Human Papillomavirus Detected in Oropharyngeal Cancers from Chilean Subjects
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Collection
2.2. DNA Extraction, HPV Detection and Genotyping
2.3. Tissue Microarray (TMA) Construction and p16 Immunohistochemistry
2.4. RNA Purification and Transcriptase-Reverse PCR
2.5. Statistical Analysis
3. Results
3.1. Clinical Pathological Characteristics
3.2. HPV Detection and Genotyping
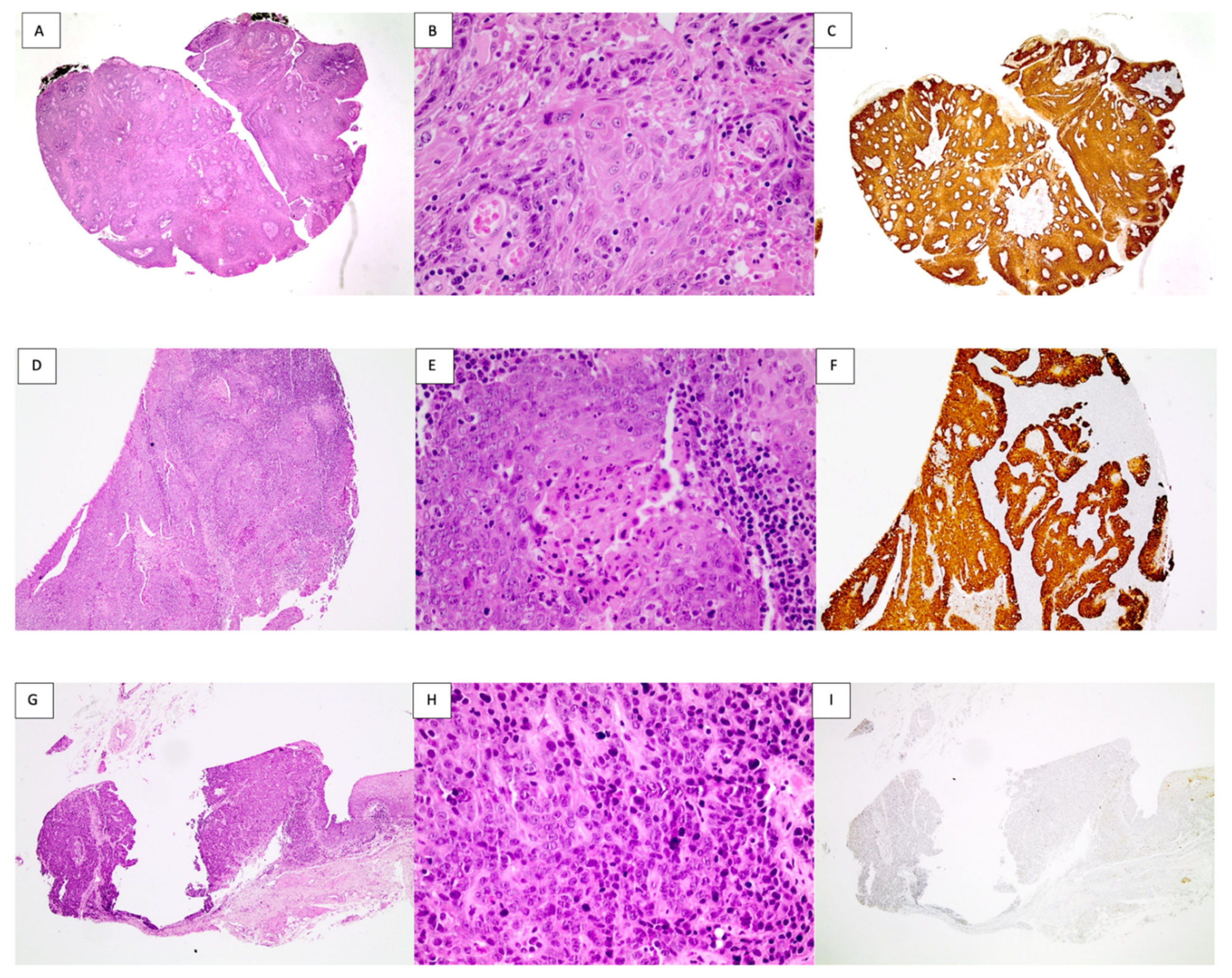
3.3. p16 Immunohistochemistry
3.4. E6/E7 Transcripts in OPSCCs
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Castellsagué, X.; Alemany, L.; Quer, M.; Halec, G.; Quirós, B.; Tous, S.; Clavero, O.; Alòs, L.; Biegner, T.; Szafarowski, T.; et al. HPV Involvement in Head and Neck Cancers: Comprehensive Assessment of Biomarkers in 3680 Patients. J. Natl. Cancer Inst. 2016, 108, djv403. [Google Scholar] [CrossRef] [PubMed]
- Mehanna, H.; Beech, T.; Nicholson, T.; El-Hariry, I.; McConkey, C.; Paleri, V.; Roberts, S. Prevalence of human papillomavirus in oropharyngeal and nonoropharyngeal head and neck cancer—Systematic review and meta-analysis of trends by time and region. Head Neck 2013, 35, 747–755. [Google Scholar] [CrossRef] [PubMed]
- Stein, A.P.; Saha, S.; Yu, M.; Kimple, R.J.; Lambert, P.F. Prevalence of human papillomavirus in oropharyngeal squamous cell carcinoma in the United States across time. Chem. Res. Toxicol. 2014, 27, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Gillison, M.L.; Chaturvedi, A.K.; Anderson, W.F.; Fakhry, C. Epidemiology of Human Papillomavirus-Positive Head and Neck Squamous Cell Carcinoma. J. Clin. Oncol. 2015, 33, 3235–3242. [Google Scholar] [CrossRef] [PubMed]
- Mallen-St Clair, J.; Alani, M.; Wang, M.B.; Srivatsan, E.S. Human papillomavirus in oropharyngeal cancer: The changing face of a disease. Biochim. Biophys. Acta 2016, 1866, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, A.L.; Caodaglio, A.S.; Sichero, L. Regulation of HPV transcription. Clinics 2018, 73, e486s. [Google Scholar] [CrossRef]
- Gheit, T. Mucosal and Cutaneous Human Papillomavirus Infections and Cancer Biology. Front. Oncol. 2019, 9, 355. [Google Scholar] [CrossRef]
- De Martel, C.; Plummer, M.; Vignat, J.; Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 2017, 141, 664–670. [Google Scholar] [CrossRef]
- Goodman, M.T.; Saraiya, M.; Thompson, T.D.; Steinau, M.; Hernandez, B.Y.; Lynch, C.F.; Lyu, C.W.; Wilkinson, E.J.; Tucker, T.; Copeland, G.; et al. Human papillomavirus genotype and oropharynx cancer survival in the United States of America. Eur. J. Cancer 2015, 51, 2759–2767. [Google Scholar] [CrossRef]
- Husain, N.; Neyaz, A. Human papillomavirus associated head and neck squamous cell carcinoma: Controversies and new concepts. J. Oral. Biol. Craniofac. Res. 2017, 7, 198–205. [Google Scholar] [CrossRef]
- Gillison, M.L.; Castellsagué, X.; Chaturvedi, A.; Goodman, M.T.; Snijders, P.; Tommasino, M.; Arbyn, M.; Franceschi, S. Eurogin Roadmap: Comparative epidemiology of HPV infection and associated cancers of the head and neck and cervix. Int. J. Cancer 2014, 134, 497–507. [Google Scholar] [CrossRef] [PubMed]
- Hübbers, C.U.; Akgül, B. HPV and cancer of the oral cavity. Virulence 2015, 6, 244–248. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Dong, Y. Human papillomavirus and oral squamous cell carcinoma: A review of HPV-positive oral squamous cell carcinoma and possible strategies for future. Curr. Probl. Cancer 2017, 41, 323–327. [Google Scholar] [CrossRef]
- Wittekindt, C.; Wuerdemann, N.; Gattenlöhner, S.; Brobeil, A.; Wierzbicka, M.; Wagner, S.; Klußmann, J.P. The role of high-risk human papillomavirus infections in laryngeal squamous cell carcinoma. Eur. Arch. Otorhinolaryngol. 2017, 274, 3837–3842. [Google Scholar] [CrossRef] [PubMed]
- Fusconi, M.; Campo, F.; Gallo, A.; Zambetti, G.; Martellucci, S.; Seccia, A.; de Vincentiis, M. Laryngeal Cancer, HPV DNA vs E6/E7 mRNA Test: A Systematic Review. J. Voice 2017, 31, e241–e248. [Google Scholar] [CrossRef] [PubMed]
- Cohen, E.; Coviello, C.; Menaker, S.; Martinez-Duarte, E.; Gomez, C.; Lo, K.; Kerr, D.; Franzmann, E.; Leibowitz, J.; Sargi, Z. P16 and human papillomavirus in sinonasal squamous cell carcinoma. Head Neck 2020, 42, 2021–2029. [Google Scholar] [CrossRef]
- Jiromaru, R.; Yamamoto, H.; Yasumatsu, R.; Hongo, T.; Nozaki, Y.; Hashimoto, K.; Taguchi, K.; Masuda, M.; Nakagawa, T.; Oda, Y. HPV-related Sinonasal Carcinoma: Clinicopathologic Features, Diagnostic Utility of p16 and Rb Immunohistochemistry, and EGFR Copy Number Alteration. Am. J. Surg. Pathol. 2020, 44, 305–315. [Google Scholar] [CrossRef]
- Sharma, A.; Tang, A.L.; Takiar, V.; Wise-Draper, T.M.; Langevin, S.M. Human Papillomavirus and Survival of Sinonasal Squamous Cell Carcinoma Patients: A Systematic Review and Meta-Analysis. Cancers 2021, 13, 1410. [Google Scholar] [CrossRef]
- Mittal, S.; Banks, L. Molecular mechanisms underlying human papillomavirus E6 and E7 oncoprotein-induced cell transformation. Mutat. Res./Rev. Mutat. Res. 2017, 772, 23–35. [Google Scholar] [CrossRef]
- Paver, E.C.; Currie, A.M.; Gupta, R.; Dahlstrom, J.E. Human papilloma virus related squamous cell carcinomas of the head and neck: Diagnosis, clinical implications and detection of HPV. Pathology 2020, 52, 179–191. [Google Scholar] [CrossRef]
- De Roda Husman, A.M.; Walboomers, J.M.; van den Brule, A.J.; Meijer, C.J.; Snijders, P.J. The use of general primers GP5 and GP6 elongated at their 3’ ends with adjacent highly conserved sequences improves human papillomavirus detection by PCR. J. Gen. Virol. 1995, 76, 1057–1062. [Google Scholar] [CrossRef] [PubMed]
- Togawa, K.; Rustgi, A.K. A novel human papillomavirus sequence based on L1 general primers. Virus Res. 1995, 36, 293–297. [Google Scholar] [CrossRef]
- Gharizadeh, B.; Kalantari, M.; Garcia, C.A.; Johansson, B.; Nyrén, P. Typing of human papillomavirus by pyrosequencing. Lab. Investig. 2001, 81, 673–679. [Google Scholar] [CrossRef]
- Lewis, J.S.; Beadle, B.; Bishop, J.A.; Chernock, R.D.; Colasacco, C.; Lacchetti, C.; Moncur, J.T.; Rocco, J.W.; Schwartz, M.R.; Seethala, R.R.; et al. Human Papillomavirus Testing in Head and Neck Carcinomas: Guideline From the College of American Pathologists. Arch. Pathol. Lab. Med. 2018, 142, 559–597. [Google Scholar] [CrossRef] [PubMed]
- Aedo-Aguilera, V.; Carrillo-Beltrán, D.; Calaf, G.M.; Muñoz, J.P.; Guerrero, N.; Osorio, J.C.; Tapia, J.C.; León, O.; Contreras, H.R.; Aguayo, F. Curcumin decreases epithelial-mesenchymal transition by a Pirin-dependent mechanism in cervical cancer cells. Oncol. Rep. 2019, 42, 2139–2148. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.H.; O’Sullivan, B. Overview of the 8th Edition TNM Classification for Head and Neck Cancer. Curr. Treat. Options Oncol. 2017, 18, 40. [Google Scholar] [CrossRef]
- Ang, K.K.; Harris, J.; Wheeler, R.; Weber, R.; Rosenthal, D.I.; Nguyen-Tan, P.F.; Westra, W.H.; Chung, C.H.; Jordan, R.C.; Lu, C.; et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N. Engl. J. Med. 2010, 363, 24–35. [Google Scholar] [CrossRef]
- Oliveira, A.C.; Cavalcanti de Lima, I.C.; Frez Marques, V.M.; Alves de Araújo, W.H.; de Campos Ferreira, C. Human papillomavirus prevalence in oral and oropharyngeal squamous cell carcinoma in South America: A systematic review and meta-analysis. Oncol. Rev. 2022, 16, 552. [Google Scholar] [CrossRef]
- De Cicco, R.; de Melo Menezes, R.; Nicolau, U.R.; Pinto, C.A.L.; Villa, L.L.; Kowalski, L.P. Impact of human papillomavirus status on survival and recurrence in a geographic region with a low prevalence of HPV-related cancer: A retrospective cohort study. Head Neck 2020, 42, 93–102. [Google Scholar] [CrossRef]
- Barros-Filho, M.C.; Reis-Rosa, L.A.; Hatakeyama, M.; Marchi, F.A.; Chulam, T.; Scapulatempo-Neto, C.; Nicolau, U.R.; Carvalho, A.L.; Pinto, C.A.L.; Drigo, S.A.; et al. Oncogenic drivers in 11q13 associated with prognosis and response to therapy in advanced oropharyngeal carcinomas. Oral. Oncol. 2018, 83, 81–90. [Google Scholar] [CrossRef]
- Betiol, J.C.; Sichero, L.; Costa, H.O.O.; de Matos, L.L.; Andreoli, M.A.; Ferreira, S.; Faraj, S.F.; de Mello, E.S.; Sobrinho, J.S.; Brandão, L.G.; et al. Prevalence of human papillomavirus types and variants and p16(INK4a) expression in head and neck squamous cells carcinomas in São Paulo, Brazil. Infect. Agent. Cancer 2016, 11, 20. [Google Scholar] [CrossRef] [PubMed]
- Buexm, L.A.; Soares-Lima, S.C.; Brennan, P.; Fernandes, P.V.; de Souza Almeida Lopes, M.; Nascimento de Carvalho, F.; Santos, I.C.; Dias, L.F.; de Queiroz Chaves Lourenço, S.; Ribeiro Pinto, L.F. Hpv impact on oropharyngeal cancer patients treated at the largest cancer center from Brazil. Cancer Lett. 2020, 477, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Reyes, M.; Rojas-Alcayaga, G.; Pennacchiotti, G.; Carrillo, D.; Muñoz, J.P.; Peña, N.; Montes, R.; Lobos, N.; Aguayo, F. Human papillomavirus infection in oral squamous cell carcinomas from Chilean patients. Exp. Mol. Pathol. 2015, 99, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Dahlstrom, K.R.; Bell, D.; Hanby, D.; Li, G.; Wang, L.E.; Wei, Q.; Williams, M.D.; Sturgis, E.M. Socioeconomic characteristics of patients with oropharyngeal carcinoma according to tumor HPV status, patient smoking status, and sexual behavior. Oral. Oncol. 2015, 51, 832–838. [Google Scholar] [CrossRef] [PubMed]
- Lechner, M.; Liu, J.; Masterson, L.; Fenton, T.R. HPV-associated oropharyngeal cancer: Epidemiology, molecular biology and clinical management. Nat. Rev. Clin. Oncol. 2022, 19, 306–327. [Google Scholar] [CrossRef]
- Lewis, J.S. Morphologic diversity in human papillomavirus-related oropharyngeal squamous cell carcinoma: Catch Me If You Can! Mod. Pathol. 2017, 30, S44–S53. [Google Scholar] [CrossRef][Green Version]
- Menezes, F.D.S.; Latorre, M.D.R.D.; Conceição, G.M.S.; Curado, M.P.; Antunes, J.L.F.; Toporcov, T.N. The emerging risk of oropharyngeal and oral cavity cancer in HPV-related subsites in young people in Brazil. PLoS ONE 2020, 15, e0232871. [Google Scholar] [CrossRef]
- Mazul, A.L.; Colditz, G.A.; Zevallos, J.P. Factors associated with HPV testing in oropharyngeal cancer in the National Cancer Data Base from 2013 to 2015. Oral. Oncol. 2020, 104, 104609. [Google Scholar] [CrossRef]
- Gilles, C.; Piette, J.; Peter, W.; Fusenig, N.E.; Foidart, J.M. Differentiation ability and oncogenic potential of HPV-33- and HPV-33 + ras-transfected keratinocytes. Int. J. Cancer 1994, 58, 847–854. [Google Scholar] [CrossRef]
- Kovacevic, G.; Milosevic, V.; Knezevic, P.; Knezevic, A.; Knezevic, I.; Radovanov, J.; Nikolic, N.; Patic, A.; Petrovic, V.; Hrnjakovic Cvjetkovic, I.; et al. Prevalence of oncogenic Human papillomavirus and genetic diversity in the L1 gene of HPV16 HPV 18 HPV31 and HPV33 found in women from Vojvodina Province Serbia. Biologicals 2019, 58, 57–63. [Google Scholar] [CrossRef]
- Melo, A.; Montenegro, S.; Hooper, T.; Capurro, I.; Roa, J.C.; Roa, I. Human papilloma virus (HPV) typing in preneoplastic and neoplastic lesions of the uterine cervix in the IX region-Chile. Rev. Med. Chile 2003, 131, 1382–1390. [Google Scholar] [PubMed]
- Sichero, L.; Sobrinho, J.S.; Villa, L.L. Oncogenic potential diverge among human papillomavirus type 16 natural variants. Virology 2012, 432, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Hochmann, J.; Sobrinho, J.S.; Villa, L.L.; Sichero, L. The Asian-American variant of human papillomavirus type 16 exhibits higher activation of MAPK and PI3K/AKT signaling pathways, transformation, migration and invasion of primary human keratinocytes. Virology 2016, 492, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Abdelhakam, D.A.; Huenerberg, K.A.; Nassar, A. Utility of p16 and HPV testing in oropharyngeal squamous cell carcinoma: An institutional review. Diagn. Cytopathol. 2021, 49, 54–59. [Google Scholar] [CrossRef]
- You, E.L.; Henry, M.; Zeitouni, A.G. Human papillomavirus-associated oropharyngeal cancer: Review of current evidence and management. Curr. Oncol. 2019, 26, 119–123. [Google Scholar] [CrossRef]
- Liyanage, C.; Wathupola, A.; Muraleetharan, S.; Perera, K.; Punyadeera, C.; Udagama, P. Promoter Hypermethylation of Tumor-Suppressor Genes. Biomolecules 2019, 9, 148. [Google Scholar] [CrossRef]
- Wu, C.L.; Roz, L.; McKown, S.; Sloan, P.; Read, A.P.; Holland, S.; Porter, S.; Scully, C.; Paterson, I.; Tavassoli, M.; et al. DNA studies underestimate the major role of CDKN2A inactivation in oral and oropharyngeal squamous cell carcinomas. Genes Chromosomes Cancer 1999, 25, 16–25. [Google Scholar] [CrossRef]
- Grønhøj Larsen, C.; Gyldenløve, M.; Jensen, D.H.; Therkildsen, M.H.; Kiss, K.; Norrild, B.; Konge, L.; von Buchwald, C. Correlation between human papillomavirus and p16 overexpression in oropharyngeal tumours: A systematic review. Br. J. Cancer 2014, 110, 1587–1594. [Google Scholar] [CrossRef]
- LaPak, K.M.; Burd, C.E. The molecular balancing act of p16(INK4a) in cancer and aging. Mol. Cancer Res. 2014, 12, 167–183. [Google Scholar] [CrossRef]
- Prigge, E.S.; Arbyn, M.; von Knebel Doeberitz, M.; Reuschenbach, M. Diagnostic accuracy of p16. Int. J. Cancer 2017, 140, 1186–1198. [Google Scholar] [CrossRef]
- Chung, C.H.; Zhang, Q.; Kong, C.S.; Harris, J.; Fertig, E.J.; Harari, P.M.; Wang, D.; Redmond, K.P.; Shenouda, G.; Trotti, A.; et al. p16 protein expression and human papillomavirus status as prognostic biomarkers of nonoropharyngeal head and neck squamous cell carcinoma. J. Clin. Oncol. 2014, 32, 3930–3938. [Google Scholar] [CrossRef] [PubMed]

| Anatomical Site | |||||
|---|---|---|---|---|---|
| Features | Palatine Tonsils N (%) | Tongue Base N (%) | Soft Palate N (%) | Total | p-Value |
| Gender | p = 0.85 | ||||
| Female | 9 (50) | 6 (33.33) | 3 (16.66) | 18 | |
| Male | 17 (54.38) | 8 (25.8) | 6 (19.35) | 31 | |
| Age | p = 0.3035 | ||||
| ≤65 years | 18 (62.07) | 7 (24.24) | 4 (13.79) | 29 | |
| >65 years | 8 (40) | 7 (35) | 5 (25) | 20 | |
| Keratinization | p = 0.2115 | ||||
| Keratinized | 15 (45.45) | 10 (30.3) | 8 (24.24) | 33 | |
| Non-Keratinized | 11 (68.75) | 4 (25) | 1 (6.25) | 16 | |
| Differentation | p = 0.0323 * | ||||
| Poor | 17 (69.56) | 5 (21.73) | 2 (8.26) | 23 | |
| Moderate | 8 (47%) | 4 (23.52) | 5 (29.41) | 17 | |
| Well | 1 (12.5) | 5 (62.5) | 2 (25) | 8 | |
| p16 IHC | p < 0.0001 *** | ||||
| Positive | 22 (78.57) | 5 (17.85) | 1 (3.57) | 28 | |
| Negative | 3 (15) | 9 (45) | 8 (40) | 20 | |
| Variable | Number of Cases (%) | |
|---|---|---|
| HPV Presence | HPV-Negative | 19 (38.8) |
| HPV-Positive | 30 (61.2) | |
| Oncogenic Risk | Low | 3 (10) |
| High | 27 (90) | |
| Genotype | HPV6 | 3 (10) |
| HPV16 | 24 (80) | |
| HVP18 | 1 (3.3) | |
| HVP33 | 2 (6.7) |
| Feature | HPV Presence | |||
|---|---|---|---|---|
| HPV-Negative | HPV-Positive | Total | p-Value | |
| Gender | p = 0.24 | |||
| Female | 9 (50) | 9 (50) | 18 | |
| Male | 10 (32.25) | 21 (67.74) | 31 | |
| Age | p = 0.3759 | |||
| ≤65 years | 9 (32.14) | 19 (67.85) | 28 | |
| >65 years | 9 (45) | 11 (55) | 20 | |
| Smoking Status | p = 0.95 | |||
| Never | 4 (33,33) | 8 (66,77) | 12 | |
| Former | 2 (40) | 3 (60) | 5 | |
| Currently | 5 (33,33) | 10 (66,77) | 15 | |
| Keratinization | p = 0.11 | |||
| Keratinized | 16 (47.06) | 18 (52.94) | 34 | |
| Non-keratinized | 3 (20) | 12 (80) | 15 | |
| Differentiation | p = 0.029 * | |||
| Poor | 7 (29.17) | 17 (70.83) | 24 | |
| Moderate | 5 (31.25) | 11 (68.75) | 16 | |
| Well | 7 (77.77) | 2 (22.22) | 9 | |
| Anatomical Site | p = 0.19 | |||
| Palatine tonsils | 7 (26.92) | 19 (73.07) | 26 | |
| Tongue base | 7 (50) | 7 (50) | 14 | |
| Soft palate | 5 (55.55) | 4 (44.44) | 9 | |
| p16 IHC | p = 0.0004 *** | |||
| Positive | 5 (17.85) | 23 (82.14) | 28 | |
| Negative | 14 (70) | 6 (30) | 20 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliva, C.; Carrillo-Beltrán, D.; Boettiger, P.; Gallegos, I.; Aguayo, F. Human Papillomavirus Detected in Oropharyngeal Cancers from Chilean Subjects. Viruses 2022, 14, 1212. https://doi.org/10.3390/v14061212
Oliva C, Carrillo-Beltrán D, Boettiger P, Gallegos I, Aguayo F. Human Papillomavirus Detected in Oropharyngeal Cancers from Chilean Subjects. Viruses. 2022; 14(6):1212. https://doi.org/10.3390/v14061212
Chicago/Turabian StyleOliva, Carolina, Diego Carrillo-Beltrán, Paul Boettiger, Iván Gallegos, and Francisco Aguayo. 2022. "Human Papillomavirus Detected in Oropharyngeal Cancers from Chilean Subjects" Viruses 14, no. 6: 1212. https://doi.org/10.3390/v14061212
APA StyleOliva, C., Carrillo-Beltrán, D., Boettiger, P., Gallegos, I., & Aguayo, F. (2022). Human Papillomavirus Detected in Oropharyngeal Cancers from Chilean Subjects. Viruses, 14(6), 1212. https://doi.org/10.3390/v14061212






