Trends and Risk Factors of In-Hospital Mortality of Patients with COVID-19 in Germany: Results of a Large Nationwide Inpatient Sample
Abstract
:1. Take-Home Message
2. Introduction
3. Methods
3.1. Data Source
3.2. Study Oversight and Support
3.3. Coding of Diagnoses, Procedures and Definitions
3.4. Statistical Analysis
4. Results
4.1. Baseline Characteristics
4.2. Comparison of Survivors vs. Non-Survivors in COVID-19 Patients
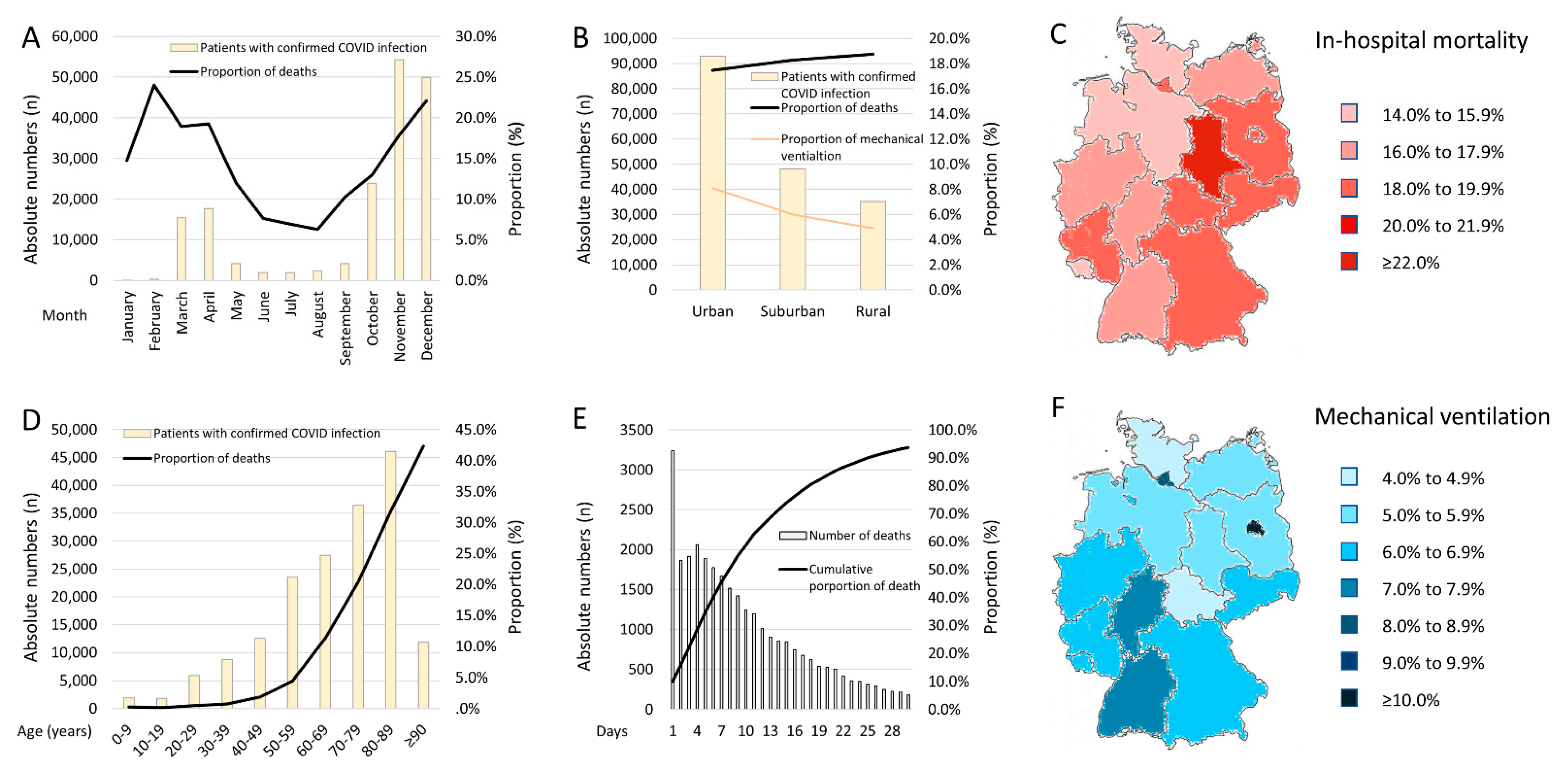
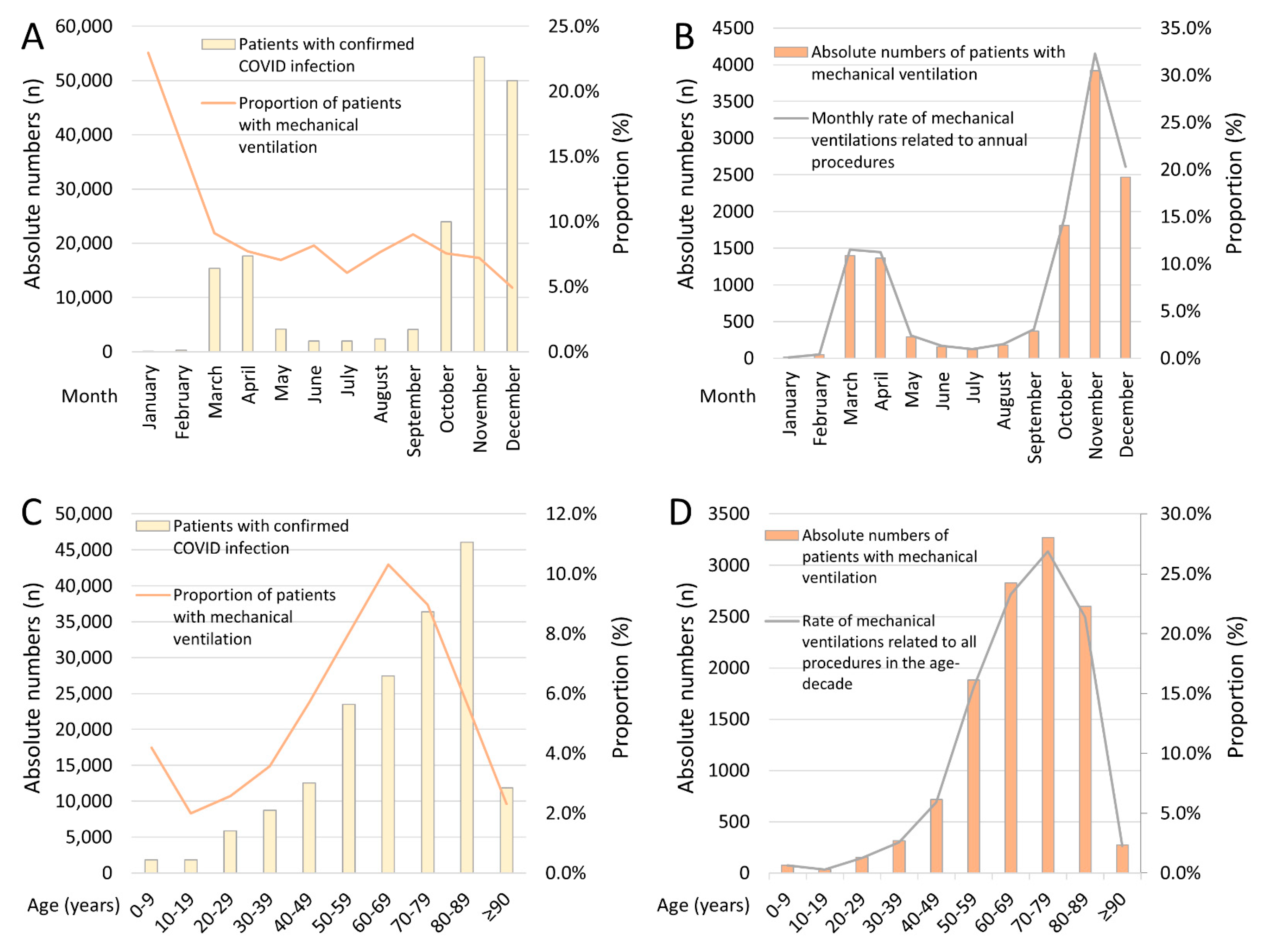
4.3. Seasonal Trends
4.4. Regional Trends of Hospitalized COVID-19 Patients
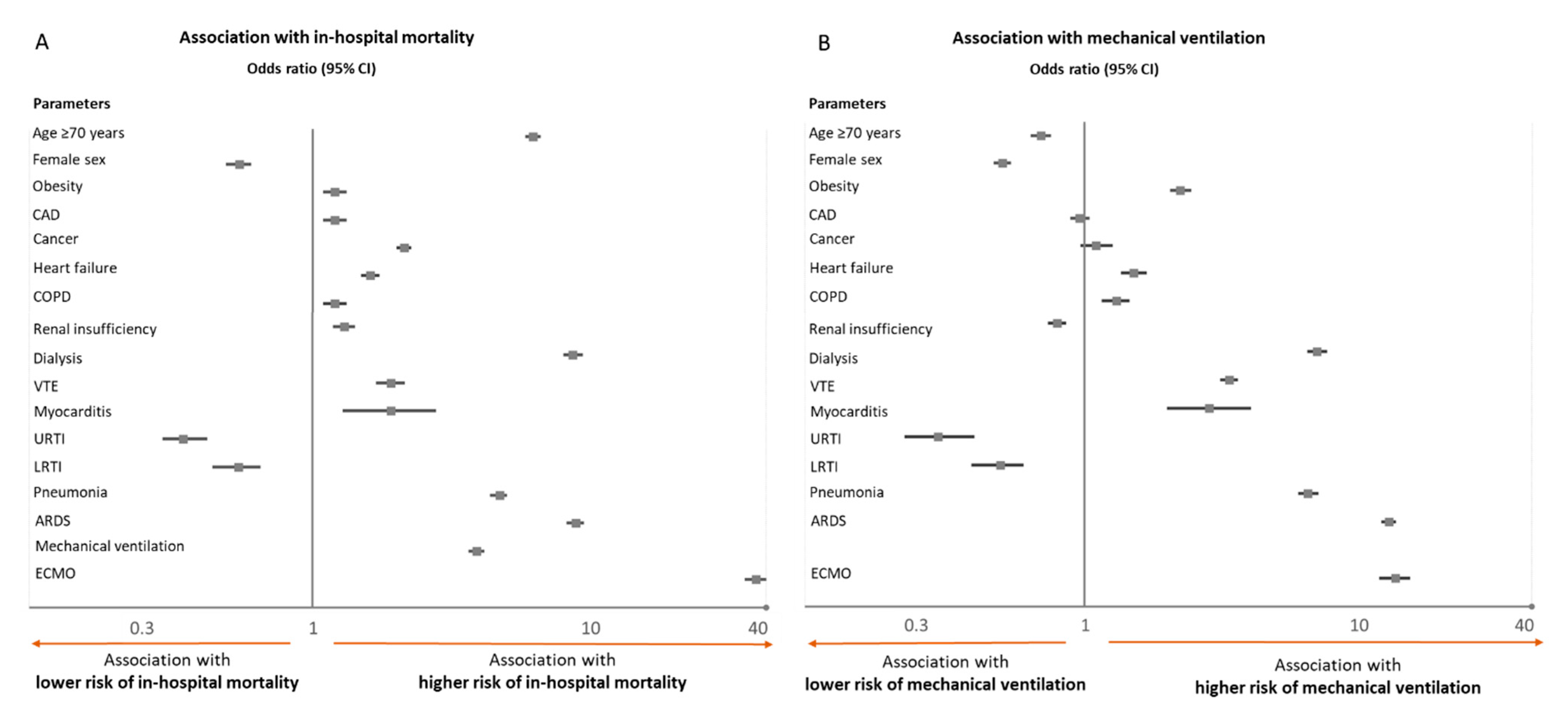
4.5. Predictors of In-Hospital Case-Fatality and Mechanical Ventilation
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guan, W.-J.; Ni, Z.-Y.; Hu, Y.; Liang, W.-H.; Ou, C.-Q.; He, J.-X.; Liu, L.; Shan, H.; Lei, C.-L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Böhmer, M.M.; Buchholz, U.; Corman, V.M.; Hoch, M.; Katz, K.; Marosevic, D.V.; Böhm, S.; Woudenberg, T.; Ackermann, N.; Konrad, R.; et al. Investigation of a COVID-19 outbreak in Germany resulting from a single travel-associated primary case: A case series. Lancet Infect. Dis. 2020, 20, 920–928. [Google Scholar] [CrossRef]
- Ullrich, A.; Schranz, M.; Rexroth, U.; Hamouda, O.; Schaade, L.; Diercke, M.; Boender, T.S. Impact of the COVID-19 pandemic and associated non-pharmaceutical interventions on other notifiable infectious diseases in Germany: An analysis of national surveillance data during week 1–2016—week 32–2020. Lancet Reg. Health Eur. 2021, 6, 100103. [Google Scholar] [CrossRef]
- Karagiannidis, C.; Windisch, W.; McAuley, D.F.; Welte, T.; Busse, R. Major differences in ICU admissions during the first and second COVID-19 wave in Germany. Lancet Respir. Med. 2021, 9, e47–e48. [Google Scholar] [CrossRef]
- Karagiannidis, C.; Mostert, C.; Hentschker, C.; Voshaar, T.; Malzahn, J.; Schillinger, G.; Klauber, J.; Janssens, U.; Marx, G.; Weber-Carstens, S.; et al. Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: An observational study. Lancet Respir. Med. 2020, 8, 853–862. [Google Scholar] [CrossRef]
- Johns Hopkins University. Center for Systems Science and Engineering CSSE. Coronavirus Resource Center. Available online: https://coronavirus.jhu.edu/ (accessed on 25 November 2021).
- Surveillance RKsID. Wöchentlicher Lagebericht des RKI zur Coronavirus-Krankheit-2019 (COVID-19). Available online: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/Wochenbericht/Wochenbericht_2021-11-25.pdf?__blob=publicationFile (accessed on 25 November 2021).
- Keller, K.; Hobohm, L.; Ostad, M.A.; Göbel, S.; Lankeit, M.; Konstantinides, S.; Münzel, T.; Wenzel, P. Temporal trends and predictors of inhospital death in patients hospitalised for heart failure in Germany. Eur. J. Prev. Cardiol. 2020, 28, 990–997. [Google Scholar] [CrossRef]
- Reinöhl, J.; Kaier, K.; Reinecke, H.; Schmoor, C.; Frankenstein, L.; Vach, W.; Cribier, A.; Beyersdorf, F.; Bode, C.; Zehender, M. Effect of Availability of Transcatheter Aortic-Valve Replacement on Clinical Practice. N. Engl. J. Med. 2015, 373, 2438–2447. [Google Scholar] [CrossRef]
- Keller, K.; Hobohm, L.; Ebner, M.; Kresoja, K.-P.; Münzel, T.; Konstantinides, S.V.; Lankeit, M. Trends in thrombolytic treatment and outcomes of acute pulmonary embolism in Germany. Eur. Heart J. 2020, 41, 522–529. [Google Scholar] [CrossRef] [Green Version]
- Gupta, A.; Gonzalez-Rojas, Y.; Juarez, E. Early Treatment for COVID-19 with SARS-CoV-2 Neutralizing Antibody Sotrovimab. N. Engl. J. Med. 2021, 385, 1941–1950. [Google Scholar] [CrossRef]
- Tragaki, A.; Richard, J. First wave of SARS-COV2 in Europe: Study and typology of the 15 worst affected European countries. Popul. Space Place 2021, e2534. [Google Scholar] [CrossRef] [PubMed]
- Souris, M.; Gonzalez, J.-P. COVID-19: Spatial analysis of hospital case-fatality rate in France. PLoS ONE 2020, 15, e0243606. [Google Scholar] [CrossRef]
- Lopez Bernal, J.; Andrews, N.; Gower, C. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on Covid-19 related symptoms, hospital admissions, and mortality in older adults in England: Test negative case-control study. BMJ 2021, 373, n1088. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Tartof, S.Y.; Slezak, J.M.; Fischer, H.; Hong, V.; Ackerson, B.K.; Ranasinghe, O.N.; Frankland, T.B.; Ogun, O.A.; Zamparo, J.M.; Gray, S.; et al. Effectiveness of mRNA BNT162b2 COVID-19 vaccine up to 6 months in a large integrated health system in the USA: A retrospective cohort study. Lancet 2021, 398, 1407–1416. [Google Scholar] [CrossRef]
- Baden, L.R.; El Sahly, H.M.; Essink, B. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef] [PubMed]
- Tenforde, M.W.; Self, W.H.; Adams, K.; Gaglani, M.; Ginde, A.A.; McNeal, T.; Ghamande, S.; Douin, D.J.; Talbot, H.K.; Casey, J.D.; et al. Association Between mRNA Vaccination and COVID-19 Hospitalization and Disease Severity. JAMA J. Am. Med Assoc. 2021, 326, 2043. [Google Scholar] [CrossRef]
- Goldberg, Y.; Mandel, M.; Bar-On, Y.M.; Bodenheimer, O.; Freedman, L.; Haas, E.J.; Milo, R.; Alroy-Preis, S.; Ash, N.; Huppert, A. Waning Immunity after the BNT162b2 Vaccine in Israel. N. Engl. J. Med. 2021, 385, e85. [Google Scholar] [CrossRef]
- Bar-On, Y.M.; Goldberg, Y.; Mandel, M.; Bodenheimer, O.; Freedman, L.; Kalkstein, N.; Mizrahi, B.; Alroy-Preis, S.; Ash, N.; Milo, R.; et al. Protection of BNT162b2 Vaccine Booster against COVID-19 in Israel. N. Engl. J. Med. 2021, 385, 1393–1400. [Google Scholar] [CrossRef]
- Goyal, P.; Choi, J.J.; Pinheiro, L.C.; Schenck, E.J.; Chen, R.; Jabri, A.; Satlin, M.J.; Campion, T.R., Jr.; Nahid, M.; Ringel, J.B.; et al. Clinical Characteristics of COVID-19 in New York City. N. Engl. J. Med. 2020, 382, 2372–2374. [Google Scholar] [CrossRef]
- Petrilli, C.M.; Jones, S.A.; Yang, J.; Rajagopalan, H.; O’Donnell, L.; Chernyak, Y.; Tobin, K.A.; Cerfolio, R.J.; Francois, F.; Horwitz, L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 2020, 369, m1966. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Ling, Y.; Bai, T.; Xie, Y.; Huang, J.; Li, J.; Xiong, W.; Yang, D.; Chen, R.; Lu, F.; et al. COVID-19 with Different Severities: A Multicenter Study of Clinical Features. Am. J. Respir. Crit. Care Med. 2020, 201, 1380–1388. [Google Scholar] [CrossRef] [PubMed]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; The Northwell COVID-19 Research Consortium. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized with COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef] [PubMed]
- O’Driscoll, M.; Ribeiro Dos Santos, G.; Wang, L. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature 2021, 590, 140–145. [Google Scholar] [CrossRef]
- Cho, S.I.; Yoon, S.; Lee, H.-J. Impact of comorbidity burden on mortality in patients with COVID-19 using the Korean health insurance database. Sci. Rep. 2021, 11, 6375. [Google Scholar] [CrossRef]
| Parameters | Survivors (n = 144,530; 82.1%) | Non-Survivors (n = 31,607; 17.9%) | p-Value |
|---|---|---|---|
| Age | 67.0 (52.0/80.0) | 82.0 (76.0/87.0) | <0.001 |
| Age ≥ 70 years | 67,207 (46.5%) | 27,122 (85.8%) | <0.001 |
| Female sex | 70,693 (48.9%) | 13,256 (41.9%) | <0.001 |
| In-hospital stay (days) | 8.0 (4.0/14.0) | 8.0 (4.0/16.0) | <0.001 |
| Cardiovascular risk factors | |||
| Obesity | 7798 (5.4%) | 1585 (5.0%) | 0.006 |
| Diabetes mellitus | 34,241 (23.7%) | 10,991 (34.8%) | <0.001 |
| Essential arterial hypertension | 66,191 (45.8%) | 16,289 (51.5%) | <0.001 |
| Hyperlipidaemia | 22,205 (15.4%) | 5368 (17.0%) | <0.001 |
| Comorbidities | |||
| Coronary artery disease | 18,356 (12.7%) | 7218 (22.8%) | <0.001 |
| Heart failure | 17,400 (12.0%) | 9719 (30.7%) | <0.001 |
| Peripheral artery disease | 3834 (2.7%) | 1806 (5.7%) | <0.001 |
| Atrial fibrillation/flutter | 23,214 (16.1%) | 10,946 (34.6%) | <0.001 |
| Chronic obstructive pulmonary disease | 8865 (6.1%) | 3289 (10.4%) | <0.001 |
| Chronic renal insufficiency (glomerular filtration rate < 60 mL/min/1.73 m2) | 17,976 (12.4%) | 9396 (29.7%) | <0.001 |
| Cancer | 6405 (4.4%) | 2596 (8.2%) | <0.001 |
| Severe liver disease | 2167 (1.5%) | 1972 (6.2%) | <0.001 |
| Charlson comorbidity index | 3.0 (1.0/5.0) | 6.0 (5.0/8.0) | <0.001 |
| Respiratory manifestations of COVID-19 | |||
| Pneumonia | 80,042 (55.4%) | 26,871 (85.0%) | <0.001 |
| Acute respiratory distress syndrome | 5990 (4.1%) | 5604 (17.7%) | <0.001 |
| Treatment | |||
| Intensive care unit | 16,662 (11.5%) | 10,391 (32.9%) | <0.001 |
| Mechanical ventilation | 7655 (5.3%) | 4487 (14.2%) | <0.001 |
| Extracorporeal membrane oxygenation (ECMO) | 445 (0.3%) | 1009 (3.2%) | <0.001 |
| Dialysis | 2388 (1.7%) | 3187 (10.1%) | <0.001 |
| Adverse events during hospitalization | |||
| Cardio-pulmonary resuscitation | 551 (0.4%) | 2308 (7.3%) | <0.001 |
| Venous thromboembolism | 3655 (2.5%) | 1332 (4.2%) | <0.001 |
| Acute kidney failure | 10,911 (7.5%) | 11,164 (35.3%) | <0.001 |
| Myocarditis | 171 (0.1%) | 55 (0.2%) | 0.012 |
| Myocardial infarction | 1677 (1.2%) | 1076 (3.4%) | <0.001 |
| Stroke (ischaemic or haemorrhagic) | 2179 (1.5%) | 1017 (3.2%) | <0.001 |
| Intracerebral bleeding | 301 (0.2%) | 275 (0.9%) | <0.001 |
| Gastro-intestinal bleeding | 1802 (1.2%) | 1146 (3.6%) | <0.001 |
| Transfusion of blood constituents | 7895 (5.5%) | 5979 (18.9%) | <0.001 |
| Parameters | No Mechanical Ventilation (n = 163,995; 93.1%) | Mechanical Ventilation (n = 12,142; 6.9%) | p-Value |
|---|---|---|---|
| Age | 72.0 (55.0/82.0) | 70.0 (59.0/79.0) | <0.001 |
| Age ≥ 70 years | 88,192 (53.8%) | 6137 (50.5%) | <0.001 |
| Female sex | 79,997 (48.8%) | 3952 (32.5%) | <0.001 |
| In-hospital stay (days) | 7.0 (3.0/13.0) | 17.0 (10.0/29.0) | <0.001 |
| Cardiovascular risk factors | |||
| Obesity | 7945 (4.8%) | 1438 (11.8%) | <0.001 |
| Diabetes mellitus | 40,795 (24.9%) | 4437 (36.5%) | <0.001 |
| Essential arterial hypertension | 75,850 (46.3%) | 6630 (54.6%) | <0.001 |
| Hyperlipidaemia | 25,470 (15.5%) | 2103 (17.3%) | <0.001 |
| Comorbidities | |||
| Coronary artery disease | 23,366 (14.2%) | 2208 (18.2%) | <0.001 |
| Heart failure | 24,316 (14.8%) | 2803 (23.1%) | <0.001 |
| Peripheral artery disease | 5122 (3.1%) | 518 (4.3%) | <0.001 |
| Atrial fibrillation/flutter | 30,877 (18.8%) | 3283 (27.0%) | <0.001 |
| Chronic obstructive pulmonary disease | 10,926 (6.7%) | 1228 (10.1%) | <0.001 |
| Chronic renal insufficiency (glomerular filtration rate < 60 mL/min/1.73 m2) | 25,373 (15.5%) | 1999 (16.5%) | 0.004 |
| Cancer | 8331 (5.1%) | 670 (5.5%) | 0.036 |
| Severe liver disease | 3206 (2.0%) | 933 (7.7%) | <0.001 |
| Charlson comorbidity index | 4.0 (2.0/6.0) | 5.0 (3.0/7.0) | <0.001 |
| Respiratory manifestations of COVID-19 | |||
| Pneumonia | 95,918 (58.5%) | 10,995 (90.6%) | <0.001 |
| Acute respiratory distress syndrome | 6847 (4.2%) | 4747 (39.1%) | <0.001 |
| Treatment | |||
| Intensive care unit | 17,631 (10.8%) | 9422 (77.6%) | <0.001 |
| Extracorporeal membrane oxygenation (ECMO) | 677 (0.4%) | 777 (6.4%) | <0.001 |
| Dialysis | 3699 (2.3%) | 1876 (15.5%) | <0.001 |
| Adverse events during hospitalization | |||
| In-hospital case fatality | 27,120 (16.5%) | 4487 (37.0%) | <0.001 |
| Cardio-pulmonary resuscitation | 2107 (1.3%) | 752 (6.2%) | <0.001 |
| Venous thromboembolism | 3993 (2.4%) | 994 (8.2%) | <0.001 |
| Acute kidney failure | 17,688 (10.8%) | 4387 (36.1%) | <0.001 |
| Myocarditis | 181 (0.1%) | 45 (0.4%) | <0.001 |
| Myocardial infarction | 2425 (1.5%) | 328 (2.7%) | <0.001 |
| Stroke (ischaemic or haemorrhagic) | 2813 (1.7%) | 383 (3.2%) | <0.001 |
| Intracerebral bleeding | 437 (0.3%) | 139 (1.1%) | <0.001 |
| Gastro-intestinal bleeding | 2559 (1.6%) | 389 (3.2%) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hobohm, L.; Sagoschen, I.; Barco, S.; Schmidtmann, I.; Espinola-Klein, C.; Konstantinides, S.; Münzel, T.; Keller, K. Trends and Risk Factors of In-Hospital Mortality of Patients with COVID-19 in Germany: Results of a Large Nationwide Inpatient Sample. Viruses 2022, 14, 275. https://doi.org/10.3390/v14020275
Hobohm L, Sagoschen I, Barco S, Schmidtmann I, Espinola-Klein C, Konstantinides S, Münzel T, Keller K. Trends and Risk Factors of In-Hospital Mortality of Patients with COVID-19 in Germany: Results of a Large Nationwide Inpatient Sample. Viruses. 2022; 14(2):275. https://doi.org/10.3390/v14020275
Chicago/Turabian StyleHobohm, Lukas, Ingo Sagoschen, Stefano Barco, Irene Schmidtmann, Christine Espinola-Klein, Stavros Konstantinides, Thomas Münzel, and Karsten Keller. 2022. "Trends and Risk Factors of In-Hospital Mortality of Patients with COVID-19 in Germany: Results of a Large Nationwide Inpatient Sample" Viruses 14, no. 2: 275. https://doi.org/10.3390/v14020275
APA StyleHobohm, L., Sagoschen, I., Barco, S., Schmidtmann, I., Espinola-Klein, C., Konstantinides, S., Münzel, T., & Keller, K. (2022). Trends and Risk Factors of In-Hospital Mortality of Patients with COVID-19 in Germany: Results of a Large Nationwide Inpatient Sample. Viruses, 14(2), 275. https://doi.org/10.3390/v14020275








