Prediction of Survival by IL-6 in a Randomized Placebo-Controlled Trial of Anakinra in COVID-19 Cytokine Storm
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Randomization and Masking
2.3. Data Collection and Outcomes
2.4. Statistical Analysis
3. Results
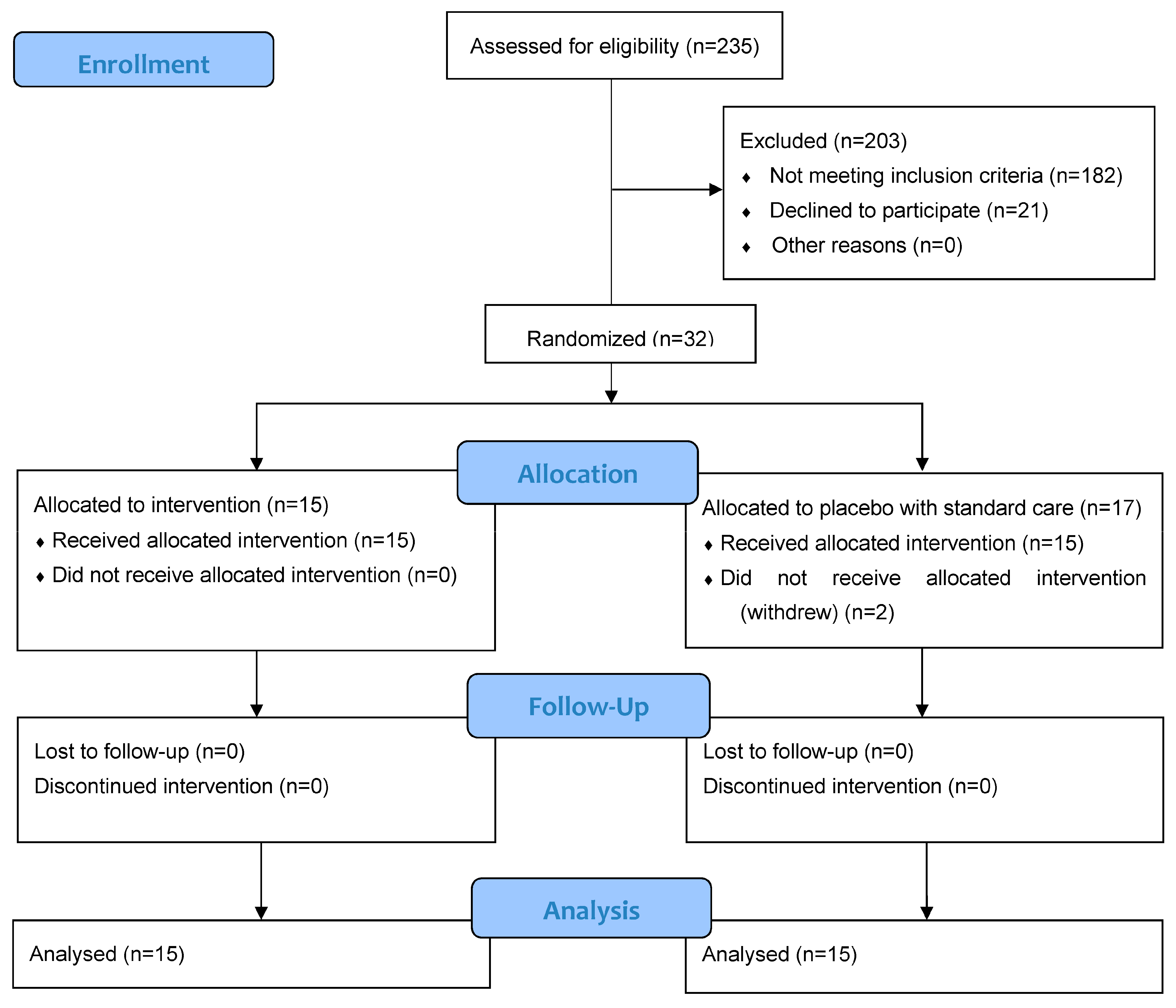
3.1. Patients
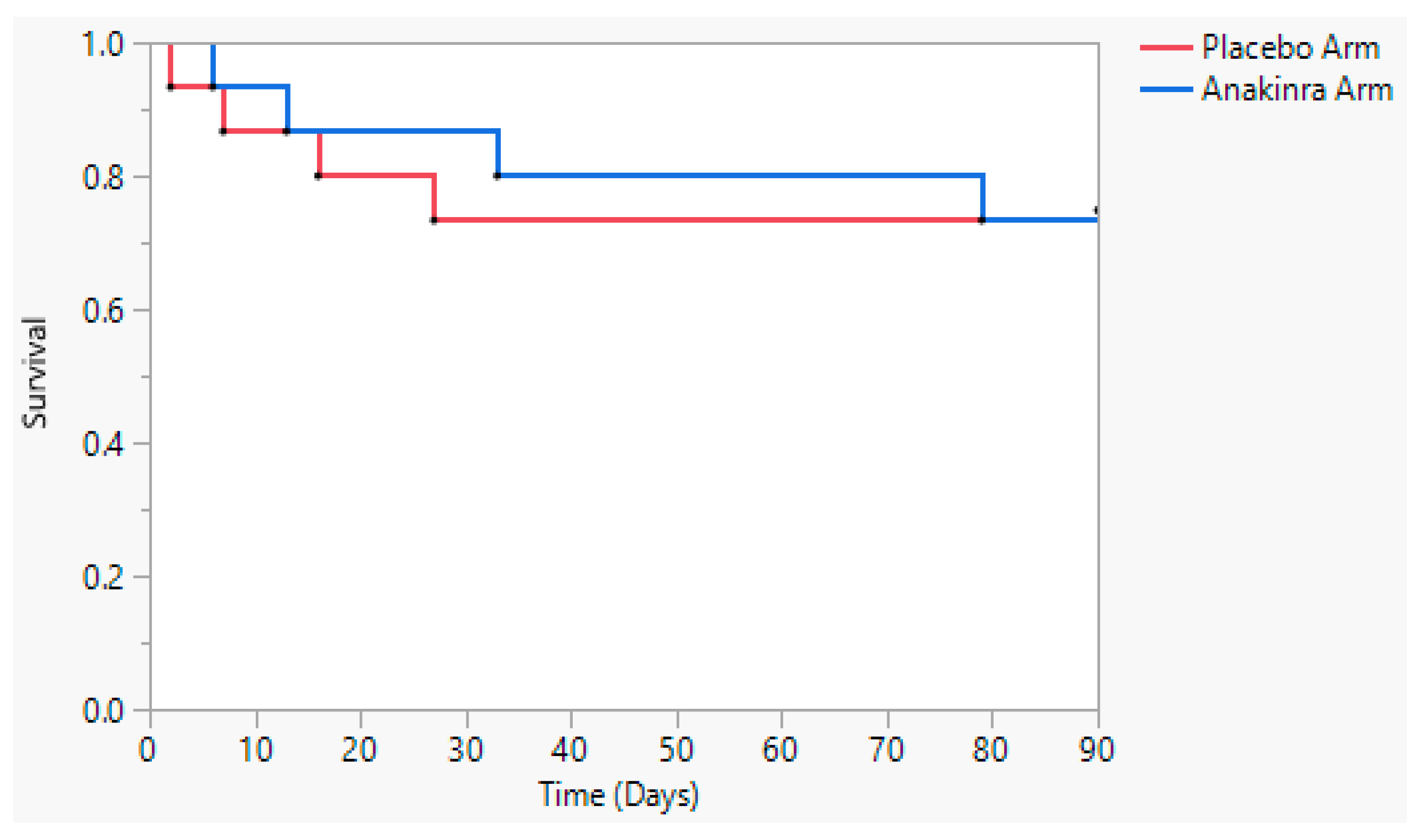
3.2. Primary Outcome
3.3. Secondary Outcomes and Exploratory Outcomes
3.4. Safety
4. Discussion
Key Messages
- In our small single-site, randomized, double-blind, placebo-controlled clinical trial that enrolled 32 participants, anakinra added to dexamethasone did not significantly impact survival in COVID-19 pneumonia CSS patients;
- The serum levels of IL-6 were significantly higher in patients who did not survive compared to patients who did survive;
- The treatment with anakinra was associated with decreases in CXCL9 levels;
- Additional studies are needed to assess the efficacy, timing, dosing, and duration of anakinra treatment in select COVID-19 CSS patients.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- Henderson, L.A.; Canna, S.W.; Schulert, G.S.; Volpi, S.; Lee, P.Y.; Kernan, K.F.; Caricchio, R.; Mahmud, S.; Hazen, M.M.; Halyabar, O.; et al. On the Alert for Cytokine Storm: Immunopathology in COVID-19. Arthritis Rheumatol. 2020, 72, 1059–1063. [Google Scholar] [CrossRef] [PubMed]
- Cron, R.Q. COVID-19 cytokine storm: Targeting the appropriate cytokine. Lancet Rheumatol. 2021, 3, e236–e237. [Google Scholar] [CrossRef] [PubMed]
- Eloseily, E.M.; Weiser, P.; Crayne, C.B.; Haines, H.; Mannion, M.L.; Stoll, M.L.; Beukelman, T.; Atkinson, T.P.; Cron, R.Q. Benefit of Anakinra in Treating Pediatric Secondary Hemophagocytic Lymphohistiocytosis. Arthritis Rheumatol. 2020, 72, 326–334. [Google Scholar] [CrossRef]
- Shakoory, B.; Carcillo, J.A.; Chatham, W.W.; Amdur, R.L.; Zhao, H.; Dinarello, C.A.; Cron, R.Q.; Opal, S.M. Interleukin-1 Receptor Blockade Is Associated With Reduced Mortality in Sepsis Patients With Features of Macrophage Activation Syndrome: Reanalysis of a Prior Phase III Trial. Crit. Care Med. 2016, 44, 275–281. [Google Scholar] [CrossRef]
- Barkas, F.; Ntekouan, S.F.; Kosmidou, M.; Liberopoulos, E.; Liontos, A.; Milionis, H. Anakinra in hospitalized non-intubated patients with coronavirus disease 2019: A systematic review and meta-analysis. Rheumatology 2021, 60, 5527–5537. [Google Scholar] [CrossRef]
- Geng, J.; Wang, F.; Huang, Z.; Chen, X.; Wang, Y. Perspectives on anti-IL-1 inhibitors as potential therapeutic interventions for severe COVID-19. Cytokine 2021, 143, 155544. [Google Scholar] [CrossRef]
- Cavalli, G.; De Luca, G.; Campochiaro, C.; Della-Torre, E.; Ripa, M.; Canetti, D.; Oltolini, C.; Castiglioni, B.; Tassan Din, C.; Boffini, N.; et al. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: A retrospective cohort study. Lancet Rheumatol. 2020, 2, e325–e331. [Google Scholar] [CrossRef]
- Huet, T.; Beaussier, H.; Voisin, O.; Jouveshomme, S.; Dauriat, G.; Lazareth, I.; Sacco, E.; Naccache, J.M.; Bezie, Y.; Laplanche, S.; et al. Anakinra for severe forms of COVID-19: A cohort study. Lancet Rheumatol. 2020, 2, e393–e400. [Google Scholar] [CrossRef]
- Aouba, A.; Baldolli, A.; Geffray, L.; Verdon, R.; Bergot, E.; Martin-Silva, N.; Justet, A. Targeting the inflammatory cascade with anakinra in moderate to severe COVID-19 pneumonia: Case series. Ann. Rheum. Dis. 2020, 79, 1381–1382. [Google Scholar] [CrossRef] [PubMed]
- Langer-Gould, A.; Smith, J.B.; Gonzales, E.G.; Castillo, R.D.; Figueroa, J.G.; Ramanathan, A.; Li, B.H.; Gould, M.K. Early identification of COVID-19 cytokine storm and treatment with anakinra or tocilizumab. Int. J. Infect. Dis. 2020, 99, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Cauchois, R.; Koubi, M.; Delarbre, D.; Manet, C.; Carvelli, J.; Blasco, V.B.; Jean, R.; Fouche, L.; Bornet, C.; Pauly, V.; et al. Early IL-1 receptor blockade in severe inflammatory respiratory failure complicating COVID-19. Proc. Natl. Acad. Sci. USA 2020, 117, 18951–18953. [Google Scholar] [CrossRef] [PubMed]
- Bozzi, G.; Mangioni, D.; Minoia, F.; Aliberti, S.; Grasselli, G.; Barbetta, L.; Castelli, V.; Palomba, E.; Alagna, L.; Lombardi, A.; et al. Anakinra combined with methylprednisolone in patients with severe COVID-19 pneumonia and hyperinflammation: An observational cohort study. J. Allergy Clin. Immunol. 2021, 147, 561–566.e564. [Google Scholar] [CrossRef] [PubMed]
- Franzetti, M.; Forastieri, A.; Borsa, N.; Pandolfo, A.; Molteni, C.; Borghesi, L.; Pontiggia, S.; Evasi, G.; Guiotto, L.; Erba, M.; et al. IL-1 Receptor Antagonist Anakinra in the Treatment of COVID-19 Acute Respiratory Distress Syndrome: A Retrospective, Observational Study. J. Immunol. 2021, 206, 1569–1575. [Google Scholar] [CrossRef]
- Erden, A.; Ozdemir, B.; Karakas, O.; Mutlu, N.M.; Izdes, S.; Kalem, A.K.; Bilir, Y.A.; Aypak, A.; Akinci, E.; Guner, R.; et al. Evaluation of 17 patients with COVID-19 pneumonia treated with anakinra according to HScore, SOFA, MuLBSTA, and Brescia-COVID respiratory severity scale (BCRSS) scoring systems. J. Med. Virol. 2021, 93, 1532–1537. [Google Scholar] [CrossRef]
- Balkhair, A.; Al-Zakwani, I.; Al Busaidi, M.; Al-Khirbash, A.; Al Mubaihsi, S.; BaTaher, H.; Al Aghbari, J.; Al Busaidi, I.; Al Kindi, M.; Baawain, S.; et al. Anakinra in hospitalized patients with severe COVID-19 pneumonia requiring oxygen therapy: Results of a prospective, open-label, interventional study. Int. J. Infect. Dis. 2021, 103, 288–296. [Google Scholar] [CrossRef]
- Kyriazopoulou, E.; Panagopoulos, P.; Metallidis, S.; Dalekos, G.N.; Poulakou, G.; Gatselis, N.; Karakike, E.; Saridaki, M.; Loli, G.; Stefos, A.; et al. An open label trial of anakinra to prevent respiratory failure in COVID-19. Elife 2021, 10, e66125. [Google Scholar] [CrossRef]
- Navarro-Millan, I.; Sattui, S.E.; Lakhanpal, A.; Zisa, D.; Siegel, C.H.; Crow, M.K. Use of Anakinra to Prevent Mechanical Ventilation in Severe COVID-19: A Case Series. Arthritis Rheumatol. 2020, 72, 1990–1997. [Google Scholar] [CrossRef]
- CORIMUNO-19 Collaborative group. Effect of anakinra versus usual care in adults in hospital with COVID-19 and mild-to-moderate pneumonia (CORIMUNO-ANA-1): A randomised controlled trial. Lancet Respir. Med. 2021, 9, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Malik, H.; Bint Abdul Jabbar, H.; Latif, F.; Sarfraz, A.; Sarfraz, Z.; Sarfraz, M. The efficacy of anakinra compared to standard care of treatment for COVID-19: A meta-analysis. Turk. J. Med. Sci. 2022, 52, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Kyriazopoulou, E.; Huet, T.; Cavalli, G.; Gori, A.; Kyprianou, M.; Pickkers, P.; Eugen-Olsen, J.; Clerici, M.; Veas, F.; Chatellier, G.; et al. Effect of anakinra on mortality in patients with COVID-19: A systematic review and patient-level meta-analysis. Lancet Rheumatol. 2021, 3, e690–e697. [Google Scholar] [CrossRef]
- Group, R.C.; Horby, P.; Lim, W.S.; Emberson, J.R.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; et al. Dexamethasone in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef]
- Kyriazopoulou, E.; Poulakou, G.; Milionis, H.; Metallidis, S.; Adamis, G.; Tsiakos, K.; Fragkou, A.; Rapti, A.; Damoulari, C.; Fantoni, M.; et al. Author Correction: Early treatment of COVID-19 with anakinra guided by soluble urokinase plasminogen receptor plasma levels: A double-blind, randomized controlled phase 3 trial. Nat. Med. 2021, 27, 1850. [Google Scholar] [CrossRef] [PubMed]
- De Benedetti, F.; Prencipe, G.; Bracaglia, C.; Marasco, E.; Grom, A.A. Targeting interferon-gamma in hyperinflammation: Opportunities and challenges. Nat. Rev. Rheumatol. 2021, 17, 678–691. [Google Scholar] [CrossRef] [PubMed]
- Ostrowski, S.R.; Katzenstein, T.L.; Pedersen, M.; Hoyer-Hansen, G.; Gerstoft, J.; Pedersen, B.K.; Ullum, H. Plasma levels of intact and cleaved urokinase receptor decrease in HIV-1-infected patients initiating highly active antiretroviral therapy. Scand. J. Immunol. 2006, 63, 478–486. [Google Scholar] [CrossRef]
- Wen, S.; He, F.; Zhu, X.; Yuan, S.; Liu, H.; Sun, L. IFN-gamma, CXCL16, uPAR: Potential biomarkers for systemic lupus erythematosus. Clin. Exp. Rheumatol. 2018, 36, 36–43. [Google Scholar]
- Kharazmi, A.B.; Moradi, O.; Haghighi, M.; Kouchek, M.; Manafi-Rasi, A.; Raoufi, M.; Shoaei, S.D.; Hadavand, F.; Nabavi, M.; Miri, M.M.; et al. A randomized controlled clinical trial on efficacy and safety of anakinra in patients with severe COVID-19. Immun. Inflamm. Dis. 2022, 10, 201–208. [Google Scholar] [CrossRef]
- Cron, R.Q.; Caricchio, R.; Chatham, W.W. Calming the cytokine storm in COVID-19. Nat. Med. 2021, 27, 1674–1675. [Google Scholar] [CrossRef]
- Kelmenson, D.A.; Cron, R.Q. Who, what, and when-effective therapy for severe COVID-19. Lancet Rheumatol. 2022, 4, e2–e3. [Google Scholar] [CrossRef] [PubMed]
| Anakinra Group (N = 15) | Placebo Group (N = 15) | p-Value | |
|---|---|---|---|
| Age, years, mean (SD) | 64.2 (8.2) | 61.8 (12.2) | 0.5 |
| Sex, female, N (%) | 5 (33.3) | 5 (33.3) | 1.0 |
| Race, N (%) | |||
| White | 11 (73.3) | 9 (60.0) | 0.7 |
| Black | 4 (26.7) | 5 (33.3) | |
| Declined/missing | 0 (0) | 1 (6.7) | |
| BMI, mean (SD) | 29.9 (6.8) | 30.5 (3.5) | 0.8 |
| Co-morbidities, N (%) | |||
| Cardiovascular disease | 4 (26.7) | 3 (20.0) | 1.0 |
| Diabetes mellitus | 5 (33.3) | 3 (20.0) | 0.7 |
| Hypertension | 11 (73.3) | 10 (66.7) | 1.0 |
| Malignancy | 1 (6.7) | 1 (6.7) | 1.0 |
| Current or former smoker, N (%) | 6 (40.0) | 5 (33.3) | 1.0 |
| Anakinra Group (N = 15) | Placebo Group (N = 15) | p-Value | |
|---|---|---|---|
| Clinical inclusion parameters at enrollment, N (%) | |||
| Elevated D-dimer (>500 ng/mL) | 10 (66.7) | 11 (73.3) | 1.0 |
| Thrombocytopenia (<130 × 103/mm3) | 2 (13.3) | 1 (6.7) | 1.0 |
| Leukopenia (WBC < 3.5 × 103/mm3) or lymphopenia (<1 × 103/mm3) | 10 (66.7) | 13 (86.7) | 0.4 |
| Elevated AST or ALT (>2X ULN) | 5 (33.3) | 2 (13.3) | 0.4 |
| Elevated LDH (>2X ULN) | 7 (46.7) | 3 (20.0) | 0.2 |
| CRP > 100 mg/L | 10 (66.7) | 11 (73.3) | 1.0 |
| Other medications at enrollment, N (%) | |||
| Dexamethasone | 15 (100.0) | 15 (100.0) | N/A |
| Azithromycin | 10 (66.67) | 8 (53.33) | 0.7 |
| Remdesivir | 12 (80.0) | 14 (93.3) | 0.6 |
| β-lactams | 13 (86.7) | 10 (66.7) | 0.4 |
| Therapeutic anticoagulation at baseline | 3 (20.0) | 0 (0.0) | 0.2 |
| Prophylactic anticoagulation at enrollment | 12 (80.0) | 15 (100.00) | 0.2 |
| Pulmonary compromise at enrollment * | 9 (60.0) | 7 (46.7) | 0.7 |
| MICU patient at enrollment | 4 (26.7) | 4 (26.7) | 1.0 |
| Laboratory values at enrollment, mean (SD) | |||
| CRP, mg/L (normal < 10.9) | 130.1 (62.3) | 180.8 (113.0) | 0.1 |
| Ferritin, ng/mL (normal < 336.2) | 1344.1 (711.2) | 1922.4 (2304.3) | 0.4 |
| LDH, IU/L (normal 120–240) | 480.7 (211.3) | 414.1 (152.5) | 0.3 |
| D-dimer, ng/mL | 1262 (1863.9) | 2080.7 (3712.2) | 0.5 |
| WBC, ×103/mm3 (normal 4–11) | 8.2 (3.7) | 11.1 (4.3) | 0.05 |
| Lymphocyte count, ×103/mm3 (normal 1.25–5.8) | 0.83 (0.4) | 0.65 (0.3) | 0.2 |
| Platelet count, ×103/mm3 (normal 150–400) | 273.3 (107.8) | 272.5 (99.1) | 1.0 |
| Fibrinogen, mg/dL | 635.9 (152.1) | 636.9 (178.2) | 1.0 |
| INR | 1.2 (0.2) | 1.1 (0.1) | 0.2 |
| Triglyceride level, mg/dL (normal 40–150) | 131.3 (46.4) | 165.6 (79.0) | 0.2 |
| AST, IU/L (normal 12–39) | 54 (23.4) | 44.3 (41.2) | 0.4 |
| ALT, IU/L (normal 7–52) | 71.6 (54.6) | 54.0 (73.4) | 0.5 |
| Creatinine, mg/dL (normal 0.7–1.3) | 1.1 (0.9) | 1.0 (0.5) | 0.7 |
| Anakinra Group (N = 15) | Placebo Group (N = 15) | p-Value | |
|---|---|---|---|
| Primary Outcomes | |||
| Survived hospitalization | 11 (73.3) | 11 (73.3) | 1.0 |
| Did not require mechanical ventilation | 10 (66.7) | 10 (66.7) | 1.0 |
| Secondary Outcomes | |||
| Did not require escalation of oxygen support after Day 2, N = 30 | 8 (53.3) | 9 (60.0) | 0.7 |
| 25% improvement in CRP and ferritin by Day 2, N = 29 | 6 (40.0) | 8 (57.1) | 0.4 |
| 75% improvement from Day 0 CRP and ferritin elevations by Day 10, N = 26 * | 6 (46.15) | 7 (53.9) | 0.7 |
| 75% improvement from Day 0 LDH and D-dimer elevations by Day 10, N = 26 * | 0 (0.0) | 7 (53.9) | 0.005 |
| Requiring no more than 2 L/min NC of oxygen support to maintain oxygen saturation ≥93% by Day 10, N = 27 | 8 (57.1) | 9 (69.2) | 0.7 |
| Able to maintain oxygen saturation ≥93% on RA by Day 10, N = 27 | 4 (28.6) | 9 (69.2) | 0.06 |
| Culture-positive infections, any | 4 (26.7) | 2 (13.3) | 0.7 |
| Bacteremia/fungemia | 1 (6.7) | 0 (0.0) | 1.0 |
| Colonization | 3 (20.0) | 2 (13.3) | 1.0 |
| Day 0 Levels | Day 10 Levels * | ||||||
|---|---|---|---|---|---|---|---|
| Cytokine | Reference ULN | Anakinra Group | Placebo Group | p-Value | Anakinra Group | Placebo Group | p-Value |
| sCD163 | <1785 | 1384.8 ± 181.8 | 1382.9 ± 181.2 | 1.0 | 1464.5 ± 209.9 | 1285.0 ± 176.2 | 0.5 |
| sCD25 | <858 | 1295.7 ± 192.1 | 1465.9 ± 168.0 | 0.5 | 1578.9 ± 517.4 | 916.5 ± 113.8 | 0.2 |
| IL-12 | <1.9 | 2.0 ± 0.1 | 1.9 ± 0.0 | 0.3 | 4.0 ± 2.1 | 1.90 ± 0.0 | 0.3 |
| IFN-γ | <4.2 | 4.2 ± 0.0 | 4.2 ± 0.0 | 1.0 | 4.2 ± 0.0 | 4.2 ± 0.0 | 0.3 |
| IL-4 | <2.2 | 2.2 ± 0.0 | 2.2 ± 0.0 | 1.0 | 2.2 ± 0.0 | 2.2 ± 0 | 1.0 |
| IL-5 | <2.1 | 2.3 ±0.2 | 2.1 ± 0 | 0.2 | 3.7 ± 1.4 | 2.2 ± 0.1 | 0.3 |
| IL-10 | <2.8 | 17.4 ± 3.9 | 9.5 ± 1.2 | 0.07 | 15.9 ± 7.2 | 9.9 ± 5.0 | 0.5 |
| IL-13 | <2.3 | 2.5 ± 0.7 | 3.0 ± 0.9 | 0.7 | 3.8 ± 1.4 | 4.2 ± 1.6 | 0.9 |
| IL-1β | <6.7 | 7.1 ± 0.6 | 6.5 ± 0.0 | 0.3 | 6.6 ± 0.1 | 7.2 ± 0.7 | 0.4 |
| IL-6 | <2.0 | 5.3 ± 0.9 | 12.6 ± 6.7 | 0.3 | 14.6 ± 6.8 | 16.2 ± 11.0 | 0.9 |
| IL-8 | <30 | 3.0 ± 0.0 | 3.0 ± 0.0 | 1.0 | 4.6 ± 1.6 | 3.6 ± 0.6 | 0.5 |
| TNF | <7.2 | 3.6 ±0.6 | 3.0 ± 0.8 | 0.5 | 8.3 ± 5.0 | 2.2 ± 0.3 | 0.3 |
| IL-2 | <2.1 | 2.1 ± 0.0 | 2.1± 0.0 | 1.0 | 2.6 ± 0.5 | 2.10 ± 0.0 | 0.3 |
| IL-17 | <1.4 | 1.4 ± 0.0 | 1.4 ± 0.0 | 0.8 | 5.9 ± 3.1 | 1.4 ± 0.0 | 0.2 |
| IL-18 | <540 | 1011.9 ± 121.1 | 825.3 ± 139.3 | 0.3 | Unavailable | Unavailable | - |
| CXCL9 | <121 | 465.9 ± 100.1 | 200.0 ± 42.0 | 0.03 | 169.0 ± 29.6 | 143.8 ± 27.3 | 0.6 |
| Anakinra Group (N = 15) | Placebo Group (N = 15) | p-Value | |
|---|---|---|---|
| Serious adverse events | |||
| Acute respiratory distress syndrome | 9 (60.0) | 7 (46.7) | 0.5 |
| Arterial ischemia | 4 (26.7) | 5 (33.3) | 0.7 |
| Sudden cardio-respiratory arrest | 4 (26.7) | 4 (26.7) | 1.0 |
| Other Adverse Events of Interest | |||
| Pulmonary embolism or deep venous thrombosis | 4 (26.7) | 3 (20.0) | 0.7 |
| Acute renal failure | 7 (46.7) | 6 (40.0) | 0.7 |
| Neutropenia | 1 (6.7) | 0 (0.0) | 0.3 |
| Anemia | 14 (93.3) | 13 (86.7) | 0.5 |
| Thrombocytopenia | 5 (33.3) | 5 (33.3) | 1.0 |
| Gastrointestinal bleeding | 1 (6.7) | 0 (0.0) | 0.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jackson, L.E.; Khullar, N.; Beukelman, T.; Chapleau, C.; Kamath, A.; Cron, R.Q.; Chatham, W.W. Prediction of Survival by IL-6 in a Randomized Placebo-Controlled Trial of Anakinra in COVID-19 Cytokine Storm. Viruses 2023, 15, 2036. https://doi.org/10.3390/v15102036
Jackson LE, Khullar N, Beukelman T, Chapleau C, Kamath A, Cron RQ, Chatham WW. Prediction of Survival by IL-6 in a Randomized Placebo-Controlled Trial of Anakinra in COVID-19 Cytokine Storm. Viruses. 2023; 15(10):2036. https://doi.org/10.3390/v15102036
Chicago/Turabian StyleJackson, Lesley E., Nitasha Khullar, Timothy Beukelman, Chris Chapleau, Abhishek Kamath, Randy Q. Cron, and Walter Winn Chatham. 2023. "Prediction of Survival by IL-6 in a Randomized Placebo-Controlled Trial of Anakinra in COVID-19 Cytokine Storm" Viruses 15, no. 10: 2036. https://doi.org/10.3390/v15102036
APA StyleJackson, L. E., Khullar, N., Beukelman, T., Chapleau, C., Kamath, A., Cron, R. Q., & Chatham, W. W. (2023). Prediction of Survival by IL-6 in a Randomized Placebo-Controlled Trial of Anakinra in COVID-19 Cytokine Storm. Viruses, 15(10), 2036. https://doi.org/10.3390/v15102036







