Uncovering the Burden of Dengue in Africa: Considerations on Magnitude, Misdiagnosis, and Ancestry
Abstract
1. Introduction
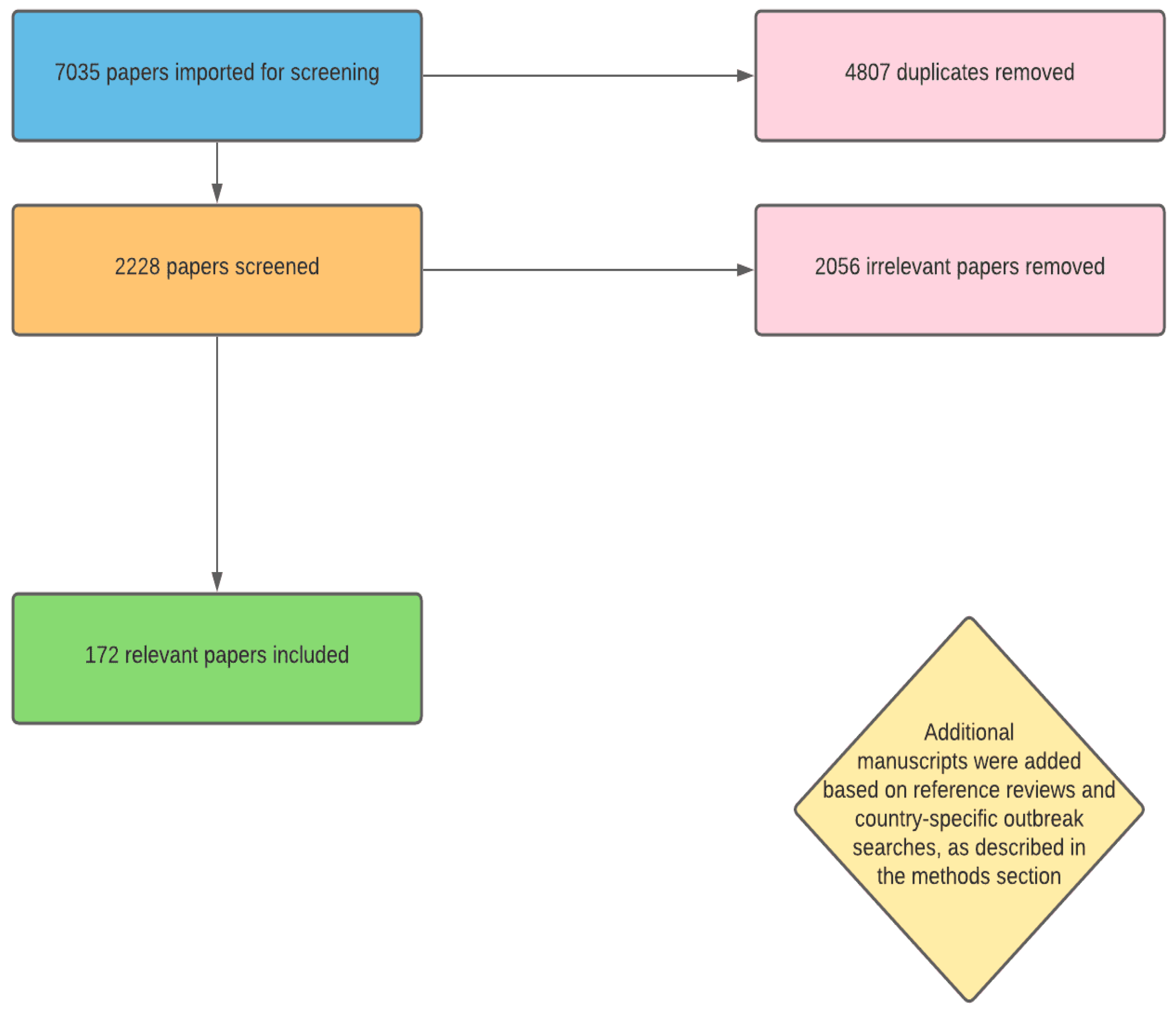
2. Methods
3. Results and Discussion
3.1. Dengue in Africa: Epidemiologic Characteristics and Considerations
3.2. Malaria and Dengue: A Diagnostic Nightmare
3.3. Malaria and Dengue: The Added Complication of Co-Infections
3.4. African Ancestry and Protection from Severe Dengue: Genetics, Social Factors, and Impacts
4. Conclusions and Next Steps
Author Contributions
Funding
Conflicts of Interest
References
- Neglected Tropical Diseases. Available online: https://www.who.int/news-room/q-a-detail/neglected-tropical-diseases (accessed on 20 June 2021).
- About Dengue: What You Need to Know. Available online: https://www.cdc.gov/dengue/about/index.html (accessed on 20 June 2021).
- Cattarino, L.; Rodriguez-Barraquer, I.; Imai, N.; Cummings, D.A.T.; Ferguson, N.M. Mapping global variation in dengue transmission intensity. Sci. Transl. Med. 2020, 12, 528. [Google Scholar] [CrossRef]
- Gubler, D.J.; Clark, G.G. Dengue/dengue hemorrhagic fever: The emergence of a global health problem. Emerg. Infect. Dis. 1995, 1, 55–57. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, S.; Gething, P.W.; Brady, O.J.; Messina, J.P.; Farlow, A.W.; Moyes, C.L.; Drake, J.M.; Brownstein, J.S.; Hoen, A.G.; Sankoh, O.; et al. The global distribution and burden of dengue. Nature 2013, 496, 504–507. [Google Scholar] [CrossRef]
- Gwee, S.X.W.; St John, A.L.; Gray, G.C.; Pang, J. Animals as potential reservoirs for dengue transmission: A systematic review. One Health 2021, 12, 100216. [Google Scholar] [CrossRef] [PubMed]
- Back, A.T.; Lundkvist, A. Dengue viruses—An overview. Infect. Ecol. Epidemiol. 2013, 3, 19839. [Google Scholar] [CrossRef]
- Murray, N.E.; Quam, M.B.; Wilder-Smith, A. Epidemiology of dengue: Past, present and future prospects. Clin. Epidemiol. 2013, 5, 299–309. [Google Scholar] [CrossRef]
- Guzman, M.G.; Harris, E. Dengue. Lancet 2015, 385, 453–465. [Google Scholar] [CrossRef]
- Dengue and Severe Dengue. Available online: https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue (accessed on 20 June 2021).
- World Health Organization. Dengue Haemorrhagic Fever: Diagnosis, Treatment, Prevention and Control, 2nd ed.; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- Kalayanarooj, S. Clinical Manifestations and Management of Dengue/DHF/DSS. Trop. Med. Health 2011, 39, 83–87. [Google Scholar] [CrossRef]
- World Health Organization. Dengue Guidelines for Diagnosis, Treatment, Prevention and Control: New Edition; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Gubler, D.J. Epidemic dengue/dengue hemorrhagic fever as a public health, social and economic problem in the 21st century. Trends Microbiol. 2002, 10, 100–103. [Google Scholar] [CrossRef]
- Chotpitayasunondh, T. Introduction on the global dengue epidemiological burden. Int. J. Infect. Dis. 2012, 16, e4. [Google Scholar] [CrossRef][Green Version]
- Braack, L.; Gouveia De Almeida, A.P.; Cornel, A.J.; Swanepoel, R.; De Jager, C. Mosquito-borne arboviruses of African origin: Review of key viruses and vectors. Parasites Vectors 2018, 11, 29. [Google Scholar] [CrossRef] [PubMed]
- Pierson, T.C.; Diamond, M.S. The continued threat of emerging flaviviruses. Nat. Microbiol. 2020, 5, 796–812. [Google Scholar] [CrossRef] [PubMed]
- Weetman, D.; Kamgang, B.; Badolo, A.; Moyes, C.L.; Shearer, F.M.; Coulibaly, M.; Pinto, J.; Lambrechts, L.; McCall, P.J. Aedes Mosquitoes and Aedes-Borne Arboviruses in Africa: Current and Future Threats. Int. J. Environ. Res. Public Health 2018, 15, 220. [Google Scholar] [CrossRef] [PubMed]
- Guzman, M.G.; Alvarez, M.; Halstead, S.B. Secondary infection as a risk factor for dengue hemorrhagic fever/dengue shock syndrome: An historical perspective and role of antibody-dependent enhancement of infection. Arch. Virol. 2013, 158, 1445–1459. [Google Scholar] [CrossRef]
- Katzelnick, L.C.; Gresh, L.; Halloran, M.E.; Mercado, J.C.; Kuan, G.; Gordon, A.; Balmaseda, A.; Harris, E. Antibody-dependent enhancement of severe dengue disease in humans. Science 2017, 358, 929–932. [Google Scholar] [CrossRef]
- Katzelnick, L.C.; Narvaez, C.; Arguello, S.; Lopez Mercado, B.; Collado, D.; Ampie, O.; Elizondo, D.; Miranda, T.; Bustos Carillo, F.; Mercado, J.C.; et al. Zika virus infection enhances future risk of severe dengue disease. Science 2020, 369, 1123–1128. [Google Scholar] [CrossRef]
- Vaccines and Immunization: Dengue. Available online: https://www.who.int/news-room/q-a-detail/dengue-vaccines (accessed on 20 June 2021).
- Wen, J.; Shresta, S. Antigenic cross-reactivity between Zika and dengue viruses: Is it time to develop a universal vaccine? Curr. Opin. Immunol. 2019, 59, 1–8. [Google Scholar] [CrossRef]
- Caldwell, J.M.; Labeaud, A.D.; Lambin, E.F.; Stewart-Ibarra, A.M.; Ndenga, B.A.; Mutuku, F.M.; Krystosik, A.R.; Ayala, E.B.; Anyamba, A.; Borbor-Cordova, M.J.; et al. Climate predicts geographic and temporal variation in mosquito-borne disease dynamics on two continents. Nat. Commun. 2021, 12, 1233. [Google Scholar] [CrossRef]
- Tjaden, N.B.; Thomas, S.M.; Fischer, D.; Beierkuhnlein, C. Extrinsic Incubation Period of Dengue: Knowledge, Backlog, and Applications of Temperature Dependence. PLoS Negl. Trop. Dis. 2013, 7, e2207. [Google Scholar] [CrossRef]
- Githeko, A.K.; Lindsay, S.W.; Confalonieri, U.E.; Patz, J.A. Climate change and vector-borne diseases: A regional analysis. Bull. World Health Org. 2000, 78, 1136–1147. [Google Scholar]
- Nosrat, C.; Altamirano, J.; Anyamba, A.; Caldwell, J.M.; Damoah, R.; Mutuku, F.; Ndenga, B.; Labeaud, A.D. Impact of recent climate extremes on mosquito-borne disease transmission in Kenya. PLoS Negl. Trop. Dis. 2021, 15, e0009182. [Google Scholar] [CrossRef] [PubMed]
- Ebi, K.L.; Nealon, J. Dengue in a changing climate. Environ. Res 2016, 151, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Krystosik, A.; Njoroge, G.; Odhiambo, L.; Forsyth, J.E.; Mutuku, F.; LaBeaud, A.D. Solid Wastes Provide Breeding Sites, Burrows, and Food for Biological Disease Vectors, and Urban Zoonotic Reservoirs: A Call to Action for Solutions-Based Research. Front. Public Health 2019, 7, 405. [Google Scholar] [CrossRef] [PubMed]
- Were, F. The dengue situation in Africa. Paediatr. Int. Child Health 2012, 32 (Suppl. S1), 18–21. [Google Scholar] [CrossRef] [PubMed]
- Harapan, H.; Michie, A.; Sasmono, R.T.; Imrie, A. Dengue: A Minireview. Viruses 2020, 12, 829. [Google Scholar] [CrossRef]
- Mulligan, K.; Dixon, J.; Joanna Sinn, C.-L.; Elliott, S.J. Is dengue a disease of poverty? A systematic review. Pathog. Glob. Health 2015, 109, 10–18. [Google Scholar] [CrossRef]
- Patel, N. Figure of the Week: Understanding Poverty in Africa; Brookings: Washington, DC, USA, 2018. [Google Scholar]
- Shepard, D.S.; Undurraga, E.A.; Halasa, Y.A.; Stanaway, J.D. The global economic burden of dengue: A systematic analysis. Lancet Infect. Dis. 2016, 16, 935–941. [Google Scholar] [CrossRef]
- Amarasinghe, A.; Kuritsk, J.N.; Letson, G.W.; Margolis, H.S. Dengue virus infection in Africa. Emerg. Infect. Dis. 2011, 17, 1349–1354. [Google Scholar] [CrossRef]
- Jaenisch, T.; Junghanss, T.; Wills, B.; Brady, O.J.; Eckerle, I.; Farlow, A.; Hay, S.I.; McCall, P.J.; Messina, J.P.; Ofula, V.; et al. Dengue expansion in Africa-not recognized or not happening? Emerg. Infect. Dis. 2014, 20, e140487. [Google Scholar] [CrossRef]
- Simo, F.B.N.; Bigna, J.J.; Kenmoe, S.; Ndangang, M.S.; Temfack, E.; Moundipa, P.F.; Demanou, M. Dengue virus infection in people residing in Africa: A systematic review and meta-analysis of prevalence studies. Sci. Rep. 2019, 9, 13626. [Google Scholar] [CrossRef]
- Humphrey, J.M.; Cleton, N.B.; Reusken, C.B.; Glesby, M.J.; Koopmans, M.P.; Abu-Raddad, L.J. Dengue in the Middle East and North Africa: A Systematic Review. PLoS Negl. Trop. Dis. 2016, 10, e0005194. [Google Scholar] [CrossRef]
- Shah, M.; Ndenga, B.; Mutuku, F.; Vu, D.; Grossi-Soyster, E.; Okuta, V.; Ronga, C.; Chebii, P.; Maina, P.; Jembe, Z.; et al. High Dengue Burden and Circulation of 4 Virus Serotypes among Children with Undifferentiated Fever, Kenya, 2014–2017. Emerg. Infect. Dis. J. 2020, 26, 2638. [Google Scholar] [CrossRef] [PubMed]
- Standard Country or Area Codes for Statistical Use. Available online: https://unstats.un.org/unsd/methodology/m49/ (accessed on 20 June 2021).
- Dengue around the World. Available online: https://www.cdc.gov/dengue/areaswithrisk/around-the-world.html (accessed on 20 June 2021).
- Dengue Fever—Republic of the Sudan, 22 November 2019. Available online: https://reliefweb.int/report/sudan/dengue-fever-republic-sudan-22-november-2019 (accessed on 20 June 2021).
- Baba, M.; Villinger, J.; Masiga, D.K. Repetitive dengue outbreaks in East Africa: A proposed phased mitigation approach may reduce its impact. Rev. Med. Virol. 2016, 26, 183–196. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Ali, Y.; Elmagboul, B.; Mohamed, O.; Elduma, A.; Bashab, H.; Mahamoud, A.; Khogali, H.; Elaagip, A.; Higazi, T. Dengue Fever in the Darfur Area, Western Sudan. Emerg. Infect. Dis. 2019, 25, 2126. [Google Scholar] [CrossRef] [PubMed]
- Dengue Fever—Egypt. Available online: https://www.who.int/emergencies/disease-outbreak-news/item/12-november-2015-dengue-en (accessed on 20 June 2021).
- Usman, A.; Ball, J.D.; Rojas, D.P.; Berhane, A.; Ghebrat, Y.; Mebrahtu, G.; Gebresellasie, A.; Zehaie, A.; Mufunda, J.; Liseth, O.; et al. Dengue fever outbreaks in Eritrea, 2005–2015: A case for strengthening surveillance, control and reporting. Glob. Health Res. Policy 2016, 1, 17. [Google Scholar] [CrossRef]
- Le Gonidec, E.; Maquart, M.; Duron, S.; Savini, H.; Cazajous, G.; Vidal, P.O.; Chenilleau, M.C.; Roseau, J.B.; Benois, A.; Dehan, C.; et al. Clinical Survey of Dengue Virus Circulation in the Republic of Djibouti between 2011 and 2014 Identifies Serotype 3 Epidemic and Recommends Clinical Diagnosis Guidelines for Resource Limited Settings. PLoS Negl. Trop. Dis. 2016, 10, e0004755. [Google Scholar] [CrossRef]
- Degife, L.H.; Worku, Y.; Belay, D.; Bekele, A.; Hailemariam, Z. Factors associated with dengue fever outbreak in Dire Dawa administration city, October, 2015, Ethiopia—Case control study. BMC Public Health 2019, 19, 650. [Google Scholar] [CrossRef]
- Gutu, M.A.; Bekele, A.; Seid, Y.; Mohammed, Y.; Gemechu, F.; Woyessa, A.B.; Tayachew, A.; Dugasa, Y.; Gizachew, L.; Idosa, M.; et al. Another dengue fever outbreak in Eastern Ethiopia-An emerging public health threat. PLoS Negl. Trop. Dis. 2021, 15, e0008992. [Google Scholar] [CrossRef]
- Salah, Y.M.A.a.A.A. Epidemiology of Dengue Fever in Ethiopian Somali Region: Retrospective Health Facility Based Study. Cent. Afr. J. Public Health 2016, 2, 51–56. [Google Scholar] [CrossRef]
- Ellis, E.M.; Neatherlin, J.C.; Delorey, M.; Ochieng, M.; Mohamed, A.H.; Mogeni, D.O.; Hunsperger, E.; Patta, S.; Gikunju, S.; Waiboic, L.; et al. A household serosurvey to estimate the magnitude of a dengue outbreak in Mombasa, Kenya, 2013. PLoS Negl. Trop. Dis. 2015, 9, e0003733. [Google Scholar] [CrossRef]
- Langat, S.K.; Eyase, F.L.; Berry, I.M.; Nyunja, A.; Bulimo, W.; Owaka, S.; Ofula, V.; Limbaso, S.; Lutomiah, J.; Jarman, R.; et al. Origin and evolution of dengue virus type 2 causing outbreaks in Kenya: Evidence of circulation of two cosmopolitan genotype lineages. Virus Evol. 2020, 6, veaa026. [Google Scholar] [CrossRef] [PubMed]
- Lutomiah, J.; Barrera, R.; Makio, A.; Mutisya, J.; Koka, H.; Owaka, S.; Koskei, E.; Nyunja, A.; Eyase, F.; Coldren, R.; et al. Dengue Outbreak in Mombasa City, Kenya, 2013–2014: Entomologic Investigations. PLoS Negl. Trop. Dis. 2016, 10, e0004981. [Google Scholar] [CrossRef] [PubMed]
- Obonyo, M.; Fidhow, A.; Ofula, V. Investigation of laboratory confirmed Dengue outbreak in North-eastern Kenya, 2011. PLoS ONE 2018, 13, e0198556. [Google Scholar] [CrossRef] [PubMed]
- Bosa, H.K.; Montgomery, J.M.; Kimuli, I.; Lutwama, J.J. Dengue fever outbreak in Mogadishu, Somalia 2011: Co-circulation of three dengue virus serotypes. Int. J. Infect. Dis. 2014, 21, 3. [Google Scholar] [CrossRef]
- Chipwaza, B.; Sumaye, R.D.; Weisser, M.; Gingo, W.; Yeo, N.K.; Amrun, S.N.; Okumu, F.O.; Ng, L.F.P. Occurrence of 4 Dengue Virus Serotypes and Chikungunya Virus in Kilombero Valley, Tanzania, During the Dengue Outbreak in 2018. Open Forum Infect. Dis. 2021, 8, ofaa626. [Google Scholar] [CrossRef]
- Mboera, L.E.; Mweya, C.N.; Rumisha, S.F.; Tungu, P.K.; Stanley, G.; Makange, M.R.; Misinzo, G.; De Nardo, P.; Vairo, F.; Oriyo, N.M. The Risk of Dengue Virus Transmission in Dar es Salaam, Tanzania during an Epidemic Period of 2014. PLoS Negl. Trop. Dis. 2016, 10, e0004313. [Google Scholar] [CrossRef]
- World Health Organization Regional Office for Africa-Weekly Bulletin on Outbreaks and Other Emergencies: Week 27: 01–07 July 2019. Available online: https://apps.who.int/iris/bitstream/handle/10665/325777/OEW27-0107072019.pdf (accessed on 3 November 2021).
- Massangaie, M.; Pinto, G.; Padama, F.; Chambe, G.; da Silva, M.; Mate, I.; Chirindza, C.; Ali, S.; Agostinho, S.; Chilaule, D.; et al. Clinical and Epidemiological Characterization of the First Recognized Outbreak of Dengue Virus-Type 2 in Mozambique, 2014. Am. J. Trop. Med. Hyg. 2016, 94, 413–416. [Google Scholar] [CrossRef]
- Lustig, Y.; Wolf, D.; Halutz, O.; Schwartz, E. An outbreak of dengue virus (DENV) type 2 Cosmopolitan genotype in Israeli travellers returning from the Seychelles, April 2017. Eurosurveillance 2017, 22, 30563. [Google Scholar] [CrossRef]
- Seychelles: Dengue Outbreak Emergency Plan of Action Final Report. Available online: https://reliefweb.int/report/seychelles/seychelles-dengue-outbreak-emergency-plan-action-final-report-dref-operation-n (accessed on 20 June 2021).
- Mazaba-Liwewe, M.L.; Siziya, S.; Monze, M.; Mweene-Ndumba, I.; Masaninga, F.; Songolo, P.; Malama, C.; Chizema, E.; Mwaba, P.; Babaniyi, O.A. First sero-prevalence of dengue fever specific immunoglobulin G antibodies in Western and North-Western provinces of Zambia: A population based cross sectional study. Virol. J. 2014, 11, 135. [Google Scholar] [CrossRef]
- Sharp, T.M.; Moreira, R.; Soares, M.J.; Miguel da Costa, L.; Mann, J.; DeLorey, M.; Hunsperger, E.; Munoz-Jordan, J.L.; Colon, C.; Margolis, H.S.; et al. Underrecognition of Dengue during 2013 Epidemic in Luanda, Angola. Emerg. Infect. Dis. 2015, 21, 1311–1316. [Google Scholar] [CrossRef]
- Nemg Simo, F.B.; Sado Yousseu, F.B.; Evouna Mbarga, A.; Bigna, J.J.; Melong, A.; Ntoude, A.; Kamgang, B.; Bouyne, R.; Moundipa Fewou, P.; Demanou, M. Investigation of an Outbreak of Dengue Virus Serotype 1 in a Rural Area of Kribi, South Cameroon: A Cross-Sectional Study. Intervirology 2018, 61, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Im, J.; Balasubramanian, R.; Ouedraogo, M.; Wandji Nana, L.R.; Mogeni, O.D.; Jeon, H.J.; van Pomeren, T.; Haselbeck, A.; Lim, J.K.; Prifti, K.; et al. The epidemiology of dengue outbreaks in 2016 and 2017 in Ouagadougou, Burkina Faso. Heliyon 2020, 6, e04389. [Google Scholar] [CrossRef] [PubMed]
- Tarnagda, Z.; Cissé, A.; Bicaba, B.W.; Diagbouga, S.; Sagna, T.; Ilboudo, A.K.; Tialla, D.; Lingani, M.; Sondo, K.A.; Yougbaré, I.; et al. Dengue Fever in Burkina Faso, 2016. Emerg. Infect. Dis. J. 2018, 24, 170. [Google Scholar] [CrossRef] [PubMed]
- Dengue Fever—Côte d’Ivoire. Available online: https://www.who.int/emergencies/disease-outbreak-news/item/04-august-2017-dengue-cote-d-ivoire-en (accessed on 20 June 2021).
- Dieng, I.; Cunha, M.; Diagne, M.M.; Sembene, P.M.; Zanotto, P.M.A.; Faye, O.; Faye, O.; Sall, A.A. Origin and Spread of the Dengue Virus Type 1, Genotype V in Senegal, 2015–2019. Viruses 2021, 13, 57. [Google Scholar] [CrossRef] [PubMed]
- Gaye, A.; Ndiaye, T.; Sy, M.; Deme, A.B.; Thiaw, A.B.; Sene, A.; Ndiaye, C.; Diedhiou, Y.; Mbaye, A.M.; Ndiaye, I.; et al. Genomic investigation of a dengue virus outbreak in Thiès, Senegal, in 2018. Sci. Rep. 2021, 11, 10321. [Google Scholar] [CrossRef] [PubMed]
- Elduma, A.H.; LaBeaud, A.D.; Plante, J.A.; Plante, K.S.; Ahmed, A. High Seroprevalence of Dengue Virus Infection in Sudan: Systematic Review and Meta-Analysis. Trop. Med. Infect. Dis. 2020, 5, 120. [Google Scholar] [CrossRef]
- Lim, J.K.; Matendechero, S.H.; Alexander, N.; Lee, J.S.; Lee, K.S.; Namkung, S.; Andia, E.; Oyembo, N.; Lim, S.K.; Kanyi, H.; et al. Clinical and epidemiologic characteristics associated with dengue fever in Mombasa, Kenya. Int. J. Infect. Dis. 2020, 100, 207–215. [Google Scholar] [CrossRef]
- Mwanyika, G.O.; Mboera, L.E.G.; Rugarabamu, S.; Ngingo, B.; Sindato, C.; Lutwama, J.J.; Paweska, J.T.; Misinzo, G. Dengue Virus Infection and Associated Risk Factors in Africa: A Systematic Review and Meta-Analysis. Viruses 2021, 13, 536. [Google Scholar] [CrossRef]
- Adam, A.; Schüttoff, T.; Reiche, S.; Jassoy, C. High seroprevalence of dengue virus indicates that dengue virus infections are frequent in central and eastern Sudan. Trop. Med. Int. Health 2018, 23, 960–967. [Google Scholar] [CrossRef]
- Botros, B.A.; Watts, D.M.; Soliman, A.K.; Salib, A.W.; Moussa, M.I.; Mursal, H.; Douglas, C.; Farah, M. Serological evidence of dengue fever among refugees, Hargeysa, Somalia. J. Med. Virol. 1989, 29, 79–81. [Google Scholar] [CrossRef]
- Budodo, R.M.; Horumpende, P.G.; Mkumbaye, S.I.; Mmbaga, B.T.; Mwakapuja, R.S.; Chilongola, J.O. Serological evidence of exposure to Rift Valley, Dengue and Chikungunya Viruses among agropastoral communities in Manyara and Morogoro regions in Tanzania: A community survey. PLoS Negl. Trop. Dis. 2020, 14, e0008061. [Google Scholar] [CrossRef] [PubMed]
- Chepkorir, E.; Tchouassi, D.P.; Konongoi, S.L.; Lutomiah, J.; Tigoi, C.; Irura, Z.; Eyase, F.; Venter, M.; Sang, R. Serological evidence of Flavivirus circulation in human populations in Northern Kenya: An assessment of disease risk 2016–2017. Virol. J. 2019, 16, 65. [Google Scholar] [CrossRef] [PubMed]
- Chisenga, C.C.; Bosomprah, S.; Musukuma, K.; Mubanga, C.; Chilyabanyama, O.N.; Velu, R.M.; Kim, Y.C.; Reyes-Sandoval, A.; Chilengi, R. Sero-prevalence of arthropod-borne viral infections among Lukanga swamp residents in Zambia. PLoS ONE 2020, 15, e0235322. [Google Scholar] [CrossRef] [PubMed]
- Collenberg, E.; Ouedraogo, T.; Ganamé, J.; Fickenscher, H.; Kynast-Wolf, G.; Becher, H.; Kouyaté, B.; Kräusslich, H.-G.; Sangaré, L.; Tebit, D.M. Seroprevalence of six different viruses among pregnant women and blood donors in rural and urban Burkina Faso: A comparative analysis. J. Med. Virol. 2006, 78, 683–692. [Google Scholar] [CrossRef]
- Elaagip, A.; Alsedig, K.; Altahir, O.; Ageep, T.; Ahmed, A.; Siam, H.A.; Samy, A.M.; Mohamed, W.; Khalid, F.; Gumaa, S.; et al. Seroprevalence and associated risk factors of Dengue fever in Kassala state, eastern Sudan. PLoS Negl. Trop. Dis. 2020, 14, e0008918. [Google Scholar] [CrossRef]
- Eshetu, D.; Shimelis, T.; Nigussie, E.; Shumie, G.; Chali, W.; Yeshitela, B.; Assefa, A.; Gadisa, E. Seropositivity to dengue and associated risk factors among non-malarias acute febrile patients in Arba Minch districts, southern Ethiopia. BMC Infect. Dis. 2020, 20, 639. [Google Scholar] [CrossRef]
- Grossi-Soyster, E.N.; Cook, E.A.J.; de Glanville, W.A.; Thomas, L.F.; Krystosik, A.R.; Lee, J.; Wamae, C.N.; Kariuki, S.; Fevre, E.M.; LaBeaud, A.D. Serological and spatial analysis of alphavirus and flavivirus prevalence and risk factors in a rural community in western Kenya. PLoS Negl. Trop. Dis. 2017, 11, e0005998. [Google Scholar] [CrossRef]
- Guyer, B. Serological survey for arboviruses in Igbo-Ora, western Nigeria. Ann. Trop. Med. Parasitol. 1972, 66, 243–250. [Google Scholar] [CrossRef]
- Himatt, S.; Osman, K.E.; Okoued, S.I.; Seidahmed, O.E.; Beatty, M.E.; Soghaier, M.A.; Elmusharaf, K. Sero-prevalence of dengue infections in the Kassala state in the eastern part of the Sudan in 2011. J. Infect. Public Health 2015, 8, 487–492. [Google Scholar] [CrossRef]
- Hortion, J.; Mutuku, F.M.; Eyherabide, A.L.; Vu, D.M.; Boothroyd, D.B.; Grossi-Soyster, E.N.; King, C.H.; Ndenga, B.A.; LaBeaud, A.D. Acute Flavivirus and Alphavirus Infections among Children in Two Different Areas of Kenya, 2015. Am. J. Trop. Med. Hyg. 2019, 100, 170–173. [Google Scholar] [CrossRef]
- Hussen, M.O.; Sayed, A.S.M.; Abushahba, M.F.N. Sero-epidemiological study on Dengue fever virus in humans and camels at Upper Egypt. Vet. World 2020, 13, 2618–2624. [Google Scholar] [CrossRef] [PubMed]
- Inziani, M.; Adungo, F.; Awando, J.; Kihoro, R.; Inoue, S.; Morita, K.; Obimbo, E.; Onyango, F.; Mwau, M. Seroprevalence of yellow fever, dengue, West Nile and chikungunya viruses in children in Teso South Sub-County, Western Kenya. Int. J. Infect. Dis. 2020, 91, 104–110. [Google Scholar] [CrossRef]
- Kuniholm, M.H.; Wolfe, N.D.; Huang, C.Y.; Mpoudi-Ngole, E.; Tamoufe, U.; LeBreton, M.; Burke, D.S.; Gubler, D.J. Seroprevalence and distribution of Flaviviridae, Togaviridae, and Bunyaviridae arboviral infections in rural Cameroonian adults. Am. J. Trop. Med. Hyg. 2006, 74, 1078–1083. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.K.; Carabali, M.; Lee, J.S.; Lee, K.S.; Namkung, S.; Lim, S.K.; Ridde, V.; Fernandes, J.; Lell, B.; Matendechero, S.H.; et al. Evaluating dengue burden in Africa in passive fever surveillance and seroprevalence studies: Protocol of field studies of the Dengue Vaccine Initiative. BMJ Open 2018, 8, e017673. [Google Scholar] [CrossRef] [PubMed]
- Mease, L.E.; Coldren, R.L.; Musila, L.A.; Prosser, T.; Ogolla, F.; Ofula, V.O.; Schoepp, R.J.; Rossi, C.A.; Adungo, N. Seroprevalence and distribution of arboviral infections among rural Kenyan adults: A cross-sectional study. Virol. J. 2011, 8, 371. [Google Scholar] [CrossRef]
- Mengesha Tsegaye, M.; Beyene, B.; Ayele, W.; Abebe, A.; Tareke, I.; Sall, A.; Yactayo, S.; Shibeshi, M.E.; Staples, E.; Belay, D.; et al. Sero-prevalence of yellow fever and related Flavi viruses in Ethiopia: A public health perspective. BMC Public Health 2018, 18, 1011. [Google Scholar] [CrossRef]
- Morrill, J.C.; Johnson, B.K.; Hyams, C.; Okoth, F.; Tukei, P.M.; Mugambi, M.; Woody, J. Serological evidence of arboviral infections among humans of coastal Kenya. J. Trop. Med. Hyg. 1991, 94, 166–168. [Google Scholar]
- Muianga, A.; Falk, K.; Oludele, J.; Pinto, G.; Ali, S.; Tivane, A.T.; Galano, G.; Gudo, E.S.; Lagerqvist, N. Serological and molecular investigation of dengue, chikungunya and rift valey fever in febrile and non-febrile patients from northern Mozambique during Dengue outbreak, 2014. Int. J. Infect. Dis. 2016, 45, 184–185. [Google Scholar] [CrossRef]
- Ochieng, C.; Ahenda, P.; Vittor, A.Y.; Nyoka, R.; Gikunju, S.; Wachira, C.; Waiboci, L.; Umuro, M.; Kim, A.A.; Nderitu, L.; et al. Seroprevalence of Infections with Dengue, Rift Valley Fever and Chikungunya Viruses in Kenya, 2007. PLoS ONE 2015, 10, e0132645. [Google Scholar] [CrossRef]
- Ofula, V.O.; Oundo, J.; Irura, Z.; Chepkorir, E.; Tigoi, C.; Ongus, J.; Coldren, R.; Sang, R.; Schoepp, R.; Rossi, C. Evidence of presence of antibodies against selected arboviruses in Ijara and Marigat Districts, Kenya. Int. J. Infect. Dis. 2016, 45, 188–189. [Google Scholar] [CrossRef][Green Version]
- Oyero, O.G.; Ayukekbong, J.A. High dengue NS1 antigenemia in febrile patients in Ibadan, Nigeria. Virus Res. 2014, 191, 59–61. [Google Scholar] [CrossRef] [PubMed]
- Sawadogo, S.; Baguiya, A.; Yougbare, F.; Bicaba, B.W.; Nebie, K.; Millogo, T.; Kamba, I.; Kaba, L.; Sangare, L.; Kafando, E.; et al. Seroprevalence and factors associated with IgG anti-DENV positivity in blood donors in Burkina Faso during the 2016 dengue outbreak and implications for blood supply. Transfus. Med. 2020, 30, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, N.G.; Girmann, M.; Randriamampionona, N.; Bialonski, A.; Maus, D.; Krefis, A.C.; Njarasoa, C.; Rajanalison, J.F.; Ramandrisoa, H.D.; Randriarison, M.L.; et al. Seroprevalence of antibodies against Chikungunya, Dengue, and Rift Valley fever viruses after febrile illness outbreak, Madagascar. Emerg. Infect. Dis. 2012, 18, 1780–1786. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, L.J.; Cash, A.A.; Huang, Y.J.; Sang, R.C.; Malhotra, I.; Moormann, A.M.; King, C.L.; Weaver, S.C.; King, C.H.; LaBeaud, A.D. Serologic evidence of arboviral infections among humans in Kenya. Am. J. Trop. Med. Hyg. 2011, 85, 158–161. [Google Scholar] [CrossRef]
- Tchuandom, S.B.; Tchouangueu, T.F.; Antonio-Nkondjio, C.; Lissom, A.; Djang, J.O.N.; Atabonkeng, E.P.; Kechia, A.; Nchinda, G.; Kuiate, J.R. Seroprevalence of dengue virus among children presenting with febrile illness in some public health facilities in Cameroon. Pan Afr. Med. J. 2018, 31, 177. [Google Scholar] [CrossRef]
- Vairo, F.; Nicastri, E.; Meschi, S.; Schepisi, M.S.; Paglia, M.G.; Bevilacqua, N.; Mangi, S.; Sciarrone, M.R.; Chiappini, R.; Mohamed, J.; et al. Seroprevalence of dengue infection: A cross-sectional survey in mainland Tanzania and on Pemba Island, Zanzibar. Int. J. Infect. Dis. 2012, 16, e44–e46. [Google Scholar] [CrossRef]
- Ward, T.; Samuel, M.; Maoz, D.; Runge-Ranzinger, S.; Boyce, R.; Toledo, J.; Velayudhan, R.; Horstick, O. Dengue data and surveillance in Tanzania: A systematic literature review. Trop. Med. Int. Health 2017, 22, 960–970. [Google Scholar] [CrossRef]
- Angelo, K.M.; Haulman, N.J.; Terry, A.C.; Leung, D.T.; Chen, L.H.; Barnett, E.D.; Hagmann, S.H.F.; Hynes, N.A.; Connor, B.A.; Anderson, S.; et al. Illness among US resident student travellers after return to the USA: A GeoSentinel analysis, 2007–2017. J. Travel. Med. 2018, 25. [Google Scholar] [CrossRef]
- Badiaga, S.; Barrau, K.; Brouqui, P.; Durant, J.; Malvy, D.; Janbon, F.; Bonnet, E.; Bosseray, A.; Sotto, A.; Peyramont, D.; et al. Imported Dengue in French University Hospitals: A 6-year survey. J. Travel. Med. 2003, 10, 286–289. [Google Scholar]
- Burdino, E.; Milia, M.G.; Sergi, G.; Gregori, G.; Allice, T.; Cazzato, M.L.; Lucchini, A.; Lipani, F.; Calleri, G.; Orofino, G.; et al. Diagnosis of dengue fever in North West Italy in travelers from endemic areas: A retrospective study. J. Clin. Virol. 2011, 51, 259–263. [Google Scholar] [CrossRef]
- Eldin, C.; Gautret, P.; Nougairede, A.; Sentis, M.; Ninove, L.; Saidani, N.; Million, M.; Brouqui, P.; Charrel, R.; Parola, P. Identification of dengue type 2 virus in febrile travellers returning from Burkina Faso to France, related to an ongoing outbreak, October to November 2016. Eurosurveillance 2016, 21, 30425. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.Q.; Sun, Y.; Zhao, G.P.; Liu, L.J.; Jiang, Z.J.; Fan, Z.W.; Wang, J.X.; Ji, Y.; Ma, M.J.; Teng, J.; et al. Travel-related infections in mainland China, 2014–2016: An active surveillance study. Lancet Public Health 2018, 3, e385–e394. [Google Scholar] [CrossRef]
- Fourie, T.; Luciani, L.; Amrane, S.; Zandotti, C.; Leparc-Goffart, I.; Ninove, L.; Nougairede, A. Dengue Virus Type 1 Infection in Traveler Returning from Benin to France, 2019. Emerg. Infect. Dis. 2020, 26, 1946–1949. [Google Scholar] [CrossRef] [PubMed]
- Gautret, P.; Botelho-Nevers, E.; Charrel, R.N.; Parola, P. Dengue virus infections in travellers returning from Benin to France, July–August 2010. Eurosurveillance 2010, 15, 19657. [Google Scholar] [CrossRef]
- Goljan, J.; Myjak, P.; Nahorski, W.; Kubica-Biernat, B.; Felczak-Korzybska, I.; Kowalczyk, D.; Kuna, A.; Kotlowski, A. Dengue antibodies in Polish travellers returning from the tropics. Evaluation of serological tests. Int. Marit. Health 2010, 61, 36–40. [Google Scholar]
- Hashimoto, T.; Kutsuna, S.; Maeki, T.; Tajima, S.; Takaya, S.; Katanami, Y.; Yamamoto, K.; Takeshita, N.; Hayakawa, K.; Kato, Y.; et al. A Case of Dengue Fever Imported from Burkina Faso to Japan in October 2016. Jpn. J. Infect. Dis. 2017, 70, 675–677. [Google Scholar] [CrossRef] [PubMed]
- Jensenius, M.; Myrvang, B. Imported fever. A diagnostic challenge. Nord. Med. 1998, 113, 107–111. [Google Scholar] [PubMed]
- Kutsuna, S.; Hayakawa, K.; Kato, Y.; Fujiya, Y.; Mawatari, M.; Takeshita, N.; Kanagawa, S.; Ohmagari, N. Comparison of clinical characteristics and laboratory findings of malaria, dengue, and enteric fever in returning travelers: 8-year experience at a referral center in Tokyo, Japan. J. Infect. Chemother. 2015, 21, 272–276. [Google Scholar] [CrossRef]
- Laferl, H.; Szell, M.; Bischof, E.; Wenisch, C. Imported dengue fever in Austria 1990–2005. Travel. Med. Infect. Dis. 2006, 4, 319–323. [Google Scholar] [CrossRef]
- Liang, H.; Luo, L.; Yang, Z.; Di, B.; Bai, Z.; He, P.; Jing, Q.; Zheng, X. Re-Emergence of Dengue Virus Type 3 in Canton, China, 2009–2010, Associated with Multiple Introductions through Different Geographical Routes. PLoS ONE 2013, 8, e55353. [Google Scholar] [CrossRef]
- Lim, P.L.; Han, P.; Chen, L.H.; MacDonald, S.; Pandey, P.; Hale, D.; Schlagenhauf, P.; Loutan, L.; Wilder-Smith, A.; Davis, X.M.; et al. Expatriates ill after travel: Results from the Geosentinel Surveillance Network. BMC Infect. Dis. 2012, 12, 386. [Google Scholar] [CrossRef] [PubMed]
- Moi, M.L.; Takasaki, T.; Kotaki, A.; Tajima, S.; Lim, C.K.; Sakamoto, M.; Iwagoe, H.; Kobayashi, K.; Kurane, I. Importation of dengue virus type 3 to Japan from Tanzania and Cote d’Ivoire. Emerg. Infect. Dis. 2010, 16, 1770–1772. [Google Scholar] [CrossRef] [PubMed]
- Nisii, C.; Carletti, F.; Castilletti, C.; Bordi, L.; Meschi, S.; Selleri, M.; Chiappini, R.; Travaglini, D.; Antonini, M.; Castorina, S.; et al. A case of dengue type 3 virus infection imported from Africa to Italy, October 2009. Eurosurveillance 2010, 15, 19487. [Google Scholar] [CrossRef] [PubMed]
- Okada, K.; Morita, R.; Egawa, K.; Hirai, Y.; Kaida, A.; Shirano, M.; Kubo, H.; Goto, T.; Yamamoto, S.P. Dengue Virus Type 1 Infection in Traveler Returning from Tanzania to Japan, 2019. Emerg. Infect. Dis. 2019, 25, 1782–1784. [Google Scholar] [CrossRef]
- Overbosch, F.W.; Schinkel, J.; Stolte, I.G.; Prins, M.; Sonder, G.J.B. Dengue virus infection among long-term travelers from the Netherlands: A prospective study, 2008–2011. PLoS ONE 2018, 13, e0192193. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Kutsuna, S.; Nakamoto, T.; Ota, M.; Ishikane, M.; Yamamoto, K.; Maeki, T.; Tajima, S.; Nakayama, E.; Taniguchi, S.; et al. Dengue Virus Serotype 1 Exported to Japan from Cote d’Ivoire, 2019. Jpn. J. Infect. Dis. 2021, 74, 148–150. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Kutsuna, S.; Taniguchi, S.; Tajima, S.; Maeki, T.; Kato, F.; Lim, C.K.; Saijo, M.; Tsuboi, M.; Yamamoto, K.; et al. Dengue Virus Exported from Cote d’Ivoire to Japan, June 2017. Emerg. Infect. Dis. 2017, 23, 1758–1760. [Google Scholar] [CrossRef]
- Toro, C.; Trevisi, P.; Lopez-Quintana, B.; Amor, A.; Iglesias, N.; Subirats, M.; de Guevara, C.L.; Lago, M.; Arsuaga, M.; de la Calle-Prieto, F.; et al. Imported Dengue Infection in a Spanish Hospital with a High Proportion of Travelers from Africa: A 9-Year Retrospective Study. Am. J. Trop. Med. Hyg. 2017, 96, 701–707. [Google Scholar] [CrossRef]
- Torres-Fernandez, D.; Prieto Tato, L.M.; Perez-Ayala, A.; Moraleda, C.; Fernandez Cooke, E.; Blazquez-Gamero, D.; Rojo, P.; Perez Rivilla, A.; Epalza, C. Etiology and outcome of febrile children coming from the tropics. Enferm. Infecc. Microbiol. Clin. 2020, 39, 498–502. [Google Scholar] [CrossRef]
- Ujiie, M.; Moi, M.L.; Kobayashi, T.; Takeshita, N.; Kato, Y.; Takasaki, T.; Kanagawa, S. Dengue virus type-3 infection in a traveler returning from Benin to Japan. J. Travel. Med. 2012, 19, 255–257. [Google Scholar] [CrossRef][Green Version]
- Vainio, K.; Noraas, S.; Holmberg, M.; Fremstad, H.; Wahlstrom, M.; Anestad, G.; Dudman, S. Fatal and mild primary dengue virus infections imported to Norway from Africa and south-east Asia, 2008–2010. Eurosurveillance 2010, 15, 19666. [Google Scholar] [CrossRef] [PubMed]
- Verschueren, J.; Cnops, L.; van Esbroeck, M. Twelve years of dengue surveillance in Belgian travellers and significant increases in the number of cases in 2010 and 2013. Clin. Microbiol. Infect. 2015, 21, 867–872. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, S.P.; Kasamatsu, Y.; Kanbayashi, D.; Kaida, A.; Shirano, M.; Kubo, H.; Goto, T.; Iritani, N. Dengue Virus in Traveler Returning to Japan from the Democratic Republic of the Congo, 2015. Jpn. J. Infect. Dis. 2019, 72, 426–428. [Google Scholar] [CrossRef] [PubMed]
- Mordecai, E.A.; Ryan, S.J.; Caldwell, J.M.; Shah, M.M.; LaBeaud, A.D. Climate change could shift disease burden from malaria to arboviruses in Africa. Lancet Planet Health 2020, 4, e416–e423. [Google Scholar] [CrossRef]
- Heath, C.J.; Grossi-Soyster, E.N.; Ndenga, B.A.; Mutuku, F.M.; Sahoo, M.K.; Ngugi, H.N.; Mbakaya, J.O.; Siema, P.; Kitron, U.; Zahiri, N.; et al. Evidence of transovarial transmission of Chikungunya and Dengue viruses in field-caught mosquitoes in Kenya. PLOS Negl. Trop. Dis. 2020, 14, e0008362. [Google Scholar] [CrossRef]
- Forsyth, J.E.; Mutuku, F.M.; Kibe, L.; Mwashee, L.; Bongo, J.; Egemba, C.; Ardoin, N.M.; Labeaud, A.D. Source reduction with a purpose: Mosquito ecology and community perspectives offer insights for improving household mosquito management in coastal Kenya. PLOS Negl. Trop. Dis. 2020, 14, e0008239. [Google Scholar] [CrossRef]
- Stoler, J.; Al Dashti, R.; Anto, F.; Fobil, J.N.; Awandare, G.A. Deconstructing “malaria”: West Africa as the next front for dengue fever surveillance and control. Acta Trop. 2014, 134, 58–65. [Google Scholar] [CrossRef]
- Hooft, A.M.; Ripp, K.; Ndenga, B.; Mutuku, F.; Vu, D.; Baltzell, K.; Masese, L.N.; Vulule, J.; Mukoko, D.; Labeaud, A.D. Principles, practices and knowledge of clinicians when assessing febrile children: A qualitative study in Kenya. Malar. J. 2017, 16. [Google Scholar] [CrossRef]
- Mohammed Yusuf, A.; Abdurashid Ibrahim, N. Knowledge, attitude and practice towards dengue fever prevention and associated factors among public health sector health-care professionals: In Dire Dawa, eastern Ethiopia. Risk Manag. Healthc. Policy 2019, 12, 91–104. [Google Scholar] [CrossRef]
- Wong, P.F.; Wong, L.P.; AbuBakar, S. Diagnosis of severe dengue: Challenges, needs and opportunities. J. Infect. Public Health 2020, 13, 193–198. [Google Scholar] [CrossRef]
- Hooft, A.M.; Ndenga, B.; Mutuku, F.; Otuka, V.; Ronga, C.; Chebii, P.K.; Maina, P.W.; Jembe, Z.; Lee, J.; Vu, D.M.; et al. High Frequency of Antibiotic Prescription in Children With Undifferentiated Febrile Illness in Kenya. Clin. Infect. Dis. 2021, 73, e2399–e2406. [Google Scholar] [CrossRef] [PubMed]
- Dengue: Symptoms and Treatment. Available online: https://www.cdc.gov/dengue/symptoms/index.html (accessed on 20 June 2021).
- Ten Bosch, Q.A.; Clapham, H.E.; Lambrechts, L.; Duong, V.; Buchy, P.; Althouse, B.M.; Lloyd, A.L.; Waller, L.A.; Morrison, A.C.; Kitron, U.; et al. Contributions from the silent majority dominate dengue virus transmission. PLoS Pathog. 2018, 14, e1006965. [Google Scholar] [CrossRef] [PubMed]
- Adam, A.; Jassoy, C. Epidemiology and Laboratory Diagnostics of Dengue, Yellow Fever, Zika, and Chikungunya Virus Infections in Africa. Pathogens 2021, 10, 1324. [Google Scholar] [CrossRef] [PubMed]
- Narvaez, F.; Gutierrez, G.; Perez, M.A.; Elizondo, D.; Nunez, A.; Balmaseda, A.; Harris, E. Evaluation of the traditional and revised WHO classifications of Dengue disease severity. PLoS Negl. Trop. Dis. 2011, 5, e1397. [Google Scholar] [CrossRef]
- Elven, J.; Dahal, P.; Ashley, E.A.; Thomas, N.V.; Shrestha, P.; Stepniewska, K.; Crump, J.A.; Newton, P.N.; Bell, D.; Reyburn, H.; et al. Non-malarial febrile illness: A systematic review of published aetiological studies and case reports from Africa, 1980–2015. BMC Med. 2020, 18, 279. [Google Scholar] [CrossRef]
- Malaria. Available online: https://www.afro.who.int/health-topics/malaria (accessed on 20 June 2021).
- Malaria: Frequently Asked Questions (FAQs). Available online: https://www.cdc.gov/malaria/about/faqs.html (accessed on 20 June 2021).
- Topics: Malaria. Available online: https://www.paho.org/en/topics/malaria (accessed on 20 June 2021).
- Autino, B.; Noris, A.; Russo, R.; Castelli, F. Epidemiology of malaria in endemic areas. Mediterr. J. Hematol. Infect. Dis. 2012, 4, e2012060. [Google Scholar] [CrossRef]
- Malaria—Symptoms and Causes. Available online: https://www.mayoclinic.org/diseases-conditions/malaria/symptoms-causes/syc-20351184 (accessed on 20 June 2021).
- Kazaura, M. Knowledge, attitude and practices about dengue fever among adults living in Pwani Region, Tanzania in 2019. Afr. Health Sci. 2020, 20, 1601–1609. [Google Scholar] [CrossRef]
- L’Azou, M.; Succo, T.; Kamagate, M.; Ouattara, A.; Gilbernair, E.; Adjogoua, E.; Luxemburger, C. Dengue: Etiology of acute febrile illness in Abidjan, Cote d’Ivoire, in 2011–2012. Trans. R. Soc. Trop. Med. Hyg. 2015, 109, 717–722. [Google Scholar] [CrossRef]
- Vu, D.M.; Mutai, N.; Heath, C.J.; Vulule, J.M.; Mutuku, F.M.; Ndenga, B.A.; Labeaud, A.D. Unrecognized Dengue Virus Infections in Children, Western Kenya, 2014–2015. Emerg. Infect. Dis. 2017, 23, 1915–1917. [Google Scholar] [CrossRef]
- Amoako, N.; Duodu, S.; Dennis, F.; Bonney, J.H.K.; Asante, K.; Ameh, J.; Mosi, L.; Hayashi, T.; Agbosu, E.; Pratt, D.; et al. Detection of Dengue Virus among Children with Suspected Malaria, Accra, Ghana. Emerg. Infect. Dis. J. 2018, 24, 1544. [Google Scholar] [CrossRef]
- Nassar, S.A.; Olayiwola, J.O.; Bakarey, A.S.; Enyhowero, S.O. Investigations of dengue virus and Plasmodium falciparum among febrile patients receiving care at a tertiary health facility in Osogbo, south-west Nigeria. Niger. J. Parasitol. 2019, 40, 18. [Google Scholar] [CrossRef]
- Onyedibe, K.; Dawurung, J.; Iroezindu, M.; Shehu, N.; Okolo, M.; Shobowale, E.; Afolaranmi, T.; Dahal, S.; Maktep, Y.; Pama, P.; et al. A cross sectional study of dengue virus infection in febrile patients presumptively diagnosed of malaria in Maiduguri and Jos plateau, Nigeria. Malawi Med. J. 2018, 30, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Stoler, J.; Awandare, G.A. Febrile illness diagnostics and the malaria-industrial complex: A socio-environmental perspective. BMC Infect. Dis. 2016, 16, 683. [Google Scholar] [CrossRef] [PubMed]
- Ndenga, B.A.; Mutuku, F.M.; Ngugi, H.N.; Mbakaya, J.O.; Aswani, P.; Musunzaji, P.S.; Vulule, J.; Mukoko, D.; Kitron, U.; Labeaud, A.D. Characteristics of Aedes aegypti adult mosquitoes in rural and urban areas of western and coastal Kenya. PLoS ONE 2017, 12, e0189971. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Dhar, M.; Mittal, G.; Bhat, N.K.; Shirazi, N.; Kalra, V.; Sati, H.C.; Gupta, V. A comparative hospital-based observational study of mono- and co-infections of malaria, dengue virus and scrub typhus causing acute undifferentiated fever. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Barua, A.; Gill, N. A Comparative Study of Concurrent Dengue and Malaria Infection with their Monoinfection in a Teaching Hospital in Mumbai. J. Assoc. Physicians India 2016, 64, 49–52. [Google Scholar] [PubMed]
- Barua, A.; Yeolekar, M.E. Concurrent dengue and malaria coinfection: Observations from a central Mumbai hospital. Int. J. Infect. Dis. 2016, 45, 165. [Google Scholar] [CrossRef][Green Version]
- Dev, N. An infection cocktail: Malaria, dengue, chikungunya and Japanese encephalitis. Trop. Doct. 2019, 49, 42–43. [Google Scholar] [CrossRef]
- Gupta, N.; Srivastava, S.; Jain, A.; Chaturvedi, U.C. Dengue in India. Indian J. Med. Res. 2012, 136, 373–390. [Google Scholar]
- Kaushik, R.M.; Varma, A.; Kaushik, R.; Gaur, K.J.B.S. Concurrent dengue and malaria due to Plasmodium falciparum and P. vivax. Trans. R. Soc. Trop. Med. Hyg. 2007, 101, 1048–1050. [Google Scholar] [CrossRef]
- Mandage, R.; Kaur, C.; Pramanik, A.; Kumar, V.; Kodan, P.; Singh, A.; Saha, S.; Pandey, S.; Wig, N.; Pandey, R.M.; et al. Association of Dengue Virus and Leptospira Co-Infections with Malaria Severity. Emerg. Infect. Dis. J. 2020, 26, 1645. [Google Scholar] [CrossRef] [PubMed]
- Mushtaq, M.B.; Qadri, M.I.; Rashid, A. Concurrent infection with dengue and malaria: An unusual presentation. Case Rep. Med. 2013, 2013, 520181. [Google Scholar] [CrossRef] [PubMed]
- Rao, M.R.; Padhy, R.N.; Das, M.K. Prevalence of dengue viral and malaria parasitic co-infections in an epidemic district, Angul of Odisha, India: An eco-epidemiological and cross-sectional study for the prospective aspects of public health. J. Infect. Public Health 2016, 9, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.D.; Mehta, T.K. Evaluation of concurrent malaria and dengue infections among febrile patients. Indian J. Med. Microbiol. 2017, 35, 402–405. [Google Scholar] [CrossRef]
- Srivatsav, S.; Mahalingam, S.; Ramineni, P.; Manya, S. Dengue and Plasmodium falciparum Coinfection With Secondary Hemophagocytic Lymphohistiocytosis in a 3-Year-Old Boy: A Clinical Conundrum. J. Pediatr. Hematol. Oncol. 2020, 44, e253–e254. [Google Scholar] [CrossRef]
- Assir, M.Z.; Masood, M.A.; Ahmad, H.I. Concurrent dengue and malaria infection in Lahore, Pakistan during the 2012 dengue outbreak. Int. J. Infect. Dis. 2014, 18, 41–46. [Google Scholar] [CrossRef]
- Carme, B.; Matheus, S.; Donutil, G.; Raulin, O.; Nacher, M.; Morvan, J. Concurrent dengue and malaria in Cayenne Hospital, French Guiana. Emerg. Infect. Dis. 2009, 15, 668–671. [Google Scholar] [CrossRef]
- Chong, S.E.; Mohamad Zaini, R.H.; Suraiya, S.; Lee, K.T.; Lim, J.A. The dangers of accepting a single diagnosis: Case report of concurrent Plasmodium knowlesi malaria and dengue infection. Malar. J. 2017, 16, 2. [Google Scholar] [CrossRef]
- Epelboin, L.; Hanf, M.; Dussart, P.; Ouar-Epelboin, S.; Djossou, F.; Nacher, M.; Carme, B. Is dengue and malaria co-infection more severe than single infections? A retrospective matched-pair study in French Guiana. Malar. J. 2012, 11, 142. [Google Scholar] [CrossRef] [PubMed]
- Halsey, E.S.; Baldeviano, G.C.; Edgel, K.A.; Vilcarromero, S.; Sihuincha, M.; Lescano, A.G. Symptoms and Immune Markers in Plasmodium/Dengue Virus Co-infection Compared with Mono-infection with Either in Peru. PLoS Negl. Trop. Dis. 2016, 10, e0004646. [Google Scholar] [CrossRef]
- na Ayuthaya, S.I.; Wangjirapan, A.; Oberdorfer, P. An 11-year-old boy with Plasmodium falciparum malaria and dengue co-infection. BMJ Case Rep. 2014, 2014, bcr2013202998. [Google Scholar] [CrossRef] [PubMed]
- Khurram, M.; Faheem, M.; Umar, M.; Yasin, A.; Qayyum, W.; Ashraf, A.; Zahid Khan, J.; Hasnain Yasir, A.; Ansari, Y.; Asad, M.; et al. Hemophagocytic Lymphohistiocytosis Complicating Dengue and Plasmodium vivax Coinfection. Case Rep. Med. 2015, 2015, 696842. [Google Scholar] [CrossRef] [PubMed]
- Lupi, O.; Ridolfi, F.; Da Silva, S.; Zanini, G.M.; Lavigne, A.; Nogueira, R.M.R.; Cruz, M.D.F.F.D.; Daniel-Ribeiro, C.T.; Brasil, P. Dengue infection as a potential trigger of an imported Plasmodium ovale malaria relapse or a long incubation period in a non-endemic malaria region. Int. J. Infect. Dis. 2016, 44, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Magalhaes, B.M.; Alexandre, M.A.; Siqueira, A.M.; Melo, G.C.; Gimaque, J.B.; Bastos, M.S.; Figueiredo, R.M.; Carvalho, R.C.; Tavares, M.A.; Naveca, F.G.; et al. Clinical profile of concurrent dengue fever and Plasmodium vivax malaria in the Brazilian Amazon: Case series of 11 hospitalized patients. Am. J. Trop. Med. Hyg. 2012, 87, 1119–1124. [Google Scholar] [CrossRef]
- Magalhaes, B.M.; Siqueira, A.M.; Alexandre, M.A.; Souza, M.S.; Gimaque, J.B.; Bastos, M.S.; Figueiredo, R.M.; Melo, G.C.; Lacerda, M.V.; Mourao, M.P. P. vivax malaria and dengue fever co-infection: A cross-sectional study in the Brazilian Amazon. PLoS Negl. Trop. Dis. 2014, 8, e3239. [Google Scholar] [CrossRef]
- Mendonca, V.R.; Andrade, B.B.; Souza, L.C.; Magalhaes, B.M.; Mourao, M.P.; Lacerda, M.V.; Barral-Netto, M. Unravelling the patterns of host immune responses in Plasmodium vivax malaria and dengue co-infection. Malar. J. 2015, 14, 315. [Google Scholar] [CrossRef]
- Santana Vdos, S.; Lavezzo, L.C.; Mondini, A.; Terzian, A.C.; Bronzoni, R.V.; Rossit, A.R.; Machado, R.L.; Rahal, P.; Nogueira, M.C.; Nogueira, M.L. Concurrent Dengue and malaria in the Amazon region. Rev. Soc. Bras. Med. Trop. 2010, 43, 508–511. [Google Scholar] [CrossRef]
- Selvaretnam, A.A.P.; Sahu, P.S.; Sahu, M.; Ambu, S. A review of concurrent infections of malaria and dengue in Asia. Asian Pac. J. Trop. Biomed. 2016, 6, 633–638. [Google Scholar] [CrossRef]
- Serre, N.; Franco, L.; Sulleiro, E.; Rubio, J.M.; Zarzuela, F.; Molero, F.; Tenorio, A. Concurrent Infection With Dengue Type 4 and Plasmodium falciparum Acquired in Haiti. J. Travel. Med. 2015, 22, 345–347. [Google Scholar] [CrossRef][Green Version]
- Shams, N.; Amjad, S.; Yousaf, N.; Ahmed, W.; Seetlani, N.K.; Qaisar, N.; Samina. Predictors of Severity of Dengue Fever in Tertiary Care Hospitals. J. Liaquat Univ. Med. Health Sci. 2016, 15, 168–173. [Google Scholar]
- Thaha, M.; Pranawa; Yogiantoro, M.; Tanimoto, M.; Tomino, Y. Acute renal failure in a patient with severe malaria and dengue shock syndrome. Clin. Nephrol. 2008, 70, 427–430. [Google Scholar] [CrossRef] [PubMed]
- Ward, D.I. A case of fatal Plasmodium falciparum malaria complicated by acute dengue fever in East Timor. Am. J. Trop. Med. Hyg. 2006, 75, 182–185. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Wu, X.; Liao, F. Severe Cerebral Falciparum Malaria with Dengue Coinfection: A Case Report. Iran. J. Parasitol. 2018, 13, 323–327. [Google Scholar] [PubMed]
- Baba, M.; Logue, C.H.; Oderinde, B.; Abdulmaleek, H.; Williams, J.; Lewis, J.; Laws, T.R.; Hewson, R.; Marcello, A.; Agaro, P.D. Evidence of arbovirus co-infection in suspected febrile malaria and typhoid patients in Nigeria. J. Infect. Dev. Ctries. 2013, 7, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Galani, B.R.T.; Mapouokam, D.W.; Simo, F.B.N.; Mohamadou, H.; Chuisseu, P.D.D.; Njintang, N.Y.; Moundipa, P.F. Investigation of dengue–malaria coinfection among febrile patients consulting at Ngaoundere Regional Hospital, Cameroon. J. Med. Virol. 2021, 93, 3350–3361. [Google Scholar] [CrossRef] [PubMed]
- Kolawole, O.M.; Seriki, A.A.; Irekeola, A.A.; Bello, K.E.; Adeyemi, O.O. Dengue virus and malaria concurrent infection among febrile subjects within Ilorin metropolis, Nigeria. J. Med. Virol. 2017, 89, 1347–1353. [Google Scholar] [CrossRef]
- Liu, E.; Vu, D.; Boothroyd, D.; Ndenga, B.; Onyango, W.; Okuta, V.; Labeaud, A.D. Evaluation of the Health-Related Quality of Life of Children with Dengue and Malaria in Western Kenya. In Open Forum Infectious Diseases; Oxford University Press: Oxford, UK, 2016; Volume 3. [Google Scholar] [CrossRef]
- Monamele, G.C.; Demanou, M. First documented evidence of dengue and malaria co-infection in children attending two health centers in Yaounde, Cameroon. Pan Afr. Med. J. 2018, 29, 227. [Google Scholar] [CrossRef]
- Olufisayo, A.A.; Johnson, A.A. Incidence of dengue virus infections in febrile episodes in Ile-Ife, Nigeria. Afr. J. Infect. Dis. 2016, 10, 21. [Google Scholar] [CrossRef][Green Version]
- Raut, C.G.; Rao, N.M.; Sinha, D.P.; Hanumaiah, H.; Manjunatha, M.J. Chikungunya, dengue, and malaria co-infection after travel to Nigeria, India. Emerg. Infect. Dis. 2015, 21, 908–909. [Google Scholar] [CrossRef]
- Sow, A.; Loucoubar, C.; Diallo, D.; Faye, O.; Ndiaye, Y.; Senghor, C.S.; Dia, A.T.; Faye, O.; Weaver, S.C.; Diallo, M.; et al. Concurrent malaria and arbovirus infections in Kedougou, southeastern Senegal. Malar. J. 2016, 15, 47. [Google Scholar] [CrossRef]
- Stoler, J.; Delimini, R.K.; Bonney, J.H.; Oduro, A.R.; Owusu-Agyei, S.; Fobil, J.N.; Awandare, G.A. Evidence of recent dengue exposure among malaria parasite-positive children in three urban centers in Ghana. Am. J. Trop. Med. Hyg. 2015, 92, 497–500. [Google Scholar] [CrossRef] [PubMed]
- Vu, D.M.; Ripp, K.; Mutai, N.; Ndenga, B.A.; Heath, C.; Labeaud, A.D. Dengue virus and malaria co-infection in Kenyan children. Ann. Glob. Health 2016, 82, 435. [Google Scholar] [CrossRef]
- Kotepui, M.; Kotepui, K.U.; Milanez, G.J.; Masangkay, F.R. Prevalence of and risk factors for severe malaria caused by Plasmodium and dengue virus co-infection: A systematic review and meta-analysis. Infect. Dis. Poverty 2020, 9, 134. [Google Scholar] [CrossRef] [PubMed]
- Kotepui, M.; Kotepui, K.U. Prevalence and laboratory analysis of malaria and dengue co-infection: A systematic review and meta-analysis. BMC Public Health 2019, 19, 1148. [Google Scholar] [CrossRef]
- Carabali, M.; Hernandez, L.M.; Arauz, M.J.; Villar, L.A.; Ridde, V. Why are people with dengue dying? A scoping review of determinants for dengue mortality. BMC Infect. Dis. 2015, 15, 301. [Google Scholar] [CrossRef]
- Toledo, J.; George, L.; Martinez, E.; Lazaro, A.; Han, W.W.; Coelho, G.E.; Runge Ranzinger, S.; Horstick, O. Relevance of Non-communicable Comorbidities for the Development of the Severe Forms of Dengue: A Systematic Literature Review. PLoS Negl. Trop. Dis. 2016, 10, e0004284. [Google Scholar] [CrossRef]
- Wilder-Smith, A.; Leong, W.Y. Risk of severe dengue is higher in patients with sickle cell disease: A scoping review. J. Travel Med. 2019, 26, 26. [Google Scholar] [CrossRef]
- Leslie, T.E. Dengue Fever and the Quandary of Race. Lat. Am. Caribb. Ethn. Stud. 2011, 6, 283–309. [Google Scholar] [CrossRef]
- Fujimura, J.H.; Rajagopalan, R. Different differences: The use of ‘genetic ancestry’ versus race in biomedical human genetic research. Soc. Stud. Sci. 2011, 41, 5–30. [Google Scholar] [CrossRef]
- McAfee, S. Race is a Social Construct; Center for Health Progress: Denver, CO, USA, 2017. [Google Scholar]
- Borrell, L.N.; Elhawary, J.R.; Fuentes-Afflick, E.; Witonsky, J.; Bhakta, N.; Wu, A.H.B.; Bibbins-Domingo, K.; Rodriguez-Santana, J.R.; Lenoir, M.A.; Gavin, J.R., III; et al. Race and Genetic Ancestry in Medicine—A Time for Reckoning with Racism. N. Engl. J. Med. 2021, 384, 474–480. [Google Scholar] [CrossRef]
- Malaria—Biology. Available online: https://www.cdc.gov/malaria/about/biology/index.html (accessed on 20 June 2021).
- Xavier-Carvalho, C.; Cardoso, C.C.; de Souza Kehdy, F.; Pacheco, A.G.; Moraes, M.O. Host genetics and dengue fever. Infect. Genet. Evol. 2017, 56, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Coffey, L.L.; Mertens, E.; Brehin, A.C.; Fernandez-Garcia, M.D.; Amara, A.; Despres, P.; Sakuntabhai, A. Human genetic determinants of dengue virus susceptibility. Microbes Infect. 2009, 11, 143–156. [Google Scholar] [CrossRef] [PubMed]
- Stephens, H.A. HLA and other gene associations with dengue disease severity. Curr. Top. Microbiol. Immunol. 2010, 338, 99–114. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Agarwal, A.; Kumar, A.; Biswas, D. Genome-Wide Analysis to Identify HLA Factors Potentially Associated With Severe Dengue. Front. Immunol. 2018, 9, 728. [Google Scholar] [CrossRef]
- Xavier Eurico De Alencar, L.; De Mendonça Braga-Neto, U.; José Moura Do Nascimento, E.; Tenório Cordeiro, M.; Maria Silva, A.; Alexandre Antunes De Brito, C.; Da Silva, M.D.P.C.; Gil, L.H.V.G.; Montenegro, S.M.L.; Marques, E.T.D.A. HLA-B*44 Is Associated with Dengue Severity Caused by DENV-3 in a Brazilian Population. J. Trop. Med. 2013, 2013, 648475. [Google Scholar] [CrossRef] [PubMed]
- Murugananthan, K.; Subramaniyam, S.; Kumanan, T.; Owens, L.; Ketheesan, N.; Noordeen, F. Blood group AB is associated with severe forms of dengue virus infection. VirusDisease 2018, 29, 103–105. [Google Scholar] [CrossRef]
- Pare, G.; Neupane, B.; Eskandarian, S.; Harris, E.; Halstead, S.; Gresh, L.; Kuan, G.; Balmaseda, A.; Villar, L.; Rojas, E.; et al. Genetic risk for dengue hemorrhagic fever and dengue fever in multiple ancestries. EBioMedicine 2020, 51, 102584. [Google Scholar] [CrossRef]
- Sierra, B.; Triska, P.; Soares, P.; Garcia, G.; Perez, A.B.; Aguirre, E.; Oliveira, M.; Cavadas, B.; Regnault, B.; Alvarez, M.; et al. OSBPL10, RXRA and lipid metabolism confer African-ancestry protection against dengue haemorrhagic fever in admixed Cubans. PLoS Pathog. 2017, 13, e1006220. [Google Scholar] [CrossRef]
- Bravo, J.R.; Guzman, M.G.; Kouri, G.P. Why dengue haemorrhagic fever in Cuba? 1. Individual risk factors for dengue haemorrhagic fever/dengue shock syndrome (DHF/DSS). Trans. R. Soc. Trop. Med. Hyg. 1987, 81, 816–820. [Google Scholar] [CrossRef]
- Sierra, B.D.L.C.; Garcia, G.; Perez, A.B.; Morier, L.; Alvarez, M.; Kouri, G.; Guzman, M.G. Ethnicity and difference in dengue virus-specific memory T cell responses in Cuban individuals. Viral. Immunol. 2006, 19, 662–668. [Google Scholar] [CrossRef]
- Sierra, B.D.L.C.; Kouri, G.; Guzman, M.G. Race: A risk factor for dengue hemorrhagic fever. Arch. Virol. 2007, 152, 533–542. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.; Saraiva, D.P.; Cavadas, B.; Fernandes, V.; Pedro, N.; Casademont, I.; Koeth, F.; Alshamali, F.; Harich, N.; Cherni, L.; et al. Population genetics-informed meta-analysis in seven genes associated with risk to dengue fever disease. Infect. Genet. Evol. 2018, 62, 60–72. [Google Scholar] [CrossRef] [PubMed]
- Halstead, S.B.; Streit, T.G.; Lafontant, J.G.; Putvatana, R.; Russell, K.; Sun, W.; Kanesa-Thasan, N.; Hayes, C.G.; Watts, D.M. Haiti: Absence of dengue hemorrhagic fever despite hyperendemic dengue virus transmission. Am. J. Trop. Med. Hyg. 2001, 65, 180–183. [Google Scholar] [CrossRef] [PubMed]
- Chacón-Duque, J.C.; Adhikari, K.; Avendaño, E.; Campo, O.; Ramirez, R.; Rojas, W.; Ruiz-Linares, A.; Restrepo, B.N.; Bedoya, G. African genetic ancestry is associated with a protective effect on Dengue severity in colombian populations. Infect. Genet. Evol. 2014, 27, 89–95. [Google Scholar] [CrossRef]
- Boillat-Blanco, N.; Klaassen, B.; Mbarack, Z.; Samaka, J.; Mlaganile, T.; Masimba, J.; Franco Narvaez, L.; Mamin, A.; Genton, B.; Kaiser, L.; et al. Dengue fever in Dar es Salaam, Tanzania: Clinical features and outcome in populations of black and non-black racial category. BMC Infect. Dis. 2018, 18, 644. [Google Scholar] [CrossRef]
- Blanton, R.E.; Silva, L.K.; Morato, V.G.; Parrado, A.R.; Dias, J.P.; Melo, P.R.; Reis, E.A.; Goddard, K.A.; Nunes, M.R.; Rodrigues, S.G.; et al. Genetic ancestry and income are associated with dengue hemorrhagic fever in a highly admixed population. Eur. J. Hum. Genet. 2008, 16, 762–765. [Google Scholar] [CrossRef]
- Mawson, A.R. Retinoids, race and the pathogenesis of dengue hemorrhagic fever. Med. Hypotheses 2013, 81, 1069–1074. [Google Scholar] [CrossRef]
- Restrepo, B.N.; Arboleda, M.; Ramirez, R.; Alvarez, G. Serum platelet-activating factor acetylhydrolase activity in dengue patients of African or mestizo descendency. Biomedica 2011, 31, 599–607. [Google Scholar] [CrossRef]
- Rojas Palacios, J.H.; Alzate, A.; Martinez Romero, H.J.; Concha-Eastman, A.I. AfroColombian ethnicity, a paradoxical protective factor against Dengue. Colomb. Med. 2016, 47, 133–141. [Google Scholar] [CrossRef]
- Malik, A.; Earhart, K.; Mohareb, E.; Saad, M.; Saeed, M.; Ageep, A.; Soliman, A. Dengue hemorrhagic fever outbreak in children in Port Sudan. J. Infect. Public Health 2011, 4, 1–6. [Google Scholar] [CrossRef]
- The Hidden Burden of Dengue Fever in West Africa. Available online: https://www.infectioncontroltoday.com/view/hidden-burden-dengue-fever-west-africa (accessed on 20 June 2021).

| Subregion of Africa | Country | Outbreaks Recorded in the Last 10 Years (by Year) | U.S. CDC Level of Risk |
|---|---|---|---|
| North Africa | Sudan | 2013 [42,43], 2014–2015 [44], 2017 [42] | Frequent/Continuous |
| Egypt | 2015 [45] | Sporadic/Uncertain | |
| Algeria | None reported in the past decade | Not listed | |
| Libya | None reported in the past decade | Not listed | |
| Morocco | None reported in the past decade | Not listed | |
| Tunisia | None reported in the past decade | Not listed | |
| East Africa | Eritrea | 2014, 2015 [46] | Frequent/Continuous |
| Djibouti | 2011–2014 [47] | Frequent/Continuous | |
| Ethiopia | 2013, 2014, 2015, 2016 [48,49,50] | Frequent/Continuous | |
| Kenya | 2011, 2013–2014, 2017–2018 [51,52,53,54] | Frequent/Continuous | |
| Somalia | 2011 [54,55] | Frequent/Continuous | |
| Tanzania | 2014, 2018, 2019 [56,57] | Frequent/Continuous | |
| Mauritius | 2019 [58] | Sporadic/Uncertain | |
| Mozambique | 2014 [59], 2015 [43] | Sporadic/Uncertain | |
| Seychelles | 2015–2017 [60,61] | Sporadic/Uncertain | |
| Burundi | None reported in the past decade | Sporadic/Uncertain | |
| Comoros | None reported in the past decade | Sporadic/Uncertain | |
| Madagascar | None reported in the past decade | Sporadic/Uncertain | |
| Malawi | None reported in the past decade | Sporadic/Uncertain | |
| Rwanda | None reported in the past decade | Sporadic/Uncertain | |
| South Sudan | None reported in the past decade | Sporadic/Uncertain | |
| Uganda | None reported in the past decade | Sporadic/Uncertain | |
| Zambia | None reported in the past decade | Sporadic/Uncertain | |
| Zimbabwe | None reported in the past decade | Sporadic/Uncertain | |
| Central Africa | Angola | 2013 [62,63] | Sporadic/Uncertain |
| Cameroon | 2017 [64] | Sporadic/Uncertain | |
| Central African Republic | None reported in the past decade | Sporadic/Uncertain | |
| Chad | None reported in the past decade | Sporadic/Uncertain | |
| Democratic Republic of the Congo | None reported in the past decade | Sporadic/Uncertain | |
| Republic of the Congo | None reported in the past decade | Sporadic/Uncertain | |
| Equatorial Guinea | None reported in the past decade | Sporadic/Uncertain | |
| Gabon | None reported in the past decade | Sporadic/Uncertain | |
| São Tomé and Príncipe | None reported in the past decade | Sporadic/Uncertain | |
| West Africa | Burkina Faso | 2013, 2016–2017 [65,66] | Frequent/Continuous |
| Ivory Coast (Côte d’Ivoire) | 2017, 2019 [58,67] | Sporadic/Uncertain | |
| Senegal | 2015, 2018–2019 [68,69] | Sporadic/Uncertain | |
| Benin | None reported in the past decade | Sporadic/Uncertain | |
| Cape Verde | None reported in the past decade | Sporadic/Uncertain | |
| Gambia | None reported in the past decade | Sporadic/Uncertain | |
| Ghana | None reported in the past decade | Sporadic/Uncertain | |
| Guinea | None reported in the past decade | Sporadic/Uncertain | |
| Guinea-Bissau | None reported in the past decade | Sporadic/Uncertain | |
| Liberia | None reported in the past decade | Sporadic/Uncertain | |
| Mali | None reported in the past decade | Sporadic/Uncertain | |
| Niger | None reported in the past decade | Sporadic/Uncertain | |
| Nigeria | None reported in the past decade | Sporadic/Uncertain | |
| Sierra Leone | None reported in the past decade | Sporadic/Uncertain | |
| Togo | None reported in the past decade | Sporadic/Uncertain | |
| Mauritania | None reported in the past decade | Not listed | |
| Southern Africa | Namibia | None reported in the past decade | Sporadic/Uncertain |
| Botswana | None reported in the past decade | Not listed | |
| Eswatini (Swaziland) | None reported in the past decade | Not listed | |
| Lesotho | None reported in the past decade | Not listed | |
| South Africa | None reported in the past decade | Not listed |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gainor, E.M.; Harris, E.; LaBeaud, A.D. Uncovering the Burden of Dengue in Africa: Considerations on Magnitude, Misdiagnosis, and Ancestry. Viruses 2022, 14, 233. https://doi.org/10.3390/v14020233
Gainor EM, Harris E, LaBeaud AD. Uncovering the Burden of Dengue in Africa: Considerations on Magnitude, Misdiagnosis, and Ancestry. Viruses. 2022; 14(2):233. https://doi.org/10.3390/v14020233
Chicago/Turabian StyleGainor, Emily Mary, Eva Harris, and A. Desiree LaBeaud. 2022. "Uncovering the Burden of Dengue in Africa: Considerations on Magnitude, Misdiagnosis, and Ancestry" Viruses 14, no. 2: 233. https://doi.org/10.3390/v14020233
APA StyleGainor, E. M., Harris, E., & LaBeaud, A. D. (2022). Uncovering the Burden of Dengue in Africa: Considerations on Magnitude, Misdiagnosis, and Ancestry. Viruses, 14(2), 233. https://doi.org/10.3390/v14020233






