diazepam; animal died during seizure | mild | - | - |
| 984/96 | 2230 Gänserndorf | mn | adult | May 1996 | ‘staggering disease’ suspected | severe | 35.2–40.5 | 1 |
| 2325/96 | 1220 Wien | mn | 5 y | December 1996 | ataxia and constipation, short-term improvement with treatment; relapse with high-grade ataxia, intestinal atony, cardiovascular failure; euthanasia | severe | - | - |
| 214/97 | 2293 Marchegg | mn | 7 y | January 1997 | for 2–3 months, signs of ‘staggering disease’ which improved briefly; for 1 month, extensor cramps of all 4 extremities, uncoordinated movements | moderate | 35.1–40.2 | 2 |
| 215/97 | 1020 Wien | fn | 6 y | January 1997 | for 2 months, only able to stand in a sawhorse stance, hyperesthesia to manipulation of the head | severe | 38.6–43.4 | 1 |
| 2175/97 | 1220 Wien | fn | 10 y | October 1997 | impaired balance, tonic–clonic convulsions | moderate | - | - |
| 142/98 | 2231 Straßhof | mn | 7 y | January 1998 | progressive paralysis beginning in posterior extremities, no fever; ‘staggering disease’ suspected | mild | 34.0–38.2 | 2 |
| 638/00 | 4722 Peuerbach | fn | 2 y | March 2000 | abnormal movement pattern, fever | mild | - | - |
| 209/02 | 1220 Wien | mn | 7 y | February 2002 | epileptic seizures | severe | - | - |
| 1114/02 | 2732 Willendorf | f | juvenile | June 2002 | progressive central nervous signs; euthanasia | severe | - | - |
| 2498/02 | 4203 Altenberg | m | 6 y | December 2002 | CNS signs, anorexia | mild | - | - |
| 2026/04 | 1210 Wien | mn | 10 y | December 2004 | sudden paraparesis on the right side, loss of sensitivity on the left side of the face | moderate | - | - |
| 1283/05 | 8130 Frohnleiten | fn | 1 y | July 2005 | salivation and vocalization, seizures, increasing weakness, unsteady gait, inappetence; euthanasia | mild | - | - |
| 1191/06 | 1210 Wien | m | juvenile | July 2006 | fever, anisocoria, disorientation, blindness, ataxia, tremor, inappetence; euthanasia | mild | - | - |
| 1263/08 | 1210 Wien | fn | 9 y | August 2008 | CNS deficits, seizures, ataxia | severe | - | - |
| 57/10 | 1220 Wien | mn | 8 y | January 2010 | inappetence, apathy, exsiccosis, rhinitis | moderate | 41.1–42.0 | 1 |
| 816/13 | 3002 Purkersdorf | fn | 6 y | July 2013 | 2x generalized epileptic seizures, head tremor, therapy-resistant convulsions | moderate | - | - |
| 200/16 | 5721 Piesendorf | mn | juvenile | March 2016 | epileptic seizures; euthanasia | moderate | - | - |
| 490/16 | 3160 Traisen | mn | 17 y | June 2016 | acute tetraparesis, progressive blindness | severe | - | - |
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kronevi, T.; Nordström, M.; Moreno, W.; Nilsson, P.O. Feline ataxia due to nonsuppurative meningoencephalomyelitis of unknown aetiology. Nord. Veterinärmedicin 1974, 26, 720–725. [Google Scholar]
- Weissenböck, H.; Nowotny, N.; Zoher, J. Feline Meningoencephalomyelitis (“Staggering Disease”) in Österreich. Wien. Tierärztl. Mon. 1994, 81, 195–201. [Google Scholar]
- Nowotny, N.; Weissenböck, H. Description of feline nonsuppurative meningoencephalomyelitis (“staggering disease”) and studies of its etiology. J. Clin. Microbiol. 1995, 33, 1668–1669. [Google Scholar] [CrossRef] [PubMed]
- Ström, B. Vingelsjuka hos katt. Sven. Veterinärtidning 1992, 44, 19–24. [Google Scholar]
- Lundgren, A.-L. Feline non-suppurative meningoencephalomyelitis. A clinical and pathological study. J. Comp. Pathol. 1992, 107, 411–425. [Google Scholar] [CrossRef]
- Matiasek, K.; Pfaff, F.; Weissenböck, H.; Wylezich, C.; Kolodziejek, J.; Tengstrand, S.; Ecke, F.; Nippert, S.; Starcky, P.; Litz, B.; et al. Mystery of fatal ‘staggering disease’ unravelled: Novel rustrela virus causes severe meningoencephalomyelitis in domestic cats. Nat. Commun. 2023, 14, 624. [Google Scholar] [CrossRef]
- De Le Roi, M.; Puff, C.; Wohlsein, P.; Pfaff, F.; Beer, M.; Baumgärtner, W.; Rubbenstroth, D. Rustrela virus as putative cause of nonsuppurative meningoencephalitis in lions. Emerg. Infect. Dis. 2023, 29, 1042. [Google Scholar] [CrossRef]
- Bennett, A.J.; Paskey, A.C.; Ebinger, A.; Pfaff, F.; Priemer, G.; Höper, D.; Breithaupt, A.; Heuser, E.; Ulrich, R.G.; Kuhn, J.H.; et al. Relatives of rubella virus in diverse mammals. Nature 2020, 586, 424–428. [Google Scholar] [CrossRef] [PubMed]
- Voss, A.; Schlieben, P.; Gerst, S.; Wylezich, C.; Pfaff, F.; Langner, C.; Niesler, M.; Schad, P.; Beer, M.; Rubbenstroth, D.; et al. Rustrela virus infection—An emerging neuropathogen of red-necked wallabies (Macropus rufogriseus ). Transbound. Emerg. Dis. 2022, 69, 4016–4021. [Google Scholar] [CrossRef] [PubMed]
- Pfaff, F.; Breithaupt, A.; Rubbenstroth, D.; Nippert, S.; Baumbach, C.; Gerst, S.; Langner, C.; Wylezich, C.; Ebinger, A.; Höper, D.; et al. Revisiting rustrela virus—New cases of encephalitis and a solution to the capsid enigma. Microbiol. Spectr. 2021, 10, e0010322. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Flanagan, J.; Su, N.; Wang, L.-C.; Bui, S.; Nielson, A.; Wu, X.; Vo, H.-T.; Ma, X.-J.; Luo, Y. RNAscope: A novel in situ RNA analysis platform for formalin-fixed paraffin-embedded tissues. J. Mol. Diagn. 2012, 14, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Toussaint, J.F.; Sailleau, C.; Breard, E.; Zientara, S.; De Clercq, K. Bluetongue virus detection by two real-time RT-qPCRs targeting two different genomic segments. J. Virol. Meth. 2007, 140, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Weissenböck, H.; Bagó, Z.; Kolodziejek, J.; Hager, B.; Palmetzhofer, G.; Dürrwald, R.; Nowotny, N. Infections of horses and shrews with Bornaviruses in Upper Austria: A novel endemic area of Borna disease. Emerg. Microb. Infect. 2017, 6, 1–9. [Google Scholar] [CrossRef]
- Weidinger, P.; Kolodziejek, J.; Khafaga, T.; Loney, T.; Howarth, B.; Sher Shah, M.; Abou Tayoun, A.; Alsheikh-Ali, A.; Camp, J.V.; Nowotny, N. Potentially zoonotic viruses in wild rodents, United Arab Emirates, 2019—A pilot study. Viruses 2023, 15, 695. [Google Scholar] [CrossRef]
- Schmidt, S.; Essbauer, S.S.; Mayer-Scholl, A.; Poppert, S.; Schmidt-Chanasit, J.; Klempa, B.; Henning, K.; Schares, G.; Groschup, M.H.; Spitzenberger, F.; et al. Multiple infections of rodents with zoonotic pathogens in Austria. Vector-Borne Zoonot. Dis. 2014, 14, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Dürrwald, R.; Kolodziejek, J.; Weissenböck, H.; Nowotny, N. The bicolored white-toothed shrew Crocidura leucodon (HERMANN 1780) is an indigenous host of mammalian Borna disease virus. PLoS ONE 2014, 9, e93659. [Google Scholar] [CrossRef] [PubMed]
- Hilbe, M.; Herrsche, R.; Kolodziejek, J.; Nowotny, N.; Zlinszky, K.; Ehrensperger, F. Shrews as reservoir hosts of Borna disease virus. Emerg. Infect. Dis. 2006, 12, 675–677. [Google Scholar] [CrossRef] [PubMed]
- Schlottau, K.; Forth, L.; Angstwurm, K.; Höper, D.; Zecher, D.; Liesche, F.; Hoffmann, B.; Kegel, V.; Seehofer, D.; Platen, S.; et al. Fatal encephalitic Borna disease virus 1 in solid-organ transplant recipients. N. Engl. J. Med. 2018, 379, 1377–1379. [Google Scholar] [CrossRef] [PubMed]
- Niller, H.H.; Angstwurm, K.; Rubbenstroth, D.; Schlottau, K.; Ebinger, A.; Giese, S.; Wunderlich, S.; Banas, B.; Forth, L.F.; Hoffmann, D.; et al. Zoonotic spillover infections with Borna disease virus 1 leading to fatal human encephalitis, 1999–2019: An epidemiological investigation. Lancet Infect. Dis. 2020, 20, 467–477. [Google Scholar] [CrossRef] [PubMed]

| Virus | PCR Set | Primer/Probe Name | Sequence (5′ to 3′) |
|---|---|---|---|
| RusV | 5F/5R (1st round) | 5F | GTCGAGGAGCAGATAAGCCC |
| 5R | GTAACATAGTCGGGCTGGGG | ||
| 203Fn/349Rn (2nd round) | 203Fn | TGCAGTCCAAGCGGTGATAC | |
| 349Rn | CTGGGRTTCACGAGGCAATG | ||
| RusV | 5113F/5681R (1st round) | 5113F | CACCGAGTTCGACATGAATC |
| 5681R | ATGTGGCGTTCACAGCTAGA | ||
| 5242Fn/5449Rn (2nd round) | 5242Fn | GTGARCCCGCGACAYTACTC | |
| 5449Rn | GTTGCCACCCGCTTGATAGG | ||
| BoDV-1 | BoDV-1 L1 RT-qPCR | 202F | AGCTGCCTAATGACCTACAA |
| 323R | TGATCAAGAAATGACCCTTG | ||
| 236P | CAGCAGACACAGCCAAGAGCAG |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weiss, V.; Weidinger, P.; Matt, J.; Weissenbacher-Lang, C.; Nowotny, N.; Weissenböck, H. Rustrela Virus-Associated Encephalomyelitis (‘Staggering Disease’) in Cats from Eastern Austria, 1994–2016. Viruses 2023, 15, 1621. https://doi.org/10.3390/v15081621
Weiss V, Weidinger P, Matt J, Weissenbacher-Lang C, Nowotny N, Weissenböck H. Rustrela Virus-Associated Encephalomyelitis (‘Staggering Disease’) in Cats from Eastern Austria, 1994–2016. Viruses. 2023; 15(8):1621. https://doi.org/10.3390/v15081621
Chicago/Turabian StyleWeiss, Viktoria, Pia Weidinger, Julia Matt, Christiane Weissenbacher-Lang, Norbert Nowotny, and Herbert Weissenböck. 2023. "Rustrela Virus-Associated Encephalomyelitis (‘Staggering Disease’) in Cats from Eastern Austria, 1994–2016" Viruses 15, no. 8: 1621. https://doi.org/10.3390/v15081621
APA StyleWeiss, V., Weidinger, P., Matt, J., Weissenbacher-Lang, C., Nowotny, N., & Weissenböck, H. (2023). Rustrela Virus-Associated Encephalomyelitis (‘Staggering Disease’) in Cats from Eastern Austria, 1994–2016. Viruses, 15(8), 1621. https://doi.org/10.3390/v15081621









