Advanced Strategies for Developing Vaccines and Diagnostic Tools for African Swine Fever
Abstract
:1. Introduction
2. Vaccine Development Model for ASFV
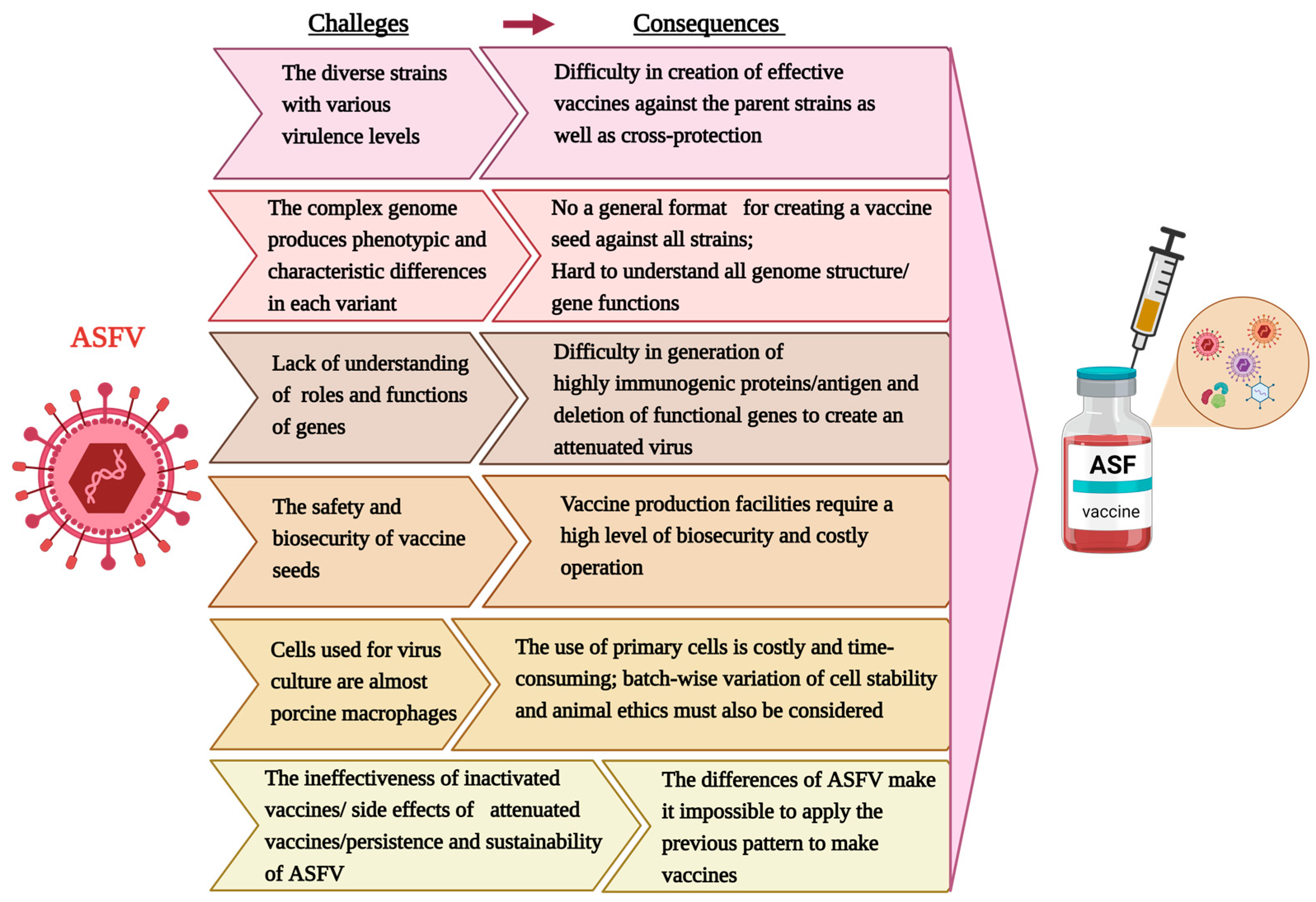
2.1. Challenges of ASF Vaccine Development
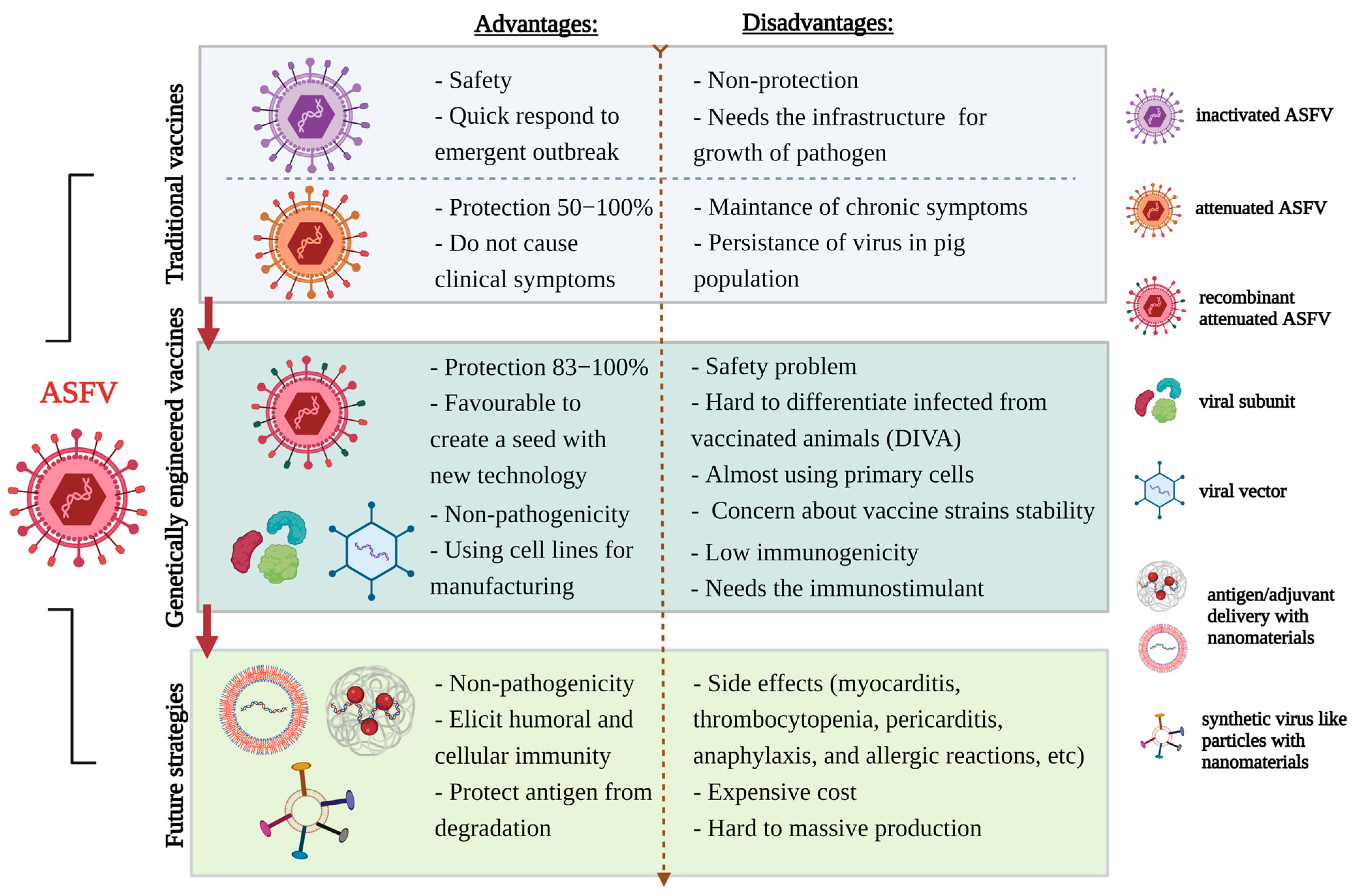
2.2. Traditional Vaccines
2.2.1. Inactivated Vaccine
2.2.2. Classical Live Attenuated Vaccine
2.3. Genetically Engineered Vaccine Platforms
2.3.1. Subunit Vaccine
2.3.2. DNA and Virus-Vectored (Delivery Vectors) Vaccines
2.3.3. Recombinant Live Attenuated Vaccine
| Type of Vaccine | Parental Strain | Genotype | Description | Challenge Strain | Safety | Efficacy | Reference |
|---|---|---|---|---|---|---|---|
| Natural live attenuated vaccine | NH/P68 | I | ASFV NH/68 produced in porcine alveolar macrophage (PAM) | Homologous strain L60 | Chronic ASF infections with side effects in the pigs | 100% | [45,88] |
| Heterologous strain Arm07 | 75% | [88] | |||||
| OUR T88/3 | I | Heterologous strain Benin 97/1 | - | 85.7% | [46] | ||
| OUR T88/3 | I | Homologous strain OURT88/1 | Fever (39.1–40 °C) | 50–100% | [47,48] | ||
| OUR T88/3 | I | Heterologous strain DRC 085/10, Heterologous strain Uganda 1965 | Fever (39.1–40 °C) | 100% | [46,47] | ||
| Lv17/WB/Rie1 | II | Homologous strain HAD Latvian ASFV | Nonspecific clinical signs | 100% | [49] | ||
| DNA and Virus-vectored vaccine | Spanish isolate E75 | I | pCMV-UbsHAPQ, encoding the three abovementioned viral determinants (sHA, p54, and p30) fused to ubiquitin | Homologous strain Spanish E75 | - | 50% | [57] |
| Ba71V | I | ASFVUblib contains 4029 clones representing 130 kbp of BA71V genome | Heterologous strain Spanish E75 | No clinical signs and adverse effects | 60% | [58] | |
| OUR T88/3 and Benin 1997/1 | I | A pool of recombinant replication-deficient human adenovirus 5 (rAd) and recombinant modified vaccinia Ankara (MVA) containing codon-optimized ASFV genes, including B602L, B646L, CP204L, E183L, E199L, EP153R, and F317L, MGF505-5R, which are known to encode ASF antigens | Virulent strain OURT88/1 | - | 100% | [60] | |
| Recombinant live attenuated vaccine | OUR T88/3 | I | Deletion of the DP71L and DP96R genes, which affect ASFV virulence | Homologous strain OURT88/1 | 50% of the pigs had swollen joints | 66% | [89] |
| Georgia 2007/1 | II | Deletion of the B119L (9 GL) gene, which affects ASFV virulence | Homologous strain Georgia 2007/1 | The degree of virulence of the ASFV-G-Δ9GL virus depends on the amount of infectious virus. Safe at low doses | 100% | [80] | |
| Georgia 2007/1 | II | Deletion of MGF505/360(6) genes, which play a role in ASFV’s ability to evade host immunity | Homologous strain Georgia 2007/1 | No clinical signs | 100% | [69] | |
| Georgia 2007/1 | II | Deletion of the DP96R(UK) and B119L (9 GL) genes, which affects ASFV virulence | Homologous strain Georgia 2007/1 | No clinical signs | 100% | [81] | |
| Benin 97/1 | II | Deletion of the MGF505/530/360 genes, which play a role in ASFV’s ability to evade host immunity | Homologous strain Benin 97/1 | Transient fever (40–40.5 °C) | 100% | [72] | |
| Benin 97/1 | II | Deletion of the DP148R gene, which affects ASFV virulence | Homologous strain Benin 97/1 | Mild clinical signs | 83% | [68] | |
| BA71 | II | Deletion of the EP402R(CD2v) gene, which affects ASFV virulence and hemadsorption | Homologous strain BA71; Heterologous strain E75 and Georgia 2007/1 | No significant clinical signs | 100% | [34] | |
| Benin 97/1 | II | Deletion of the MGF505/360 genes, which play a role in ASFV’s ability to evade host immunity | Homologous strain Benin 97/1 | Fever (40.5–41.5 °C) | 83% | [90] | |
| HLJ/18 | II | Deletion of the MGF505-1R/505-2R/505-3R/360-12L/360-13L/360-14L genes, which play a role in ASFV’s ability to evade host immunity as well as CD2v, 9GL, DP148R, and UK genes, which affect ASFV virulence | Homologous strain HLJ/18 | No clinical signs; unlikely to revert to virulence | 100% | [84] | |
| Georgia 2007/1 | II | Deletion of the I177L gene, with unknown function | Homologous strain Georgia 2007 | No clinical signs; unlikely to revert to virulence | 100% | [73,76,77,78] | |
| Georgia 2010 | II | Deletion of the A137R gene, with unknown function | Homologous strain Georgia 2010 | Transient fever (≤103.4°F) | 100% | [75] | |
| Georgia 2007/1 | II | Deletion of the I177l/LVR genes, with unknown function | Homologous strain Georgia 2007 | No clinical signs | 100% | [35] | |
| Arm/07/CBM/c2 | II | Deletion of the CDv2/A238L genes, which are involved in regulation of immune response | Heterologous virulent Korean Paju strain | No fever, no significant clinical signs | 100% | [33] | |
| SY18 | II | Deletion of the I226R gene, with unknown function | Homologous strain SY18 | No clinical signs | 100% | [85] | |
| CN/GS/2018 | II | Deletion of the MGF110-9L and MGF360-9L genes, which affect ASFV virulence | Homologous strain CN/GS/2018 | Fever (short duration and below 40.5 °C) | 100% | [86] | |
| CN/GS/2018 | II | Deletion of the DP148R, DP71L, and DP96R genes, which affect ASFV virulence | Homologous strain CN/GS/2018 | No fever, low viral load in sera (<103 HAD/mL) | 100% | [87] |
2.4. Future Strategies for ASF Vaccines
3. Advanced Detection of ASFV
3.1. Hemadsorption Test
3.2. Polymerase Chain Reaction
3.3. Isothermal Amplification-Based Molecular Diagnostics
3.4. CRISPR
3.5. Antibody-Based Immunoassay
3.6. Future Direction of ASFV Diagnostics
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Galindo, I.; Alonso, C. African swine fever virus: A review. Viruses 2017, 9, 103. [Google Scholar] [CrossRef] [PubMed]
- Gaudreault, N.N.; Madden, D.W.; Wilson, W.C.; Trujillo, J.D.; Richt, J.A. African swine fever virus: An emerging DNA arbovirus. Front. Vet. Sci. 2020, 7, 215. [Google Scholar] [CrossRef] [PubMed]
- Cwynar, P.; Stojkov, J.; Wlazlak, K. African Swine Fever Status in Europe. Viruses 2019, 11, 310. [Google Scholar] [CrossRef] [PubMed]
- Qu, H.; Ge, S.; Zhang, Y.; Wu, X.; Wang, Z. A systematic review of genotypes and serogroups of African swine fever virus. Virus Genes 2022, 58, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Authority, E.F.S.; Cortiñas Abrahantes, J.; Gogin, A.; Richardson, J.; Gervelmeyer, A. Epidemiological analyses on African swine fever in the Baltic countries and Poland. EFSA J. 2017, 15, e04732. [Google Scholar]
- Authority, E.F.S.; Boklund, A.; Cay, B.; Depner, K.; Földi, Z.; Guberti, V.; Masiulis, M.; Miteva, A.; More, S.; Olsevskis, E. Epidemiological analyses of African swine fever in the European Union (November 2017 until November 2018). EFSA J. 2018, 16, e05494. [Google Scholar]
- Zhou, X.; Li, N.; Luo, Y.; Liu, Y.; Miao, F.; Chen, T.; Zhang, S.; Cao, P.; Li, X.; Tian, K.; et al. Emergence of African Swine Fever in China, 2018. Transbound. Emerg. Dis. 2018, 65, 1482–1484. [Google Scholar] [CrossRef]
- Ge, S.; Li, J.; Fan, X.; Liu, F.; Li, L.; Wang, Q.; Ren, W.; Bao, J.; Liu, C.; Wang, H.; et al. Molecular Characterization of African Swine Fever Virus, China, 2018. Emerg. Infect. Dis. J. 2018, 24, 2131. [Google Scholar] [CrossRef]
- Li, L.; Ren, Z.; Wang, Q.; Ge, S.; Liu, Y.; Liu, C.; Liu, F.; Hu, Y.; Li, J.; Bao, J.; et al. Infection of African swine fever in wild boar, China, 2018. Transbound. Emerg. Dis. 2019, 66, 1395–1398. [Google Scholar] [CrossRef]
- Muñoz-Pérez, C.; Jurado, C.; Sánchez-Vizcaíno, J.M. African swine fever vaccine: Turning a dream into reality. Transbound. Emerg. Dis. 2021, 68, 2657–2668. [Google Scholar] [CrossRef]
- Urbano, A.C.; Ferreira, F. African swine fever control and prevention: An update on vaccine development. Emerg. Microbes Infect. 2022, 11, 2021–2033. [Google Scholar] [CrossRef] [PubMed]
- Blome, S.; Gabriel, C.; Beer, M. Pathogenesis of African swine fever in domestic pigs and European wild boar. Virus Res. 2013, 173, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Gallardo, C.; Fernández-Pinero, J.; Arias, M. African swine fever (ASF) diagnosis, an essential tool in the epidemiological investigation. Virus Res. 2019, 271, 197676. [Google Scholar] [CrossRef] [PubMed]
- Dixon, L.K.; Chapman, D.A.G.; Netherton, C.L.; Upton, C. African swine fever virus replication and genomics. Virus Res. 2013, 173, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Quembo, C.J.; Jori, F.; Vosloo, W.; Heath, L. Genetic characterization of African swine fever virus isolates from soft ticks at the wildlife/domestic interface in Mozambique and identification of a novel genotype. Transbound. Emerg. Dis. 2018, 65, 420–431. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, J.E.; Gallardo, C.; Nieto-Pelegrín, E.; Rivera-Arroyo, B.; Degefa-Negi, T.; Arias, M.; Jenberie, S.; Mulisa, D.D.; Gizaw, D.; Gelaye, E.; et al. Identification of a New Genotype of African Swine Fever Virus in Domestic Pigs from Ethiopia. Transbound. Emerg. Dis. 2017, 64, 1393–1404. [Google Scholar] [CrossRef] [PubMed]
- Boshoff, C.I.; Bastos, A.D.S.; Gerber, L.J.; Vosloo, W. Genetic characterisation of African swine fever viruses from outbreaks in southern Africa (1973–1999). Vet. Microbiol. 2007, 121, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Cisek, A.A.; Dąbrowska, I.; Gregorczyk, K.P.; Wyżewski, Z. African Swine Fever Virus: A new old enemy of Europe. Ann. Parasitol. 2016, 62, 161–167. [Google Scholar]
- Revilla, Y.; Pérez-Núñez, D.; Richt, J.A. African Swine Fever Virus Biology and Vaccine Approaches. Adv. Virus Res. 2018, 100, 41–74. [Google Scholar]
- Sánchez-Vizcaíno, J.M.; Mur, L.; Gomez-Villamandos, J.C.; Carrasco, L. An Update on the Epidemiology and Pathology of African Swine Fever. J. Comp. Pathol. 2015, 152, 9–21. [Google Scholar] [CrossRef]
- Sun, E.; Huang, L.; Zhang, X.; Zhang, J.; Shen, D.; Zhang, Z.; Wang, Z.; Huo, H.; Wang, W.; Huangfu, H.; et al. Genotype I African swine fever viruses emerged in domestic pigs in China and caused chronic infection. Emerg. Microbes Infect. 2021, 10, 2183–2193. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Liu, R.; Zhang, X.; Li, F.; Wang, J.; Zhang, J.; Liu, X.; Wang, L.; Zhang, J.; Wu, X.; et al. Replication and virulence in pigs of the first African swine fever virus isolated in China. Emerg. Microbes Infect. 2019, 8, 438–447. [Google Scholar] [CrossRef] [PubMed]
- Dixon, L.K.; Sun, H.; Roberts, H. African swine fever. Antivir. Res. 2019, 165, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Medina, E.; O’Donnell, V.; Silva, E.; Espinoza, N.; Velazquez-Salinas, L.; Moran, K.; Daite, D.A.; Barrette, R.; Faburay, B.; Holland, R.; et al. Experimental Infection of Domestic Pigs with an African Swine Fever Virus Field Strain Isolated in 2021 from the Dominican Republic. Viruses 2022, 14, 1090. [Google Scholar] [CrossRef] [PubMed]
- Pan, I.; Hess, W. Virulence in African swine fever: Its measurement and implications. Am. J. Vet. Res. 1984, 45, 361–366. [Google Scholar] [PubMed]
- Krug, P.W.; Holinka, L.G.; O’Donnell, V.; Reese, B.; Sanford, B.; Fernandez-Sainz, I.; Gladue, D.P.; Arzt, J.; Rodriguez, L.; Risatti, G.R.; et al. The Progressive Adaptation of a Georgian Isolate of African Swine Fever Virus to Vero Cells Leads to a Gradual Attenuation of Virulence in Swine Corresponding to Major Modifications of the Viral Genome. J. Virol. 2015, 89, 2324–2332. [Google Scholar] [CrossRef]
- Hurtado, C.; Bustos, M.J.; Carrascosa, A.L. The use of COS-1 cells for studies of field and laboratory African swine fever virus samples. J. Virol. Methods 2010, 164, 131–134. [Google Scholar] [CrossRef]
- Rai, A.; Pruitt, S.; Ramirez-Medina, E.; Vuono, E.A.; Silva, E.; Velazquez-Salinas, L.; Carrillo, C.; Borca, M.V.; Gladue, D.P. Identification of a Continuously Stable and Commercially Available Cell Line for the Identification of Infectious African Swine Fever Virus in Clinical Samples. Viruses 2020, 12, 820. [Google Scholar] [CrossRef]
- Meloni, D.; Franzoni, G.; Oggiano, A. Cell Lines for the Development of African Swine Fever Virus Vaccine Candidates: An Update. Vaccines 2022, 10, 707. [Google Scholar] [CrossRef]
- Masujin, K.; Kitamura, T.; Kameyama, K.i.; Okadera, K.; Nishi, T.; Takenouchi, T.; Kitani, H.; Kokuho, T. An immortalized porcine macrophage cell line competent for the isolation of African swine fever virus. Sci. Rep. 2021, 11, 4759. [Google Scholar] [CrossRef]
- Takenouchi, T.; Kitani, H.; Suzuki, S.; Nakai, M.; Fuchimoto, D.-i.; Tsukimoto, M.; Shinkai, H.; Sato, M.; Uenishi, H. Immortalization and Characterization of Porcine Macrophages That Had Been Transduced with Lentiviral Vectors Encoding the SV40 Large T Antigen and Porcine Telomerase Reverse Transcriptase. Front. Vet. Sci. 2017, 4. [Google Scholar] [CrossRef] [PubMed]
- Portugal, R.; Goatley, L.C.; Husmann, R.; Zuckermann, F.A.; Dixon, L.K. A porcine macrophage cell line that supports high levels of replication of OURT88/3, an attenuated strain of African swine fever virus. Emerg. Microbes Infect. 2020, 9, 1245–1253. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Núñez, D.; Sunwoo, S.-Y.; García-Belmonte, R.; Kim, C.; Vigara-Astillero, G.; Riera, E.; Kim, D.-m.; Jeong, J.; Tark, D.; Ko, Y.-S.; et al. Recombinant African Swine Fever Virus Arm/07/CBM/c2 Lacking CD2v and A238L Is Attenuated and Protects Pigs against Virulent Korean Paju Strain. Vaccines 2022, 10, 1992. [Google Scholar] [CrossRef] [PubMed]
- Monteagudo, P.L.; Lacasta, A.; López, E.; Bosch, L.; Collado, J.; Pina-Pedrero, S.; Correa-Fiz, F.; Accensi, F.; Navas, M.J.; Vidal, E.; et al. BA71ΔCD2: A New Recombinant Live Attenuated African Swine Fever Virus with Cross-Protective Capabilities. J. Virol. 2017, 91, e01058-17. [Google Scholar] [CrossRef] [PubMed]
- Borca, M.V.; Rai, A.; Ramirez-Medina, E.; Silva, E.; Velazquez-Salinas, L.; Vuono, E.; Pruitt, S.; Espinoza, N.; Gladue, D.P.; Jung, J.U. A Cell Culture-Adapted Vaccine Virus against the Current African Swine Fever Virus Pandemic Strain. J. Virol. 2021, 95, e00123-21. [Google Scholar] [CrossRef] [PubMed]
- LaRocco, M.; Krug, P.W.; Kramer, E.; Ahmed, Z.; Pacheco, J.M.; Duque, H.; Baxt, B.; Rodriguez, L.L. A continuous bovine kidney cell line constitutively expressing bovine αvβ6 integrin has increased susceptibility to foot-and-mouth disease virus. J. Clin. Microbiol. 2013, 51, 1714–1720. [Google Scholar] [CrossRef] [PubMed]
- McVey, S.; Shi, J. Vaccines in veterinary medicine: A brief review of history and technology. Vet. Clin. Small Anim. Pract. 2010, 40, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Tizard, I.R. Chapter 18—Porcine vaccines. In Vaccines for Veterinarians; Tizard, I.R., Ed.; Elsevier: Amsterdam, The Netherlands, 2021; pp. 225–242.e1. [Google Scholar]
- Wattanaphansak, S. Autogenous Vaccines: An Alternative to Reduce Loss and Less Antibiotics Used in Swine Production; WOAH Regional Representation for Asia and the Pacific: Tokyo, Japan, 2020. [Google Scholar]
- Stone, S.S.; Hess, W.R. Antibody response to inactivated preparations of African swine fever virus in pigs. Am. J. Vet. Res. 1967, 28, 475–481. [Google Scholar]
- Forman, A.J.; Wardley, R.C.; Wilkinson, P.J. The immunological response of pigs and guinea pigs to antigens of African swine fever virus. Arch. Virol. 1982, 74, 91–100. [Google Scholar] [CrossRef]
- Pikalo, J.; Porfiri, L.; Akimkin, V.; Roszyk, H.; Pannhorst, K.; Kangethe, R.T.; Wijewardana, V.; Sehl-Ewert, J.; Beer, M.; Cattoli, G.; et al. Vaccination With a Gamma Irradiation-Inactivated African Swine Fever Virus Is Safe But Does Not Protect Against a Challenge. Front. Immunol. 2022, 13, 832264. [Google Scholar] [CrossRef]
- Cadenas-Fernández, E.; Sánchez-Vizcaíno, J.M.; van den Born, E.; Kosowska, A.; van Kilsdonk, E.; Fernández-Pacheco, P.; Gallardo, C.; Arias, M.; Barasona, J.A. High Doses of Inactivated African Swine Fever Virus Are Safe, but Do Not Confer Protection against a Virulent Challenge. Vaccines 2021, 9, 242. [Google Scholar] [CrossRef] [PubMed]
- Blome, S.; Gabriel, C.; Beer, M. Modern adjuvants do not enhance the efficacy of an inactivated African swine fever virus vaccine preparation. Vaccine 2014, 32, 3879–3882. [Google Scholar] [CrossRef] [PubMed]
- Leitão, A.; Cartaxeiro, C.; Coelho, R.; Cruz, B.; Parkhouse, R.; Portugal, F.C.; Vigário, J.D.; Martins, C.L. The non-haemadsorbing African swine fever virus isolate ASFV/NH/P68 provides a model for defining the protective anti-virus immune response. J. Gen. Virol. 2001, 82, 513–523. [Google Scholar] [CrossRef] [PubMed]
- King, K.; Chapman, D.; Argilaguet, J.M.; Fishbourne, E.; Hutet, E.; Cariolet, R.; Hutchings, G.; Oura, C.A.L.; Netherton, C.L.; Moffat, K.; et al. Protection of European domestic pigs from virulent African isolates of African swine fever virus by experimental immunisation. Vaccine 2011, 29, 4593–4600. [Google Scholar] [CrossRef] [PubMed]
- Mulumba-Mfumu, L.K.; Goatley, L.C.; Saegerman, C.; Takamatsu, H.-H.; Dixon, L.K. Immunization of African Indigenous Pigs with Attenuated Genotype I African Swine Fever Virus OURT88/3 Induces Protection Against Challenge with Virulent Strains of Genotype I. Transbound. Emerg. Dis. 2016, 63, e323–e327. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Cordón, P.J.; Chapman, D.; Jabbar, T.; Reis, A.L.; Goatley, L.; Netherton, C.L.; Taylor, G.; Montoya, M.; Dixon, L. Different routes and doses influence protection in pigs immunised with the naturally attenuated African swine fever virus isolate OURT88/3. Antivir. Res. 2017, 138, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Gallardo, C.; Soler, A.; Rodze, I.; Nieto, R.; Cano-Gómez, C.; Fernandez-Pinero, J.; Arias, M. Attenuated and non-haemadsorbing (non-HAD) genotype II African swine fever virus (ASFV) isolated in Europe, Latvia 2017. Transbound. Emerg. Dis. 2019, 66, 1399–1404. [Google Scholar] [CrossRef]
- Balysheva, V.I.; Prudnikova, E.Y.; Galnbek, T.V.; Balyshev, V.M. Immunological properties of attenuated variants of African swine fever virus isolated in the Russian Federation. Russ. Agric. Sci. 2015, 41, 178–182. [Google Scholar] [CrossRef]
- Zsak, L.; Onisk, D.V.; Afonso, C.L.; Rock, D.L. Virulent African Swine Fever Virus Isolates Are Neutralized by Swine Immune Serum and by Monoclonal Antibodies Recognizing a 72-kDa Viral Protein. Virology 1993, 196, 596–602. [Google Scholar] [CrossRef]
- Gómez-Puertas, P.; Rodríguez, F.; Oviedo, J.M.; Ramiro-Ibáñez, F.; Ruiz-Gonzalvo, F.; Alonso, C.; Escribano, J.M. Neutralizing antibodies to different proteins of African swine fever virus inhibit both virus attachment and internalization. J. Virol. 1996, 70, 5689–5694. [Google Scholar] [CrossRef]
- Gómez-Puertas, P.; Rodríguez, F.; Oviedo, J.M.; Brun, A.; Alonso, C.; Escribano, J.M. The African swine fever virus proteins p54 and p30 are involved in two distinct steps of virus attachment and both contribute to the antibody-mediated protective immune response. Virology 1998, 243, 461–471. [Google Scholar] [CrossRef] [PubMed]
- Barderas, M.G.; Rodríguez, F.; Gómez-Puertas, P.; Avilés, M.; Beitia, F.; Alonso, C.; Escribano, J.M. Antigenic and immunogenic properties of a chimera of two immunodominant African swine fever virus proteins. Arch. Virol. 2001, 146, 1681–1691. [Google Scholar] [CrossRef] [PubMed]
- Neilan, J.G.; Zsak, L.; Lu, Z.; Burrage, T.G.; Kutish, G.F.; Rock, D.L. Neutralizing antibodies to African swine fever virus proteins p30, p54, and p72 are not sufficient for antibody-mediated protection. Virology 2004, 319, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Liu, W.; Yang, S.; Song, S.; Ma, Y.; Zhou, G.; Liang, X.; Miao, C.; Li, J.; Liu, Y.; et al. Evaluation of humoral and cellular immune responses induced by a cocktail of recombinant African swine fever virus antigens fused with OprI in domestic pigs. Virol. J. 2023, 20, 104. [Google Scholar] [CrossRef] [PubMed]
- Argilaguet, J.M.; Pérez-Martín, E.; Nofrarías, M.; Gallardo, C.; Accensi, F.; Lacasta, A.; Mora, M.; Ballester, M.; Galindo-Cardiel, I.; López-Soria, S.; et al. DNA Vaccination Partially Protects against African Swine Fever Virus Lethal Challenge in the Absence of Antibodies. PLoS ONE 2012, 7, e40942. [Google Scholar] [CrossRef] [PubMed]
- Lacasta, A.; Ballester, M.; Monteagudo, P.L.; Rodríguez, J.M.; Salas, M.L.; Accensi, F.; Pina-Pedrero, S.; Bensaid, A.; Argilaguet, J.; López-Soria, S.; et al. Expression Library Immunization Can Confer Protection against Lethal Challenge with African Swine Fever Virus. J. Virol. 2014, 88, 13322–13332. [Google Scholar] [CrossRef] [PubMed]
- Jancovich, J.K.; Chapman, D.; Hansen, D.T.; Robida, M.D.; Loskutov, A.; Craciunescu, F.; Borovkov, A.; Kibler, K.; Goatley, L.; King, K.; et al. Immunization of Pigs by DNA Prime and Recombinant Vaccinia Virus Boost To Identify and Rank African Swine Fever Virus Immunogenic and Protective Proteins. J. Virol. 2018, 92, e02219-17. [Google Scholar] [CrossRef] [PubMed]
- Goatley, L.C.; Reis, A.L.; Portugal, R.; Goldswain, H.; Shimmon, G.L.; Hargreaves, Z.; Ho, C.-S.; Montoya, M.; Sánchez-Cordón, P.J.; Taylor, G.; et al. A Pool of Eight Virally Vectored African Swine Fever Antigens Protect Pigs against Fatal Disease. Vaccines 2020, 8, 234. [Google Scholar] [CrossRef]
- Lokhandwala, S.; Petrovan, V.; Popescu, L.; Sangewar, N.; Elijah, C.; Stoian, A.; Olcha, M.; Ennen, L.; Bray, J.; Bishop, R.P.; et al. Adenovirus-vectored African Swine Fever Virus antigen cocktails are immunogenic but not protective against intranasal challenge with Georgia 2007/1 isolate. Vet. Microbiol. 2019, 235, 10–20. [Google Scholar] [CrossRef]
- Sunwoo, S.-Y.; Pérez-Núñez, D.; Morozov, I.; Sánchez, E.G.; Gaudreault, N.N.; Trujillo, J.D.; Mur, L.; Nogal, M.; Madden, D.; Urbaniak, K.; et al. DNA-Protein Vaccination Strategy Does Not Protect from Challenge with African Swine Fever Virus Armenia 2007 Strain. Vaccines 2019, 7, 12. [Google Scholar] [CrossRef]
- Zsak, L.; Lu, Z.; Kutish, G.; Neilan, J.; Rock, D. An African swine fever virus virulence-associated gene NL-S with similarity to the herpes simplex virus ICP34. 5 gene. J. Virol. 1996, 70, 8865–8871. [Google Scholar] [CrossRef]
- Lewis, T.; Zsak, L.; Burrage, T.; Lu, Z.; Kutish, G.; Neilan, J.; Rock, D. An African swine fever virus ERV1-ALR homologue, 9GL, affects virion maturation and viral growth in macrophages and viral virulence in swine. J. Virol. 2000, 74, 1275–1285. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Medina, E.; Vuono, E.; O’Donnell, V.; Holinka, L.G.; Silva, E.; Rai, A.; Pruitt, S.; Carrillo, C.; Gladue, D.P.; Borca, M.V. Differential effect of the deletion of African swine fever virus virulence-associated genes in the induction of attenuation of the highly virulent Georgia strain. Viruses 2019, 11, 599. [Google Scholar] [CrossRef]
- Sanford, B.; Holinka, L.; O’Donnell, V.; Krug, P.; Carlson, J.; Alfano, M.; Carrillo, C.; Wu, P.; Lowe, A.; Risatti, G. Deletion of the thymidine kinase gene induces complete attenuation of the Georgia isolate of African swine fever virus. Virus Res. 2016, 213, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Carlson, J.; O’Donnell, V.; Alfano, M.; Velazquez Salinas, L.; Holinka, L.G.; Krug, P.W.; Gladue, D.P.; Higgs, S.; Borca, M.V. Association of the host immune response with protection using a live attenuated African swine fever virus model. Viruses 2016, 8, 291. [Google Scholar] [CrossRef] [PubMed]
- Reis, A.L.; Goatley, L.C.; Jabbar, T.; Sanchez-Cordon, P.J.; Netherton, C.L.; Chapman, D.A.; Dixon, L.K. Deletion of the African swine fever virus gene DP148R does not reduce virus replication in culture but reduces virus virulence in pigs and induces high levels of protection against challenge. J. Virol. 2017, 91, e01428-17. [Google Scholar] [CrossRef]
- O’Donnell, V.; Holinka, L.G.; Gladue, D.P.; Sanford, B.; Krug, P.W.; Lu, X.; Arzt, J.; Reese, B.; Carrillo, C.; Risatti, G.R.; et al. African Swine Fever Virus Georgia Isolate Harboring Deletions of MGF360 and MGF505 Genes Is Attenuated in Swine and Confers Protection against Challenge with Virulent Parental Virus. J. Virol. 2015, 89, 6048–6056. [Google Scholar] [CrossRef] [PubMed]
- Ding, M.; Dang, W.; Liu, H.; Xu, F.; Huang, H.; Sunkang, Y.; Li, T.; Pei, J.; Liu, X.; Zhang, Y.; et al. Combinational Deletions of MGF360-9L and MGF505-7R Attenuated Highly Virulent African Swine Fever Virus and Conferred Protection against Homologous Challenge. J. Virol. 2022, 96, e00329-22. [Google Scholar] [CrossRef]
- Zhang, K.; Yang, B.; Shen, C.; Zhang, T.; Hao, Y.; Zhang, D.; Liu, H.; Shi, X.; Li, G.; Yang, J.; et al. MGF360-9L Is a Major Virulence Factor Associated with the African Swine Fever Virus by Antagonizing the JAK/STAT Signaling Pathway. mBio 2022, 13, e02330-21. [Google Scholar] [CrossRef]
- Reis, A.L.; Abrams, C.C.; Goatley, L.C.; Netherton, C.; Chapman, D.G.; Sanchez-Cordon, P.; Dixon, L.K. Deletion of African swine fever virus interferon inhibitors from the genome of a virulent isolate reduces virulence in domestic pigs and induces a protective response. Vaccine 2016, 34, 4698–4705. [Google Scholar] [CrossRef]
- Borca, M.V.; Ramirez-Medina, E.; Silva, E.; Vuono, E.; Rai, A.; Pruitt, S.; Espinoza, N.; Velazquez-Salinas, L.; Gay, C.G.; Gladue, D.P. ASFV-G-∆I177L as an Effective Oral Nasal Vaccine against the Eurasia Strain of Africa Swine Fever. Viruses 2021, 13, 765. [Google Scholar] [CrossRef]
- Borca, M.V.; Holinka, L.G.; Berggren, K.A.; Gladue, D.P. CRISPR-Cas9, a tool to efficiently increase the development of recombinant African swine fever viruses. Sci. Rep. 2018, 8, 3154. [Google Scholar] [CrossRef] [PubMed]
- Gladue, D.P.; Ramirez-Medina, E.; Vuono, E.; Silva, E.; Rai, A.; Pruitt, S.; Espinoza, N.; Velazquez-Salinas, L.; Borca, M.V. Deletion of the A137R Gene from the Pandemic Strain of African Swine Fever Virus Attenuates the Strain and Offers Protection against the Virulent Pandemic Virus. J. Virol. 2021, 95, e0113921. [Google Scholar] [CrossRef] [PubMed]
- Borca, M.V.; Ramirez-Medina, E.; Silva, E.; Vuono, E.; Rai, A.; Pruitt, S.; Holinka, L.G.; Velazquez-Salinas, L.; Zhu, J.; Gladue, D.P.; et al. Development of a Highly Effective African Swine Fever Virus Vaccine by Deletion of the I177L Gene Results in Sterile Immunity against the Current Epidemic Eurasia Strain. J. Virol. 2020, 94, e02017-19. [Google Scholar] [CrossRef] [PubMed]
- Tran, X.H.; Le, T.T.P.; Nguyen, Q.H.; Do, T.T.; Nguyen, V.D.; Gay, C.G.; Borca, M.V.; Gladue, D.P. African swine fever virus vaccine candidate ASFV-G-ΔI177L efficiently protects European and native pig breeds against circulating Vietnamese field strain. Transbound. Emerg. Dis. 2021, 69, e497–e504. [Google Scholar] [PubMed]
- Tran, X.H.; Phuong, L.T.T.; Huy, N.Q.; Thuy, D.T.; Nguyen, V.D.; Quang, P.H.; Ngôn, Q.V.; Rai, A.; Gay, C.G.; Gladue, D.P.; et al. Evaluation of the Safety Profile of the ASFV Vaccine Candidate ASFV-G-∆I177L. Viruses 2022, 14, 896. [Google Scholar] [CrossRef] [PubMed]
- Ta, H.L. Quality Control of A Live—Attenuated African Swine Fever Vaccine in Viet Nam; WOAH Regional Representation for Asia and the Pacific, Tokyo, Japan, 2022.
- O’Donnell, V.; Holinka, L.G.; Krug, P.W.; Gladue, D.P.; Carlson, J.; Sanford, B.; Alfano, M.; Kramer, E.; Lu, Z.; Arzt, J.; et al. African Swine Fever Virus Georgia 2007 with a Deletion of Virulence-Associated Gene 9GL (B119L), when Administered at Low Doses, Leads to Virus Attenuation in Swine and Induces an Effective Protection against Homologous Challenge. J. Virol. 2015, 89, 8556–8566. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, V.; Risatti, G.R.; Holinka, L.G.; Krug, P.W.; Carlson, J.; Velazquez-Salinas, L.; Azzinaro, P.A.; Gladue, D.P.; Borca, M.V.; Perlman, S. Simultaneous Deletion of the 9GL and UK Genes from the African Swine Fever Virus Georgia 2007 Isolate Offers Increased Safety and Protection against Homologous Challenge. J. Virol. 2017, 91, e01760-16. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, V.; Holinka, L.G.; Sanford, B.; Krug, P.W.; Carlson, J.; Pacheco, J.M.; Reese, B.; Risatti, G.R.; Gladue, D.P.; Borca, M.V. African swine fever virus Georgia isolate harboring deletions of 9GL and MGF360/505 genes is highly attenuated in swine but does not confer protection against parental virus challenge. Virus Res. 2016, 221, 8–14. [Google Scholar] [CrossRef]
- Han, N.; Qu, H.; Xu, T.; Hu, Y.; Zhang, Y.; Ge, S. Summary of the Current Status of African Swine Fever Vaccine Development in China. Vaccines 2023, 11, 762. [Google Scholar] [CrossRef]
- Chen, W.; Zhao, D.; He, X.; Liu, R.; Wang, Z.; Zhang, X.; Li, F.; Shan, D.; Chen, H.; Zhang, J.; et al. A seven-gene-deleted African swine fever virus is safe and effective as a live attenuated vaccine in pigs. Sci. China Life Sci. 2020, 63, 623–634. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ke, J.; Zhang, J.; Yang, J.; Yue, H.; Zhou, X.; Qi, Y.; Zhu, R.; Miao, F.; Li, Q.; et al. African Swine Fever Virus Bearing an I226R Gene Deletion Elicits Robust Immunity in Pigs to African Swine Fever. J. Virol. 2021, 95, e0119921. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Ren, J.; Zhu, G.; Wu, P.; Yang, W.; Ru, Y.; Feng, T.; Liu, H.; Zhang, J.; Peng, J.; et al. Deletions of MGF110-9L and MGF360-9L from African swine fever virus are highly attenuated in swine and confer protection against homologous challenge. J. Biol. Chem. 2023, 299, 104767. [Google Scholar] [CrossRef]
- Qi, X.; Feng, T.; Ma, Z.; Zheng, L.; Liu, H.; Shi, Z.; Shen, C.; Li, P.; Wu, P.; Ru, Y.; et al. Deletion of DP148R, DP71L, and DP96R Attenuates African Swine Fever Virus, and the Mutant Strain Confers Complete Protection against Homologous Challenges in Pigs. J. Virol. 2023, 97, e00247-23. [Google Scholar] [CrossRef] [PubMed]
- Gallardo, C.; Sánchez, E.G.; Pérez-Núñez, D.; Nogal, M.; de León, P.; Carrascosa, Á.L.; Nieto, R.; Soler, A.; Arias, M.L.; Revilla, Y. African swine fever virus (ASFV) protection mediated by NH/P68 and NH/P68 recombinant live-attenuated viruses. Vaccine 2018, 36, 2694–2704. [Google Scholar] [CrossRef] [PubMed]
- Abrams, C.C.; Goatley, L.; Fishbourne, E.; Chapman, D.; Cooke, L.; Oura, C.A.; Netherton, C.L.; Takamatsu, H.-H.; Dixon, L.K. Deletion of virulence associated genes from attenuated African swine fever virus isolate OUR T88/3 decreases its ability to protect against challenge with virulent virus. Virology 2013, 443, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Cordón, P.J.; Jabbar, T.; Berrezaie, M.; Chapman, D.; Reis, A.; Sastre, P.; Rueda, P.; Goatley, L.; Dixon, L.K. Evaluation of protection induced by immunisation of domestic pigs with deletion mutant African swine fever virus BeninΔMGF by different doses and routes. Vaccine 2018, 36, 707–715. [Google Scholar] [CrossRef]
- Sereda, A.D.; Balyshev, V.M.; Kazakova, A.S.; Imatdinov, A.R.; Kolbasov, D.V. Protective Properties of Attenuated Strains of African Swine Fever Virus Belonging to Seroimmunotypes I–VIII. Pathogens 2020, 9, 274. [Google Scholar] [CrossRef]
- Pérez-Núñez, D.; Castillo-Rosa, E.; Vigara-Astillero, G.; García-Belmonte, R.; Gallardo, C.; Revilla, Y. Identification and Isolation of Two Different Subpopulations Within African Swine Fever Virus Arm/07 Stock. Vaccines 2020, 8, 625. [Google Scholar] [CrossRef]
- FAS. Livestock and Poultry: World Markets and Trade; US Department of Agriculture, & USDA Foreign Agricultural Service: Washington, DC, USA, 2023. [Google Scholar]
- Nga, B.T.T.; Padungtod, P.; Depner, K.; Chuong, V.D.; Duy, D.T.; Anh, N.D.; Dietze, K. Implications of partial culling on African swine fever control effectiveness in Vietnam. Front. Vet. Sci. 2022, 9, 957918. [Google Scholar] [CrossRef]
- Chan, W.C.W. Nano Research for COVID-19. ACS Nano 2020, 14, 3719–3720. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.W.; Na, W.; Kim, H.O.; Yeom, M.; Park, G.; Kang, A.; Chun, H.; Park, C.; Oh, S.; Le, V.P. Cationic Poly (Amino Acid) Vaccine Adjuvant for Promoting Both Cell-Mediated and Humoral Immunity Against Influenza Virus. Adv. Healthc. Mater. 2019, 8, 1800953. [Google Scholar] [CrossRef] [PubMed]
- Dhakal, S.; Hiremath, J.; Bondra, K.; Lakshmanappa, Y.S.; Shyu, D.-L.; Ouyang, K.; Kang, K.-i.; Binjawadagi, B.; Goodman, J.; Tabynov, K.; et al. Biodegradable nanoparticle delivery of inactivated swine influenza virus vaccine provides heterologous cell-mediated immune response in pigs. J. Control Release 2017, 247, 194–205. [Google Scholar] [CrossRef] [PubMed]
- Dhakal, S.; Goodman, J.; Bondra, K.; Lakshmanappa, Y.S.; Hiremath, J.; Shyu, D.-L.; Ouyang, K.; Kang, K.-i.; Krakowka, S.; Wannemuehler, M.J.; et al. Polyanhydride nanovaccine against swine influenza virus in pigs. Vaccine 2017, 35, 1124–1131. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Du, L.; Yu, Z.; Sun, B.; Xu, X.; Fan, B.; Guo, R.; Yuan, W.; He, K. Poly (d,l-lactide-co-glycolide) nanoparticle-entrapped vaccine induces a protective immune response against porcine epidemic diarrhea virus infection in piglets. Vaccine 2017, 35, 7010–7017. [Google Scholar] [CrossRef] [PubMed]
- Sun, B.; Xia, T. Nanomaterial-based vaccine adjuvants. J. Mater. Chem. B 2016, 4, 5496–5509. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.-W.; Na, W.; Kim, H.-O.; Yeom, M.; Kang, A.; Park, G.; Park, C.; Ki, J.; Lee, S.; Jung, B. Co-delivery of antigens and immunostimulants via a polymersome for improvement of antigen-specific immune response. J. Mater. Chem. B 2020, 8, 5620–5626. [Google Scholar] [CrossRef] [PubMed]
- Zeng, C.; Hou, X.; Yan, J.; Zhang, C.; Li, W.; Zhao, W.; Du, S.; Dong, Y. Leveraging mRNA Sequences and Nanoparticles to Deliver SARS-CoV-2 Antigens In Vivo. Adv. Mater. 2020, 32, 2004452. [Google Scholar] [CrossRef]
- Pardi, N.; Hogan, M.J.; Porter, F.W.; Weissman, D. mRNA vaccines—A new era in vaccinology. Nat. Rev. Drug Discov. 2018, 17, 261–279. [Google Scholar] [CrossRef]
- Lim, M.; Badruddoza, A.Z.M.; Firdous, J.; Azad, M.; Mannan, A.; Al-Hilal, T.A.; Cho, C.-S.; Islam, M.A. Engineered nanodelivery systems to improve DNA vaccine technologies. Pharmaceutics 2020, 12, 30. [Google Scholar] [CrossRef]
- Lim, J.-W.; Ahn, Y.-R.; Park, G.; Kim, H.-O.; Haam, S. Application of nanomaterials as an advanced strategy for the diagnosis, prevention, and treatment of viral diseases. Pharmaceutics 2021, 13, 1570. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Pinero, J.; Gallardo, C.; Elizalde, M.; Robles, A.; Gómez, C.; Bishop, R.; Heath, L.; Couacy-Hymann, E.; Fasina, F.O.; Pelayo, V.; et al. Molecular Diagnosis of African Swine Fever by a New Real-Time PCR Using Universal Probe Library. Transbound. Emerg. Dis. 2013, 60, 48–58. [Google Scholar] [CrossRef] [PubMed]
- King, D.P.; Reid, S.M.; Hutchings, G.H.; Grierson, S.S.; Wilkinson, P.J.; Dixon, L.K.; Bastos, A.D.S.; Drew, T.W. Development of a TaqMan® PCR assay with internal amplification control for the detection of African swine fever virus. J. Virol. Methods 2003, 107, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Agüero, M.; Fernández, J.; Romero, L.; Mascaraque, C.S.; Arias, M.; Sánchez-Vizcaíno, J.M. Highly Sensitive PCR Assay for Routine Diagnosis of African Swine Fever Virus in Clinical Samples. J. Clin. Microbiol. 2003, 41, 4431–4434. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xu, L.Z.; Noll, L.; Stoy, C.; Porter, E.; Fu, J.P.; Feng, Y.; Peddireddi, L.; Liu, X.M.; Dodd, K.A.; et al. Development of a real-time PCR assay for detection of African swine fever virus with an endogenous internal control. Transbound. Emerg. Dis. 2020, 67, 2446–2454. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Jia, R.; Liu, Y.; Zhou, J.; Qi, Y.; Chen, Y.; Liu, D.; Zhao, J.; Shi, H.; Zhang, J.; et al. Development of a novel quantitative real-time PCR assay with lyophilized powder reagent to detect African swine fever virus in blood samples of domestic pigs in China. Transbound. Emerg. Dis. 2020, 67, 284–297. [Google Scholar] [CrossRef] [PubMed]
- Trinh, T.B.N.; Truong, T.; Nguyen, V.T.; Vu, X.D.; Dao, L.A.; Nguyen, T.L.; Ambagala, A.; Babiuk, S.; Oh, J.; Song, D.; et al. Development of a novel real-time PCR assay targeting p54 gene for rapid detection of African swine fever virus (ASFV) strains circulating in Vietnam. Vet. Med. Sci. 2021, 7, 2268–2272. [Google Scholar] [CrossRef] [PubMed]
- Hwang, H.J.; Choi, Y.S.; Song, K.; Frant, M.; Kim, J.H. Development and validation of a fast quantitative real-time PCR assay for the detection of African swine fever virus. Front. Vet. Sci. 2023, 9, 1037728. [Google Scholar] [CrossRef]
- Song, X.-p.; Xia, Y.-j.; Xu, L.; Zhao, J.-j.; Wang, Z.; Zhao, Q.-z.; Liu, Y.-b.; Zhang, Q.-y.; Wang, Q. A multiplex real-time PCR assay for simultaneous detection of classical swine fever virus, African swine fever virus, and atypical porcine pestivirus. J. Integr. Agric. 2023, 22, 559–567. [Google Scholar] [CrossRef]
- Liu, H.; Zou, J.; Liu, R.; Chen, J.; Li, X.; Zheng, H.; Li, L.; Zhou, B. Development of a TaqMan-Probe-Based Multiplex Real-Time PCR for the Simultaneous Detection of African Swine Fever Virus, Porcine Circovirus 2, and Pseudorabies Virus in East China from 2020 to 2022. Veterinary Sciences 2023, 10, 106. [Google Scholar] [CrossRef]
- Daigle, J.; Onyilagha, C.; Truong, T.; Le, V.P.; Nga, B.T.T.; Nguyen, T.L.; Clavijo, A.; Ambagala, A. Rapid and highly sensitive portable detection of African swine fever virus. Transbound. Emerg. Dis. 2021, 68, 952–959. [Google Scholar] [CrossRef] [PubMed]
- Tran, H.N.T.; Le, N.-C.T.; Pham, B.P.; Luu, V.Q.; Nguyen, V.-L. Evaluation of an automated insulated isothermal polymerase chain reaction system for rapid and reliable, on-site detection of African swine fever virus. J. Am. Vet. Med. Assoc. 2021, 259, 662–668. [Google Scholar] [CrossRef] [PubMed]
- Song, R.; Liu, P.; Yang, Y.; Lee, H.S.; Chen, C.; Wu, X.; Li, X. Development of a Duplex Insulated Isothermal PCR Assay for Rapid On-Site Detection and Differentiation of Genotypes 1 and 2 of African Swine Fever Virus. Front. Cell. Infect. Microbiol. 2022, 12, 948771. [Google Scholar] [CrossRef] [PubMed]
- Zou, T.; Deng, J.; Li, X.; Zhang, S.; Chen, L.; Hao, L.; Zhuang, J.; Wang, H.; Zhang, G.; Ge, S.; et al. Development of a fluorescent probe hydrolysis-insulated isothermal PCR for rapid and sensitive on-site detection of African swine fever virus. Virol. Sin. 2022, 37, 462–464. [Google Scholar] [CrossRef]
- Lin, Y.-H.; Lin, Y.-J.; Chang, T.-D.; Hong, L.-L.; Chen, T.-Y.; Chang, P.-F.L. Development of a TaqMan Probe-Based Insulated Isothermal Polymerase Chain Reaction (iiPCR) Assay for Detection of Fusarium oxysporum f. sp. cubense Race 4. PLoS ONE 2016, 11, e0159681. [Google Scholar] [CrossRef]
- Wilkes, R.P.; Tsai, Y.-L.; Lee, P.-Y.; Lee, F.-C.; Chang, H.-F.G.; Wang, H.-T.T. Rapid and sensitive detection of canine distemper virus by one-tube reverse transcription-insulated isothermal polymerase chain reaction. BMC Vet. Res. 2014, 10, 213. [Google Scholar] [CrossRef]
- Reid, M.S.; Le, X.C.; Zhang, H. Exponential Isothermal Amplification of Nucleic Acids and Assays for Proteins, Cells, Small Molecules, and Enzyme Activities: An EXPAR Example. Angew. Chem. Int. Ed. Engl. 2018, 57, 11856–11866. [Google Scholar] [CrossRef]
- Zhao, Y.; Chen, F.; Li, Q.; Wang, L.; Fan, C. Isothermal Amplification of Nucleic Acids. Chem. Rev. 2015, 115, 12491–12545. [Google Scholar] [CrossRef]
- Pumford, E.A.; Lu, J.; Spaczai, I.; Prasetyo, M.E.; Zheng, E.M.; Zhang, H.; Kamei, D.T. Developments in integrating nucleic acid isothermal amplification and detection systems for point-of-care diagnostics. Biosens. Bioelectron. 2020, 170, 112674. [Google Scholar] [CrossRef]
- Notomi, T.; Mori, Y.; Tomita, N.; Kanda, H. Loop-mediated isothermal amplification (LAMP): Principle, features, and future prospects. J. Microbiol. 2015, 53, 1–5. [Google Scholar] [CrossRef]
- Lee, H.; Lee, S.; Park, C.; Yeom, M.; Lim, J.-W.; Vu, T.T.H.; Kim, E.; Song, D.; Haam, S. Rapid Visible Detection of African Swine Fever Virus Using Hybridization Chain Reaction-Sensitized Magnetic Nanoclusters and Affinity Chromatography. Small 2023, 19, 2207117. [Google Scholar] [CrossRef] [PubMed]
- Asadi, R.; Mollasalehi, H. The mechanism and improvements to the isothermal amplification of nucleic acids, at a glance. Anal. Biochem. 2021, 631, 114260. [Google Scholar] [CrossRef]
- Parida, M.; Sannarangaiah, S.; Dash, P.K.; Rao, P.V.L.; Morita, K. Loop mediated isothermal amplification (LAMP): A new generation of innovative gene amplification technique; perspectives in clinical diagnosis of infectious diseases. Rev. Med. Virol. 2008, 18, 407–421. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.E.; Lim, B.; Hsu, C.-C.; Xiong, D.; Wu, W.; Yu, Y.; Jia, H.; Wang, Y.; Zeng, Y.; Ji, M.; et al. RT-LAMP for rapid diagnosis of coronavirus SARS-CoV-2. Microb. Biotechnol. 2020, 13, 950–961. [Google Scholar] [CrossRef] [PubMed]
- Oscorbin, I.P.; Belousova, E.A.; Zakabunin, A.I.; Boyarskikh, U.A.; Filipenko, M.L. Comparison of fluorescent intercalating dyes for quantitative loop-mediated isothermal amplification (qLAMP). BioTechniques 2016, 61, 20–25. [Google Scholar] [CrossRef] [PubMed]
- James, H.E.; Ebert, K.; McGonigle, R.; Reid, S.M.; Boonham, N.; Tomlinson, J.A.; Hutchings, G.H.; Denyer, M.; Oura, C.A.L.; Dukes, J.P.; et al. Detection of African swine fever virus by loop-mediated isothermal amplification. J. Virol. Methods 2010, 164, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Yu, J.; Wang, Y.; Zhang, M.; Li, P.; Liu, M.; Liu, Y. Development of a real-time loop-mediated isothermal amplification (LAMP) assay and visual LAMP assay for detection of African swine fever virus (ASFV). J. Virol. Methods 2020, 276, 113775. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Dai, J.; Liu, Y.; Yang, J.; Hou, Q.; Ou, Y.; Ding, Y.; Ma, B.; Chen, H.; Li, M.; et al. Development of a Potential Penside Colorimetric LAMP Assay Using Neutral Red for Detection of African Swine Fever Virus. Front. Microbiol. 2021, 12, 609821. [Google Scholar] [CrossRef]
- Tran, D.H.; Tran, H.T.; Le, U.P.; Vu, X.D.; Trinh, T.B.N.; Do, H.D.K.; Than, V.T.; Bui, L.M.; Vu, V.V.; Nguyen, T.L.; et al. Direct colorimetric LAMP assay for rapid detection of African swine fever virus: A validation study during an outbreak in Vietnam. Transbound. Emerg. Dis. 2021, 68, 2595–2602. [Google Scholar] [CrossRef]
- Ceruti, A.; Kobialka, R.M.; Ssekitoleko, J.; Okuni, J.B.; Blome, S.; Abd El Wahed, A.; Truyen, U. Rapid Extraction and Detection of African Swine Fever Virus DNA Based on Isothermal Recombinase Polymerase Amplification Assay. Viruses 2021, 13, 1731. [Google Scholar] [CrossRef]
- Ilya, T.; Monoldorova, S.; Kang, S.-S.; Yun, S.; Byeon, H.-S.; Mariia, N.; Jeon, B.-Y. Development of a Real-Time Recombinase Polymerase Amplification Assay for the Rapid Detection of African Swine Fever Virus Genotype I and II. Pathogens 2022, 11, 439. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.; Li, L.; Zhao, Y.; Liu, Y.; Liu, C.; Wang, Q.; Dong, Y.; Wang, S.; Chi, T.; Song, F.; et al. Clinical Validation of Two Recombinase-Based Isothermal Amplification Assays (RPA/RAA) for the Rapid Detection of African Swine Fever Virus. Front. Microbiol. 2020, 11, 1619. [Google Scholar] [CrossRef] [PubMed]
- Miao, F.; Zhang, J.; Li, N.; Chen, T.; Wang, L.; Zhang, F.; Mi, L.; Zhang, J.; Wang, S.; Wang, Y.; et al. Rapid and Sensitive Recombinase Polymerase Amplification Combined With Lateral Flow Strip for Detecting African Swine Fever Virus. Front. Microbiol. 2019, 10, 1004. [Google Scholar] [CrossRef] [PubMed]
- Zhai, Y.; Ma, P.; Fu, X.; Zhang, L.; Cui, P.; Li, H.; Yan, W.; Wang, H.; Yang, X. A recombinase polymerase amplification combined with lateral flow dipstick for rapid and specific detection of African swine fever virus. J. Virol. Methods 2020, 285, 113885. [Google Scholar] [CrossRef] [PubMed]
- Wen, X.; Xie, Q.; Li, J.; Pei, Y.; Bai, Y.; Liu, F.; Cui, H.; Shao, G.; Feng, Z. Rapid and sensitive detection of African swine fever virus in pork using recombinase aided amplification combined with QDMs-based test strip. Anal. Bioanal. Chem. 2022, 414, 3885–3894. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhan, L.; Qin, Z.; Sackrison, J.; Bischof, J.C. Ultrasensitive and Highly Specific Lateral Flow Assays for Point-of-Care Diagnosis. ACS Nano 2021, 15, 3593–3611. [Google Scholar] [CrossRef] [PubMed]
- Yue, H.; Shu, B.; Tian, T.; Xiong, E.; Huang, M.; Zhu, D.; Sun, J.; Liu, Q.; Wang, S.; Li, Y.; et al. Droplet Cas12a Assay Enables DNA Quantification from Unamplified Samples at the Single-Molecule Level. Nano Lett. 2021, 21, 4643–4653. [Google Scholar] [CrossRef] [PubMed]
- Qian, S.; Chen, Y.; Peng, C.; Wang, X.; Wu, H.; Che, Y.; Wang, H.; Xu, J.; Wu, J. Dipstick-based rapid nucleic acids purification and CRISPR/Cas12a-mediated isothermal amplification for visual detection of African swine fever virus. Talanta 2022, 242, 123294. [Google Scholar] [CrossRef]
- Fu, J.; Zhang, Y.; Cai, G.; Meng, G.; Shi, S. Rapid and sensitive RPA-Cas12a-fluorescence assay for point-of-care detection of African swine fever virus. PLoS ONE 2021, 16, e0254815. [Google Scholar] [CrossRef]
- Tao, D.; Liu, J.; Nie, X.; Xu, B.; Tran-Thi, T.-N.; Niu, L.; Liu, X.; Ruan, J.; Lan, X.; Peng, G.; et al. Application of CRISPR-Cas12a Enhanced Fluorescence Assay Coupled with Nucleic Acid Amplification for the Sensitive Detection of African Swine Fever Virus. ACS Synth. Biol. 2020, 9, 2339–2350. [Google Scholar] [CrossRef]
- Zhu, M.; Huangfu, C.; Wan, W.; Wang, M.; Lv, H.; Zhang, X.; Wang, F.; Zhi, H.; Huang, Y.; Chen, M.; et al. A Novel Virus Detection Strategy Enabled by TR512-Peptide-Based Bioorthogonal Capture and Enrichment of Preamplified Nucleic Acid. Anal. Chem. 2022, 94, 5591–5598. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Li, F.; Chen, Q.; Wu, J.; Duan, J.; Lei, X.; Zhang, Y.; Zhao, D.; Bu, Z.; Yin, H. Rapid detection of African swine fever virus using Cas12a-based portable paper diagnostics. Cell Discov. 2020, 6, 18. [Google Scholar] [CrossRef] [PubMed]
- He, Q.; Yu, D.; Bao, M.; Korensky, G.; Chen, J.; Shin, M.; Kim, J.; Park, M.; Qin, P.; Du, K. High-throughput and all-solution phase African Swine Fever Virus (ASFV) detection using CRISPR-Cas12a and fluorescence based point-of-care system. Biosens. Bioelectron. 2020, 154, 112068. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ji, P.; Fan, H.; Dang, L.; Wan, W.; Liu, S.; Li, Y.; Yu, W.; Li, X.; Ma, X.; et al. CRISPR/Cas12a technology combined with immunochromatographic strips for portable detection of African swine fever virus. Commun. Biol. 2020, 3, 62. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Mukama, O.; Wu, W.; Li, Z.; Habimana, J.D.D.; Zhang, Y.; Zeng, R.; Nie, C.; Zeng, L. A CRISPR/Cas12a Based Universal Lateral Flow Biosensor for the Sensitive and Specific Detection of African Swine-Fever Viruses in Whole Blood. Biosensors 2020, 10, 203. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Xiong, E.; Tian, T.; Cheng, M.; Lin, W.; Wang, H.; Zhang, G.; Sun, J.; Zhou, X. Clustered Regularly Interspaced Short Palindromic Repeats/Cas9-Mediated Lateral Flow Nucleic Acid Assay. ACS Nano 2020, 14, 2497–2508. [Google Scholar] [CrossRef] [PubMed]
- Tian, T.; Qiu, Z.; Jiang, Y.; Zhu, D.; Zhou, X. Exploiting the orthogonal CRISPR-Cas12a/Cas13a trans-cleavage for dual-gene virus detection using a handheld device. Biosens. Bioelectron. 2022, 196, 113701. [Google Scholar] [CrossRef] [PubMed]
- Ki, J.; Na, H.-K.; Yoon, S.W.; Le, V.P.; Lee, T.G.; Lim, E.-K. CRISPR/Cas-Assisted Colorimetric Biosensor for Point-of-Use Testing for African Swine Fever Virus. ACS Sens. 2022, 7, 3940–3946. [Google Scholar] [CrossRef]
- Cao, Y.; Han, D.; Zhang, Y.; Zhang, K.; Du, N.; Tong, W.; Li, G.; Zheng, H.; Liu, C.; Gao, F.; et al. Identification of one novel epitope targeting p54 protein of African swine fever virus using monoclonal antibody and development of a capable ELISA. Res. Vet. Sci. 2021, 141, 19–25. [Google Scholar] [CrossRef]
- Giménez-Lirola, L.G.; Mur, L.; Rivera, B.; Mogler, M.; Sun, Y.; Lizano, S.; Goodell, C.; Harris, D.L.H.; Rowland, R.R.R.; Gallardo, C.; et al. Detection of African Swine Fever Virus Antibodies in Serum and Oral Fluid Specimens Using a Recombinant Protein 30 (p30) Dual Matrix Indirect ELISA. PLoS ONE 2016, 11, e0161230. [Google Scholar] [CrossRef]
- Sastre, P.; Pérez, T.; Costa, S.; Yang, X.; Räber, A.; Blome, S.; Goller, K.V.; Gallardo, C.; Tapia, I.; García, J.; et al. Development of a duplex lateral flow assay for simultaneous detection of antibodies against African and Classical swine fever viruses. J. Vet. Diagn. Investig. 2016, 28, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Caixia, W.; Songyin, Q.; Ying, X.; Haoyang, Y.; Haoxuan, L.; Shaoqiang, W.; Chunyan, F.; Xiangmei, L. Development of a Blocking ELISA Kit for Detection of ASFV Antibody Based on a Monoclonal Antibody Against Full-Length p72. J. AOAC Int. 2022, 105, qsac050. [Google Scholar] [CrossRef] [PubMed]
- Aira, C.; Ruiz, T.; Dixon, L.; Blome, S.; Rueda, P.; Sastre, P. Bead-Based Multiplex Assay for the Simultaneous Detection of Antibodies to African Swine Fever Virus and Classical Swine Fever Virus. Front. Vet. Sci. 2019, 6, 306. [Google Scholar] [CrossRef] [PubMed]
- Rowlands, R.J.; Duarte, M.M.; Boinas, F.; Hutchings, G.; Dixon, L.K. The CD2v protein enhances African swine fever virus replication in the tick vector, Ornithodoros erraticus. Virology 2009, 393, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Chaulagain, S.; Delhon, G.A.; Khatiwada, S.; Rock, D.L. African Swine Fever Virus CD2v Protein Induces β-Interferon Expression and Apoptosis in Swine Peripheral Blood Mononuclear Cells. Viruses 2021, 13, 1480. [Google Scholar] [CrossRef] [PubMed]
- Malogolovkin, A.; Sereda, A. African Swine Fever Virus: African swine fever virus Hemadsorption Inhibition Assay. In African Swine Fever Virus: Methods and Protocols; Netherton, C.L., Ed.; Springer: New York, NY, USA, 2022; pp. 159–167. [Google Scholar]
- Lv, C.; Zhao, Y.; Jiang, L.; Zhao, L.; Wu, C.; Hui, X.; Hu, X.; Shao, Z.; Xia, X.; Sun, X.; et al. Development of a Dual ELISA for the Detection of CD2v-Unexpressed Lower-Virulence Mutational ASFV. Life 2021, 11, 1214. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; He, P.; Meng, F.; Jiang, M.; Xiong, J.; Li, J.; Yu, J.; Wei, H. A Semiautomated Luciferase Immunoprecipitation Assay for Rapid and Easy Detection of African Swine Fever Virus Antibody. J. Clin. Microbiol. 2021, 59, e00990-21. [Google Scholar] [CrossRef]
- Chen, D.; Wang, D.; Wang, C.; Wei, F.; Zhao, H.; Lin, X.; Wu, S. Application of an AlphaLISA method for rapid sensitive detection of African swine fever virus in porcine serum. Appl. Microbiol. Biotechnol. 2021, 105, 4751–4759. [Google Scholar] [CrossRef]
- Chen, C.; Lai, H.; Liang, H.; He, Y.; Guo, G.; Li, L. A New Method for Detection African Swine Fever Virus: Time-resolved Fluorescence Immunoassay. J. Fluoresc. 2021, 31, 1291–1296. [Google Scholar] [CrossRef]
- Onyilagha, C.; Nguyen, K.; Luka, P.D.; Hussaini, U.; Adedeji, A.; Odoom, T.; Ambagala, A. Evaluation of a Lateral Flow Assay for Rapid Detection of African Swine Fever Virus in Multiple Sample Types. Pathogens 2022, 11, 138. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, X.; Wu, X.; Ren, W.; Zou, Y.; Xia, X.; Sun, H. A colloidal gold test strip assay for the detection of African swine fever virus based on two monoclonal antibodies against P30. Arch. Virol. 2021, 166, 871–879. [Google Scholar] [CrossRef] [PubMed]
- Wan, Y.; Shi, Z.; Peng, G.; Wang, L.; Luo, J.; Ru, Y.; Zhou, G.; Ma, Y.; Song, R.; Yang, B.; et al. Development and application of a colloidal-gold dual immunochromatography strip for detecting African swine fever virus antibodies. Appl. Microbiol. Biotechnol. 2022, 106, 799–810. [Google Scholar] [CrossRef] [PubMed]
- Prados, F.J.; Viñuela, E.; Alcamí, A. Sequence and characterization of the major early phosphoprotein p32 of African swine fever virus. J. Virol. 1993, 67, 2475–2485. [Google Scholar] [CrossRef] [PubMed]
- Niu, Y.; Zhang, G.; Zhou, J.; Liu, H.; Chen, Y.; Ding, P.; Qi, Y.; Liang, C.; Zhu, X.; Wang, A. Differential diagnosis of the infection caused by wild-type or CD2v-deleted ASFV strains by quantum dots-based immunochromatographic assay. Lett. Appl. Microbiol. 2022, 74, 1001–1007. [Google Scholar] [CrossRef] [PubMed]
- Luskin, M.S.; Moore, J.H.; Mendes, C.P.; Nasardin, M.B.; Onuma, M.; Davies, S.J. The mass mortality of Asia’s native pigs induced by African swine fever. Wildl. Lett. 2023, 1, 8–14. [Google Scholar] [CrossRef]
- You, S.; Liu, T.; Zhang, M.; Zhao, X.; Dong, Y.; Wu, B.; Wang, Y.; Li, J.; Wei, X.; Shi, B. African swine fever outbreaks in China led to gross domestic product and economic losses. Nat. Food 2021, 2, 802–808. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Lim, E.K.; Park, G.; Park, C.; Lim, J.W.; Lee, H.; Na, W.; Yeom, M.; Kim, J.; Song, D. Advanced Nanomaterials for Preparedness Against (Re-) Emerging Viral Diseases. Adv. Mater. 2021, 33, 2005927. [Google Scholar] [CrossRef]
| Technique | Device | Target Analyte | LOD | Time | Ref |
|---|---|---|---|---|---|
| PCR | Real-time PCR with portable thermocycler | P54 (E183L) | Comparable to laboratory real-time PCR | 2 h | [115] |
| Portable iiPCR | P72 (B646L) | Comparable to real-time PCR | 1.5 h | [116] | |
| iiPCR, POCKITTM Micro Duo | AP endonuclease (E296R) | 20 copies/μL | 40 min | [117] | |
| Isothermal amplification | LAMP-colorimetric | P10 (A78R) | 30 copies/μL | 1 h | [131] |
| LAMP-colorimetric | P72 (B646L) | 10 copies/reaction | 45 min | [132] | |
| LAMP-colorimetric | Topoisomerase II gene (P1192R) | 1 HAD50/mL in viral genomic DNA 10 HAD50/ mL in serum samples | 30 min | [133] | |
| RPA | B646L gene | 3.5 copies/μL | 7 min | [134] | |
| Real-time RPA | P30 (CP204L) | 5 × 101 copies/reaction | 6 min | [135] | |
| RPA and RAA | P72 (B646L) | 93.4 and 53.6 copies/reaction | 16 min | [136] | |
| RPA-LFA | P72 (B646L) | 150 copies/reaction | 10 min | [137] | |
| RPA-LFD | K205R gene | 1 × 102 copies/reaction | 30 min | [138] | |
| RAA-QD-LFA | P72 (B646L) | 100 copies/g for DNA extracts | 25 min | [139] | |
| CRISPR | CRISPR/Cas12a-LAMP-Fluorescent | P72 (B646L) | 1 copies/μL | 50 min | [142] |
| CRISPR/Cas12a-RPA-Fluorescent | P72 (B646L) | 2 copies/reaction | 30–40 min | [143] | |
| CRISPR/Cas12a-LAMP-Fluorescent | P72 (B646L) | 2 copies/μL reaction | 1 h | [144] | |
| CRISPR/Cas12a-RPA-LFA | PP220 polyprotein (CP2475L) | 200 copies of viral genome | 90–100 min | [146] | |
| CRISPR/Cas12a- Fluorescenct | P72 (B646L) | 100 fM (5.7 × 107 copies/mL) | 2 h | [147] | |
| CRISPR/Cas12a-LFA | P72 (B646L) | 20 copies/reaction | 1 h | [148] | |
| LFA | PenCheck® LFA kit | P30 (CP204L) | 107.80 TCID50/mL | 25 min | [165] |
| Colloidal gold-LFA | P30 (CP204L) | 2.16 ng of P30 | 5–7 min | [166] | |
| Colloidal-gold dual immunochromatography strip | P30 (CP204L) and P72 (B646L) Ab | Equivalent to commercial ELISA kits (1:256 dilution to positive sample) | 5–10 min | [167] | |
| QDs-based fluorescent LFA | CD2v (EP402R) Ab | 1:5.12 × 105 dilution to positive serum | 20 min | [169] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, J.-W.; Vu, T.T.H.; Le, V.P.; Yeom, M.; Song, D.; Jeong, D.G.; Park, S.-K. Advanced Strategies for Developing Vaccines and Diagnostic Tools for African Swine Fever. Viruses 2023, 15, 2169. https://doi.org/10.3390/v15112169
Lim J-W, Vu TTH, Le VP, Yeom M, Song D, Jeong DG, Park S-K. Advanced Strategies for Developing Vaccines and Diagnostic Tools for African Swine Fever. Viruses. 2023; 15(11):2169. https://doi.org/10.3390/v15112169
Chicago/Turabian StyleLim, Jong-Woo, Thi Thu Hang Vu, Van Phan Le, Minjoo Yeom, Daesub Song, Dae Gwin Jeong, and Song-Kyu Park. 2023. "Advanced Strategies for Developing Vaccines and Diagnostic Tools for African Swine Fever" Viruses 15, no. 11: 2169. https://doi.org/10.3390/v15112169
APA StyleLim, J.-W., Vu, T. T. H., Le, V. P., Yeom, M., Song, D., Jeong, D. G., & Park, S.-K. (2023). Advanced Strategies for Developing Vaccines and Diagnostic Tools for African Swine Fever. Viruses, 15(11), 2169. https://doi.org/10.3390/v15112169








