Abstract
The Schlafen gene family encodes for proteins involved in various biological tasks, including cell proliferation, differentiation, and T cell development. Schlafens were initially discovered in mice, and have been studied in the context of cancer biology, as well as their role in protecting cells during viral infection. This protein family provides antiviral barriers via direct and indirect effects on virus infection. Schlafens can inhibit the replication of viruses with both RNA and DNA genomes. In this review, we summarize the cellular functions and the emerging relationship between Schlafens and innate immunity. We also discuss the functions and distinctions of this emerging family of proteins as host restriction factors against viral infection. Further research into Schlafen protein function will provide insight into their mechanisms that contribute to intrinsic and innate host immunity.
1. Introduction
In 1998, the Schlafen (SLFN for humans; Slfn for mice) gene was first reported in the study of murine thymus development. The first Schlafens discovered were the murine genes Slfn1–4. When Slfn1 is expressed ectopically in NIH-3T3 fibroblasts, it induces G0/G1 cell cycle arrest; this observation led to the coining of the term “schlafen” from the German word meaning “to sleep” [1]. Later research found that Schlafens play roles in a variety of cellular functions, including anti-proliferation and cell differentiation [2,3,4,5,6,7], cancer cell migration, proliferation and invasion prevention [8,9,10,11], sensitization of cancer cells to DNA-damaging drugs [12,13,14,15,16,17], and inhibition of viral replication [18,19,20,21,22,23,24]. As studies on the Schlafen family have expanded in recent years, substantial progress has been achieved towards understanding how the proteins in this family have distinct functions. Excellent recent review articles have described their significance for the field of cancer biology [25]. The Schlafen proteins also have roles in controlling viruses and the host immune system. Here, we address the functional similarities and differences amongst Schlafen family members in terms of their roles in regulating virological and immunological features. These recent findings provide inspiration for future research directions into this emerging protein family.
2. Schlafen Family Members and Protein Composition
Schlafen gene family members are highly homologous across many mammalian species. Nine Schlafen proteins are expressed in mice from chromosome 11, and six have been found in humans from chromosome 17 (Figure 1) [3,26]. Despite the fact that Slfn-like 1 (Slfn1L) is expressed on mouse chromosome 4, there is an opinion that it is not considered a ‘bona fide’ Schlafen family member due to the extremely low similarity to Slfn genes [26,27]. In addition, Slfn6 and Slfn7 are considered to be sequences derived from either Slfn3 or Slfn4 isoforms or other mouse paralogues [1,27].
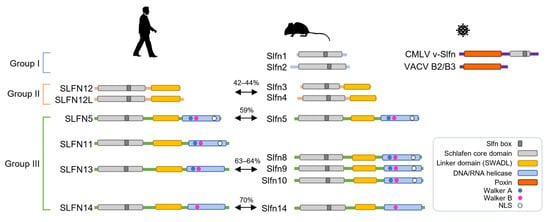
Figure 1.
A comparison of the linear domain structures of the Schlafen family members. The domains of Schlafens in humans, mice, and viruses are depicted. The percentage of sequence identity between orthologous proteins is indicated. Walker A and Walker B motifs are located within the C-terminal helicase domain of some group III Schlafens. NLS, nuclear localization signal.
Schlafen members fall into three distinct groups, each with its unique set of characteristics and functions (Figure 1). Group I has a divergent AAA ATPase-associated domain containing a common Slfn-box region that has been termed the Schlafen core domain, and is shared with the other two groups [2,28,29,30,31]. The Schlafen core domain is horseshoe-shaped and contains zinc finger motifs that are highly conserved in all members of the Schlafen family proteins. Groups II and III contain an additional linker domain following the Schlafen core domain, which harbors the SWADL motif defined by the amino acid sequence pattern S-W-(A/S)-(V/G/L)-D-(L/I/V) with unknown function [3,29]. Only group III proteins feature an extended carboxyl (C)-terminal domain that matches superfamily I of DNA/RNA helicases [2]. The Schlafen core domain lacks the Walker motif. The Walker A and B represent structural motifs for nucleotide binding, and were discovered in the AAA family of ATPases [32]. Due to the absence of Walker motifs, Schlafen proteins in groups I and II may lack ATPase activity. Putative DNA/RNA helicase domains of some group III Schlafen members have AAA domains with Walker motifs that appear to be enzymatically functional [18,33,34]. These are incomplete in murine and human Schlafen 14, which possess only the Walker B motif [31]. In addition, the C-terminal extension of some group III Schlafens possesses a nuclear localization signal (NLS) and may have nuclear functions (Figure 1) [20,24,25].
Except for the platypus, a monotreme, the Schlafen family is found in practically all mammals. Sequences similar to Schlafen genes were discovered in the amphibian Xenopus laevis and the fish species Callorhincuys milii, but not in any other non-mammalian organism. Interestingly, sequences similar to Schlafens have been found by bioinformatic analysis of genomes for orthopoxvirus (OPV), such as vaccinia, variola (smallpox), and cowpox viruses [1]. Subsequent sequencing of the camelpox virus (CMLV) identified another Schlafen-like protein called 176R. This protein consists of 502 amino acids and has a C-terminal sequence that is comparable to the Schlafen core domain of murine Schlafens. Some of these viral Schlafen (v-Slfn) genes retain an entire open reading frame (ORF). While the ORF for v-Slfn is intact in the genomes of camelpox, monkeypox, cowpox, mousepox, and taterapox viruses, protein expression is restricted in other OPVs, such as the vaccinia virus (VACV), due to ORF fragmentation [1,26,35]. Sequences of v-Slfn were found to be similar to the mouse and rat group I Schlafen, but lack the C-terminal domain. This implies that, while the progenitor virus of OPV may have acquired an intact Schlafen from rodents, the ORF was fragmented due to mutations acquired over time [26,27].
3. Regulated Expression of Schlafens in the Immune System
Schlafen family members have been revealed to be induced by several stimuli, including CpG-DNA [36], LPS [36,37,38], and pathogens, such as Brucella, Listeria [39], and rhinovirus [37]. Type I IFN and IFN receptors have been implicated in the induction of Schlafen genes, implying that Schlafens are IFN-stimulated genes (ISGs). In 2010, it was first reported that IFNα influences the expression of members of the Schlafen gene family [40]. The data presented in this study reveal that type I IFN is a potent inducer of numerous mouse Schlafen family members, including members of group I (Slfn1 and Slfn2), group II (Slfn3), and group III (Slfn5 and Slfn8). IFN-activated Stat proteins and p38 MAP kinase operated differently in their regulation of interferon-induced expression [41]. In Stat1 deletion in mouse embryonic fibroblasts, IFN-dependent expression of all Schlafen genes was reduced relative to parental cells, ranging from a partial reduction in Slfn3 to total transcriptional defects in Slfn1, 2, 5, and 8. Interestingly, Slfn5 expression was completely independent of Stat3, but it was increased in Stat3 knockout cells. The function of p38 MAPK-activated signaling cascades is required for the complete transcriptional activation of ISGs. However, while p38 MAPK is required for IFN-dependent expression of Schlafen genes in groups I and II, interestingly, group III gene expression is not dependent on p38 MAPK. In the absence of p38 MAPK, IFN-dependent mRNA expression of Slfn1, Slfn2, and to a lesser extent Slfn3, was suppressed. The group III Schlafen genes, SLFN5 and SLFN8, on the other hand, were induced by IFN in a p38 MAPK-independent manner [41]. Notably, neither Stat3 nor p38 MAPK was necessary for Slfn5 induction, indicating that alternative regulatory mechanisms are involved in this process.
The induction of ISGs by type I IFNs requires the presence of interferon-stimulated response elements (ISREs) in the promoter region of the ISG, which enables transcriptional activation via the binding of the ISGF3 transcription factor, a complex of phosphorylated STAT1/STAT2 heterodimers, and IRF9 [42]. The inducibility of Schlafens by IFNα or IFN stimuli was lower than for MxA, a conventional ISG [37]. Analysis of transcription factor binding sites using the MatInspector program [43] showed that MxA has six ISRE sites, whereas most human Schlafen genes have just one canonical ISRE [37]. Although the Schlafen family belongs to the group of classical ISGs regulated by the STAT complex, some Schlafens are expressed through the noncanonical IFN pathways or undefined mechanisms. Considerable levels of Schlafens are expressed in various cells, including primary fibroblasts and malignant cancer cells, in the absence of IFN activation [18,20,44]. The sensitivity of Schlafen expression to IFN varies according to cell type. For example, SLFN5 expression is suppressed in malignant melanoma compared to normal melanocytes. IFNα stimulation, on the other hand, significantly increased SLFN5 expression, whereas SLFN11, SLFN12, SLFN13 were not affected [40]. In contrast, IFN stimulants, such as poly I:C and 5′ ppp-dsRNA, increased Slfn5 expression slightly, but not significantly, in mouse macrophage RAW 264.7 cells, whereas Slfn14 expression was significantly increased [19].
In the 5′-flanking region of the Slfn2 gene, one copy of a putative NF-κB binding site and two copies of AP-1 binding sequences are found. It has been demonstrated that CpG-DNA and LPS treatment of macrophages requires the functional interaction of NF-κB and AP1 within the promoter element [36]. Scanning the promoter region of Slfn4 with JASPAR (jaspar.cgb.ki.se) revealed the presence of AP1 and PU. 1 binding sequences, as well as two copies of IFN response elements STAT1 and IRF1 binding sequences [38]. In addition, a Gli1 binding site also exists within the promoter. Gli1, a Hedgehog signaling effector, is required for the activation of the Slfn4 promoter, which means that the role of Slfn4 is critical in the appearance of macrophages expressing IL1β or TNFα [45]. In cancer cells, epigenetic inhibition of gene expression via CpG promoter island hypermethylation is a frequent occurrence [46]. Several studies have reported hypermethylation of the SLFN11 gene promoter [14,46,47,48,49]. The silencing of SLFN11 by promoter CpG island hypermethylation is linked to a greater resistance to platinum compounds for cancer chemotherapy [14]. Hypermethylation of a CpG promoter island inactivates SLFN11 gene expression. This methylation is catalyzed by two main DNA methyltransferases, DNMT1 and DNMT3B [14]. The fact that DNMT3B expression in monocytes is very low, or barely detectable [50], may imply that elevated levels of SLFN11 expression in monocytes are related to hypermethylation. It is also known from germinal center B cell differentiation studies that histone modifiers, such as EZH2 and HDACs, regulate epigenetic expression of SLFN11 [48]. In addition, SLFN11 expression and the B cell lineage-specific repressor PAX5 have been shown to have a nearly perfect inverse correlation [48]. A potential PAX5 binding site (GCGTGAC) exists in the promoter region of SLFN11, suggesting that PAX5 may be one of the repressors of SLFN11 in B cells.
The Schlafen members are expressed at different phases of thymocyte development and peripheral T cell activation in mice. Slfn1 and Slfn2 are drastically elevated during the transition from CD4 and CD8 double-positive to single-positive maturation stages. However, expression levels of both genes decrease after T cell activation [1,2,51]. Slfn3 is highly expressed in single-positive T cells throughout thymocyte development. Slfn3 is also expressed at a higher level in natural CD4+ CD25+ regulatory T cells than in CD4+ CD25− cells. Slfn3 expression is increased in CD4+ CD25- T cells upon activation, but decreased in CD4+ CD25+ T cells following activation with anti-CD3/CD28 stimulation. TGF-β stimulation also decreases Slfn3 expression in the CD4+ T cell subset, suggesting that Slfn3 may be a novel marker of T cell activation [52]. Slfn4 is detected early and decreased during thymocyte development, showing the opposite phenomenon to Slfn1 [1,2]. Slfn4 mRNA levels are upregulated during macrophage activation, whereas they are downregulated throughout differentiation. Myelopoiesis is disrupted by constitutive Slfn4 expression in the myeloid lineage, implying that downregulation of Slfn4 gene expression during macrophage differentiation is critical, and Slfn4 may act as a modulator of this lineage [38]. Unlike the other groups, Slfn5, 8, 9, and 10 in group III do not change quantitatively during thymocyte development. During T cell activation, however, there was a significant downregulation of Slfn5 and Slfn8 expression, while Slfn9 expression increased and Slfn10 expression remained relatively constant [2]. Since SLFN14 is expressed at an exceedingly low level in T cells, it is unlikely to be linked to T cell fate [37].
The human Schlafen family is also associated with immune cell proliferation and T cell maturation. With the exception of SLFN14, all human Schlafen proteins are expressed natively in monocytes, monocyte-derived dendritic cells (moDCs), and T cells [37]. The expression levels of SLFN5 in T cells, and SLFN11 in monocytes and moDCs, are notably high. The expression of SLFN5 and SLFN11 changes slightly throughout moDC differentiation. The expression of SLFN12L and SLFN13 is relatively modest in monocytes at rest, but appears to be elevated during differentiation into moDCs, whereas SLFN12 expression is markedly reduced [37]. Thus, the downregulation and upregulation of each Schlafen family protein may represent distinct requirements for these proteins in moDC function.
It is intriguing that there appears to be a regulatory feedback mechanism for transcriptional control within the Schlafen family [53]. The loss of Slfn3 by knockout decreases Slfn4, Slfn8, and Slfn9 expression in the ileal mucosa, while increasing Slfn1 and Slfn5. In addition, Slfn3 deficiency decreases Slfn4 expression and increases Slfn8 and Slfn9 expression in the thymus and spleen, where immune cells mature and/or proliferate [53]. The promoters of all members of the Schlafen family contain regions for binding of the Kruppel-like factor-6 (KLF6) transcription factor. The NFAT-related factors ING4, ZNF333, and KLF4, are also predicted to bind to most Schlafen promoters. These transcription factors from the KLF family play different roles in gastrointestinal cell differentiation and proliferation, and have different expression patterns [54]. This suggests that members of the KLF and Schlafen families may have feedback loops that act as regulators of gastrointestinal and immune cell fate in different ways [53].
4. Immunodeficiency of Schlafen Mutants
It has been observed that the Elektra mutant is a homozygous mutation of murine Slfn2, and confers vulnerability to viral and bacterial infections [55]. The mortality rate of mice after murine cytomegalovirus (MCMV) infection was significantly high compared to that of the wild-type control mice [55]. In mice with the Elektra phenotype, CD8+ and CD4+ T lymphocytes fail to expand. When compared to the wild-type cells, these cells had a higher rate of apoptosis. In response to T cell activation signals, this mutation is thought to cause apoptosis [9]. Elektra mice also showed a significantly lower level of T cells in response to infection with lymphocytic choriomeningitis virus. Elektra T cells, similar to recently activated T cells, fail to maintain cellular quiescence, and enter a post-mitotic phase. T cells lose their proliferation potential and die in response to proliferation/activation signals, resulting in reduced T cell populations in the Elektra mutant mice [9].
There have been reports of a patient with a large heterozygous loss of the SLFN11, SLFN12, and SLFN13 genes on chromosome 17 [56]. This patient was discovered to have substantial abnormalities in T cell proliferation and cell cycle regulation. Interestingly, the patient had upper thigh Merkel cell carcinoma, a kind of carcinoma associated with viral infection, and was regarded to be susceptible to cancer, having been diagnosed with T cell lymphoma. The patient’s blood and plasma had substantial Epstein–Barr virus and Torque teno virus DNA, indicating that the patient was vulnerable to viral infections. The patient had normal CD4+/CD8+ immune cell distribution and a typical distribution of naïve and memory cells, but had aberrant T cell proliferation and excessive T cell death [56].
Mutations in SLFN14 have been linked to macrothrombocytopenia and excessive bleeding [57,58,59,60,61]. In addition, platelet function is diminished in patients with these mutations [61]. This SLFN14 mutation presents a species-specific phenotype, with platelet abnormalities in humans and severe microcytic erythrocytosis in mice [62]. Thus, SLFN14 may be an essential player in mammalian hematopoiesis, and may play a role in determining platelet and erythroid lineage commitment in particular species. Furthermore, platelets are now known to have roles in a variety of innate and adaptive immunological responses, which goes far beyond the classic conception of platelets as only hemostatic and thrombolytic agents [63]. Therefore, it can be demonstrated that SLFN14 is profoundly implicated in immunological control through platelet formation and function regulation.
5. SLFN5 as an Innate Immune Signal Modulator
Although type I IFNs play an important role in host defense against pathogen infection, their production must be properly regulated to avoid inordinately harmful immune responses. Thus, negative regulators are essential for cells to recover from IFN signaling, since IFN production dysregulation leads to autoimmune disorders. Some ISGs have the ability to regulate pathways that impact their own expression, either positively or negatively. For example, ISG56 is associated with the adapter protein STING, and disrupts STING interaction with downstream molecules VISA/MAVS or TBK1, inhibiting virus-induced IRF3 activation, IFN-expression, and cellular antiviral responses. Another negative regulator is the ISG15 deconjugating protease ubiquitin-specific peptidase 18 (USP18). USP18 inhibits JAK-STAT signaling by interacting with IFNAR2 in a protease-independent manner [64].
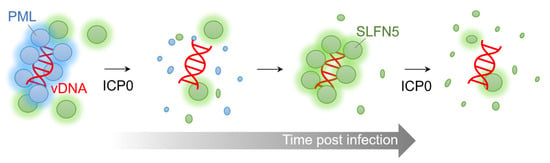
Human SLFN5 has been reported to be a negative regulator of IFN-induced gene transcription [65]. It was found that STAT1 is present as a complex that binds the SLFN5 protein in a type I IFN-dependent manner, and binds to the ISRE element in the promoter of ISGs. SLFN5 appears to serve as a repressor of STAT1-induced gene transcription through direct protein interaction. Consistent with this, it was demonstrated that SLFN5 is enriched on the promoters of type I IFN-inducible ISGs, where STAT1 binds. Microarray experiments revealed that SLFN5 knockout cells expressed more ISGs than wild-type cells, suggesting a potential role for SLFN5 in regulating STAT1-mediated type I IFN-induced transcriptional activation of ISGs [65]. Similarly, in human foreskin fibroblasts and HeLa cells, basal level ISG15, a well-known antiviral protein, increased due to SLFN5 depletion; additionally, a rapid induction of ISG15 protein expression by DNA viruses, such as human cytomegalovirus (HCMV), was observed [20]. Accordingly, SLFN5 appears to be a transcriptional repressor of IFN-gene transcription, as well as an IFN-stimulated response gene.
ZEB proteins are zinc-finger E homeobox-binding transcription factors best known for their role in driving epithelial-to-mesenchymal transition and metastasis in some cancers, including BRCA mutant cancer cells [66,67]. They are also widely expressed by immune cells, and regulate important transcriptional networks necessary for immune cell differentiation, maintenance, and function [68]. It has been found recently that human SLFN5 can inhibit ZEB1 transcription by directly binding to the SLFN5 binding motif on the ZEB1 promoter, thereby maintaining the epithelial cell morphology and inhibiting metastasis in BRCA mutant cancer cells [69,70]. SLFN5 increases PTEN by downregulating the transcription of ZEB1. Through the PTEN/PI3K/AKT/mTOR axis, an increase in PTEN inhibits lung adenocarcinoma growth and promotes apoptosis [47]. Although the SLFN5 interaction with the ZEB1 promoter in immune cells has not been validated, these reports suggest roles for SLFN5 as a multifunctional modulator of immune cells. Interestingly, SLFN12 inhibits ZEB1; however, unlike SLFN5, it is assumed to influence post-transcriptional regulation due to its cytoplasmic localization without the nuclear localization signal sequence. SLFN12 overexpression accelerated ZEB1 proteasome degradation and slowed ZEB1 translation in triple-negative breast cancer cells [9].
6. SLFN5, a Double-Edged Sword in IFN Therapy
Some malignancies can be treated with IFN therapy in combination with chemotherapy and radiation. Hematological malignancies and lymphomas can be treated with this therapeutic approach [71]. Recombinant IFNα2b is given to patients with recurrences of melanomas [72]. Hepatitis B and hepatitis C are treated with IFNα and other antiviral drugs, typically combined [73,74]. The anticancer effects of type I IFNs have become extensively recognized in recent decades, particularly their involvement in mediating interactions between tumors and the immune system.
In mouse malignant melanoma and renal cell carcinoma, IFNα promotes the expression of Slfn1, Slfn2, Slfn3, Slfn5, and Slfn8. The loss of Slfn2, Slfn4, or Slfn5 increased cell proliferation and anchorage-independent malignant growth, while decreasing the antiproliferative effect of IFN, implying crucial roles for Schlafens in tumorigenesis and neoplastic cell growth control [75]. All human Schlafen mRNA expression was induced in normal melanocytes by IFN therapy, while only SLFN5 was induced in malignant melanoma cells and renal cell carcinoma cells [8,40]. When melanoma cells are stimulated with IFN, SLFN5 expression is considerably increased, decreasing cancer cell proliferation. In contrast, the depletion of SLFN5 boosted the ability of melanomas to form colonies, even in the presence of IFN [40]. This suggests a potential role of SLFN5 in the anticancer effects of IFNα. However, SLFN5 also potentially reduces the anticancer effect of IFN in glioma cancer cells by transcriptionally co-repressing STAT1-mediated IFN responses, in contrast to its beneficial role in melanoma and renal cell carcinoma [65]. Decreasing SLFN5 leads to increased cellular susceptibility to IFN-induced antiproliferative responses in glioblastoma cells, implying that SLFN5 functions as a negative regulator of the IFN response in glioma cancer cells [65]. Thus, future therapeutic targeting of SLFN5 in malignancies may require precise analysis of other associated factors, and the design of therapeutic targeting of a particular tumor may be required for the selective targeting of SLFN5.
7. Functions of Viral Schlafen
The presence of intact v-Slfn ORFs in some OPVs suggests that it may be preserved for a critical function. Although there are few investigations into the function of v-Slfn, relatively detailed in vitro and in vivo studies on v-Slfn from CMLV have been reported. The expression of this gene was confirmed 2 h after CMLV infection, and was expressed at the early stage of infection independent of viral DNA replication [35]. In contrast to mouse Slfn1, the expression of CMLV v-Slfn does not affect the proliferation of mouse fibroblasts. This is thought to be due to the lack of similarity between the first 27 amino acids of mouse Slfn1 and v-Slfn, a region that is essential for mouse Slfn1-mediated fibroblast cell growth inhibition. When the CMLV v-Slfn protein was expressed in VACV lacking intact v-Slfn, it had no effect on recombinant virus replication or plaque morphology [35]. Additionally, intradermal infection of mice with this recombinant VACV did not affect skin lesion size [35]. However, in mice with intranasal infection, v-Slfn caused less weight loss and faster recovery compared to the control groups. At three days following in vivo infection, the viral titer was the same as in the control group, but by seven days v-Slfn-mediated attenuation was clearly observed. This suggests that v-Slfn expression does not impede viral replication, but rather accelerates viral clearance by the immune system. This is consistent with the observation that the v-Slfn-bearing recombinant virus was delayed in spreading to the spleen, and was more rapidly cleared from this organ. In addition, more extensive recruitment of lymphocytes into infected lung tissue was observed in the presence of v-Slfn expression, although these cells were less activated. Highly virulent viruses can quickly overwhelm their host, limiting viral transmission. The idea that v-Slfn can reduce the virulence of poxviruses, allowing the virus to spread appropriately in the host population, is compelling [35].
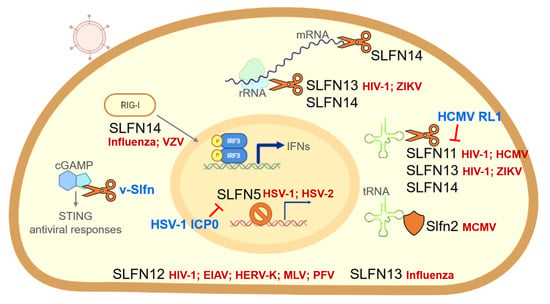
A novel feature of v-Slfn in poxviruses was recently discovered (Figure 1). Cyclic GMP-AMP synthase (cGAS) detects cytosolic DNA during virus infection, and induces an antiviral state. cGAS activates the stimulator of interferon genes (STING) by synthesizing a second messenger, cyclic GMP-AMP (cGAMP) [76,77,78]. With the discovery of a viral cGAMP nuclease named Poxin (poxvirus immune nuclease), the immunomodulatory potential of poxviruses was given a new perspective [6]. Recent studies have demonstrated that Poxin, which is a domain of v-Slfns, can degrade cGAMP and is required to avoid cGAS-STING activation [79,80,81]. Poxin was discovered to be a product of the VACV gene B2R. This gene is also known as p26 in entomopoxviruses and baculoviruses [80]. Most orthopoxviruses include a v-Slfn protein composed of two domains that have evolved from different origins. According to amino acid sequence analysis, a domain resembling the baculovirus p26 sequence is fused to the N-terminus of a v-Slfn domain similar to the murine short form Schlafen [35]; this p26-like domain is Poxin, the cGAMP nuclease. VACV, in which Poxin activity was first reported, does not retain the intact v-Slfn. The loss of Poxin resulted in a considerable reduction in VACV replication in vivo [80]. The importance of v-Slfn, which includes the Poxin domain, was studied extensively in ectromelia virus (ECTV), which causes mousepox. The Poxin domain, but not the Slfn-like domain, was sufficient to inhibit cGAS-STING signaling with cGAMP nuclease activity in a manner comparable to full-length Poxin–Schlafen-like domain fusion. This suggests that the ECTV Poxin domain preserves the full potential of v-Slfn to prevent the activation of DNA sensing via the cGAS-STING axis [79]. In several mouse infection models, the replication of ECTV lacking v-Slfn was significantly attenuated, and mice displayed a robust IFN response [79]. The Poxin–Schlafen-like domain fusion of v-Slfn is highly conserved across orthopoxviruses, such as ECTV, CMLV, and the emerging zoonotic monkeypox virus, implying the importance of cGAMP nuclease activity.
The role of the Slfn-like domain in the activation of Poxin is unclear. Poxin retained its cGAMP nuclease activity in the absence of the Slfn-like domain. Nevertheless, it remains necessary to investigate why the Slfn-like domain is conserved in many OPVs. Given the aforementioned observation that the virulence of chimeric viruses was reduced by adding the Slfn-like domain of CMLV to VACV, it is a plausible hypothesis that regulating viral virulence may contribute to creating favorable conditions for virus propagation in nature.
9. Conclusions and Future Perspectives
Continuous and in-depth research on the Schlafen family has made significant progress toward elucidating the roles of Schlafen proteins in recent years. Current studies have shown that Schlafen proteins play critical roles in regulating both the immune response and the cell cycle. Some of these proteins are associated with tumor treatment susceptibility and drug resistance [13,14,15,135]; thus, the biological function of Schlafen family proteins in tumor cells provides new methods and ideas for tumor detection and treatment. In addition, the Schlafen proteins exhibit a relatively broad inhibitory effect on retroviruses via RNA modulation to inhibit translation. Schlafen proteins have also been implicated in viral infection indirectly via interferon signaling. The discovery of a mechanism for the direct inhibition of viral gene expression through SLFN5 binding to viral DNA in the nucleus has highlighted the potential diversity in the antiviral mechanisms of the Schlafen family.
Numerous findings to date demonstrate that the Schlafen family has a role in a variety of cellular responses, including immune cell development and intrinsic/innate immunity. This protein family is, unquestionably, an important target for cancer treatment, as well as research into understanding and preventing viral infections. However, functional studies on the Schlafen proteins are still in their infancy, and there are many important questions that remain to be solved. Although the Schlafen family shares several similar domains, they show functional differences. These distinctions imply that the Schlafen family members confer specificity to their antiviral activities, highlighting the importance of studying structural properties and functional mechanisms. Fortunately, structures have been determined for rat Slfn13 [24] and human SLFN5 [31], providing insight for ongoing studies of Schlafen family proteins. Furthermore, the limitations of animal experiments for clinical application must be overcome. The Schlafen family showed a rapid evolutionary tendency in several rodents, and the degree of conservation between rodent and human Schlafen genes is not high. For example, SLFN5 and SLFN11 are the most abundant and highly studied in various cells, but the similarity between mouse and human of SLFN5 is only 59% based on the amino acid sequence identity, and there is no SLFN11 ortholog in mice. SLFN5 and SLFN14 are the only orthologs shared between mice and humans (Figure 1). Therefore, there is a need to develop a new platform, such as organoid models, that can substitute for in vivo studies.
Given the diverse functions of Schlafen family proteins, various binding partner proteins in the cell are expected to play roles in their regulation. Although no report on the results of a global proteomic approach to interactome has been published, it is critical to discover and study the role of binding partners as factors that differentiate the function and regulation of intracellular activity of Schlafen family proteins. The study of associations between Schlafen expression level and cancer prognosis can be applied to virus-mediated tumor research or treatment using viral vectors. Despite their name, the Schlafen field is far from a sleepy one. Ongoing studies will provide important insight into both virus and tumor biology, and will suggest ways that their unique activities can be harnessed for therapeutic applications.
Author Contributions
Conceptualization, E.T.K. and M.D.W.; writing—original draft preparation, E.T.K.; writing—review and editing, M.D.W.; visualization, E.T.K. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2021R1A2C1010313). M.D.W. was supported in part by grants from the National Institutes of Health (AI115104 and NS082240) and funds from the Children’s Hospital of Philadelphia.
Acknowledgments
We thank Joe Dybas for his comments on the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Schwarz, D.A.; Katayama, C.D.; Hedrick, S.M. Schlafen, a new family of growth regulatory genes that affect thymocyte development. Immunity 1998, 9, 657–668. [Google Scholar] [CrossRef]
- Geserick, P.; Kaiser, F.; Klemm, U.; Kaufmann, S.H.E.; Zerrahn, J. Modulation of T cell development and activation by novel members of the Schlafen (slfn) gene family harbouring an RNA helicase-like motif. Int. Immunol. 2004, 16, 1535–1548. [Google Scholar] [CrossRef] [PubMed]
- Neumann, B.; Zhao, L.; Murphy, K.; Gonda, T.J. Subcellular localization of the Schlafen protein family. Biochem. Biophys. Res. Commun. 2008, 370, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Kuang, C.; Yang, T.; Zhang, Y.; Zhang, L.; Wu, Q. Schlafen 1 inhibits the proliferation and tube formation of endothelial progenitor cells. PLoS One 2014, 9, e109711. [Google Scholar] [CrossRef] [PubMed]
- Brady, G.; Boggan, L.; Bowie, A.; O’Neill, L.A.J. Schlafen-1 Causes a Cell Cycle Arrest by Inhibiting Induction of Cyclin D1. J. Biol. Chem. 2005, 280, 30723–30734. [Google Scholar] [CrossRef]
- Oh, P.-S.; Patel, V.B.; Sanders, M.A.; Kanwar, S.S.; Yu, Y.; Nautiyal, J.; Patel, B.B.; Majumdar, A.P.N. Schlafen-3 decreases cancer stem cell marker expression and autocrine/juxtacrine signaling in FOLFOX-resistant colon cancer cells. Am. J. Physiol. Gastrointest. Liver Physiol. 2011, 301, G347–G355. [Google Scholar] [CrossRef]
- Patel, V.B.; Yu, Y.; Das, J.K.; Patel, B.B.; Majumdar, A.P.N. Schlafen-3: A novel regulator of intestinal differentiation. Biochem. Biophys. Res. Commun. 2009, 388, 752–756. [Google Scholar] [CrossRef]
- Sassano, A.; Mavrommatis, E.; Arslan, A.D.; Kroczynska, B.; Beauchamp, E.M.; Khuon, S.; Chew, T.-L.; Green, K.J.; Munshi, H.G.; Verma, A.K.; et al. Human Schlafen 5 (SLFN5) Is a Regulator of Motility and Invasiveness of Renal Cell Carcinoma Cells. Mol. Cell. Biol. 2015, 35, 2684–2698. [Google Scholar] [CrossRef]
- Al-Marsoummi, S.; Vomhof-DeKrey, E.; Basson, M.D. Schlafen12 Reduces the Aggressiveness of Triple Negative Breast Cancer through Post-Transcriptional Regulation of ZEB1 That Drives Stem Cell Differentiation. Cell. Physiol. Biochem. 2019, 53, 999–1014. [Google Scholar] [CrossRef]
- Al-Marsoummi, S.; Pacella, J.; Dockter, K.; Soderberg, M.; Singhal, S.K.; Vomhof-Dekrey, E.E.; Basson, M.D. Schlafen 12 Is Prognostically Favorable and Reduces C-Myc and Proliferation in Lung Adenocarcinoma but Not in Lung Squamous Cell Carcinoma. Cancers 2020, 12, 2738. [Google Scholar] [CrossRef]
- Companioni Nápoles, O.; Tsao, A.C.; Sanz-Anquela, J.M.; Sala, N.; Bonet, C.; Pardo, M.L.; Ding, L.; Simo, O.; Saqui-Salces, M.; Blanco, V.P.; et al. SCHLAFEN 5 expression correlates with intestinal metaplasia that progresses to gastric cancer. J. Gastroenterol. 2016, 52, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Zoppoli, G.; Regairaz, M.; Leo, E.; Reinhold, W.C.; Varma, S.; Ballestrero, A.; Doroshow, J.H.; Pommier, Y. Putative DNA/RNA helicase Schlafen-11 (SLFN11) sensitizes cancer cells to DNA-damaging agents. Proc. Natl. Acad. Sci. USA 2012, 109, 15030–15035. [Google Scholar] [CrossRef] [PubMed]
- Tian, L.; Song, S.; Liu, X.; Wang, Y.; Xu, X.; Hu, Y.; Xu, J. Schlafen-11 sensitizes colorectal carcinoma cells to irinotecan. Anticancer. Drugs 2014, 25, 1175–1181. [Google Scholar] [CrossRef] [PubMed]
- Nogales, V.; Reinhold, W.C.; Varma, S.; Martinez-Cardus, A.; Moutinho, C.; Moran, S.; Heyn, H.; Sebio, A.; Barnadas, A.; Pommier, Y.; et al. Epigenetic inactivation of the putative DNA/RNA helicase SLFN11 in human cancer confers resistance to platinum drugs. Oncotarget 2015, 7, 3084–3097. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.A.; Tong, P.; Cardnell, R.J.; Sen, T.; Li, L.; Gay, C.M.; Masrorpour, F.; Fan, Y.; Bara, R.O.; Feng, Y.; et al. Dynamic variations in epithelial-to-mesenchymal transition (EMT), ATM, and SLFN11 govern response to PARP inhibitors and cisplatin in small cell lung cancer. Oncotarget 2017, 8, 28575–28587. [Google Scholar] [CrossRef] [PubMed]
- Shee, K.; Wells, J.D.; Jiang, A.; Miller, T.W. Integrated pan-cancer gene expression and drug sensitivity analysis reveals SLFN11 mRNA as a solid tumor biomarker predictive of sensitivity to DNA-damaging chemotherapy. PLoS One 2019, 14, e0224267. [Google Scholar] [CrossRef]
- Winkler, C.; Armenia, J.; Jones, G.N.; Tobalina, L.; Sale, M.J.; Petreus, T.; Baird, T.; Serra, V.; Wang, A.T.; Lau, A.; et al. SLFN11 informs on standard of care and novel treatments in a wide range of cancer models. Br. J. Cancer 2021, 124, 951–962. [Google Scholar] [CrossRef]
- Li, M.; Kao, E.; Gao, X.; Sandig, H.; Limmer, K.; Pavon-Eternod, M.; Jones, T.E.; Landry, S.; Pan, T.; Weitzman, M.D.; et al. Codon-usage-based inhibition of HIV protein synthesis by human schlafen 11. Nature 2012, 491, 125–128. [Google Scholar] [CrossRef]
- Seong, R.-K.; Seo, S.; Kim, J.-A.; Fletcher, S.J.; Morgan, N.V.; Kumar, M.; Choi, Y.-K.; Shin, O.S. Schlafen 14 (SLFN14) is a novel antiviral factor involved in the control of viral replication. Immunobiology 2017, 222, 979–988. [Google Scholar] [CrossRef]
- Kim, E.T.; Dybas, J.M.; Kulej, K.; Reyes, E.D.; Price, A.M.; Akhtar, L.N.; Orr, A.; Garcia, B.A.; Boutell, C.; Weitzman, M.D. Comparative proteomics identifies Schlafen 5 (SLFN5) as a herpes simplex virus restriction factor that suppresses viral transcription. Nat. Microbiol. 2021, 6, 234–245. [Google Scholar] [CrossRef]
- Valdez, F.; Salvador, J.; Palermo, P.M.; Mohl, J.E.; Hanley, K.A.; Watts, D.; Llano, M. Schlafen 11 Restricts Flavivirus Replication. J. Virol. 2019, 93, 104–123. [Google Scholar] [CrossRef] [PubMed]
- Stabell, A.C.; Hawkins, J.; Li, M.; Gao, X.; David, M.; Press, W.H.; Sawyer, S.L. Non-human primate schlafen11 inhibits production of both host and viral proteins. PLoS Pathog. 2016, 12, e1006066. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.Z.; Sun, L.K.; Zhu, D.T.; Hu, Z.; Wang, X.F.; Du, C.; Wang, Y.H.; Wang, X.J.; Zhou, J.H. Equine schlafen 11 restricts the production of equine infectious anemia virus via a codon usage-dependent mechanism. Virology 2016, 495, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.Y.; Deng, X.Y.; Li, Y.S.; Ma, X.C.; Feng, J.X.; Yu, B.; Chen, Y.; Luo, Y.L.; Wang, X.; Chen, M.L.; et al. Structure of Schlafen13 reveals a new class of tRNA/rRNA-targeting RNase engaged in translational control. Nat. Commun. 2018, 9, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Al-Marsoummi, S.; Vomhof-DeKrey, E.E.; Basson, M.D. Schlafens: Emerging Proteins in Cancer Cell Biology. Cells 2021, 10, 2238. [Google Scholar] [CrossRef] [PubMed]
- Bustos, O.; Naik, S.; Ayers, G.; Casola, C.; Perez-Lamigueiro, M.A.; Chippindale, P.T.; Pritham, E.J.; de la Casa-Esperón, E. Evolution of the Schlafen genes, a gene family associated with embryonic lethality, meiotic drive, immune processes and orthopoxvirus virulence. Gene 2009, 447, 1–11. [Google Scholar] [CrossRef]
- De La Casa-Espero’n, E. From mammals to viruses: The Schlafen genes in developmental, proliferative and immune processes. Biomol. Concepts 2011, 2, 159–169. [Google Scholar] [CrossRef]
- Liu, F.; Zhou, P.; Wang, Q.; Zhang, M.; Li, D. The Schlafen family: Complex roles in different cell types and virus replication. Cell Biol. Int. 2018, 42, 2–8. [Google Scholar] [CrossRef]
- Chen, J.; Kuhn, L.A. Deciphering the Three-Domain Architecture in Schlafens and the Structures and Roles of Human Schlafen12 and SerpinB12 in Transcriptional Regulation. J. Mol. Graph. Model. 2019, 90, 59. [Google Scholar] [CrossRef]
- Basson, M.D.; Wang, Q.; Chaturvedi, L.S.; More, S.; Vomhof-Dekrey, E.E.; Al-Marsoummi, S.; Sun, K.; Kuhn, L.A.; Kovalenko, P.; Kiupel, M. Schlafen 12 Interaction with SerpinB12 and Deubiquitylases Drives Human Enterocyte Differentiation. Cell. Physiol. Biochem. 2018, 48, 1274–1290. [Google Scholar] [CrossRef]
- Metzner, F.J.; Huber, E.; Hopfner, K.-P.; Lammens, K. Structural and biochemical characterization of human Schlafen 5. Nucleic Acids Res. 2022, 1, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.E.; Saraste, M.; Runswick, M.J.; Gay, N.J. Distantly related sequences in the alpha- and beta-subunits of ATP synthase, myosin, kinases and other ATP-requiring enzymes and a common nucleotide binding fold. EMBO J. 1982, 1, 945. [Google Scholar] [CrossRef] [PubMed]
- Mu, Y.; Lou, J.; Srivastava, M.; Zhao, B.; Feng, X.; Liu, T.; Chen, J.; Huang, J. SLFN11 inhibits checkpoint maintenance and homologous recombination repair. EMBO Rep. 2016, 17, 94. [Google Scholar] [CrossRef] [PubMed]
- Murai, J.; Tang, S.W.; Leo, E.; Baechler, S.A.; Redon, C.E.; Zhang, H.; Al Abo, M.; Rajapakse, V.N.; Nakamura, E.; Jenkins, L.M.M.; et al. SLFN11 Blocks Stressed Replication Forks Independently of ATR. Mol. Cell 2018, 69, 371–384.e6. [Google Scholar] [CrossRef]
- Gubse, C.; Goodbody, R.; Ecker, A.; Brady, G.; O’Neill, L.A.J.; Jacobs, N.; Smith, G.L. Camelpox virus encodes a schlafen-like protein that affects orthopoxvirus virulence. J. Gen. Virol. 2007, 88, 1667–1676. [Google Scholar] [CrossRef]
- Sohn, W.-J.; Kim, D.; Lee, K.-W.; Kim, M.-S.; Kwon, S.; Lee, Y.; Kim, D.-S.; Kwon, H.-J. Novel transcriptional regulation of the schlafen-2 gene in macrophages in response to TLR-triggered stimulation. Mol. Immunol. 2007, 44, 3273–3282. [Google Scholar] [CrossRef]
- Puck, A.; Aigner, R.; Modak, M.; Cejka, P.; Blaas, D.; Stöckl, J. Expression and regulation of Schlafen (SLFN) family members in primary human monocytes, monocyte-derived dendritic cells and T cells. Results Immunol. 2015, 5, 23–32. [Google Scholar] [CrossRef]
- van Zuylen, W.J.; Garceau, V.; Idris, A.; Schroder, K.; Irvine, K.M.; Lattin, J.E.; Ovchinnikov, D.A.; Perkins, A.C.; Cook, A.D.; Hamilton, J.A.; et al. Macrophage activation and differentiation signals regulate schlafen-4 gene expression: Evidence for Schlafen-4 as a modulator of myelopoiesis. PLoS One 2011, 6, e15723. [Google Scholar] [CrossRef]
- Eskra, L.; Mathison, A.; Splitter, G. Microarray analysis of mRNA levels from RAW264.7 macrophages infected with Brucella abortus. Infect. Immun. 2003, 71, 1125–1133. [Google Scholar] [CrossRef]
- Katsoulidis, E.; Mavrommatis, E.; Woodard, J.; Shields, M.A.; Sassano, A.; Carayol, N.; Sawicki, K.T.; Munshi, H.G.; Platanias, L.C. Role of Interferon α (IFNα)-inducible Schlafen-5 in Regulation of Anchorage-independent Growth and Invasion of Malignant Melanoma Cells. J. Biol. Chem. 2010, 285, 40333–40341. [Google Scholar] [CrossRef]
- Katsoulidis, E.; Carayol, N.; Woodard, J.; Konieczna, I.; Majchrzak-Kita, B.; Jordan, A.; Sassano, A.; Eklund, E.A.; Fish, E.N.; Platanias, L.C. Role of Schlafen 2 (SLFN2) in the Generation of Interferon α-induced Growth Inhibitory Responses. J. Biol. Chem. 2009, 284, 25051. [Google Scholar] [CrossRef] [PubMed]
- Sadler, A.J.; Williams, B.R.G. Interferon-inducible antiviral effectors. Nat. Rev. Immunol. 2008, 8, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Cartharius, K.; Frech, K.; Grote, K.; Klocke, B.; Haltmeier, M.; Klingenhoff, A.; Frisch, M.; Bayerlein, M.; Werner, T. MatInspector and beyond: Promoter analysis based on transcription factor binding sites. Bioinformatics 2005, 21, 2933–2942. [Google Scholar] [CrossRef] [PubMed]
- Murai, Y.; Jo, U.; Murai, J.; Fukuda, S.; Takebe, N.; Pommier, Y. Schlafen 11 expression in human acute leukemia cells with gain-of-function mutations in the interferon-JAK signaling pathway. iScience 2021, 24, 103173. [Google Scholar] [CrossRef] [PubMed]
- El-Zaatari, M.; Kao, J.Y.; Tessier, A.; Bai, L.; Hayes, M.M.; Fontaine, C.; Eaton, K.A.; Merchant, J.L. Gli1 Deletion Prevents Helicobacter-Induced Gastric Metaplasia and Expansion of Myeloid Cell Subsets. PLoS One 2013, 8, e58935. [Google Scholar] [CrossRef]
- Esteller, M. CpG island hypermethylation and tumor suppressor genes: A booming present, a brighter future. Oncogene 2002, 21, 5427–5440. [Google Scholar] [CrossRef]
- Kaur, S.; Schwartz, A.L.; Jordan, D.G.; Soto-Pantoja, D.R.; Kuo, B.; Elkahloun, A.G.; Mathews Griner, L.; Thomas, C.J.; Ferrer, M.; Thomas, A.; et al. Identification of Schlafen-11 as a Target of CD47 Signaling That Regulates Sensitivity to Ionizing Radiation and Topoisomerase Inhibitors. Front. Oncol. 2019, 9, 994. [Google Scholar] [CrossRef]
- Moribe, F.; Nishikori, M.; Takashima, T.; Taniyama, D.; Onishi, N.; Arima, H.; Sasanuma, H.; Akagawa, R.; Elloumi, F.; Takeda, S.; et al. Epigenetic suppression of SLFN11 in germinal center B-cells during B-cell development. PLoS One 2021, 16, e0237554. [Google Scholar] [CrossRef]
- Reinhold, W.C.; Sunshine, M.; Varma, S.; Doroshow, J.H.; Pommier, Y. Using CellMiner 1.6 for Systems Pharmacology and Genomic Analysis of the NCI-60. Clin. Cancer Res. 2015, 21, 3841–3852. [Google Scholar] [CrossRef]
- Mizuno, S.I.; Chijiwa, T.; Okamura, T.; Akashi, K.; Fukumaki, Y.; Niho, Y.; Sasaki, H. Expression of DNA methyltransferases DNMT1,3A, and 3B in normal hematopoiesis and in acute and chronic myelogenous leukemia. Blood 2001, 97, 1172–1179. [Google Scholar] [CrossRef]
- Zhang, Y.; Yang, Z.; Cao, Y.; Zhang, S.; Li, H.; Huang, Y.; Ding, Y.Q.; Liu, X. The Hsp40 family chaperone protein DnaJB6 enhances Schlafen1 nuclear localization which is critical for promotion of cell-cycle arrest in T-cells. Biochem. J. 2008, 413, 239–250. [Google Scholar] [CrossRef] [PubMed]
- Condamine, T.; Benoıˆt, J.-B.; Luduec, L.; Chiffoleau, E.; Bériou, G.; Louvet, C.; Heslan, M.; Tilly, G.; Cuturi, M.-C. Characterization of Schlafen-3 expression in effector and regulatory T cells. J. Leukoc. Biol. 2010, 87, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Vomhof-DeKrey, E.E.; Umthun, J.; Basson, M.D. Loss of Schlafen3 influences the expression levels of Schlafen family members in ileum, thymus, and spleen tissue. PeerJ 2020, 8, e8461. [Google Scholar] [CrossRef] [PubMed]
- Flandez, M.; Guilmeau, S.; Blache, P.; Augenlicht, L.H. KLF4 regulation in intestinal epithelial cell maturation. Exp. Cell Res. 2008, 314, 3712–3723. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.; Krebs, P.; Crozat, K.; Li, X.; Croker, B.A.; Siggs, O.M.; Popkin, D.; Du, X.; Lawson, B.R.; Theofilopoulos, A.N.; et al. An Slfn2 mutation causes lymphoid and myeloid immunodeficiency due to loss of immune cell quiescence. Nat. Immunol. 2010, 11, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Recher, M.; Karjalainen-Lindsberg, M.L.; Lindlöf, M.; Söderlund-Venermo, M.; Lanzi, G.; Väisänen, E.; Kumar, A.; Sadeghi, M.; Berger, C.T.; Alitalo, T.; et al. Genetic variation in schlafen genes in a patient with a recapitulation of the murine Elektra phenotype. J. Allergy Clin. Immunol. 2014, 133, 1462–1465.e5. [Google Scholar] [CrossRef]
- Marconi, C.; Di Buduo, C.A.; Barozzi, S.; Palombo, F.; Pardini, S.; Zaninetti, C.; Pippucci, T.; Noris, P.; Balduini, A.; Seri, M.; et al. SLFN14-related thrombocytopenia: Identification within a large series of patients with inherited thrombocytopenia. Thromb. Haemost. 2016, 115, 1076–1079. [Google Scholar] [CrossRef]
- Saes, J.L.; Simons, A.; de Munnik, S.A.; Nijziel, M.R.; Blijlevens, N.M.A.; Jongmans, M.C.; van der Reijden, B.A.; Smit, Y.; Brons, P.P.; van Heerde, W.L.; et al. Whole exome sequencing in the diagnostic workup of patients with a bleeding diathesis. Haemophilia 2019, 25, 127–135. [Google Scholar] [CrossRef]
- Almazni, I.; Stapley, R.J.; Khan, A.O.; Morgan, N.V. A comprehensive bioinformatic analysis of 126 patients with an inherited platelet disorder to identify both sequence and copy number genetic variants. Hum. Mutat. 2020, 41, 1848–1865. [Google Scholar] [CrossRef]
- Khan, A.O.; Stapley, R.J.; Pike, J.A.; Wijesinghe, S.N.; Reyat, J.S.; Almazni, I.; Machlus, K.R.; Morgan, N.V. Novel gene variants in patients with platelet-based bleeding using combined exome sequencing and RNAseq murine expression data. J. Thromb. Haemost. 2021, 19, 262–268. [Google Scholar] [CrossRef]
- Fletcher, S.J.; Johnson, B.; Lowe, G.C.; Bem, D.; Drake, S.; Lordkipanidzé, M.; Guiu, I.S.; Dawood, B.; Rivera, J.; Simpson, M.A.; et al. SLFN14 mutations underlie thrombocytopenia with excessive bleeding and platelet secretion defects. J. Clin. Invest. 2015, 125, 3600–3605. [Google Scholar] [CrossRef] [PubMed]
- Stapley, R.J.; Smith, C.W.; Haining, E.J.; Bacon, A.; Lax, S.; Pisareva, V.P.; Pisarev, A.V.; Watson, S.P.; Khan, A.O.; Morgan, N.V. Heterozygous mutation SLFN14 K208N in mice mediates species-specific differences in platelet and erythroid lineage commitment. Blood Adv. 2021, 5, 377–390. [Google Scholar] [CrossRef] [PubMed]
- Ali, R.A.; Wuescher, L.M.; Worth, R.G. Platelets: Essential components of the immune system. Curr. Trends Immunol. 2015, 16, 65–78. [Google Scholar] [PubMed]
- Malakhova, O.A.; Kim, K.I.; Luo, J.K.; Zou, W.; Kumar, K.G.S.; Fuchs, S.Y.; Shuai, K.; Zhang, D.E. UBP43 is a novel regulator of interferon signaling independent of its ISG15 isopeptidase activity. EMBO J. 2006, 25, 2358–2367. [Google Scholar] [CrossRef]
- Arslan, A.D.; Sassano, A.; Saleiro, D.; Lisowski, P.; Kosciuczuk, E.M.; Fischietti, M.; Eckerdt, F.; Fish, E.N.; Platanias, L.C. Human SLFN5 is a transcriptional co-repressor of STAT1-mediated interferon responses and promotes the malignant phenotype in glioblastoma. Oncogene 2017, 36, 6006–6019. [Google Scholar] [CrossRef]
- Spaderna, S.; Schmalhofer, O.; Wahlbuhl, M.; Dimmler, A.; Bauer, K.; Sultan, A.; Hlubek, F.; Jung, A.; Strand, D.; Eger, A.; et al. The transcriptional repressor ZEB1 promotes metastasis and loss of cell polarity in cancer. Cancer Res. 2008, 68, 537–544. [Google Scholar] [CrossRef]
- Larsen, J.E.; Nathan, V.; Osborne, J.K.; Farrow, R.K.; Deb, D.; Sullivan, J.P.; Dospoy, P.D.; Augustyn, A.; Hight, S.K.; Sato, M.; et al. ZEB1 drives epithelial-to-mesenchymal transition in lung cancer. J. Clin. Invest. 2016, 126, 3219. [Google Scholar] [CrossRef]
- Scott, C.L.; Omilusik, K.D.; Scott, C.L.; Omilusik, K.D. ZEBs: Novel Players in Immune Cell Development and Function. Trends Immunol. 2019, 40, 431–446. [Google Scholar] [CrossRef]
- Wan, G.; Zhu, J.; Gu, X.; Yang, Y.; Liu, Y.; Wang, Z.; Zhao, Y.; Wu, H.; Huang, G.; Lu, C. Human Schlafen 5 regulates reversible epithelial and mesenchymal transitions in breast cancer by suppression of ZEB1 transcription. Br. J. Cancer 2020, 123, 633–643. [Google Scholar] [CrossRef]
- Gu, X.; Wan, G.; Yang, Y.; Liu, Y.; Yang, X.; Zheng, Y.; Jiang, L.; Zhang, P.; Liu, D.; Zhao, W.; et al. SLFN5 influences proliferation and apoptosis by upregulating PTEN transcription via ZEB1 and inhibits the purine metabolic pathway in breast cancer. Am. J. Cancer Res. 2020, 10, 2832. [Google Scholar]
- Goldstein, D.; Laszlo, J. The role of interferon in cancer therapy: A current perspective. CA. Cancer J. Clin. 1988, 38, 258–277. [Google Scholar] [CrossRef]
- Hauschild, A.; Gogas, H.; Tarhini, A.; Middleton, M.R.; Testori, A.; Dréno, B.; Kirkwood, J.M. Practical guidelines for the management of interferon-alpha-2b side effects in patients receiving adjuvant treatment for melanoma: Expert opinion. Cancer 2008, 112, 982–994. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, J.; Waugh, N.; Hewitson, P. Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: A rapid and systematic review. Health Technol. Assess. (Rockv). 2000, 4, 1–67. [Google Scholar] [CrossRef]
- Cooksley, W.G.E. Gastroenterology Expert Column: The Role of Interferon Therapy in Hepatitis B. Medscape Gen. Med. 2004, 6, 16. [Google Scholar]
- Mavrommatis, E.; Arslan, A.D.; Sassano, A.; Hua, Y.; Kroczynska, B.; Platanias, L.C. Expression and Regulatory Effects of Murine Schlafen (Slfn) Genes in Malignant Melanoma and Renal Cell Carcinoma. J. Biol. Chem. 2013, 288, 33006. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Wu, J.; Du, F.; Chen, X.; Chen, Z.J. Cyclic GMP-AMP synthase is a cytosolic DNA sensor that activates the type I interferon pathway. Science 2013, 339, 786–791. [Google Scholar] [CrossRef]
- Wu, J.; Sun, L.; Chen, X.; Du, F.; Shi, H.; Chen, C.; Chen, Z.J. Cyclic GMP-AMP is an endogenous second messenger in innate immune signaling by cytosolic DNA. Science 2013, 339, 826–830. [Google Scholar] [CrossRef]
- Gao, P.; Ascano, M.; Zillinger, T.; Wang, W.; Dai, P.; Serganov, A.A.; Gaffney, B.L.; Shuman, S.; Jones, R.A.; Deng, L.; et al. Structure-function analysis of STING activation by c[G(2’,5’)pA(3’,5’)p] and targeting by antiviral DMXAA. Cell 2013, 154, 748–762. [Google Scholar] [CrossRef]
- Hernaez, B.; Alonso, G.; Georgana, I.; El-Jesr, M.; Martin, R.; Shair, K.H.Y.; Fischer, C.; Sauer, S.; De Motes, C.M.; Alcami, A. Viral cGAMP nuclease reveals the essential role of DNA sensing in protection against acute lethal virus infection. Sci. Adv. 2020, 6, 4565–4583. [Google Scholar] [CrossRef]
- Eaglesham, J.B.; Pan, Y.; Kupper, T.S.; Kranzusch, P.J. Viral and metazoan poxins are cGAMP-specific nucleases that restrict cGAS–STING signalling. Nature 2019, 566, 259–263. [Google Scholar] [CrossRef]
- Eaglesham, J.B.; McCarty, K.L.; Kranzusch, P.J. Structures of diverse poxin cGAMP nucleases reveal a widespread role for cGAS-STING evasion in host-pathogen conflict. Elife 2020, 9, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Melo, D.; Venkatesh, S.; Bieniasz, P.D. Intrinsic Cellular Defenses against Human Immunodeficiency Viruses. Immunity 2012, 37, 399–411. [Google Scholar] [CrossRef] [PubMed]
- Hotter, D.; Kirchhoff, F. Interferons and beyond: Induction of antiretroviral restriction factors. J. Leukoc. Biol. 2018, 103, 465–477. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.-Y.; Sanchez, D.J.; Aliyari, R.; Lu, S.; Cheng, G. Systematic identification of type I and type II interferon-induced antiviral factors. Proc. Natl Acad. Sci. USA 2012, 109, 4239–4244. [Google Scholar] [CrossRef] [PubMed]
- Kane, M.; Zang, T.M.; Rihn, S.J.; Zhang, F.; Kueck, T.; Alim, M.; Schoggins, J.; Rice, C.M.; Wilson, S.J.; Bieniasz, P.D. Identification of Interferon-Stimulated Genes with Antiretroviral Activity. Cell Host Microbe 2016, 20, 392–405. [Google Scholar] [CrossRef]
- Coccia, E.M.; Krust, B.; Hovanessian, A.G. Specific inhibition of viral protein synthesis in HIV-infected cells in response to interferon treatment. J. Biol. Chem. 1994, 269, 23087–23094. [Google Scholar] [CrossRef]
- Abdel-Mohsen, M.; Raposo, R.A.S.; Deng, X.; Li, M.; Liegler, T.; Sinclair, E.; Salama, M.S.; Ghanem, H.E.-D.A.; Hoh, R.; Wong, J.K.; et al. Expression profile of host restriction factors in HIV-1 elite controllers. Retrovirology 2013, 10, 106. [Google Scholar] [CrossRef]
- Kumar, A.; Abbas, W.; Herbein, G. HIV-1 latency in monocytes/macrophages. Viruses 2014, 6, 1837–1860. [Google Scholar] [CrossRef]
- Yue, T.; Zhan, X.; Zhang, D.; Jain, R.; Wang, K.-W.; Choi, J.H.; Misawa, T.; Su, L.; Quan, J.; Hildebrand, S.; et al. SLFN2 protection of tRNAs from stress-induced cleavage is essential for T cell–mediated immunity. Science 2021, 372, eaba4220. [Google Scholar] [CrossRef]
- Pisareva, V.P.; Muslimov, I.A.; Tcherepanov, A.; Pisarev, A.V. Characterization of novel ribosome-associated endoribonuclease SLFN14 from rabbit reticulocytes. Biochemistry 2015, 54, 3286–3301. [Google Scholar] [CrossRef]
- Gardner, E.E.; Lok, B.H.; Schneeberger, V.E.; Desmeules, P.; Miles, L.A.; Arnold, P.K.; Ni, A.; Khodos, I.; de Stanchina, E.; Nguyen, T.; et al. Chemosensitive Relapse in Small Cell Lung Cancer Proceeds through an EZH2-SLFN11 Axis. Cancer Cell 2017, 31, 286–299. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.W.; Bilke, S.; Cao, L.; Murai, J.; Sousa, F.G.; Yamade, M.; Rajapakse, V.; Varma, S.; Helman, L.J.; Khan, J.; et al. SLFN11 Is a Transcriptional Target of EWS-FLI1 and a Determinant of Drug Response in Ewing Sarcoma. Clin. Cancer Res. 2015, 21, 4184–4193. [Google Scholar] [CrossRef]
- Li, M.; Kao, E.; Malone, D.; Gao, X.; Wang, J.Y.J.J.; David, M. DNA damage-induced cell death relies on SLFN11-dependent cleavage of distinct type II tRNAs. Nat. Struct. Mol. Biol. 2018, 25, 1047–1058. [Google Scholar] [CrossRef] [PubMed]
- Jo, U.; Murai, Y.; Chakka, S.; Chen, L.; Cheng, K.; Murai, J.; Saha, L.K.; Miller Jenkins, L.M.; Pommier, Y. SLFN11 promotes CDT1 degradation by CUL4 in response to replicative DNA damage, while its absence leads to synthetic lethality with ATR/CHK1 inhibitors. Proc. Natl. Acad. Sci. USA 2021, 118, e2015654118. [Google Scholar] [CrossRef] [PubMed]
- Weitzman, M.D.; Fradet-Turcotte, A. Virus DNA Replication and the Host DNA Damage Response. Annu. Rev. Virol. 2018, 5, 141. [Google Scholar] [CrossRef]
- Ariumi, Y.; Trono, D. Ataxia-Telangiectasia-Mutated (ATM) Protein Can Enhance Human Immunodeficiency Virus Type 1 Replication by Stimulating Rev Function. J. Virol. 2006, 80, 2445. [Google Scholar] [CrossRef]
- Daniel, R.; Kao, G.; Taganov, K.; Greger, J.G.; Favorova, O.; Merke, G.; Yen, T.J.; Katz, R.A.; Skalka, A.M. Evidence that the retroviral DNA integration process triggers an ATR-dependent DNA damage response. Proc. Natl. Acad. Sci. USA 2003, 100, 4778–4783. [Google Scholar] [CrossRef]
- Hammack, C.; Ogden, S.C.; Madden, J.C.; Medina, A.; Xu, C.; Phillips, E.; Son, Y.; Cone, A.; Giovinazzi, S.; Didier, R.A.; et al. Zika Virus Infection Induces DNA Damage Response in Human Neural Progenitors That Enhances Viral Replication. J. Virol. 2019, 93. [Google Scholar] [CrossRef]
- Mansuy, J.M.; Suberbielle, E.; Chapuy-Regaud, S.; Mengelle, C.; Bujan, L.; Marchou, B.; Delobel, P.; Gonzalez-Dunia, D.; Malnou, C.E.; Izopet, J.; et al. Zika virus in semen and spermatozoa. Lancet. Infect. Dis. 2016, 16, 1106–1107. [Google Scholar] [CrossRef]
- Zanluca, C.; de Noronha, L.; Duarte dos Santos, C.N. Maternal-fetal transmission of the zika virus: An intriguing interplay. Tissue Barriers 2018, 6, e1402143. [Google Scholar] [CrossRef]
- Weekes, M.P.; Tomasec, P.; Huttlin, E.L.; Fielding, C.A.; Nusinow, D.; Stanton, R.J.; Wang, E.C.Y.; Aicheler, R.; Murrell, I.; Wilkinson, G.W.G.; et al. Quantitative temporal viromics: An approach to investigate host-pathogen interaction. Cell 2014, 157, 1460–1472. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, K.; Potts, M.; Hunter, L.M.; Fielding, C.A.; Zerbe, C.M.; Fletcher-Etherington, A.; Nobre, L.; Wang, E.C.Y.; Strang, B.L.; Houghton, J.W.; et al. Human cytomegalovirus protein RL1 degrades the antiviral factor SLFN11 via recruitment of the CRL4 E3 ubiquitin ligase complex. Proc. Natl. Acad. Sci. USA 2022, 119, e2108173119. [Google Scholar] [CrossRef] [PubMed]
- Malone, D.; Lardelli, R.M.; Li, M.; David, M. Dephosphorylation activates the interferon-stimulated Schlafen family member 11 in the DNA damage response. J. Biol. Chem. 2019, 294, 14674–14685. [Google Scholar] [CrossRef] [PubMed]
- Jacob, T.; Van den Broeke, C.; Favoreel, H.W. Viral Serine/Threonine Protein Kinases. J. Virol. 2011, 85, 1158–1173. [Google Scholar] [CrossRef]
- Deutschmann, J.; Schneider, A.; Gruska, I.; Vetter, B.; Thomas, D.; Kießling, M.; Wittmann, S.; Herrmann, A.; Schindler, M.; Milbradt, J.; et al. A viral kinase counteracts in vivo restriction of murine cytomegalovirus by SAMHD1. Nat. Microbiol. 2019, 4, 2273–2284. [Google Scholar] [CrossRef]
- de Meo, S.; Dell’Oste, V.; Molfetta, R.; Tassinari, V.; Lotti, L.V.; Vespa, S.; Pignoloni, B.; Covino, D.A.; Fantuzzi, L.; Bona, R.; et al. SAMHD1 phosphorylation and cytoplasmic relocalization after human cytomegalovirus infection limits its antiviral activity. PLoS Pathog. 2020, 16, e1008855. [Google Scholar] [CrossRef]
- Businger, R.; Deutschmann, J.; Gruska, I.; Milbradt, J.; Wiebusch, L.; Gramberg, T.; Schindler, M. Human cytomegalovirus overcomes SAMHD1 restriction in macrophages via pUL97. Nat. Microbiol. 2019, 4, 2260–2272. [Google Scholar] [CrossRef]
- Zhang, K.; Lv, D.W.; Li, R. Conserved Herpesvirus Protein Kinases Target SAMHD1 to Facilitate Virus Replication. Cell Rep. 2019, 28, 449–459.e5. [Google Scholar] [CrossRef]
- Betancor, G.; Jimenez-Guardeño, J.M.; Lynham, S.; Antrobus, R.; Khan, H.; Sobala, A.; Dicks, M.D.J.; Malim, M.H. MX2-mediated innate immunity against HIV-1 is regulated by serine phosphorylation. Nat. Microbiol. 2021, 6, 1031–1042. [Google Scholar] [CrossRef]
- Shirakawa, K.; Takaori-Kondo, A.; Yokoyama, M.; Izumi, T.; Matsui, M.; Io, K.; Sato, T.; Sato, H.; Uchiyama, T. Phosphorylation of APOBEC3G by protein kinase A regulates its interaction with HIV-1 Vif. Nat. Struct. Mol. Biol. 2008, 15, 1184–1191. [Google Scholar] [CrossRef][Green Version]
- Narayana, S.K.; Helbig, K.J.; McCartney, E.M.; Eyre, N.S.; Bull, R.A.; Eltahla, A.; Lloyd, A.R.; Beard, M.R. The Interferon-induced Transmembrane Proteins, IFITM1, IFITM2, and IFITM3 Inhibit Hepatitis C Virus Entry. J. Biol. Chem. 2015, 290, 25946–25959. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.T.; Roche, K.L.; Kulej, K.; Spruce, L.A.; Seeholzer, S.H.; Coen, D.M.; Diaz-Griffero, F.; Murphy, E.A.; Weitzman, M.D. SAMHD1 Modulates Early Steps during Human Cytomegalovirus Infection by Limiting NF-κB Activation. Cell Rep. 2019, 28, 434–448.e6. [Google Scholar] [CrossRef] [PubMed]
- Rückle, A.; Haasbach, E.; Julkunen, I.; Planz, O.; Ehrhardt, C.; Ludwig, S. The NS1 Protein of Influenza A Virus Blocks RIG-I-Mediated Activation of the Noncanonical NF-κB Pathway and p52/RelB-Dependent Gene Expression in Lung Epithelial Cells. J. Virol. 2012, 86, 10211–10217. [Google Scholar] [CrossRef]
- Fullam, A.; Schröder, M. DExD/H-box RNA helicases as mediators of anti-viral innate immunity and essential host factors for viral replication. Biochim. Biophys. Acta. 2013, 1829, 854–865. [Google Scholar] [CrossRef] [PubMed]
- SLFN14 Protein Expression Summary—The Human Protein Atlas. Available online: https://www.proteinatlas.org/ENSG00000236320-SLFN14#gene_information (accessed on 10 December 2021).
- Chakrabarti, A.; Jha, B.K.; Silverman, R.H. New Insights into the Role of RNase L in Innate Immunity. J. Interf. Cytokine Res. 2011, 31, 49. [Google Scholar] [CrossRef] [PubMed]
- Mavrommatis, E.; Fish, E.N.; Platanias, L.C. The schlafen family of proteins and their regulation by interferons. J. Interferon Cytokine Res. 2013, 33, 206–210. [Google Scholar] [CrossRef]
- Sun, J.; Vera, J.C.; Drnevich, J.; Lin, Y.T.; Ke, R.; Brooke, C.B. Single cell heterogeneity in influenza A virus gene expression shapes the innate antiviral response to infection. PLoS Pathog. 2020, 16, e1008671. [Google Scholar] [CrossRef]
- Kumar, M.; Hughes, L.; Nerurkar, V.R. Expression and regulatory effects of Schlafen genes in flavivirus infection. J. Immunol. 2016, 196, 217–228. [Google Scholar]
- Reyes, E.D.; Kulej, K.; Pancholi, N.J.; Akhtar, L.N.; Avgousti, D.C.; Kim, E.T.; Bricker, D.K.; Spruce, L.A.; Koniski, S.A.; Seeholzer, S.H.; et al. Identifying Host Factors Associated with DNA Replicated During Virus Infection. Mol. Cell. Proteomics 2017, 16, 2079–2097. [Google Scholar] [CrossRef]
- Sirbu, B.M.; Couch, F.B.; Feigerle, J.T.; Bhaskara, S.; Hiebert, S.W.; Cortez, D. Analysis of protein dynamics at active, stalled, and collapsed replication forks. Genes Dev. 2011, 25, 1320–1327. [Google Scholar] [CrossRef]
- Dembowski, J.A.; DeLuca, N.A. Selective recruitment of nuclear factors to productively replicating herpes simplex virus genomes. PLoS Pathog. 2015, 11, e1004939. [Google Scholar] [CrossRef] [PubMed]
- Boutell, C.; Everett, R.D. Regulation of alphaherpesvirus infections by the ICP0 family of proteins. J. Gen. Virol. 2013, 94, 465–481. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, M.C.; Dybas, J.M.; Hughes, J.; Weitzman, M.D.; Boutell, C. The HSV-1 ubiquitin ligase ICP0: Modifying the cellular proteome to promote infection. Virus Res. 2020, 285, 198015. [Google Scholar] [CrossRef] [PubMed]
- Lou, D.I.; Kim, E.T.; Meyerson, N.R.; Pancholi, N.J.; Mohni, K.N.; Enard, D.; Petrov, D.A.; Weller, S.K.; Weitzman, M.D.; Sawyer, S.L. An Intrinsically Disordered Region of the DNA Repair Protein Nbs1 Is a Species-Specific Barrier to Herpes Simplex Virus 1 in Primates. Cell Host Microbe 2016, 20, 178–188. [Google Scholar] [CrossRef] [PubMed]
- Knipe, D.M.; Cliffe, A. Chromatin control of herpes simplex virus lytic and latent infection. Nat. Rev. Microbiol. 2008, 6, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Lukashchuk, V.; Everett, R.D. Regulation of ICP0-Null Mutant Herpes Simplex Virus Type 1 Infection by ND10 Components ATRX and hDaxx. J. Virol. 2010, 84, 4026–4040. [Google Scholar] [CrossRef] [PubMed]
- Lilley, C.E.; Chaurushiya, M.S.; Boutell, C.; Everett, R.D.; Weitzman, M.D. The intrinsic antiviral defense to incoming HSV-1 genomes includes specific DNA repair proteins and is counteracted by the viral protein ICP0. PLoS Pathog. 2011, 7, e1002084. [Google Scholar] [CrossRef]
- Alandijany, T.; Roberts, A.P.E.; Conn, K.L.; Loney, C.; McFarlane, S.; Orr, A.; Boutell, C. Distinct temporal roles for the promyelocytic leukaemia (PML) protein in the sequential regulation of intracellular host immunity to HSV-1 infection. PLoS Pathog. 2018, 14, e1006769. [Google Scholar] [CrossRef]
- Cohen, C.; Corpet, A.; Roubille, S.; Maroui, M.A.; Poccardi, N.; Rousseau, A.; Kleijwegt, C.; Binda, O.; Texier, P.; Sawtell, N.; et al. Promyelocytic leukemia (PML) nuclear bodies (NBs) induce latent/quiescent HSV-1 genomes chromatinization through a PML NB/Histone H3.3/H3.3 Chaperone Axis. PLoS Pathog. 2018, 14, e1007313. [Google Scholar] [CrossRef] [PubMed]
- Gaidt, M.M.; Morrow, A.; Fairgrieve, M.R.; Karr, J.P.; Yosef, N.; Vance, R.E. Self-guarding of MORC3 enables virulence factor-triggered immunity. Nature 2021, 600, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Drayman, N.; Patel, P.; Vistain, L.; Tay, S. HSV-1 single cell analysis reveals anti-viral and developmental programs activation in distinct sub-populations. Elife 2019, 8, e46339. [Google Scholar] [CrossRef] [PubMed]
- Wan, G.; Liu, Y.; Zhu, J.; Guo, L.; Li, C.; Yang, Y.; Gu, X.; Deng, L.L.; Lu, C. SLFN5 suppresses cancer cell migration and invasion by inhibiting MT1-MMP expression via AKT/GSK-3β/β-catenin pathway. Cell. Signal. 2019, 59, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Zhou, L.; Chen, L.; Pan, H.; Zhao, R.; Guang, W.; Wan, G.; Zhang, P.; Liu, D.; Deng, L.-L.; et al. Human Schlafen 5 Inhibits Proliferation and Promotes Apoptosis in Lung Adenocarcinoma via the PTEN/PI3K/AKT/mTOR Pathway. Biomed Res. Int. 2021, 2021, 1–11. [Google Scholar] [CrossRef] [PubMed]
- He, T.; Zhang, M.; Zheng, R.; Zheng, S.; Linghu, E.; Herman, J.G.; Guo, M. Methylation of SLFN11 is a marker of poor prognosis and cisplatin resistance in colorectal cancer. Epigenomics 2017, 9, 849–862. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).