CMV and EBV Co-Infection in HIV-Infected Children: Infection Rates and Analysis of Differential Expression of Cytokines in HIV Mono- and HIV–CMV–EBV Co-Infected Groups
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Samples
2.2. Nucleic Acid (DNA and RNA) Extraction and cDNA Synthesis
2.3. Quantitative PCR for Detection of CMV and EBV
2.4. Quantitative PCR for Assessment of Cytokine Expression in HIV Mono- and CMV/EBV Co-Infected Samples
2.5. Statistical Analysis
3. Results
3.1. Study Subjects and EBV and CMV Status
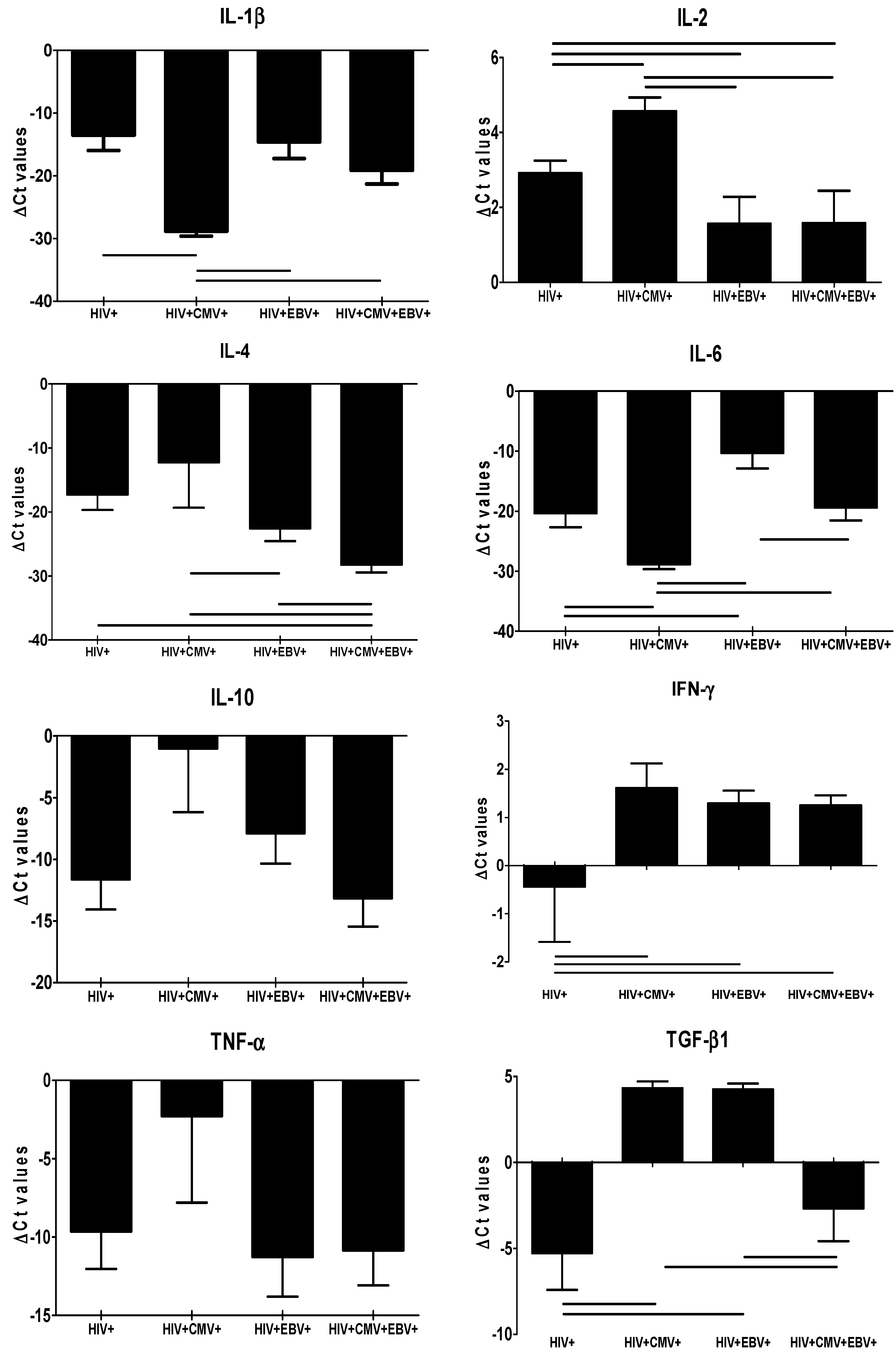
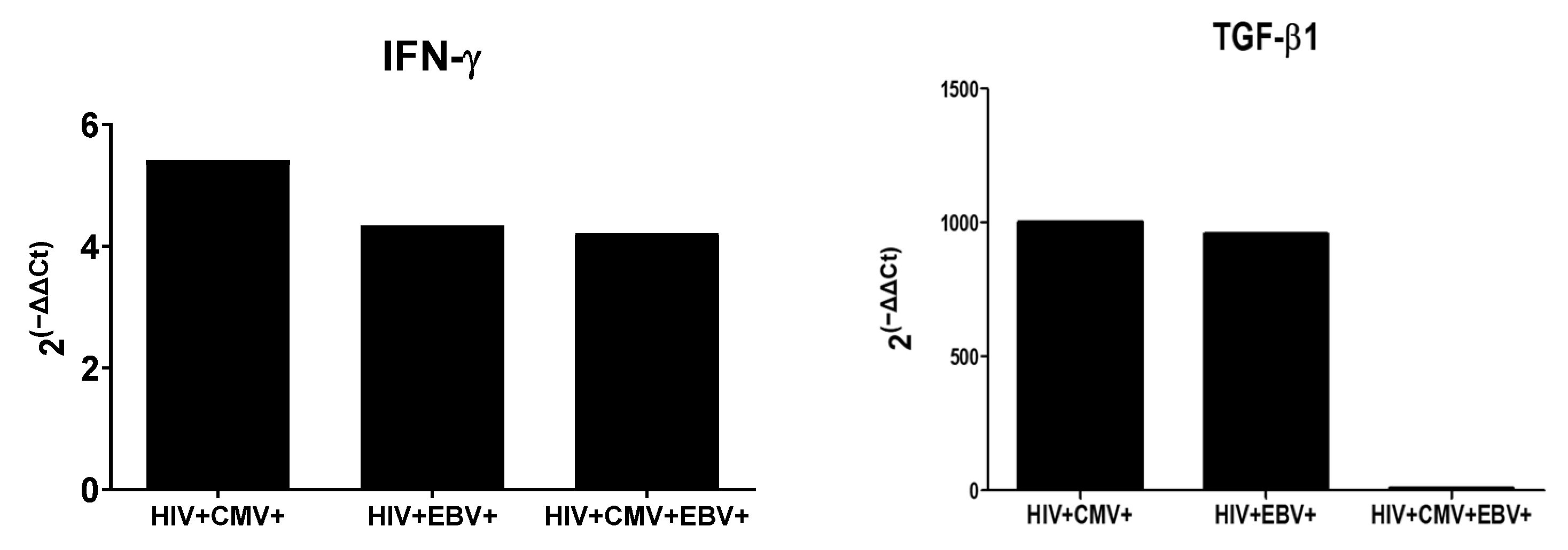
3.2. Differential Expression of Cytokines in HIV Mono- and Co-Infected Groups
3.3. Correlation between Differentially Expressed Cytokines in HIV Mono- and Co-Infected Groups
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hunt, P.W. HIV and Inflammation: Mechanisms and Consequences. Curr. HIV/AIDS Rep. 2012, 9, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.L.; Lederman, M.M.; Gianella, S. Partners in Crime: The Role of CMV in Immune Dysregulation and Clinical Outcome During HIV Infection. Curr. HIV/AIDS Rep. 2016, 13, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Cannon, M.J.; Schmid, D.S.; Hyde, T.B. Review of cytomegalovirus seroprevalence and demographic characteristics associated with infection. Rev. Med Virol. 2010, 20, 202–213. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Gao, Y.; Peng, Y.; Fu, M.; Liu, Y.-Q.; Zhou, Q.-J.; Yu, J.; Zheng, X.-Q. Epidemiological survey of human cytomegalovirus antibody levels in children from Southeastern China. Virol. J. 2014, 11, 123. [Google Scholar] [CrossRef]
- Bolis, V.; Karadedos, C.; Chiotis, I.; Chaliasos, N.; Tsabouri, S. Atypical manifestations of Epstein–Barr virus in children: A diagnostic challenge. J. Pediatr. 2016, 92, 113–121. [Google Scholar] [CrossRef]
- Adland, E.; Klenerman, P.; Goulder, P.; Matthews, P.C. Ongoing burden of disease and mortality from HIV/CMV coinfection in Africa in the antiretroviral therapy era. Front. Microbiol. 2015, 6, 1016. [Google Scholar] [CrossRef]
- de Oliveira, J.L.; Freitas, R.T.; Arcuri, L.J.; Gomes, A.P.; Vitorino, R.R.; Rodrigues, D.C.; de Paula, S.O.; Santana, L.A.; Siqueira-Batista, R. O vírus Epstein-Barr e a mononucleose infecciosa. Rev. Bras. Clin. Med. São Paulo 2012, 10, 535–543. [Google Scholar]
- Miller, C.S.; Berger, J.R.; Mootoor, Y.; Avdiushko, S.A.; Zhu, H.; Kryscio, R.J. High prevalence of multiple human herpesviruses in saliva from human immunodeficiency virus-infected persons in the era of highly active antiretroviral therapy. J. Clin. Microbiol. 2006, 44, 2409–2415. [Google Scholar] [CrossRef]
- Ammatuna, P.; Campisi, G.; Giovannelli, L.; Giambelluca, D.; Alaimo, C.; Mancuso, S.; Margiotta, V. Presence of Epstein–Barr virus, cytomegalovirus and human papillomavirus in normal oral mucosa of HIV-infected and renal transplant patients. Oral Dis. 2001, 7, 34–40. [Google Scholar]
- Wang, X.; Yang, K.; Wei, C.; Huang, Y.; Zhao, D. Coinfection with EBV/CMV and other respiratory agents in children with suspected infectious mononucleosis. Virol. J. 2010, 7, 247. [Google Scholar] [CrossRef]
- Patekar, D.; Kheur, S.; More, P.; Hambire, C.; Kheur, M. Prevalence of viral coinfections with EBV and CMV and its correlation with CD4 count in HIV-1 serpositive patients. J. AIDS Clin. Res. 2015, 6, 6–9. [Google Scholar] [CrossRef]
- Robain, M.; Boufassa, F.; Hubert, J.-B.; Persoz, A.; Burgard, M.; Meyer, L. Cytomegalovirus seroconversion as a cofactor for progression to AIDS. Aids 2001, 15, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Mitoma, F.; Ruiz, A.; Flowerdew, G.; Houston, S.; Romanowski, B.; Kovithavongs, T.; Preiksaitis, J.; Tyrrell, D.L. High levels of Epstein-Barr virus in the oropharynx: A predictor of disease progression in human immunodeficiency virus infection. J. Med. Virol. 1990, 31, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Hernández, D.M.; Valderrama, S.; Gualtero, S.; Hernández, C.; López, M.; Herrera, M.V.; Solano, J.; Fiorentino, S.; Quijano, S. Loss of T-Cell Multifunctionality and TCR-Vβ Repertoire Against Epstein-Barr Virus Is Associated with Worse Prognosis and Clinical Parameters in HIV+ Patients. Front. Immunol. 2018, 9, 2291. [Google Scholar] [CrossRef] [PubMed]
- Breen, E.C. Pro- and anti-inflammatory cytokines in human immunodeficiency virus infection and acquired immunodeficiency syndrome. Pharmacol. Ther. 2002, 95, 295–304. [Google Scholar] [CrossRef]
- Osborn, L.; Kunkel, S.; Nabel, G.J. Tumor necrosis factor alpha and interleukin 1 stimulate the human immunodeficiency virus enhancer by activation of the nuclear factor kappa B. Proc. Natl. Acad. Sci. USA 1989, 86, 2336–2340. [Google Scholar] [CrossRef]
- Kedzierska, K.; Crowe, S.M. Cytokines and HIV-1: Interactions and Clinical Implications. Antivir. Chem. Chemother. 2001, 12, 133–150. [Google Scholar] [CrossRef]
- Poli, G.; Kinter, A.L.; Justement, J.S.; Biswas, P.; Weissman, E.; Fox, L.M.; Goletti, D.; Bressler, P.; Stanley, S.K.; Fauci, A.S. The Chronically Infected Promonocytic Cell Line U1: A Model of HIV Expression Regulated by Cytokines. ImmunoMethods 1993, 3, 50–55. [Google Scholar] [CrossRef]
- Kaur, R.; Dhakad, M.S.; Goal, R.; Bhalla, P.; Dewan, R. Study of TH1/TH2 cytokine profiles in HIV/AIDS patients in a tertiary care hospital India. J. Med. Microbiol. Diagn. 2016, 5. [Google Scholar] [CrossRef]
- Theron, A.J.; Anderson, R.; Rossouw, T.; Steel, H.C. The Role of Transforming Growth Factor Beta-1 in the Progression of HIV/AIDS and Development of Non-AIDS-Defining Fibrotic Disorders. Front. Immunol. 2017, 8, 1461. [Google Scholar] [CrossRef]
- Lurain, N.S.; Robert, E.S.; Xu, J.; Camarca, M.; Landay, A.; Kovacs, A.A.; Reichelderfer, P.S. HIV Type 1 and Cytomegalovirus Coinfection in the Female Genital Tract. J. Infect. Dis. 2004, 190, 619–623. [Google Scholar] [CrossRef] [PubMed]
- Baqi, S.; Nabi, N.; Hasan, S.N.; Khan, A.J.; Pasha, O.; Kayani, N.; Haque, R.A.; Haq-IU; Khurshid, M.; Fisher-Hoch, S.; et al. HIV antibody seroprevalence and associated risk factors in sex workers, drug users, and prisoners in Sindh, Pakistan. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. Off. Publ. Int. Retrovirol. Assoc. 1998, 18, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Raees, M.A.; Abidi, S.H.; Ali, W.; Khanani, M.R.; Ali, S. HIV among women and children in Pakistan. Trends Microbiol. 2013, 21, 213–214. [Google Scholar] [CrossRef] [PubMed]
- Waheed, Y.; Waheed, H.W.Y. Pakistan needs to speed up its human immunodeficiency virus control strategy to achieve targets in fast-track acquired immune deficiency syndrome response. World J. Virol. 2017, 6, 46–48. [Google Scholar] [CrossRef]
- Mir, F.; Mahmood, F.; Siddiqui, A.R.; Baqi, S.; Abidi, S.H.; Kazi, A.M.; Nathwani, A.A.; Ladhani, A.; Qamar, F.N.; Soofi, S.B.; et al. HIV infection predominantly affecting children in Sindh, Pakistan, 2019: A cross-sectional study of an outbreak. Lancet Infect. Dis. 2020, 20, 362–370. [Google Scholar] [CrossRef]
- Mir, F.; Nathwani, A.A.; Simms, V.; Abidi, S.H.; Siddiqui, A.R.; Hotwani, A.; Memon, S.A.; Shaikh, S.A.; Soomro, J.; Shah, S.A.; et al. Factors associated with HIV infection among children in Larkana District, Pakistan: A matched case-control study. Lancet HIV 2021, 8, e342–e352. [Google Scholar] [CrossRef]
- Siddiqui, A.R.; Nathwani, A.A.; Abidi, S.H.; Mahmood, S.F.; Azam, I.; Sawani, S.; Kazi, A.M.; Hotwani, A.; Memon, S.A.; Soomro, J.; et al. Investigation of an extensive outbreak of HIV infection among children in Sindh, Pakistan: Protocol for a matched case–control study. BMJ Open 2020, 10, e036723. [Google Scholar] [CrossRef]
- Rizwan-Ul-Hasan, S.; Farrukh, F.; Ahmed, S.; Abidi, S.H. A mathematical modeling approach to measure the probability of HIV-1 transmission for different high-risk groups of Pakistan. J. Infect. Dev. Ctries 2021, 15, 1212–1215. [Google Scholar] [CrossRef]
- Abidi, S.H.; Nduva, G.M.; Siddiqui, D.; Rafaqat, W.; Mahmood, S.F.; Siddiqui, A.R.; Nathwani, A.A.; Hotwani, A.; Shah, S.A.; Memon, S.; et al. Phylogenetic and Drug-Resistance Analysis of HIV-1 Sequences From an Extensive Paediatric HIV-1 Outbreak in Larkana, Pakistan. Front. Microbiol. 2021, 12, 2305. [Google Scholar] [CrossRef]
- Rizwan, S.; Abdullah, A.; Ahmed, S.; Shah, S.A.; Mir, F.; Abidi, S.H. Research Article Probabilistic measures of HIV-1 transmission in different HIV-1 key population groups of Larkana, Pakistan. J. Pak. Med. Assoc. 2021, 71, 617. [Google Scholar]
- Gupta, K.K.; Attri, J.P.; Singh, A.; Kaur, H.; Kaur, G. Basic concepts for sample size calculation: Critical step for any clinical trials! Saudi J. Anaesth. 2016, 10, 328. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.A.; Anwar, M.F.; Ahmed, K.; Aftab, M.; Nazim, F.; Bari, M.F.; Mustafa, M.; Vohra, F.; Alrahlah, A.; Mughal, N.; et al. Baseline MMP expression in periapical granuloma and its relationship with periapical wound healing after surgical endodontic treatment. BMC Oral Health 2021, 21, 562. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, K.; Sheikh, A.; Fatima, S.; Haider, G.; Ghias, K.; Abbas, F.; Mughal, N.; Abidi, S.H. Detection and characterization of latency stage of EBV and histopathological analysis of prostatic adenocarcinoma tissues. Sci. Rep. 2022, 12, 10399. [Google Scholar] [CrossRef] [PubMed]
- Ghulam, U.; Nazim, F.; Farooqui, N.; Anwar, M.F.; Jamal, A.; Keyani, H.A.; Mughal, N.; Hussain, A.; Abidi, S.H. Correlation of nasopharyngeal viral load and pro-inflammatory cytokines with COVID-19 disease severity. Res. Sq. 2022. [Google Scholar] [CrossRef]
- Schmittgen, T.D.; Livak, K.J. Analyzing real-time PCR data by the comparative CT method. Nat. Protoc. 2008, 3, 1101–1108. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]
- Young, S.; Fenn, J.; Arriero, E.; Lowe, A.; Poulin, B.; MacColl, A.D.; Bradley, J.E. Relationships between immune gene expression and circulating cytokine levels in wild house mice. Ecol. Evol. 2020, 10, 13860–13871. [Google Scholar] [CrossRef]
- Galgamuwa, L.S.; Sumanasena, B.; Iddawela, D.; Wickramasinghe, S.; Yatawara, L. Assessment of intralesional cytokine profile of cutaneous leishmaniasis caused by Leishmania donovani in Sri Lanka. BMC Microbiol. 2019, 19, 14. [Google Scholar] [CrossRef]
- Mujtaba, S.; Varma, S.; Sehgal, S. Cytomegalovirus co-infection in patients with HIV/AIDS in north India. Indian J. Med Res. 2003, 117, 99–103. [Google Scholar]
- Mehrkhani, F.; Jam, S.; Sabzvari, D.; Fattahi, F.; Kourorian, Z.; SeyedAlinaghi, S.; Jabbari, H.; Mohraz, M. Cytomegalovirus co-infection in patients with human immunodeficiency virus in Iran. Acta Med. Iran. 2011, 49, 551–555. [Google Scholar]
- Anigilaje, E.A.; Dabit, J.O.; Nweke, N.O.; Agbedeh, A.A. Prevalence and risk factors of cytomegalovirus infection among HIV-infected and HIV-exposed uninfected infants in Nigeria. J. Infect. Dev. Ctries. 2015, 9, 977–987. [Google Scholar] [CrossRef] [PubMed]
- Gumbo, H.; Chasekwa, B.; Church, J.A.; Ntozini, R.; Mutasa, K.; Humphrey, J.H.; Prendergast, A.J. Congenital and Postnatal CMV and EBV Acquisition in HIV-Infected Zimbabwean Infants. PLoS ONE 2014, 9, e114870. [Google Scholar] [CrossRef] [PubMed]
- Guibert, G.; Warszawski, J.; Le Chenadec, J.; Blanche, S.; Benmebarek, Y.; Mandelbrot, L.; Tubiana, R.; Rouzioux, C.; Leruez-Ville, M.; Cohort, F.P. Decreased Risk of Congenital Cytomegalovirus Infection in Children Born to HIV-1-Infected Mothers in the Era of Highly Active Antiretroviral Therapy. Clin. Infect. Dis. 2009, 48, 1516–1525. [Google Scholar] [CrossRef]
- Mujtaba, S.; Varma, S.; Sehgal, S. Coinfection with epstein barr virus in north Indian patients with HIV/AIDS. Indian J. Pathol. Microbiol. 2005, 48, 349–353. [Google Scholar] [PubMed]
- Stevens, S.J.; Blank, B.S.N.; Smits, P.H.M.; Meenhorst, P.L.; Middeldorp, J. High Epstein–Barr virus (EBV) DNA loads in HIV-infected patients: Correlation with antiretroviral therapy and quantitative EBV serology. AIDS 2002, 16, 993–1001. [Google Scholar] [CrossRef] [PubMed]
- Slyker, J.A.; Casper, C.; Tapia, K.; Richardson, B.; Bunts, L.; Huang, M.-L.; Maleche-Obimbo, E.; Nduati, R.; John-Stewart, G. Clinical and Virologic Manifestations of Primary Epstein-Barr Virus (EBV) Infection in Kenyan Infants Born to HIV-Infected Women. J. Infect. Dis. 2013, 207, 1798–1806. [Google Scholar] [CrossRef]
- Gianella, S.; Moser, C.; Vitomirov, A.; McKhann, A.; Layman, L.; Scott, B.; Caballero, G.; Lada, S.; Bosch, R.J.; Hoenigl, M.; et al. Presence of asymptomatic cytomegalovirus and Epstein--Barr virus DNA in blood of persons with HIV starting antiretroviral therapy is associated with non-AIDS clinical events. AIDS 2020, 34, 849–857. [Google Scholar] [CrossRef]
- Viljoen, J.; Tuaillon, E.; Nagot, N.; Danaviah, S.; Peries, M.; Padayachee, P.; Foulongne, V.; Bland, R.; Rollins, N.; Newell, M.-L.; et al. Cytomegalovirus, and possibly Epstein–Barr virus, shedding in breast milk is associated with HIV-1 transmission by breastfeeding. AIDS 2015, 29, 145–153. [Google Scholar] [CrossRef]
- Santos, L.; Azevedo, K.; Silva, L.; Oliveira, L. Epstein-Barr virus in oral mucosa from human immunodeficiency virus positive patients. Rev. Assoc. Méd. Bras. 2014, 60, 262–269. [Google Scholar] [CrossRef]
- Zhao, M.; Zhuo, C.; Li, Q.; Liu, L. Cytomegalovirus (CMV) infection in HIV/AIDS patients and diagnostic values of CMV-DNA detection across different sample types. Ann. Palliat. Med. 2020, 9, 2710–2715. [Google Scholar] [CrossRef]
- Piriou, E.; Jansen, C.A.; van Dort, K.; De Cuyper, I.; Nanlohy, N.M.; Lange, J.M.A.; van Oers, M.H.J.; Miedema, F.; van Baarle, D. Reconstitution of EBV Latent but Not Lytic Antigen-Specific CD4+and CD8+T Cells after HIV Treatment with Highly Active Antiretroviral Therapy. J. Immunol. 2005, 175, 2010–2017. [Google Scholar] [CrossRef] [PubMed]
- Lusso, P.; De Maria, A.; Malnati, M.; Lori, F.; DeRocco, S.E.; Baseler, M.; Gallo, R.C. Induction of CD4 and susceptibility to HIV-1 infection in human CD8+ T lymphocytes by human herpesvirus 6. Nature 1991, 349, 533–535. [Google Scholar] [CrossRef] [PubMed]
- Ensoli, B.; Lusso, P.; Schachter, F.; Josephs, S.; Rappaport, J.; Negro, F.; Gallo, R.; Wong-Staal, F. Human herpes virus-6 increases HIV-1 expression in co-infected T cells via nuclear factors binding to the HIV-1 enhancer. EMBO J. 1989, 8, 3019–3027. [Google Scholar] [CrossRef] [PubMed]
- Lusso, P.; Ensoli, B.; Markham, P.D.; Ablashi, D.V.; Salahuddin, S.Z.; Tschachler, E.; Wong-Staal, F.; Gallo, R.C. Productive dual infection of human CD4+ T lymphocytes by HIV-1 and HHV-6. Nature 1989, 337, 370–373. [Google Scholar] [CrossRef] [PubMed]
- Wilson, C.B.; Westall, J.; Johnston, L.; Lewis, D.B.; Dower, S.K.; Alpert, A.R. Decreased production of interferon-gamma by human neonatal cells. Intrinsic and regulatory deficiencies. J. Clin. Investig. 1986, 77, 860–867. [Google Scholar] [CrossRef]
- Lohman, B.L.; Slyker, J.A.; Richardson, B.A.; Farquhar, C.; Mabuka, J.M.; Crudder, C.; Dong, T.; Obimbo, E.; Mbori-Ngacha, D.; Overbaugh, J.; et al. Longitudinal Assessment of Human Immunodeficiency Virus Type 1 (HIV-1)-Specific Gamma Interferon Responses during the First Year of Life in HIV-1-Infected Infants. J. Virol. 2005, 79, 8121–8130. [Google Scholar] [CrossRef]
- Steed, A.L.; Barton, E.S.; Tibbetts, S.A.; Popkin, D.L.; Lutzke, M.L.; Rochford, R.; Virgin, H.W. Gamma Interferon Blocks Gammaherpesvirus Reactivation from Latency. J. Virol. 2006, 80, 192–200. [Google Scholar] [CrossRef]
- Presti, R.; Pollock, J.L.; Canto, A.J.D.; O’Guin, A.K.; Iv, H.W.V. Interferon γ Regulates Acute and Latent Murine Cytomegalovirus Infection and Chronic Disease of the Great Vessels. J. Exp. Med. 1998, 188, 577–588. [Google Scholar] [CrossRef]
- Minami, M.; Kita, M.; Yan, X.Q.; Yamamoto, T.; Iida, T.; Sekikawa, K.; Iwakura, Y.; Imanishi, J. Role of IFN-γ and tumor necrosis factor-α in herpes simplex virus type 1 infection. J. Interferon Cytokine Res. 2002, 22, 671–676. [Google Scholar] [CrossRef]
- La Rosa, C.; Diamond, D.J. The immune response to human CMV. Futur. Virol. 2012, 7, 279–293. [Google Scholar] [CrossRef]
- Cárdenas-Mondragón, M.G.; Torres, J.; Sánchez-Zauco, N.; Gómez-Delgado, A.; Camorlinga-Ponce, M.; Maldonado-Bernal, C.; Fuentes-Pananá, E.M. Elevated Levels of Interferon-γ Are Associated with High Levels of Epstein-Barr Virus Reactivation in Patients with the Intestinal Type of Gastric Cancer. J. Immunol. Res. 2017, 2017, 7069242. [Google Scholar] [CrossRef]
- Strong, M.; Xu, G.; Coco, J.; Baribault, C.; Vinay, D.S.; Lacey, M.; Strong, A.; Lehman, T.A.; Seddon, M.B.; Lin, Z.; et al. Differences in Gastric Carcinoma Microenvironment Stratify According to EBV Infection Intensity: Implications for Possible Immune Adjuvant Therapy. PLoS Pathog. 2013, 9, e1003341. [Google Scholar] [CrossRef] [PubMed]
- Leeansyah, E.; Malone, D.; Anthony, D.D.; Sandberg, J. Soluble biomarkers of HIV transmission, disease progression and comorbidities. Curr. Opin. HIV AIDS 2013, 8, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Dickinson, M.; Kliszczak, A.E.; Giannoulatou, E.; Peppa, D.; Pellegrino, P.; Williams, I.; Drakesmith, H.; Borrow, P. Dynamics of Transforming Growth Factor (TGF)-β Superfamily Cytokine Induction During HIV-1 Infection Are Distinct From Other Innate Cytokines. Front. Immunol. 2020, 11, 3044. [Google Scholar] [CrossRef] [PubMed]
- Wiercińska-Drapalo, A.; Flisiak, R.; Jaroszewicz, J.; Prokopowicz, D. Increased Plasma Transforming Growth Factor-β1 Is Associated with Disease Progression in HIV-1-Infected Patients. Viral Immunol. 2004, 17, 109–113. [Google Scholar] [CrossRef]
- Maina, E.K.; Abana, C.; Bukusi, E.; Sedegah, M.; Lartey, M.; Ampofo, W. Plasma concentrations of transforming growth factor beta 1 in non-progressive HIV-1 infection correlates with markers of disease progression. Cytokine 2016, 81, 109–116. [Google Scholar] [CrossRef]
- El Baba, R.; Herbein, G. Immune Landscape of CMV Infection in Cancer Patients: From “Canonical” Diseases Toward Virus-Elicited Oncomodulation. Front. Immunol. 2021, 12, 3659. [Google Scholar] [CrossRef]
- Herbein, G. Tumors and Cytomegalovirus: An Intimate Interplay. Viruses 2022, 14, 812. [Google Scholar] [CrossRef]
- Michelson, S.; Alcami, J.; Kim, S.J.; Danielpour, D.; Bachelerie, F.; Picard, L.; Bessia, C.; Paya, C.; Virelizier, J.L. Human cytomegalovirus infection induces transcription and secretion of transforming growth factor beta 1. J. Virol. 1994, 68, 5730–5737. [Google Scholar] [CrossRef]
- Fukuda, M.; Ikuta, K.; Yanagihara, K.; Tajima, M.; Kuratsune, H.; Kurata, T.; Sairenji, T. Effect of Transforming Growth Factor-β1 on the Cell Growth and Epstein–Barr Virus Reactivation in EBV-Infected Epithelial Cell Lines. Virology 2001, 288, 109–118. [Google Scholar] [CrossRef]
- Blackard, J.T.; Pradel, F.; Perret, M.; Sodoyer, M.; Smeaton, L.; Clair, J.B.S.; Chapman, S.; Taylor, L.E.; Paranhos-Baccalà, G.; Chung, R.T. Intrahepatic cytokine expression is downregulated during HCV/HIV co-infection. J. Med Virol. 2006, 78, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.; Weinberg, E.M.; Tai, A.W.; Peng, L.F.; Brockman, M.A.; Kim, K.A.; Kim, S.S.; Borges, C.B.; Shao, R.-X.; Chung, R.T. HIV Increases HCV Replication in a TGF-β1–Dependent Manner. Gastroenterology 2008, 134, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Kossmann, T.; Morganti-Kossmann, C.; Orenstein, J.M.; Britt, W.J.; Wahl, S.M.; Smith, P.D. Cytomegalovirus Production by Infected Astrocytes Correlates with Transforming Growth Factor-β Release. J. Infect. Dis. 2003, 187, 534–541. [Google Scholar] [CrossRef] [PubMed]
- El-Meguid, M.A.; Dawood, R.M.; Ibrahim, M.K.; Salum, G.M.; Alla, M.D.A.A.; El Awady, M.K. Reactivation of human cytomegalovirus inhibits expression of liver fibrosis related cytokines in patients chronically infected with hepatitis C virus genotype 4a. Microb. Pathog. 2020, 152, 104596. [Google Scholar] [CrossRef] [PubMed]
- Sampey, G.C.; Saifuddin, M.; Schwab, A.; Barclay, R.; Punya, S.; Chung, M.-C.; Hakami, R.M.; Zadeh, M.A.; Lepene, B.; Klase, Z.A.; et al. Exosomes from HIV-1-infected Cells Stimulate Production of Pro-inflammatory Cytokines through Trans-activating Response (TAR) RNA. J. Biol. Chem. 2016, 291, 1251–1266. [Google Scholar] [CrossRef] [PubMed]
| Gene | Forward Primer (5′ to 3′) | Reverse Primer (5′ to 3′) |
|---|---|---|
| Β-actin | GCGCGGCTACAGCTTCA | CTCCTTAATGTCACGCACGAT |
| IL-1β | ATGATGGCTTATTACAGTGGCAA | GTCGGAGATTCGTAGCTGGA |
| IL-2 | GAAGATCGTCATGGGAAGAAGC | CGGGTATTTATAGTGGCATGGG |
| IL-4 | CCAACTGCTTCCCCCTCTG | TCTGTTACGGTCAACTCGGTG |
| IL-6 | ACTCACCTCTTCAGAACGAATTG | CCATCTTTGGAAGGTTCAGGTTG |
| IL-10 | GACTTTAAGGGTTACCTGGGTTG | TCACATGCGCCTTGATGTCTG |
| IFN-γ | TCGGTAACTGACTTGAATGTCCA | TCGCTTCCCTGTTTTAGCTGC |
| TNF-α | GAGGCCAAGCCCTGGTATG | CGGGCCGATTGATCTCAGC |
| TGF-β1 | CAATTCCTGGCGATACCTCAG | GCACAACTCCGGTGACATCAA |
| Variables | HIV+ | HIV/CMV/EBV+ | HIV/CMV+ | HIV/EBV+ | p-Value |
|---|---|---|---|---|---|
| CMV q-PCR (average Ct) | - | 34.94 | 33.71 | - | - |
| EBV q-PCR (average Ct) | - | 33.37 | - | 34.52 | - |
| Mean HIV viral load | 42,396.2 | 24,154.30 | 341.25 | 147,030.21 | 0.001–0.002 * |
| Mean CD4 count | 1144 | 1133 | 1105.5 | 1093.92 | 0.6–0.9 |
| HIV+ Mono-Infected Group | ||||||||
| Cytokines | IL-1β | IL-2 | IL-4 | IL-6 | IL-10 | IFN-γ | TNF-α | TGF-β1 |
| IFN-γ | 0.20 | 0.37 ** | −0.02 | 0.14 | 0.30 * | - | 0.17 | 0.14 |
| TGF-β | 0.06 | 0.11 | 0.63 ** | 0.20 | 0.54 ** | 0.14 | 0.48 ** | - |
| HIV+/CMV+ co-infected group | ||||||||
| Cytokines | IL-1β | IL-2 | IL-4 | IL-6 | IL-10 | IFN-γ | TNF-α | TGF-β1 |
| IFN-γ | 0.43 | 0.71 | −0.77 | 0.43 | 0.03 | - | −0.09 | 0.43 |
| TGF-β | −0.31 | 0.14 | −0.37 | −0.31 | 0.26 | 0.43 | −0.20 | - |
| HIV+/EBV+ co-infected group | ||||||||
| Cytokines | IL-1β | IL-2 | IL-4 | IL-6 | IL-10 | IFN-γ | TNF-α | TGF-β1 |
| IFN-γ | 0.49 ** | 0.68 ** | 0.22 | 0.24 | 0.49 ** | - | 0.53 ** | 0.32 * |
| TGF-β1 | 0.22 | 0.37 ** | 0.03 | 0.26 | 0.10 | 0.32 * | 0.01 | - |
| HIV+/CMV+/EBV+ co-infected group | ||||||||
| Cytokines | IL-1β | IL-2 | IL-4 | IL-6 | IL-10 | IFN-γ | TNF-α | TGF-β1 |
| IFN-γ | 0.14 | 0.50 ** | 0.45 ** | 0.28 * | 0.23 | - | −0.20 | 0.50 ** |
| TGF-β | 0.37 ** | 0.18 | 0.38 ** | 0.40 ** | 0.37 ** | 0.50 ** | 0.15 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nazim, F.; Kayani, H.A.; Ali Nathwani, A.; Mir, F.; Abidi, S.H. CMV and EBV Co-Infection in HIV-Infected Children: Infection Rates and Analysis of Differential Expression of Cytokines in HIV Mono- and HIV–CMV–EBV Co-Infected Groups. Viruses 2022, 14, 1823. https://doi.org/10.3390/v14081823
Nazim F, Kayani HA, Ali Nathwani A, Mir F, Abidi SH. CMV and EBV Co-Infection in HIV-Infected Children: Infection Rates and Analysis of Differential Expression of Cytokines in HIV Mono- and HIV–CMV–EBV Co-Infected Groups. Viruses. 2022; 14(8):1823. https://doi.org/10.3390/v14081823
Chicago/Turabian StyleNazim, Fizza, Hammad Afzal Kayani, Apsara Ali Nathwani, Fatima Mir, and Syed Hani Abidi. 2022. "CMV and EBV Co-Infection in HIV-Infected Children: Infection Rates and Analysis of Differential Expression of Cytokines in HIV Mono- and HIV–CMV–EBV Co-Infected Groups" Viruses 14, no. 8: 1823. https://doi.org/10.3390/v14081823
APA StyleNazim, F., Kayani, H. A., Ali Nathwani, A., Mir, F., & Abidi, S. H. (2022). CMV and EBV Co-Infection in HIV-Infected Children: Infection Rates and Analysis of Differential Expression of Cytokines in HIV Mono- and HIV–CMV–EBV Co-Infected Groups. Viruses, 14(8), 1823. https://doi.org/10.3390/v14081823







