Treatment with Toll-like Receptor (TLR) Ligands 3 and 21 Prevents Fecal Contact Transmission of Low Pathogenic H9N2 Avian Influenza Virus (AIV) in Chickens
Abstract
1. Introduction
2. Materials and Methods
2.1. Chickens
2.2. Virus Propagation
2.3. Infectious Dose
2.4. TLR Ligands
2.5. Experimental Design
2.5.1. Model A: Feces from H9N2 AIV-Infected Chickens
2.5.2. Model B: Experimentally Spiked Feces
2.6. Collection of Samples and Virus Titration
2.6.1. Virus Isolation
2.6.2. Virus Persistence
2.6.3. pH
2.6.4. Hemagglutination Inhibition (HI) Assay
2.6.5. RNA Extraction, cDNA Synthesis and Real-Time PCR
2.7. Statistical Analysis
3. Results
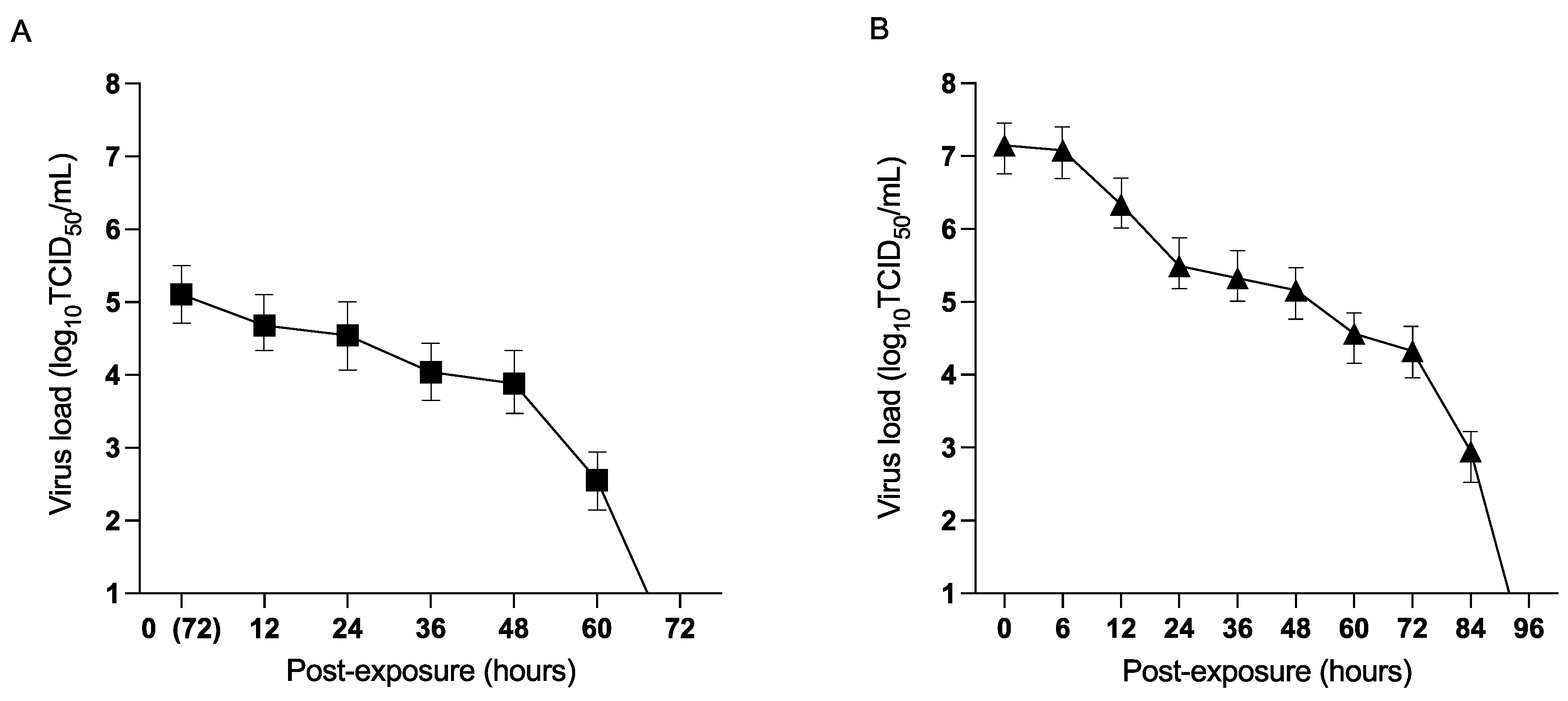
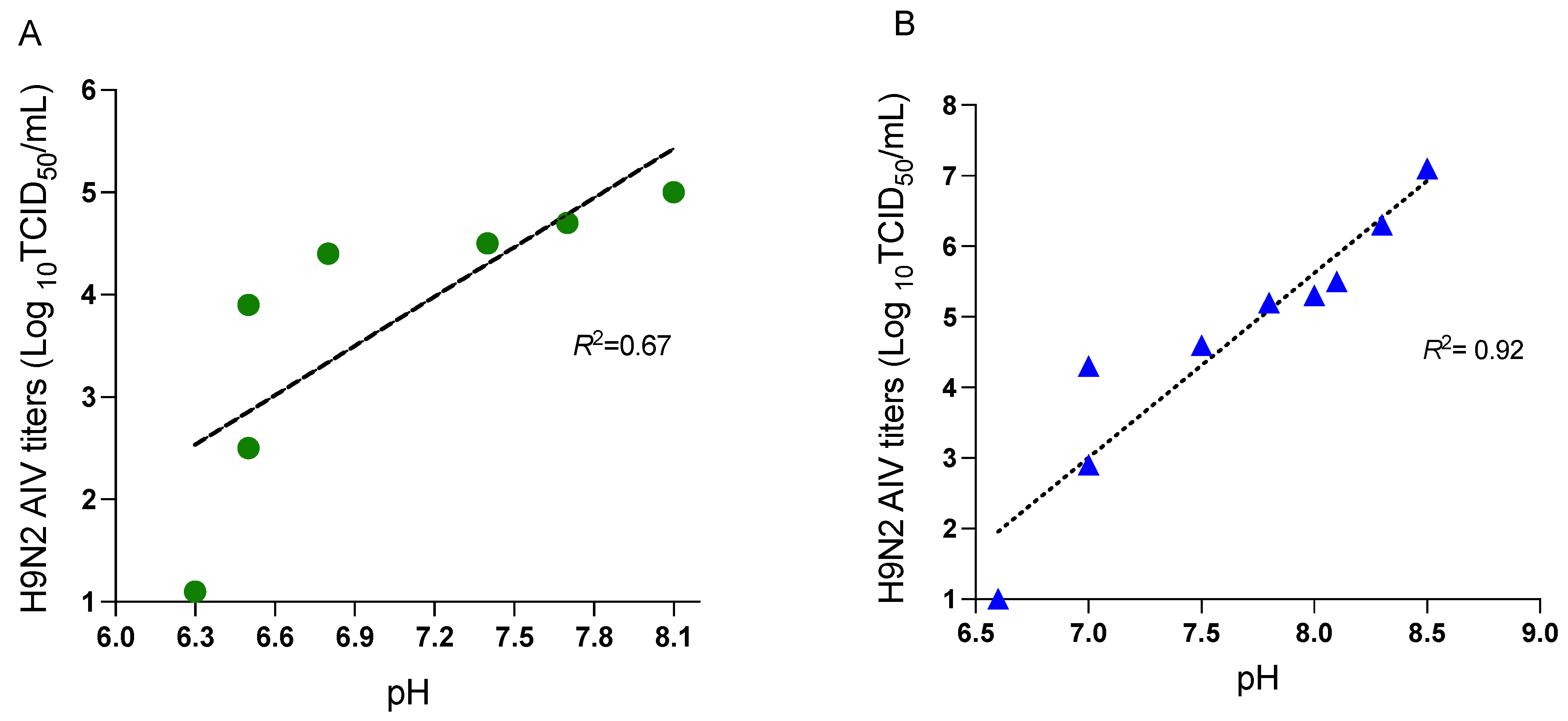
3.1. Persistence of H9N2 AIV in Feces from Virus-Inoculated Chickens and Spiked Fecal Material
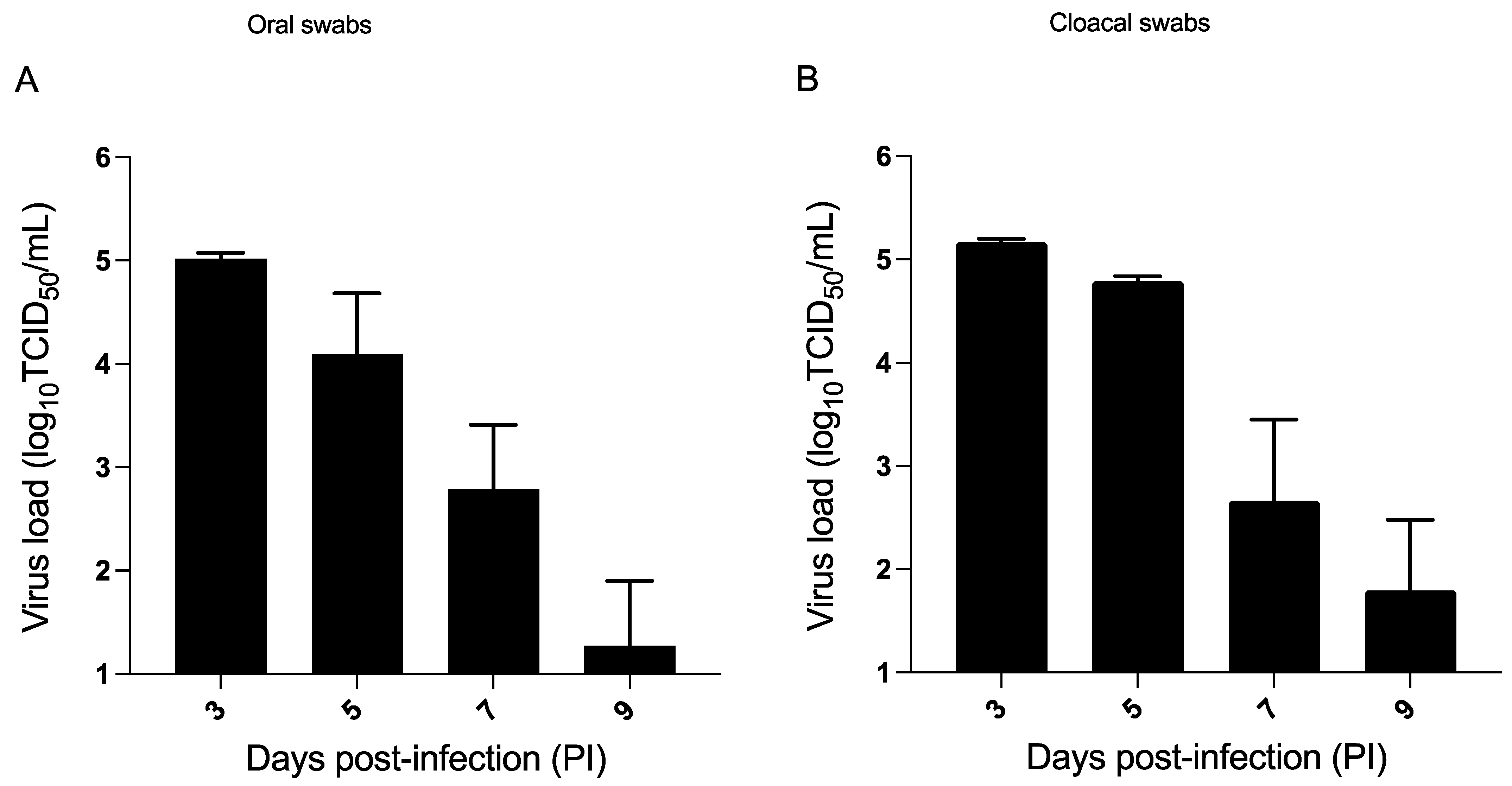
3.2. H9N2 AIV Challenge in the Seeder Chickens in Model A
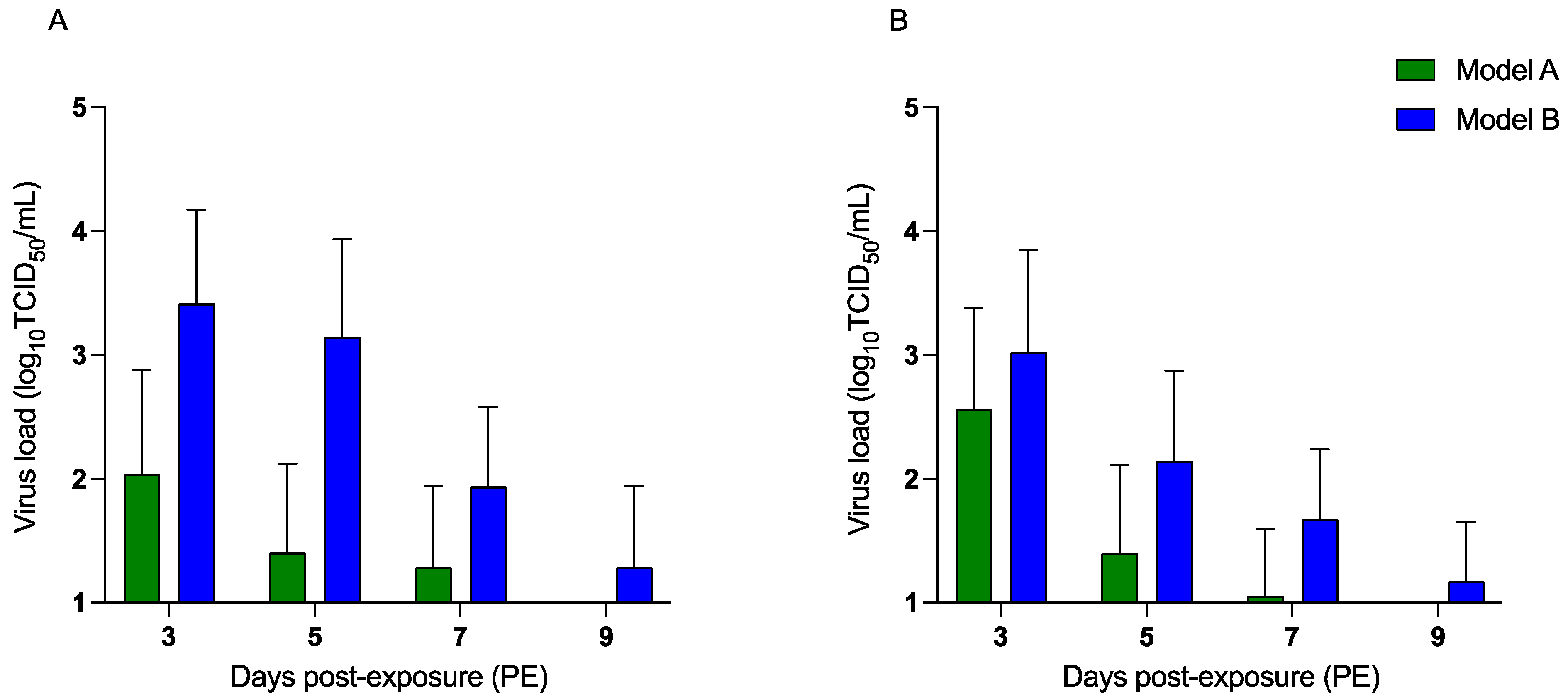
3.3. H9N2 AIV Transmission to Exposed Chickens
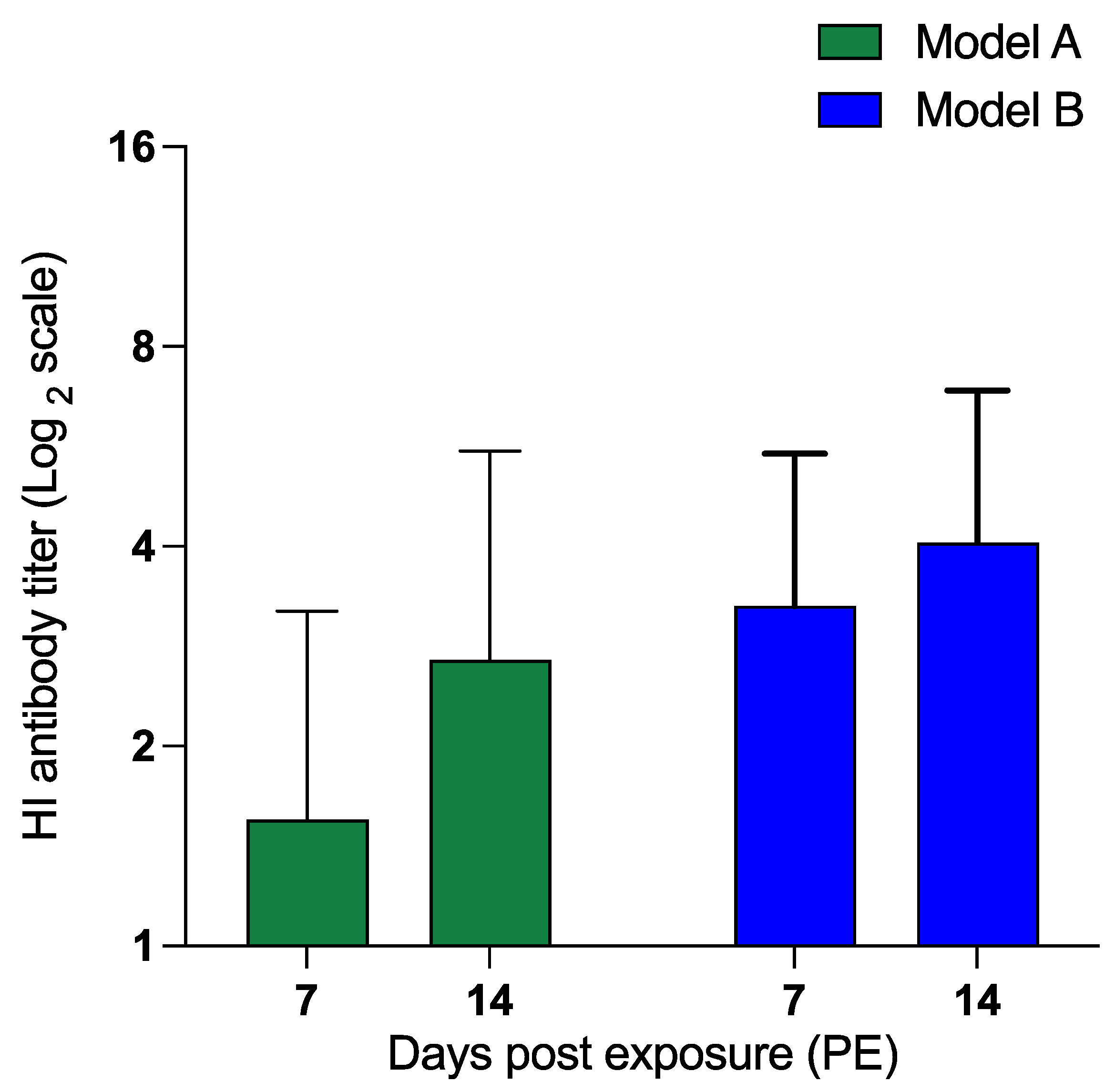
3.4. Virus Isolation and HI Antibody Titers
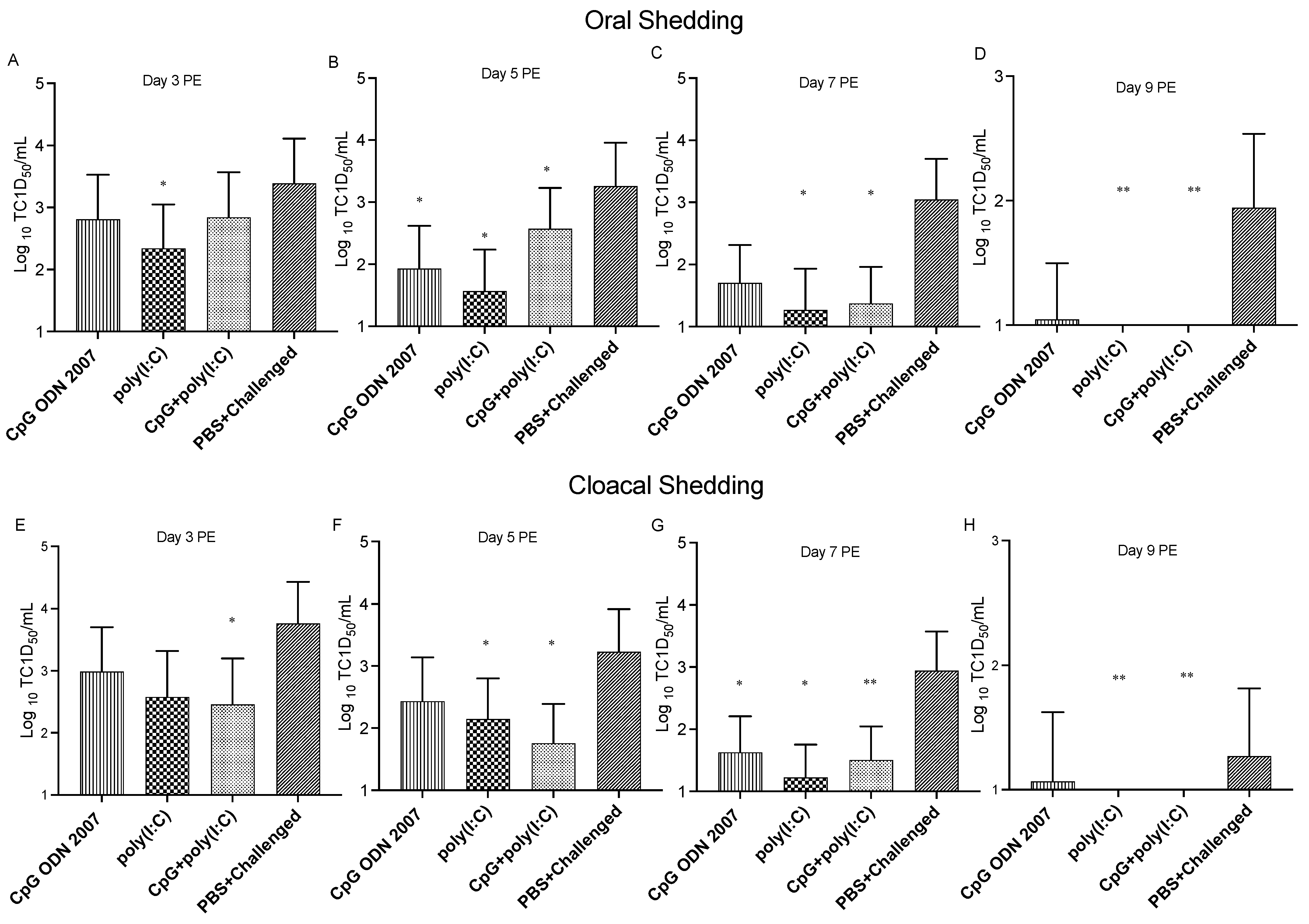
3.5. Administration of CpG ODN 2007 and Poly(I:C) Reduces Transmission of H9N2 AIV from Exposed Chickens in the Fecal Transmission Model
3.6. Treatment with TLR Ligands Induces Antiviral Responses in Different Sections of Small Intestine
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Bouvier, N.M.; Palese, P. The biology of influenza viruses. Vaccine 2008, 26, D49–D53. [Google Scholar] [CrossRef]
- Krammer, F.; Smith, G.J.D.; Fouchier, R.A.M.; Peiris, M.; Kedzierska, K.; Doherty, P.C.; Palese, P.; Shaw, M.L.; Treanor, J.; Webster, R.G.; et al. Influenza. Nat. Rev. Dis. Prim. 2018, 4, 3. [Google Scholar] [CrossRef]
- Nagy, A.; Mettenleiter, T.C.; Abdelwhab, E.M. A Brief Summary of the Epidemiology and Genetic Relatedness of Avian Influenza H9N2 Virus in Birds and Mammals in the Middle East and North Africa. Epidemiol. Infect. 2017, 145, 3320–3333. [Google Scholar] [CrossRef]
- Dhama, K.; Chauhan, R.S.; Kataria, J.M.; Mahendran, M.; Tomar, S. Avian Influenza: The Current Perspectives. J. Immunol. Immunopathol. 2005, 7, 1–33. [Google Scholar]
- Yassine, H.M.; Lee, C.-W.; Gourapura, R.; Saif, Y.M. Interspecies and Intraspecies Transmission of Influenza A Viruses: Viral, Host and Environmental Factors. Anim. Health Res. Rev. 2010, 11, 53–72. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Wang, W.; Zhang, H.; Wang, J.; Zhang, W.; Gao, J.; Wu, S.; Qi, G. Supplemental Bacillus Subtilis DSM 32315 Manipulates Intestinal Structure and Microbial Composition in Broiler Chickens. Sci. Rep. 2018, 8, 15358. [Google Scholar] [CrossRef]
- WHO. Weekly Epidemiological Record, 24 March 2017, Vol. 92, 12 (pp. 129–144). Available online: http://www.who.int/wer/2017/wer9212/en/ (accessed on 4 May 2017).
- Thompson, K.-A.; Bennett, A.M. Persistence of Influenza on Surfaces. J. Hosp. Infect. 2017, 95, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Richard, M.; Fouchier, R.A.M. Influenza A Virus Transmission via Respiratory Aerosols or Droplets as It Relates to Pandemic Potential. FEMS Microbiol. Rev. 2016, 40, 68–85. [Google Scholar] [CrossRef] [PubMed]
- Asadi, S.; Gaaloul ben Hnia, N.; Barre, R.S.; Wexler, A.S.; Ristenpart, W.D.; Bouvier, N.M. Influenza a Virus Is Transmissible via Aerosolized Fomites. Nat. Commun. 2020, 11, 4062. [Google Scholar] [CrossRef] [PubMed]
- Mubareka, S.; Lowen, A.C.; Steel, J.; Coates, A.L.; García-Sastre, A.; Palese, P. Transmission of Influenza Virus via Aerosols and Fomites in the Guinea Pig Model. J. Infect. Dis. 2009, 199, 858–865. [Google Scholar] [CrossRef]
- Hauck, R.; Crossley, B.; Rejmanek, D.; Zhou, H.; Gallardo, R.A. Persistence of Highly Pathogenic and Low Pathogenic Avian Influenza Viruses in Footbaths and Poultry Manure. Avian Dis. 2017, 61, 64–69. [Google Scholar] [CrossRef]
- Dalziel, A.E.; Delean, S.; Heinrich, S.; Cassey, P. Persistence of Low Pathogenic Influenza A Virus in Water: A Systematic Review and Quantitative Meta-Analysis. PLoS ONE 2016, 11, e0161929. [Google Scholar] [CrossRef]
- Pathak, A.P.; Murugkar, H.V.; Nagarajan, S.; Sood, R.; Tosh, C.; Kumar, M.; Athira, C.K.; Praveen, A. Survivability of Low Pathogenic (H9N2) Avian Influenza Virus in Water in the Presence of Atyopsis Moluccensis (Bamboo Shrimp). Zoonoses Public Health 2018, 65, e124–e129. [Google Scholar] [CrossRef]
- Zhang, H.; Li, Y.; Chen, J.; Chen, Q.; Chen, Z. Perpetuation of H5N1 and H9N2 Avian Influenza Viruses in Natural Water Bodies. J. Gen. Virol. 2014, 95, 1430–1435. [Google Scholar] [CrossRef] [PubMed]
- Chumpolbanchorn, K.; Suemanotham, N.; Siripara, N.; Puyati, B.; Chaichoune, K. The effect of temperature and uv light on infectivity of avian influenza virus (H5N1, Thai field strain) in chicken fecal manure. Southeast Asian J. Trop. Med. Public. Health 2006, 37, 102–105. [Google Scholar] [PubMed]
- Lu, H.; Castro, A.E.; Pennick, K.; Liu, J.; Yang, Q.; Dunn, P.; Weinstock, D.; Henzler, D. Survival of Avian Influenza Virus H7N2 in SPF Chickens and Their Environments. Avian Dis. 2003, 47, 1015–1021. [Google Scholar] [CrossRef] [PubMed]
- Nazir, J.; Haumacher, R.; Ike, A.C.; Marschang, R.E. Persistence of Avian Influenza Viruses in Lake Sediment, Duck Feces, and Duck Meat. Appl. Env. Microbiol. 2011, 77, 4981–4985. [Google Scholar] [CrossRef]
- Webster, R.G.; Yakhno, M.; Hinshaw, V.S.; Bean, W.J.; Copal Murti, K. Intestinal Influenza: Replication and Characterization of Influenza Viruses in Ducks. Virology 1978, 84, 268–278. [Google Scholar] [CrossRef]
- Zarkov, I. Survival of avian influenza virus H6N2 in faecal samples of chickens experimentally infected. Trakia J. Sci. 2013, 1, 91–94. [Google Scholar]
- De Benedictis, P.; Beato, M.S.; Capua, I. Inactivation of Avian Influenza Viruses by Chemical Agents and Physical Conditions: A Review. Zoonoses Public Health 2007, 54, 51–68. [Google Scholar] [CrossRef]
- Beard, C.W.; Brugh, M.; Johnson, D.C. Laboratory Studies with the Pennsylvania Avian Influenza Viruses (H5N2). Proceedings Annual Meeting—United States Animal Health Association (USA). 1984. Available online: https://agris.fao.org/agris-search/search.do?recordID=US8910081# (accessed on 20 March 2023).
- Yao, M.; Lv, J.; Huang, R.; Yang, Y.; Chai, T. Determination of Infective Dose of H9N2 Avian Influenza Virus in Different Routes: Aerosol, Intranasal, and Gastrointestinal. Intervirology 2014, 57, 369–374. [Google Scholar] [CrossRef]
- Raj, S.; Astill, J.; Alqazlan, N.; Boodhoo, N.; Hodgins, D.C.; Nagy, É.; Mubareka, S.; Karimi, K.; Sharif, S. Transmission of H9N2 Low Pathogenicity Avian Influenza Virus (LPAIV) in a Challenge-Transmission Model. Vaccines 2022, 10, 1040. [Google Scholar] [CrossRef]
- Alqazlan, N.; Alizadeh, M.; Boodhoo, N.; Taha-Abdelaziz, K.; Nagy, E.; Bridle, B.; Sharif, S. Probiotic Lactobacilli Limit Avian Influenza Virus Subtype H9N2 Replication in Chicken Cecal Tonsil Mononuclear Cells. Vaccines 2020, 8, 605. [Google Scholar] [CrossRef]
- Astill, J.; Alkie, T.; Yitbarek, A.; Taha-Abdelaziz, K.; Bavananthasivam, J.; Nagy, É.; Petrik, J.J.; Sharif, S. Examination of the Effects of Virus Inactivation Methods on the Induction of Antibody- and Cell-Mediated Immune Responses against Whole Inactivated H9N2 Avian Influenza Virus Vaccines in Chickens. Vaccine 2018, 36, 3908–3916. [Google Scholar] [CrossRef]
- Shojadoost, B.; Kulkarni, R.R.; Brisbin, J.T.; Quinteiro-Filho, W.; Alkie, T.N.; Sharif, S. Interactions between Lactobacilli and Chicken Macrophages Induce Antiviral Responses against Avian Influenza Virus. Res. Vet. Sci. 2019, 125, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.M.; Alkie, T.N.; Hodgins, D.C.; Nagy, É.; Shojadoost, B.; Sharif, S. Systemic Immune Responses to an Inactivated, Whole H9N2 Avian Influenza Virus Vaccine Using Class B CpG Oligonucleotides in Chickens. Vaccine 2015, 33, 3947–3952. [Google Scholar] [CrossRef] [PubMed]
- St. Paul, M.; Mallick, A.I.; Read, L.R.; Villanueva, A.I.; Parvizi, P.; Abdul-Careem, M.F.; Nagy, É.; Sharif, S. Prophylactic Treatment with Toll-like Receptor Ligands Enhances Host Immunity to Avian Influenza Virus in Chickens. Vaccine 2012, 30, 4524–4531. [Google Scholar] [CrossRef]
- Akira, S.; Takeda, K. Toll-like Receptor Signalling. Nat. Rev. Immunol. 2004, 4, 499–511. [Google Scholar] [CrossRef] [PubMed]
- Abdul-Cader, M.S.; Ahmed-Hassan, H.; Amarasinghe, A.; Nagy, E.; Sharif, S.; Abdul-Careem, M.F. Toll-like Receptor (TLR)21 Signalling-Mediated Antiviral Response against Avian Influenza Virus Infection Correlates with Macrophage Recruitment and Nitric Oxide Production. J. Gen. Virol. 2017, 98, 1209–1223. [Google Scholar] [CrossRef]
- Barjesteh, N.; Shojadoost, B.; Brisbin, J.T.; Emam, M.; Hodgins, D.C.; Nagy, É.; Sharif, S. Reduction of Avian Influenza Virus Shedding by Administration of Toll-like Receptor Ligands to Chickens. Vaccine 2015, 33, 4843–4849. [Google Scholar] [CrossRef]
- MacKinnon, K.M.; He, H.; Nerren, J.R.; Swaggerty, C.L.; Genovese, K.J.; Kogut, M.H. Expression Profile of Toll-like Receptors within the Gastrointestinal Tract of 2-Day-Old Salmonella Enteriditis-Infected Broiler Chickens. Vet. Microbiol. 2009, 137, 313–319. [Google Scholar] [CrossRef]
- St. Paul, M.; Mallick, A.I.; Haq, K.; Orouji, S.; Abdul-Careem, M.F.; Sharif, S. In Vivo Administration of Ligands for Chicken Toll-like Receptors 4 and 21 Induces the Expression of Immune System Genes in the Spleen. Vet. Immunol. Immunopathol. 2011, 144, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Reed, L.J.; Muench, H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Weber, T.P.; Stilianakis, N.I. Inactivation of Influenza A Viruses in the Environment and Modes of Transmission: A Critical Review. J. Infect. 2008, 57, 361–373. [Google Scholar] [CrossRef] [PubMed]
- Raj, S.; Alizadeh, M.; Shoojadoost, B.; Hodgins, D.; Nagy, É.; Mubareka, S.; Karimi, K.; Behboudi, S.; Sharif, S. Determining the Protective Efficacy of Toll-Like Receptor Ligands to Minimize H9N2 Avian Influenza Virus Transmission in Chickens. Viruses 2023, 15, 238. [Google Scholar] [CrossRef]
- Brisbin, J.T.; Gong, J.; Parvizi, P.; Sharif, S. Effects of Lactobacilli on Cytokine Expression by Chicken Spleen and Cecal Tonsil Cells. Clin. Vaccine Immunol. 2010, 17, 1337–1343. [Google Scholar] [CrossRef]
- Villanueva, A.I.; Kulkarni, R.R.; Sharif, S. Synthetic Double-Stranded RNA Oligonucleotides Are Immunostimulatory for Chicken Spleen Cells. Dev. Comp. Immunol. 2011, 35, 28–34. [Google Scholar] [CrossRef]
- Sorrell, E.M.; Wan, H.; Araya, Y.; Song, H.; Perez, D.R. Minimal Molecular Constraints for Respiratory Droplet Transmission of an Avian-Human H9N2 Influenza A Virus. Proc. Natl. Acad. Sci. USA 2009, 106, 7565–7570. [Google Scholar] [CrossRef]
- Figueroa, A.; Derksen, T.; Biswas, S.; Nazmi, A.; Rejmanek, D.; Crossley, B.; Pandey, P.; Gallardo, R.A. Persistence of Low and Highly Pathogenic Avian Influenza Virus in Reused Poultry Litter, Effects of Litter Amendment Use, and Composting Temperatures. J. Appl. Poult. Res. 2021, 30, 100096. [Google Scholar] [CrossRef]
- Schmitz, A.; Pertusa, M.; Le Bouquin, S.; Rousset, N.; Ogor, K.; LeBras, M.-O.; Martenot, C.; Daniel, P.; Belen Cepeda Hontecillas, A.; Scoizec, A.; et al. Natural and Experimental Persistence of Highly Pathogenic H5 Influenza Viruses in Slurry of Domestic Ducks, with or without Lime Treatment. Appl. Environ. Microbiol. 2020, 86, e02288-20. [Google Scholar] [CrossRef]
- Ku, K.B.; Park, E.H.; Yum, J.; Kim, H.M.; Kang, Y.M.; Kim, J.C.; Kim, J.A.; Kim, H.S.; Seo, S.H. Transmissibility of Novel H7N9 and H9N2 Avian Influenza Viruses between Chickens and Ferrets. Virology 2014, 450, 316–323. [Google Scholar] [CrossRef]
- Brown, J.D.; Goekjian, G.; Poulson, R.; Valeika, S.; Stallknecht, D.E. Avian Influenza Virus in Water: Infectivity Is Dependent on PH, Salinity and Temperature. Vet. Microbiol. 2009, 136, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Pawar, S.D.; Pande, S.A.; Tare, D.S.; Keng, S.S.; Kode, S.S.; Singh, D.K.; Mullick, J. Morphological and Biochemical Characteristics of Avian Faecal Droppings and Their Impact on Survival of Avian Influenza Virus. Food Env. Virol. 2018, 10, 99–106. [Google Scholar] [CrossRef]
- Stegmann, T.; Morselt, H.W.M.; Scholma, J.; Wilschut, J. Fusion of Influenza Virus in an Intracellular Acidic Compartment Measured by Fluorescence Dequenching. Biochim. Biophys. Acta-Biomembr. 1987, 904, 165–170. [Google Scholar] [CrossRef]
- Stallknecht, D.E.; Kearney, M.T.; Shane, S.M.; Zwank, P.J. Effects of PH, Temperature, and Salinity on Persistence of Avian Influenza Viruses in Water. Avian Dis. 1990, 34, 412–418. [Google Scholar] [CrossRef] [PubMed]
- Ahrens, A.K.; Selinka, H.-C.; Mettenleiter, T.C.; Beer, M.; Harder, T.C. Exploring Surface Water as a Transmission Medium of Avian Influenza Viruses—Systematic Infection Studies in Mallards. Emerg. Microbes Infect. 2022, 11, 1250–1261. [Google Scholar] [CrossRef] [PubMed]
- Globig, A.; Staubach, C.; Sauter-Louis, C.; Dietze, K.; Homeier-Bachmann, T.; Probst, C.; Gethmann, J.; Depner, K.R.; Grund, C.; Harder, T.C.; et al. Highly Pathogenic Avian Influenza H5N8 Clade 2.3.4.4b in Germany in 2016/2017. Front. Vet. Sci. 2018, 4, 240. [Google Scholar] [CrossRef]
- Pannwitz, G.; Wolf, C.; Harder, T. Active Surveillance for Avian Influenza Virus Infection in Wild Birds by Analysis of Avian Fecal Samples from the Environment. J. Wildl. Dis. 2009, 45, 512–518. [Google Scholar] [CrossRef]
- Stallknecht, D.E.; Shane, S.M.; Kearney, M.T.; Zwank, P.J. Persistence of Avian Influenza Viruses in Water. Avian Dis. 1990, 34, 406–411. [Google Scholar] [CrossRef]
- van der Sluis, H.J.; Dwars, R.M.; Vernooij, J.C.M.; Landman, W.J.M. Cloacal Reflexes and Uptake of Fluorescein-Labeled Polystyrene Beads in Broiler Chickens. Poult. Sci. 2009, 88, 1242–1249. [Google Scholar] [CrossRef]
- Wille, M.; Bröjer, C.; Lundkvist, Å.; Järhult, J.D. Alternate Routes of Influenza A Virus Infection in Mallard (Anas Platyrhynchos). Vet. Res. 2018, 49, 110. [Google Scholar] [CrossRef]
- Sedlmaier, N.; Hoppenheidt, K.; Krist, H.; Lehmann, S.; Lang, H.; Büttner, M. Generation of Avian Influenza Virus (AIV) Contaminated Fecal Fine Particulate Matter (PM2.5): Genome and Infectivity Detection and Calculation of Immission. Vet. Microbiol. 2009, 139, 156–164. [Google Scholar] [CrossRef]
- Umar, S.; Munir, M.T.; Kaboudi, K.; Rehman, A.; Asif, S.; Usman, M.; Ali, A.; Shahzad, M.; Subhan, S.; Shah, M.A.A. Effect of Route of Inoculation on Replication of Avian Influenza Virus (H9N2) and Interferon Gene Expression in Guinea Fowl (Numida meleagridis). Br. Poult. Sci. 2016, 57, 451–461. [Google Scholar] [CrossRef]
- Iqbal, M.; Yaqub, T.; Mukhtar, N.; Shabbir, M.Z.; McCauley, J.W. Infectivity and Transmissibility of H9N2 Avian Influenza Virus in Chickens and Wild Terrestrial Birds. Vet. Res. 2013, 44, 100. [Google Scholar] [CrossRef]
- de Geus, E.D.; Rebel, J.M.J.; Vervelde, L. Kinetics of the Avian Influenza-Specific Humoral Responses in Lung Are Indicative of Local Antibody Production. Dev. Comp. Immunol. 2012, 36, 317–322. [Google Scholar] [CrossRef]
- Kreijtz, J.H.C.M.; Fouchier, R.A.M.; Rimmelzwaan, G.F. Immune Responses to Influenza Virus Infection. Virus Res. 2011, 162, 19–30. [Google Scholar] [CrossRef] [PubMed]
- Taha-abdelaziz, K.; Alkie, T.N.; Hodgins, D.C.; Shojadoost, B.; Sharif, S. Characterization of Host Responses Induced by Toll-like Receptor Ligands in Chicken Cecal Tonsil Cells. Vet. Immunol. Immunopathol. 2016, 174, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Yitbarek, A.; Astill, J.; Hodgins, D.C.; Parkinson, J.; Nagy, É.; Sharif, S. Commensal Gut Microbiota Can Modulate Adaptive Immune Responses in Chickens Vaccinated with Whole Inactivated Avian Influenza Virus Subtype H9N2. Vaccine 2019, 37, 6640–6647. [Google Scholar] [CrossRef] [PubMed]
- Barjesteh, N.; Alkie, T.N.; Hodgins, D.C.; Nagy, É.; Sharif, S. Local Innate Responses to TLR Ligands in the Chicken Trachea. Viruses 2016, 8, 207. [Google Scholar] [CrossRef]
- He, H.; Genovese, K.J.; Swaggerty, C.L.; MacKinnon, K.M.; Kogut, M.H. Co-Stimulation with TLR3 and TLR21 Ligands Synergistically up-Regulates Th1-Cytokine IFN-γ and Regulatory Cytokine IL-10 Expression in Chicken Monocytes. Dev. Comp. Immunol. 2012, 36, 756–760. [Google Scholar] [CrossRef]
- Terada, T.; Nii, T.; Isobe, N.; Yoshimura, Y. Effects of Toll-like Receptor Ligands on the Expression of Proinflammatory Cytokines and Avian β-Defensins in Cultured Chick Intestine. J. Poult. Sci. 2020, 57, 210–222. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, M.; Seya, T. TLR3: Interferon Induction by Double-Stranded RNA Including Poly(I:C). Adv. Drug Deliv. Rev. 2008, 60, 805–812. [Google Scholar] [CrossRef]
- Barjesteh, N.; Behboudi, S.; Brisbin, J.T.; Villanueva, A.I.; Nagy, É.; Sharif, S. TLR Ligands Induce Antiviral Responses in Chicken Macrophages. PLoS ONE 2014, 9, e105713. [Google Scholar] [CrossRef] [PubMed]
- He, H.; Genovese, K.J.; Nisbet, D.J.; Kogut, M.H. Synergy of CpG Oligodeoxynucleotide and Double-Stranded RNA (Poly I:C) on Nitric Oxide Induction in Chicken Peripheral Blood Monocytes. Mol. Immunol. 2007, 44, 3234–3242. [Google Scholar] [CrossRef] [PubMed]
 and #: p < 0.05 between two treatment groups.
and #: p < 0.05 between two treatment groups.
 and #: p < 0.05 between two treatment groups.
and #: p < 0.05 between two treatment groups.
 and #/~: p < 0.05 between two treatment groups.
and #/~: p < 0.05 between two treatment groups.
 and #/~: p < 0.05 between two treatment groups.
and #/~: p < 0.05 between two treatment groups.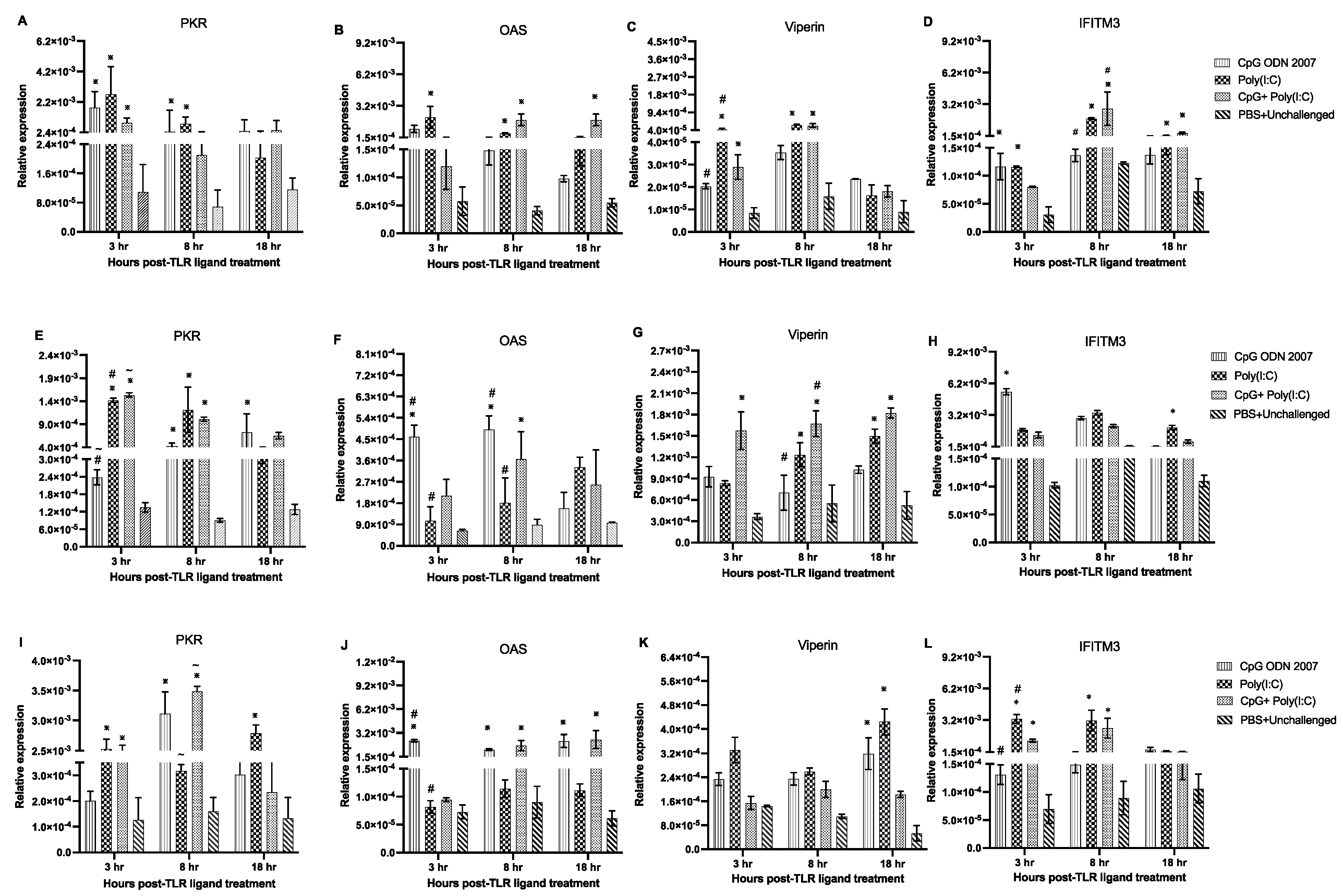
| Gene | Primer Sequence | Annealing Temperature | References |
|---|---|---|---|
| ß-actin | F:5′-CAACACAGTGCTGTCTGGTGGTA-3′ | 58 | [34] |
| R: 5′-ATCGTACTCCTGCTTGCTGATCC-3′ | |||
| IFN-γ | F: 5′-ACA CTG ACA AGT CAA AGC CGC ACA-3′ | 60 | [38] |
| R: 5′-AGT CGT TCA TCG GGA GCT TGG C-3′ | |||
| IFN-α | F: 5′-ATCCTGCTGCTCACGCTCCTTCT-3′ | 64 | [39] |
| R: 5′-GGTGTTGCTGGTGTCCAGGATG-3′ | |||
| IFN-β | F: 5′-GCCTCCAGCTCCTTCAGAATACG-3′ | 64 | [39] |
| R: 5′-CTGGATCTGGTTGAGGAGGCTGT-3′ | |||
| PKR | F: 5′-TGGTACAGGCGTTGGTAAGAG-3′ | 60 | [32] |
| R: 5′-GAGCACATCCGCAGGTAGAG-3′ | |||
| IFITM3 | F: 5′-CACACCAGCATCAACATGCC-3′ | 60 | [32] |
| R: 5′-CCTACGAAGTCCTTGGCGAT-3′ | |||
| Viperin | F: 5′-GGAGGCGGGAATGGAGAAAA-3′ | 60 | [32] |
| R: 5′-CAGCTGGCCTACAAATTCGC-3′ | |||
| OAS | F: 5′-AGAACTGCAGAAGAACTTTGT-3′ | 60 | [39] |
| R: 5′-AGAACTGCAGAAGAACTTTGT-3′ |
| No. of Swabs Positive/No. of Swabs Tested | |||
|---|---|---|---|
| Oral Swabs (Days PE) | Model A | Model B | PBS + Challenged |
| 3 | 4/10 | 7/10 | 9/10 |
| 5 | 3/10 | 6/10 | 9/10 |
| 7 | 2/10 | 5/10 | 6/10 |
| 9 | 0/10 | 0/10 | 5/10 |
| No. of Swabs Positive/No. of Swabs Tested | |||
|---|---|---|---|
| Cloacal Swabs (Days PE) | Model A | Model B | PBS + Challenged |
| 3 | 3/10 | 8/10 | 8/10 |
| 5 | 3/10 | 6/10 | 8/10 |
| 7 | 2/10 | 6/10 | 7/10 |
| 9 | 0/10 | 1/10 | 6/10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raj, S.; Matsuyama-Kato, A.; Alizadeh, M.; Boodhoo, N.; Nagy, E.; Mubareka, S.; Karimi, K.; Behboudi, S.; Sharif, S. Treatment with Toll-like Receptor (TLR) Ligands 3 and 21 Prevents Fecal Contact Transmission of Low Pathogenic H9N2 Avian Influenza Virus (AIV) in Chickens. Viruses 2023, 15, 977. https://doi.org/10.3390/v15040977
Raj S, Matsuyama-Kato A, Alizadeh M, Boodhoo N, Nagy E, Mubareka S, Karimi K, Behboudi S, Sharif S. Treatment with Toll-like Receptor (TLR) Ligands 3 and 21 Prevents Fecal Contact Transmission of Low Pathogenic H9N2 Avian Influenza Virus (AIV) in Chickens. Viruses. 2023; 15(4):977. https://doi.org/10.3390/v15040977
Chicago/Turabian StyleRaj, Sugandha, Ayumi Matsuyama-Kato, Mohammadali Alizadeh, Nitish Boodhoo, Eva Nagy, Samira Mubareka, Khalil Karimi, Shahriar Behboudi, and Shayan Sharif. 2023. "Treatment with Toll-like Receptor (TLR) Ligands 3 and 21 Prevents Fecal Contact Transmission of Low Pathogenic H9N2 Avian Influenza Virus (AIV) in Chickens" Viruses 15, no. 4: 977. https://doi.org/10.3390/v15040977
APA StyleRaj, S., Matsuyama-Kato, A., Alizadeh, M., Boodhoo, N., Nagy, E., Mubareka, S., Karimi, K., Behboudi, S., & Sharif, S. (2023). Treatment with Toll-like Receptor (TLR) Ligands 3 and 21 Prevents Fecal Contact Transmission of Low Pathogenic H9N2 Avian Influenza Virus (AIV) in Chickens. Viruses, 15(4), 977. https://doi.org/10.3390/v15040977







