Mucin Transiently Sustains Coronavirus Infectivity through Heterogenous Changes in Phase Morphology of Evaporating Aerosol
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Culture Methods
2.2. Virus Propagation and Titration
2.3. Airborne Viral Stability Measurements Using CELEBS
2.4. Bulk Phase Viral Viability Measurements
2.5. Viral Stability Statistics
2.6. Comparative Kinetic Electrodynamic Balance Measurements
2.7. Falling Droplet Column
3. Results
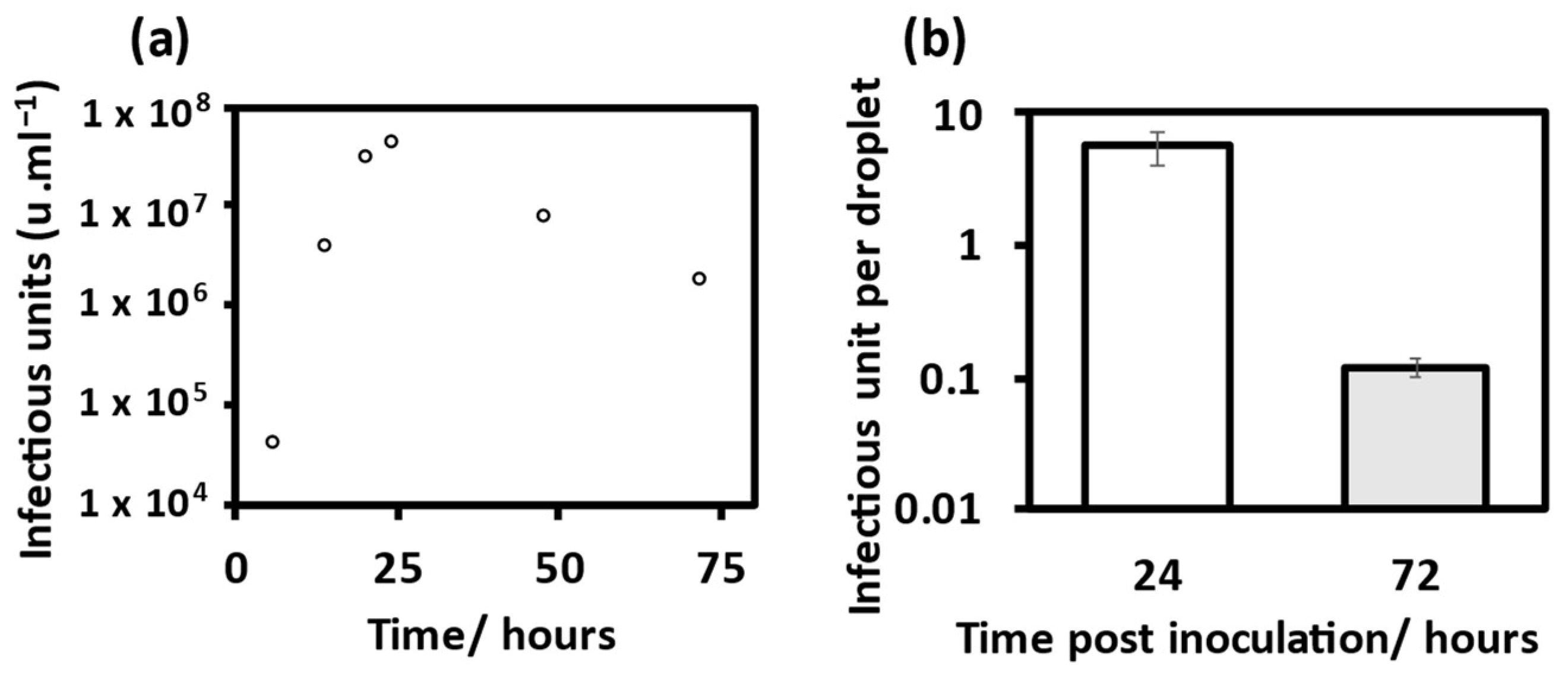
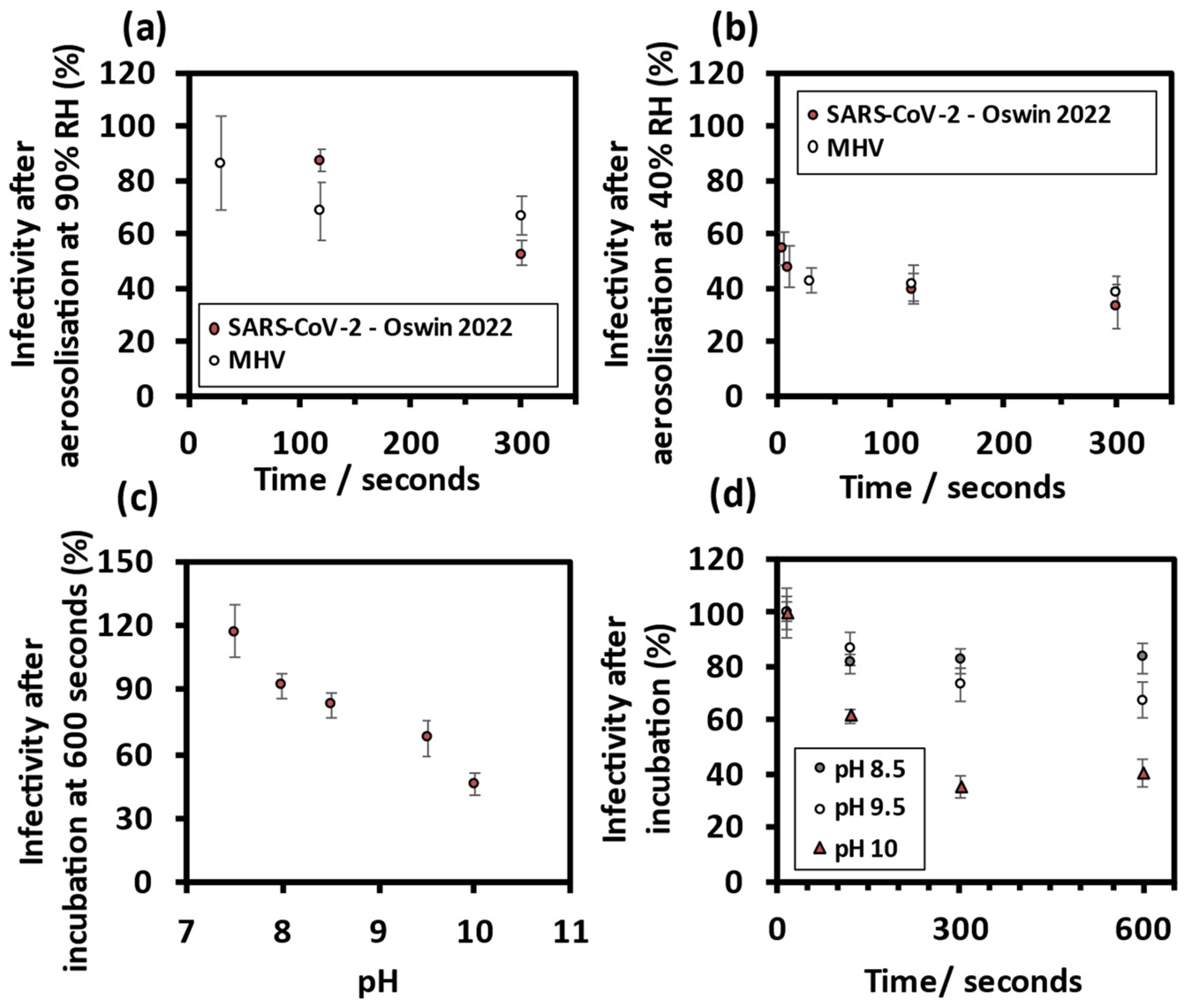
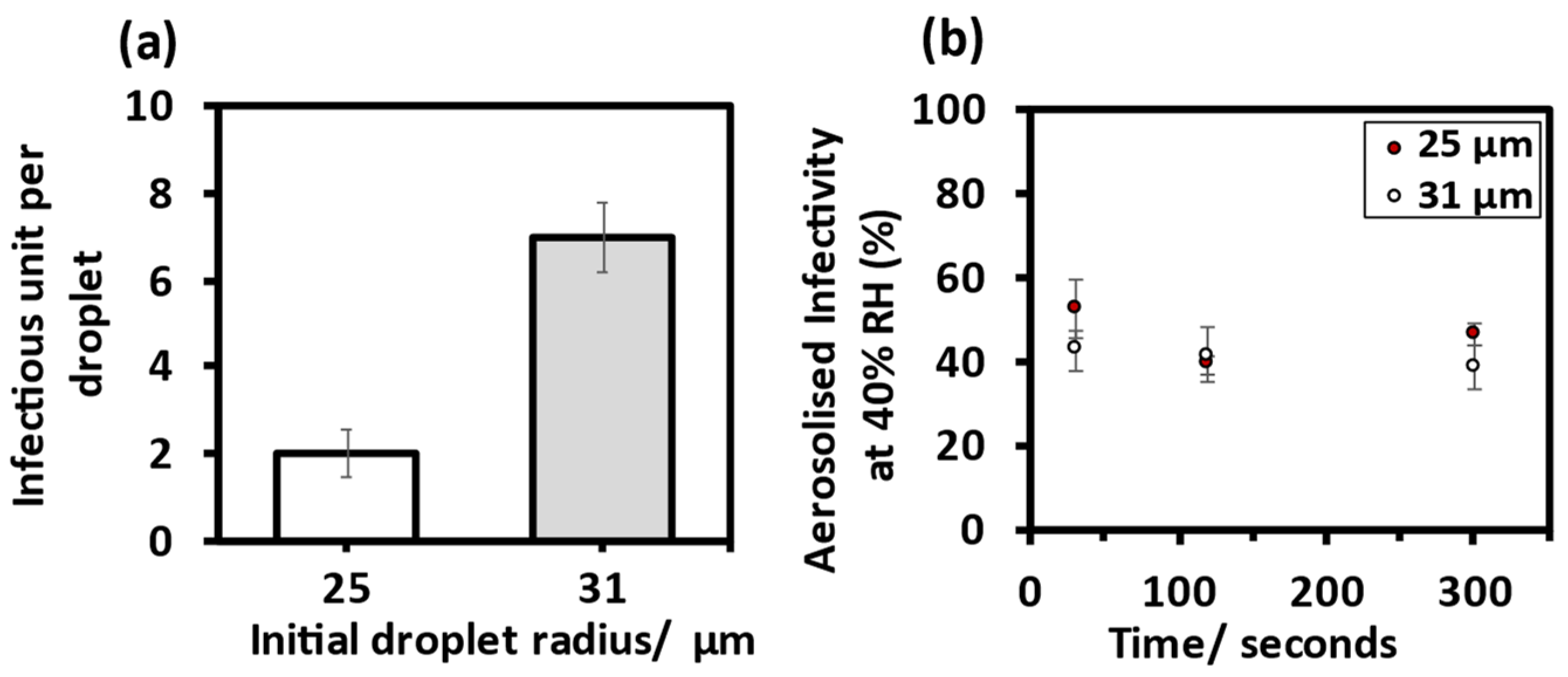
3.1. Viral Infectivity Measurements
3.1.1. MHV Is an Appropriate Surrogate for SARS-CoV-2
3.1.2. Comparing MHV Infectivity in Droplets of Different Size
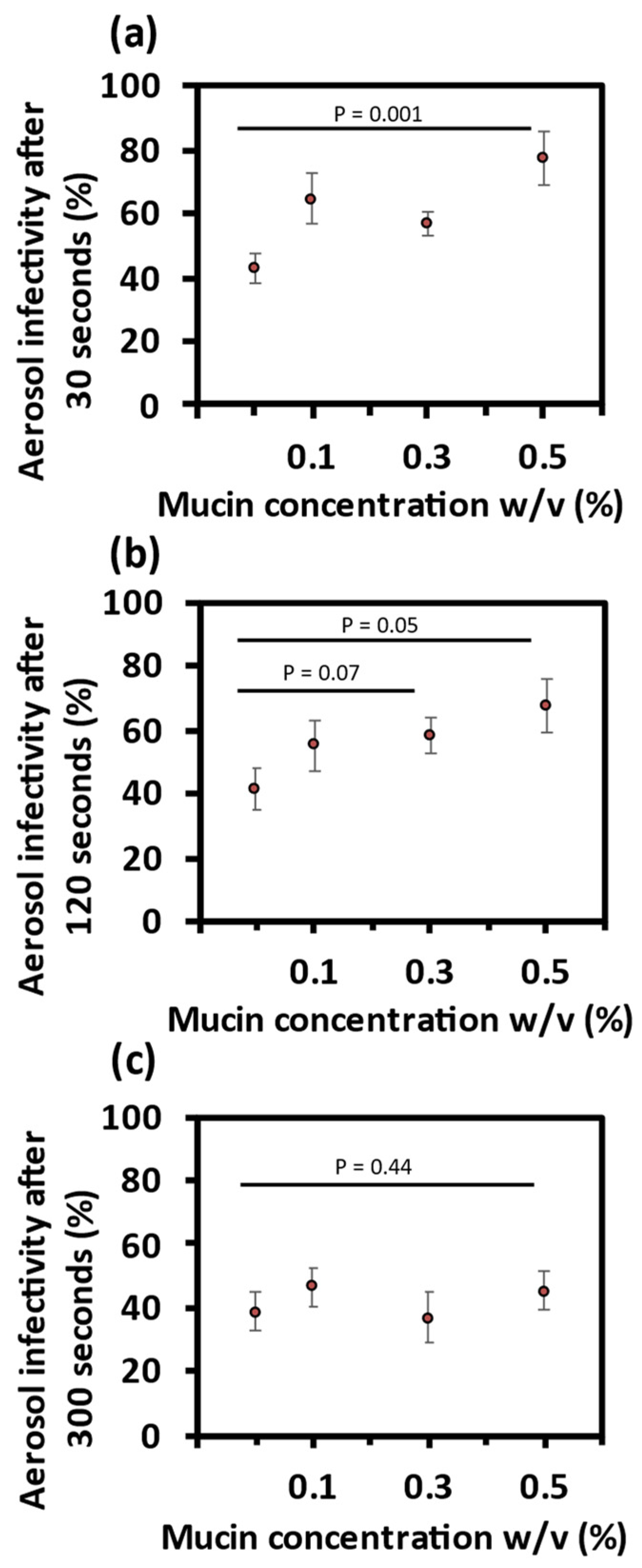
3.1.3. Mucin Sustains Aerosolised MHV Infectivity
3.2. Aerosol Phase Evaporation Dynamics
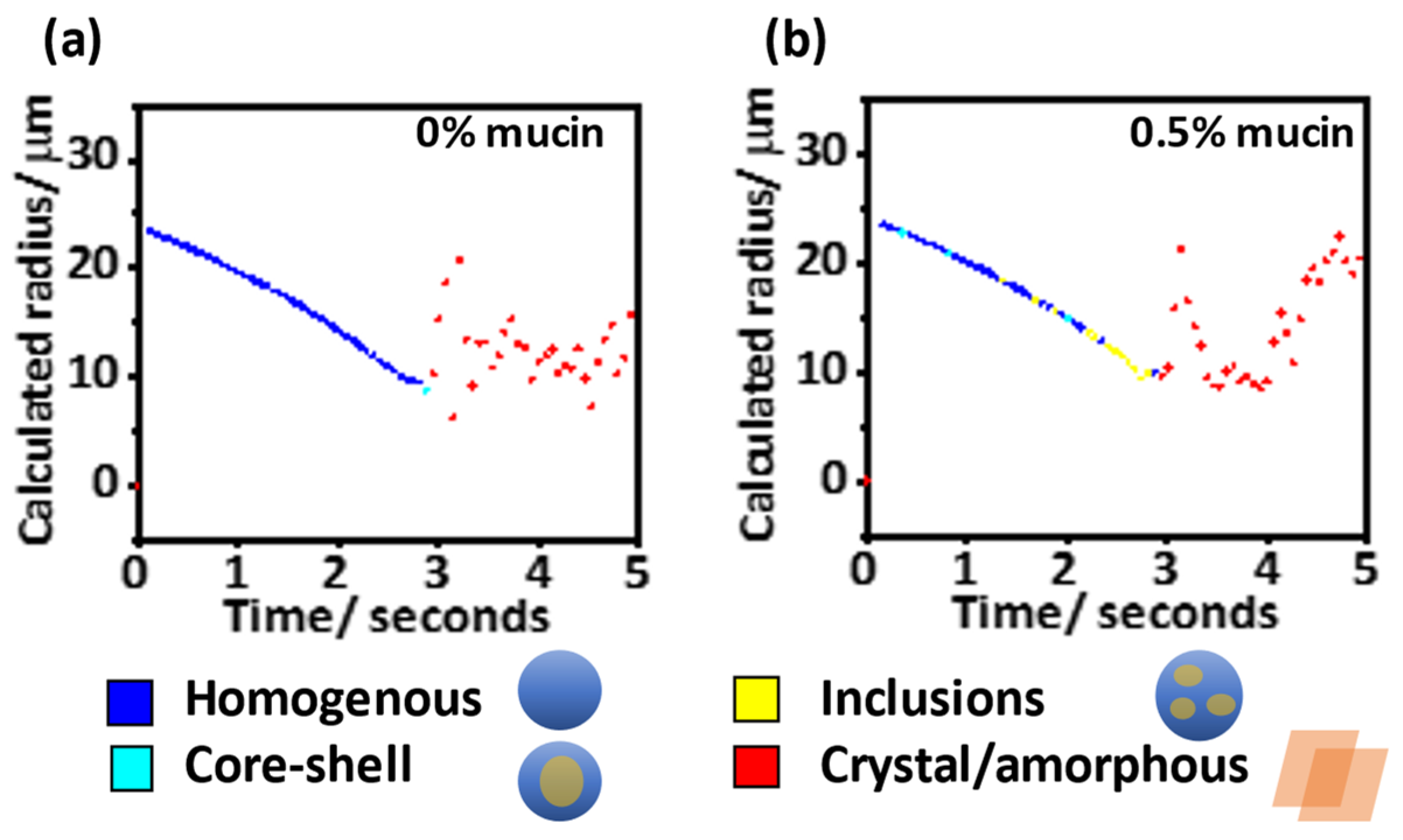
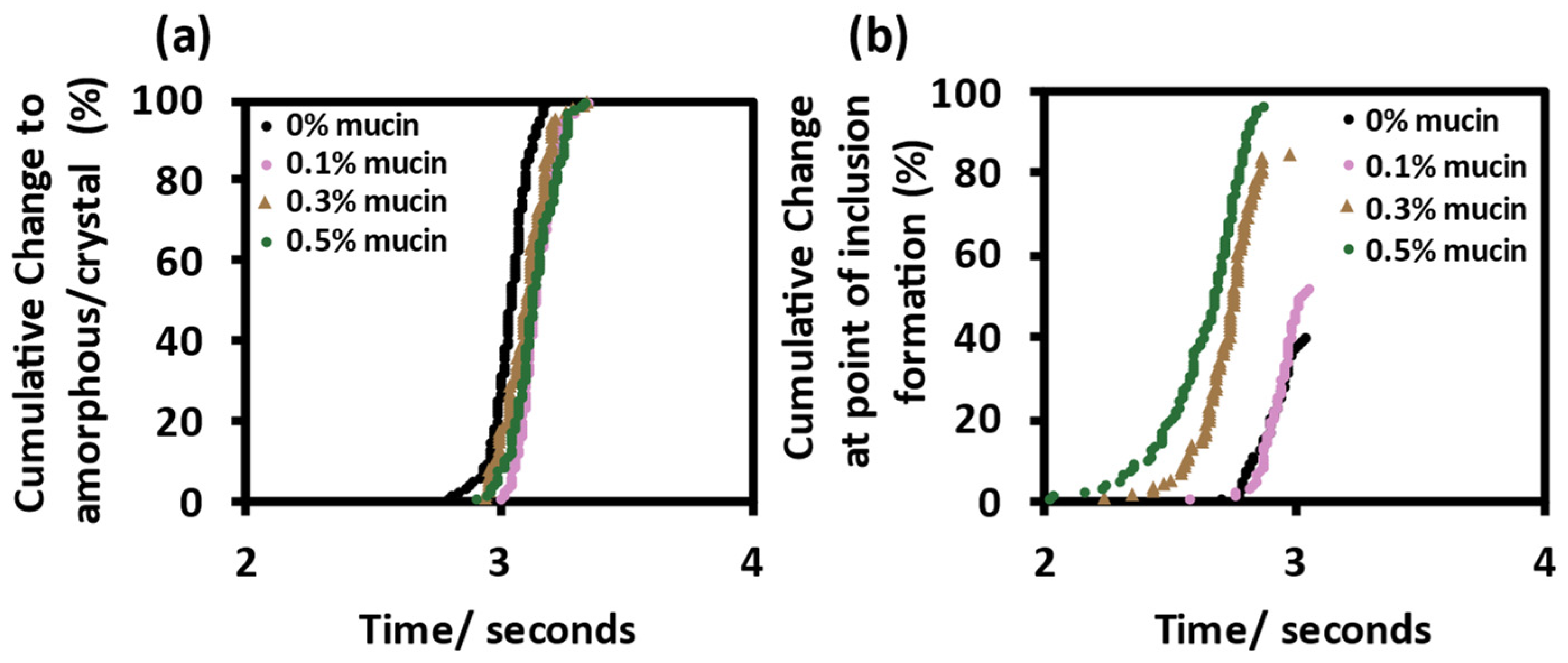
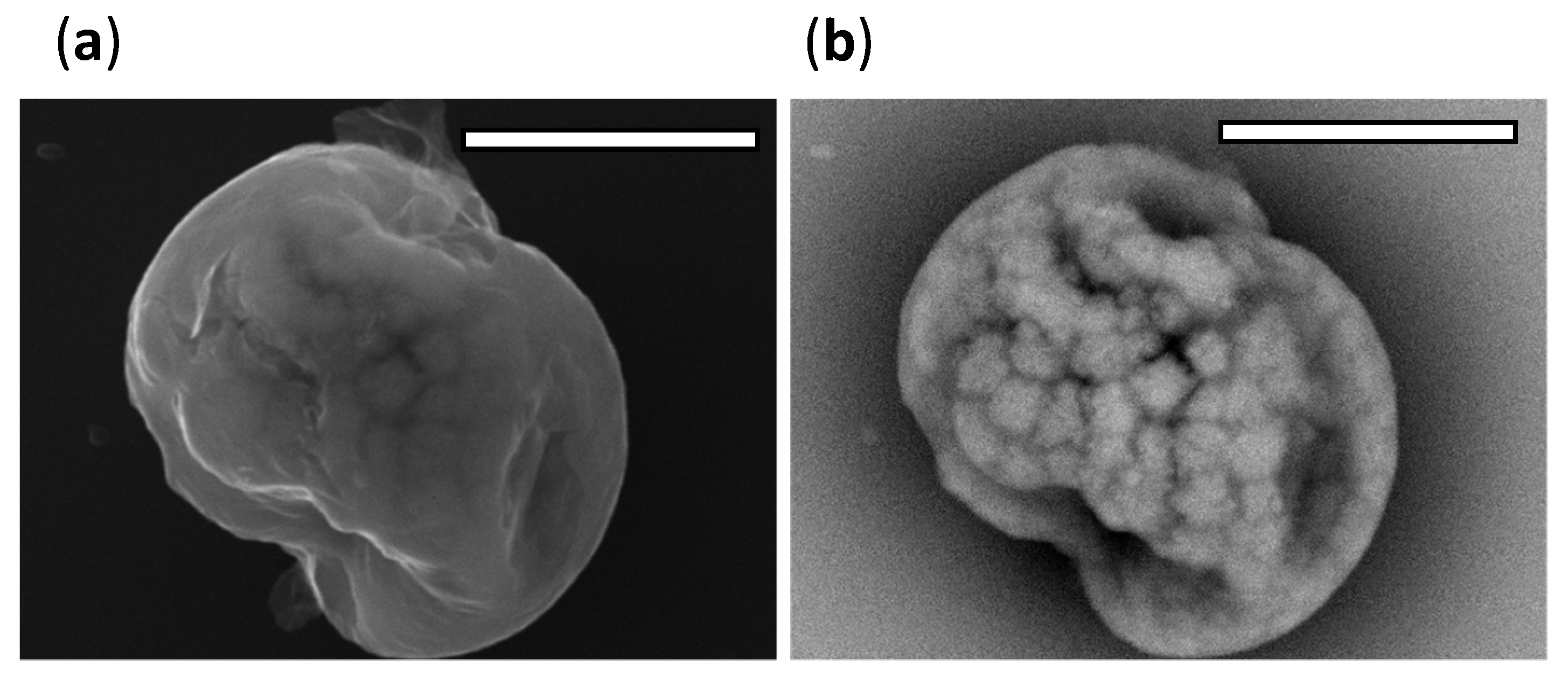
Mucin Promotes Heterogenous Bioaerosol Phase Change
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tang, J.W.; Bahnfleth, W.P.; Bluyssen, P.M.; Buonanno, G.; Jimenez, J.L.; Kurnitski, J.; Li, Y.; Miller, S.; Sekhar, C.; Morawska, L.; et al. Dismantling Myths on the Airborne Transmission of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2). J. Hosp. Infect. 2021, 110, 89–96. [Google Scholar] [CrossRef]
- Port, J.R.; Yinda, C.K.; Owusu, I.O.; Holbrook, M.; Fischer, R.; Bushmaker, T.; Avanzato, V.A.; Schulz, J.E.; Martens, C.; van Doremalen, N.; et al. SARS-CoV-2 Disease Severity and Transmission Efficiency Is Increased for Airborne Compared to Fomite Exposure in Syrian Hamsters. Nat. Commun. 2021, 12, 4985. [Google Scholar] [CrossRef]
- Kutter, J.S.; de Meulder, D.; Bestebroer, T.M.; Lexmond, P.; Mulders, A.; Richard, M.; Fouchier, R.A.M.; Herfst, S. SARS-CoV and SARS-CoV-2 Are Transmitted through the Air between Ferrets over More than One Meter Distance. Nat. Commun. 2021, 12, 1653. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, M.O.; Thomas, R.J.; Oswin, H.; Haddrell, A.E.; Reid, J.P. Transformative Approach to Investigate the Microphysical Factors Influencing Airborne Transmission of Pathogens. Appl. Environ. Microbiol. 2020, 86, e01543-20. [Google Scholar] [CrossRef] [PubMed]
- Oswin, H.; Haddrell, A.; Otero-Fernandez, M.; Cogan, T.; Mann, J.F.S.; Morley, C.; Hill, D.; Davidson, A.D.; Finn, A.; Thomas, R.; et al. Measuring Stability of Virus in Aerosols under Varying Environmental Conditions. Aerosol Sci. Technol. 2021, 55, 1315–1320. [Google Scholar] [CrossRef]
- Walker, J.S.; Archer, J.; Gregson, F.K.A.; Michel, S.E.S.; Bzdek, B.R.; Reid, J.P. Accurate Representations of the Microphysical Processes Occurring during the Transport of Exhaled Aerosols and Droplets. ACS Cent. Sci. 2021, 7, 200–209. [Google Scholar] [CrossRef]
- Niazi, S.; Groth, R.; Cravigan, L.; He, C.; Tang, J.W.; Spann, K.; Johnson, G.R. Susceptibility of an Airborne Common Cold Virus to Relative Humidity. Environ. Sci. Technol. 2021, 55, 499–508. [Google Scholar] [CrossRef]
- Huynh, E.; Olinger, A.; Woolley, D.; Kohli, R.K.; Choczynski, J.M.; Davies, J.F.; Lin, K.; Marr, L.C.; Davis, R.D. Evidence for a Semisolid Phase State of Aerosols and Droplets Relevant to the Airborne and Surface Survival of Pathogens. Proc. Natl. Acad. Sci. USA 2022, 119, e2109750119. [Google Scholar] [CrossRef]
- Morawska, L.; Johnson, G.R.; Ristovski, Z.D.; Hargreaves, M.; Mengersen, K.; Corbett, S.; Chao, C.Y.H.; Li, Y.; Katoshevski, D. Size Distribution and Sites of Origin of Droplets Expelled from the Human Respiratory Tract during Expiratory Activities. J. Aerosol Sci. 2009, 40, 256–269. [Google Scholar] [CrossRef] [Green Version]
- Gregson, F.K.A.; Watson, N.A.; Orton, C.M.; Haddrell, A.E.; McCarthy, L.P.; Finnie, T.J.R.; Gent, N.; Donaldson, G.C.; Shah, P.L.; Calder, J.D.; et al. Comparing Aerosol Concentrations and Particle Size Distributions Generated by Singing, Speaking and Breathing. Aerosol Sci. Technol. 2021, 55, 681–691. [Google Scholar] [CrossRef]
- Bardow, A.; Moe, D.; Nyvad, B.; Nauntofte, B. The Buffer Capacity and Buffer Systems of Human Whole Saliva Measured without Loss of CO2. Arch. Oral Biol. 2000, 45, 1–12. [Google Scholar] [CrossRef]
- Oswin, H.P.; Haddrell, A.E.; Otero-Fernandez, M.; Mann, J.F.S.; Cogan, T.A.; Hilditch, T.G.; Tian, J.; Hardy, D.A.; Hill, D.J.; Finn, A.; et al. The Dynamics of SARS-CoV-2 Infectivity with Changes in Aerosol Microenvironment. Proc. Natl. Acad. Sci. USA 2022, 119, e2200109119. [Google Scholar] [CrossRef] [PubMed]
- Sturman, L.S.; Ricard, C.S.; Holmes, K.V. Conformational Change of the Coronavirus Peplomer Glycoprotein at pH 8.0 and 37 Degrees C Correlates with Virus Aggregation and Virus-Induced Cell Fusion. J. Virol. 1990, 64, 3042–3050. [Google Scholar] [CrossRef] [Green Version]
- Vejerano, E.P.; Marr, L.C. Physico-Chemical Characteristics of Evaporating Respiratory Fluid Droplets. J. R. Soc. Interface 2018, 15, 20170939. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kormuth, K.A.; Lin, K.; Prussin, A.J., II; Vejerano, E.P.; Tiwari, A.J.; Cox, S.S.; Myerburg, M.M.; Lakdawala, S.S.; Marr, L.C. Influenza Virus Infectivity Is Retained in Aerosols and Droplets Independent of Relative Humidity. J. Infect. Dis. 2018, 218, 739–747. [Google Scholar] [CrossRef]
- Dommer, A.; Casalino, L.; Kearns, F.; Rosenfeld, M.; Wauer, N.; Ahn, S.H.; Russo, J.; Oliveira, S.; Morris, C.; Bogetti, A.; et al. #COVIDisAirborne: AI-Enabled Multiscale Computational Microscopy of Delta SARS-CoV-2 in a Respiratory Aerosol. bioRxiv 2021. preprint. [Google Scholar] [CrossRef]
- Bansil, R.; Turner, B.S. The Biology of Mucus: Composition, Synthesis and Organization. Adv. Drug Deliv. Rev. 2018, 124, 3–15. [Google Scholar] [CrossRef]
- Fahy, J.V.; Dickey, B.F. Airway Mucus Function and Dysfunction. N. Engl. J. Med. 2010, 363, 2233–2247. [Google Scholar] [CrossRef] [Green Version]
- Gabryel-Porowska, H.; Gornowicz, A.; Bielawska, A.; Wójcicka, A.; Maciorkowska, E.; Grabowska, S.Z.; Bielawski, K. Mucin Levels in Saliva of Adolescents with Dental Caries. Med. Sci. Monit. 2014, 20, 72–77. [Google Scholar] [CrossRef] [Green Version]
- Bonser, L.R.; Erle, D.J. Airway Mucus and Asthma: The Role of MUC5AC and MUC5B. J. Clin. Med. 2017, 6, 112. [Google Scholar] [CrossRef] [Green Version]
- Kesimer, M.; Ford, A.A.; Ceppe, A.; Radicioni, G.; Cao, R.; Davis, C.W.; Doerschuk, C.M.; Alexis, N.E.; Anderson, W.H.; Henderson, A.G.; et al. Airway Mucin Concentration as a Marker of Chronic Bronchitis. N. Engl. J. Med. 2017, 377, 911–922. [Google Scholar] [CrossRef]
- Li, Y.; Tang, X.X. Abnormal Airway Mucus Secretion Induced by Virus Infection. Front. Immunol. 2021, 12, 3897. [Google Scholar] [CrossRef] [PubMed]
- Moniaux, N.; Escande, F.; Porchet, N.; Aubert, J.-P.; Batra, S.K. Structural Organization and Classification of the Human Mucin Genes. Front. Biosci. 2001, 6, 1192–1206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bergstrom, K.S.B.; Xia, L. Mucin-Type O-Glycans and Their Roles in Intestinal Homeostasis. Glycobiology 2013, 23, 1026–1037. [Google Scholar] [CrossRef] [PubMed]
- Stürmer, R.; Harder, S.; Schlüter, H.; Hoffmann, W. Commercial Porcine Gastric Mucin Preparations, also Used as Artificial Saliva, Are a Rich Source for the Lectin TFF2: In Vitro Binding Studies. ChemBioChem 2018, 19, 2598–2608. [Google Scholar] [CrossRef] [PubMed]
- Mucin Type II 84082-64-4. Available online: http://www.sigmaaldrich.com (accessed on 19 July 2022).
- Lillehoj, E.P.; Kato, K.; Lu, W.; Kim, K.C. Cellular and Molecular Biology of Airway Mucins. Int. Rev. Cell Mol. Biol. 2013, 303, 139–202. [Google Scholar] [CrossRef] [Green Version]
- Allen, A.; Hutton, D.A.; Pearson, J.P. The MUC2 Gene Product: A Human Intestinal Mucin. Int. J. Biochem. Cell Biol. 1998, 30, 797–801. [Google Scholar] [CrossRef]
- Ali, J.; Lee, J.B.; Gittings, S.; Iachelini, A.; Bennett, J.; Cram, A.; Garnett, M.; Roberts, C.J.; Gershkovich, P. Development and Optimisation of Simulated Salivary Fluid for Biorelevant Oral Cavity Dissolution. Eur. J. Pharm. Biopharm. 2021, 160, 125–133. [Google Scholar] [CrossRef]
- Woo, M.-H.; Hsu, Y.-M.; Wu, C.-Y.; Heimbuch, B.; Wander, J. Method for Contamination of Filtering Facepiece Respirators by Deposition of MS2 Viral Aerosols. J. Aerosol Sci. 2010, 41, 944–952. [Google Scholar] [CrossRef]
- Zuo, Z.; Kuehn, T.H.; Bekele, A.Z.; Mor, S.K.; Verma, H.; Goyal, S.M.; Raynor, P.C.; Pui, D.Y.H. Survival of Airborne MS2 Bacteriophage Generated from Human Saliva, Artificial Saliva, and Cell Culture Medium. Appl. Environ. Microbiol. 2014, 80, 2796–2803. [Google Scholar] [CrossRef] [Green Version]
- Ratnesar-Shumate, S.; Williams, G.; Green, B.; Krause, M.; Holland, B.; Wood, S.; Bohannon, J.; Boydston, J.; Freeburger, D.; Hooper, I.; et al. Simulated Sunlight Rapidly Inactivates SARS-CoV-2 on Surfaces. J. Infect. Dis. 2020, 222, 214–222. [Google Scholar] [CrossRef]
- Fernandez, M.O.; Thomas, R.J.; Garton, N.J.; Hudson, A.; Haddrell, A.; Reid, J.P. Assessing the Airborne Survival of Bacteria in Populations of Aerosol Droplets with a Novel Technology. J. R. Soc. Interface 2019, 16, 20180779. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rovelli, G.; Miles, R.E.H.; Reid, J.P.; Clegg, S.L. Accurate Measurements of Aerosol Hygroscopic Growth over a Wide Range in Relative Humidity. J. Phys. Chem. A 2016, 120, 4376–4388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sturman, L.S.; Takemoto, K.K. Enhanced Growth of a Murine Coronavirus in Transformed Mouse Cells. Infect. Immun. 1972, 6, 501–507. [Google Scholar] [CrossRef] [Green Version]
- Stokes, H.L.; Baliji, S.; Hui, C.G.; Sawicki, S.G.; Baker, S.C.; Siddell, S.G. A New Cistron in the Murine Hepatitis Virus Replicase Gene. J. Virol. 2010, 84, 10148–10158. [Google Scholar] [CrossRef] [Green Version]
- Leibowitz, J.; Kaufman, G.; Liu, P. Coronaviruses: Propagation, Quantification, Storage, and Construction of Recombinant Mouse Hepatitis Virus. Curr. Protoc. Microbiol. 2011, 21, 15E.1.1–15E.1.46. [Google Scholar] [CrossRef] [PubMed]
- Reed, L.J.; Muench, H. A Simple Method of Estimating Fifty per Cent Endpoints12. Am. J. Epidemiol. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Haddrell, A.; Rovelli, G.; Lewis, D.; Church, T.; Reid, J. Identifying Time-Dependent Changes in the Morphology of an Individual Aerosol Particle from Its Light Scattering Pattern. Aerosol Sci. Technol. 2019, 53, 1334–1351. [Google Scholar] [CrossRef]
- Hardy, D.A.; Archer, J.; Lemaitre, P.; Vehring, R.; Reid, J.P.; Walker, J.S. High Time Resolution Measurements of Droplet Evaporation Kinetics and Particle Crystallisation. Phys. Chem. Chem. Phys. 2021, 23, 18568–18579. [Google Scholar] [CrossRef]
- Wei, H.; Vejerano, E.P.; Leng, W.; Huang, Q.; Willner, M.R.; Marr, L.C.; Vikesland, P.J. Aerosol Microdroplets Exhibit a Stable PH Gradient. Proc. Natl. Acad. Sci. USA 2018, 115, 7272–7277. [Google Scholar] [CrossRef] [Green Version]
- Xie, X.; Li, Y.; Chwang, A.T.Y.; Ho, P.L.; Seto, W.H. How Far Droplets Can Move in Indoor Environments—Revisiting the Wells Evaporation-Falling Curve. Indoor Air 2007, 17, 211–225. [Google Scholar] [CrossRef]
- Johnson, G.R.; Morawska, L.; Ristovski, Z.D.; Hargreaves, M.; Mengersen, K.; Chao, C.Y.H.; Wan, M.P.; Li, Y.; Xie, X.; Katoshevski, D.; et al. Modality of Human Expired Aerosol Size Distributions. J. Aerosol Sci. 2011, 42, 839–851. [Google Scholar] [CrossRef]
- Tang, J.W.; Li, Y.; Eames, I.; Chan, P.K.S.; Ridgway, G.L. Factors Involved in the Aerosol Transmission of Infection and Control of Ventilation in Healthcare Premises. J. Hosp. Infect. 2006, 64, 100–114. [Google Scholar] [CrossRef] [PubMed]
- Tellier, R.; Li, Y.; Cowling, B.J.; Tang, J.W. Recognition of Aerosol Transmission of Infectious Agents: A Commentary. BMC Infect. Dis. 2019, 19, 101. [Google Scholar] [CrossRef] [PubMed]
- Lai, S.K.; Wang, Y.-Y.; Wirtz, D.; Hanes, J. Micro- and Macrorheology of Mucus. Adv. Drug Deliv. Rev. 2009, 61, 86–100. [Google Scholar] [CrossRef] [Green Version]
- Raynal, B.D.E.; Hardingham, T.E.; Sheehan, J.K.; Thornton, D.J. Calcium-Dependent Protein Interactions in MUC5B Provide Reversible Cross-Links in Salivary Mucus. J. Biol. Chem. 2003, 278, 28703–28710. [Google Scholar] [CrossRef] [Green Version]
- Ambort, D.; Johansson, M.E.V.; Gustafsson, J.K.; Nilsson, H.E.; Ermund, A.; Johansson, B.R.; Koeck, P.J.B.; Hebert, H.; Hansson, G.C. Calcium and PH-Dependent Packing and Release of the Gel-Forming MUC2 Mucin. Proc. Natl. Acad. Sci. USA 2012, 109, 5645–5650. [Google Scholar] [CrossRef] [Green Version]
- Kufe, D.W. Mucins in Cancer: Function, Prognosis and Therapy. Nat. Rev. Cancer 2009, 9, 874–885. [Google Scholar] [CrossRef] [Green Version]
- Kim, W.M.; Huang, Y.-H.; Gandhi, A.; Blumberg, R.S. CEACAM1 Structure and Function in Immunity and Its Therapeutic Implications. Semin. Immunol. 2019, 42, 101296. [Google Scholar] [CrossRef]
- Dveksler, G.S.; Pensiero, M.N.; Cardellichio, C.B.; Williams, R.K.; Jiang, G.S.; Holmes, K.V.; Dieffenbach, C.W. Cloning of the Mouse Hepatitis Virus (MHV) Receptor: Expression in Human and Hamster Cell Lines Confers Susceptibility to MHV. J. Virol. 1991, 65, 6881–6891. [Google Scholar] [CrossRef] [Green Version]
- Regl, G.; Kaser, A.; Iwersen, M.; Schmid, H.; Kohla, G.; Strobl, B.; Vilas, U.; Schauer, R.; Vlasak, R. The Hemagglutinin-Esterase of Mouse Hepatitis Virus Strain S Is a Sialate-4-O-Acetylesterase. J. Virol. 1999, 73, 4721–4727. [Google Scholar] [CrossRef] [Green Version]
- Langereis, M.; van Vliet, A.L.W.; Boot, W.; de Groot, R.J.; Langereis, M.; van Vliet, A.L.W.; Boot, W.; de Groot, R.J. Attachment of Mouse Hepatitis Virus to O-Acetylated Sialic Acid Is Mediated by Hemagglutinin-Esterase and Not by the Spike Protein. J. Virol. 2010, 84, 8970–8974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wardzala, C.L.; Wood, A.M.; Belnap, D.M.; Kramer, J.R. Mucins Inhibit Coronavirus Infection in a Glycan-Dependent Manner. ACS Cent. Sci. 2022, 8, 351–360. [Google Scholar] [CrossRef] [PubMed]
- Thermo Fisher Scientific 11965-DMEM, High Glucose-UK. Available online: https://www.thermofisher.com/uk/en/home/technical-resources/media-formulation.8.html (accessed on 24 November 2021).
- Smither, S.J.; Eastaugh, L.S.; Findlay, J.S.; Lever, M.S. Experimental Aerosol Survival of SARS-CoV-2 in Artificial Saliva and Tissue Culture Media at Medium and High Humidity. Emerg. Microbes Infect. 2020, 9, 1415–1417. [Google Scholar] [CrossRef] [PubMed]
- Chauncey, H.H.; Levine, D.M.; Kass, G.; Shwachman, H.; Henriques, B.L.; Kulczyeki, L.L. Composition of Human Saliva: Parotid Gland Secretory Rate and Electrolyte Concentration in Children with Cystic Fibrosis. Arch. Oral Biol. 1962, 7, 707–713. [Google Scholar] [CrossRef]
- Meurman, J.H.; Rantonen, P.; Pajukoski, H.; Sulkava, R. Salivary Albumin and Other Constituents and Their Relation to Oral and General Health in the Elderly. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2002, 94, 432–438. [Google Scholar] [CrossRef]
- Kallapur, B.; Ramalingam, K.; Bastian; Mujib, A.; Sarkar, A.; Sethuraman, S. Quantitative Estimation of Sodium, Potassium and Total Protein in Saliva of Diabetic Smokers and Nonsmokers: A Novel Study. J. Nat. Sci. Biol. Med. 2013, 4, 341–345. [Google Scholar] [CrossRef] [Green Version]
- Maddu, N.; Gokul, S. Functions of Saliva and Salivary Diagnostics. Available online: https://www.intechopen.com/chapters/66233 (accessed on 17 January 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alexander, R.W.; Tian, J.; Haddrell, A.E.; Oswin, H.P.; Neal, E.; Hardy, D.A.; Otero-Fernandez, M.; Mann, J.F.S.; Cogan, T.A.; Finn, A.; et al. Mucin Transiently Sustains Coronavirus Infectivity through Heterogenous Changes in Phase Morphology of Evaporating Aerosol. Viruses 2022, 14, 1856. https://doi.org/10.3390/v14091856
Alexander RW, Tian J, Haddrell AE, Oswin HP, Neal E, Hardy DA, Otero-Fernandez M, Mann JFS, Cogan TA, Finn A, et al. Mucin Transiently Sustains Coronavirus Infectivity through Heterogenous Changes in Phase Morphology of Evaporating Aerosol. Viruses. 2022; 14(9):1856. https://doi.org/10.3390/v14091856
Chicago/Turabian StyleAlexander, Robert W., Jianghan Tian, Allen E. Haddrell, Henry P. Oswin, Edward Neal, Daniel A. Hardy, Mara Otero-Fernandez, Jamie F. S. Mann, Tristan A. Cogan, Adam Finn, and et al. 2022. "Mucin Transiently Sustains Coronavirus Infectivity through Heterogenous Changes in Phase Morphology of Evaporating Aerosol" Viruses 14, no. 9: 1856. https://doi.org/10.3390/v14091856
APA StyleAlexander, R. W., Tian, J., Haddrell, A. E., Oswin, H. P., Neal, E., Hardy, D. A., Otero-Fernandez, M., Mann, J. F. S., Cogan, T. A., Finn, A., Davidson, A. D., Hill, D. J., & Reid, J. P. (2022). Mucin Transiently Sustains Coronavirus Infectivity through Heterogenous Changes in Phase Morphology of Evaporating Aerosol. Viruses, 14(9), 1856. https://doi.org/10.3390/v14091856





