Oronasal or Intramuscular Immunization with a Thermo-Attenuated ASFV Strain Provides Full Clinical Protection against Georgia 2007/1 Challenge
Abstract
1. Introduction
2. Materials and Methods
2.1. Viruses and Cells
2.2. Full-Genome Sequencing and Comparison
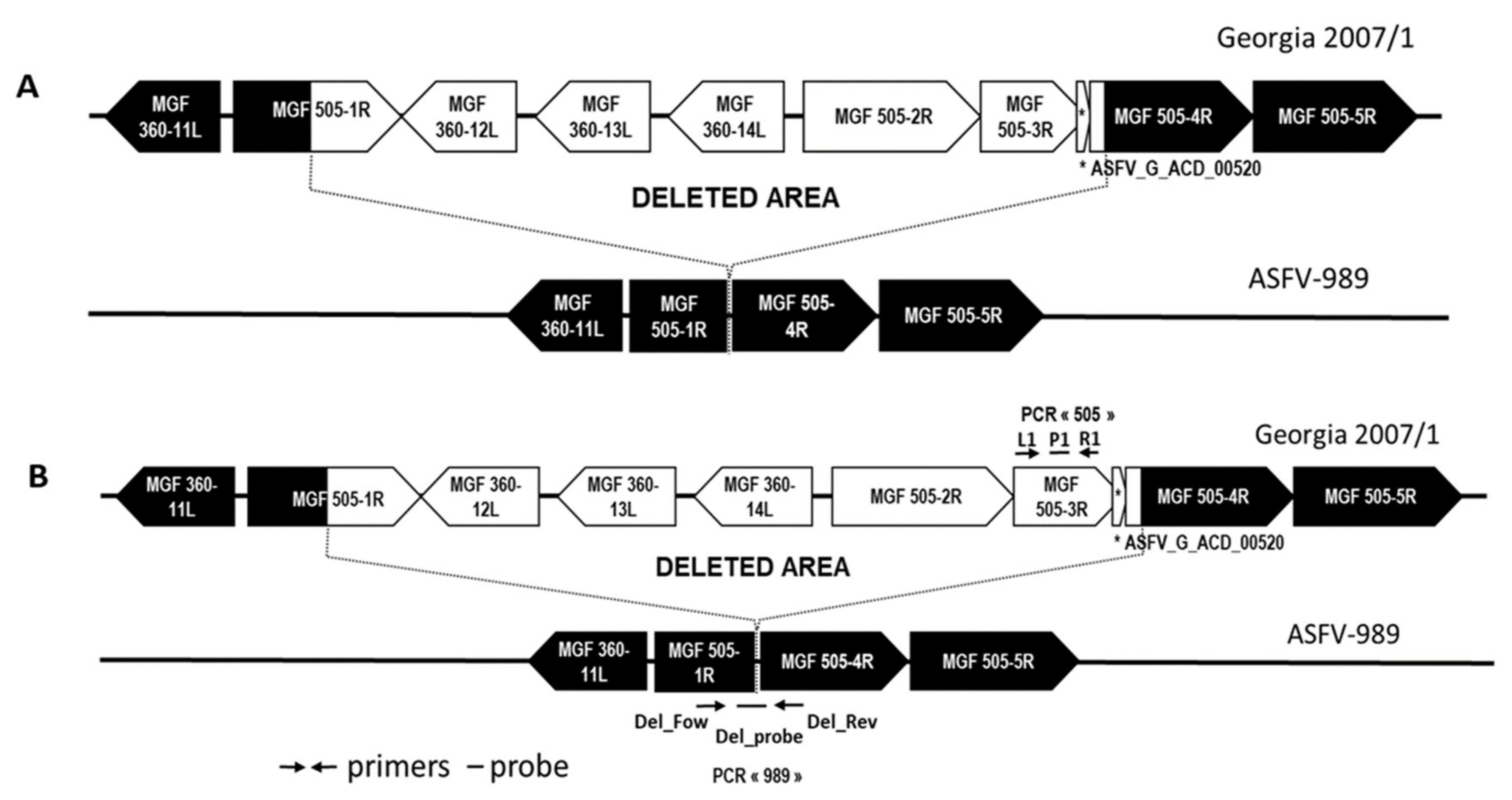
2.3. Design of Specific PCR Systems to Detect the ASFV-989 and Georgia Strains
2.4. In Vivo Study
2.5. Virological and Immunological Assays
3. Results
3.1. Genome Sequence and In Vitro Characterization of ASFV-989
3.1.1. Full-Genome Sequencing of the ASFV-989 Strain
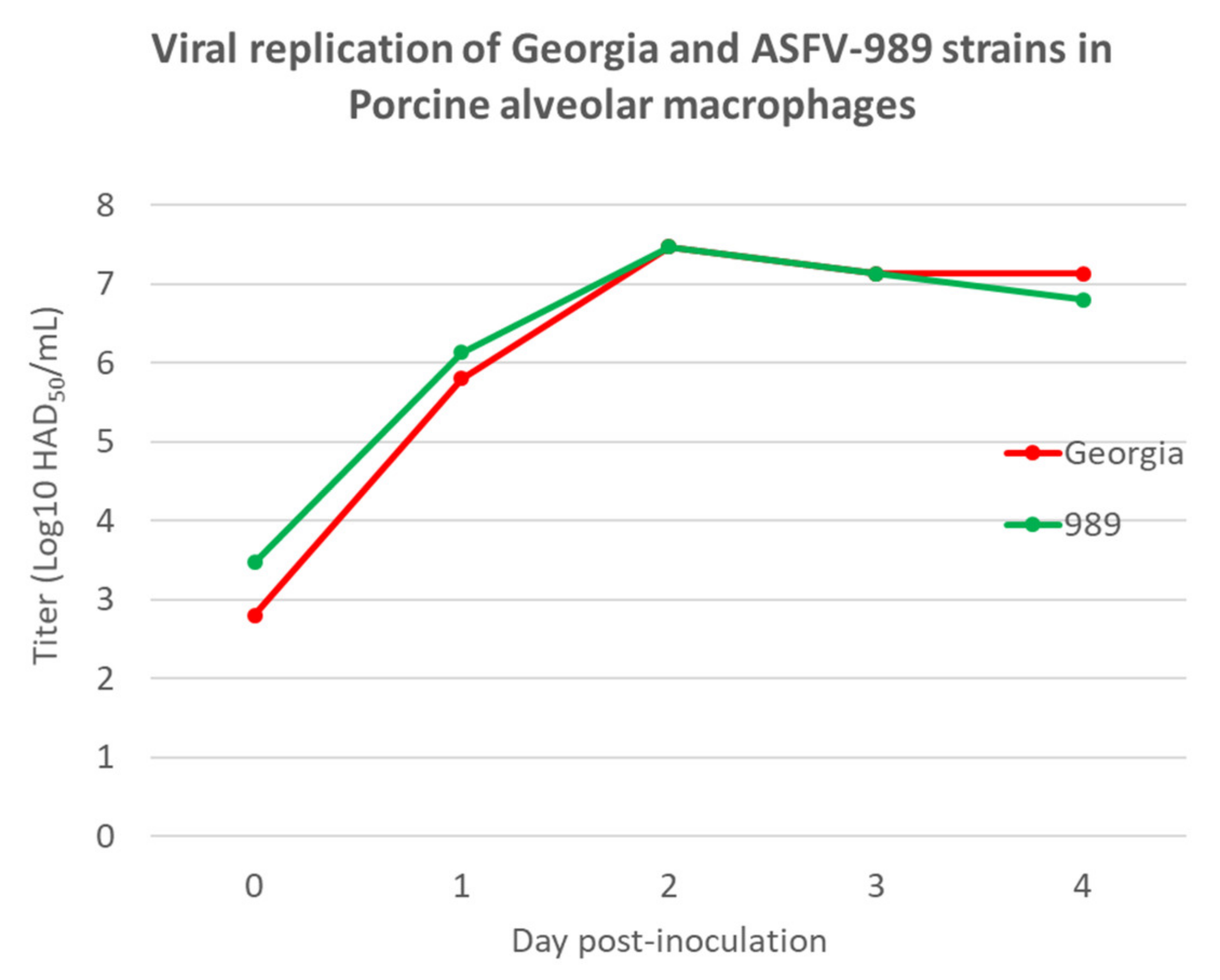
3.1.2. In vitro Replication of the ASFV-989 and Georgia Strains
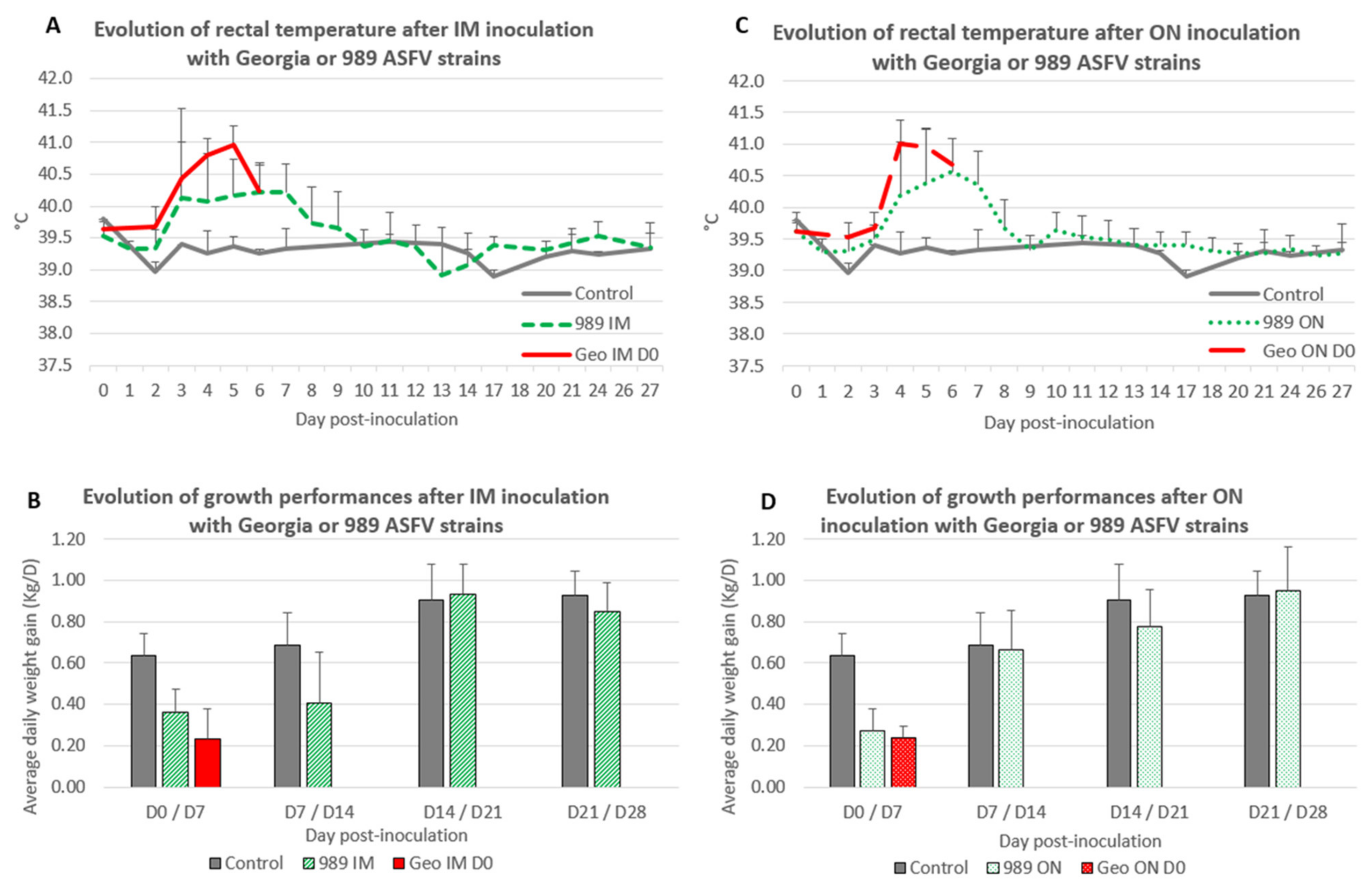
3.2. In Vivo Characterization of the Virulence of ASFV-989 Strain in Comparison to Georgia Strain
3.2.1. Clinical and Zootechnical Data
- Intramuscular inoculation
- Oronasal inoculation
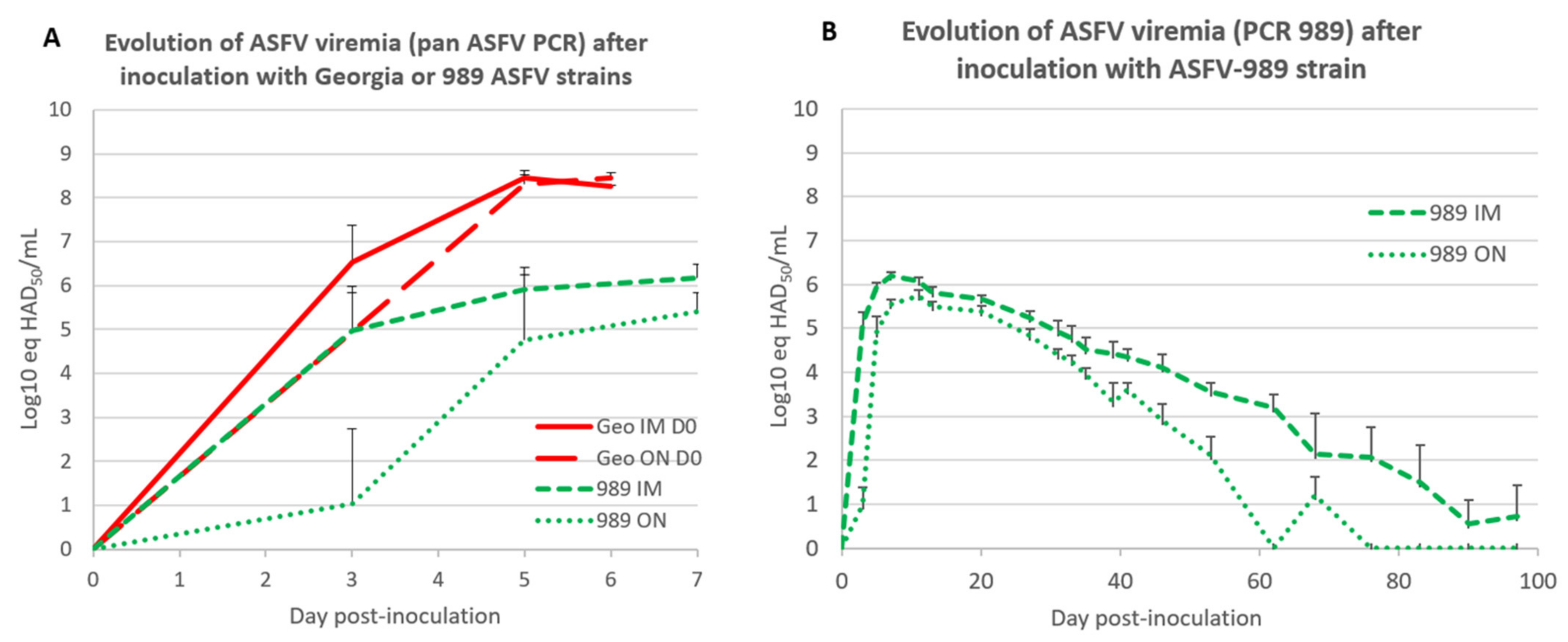
3.2.2. Virological Data
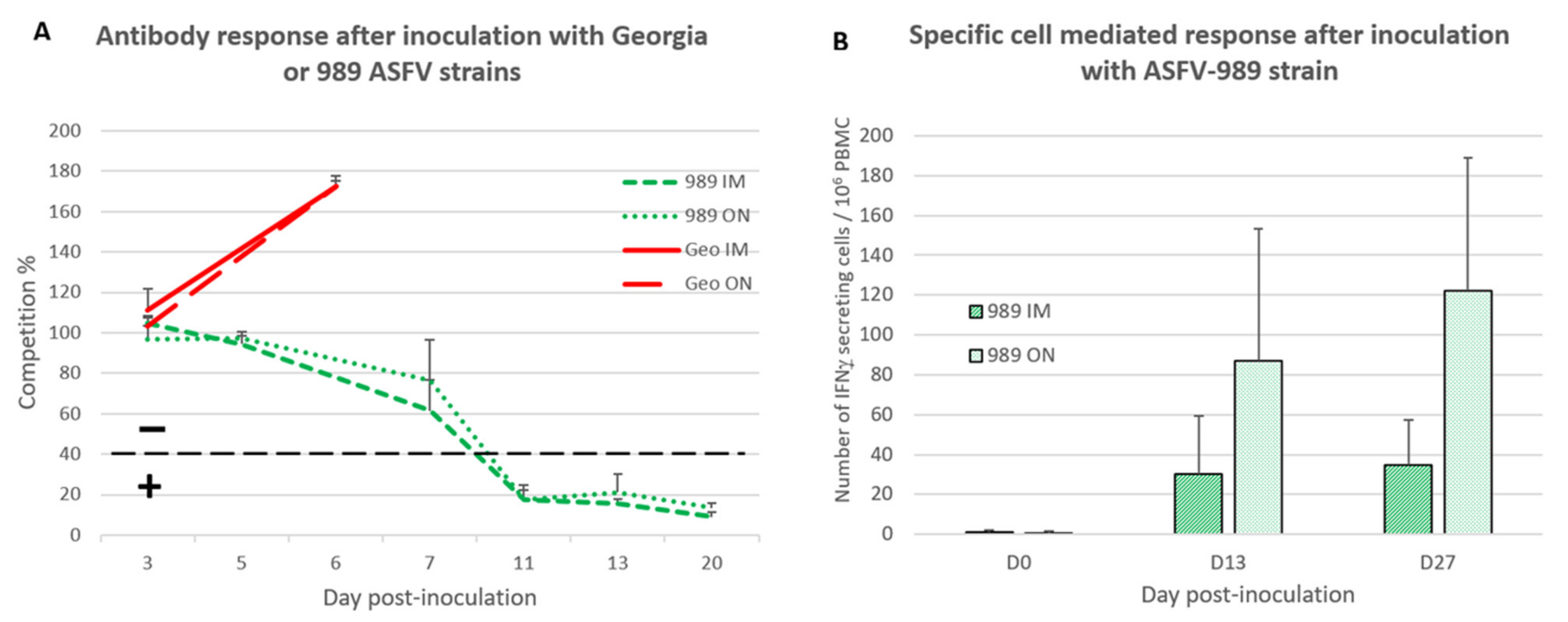
3.3. Development of ASFV-Specific Immune Response after Inoculation with Georgia or ASFV-989 Strains
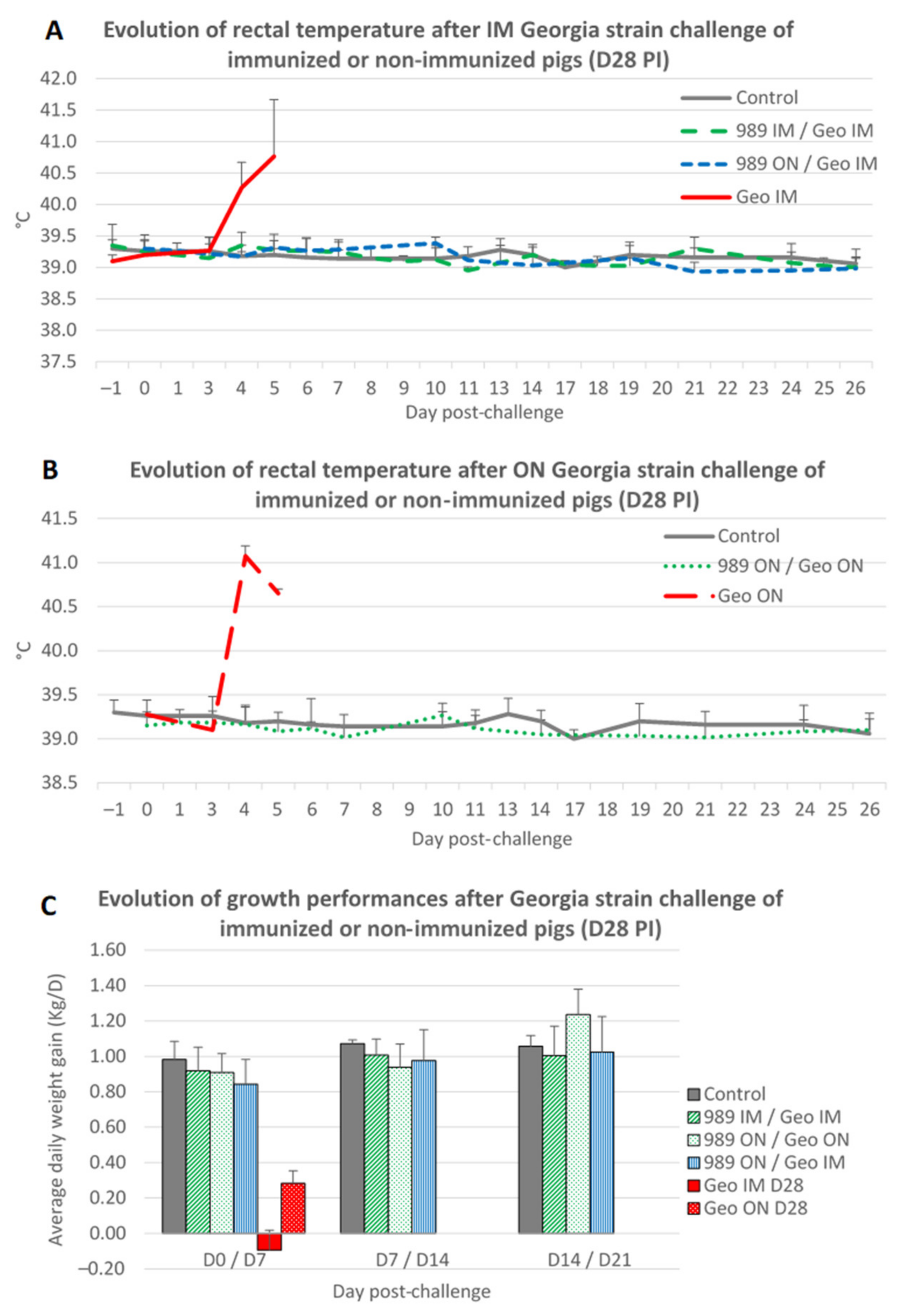
3.4. Protective Effect of ASFV-989 Strain Inoculation against a Challenge with the Georgia Strain Occurring 4 Weeks Later
3.4.1. Clinical and Zootechnical Data
3.4.2. Virological Data
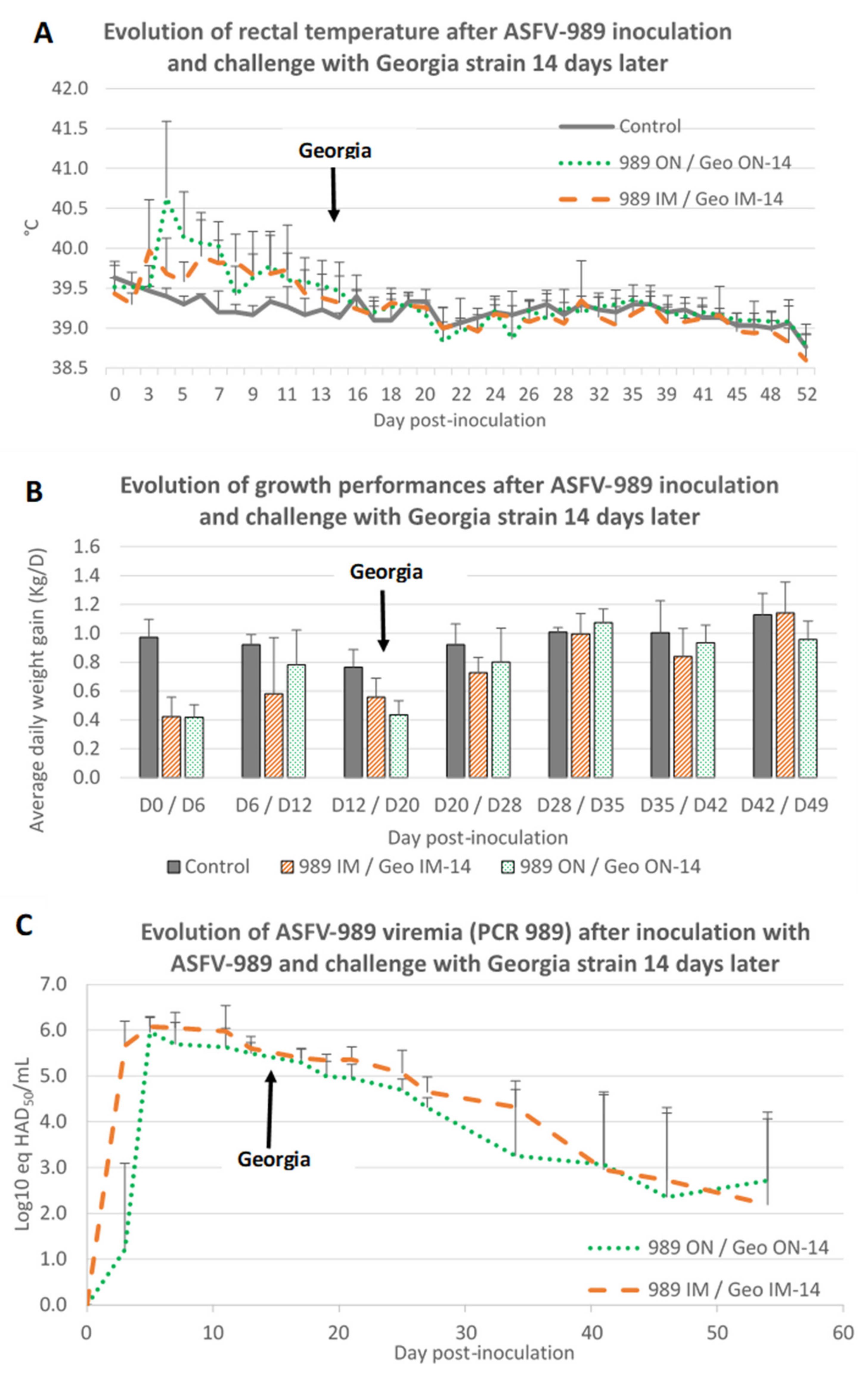
3.5. Protective Effect of ASFV-989 Strain Inoculation against a Challenge with the Georgia Strain Occurring 2 Weeks Later
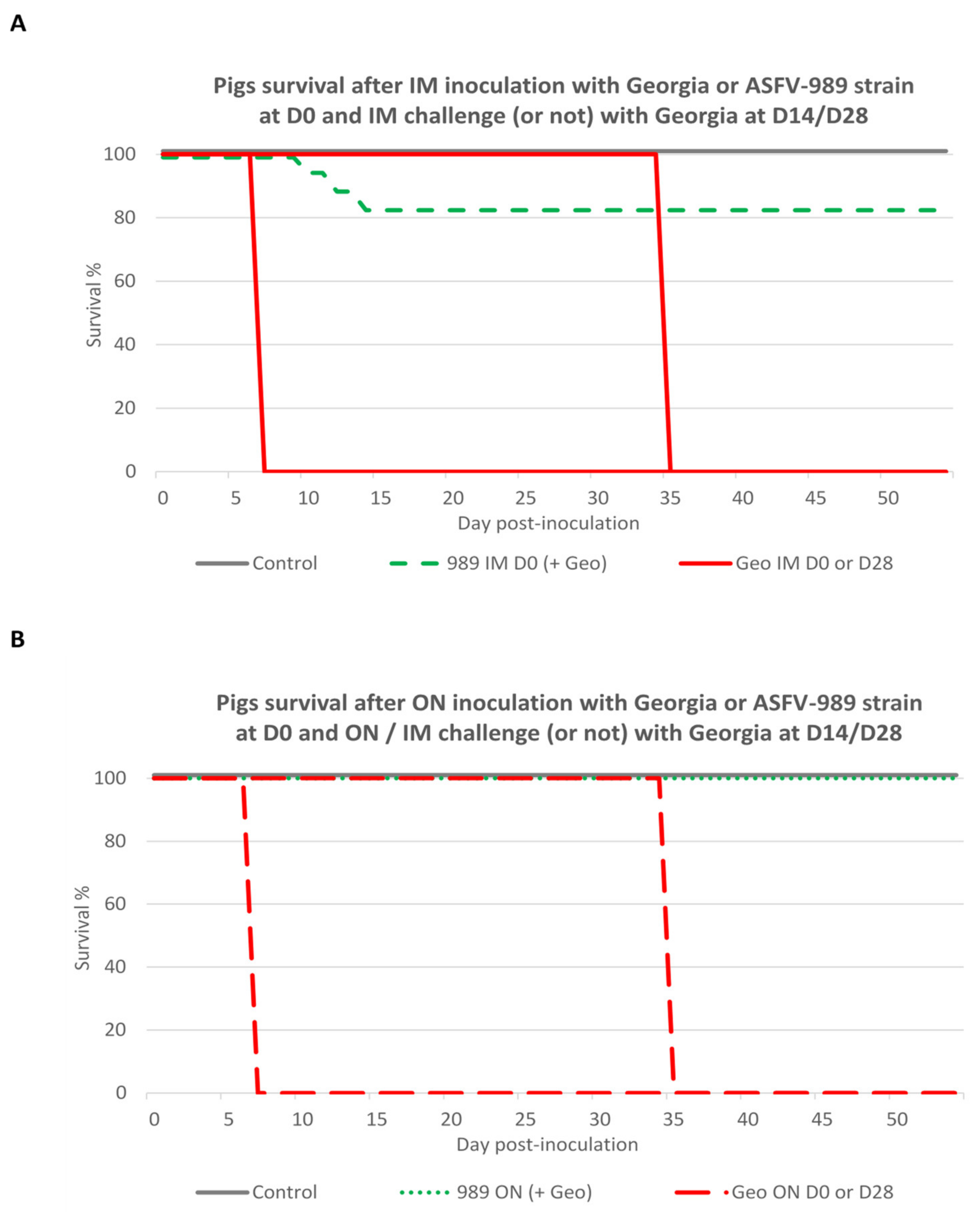
3.6. Global Safety and Efficacy of ASFV-989 as a Candidate Vaccine Strain
4. Discussion
5. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sanchez-Cordon, P.J.; Floyd, T.; Hicks, D.; Crooke, H.R.; McCleary, S.; McCarthy, R.R.; Strong, R.; Dixon, L.K.; Neimanis, A.; Wikstrom-Lassa, E.; et al. Evaluation of Lesions and Viral Antigen Distribution in Domestic Pigs Inoculated Intranasally with African Swine Fever Virus Ken05/Tk1 (Genotype X). Pathogens 2021, 10, 768. [Google Scholar] [CrossRef] [PubMed]
- Karger, A.; Pérez-Núñez, D.; Urquiza, J.; Hinojar, P.; Alonso, C.; Freitas, F.-B.; Revilla, Y.; Le Potier, M.-F.; Montoya, M. An Update on African Swine Fever Virology. Viruses 2019, 11, 864. [Google Scholar] [CrossRef] [PubMed]
- Qu, H.; Ge, S.; Zhang, Y.; Wu, X.; Wang, Z. A systematic review of genotypes and serogroups of African swine fever virus. Virus Genes 2022, 58, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, E. On a form of swine fever occurring in British East Africa (Kenya Colony). J. Comp. Pathol. Ther. 1921, XXXIV, 161–191. [Google Scholar]
- Mur, L.; Atzeni, M.; Martinez-Lopez, B.; Feliziani, F.; Rolesu, S.; Sanchez-Vizcaino, J.M. Thirty-Five-Year Presence of African Swine Fever in Sardinia: History, Evolution and Risk Factors for Disease Maintenance. Transbound. Emerg. Dis. 2014, 63, e165–e177. [Google Scholar] [CrossRef] [PubMed]
- Rowlands, R.J.; Michaud, V.; Heath, L.; Hutchings, G.; Oura, C.; Vosloo, W.; Dwarka, R.; Onashvili, T.; Albina, E.; Dixon, L.K. African swine fever virus isolate, Georgia, 2007. Emerg. Infect. Dis. 2008, 14, 1870–1874. [Google Scholar] [CrossRef]
- Gogin, A.; Gerasimov, V.; Malogolovkin, A.; Kolbasov, D. African swine fever in the North Caucasus region and the Russian Federation in years 2007–2012. Virus Res. 2013, 173, 198–203. [Google Scholar] [CrossRef]
- Chenais, E.; Depner, K.; Guberti, V.; Dietze, K.; Viltrop, A.; Stahl, K. Epidemiological considerations on African swine fever in Europe 2014–2018. Porcine Health Manag. 2019, 5, 6. [Google Scholar] [CrossRef]
- Zhou, X.; Li, N.; Luo, Y.; Liu, Y.; Miao, F.; Chen, T.; Zhang, S.; Cao, P.; Li, X.; Tian, K.; et al. Emergence of African Swine Fever in China, 2018. Transbound. Emerg. Dis. 2018, 65, 1482–1484. [Google Scholar] [CrossRef]
- Le, V.P.; Jeong, D.G.; Yoon, S.W.; Kwon, H.M.; Trinh, T.B.N.; Nguyen, T.L.; Bui, T.T.N.; Oh, J.; Kim, J.B.; Cheong, K.M.; et al. Outbreak of African Swine Fever, Vietnam, 2019. Emerg. Infect. Dis. 2019, 25, 1433–1435. [Google Scholar] [CrossRef]
- Gonzales, W.; Moreno, C.; Duran, U.; Henao, N.; Bencosme, M.; Lora, P.; Reyes, R.; Nunez, R.; De Gracia, A.; Perez, A.M. African swine fever in the Dominican Republic. Transbound. Emerg. Dis. 2021, 68, 3018–3019. [Google Scholar] [CrossRef] [PubMed]
- Sauter-Louis, C.; Forth, J.H.; Probst, C.; Staubach, C.; Hlinak, A.; Rudovsky, A.; Holland, D.; Schlieben, P.; Goldner, M.; Schatz, J.; et al. Joining the club: First detection of African swine fever in wild boar in Germany. Transbound. Emerg. Dis. 2021, 68, 1744–1752. [Google Scholar] [CrossRef] [PubMed]
- Iscaro, C.; Dondo, A.; Ruocco, L.; Masoero, L.; Giammarioli, M.; Zoppi, S.; Guberti, V.; Feliziani, F. January 2022: Index case of new African Swine Fever incursion in mainland Italy. Transbound Emerg. Dis. 2022, 69, 1707–1711. [Google Scholar] [CrossRef] [PubMed]
- EFSA; Banos, J.V.; Boklund, A.; Gogin, A.; Gortazar, C.; Guberti, V.; Helyes, G.; Kantere, M.; Korytarova, D.; Linden, A.; et al. Epidemiological analyses of African swine fever in the European Union: (September 2020 to August 2021). EFSA J. 2022, 20, e07290. [Google Scholar] [CrossRef]
- Sauter-Louis, C.; Conraths, F.J.; Probst, C.; Blohm, U.; Schulz, K.; Sehl, J.; Fischer, M.; Forth, J.H.; Zani, L.; Depner, K.; et al. African Swine Fever in Wild Boar in Europe—A Review. Viruses 2021, 13, 1717. [Google Scholar] [CrossRef]
- Sauter-Louis, C.; Schulz, K.; Richter, M.; Staubach, C.; Mettenleiter, T.C.; Conraths, F.J. African swine fever: Why the situation in Germany is not comparable to that in the Czech Republic or Belgium. Transbound. Emerg. Dis. 2021, 69, 2201–2208. [Google Scholar] [CrossRef]
- Gaudreault, N.N.; Richt, J.A. Subunit Vaccine Approaches for African Swine Fever Virus. Vaccines 2019, 7, 56. [Google Scholar] [CrossRef]
- Munoz-Perez, C.; Jurado, C.; Sanchez-Vizcaino, J.M. African swine fever vaccine: Turning a dream into reality. Transbound. Emerg. Dis. 2021, 68, 2657–2668. [Google Scholar] [CrossRef]
- Netherton, C.L. 6. African swine fever vaccines. In Understanding and Combatting African Swine Fever; Wageningen Academic Publishers: Wageningen, The Netherlands, 2021; pp. 161–182. [Google Scholar]
- Ravilov, R.K.; Rizvanov, A.A.; Mingaleev, D.N.; Galeeva, A.G.; Zakirova, E.Y.; Shuralev, E.A.; Rutland, C.S.; Khammadov, N.I.; Efimova, M.A. Viral Vector Vaccines Against ASF: Problems and Prospectives. Front. Vet. Sci. 2022, 9, 830244. [Google Scholar] [CrossRef]
- Revilla, Y.; Perez-Nunez, D.; Richt, J.A. African Swine Fever Virus Biology and Vaccine Approaches. Adv. Virus Res. 2018, 100, 41–74. [Google Scholar] [CrossRef]
- Wang, Z.; Ai, Q.; Huang, S.; Ou, Y.; Gao, Y.; Tong, T.; Fan, H. Immune Escape Mechanism and Vaccine Research Progress of African Swine Fever Virus. Vaccines 2022, 10, 344. [Google Scholar] [CrossRef] [PubMed]
- Blome, S.; Gabriel, C.; Beer, M. Modern adjuvants do not enhance the efficacy of an inactivated African swine fever virus vaccine preparation. Vaccine 2014, 32, 3879–3882. [Google Scholar] [CrossRef] [PubMed]
- Cadenas-Fernandez, E.; Sanchez-Vizcaino, J.M.; van den Born, E.; Kosowska, A.; van Kilsdonk, E.; Fernandez-Pacheco, P.; Gallardo, C.; Arias, M.; Barasona, J.A. High Doses of Inactivated African Swine Fever Virus Are Safe, but Do Not Confer Protection against a Virulent Challenge. Vaccines 2021, 9, 242. [Google Scholar] [CrossRef]
- Argilaguet, J.M.; Perez-Martin, E.; Nofrarias, M.; Gallardo, C.; Accensi, F.; Lacasta, A.; Mora, M.; Ballester, M.; Galindo-Cardiel, I.; Lopez-Soria, S.; et al. DNA vaccination partially protects against African swine fever virus lethal challenge in the absence of antibodies. PLoS ONE 2012, 7, e40942. [Google Scholar] [CrossRef]
- Lacasta, A.; Ballester, M.; Monteagudo, P.L.; Rodriguez, J.M.; Salas, M.L.; Accensi, F.; Pina-Pedrero, S.; Bensaid, A.; Argilaguet, J.; Lopez-Soria, S.; et al. Expression library immunization can confer protection against African swine fever virus lethal challenge. J. Virol. 2014, 88, 13322–13332. [Google Scholar] [CrossRef] [PubMed]
- Cadenas-Fernandez, E.; Sanchez-Vizcaino, J.M.; Kosowska, A.; Rivera, B.; Mayoral-Alegre, F.; Rodriguez-Bertos, A.; Yao, J.; Bray, J.; Lokhandwala, S.; Mwangi, W.; et al. Adenovirus-vectored African Swine Fever Virus Antigens Cocktail Is Not Protective against Virulent Arm07 Isolate in Eurasian Wild Boar. Pathogens 2020, 9, 171. [Google Scholar] [CrossRef] [PubMed]
- Lokhandwala, S.; Petrovan, V.; Popescu, L.; Sangewar, N.; Elijah, C.; Stoian, A.; Olcha, M.; Ennen, L.; Bray, J.; Bishop, R.P.; et al. Adenovirus-vectored African Swine Fever Virus antigen cocktails are immunogenic but not protective against intranasal challenge with Georgia 2007/1 isolate. Vet. Microbiol. 2019, 235, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Goatley, L.C.; Reis, A.L.; Portugal, R.; Goldswain, H.; Shimmon, G.L.; Hargreaves, Z.; Ho, C.S.; Montoya, M.; Sanchez-Cordon, P.J.; Taylor, G.; et al. A Pool of Eight Virally Vectored African Swine Fever Antigens Protect Pigs Against Fatal Disease. Vaccines 2020, 8, 234. [Google Scholar] [CrossRef]
- King, K.; Chapman, D.; Argilaguet, J.M.; Fishbourne, E.; Hutet, E.; Cariolet, R.; Hutchings, G.; Oura, C.A.L.; Netherton, C.L.; Moffat, K.; et al. Protection of European domestic pigs from virulent African isolates of African swine fever virus by experimental immunisation. Vaccine 2011, 29, 4593–4600. [Google Scholar] [CrossRef]
- Abrams, C.C.; Goatley, L.; Fishbourne, E.; Chapman, D.; Cooke, L.; Oura, C.A.; Netherton, C.L.; Takamatsu, H.H.; Dixon, L.K. Deletion of virulence associated genes from attenuated African swine fever virus isolate OUR T88/3 decreases its ability to protect against challenge with virulent virus. Virology 2013, 443, 99–105. [Google Scholar] [CrossRef]
- Reis, A.L.; Goatley, L.C.; Jabbar, T.; Sanchez-Cordon, P.J.; Netherton, C.L.; Chapman, D.A.G.; Dixon, L.K. Deletion of the African Swine Fever Virus Gene DP148R Does Not Reduce Virus Replication in Culture but Reduces Virus Virulence in Pigs and Induces High Levels of Protection against Challenge. J. Virol. 2017, 91, e01428-17. [Google Scholar] [CrossRef] [PubMed]
- ODonnell, V.; Holinka, L.G.; Gladue, D.P.; Sanford, B.; Krug, P.W.; Lu, X.; Arzt, J.; Reese, B.; Carrillo, C.; Risatti, G.R.; et al. African Swine Fever Virus Georgia Isolate Harboring Deletions of MGF360 and MGF505 Genes Is Attenuated in Swine and Confers Protection against Challenge with Virulent Parental Virus. J. Virol. 2015, 89, 6048–6056. [Google Scholar] [CrossRef] [PubMed]
- Borca, M.V.; O’Donnell, V.; Holinka, L.G.; Risatti, G.R.; Ramirez-Medina, E.; Vuono, E.A.; Shi, J.; Pruitt, S.; Rai, A.; Silva, E.; et al. Deletion of CD2-like gene from the genome of African swine fever virus strain Georgia does not attenuate virulence in swine. Sci. Rep. 2020, 10, 494. [Google Scholar] [CrossRef]
- Monteagudo, P.L.; Lacasta, A.; Lopez, E.; Bosch, L.; Collado, J.; Pina-Pedrero, S.; Correa-Fiz, F.; Accensi, F.; Navas, M.J.; Vidal, E.; et al. BA71DeltaCD2: A New Recombinant Live Attenuated African Swine Fever Virus with Cross-Protective Capabilities. J. Virol. 2017, 91. [Google Scholar] [CrossRef]
- Tran, X.H.; Phuong, L.T.T.; Huy, N.Q.; Thuy, D.T.; Nguyen, V.D.; Quang, P.H.; Ngon, Q.V.; Rai, A.; Gay, C.G.; Gladue, D.P.; et al. Evaluation of the Safety Profile of the ASFV Vaccine Candidate ASFV-G-DeltaI177L. Viruses 2022, 14, 896. [Google Scholar] [CrossRef] [PubMed]
- Carrascosa, A.L.; Bustos, M.J.; de Leon, P. Methods for growing and titrating African swine fever virus: Field and laboratory samples. Curr. Protoc. Cell Biol. 2011, 53, 26.14.1–26.14.25. [Google Scholar] [CrossRef]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef]
- Li, H.; Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 2009, 25, 1754–1760. [Google Scholar] [CrossRef]
- Li, H.; Handsaker, B.; Wysoker, A.; Fennell, T.; Ruan, J.; Homer, N.; Marth, G.; Abecasis, G.; Durbin, R.; Genome Project Data Processing, S. The Sequence Alignment/Map format and SAMtools. Bioinformatics 2009, 25, 2078–2079. [Google Scholar] [CrossRef]
- Tignon, M.; Gallardo, C.; Iscaro, C.; Hutet, E.; Van der Stede, Y.; Kolbasov, D.; De Mia, G.M.; Le Potier, M.F.; Bishop, R.P.; Arias, M.; et al. Development and inter-laboratory validation study of an improved new real-time PCR assay with internal control for detection and laboratory diagnosis of African swine fever virus. J. Virol. Methods 2011, 178, 161–170. [Google Scholar] [CrossRef]
- Jackwood, M.W.; Hilt, D.A.; Sellers, H.S.; Williams, S.M.; Lasher, H.N. Rapid heat-treatment attenuation of infectious bronchitis virus. Avian Pathol. 2010, 39, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Lim, T.H.; Youn, H.N.; Yuk, S.S.; Kwon, J.H.; Hong, W.T.; Gwon, G.B.; Lee, J.A.; Lee, J.B.; Lee, S.W.; Song, C.S. Successful cross-protective efficacy induced by heat-adapted live attenuated nephropathogenic infectious bronchitis virus derived from a natural recombinant strain. Vaccine 2015, 33, 7370–7374. [Google Scholar] [CrossRef]
- Dixon, L.K.; Islam, M.; Nash, R.; Reis, A.L. African swine fever virus evasion of host defences. Virus Res. 2019, 266, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Rathakrishnan, A.; Connell, S.; Petrovan, V.; Moffat, K.; Goatley, L.C.; Jabbar, T.; Sanchez-Cordon, P.J.; Reis, A.L.; Dixon, L.K. Differential effect of deleting members of African swine fever virus multigene families 360 and 505 from the genotype II Georgia 2007/1 isolate on virus replication, virulence and induction of protection. J. Virol. 2022, 96, e01899-21. [Google Scholar] [CrossRef] [PubMed]
- Correa-Fiz, F.; Blanco-Fuertes, M.; Navas, M.J.; Lacasta, A.; Bishop, R.P.; Githaka, N.; Onzere, C.; Le Potier, M.F.; Almagro-Delgado, V.; Martinez, J.; et al. Comparative analysis of the fecal microbiota from different species of domesticated and wild suids. Sci. Rep. 2019, 9, 13616. [Google Scholar] [CrossRef] [PubMed]
- Takamatsu, H.H.; Denyer, M.S.; Lacasta, A.; Stirling, C.M.; Argilaguet, J.M.; Netherton, C.L.; Oura, C.A.; Martins, C.; Rodriguez, F. Cellular immunity in ASFV responses. Virus Res. 2013, 173, 110–121. [Google Scholar] [CrossRef]
- Borca, M.V.; Rai, A.; Ramirez-Medina, E.; Silva, E.; Velazquez-Salinas, L.; Vuono, E.; Pruitt, S.; Espinoza, N.; Gladue, D.P. A Cell Culture-Adapted Vaccine Virus against the Current African Swine Fever Virus Pandemic Strain. J. Virol. 2021, 95, e0012321. [Google Scholar] [CrossRef]
- Rossi, S.; Staubach, C.; Blome, S.; Guberti, V.; Thulke, H.-H.; Vos, A.; Koenen, F.; Le Potier, M.-F. Controlling of CSFV in European wild boar using oral vaccination: A review. Front. Microbiol. 2015, 6, 1141. [Google Scholar] [CrossRef]
- Saubusse, T.; Masson, J.D.; Le Dimma, M.; Abrial, D.; Marce, C.; Martin-Schaller, R.; Dupire, A.; Le Potier, M.F.; Rossi, S. How to survey classical swine fever in wild boar (Sus scrofa) after the completion of oral vaccination? Chasing away the ghost of infection at different spatial scales. Vet. Res. 2016, 47, 21. [Google Scholar] [CrossRef]
| Trial # | Group Number | Group Name | Nb of Pigs | Inoculation (D0) | Challenge | Necropsy |
|---|---|---|---|---|---|---|
| 1 | A1 | Control | 3 | / | / | D100 |
| B | 989 ON LT | 5 | 989 ON | / | D100 | |
| C | 989 IM LT | 5 | 989 IM | / | D100 | |
| D | 989 IM/Geo IM D28 | 6 | 989 IM | Georgia IM D28 | D68 | |
| E | Geo IM D0 | 3 | Georgia IM | D6 | ||
| F | Geo ON D0 | 4 | Georgia ON | D6 | ||
| G | Geo IM D28 | 3 | / | Georgia IM D28 | D34 | |
| 2 | A2 | Control | 5 | / | / | D54 |
| H | 989 ON/Geo ON D28 | 6 | 989 ON | Georgia ON D28 | D68 | |
| I | 989 ON/Geo IM D28 | 6 | 989 ON | Georgia IM D28 | D68 | |
| J | Geo ON D28 | 4 | Georgia ON D28 | D34 | ||
| 3 | A3 | Control | 3 | / | / | D54 |
| K | 989 IM/Geo IM D14 | 6 | 989 IM | Georgia IM D14 | D54 | |
| L | 989 ON/Geo ON D14 | 6 | 989 ON | Georgia ON D14 | D54 |
| Day Post-Challenge | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | Pig # | −1 | 3 | 5 | 7 | 11 | 13 | 18 | 25 | ||||||||
| PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | ||
| Geo IM D28 (group G) | 370 | ND | 6.1 | 8.8 | † | † | † | † | † | ||||||||
| 532 | ND | 5.4 | 8.9 | † | † | † | † | † | |||||||||
| 7301 | ND | 6.5 | 9.2 | † | † | † | † | † | |||||||||
| mean | 6.0 | 8.9 | |||||||||||||||
| 989 IM/Geo IM (group D) | 130 | 5.7 | ND | 5.4 | ND | 5.3 | ND | 5.1 | ND | 5.0 | ND | 5.1 | ND | 4.8 | ND | 4.6 | |
| 151 | 4.7 | ND | 4.6 | ND | 4.4 | ND | 4.2 | ND | 3.8 | ND | 4.2 | ND | 3.5 | ND | 3.7 | ||
| 159 | 4.6 | ND | 4.4 | 5.7 | 4.3 | ND | 4.0 | ND | 4.0 | ND | 4.2 | ND | 3.9 | ND | 3.9 | ||
| 7313 | 5.3 | ND | 5.3 | ND | 5.2 | ND | 5.0 | ND | 4.8 | ND | 4.7 | ND | 4.4 | ND | 4.4 | ||
| mean | 5.1 | 4.9 | 4.8 | 4.6 | 4.4 | 4.6 | 4.1 | 4.1 | |||||||||
| 989 ON/Geo IM (group I) | 7357 | 5.2 | ND | 4.6 | ND | 4.4 | ND | 4.1 | ND | 3.7 | ND | 3.6 | ND | 3.3 | ND | 3.3 | |
| 7374 | 5.2 | ND | 4.8 | ND | 4.7 | ND | 4.7 | ND | 4.0 | ND | 4.2 | ND | 3.1 | ND | 3.0 | ||
| 7386 | 4.5 | ND | 3.8 | ND | 3.8 | ND | 3.2 | ND | ND | ND | 2.7 | ND | ND | ND | ND | ||
| 7391 | 5.7 | ND | 5.0 | ND | 5.0 | ND | 5.2 | ND | 4.6 | ND | 5.0 | ND | 4.9 | ND | 4.2 | ||
| 7399 | 5.2 | ND | 4.3 | ND | 4.5 | ND | 4.6 | ND | 4.0 | ND | 4.0 | ND | 4.0 | ND | 3.4 | ||
| 7401 | 5.2 | ND | 5.0 | ND | 4.6 | ND | 4.6 | ND | 4.2 | ND | 4.5 | ND | 4.1 | ND | 3.9 | ||
| mean | 5.2 | 4.6 | 4.5 | 4.4 | 4.1 | 4.0 | 3.9 | 3.6 | |||||||||
| Day Post-Challenge | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | Pig # | −1 | 3 | 5 | 7 | 11 | 13 | 18 | 25 | ||||||||
| PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | ||
| Geo ON D28 (group J) | 7356 | ND | 4.4 | 8.8 | † | † | † | † | † | ||||||||
| 7365 | ND | 3.3 | 8.4 | † | † | † | † | † | |||||||||
| 7382 | ND | 4.2 | 9.3 | † | † | † | † | † | |||||||||
| 7400 | ND | 4.9 | 9.4 | † | † | † | † | † | |||||||||
| mean | 4.2 | 9.0 | |||||||||||||||
| 989 ON/Geo ON (group H) | 7358 | 5.0 | ND | 4.5 | ND | 4.1 | ND | 3.9 | ND | 4.0 | ND | 3.2 | ND | 3.4 | ND | 2.6 | |
| 7372 | 5.2 | ND | 4.7 | ND | 4.4 | ND | 3.9 | ND | 3.7 | ND | 3.6 | ND | 2.4 | ND | ND | ||
| 7375 | 4.9 | ND | 4.0 | ND | 4.1 | ND | 3.5 | ND | 3.6 | ND | 3.0 | ND | ND | ND | 3.4 | ||
| 7397 | 5.2 | ND | 4.3 | ND | 4.3 | ND | 4.3 | ND | 4.2 | ND | 4.1 | ND | 3.9 | ND | 3.8 | ||
| 7403 | 5.0 | ND | 4.0 | ND | 3.9 | ND | 3.9 | ND | 3.7 | ND | 3.4 | ND | 3.9 | ND | 3.3 | ||
| 7404 | 4.7 | ND | 3.8 | ND | 3.4 | ND | 3.5 | ND | ND | ND | 3.2 | ND | 3.7 | ND | ND | ||
| mean | 5.0 | 4.2 | 4.0 | 3.8 | 3.9 | 3.4 | 3.4 | 3.3 | |||||||||
| Group | Pig # | Day Post-Challenge | Tonsil | Spleen | Hepato-Gastric LN | |||
|---|---|---|---|---|---|---|---|---|
| PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | |||
| 989 IM/Geo IM (group D) | 130 | 41 | ND | ND | ND | ND | ND | ND |
| 151 | 41 | ND | ND | ND | ND | ND | 41.0 | |
| 159 | 41 | ND | 36.8 | ND | ND | ND | ND | |
| 7313 | 41 | ND | 37.5 | ND | 39.7 | ND | 39.9 | |
| 989 ON/Geo IM (group I) | 7357 | 40 | ND | ND | ND | 40.9 | ND | ND |
| 7374 | 40 | ND | 36.8 | ND | ND | ND | ND | |
| 7386 | 40 | ND | 38.1 | ND | ND | ND | ND | |
| 7391 | 40 | ND | 37.2 | ND | ND | ND | 43.6 | |
| 7399 | 40 | 27.6 | ND | 36.7 | ND | 41.1 | ND | |
| 7401 | 40 | 32.6 | ND | ND | ND | 32.2 | ND | |
| 989 ON/Geo ON (group H) | 7358 | 39 | ND | ND | ND | ND | ND | ND |
| 7372 | 39 | ND | 30.9 | ND | 41.9 | ND | ND | |
| 7375 | 39 | ND | ND | ND | 39.6 | ND | ND | |
| 7397 | 39 | ND | ND | 37.5 | ND | ND | ND | |
| 7403 | 39 | ND | ND | ND | 39.6 | ND | 39.8 | |
| 7404 | 39 | ND | ND | 43.4 | 40.8 | ND | ND | |
| Day Post-Immunization (Georgia Challenge à D14) | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | Pig # | 0 | 3 | 5 | 7 | 11 | 13 | 17 | 19 | 21 | 25 | 27 | 34 | 41 | 46 | 54 | ||||||||||
| PCR 989 | PCR 989 | PCR 989 | PCR 989 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | ||
| 989 IM/Geo IM D14 | 7883 | 0.0 | 5.7 | 6.1 | 6.3 | 6.4 | ND | 5.7 | ND | 5.6 | ND | 5.4 | ND | 5.7 | ND | 5.5 | ND | 5.0 | ND | 4.7 | ND | 4.2 | ND | 4.2 | ND | 3.8 |
| 7890 | 0.0 | 5.3 | 5.9 | 5.9 | 5.9 | ND | 5.7 | ND | 5.3 | ND | 5.3 | ND | 5.4 | ND | 5.3 | ND | 4.8 | ND | 4.5 | ND | 3.6 | ND | 3.0 | ND | 0.0 | |
| 7891 | 0.0 | 6.2 | 6.4 | 6.6 | 6.8 | † | † | † | † | † | † | † | † | † | † | |||||||||||
| 7895 | 0.0 | 5.8 | 5.9 | 5.9 | 5.4 | ND | 5.5 | ND | 5.2 | ND | 5.2 | ND | 5.1 | ND | 5.1 | ND | 4.7 | ND | 4.6 | ND | 3.1 | ND | 3.1 | ND | 4.0 | |
| 7901 | 0.0 | 4.8 | 6.3 | 6.1 | 5.9 | ND | 5.7 | ND | 5.6 | ND | 5.5 | ND | 5.5 | ND | 5.2 | ND | 4.7 | ND | 4.0 | ND | 3.8 | ND | 3.3 | ND | 0.0 | |
| 7908 | 0.0 | 6.2 | 5.8 | 5.6 | 5.3 | ND | 5.4 | ND | 5.2 | ND | 5.3 | ND | 5.1 | ND | 4.2 | ND | 4.1 | ND | 3.8 | ND | 0.0 | ND | 0.0 | ND | 3.1 | |
| mean | 0.0 | 5.7 | 6.1 | 6.1 | 6.0 | 5.6 | 5.4 | 5.3 | 5.4 | 5.1 | 4.6 | 4.3 | 3.0 | 2.7 | 2.2 | |||||||||||
| 989 ON/Geo ON D14 | 7882 | 0.0 | 3.2 | 6.4 | 6.5 | 5.8 | ND | 5.8 | ND | 5.8 | ND | 5.5 | ND | 5.3 | ND | 5.0 | ND | 4.5 | ND | 4.1 | ND | 3.5 | ND | 0.0 | ND | 3.5 |
| 7888 | 0.0 | 4.0 | 5.9 | 5.5 | 5.7 | ND | 5.5 | ND | 5.3 | ND | 4.7 | ND | 4.8 | ND | 4.4 | ND | 4.1 | ND | 0.0 | ND | 3.6 | ND | 3.3 | ND | 0.0 | |
| 7889 | 0.0 | 0.0 | 6.0 | 5.7 | 5.8 | ND | 5.8 | ND | 5.3 | ND | 5.2 | ND | 5.3 | ND | 4.7 | ND | 4.0 | ND | 3.5 | ND | 3.7 | ND | 0.0 | ND | 3.4 | |
| 7893 | 0.0 | 0.0 | 6.0 | 5.9 | 6.2 | ND | 5.9 | ND | 5.4 | ND | 5.2 | ND | 4.7 | ND | 4.5 | ND | 4.2 | ND | 3.6 | ND | 3.4 | ND | 3.8 | ND | 3.0 | |
| 7904 | 0.0 | 0.0 | 5.8 | 5.2 | 5.1 | ND | 5.0 | ND | 5.1 | ND | 4.7 | ND | 4.6 | ND | 4.6 | ND | 4.5 | ND | 4.1 | ND | 4.1 | ND | 3.5 | ND | 3.1 | |
| 7907 | 0.0 | 0.0 | 5.4 | 5.3 | 5.2 | ND | 5.1 | ND | 4.8 | ND | 4.7 | ND | 5.0 | ND | 5.0 | ND | 4.5 | ND | 4.4 | ND | 0.0 | ND | 3.6 | ND | 3.4 | |
| mean | 0.0 | 1.2 | 6.0 | 5.7 | 5.6 | 5.5 | 5.3 | 5.0 | 5.0 | 4.7 | 4.3 | 3.3 | 3.1 | 2.4 | 2.7 | |||||||||||
| Group | Pig # | Day Post-Challenge | Tonsil | Spleen | Hepato-Gastric LN | |||
|---|---|---|---|---|---|---|---|---|
| PCR 505 | PCR 989 | PCR 505 | PCR 989 | PCR 505 | PCR 989 | |||
| 989 IM/Geo IM D14 | 7883 | 53-55 | ND | 27.6 | ND | 32.5 | ND | 36.3 |
| 7890 | 53-55 | ND | 40.5 | ND | 38.3 | ND | 38.5 | |
| 7891 | 12 | ND | 30.2 | ND | 25.9 | ND | 29.1 | |
| 7895 | 53-55 | ND | 31.7 | ND | 36.1 | ND | 35.0 | |
| 7901 | 53-55 | ND | 34.9 | ND | 37.2 | ND | 40.1 | |
| 7908 | 53-55 | ND | 35.2 | ND | 40.7 | ND | ND | |
| 989 ON/Geo ON D14 | 7882 | 53-55 | ND | ND | ND | 39.7 | ND | ND |
| 7888 | 53-55 | ND | 40.7 | ND | 43.5 | ND | 35.1 | |
| 7889 | 53-55 | ND | 38.8 | ND | 39.8 | ND | 34.9 | |
| 7893 | 53-55 | ND | ND | ND | 35.5 | ND | 35.7 | |
| 7904 | 53-55 | ND | 41.1 | ND | ND | ND | ND | |
| 7907 | 53-55 | ND | 30.7 | ND | 40.0 | ND | 36.1 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bourry, O.; Hutet, E.; Le Dimna, M.; Lucas, P.; Blanchard, Y.; Chastagner, A.; Paboeuf, F.; Le Potier, M.-F. Oronasal or Intramuscular Immunization with a Thermo-Attenuated ASFV Strain Provides Full Clinical Protection against Georgia 2007/1 Challenge. Viruses 2022, 14, 2777. https://doi.org/10.3390/v14122777
Bourry O, Hutet E, Le Dimna M, Lucas P, Blanchard Y, Chastagner A, Paboeuf F, Le Potier M-F. Oronasal or Intramuscular Immunization with a Thermo-Attenuated ASFV Strain Provides Full Clinical Protection against Georgia 2007/1 Challenge. Viruses. 2022; 14(12):2777. https://doi.org/10.3390/v14122777
Chicago/Turabian StyleBourry, Olivier, Evelyne Hutet, Mireille Le Dimna, Pierrick Lucas, Yannick Blanchard, Amélie Chastagner, Frédéric Paboeuf, and Marie-Frédérique Le Potier. 2022. "Oronasal or Intramuscular Immunization with a Thermo-Attenuated ASFV Strain Provides Full Clinical Protection against Georgia 2007/1 Challenge" Viruses 14, no. 12: 2777. https://doi.org/10.3390/v14122777
APA StyleBourry, O., Hutet, E., Le Dimna, M., Lucas, P., Blanchard, Y., Chastagner, A., Paboeuf, F., & Le Potier, M.-F. (2022). Oronasal or Intramuscular Immunization with a Thermo-Attenuated ASFV Strain Provides Full Clinical Protection against Georgia 2007/1 Challenge. Viruses, 14(12), 2777. https://doi.org/10.3390/v14122777





