Would Zika virus Infection in Pregnancy Be a Sentence of Poor Neurological Prognosis for Exposed Children? Neurodevelopmental Outcomes in a Cohort from Brazilian Amazon
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Patient Care
2.4. Laboratory Testing
2.5. Definitions
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Coyne, C.B.; Lazear, H.M. Zika virus-reigniting the TORCH. Nat. Rev. Microbiol. 2016, 14, 707–715. [Google Scholar] [CrossRef]
- De Barros Miranda-Filho, D.; Martelli, C.M.T.; de Alencar Ximenes, R.A.; Araújo, T.V.B.; Rocha, M.A.W.; Ramos, R.C.F.; Dhalia, R.; de Oliveira França, R.F.; de Azevedo Marques Júnior, E.T.; Rodrigues, L.C. Initial description of the presumed congenital Zika syndrome. Am. J. Public Health 2016, 106, 598–600. [Google Scholar] [CrossRef] [PubMed]
- De Araújo, T.V.B.; Rodrigues, L.C.; de Alencar Ximenes, R.A.; de Barros Miranda-Filho, D.; Montarroyos, U.R.; de Melo, A.P.L.; Valongueiro, S.; de Albuquerque, M.D.P.M.; Souza, W.V.; Braga, C.; et al. Association between Zika virus infection and microcephaly in Brazil, January to May, 2016: Preliminary report of a case-control study. Lancet Infect. Dis. 2016, 16, 1356–1363. [Google Scholar] [CrossRef] [PubMed]
- Secretaria Municipal de Saúde P de, M. 68o Informe Epidemiológico, 12/01/2017, Febre do Zika Vírus. 2017. Available online: http://semsa.manaus.am.gov.br/semsa-divulga-novo-informe-sobre-o-zika-virus-2/ (accessed on 13 May 2021).
- Cugola, F.R.; Fernandes, I.R.; Russo, F.B.; Freitas, B.C.; Dias, J.L.M.; Guimarães, K.P.; Benazzato, C.; Almeida, N.; Pignatari, G.C.; Romero, S.; et al. The Brazilian Zika virus strain causes birth defects in experimental models. Nat. Cell Biol. 2016, 534, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Moore, C.A.; Staples, E.J.; Dobynns, W.B.; Pessoa, A.; Ventura, C.V.; Fonseca, E.B.; Ribeiro, E.M.; Ventura, L.O.; Nogueira Neto, N.; Arena, J.F. Congenital Zika Syndrome: Characterizing the Pattern of Anomalies for Pediatric Healthcare Providers. N. Engl. J. Med. 2016, 374, 331–333. [Google Scholar]
- Del Campo, M.; Feitosa, I.M.L.; Ribeiro, E.M.; Horovitz, D.D.G.; Pessoa, A.L.S.; França, G.V.A.; García-Alix, A.; Doriqui, M.J.R.; Wanderley, H.Y.C.; Sanseverino, M.V.T.; et al. The phenotypic spectrum of congenital Zika syndrome. Am. J. Med. Genet. Part A 2017, 173, 841–857. [Google Scholar] [CrossRef]
- Cranston, J.S.; Tiene, S.F.; Nielsen-Saines, K.; Vasconcelos, Z.; Pone, M.V.; Pone, S.; Zin, A.; Salles, T.S.; Pereira, J.P., Jr.; Orofino, D.; et al. Association Between Antenatal Exposure to Zika virus and Anatomical and Neurodevelopmental Abnormalities in Children. JAMA Netw. Open 2020, 3, e209303. [Google Scholar] [CrossRef] [PubMed]
- Brasil, P.; Pereira, J.P.; Moreira, M.E.; Ribeiro Nogueira, R.M.; Damasceno, L.; Wakimoto, M.; Rabello, R.S.; Valderramos, S.G.; Halai, U.-A.; Salles, T.S.; et al. Zika virus Infection in Pregnant Women in Rio de Janeiro. N. Engl. J. Med. 2016, 375, 2321–2334. [Google Scholar] [CrossRef]
- Redivo, E.d.F.; Bôtto Menezes, C.; da Costa Castilho, M.; Brock, M.; da Silva Magno, E.; Gomes Saraiva, M.d.G.; Alvarez Fernandes, S.S.; Costa Antony de Andrade, A.B.; Costa Alecrim, M.d.G.; Martinez-Espinosa, F.E. Zika virus Infection in a Cohort of Pregnant Women with Exanthematic Disease in Manaus, Brazilian Amazon. Viruses 2020, 12, 1362. [Google Scholar] [CrossRef]
- Villar, J.; Ismail, L.C.; Victora, C.G.; Ohuma, E.O.; Bertino, E.; Altman, D.G.; Lambert, A.; Papageorghiou, A.T.; Carvalho, M.; Jaffer, Y.A.; et al. International standards for newborn weight, length, and head circumference by gestational age and sex: The Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 2014, 384, 857–868. [Google Scholar] [CrossRef]
- International Fetal and Newborn Growth Consortium for the 21st Century I-21st. Neonatal Size Calculator for Newborn Infants between 24+0 and 42+6 Weeks’ Gestation; University of Oxford: Oxford, UK, 2009; Available online: https://intergrowth21.tghn.org/newborn-size-birth/#c4 (accessed on 7 April 2020).
- Babson, S.G. Growth of low-birth-weight infants. J. Pediatr. 1970, 77, 11–18. [Google Scholar] [CrossRef]
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Head Circumference-for-Age, Arm Circumference-for-Age, Triceps Skinfold-for-Age and Subscapular Skinfold-for-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2007; p. 217.
- World Health Organization. The WHO Anthro Software; WHO, Department of Nutrition: Geneva, Switzerland. Available online: https://www.who.int/tools/child-growth-standards/software (accessed on 7 April 2020).
- Brasil. Ministério da Saúde. Caderneta de Saúde da Criança Menina [Internet]. 11a Edição. Brasília—DF. 2017; pp. 44–47. Available online: http://bvsms.saude.gov.br/bvs/publicacoes/caderneta_saude_crianca_menina_11ed.pdf (accessed on 20 March 2019).
- Brasil. Ministério da Saúde. Caderneta de Saúde da Criança Menino [Internet]. 11o Edição. Brasília—DF. 2017; pp. 44–47. Available online: http://bvsms.saude.gov.br/bvs/publicacoes/caderneta_saude_crianca_menino_11ed.pdf (accessed on 20 March 2019).
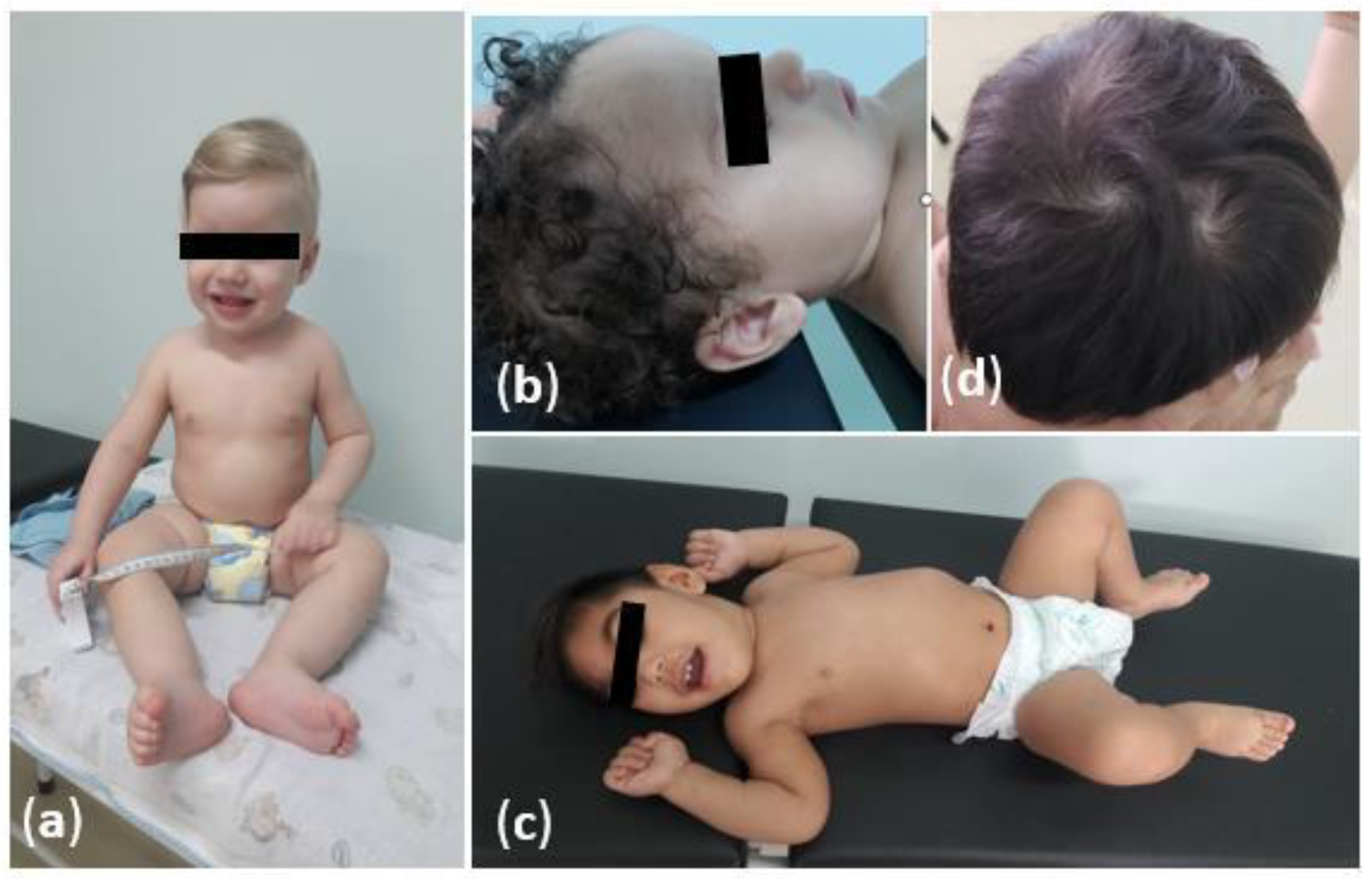
- Abtibol-Bernardino, M.; Peixoto, L.D.A.; De Oliveira, G.; De Almeida, T.; Rodrigues, G.; Otani, R.; Chaves, B.S.; Rodrigues, C.D.S.; De Andrade, A.; Redivo, E.D.F.; et al. Neurological Findings in Children without Congenital Microcephaly Exposed to Zika virus in Utero: A Case Series Study. Viruses 2020, 12, 1335. [Google Scholar] [CrossRef]
- Prechtl, H.; Beintema, D. The Neurological Examination of the Full-term Neborn Infant. A Manual for Clinical Use from the Department of Expeimental Neurology University of Groningen; The Spastics Society (Medical Education and Information Unit) in Association with William Heinemann Medical Books; Cambridge University Press: London, UK, 1964; p. 529. [Google Scholar]
- Funayama, C.A.R. Exame neurológico em crianças. Semiologia Espec. 1996, 29, 32–43. [Google Scholar] [CrossRef][Green Version]
- Lanciotti, R.S.; Kosoy, O.L.; Laven, J.J.; Velez, J.O.; Lambert, A.J.; Johnson, A.J.; Stanfield, S.M.; Duffy, M.R. Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg. Infect. Dis. 2008, 14, 1232–1239. [Google Scholar] [CrossRef] [PubMed]
- Moore, C.A.; Staples, J.E.; Dobyns, W.B.; Pessoa, A.; Ventura, C.V.; Da Fonseca, E.B.; Ribeiro, E.M.; Ventura, L.O.; Neto, N.N.; Arena, J.F.; et al. Characterizing the pattern of anomalies in congenital zika syndrome for pediatric clinicians. JAMA Pediatr. 2017, 171, 288–295. [Google Scholar] [CrossRef]
- Fisher, R.S.; Acevedo, C.; Arzimanoglou, A.; Bogacz, A.; Cross, J.H.; Elger, C.E.; Engel, J., Jr.; Forsgren, L.; French, J.A.; Glynn, M.; et al. ILAE Official Report: A practical clinical definition of epilepsy. Epilepsia 2014, 55, 475–482. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Neurodevelopmental disorders. In Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Palisano, R.; Rosenbaum, P.; Bartlett, D.; Livingston, M.; Walter, S.; Russell, D. GMFCS-E & R- Sistema de Classificação da Função Motora Grossa. Ref. Dev. Med. Child Neurol. 2007, 39, 214–223. Available online: www.canchild.ca (accessed on 17 January 2020).
- Alves, L.V.; Paredes, C.E.; Silva, G.C.; Mello, J.G.; Alves, J.G. Neurodevelopment of 24 children born in Brazil with congenital Zika syndrome in 2015: A case series study. BMJ Open 2018, 8, e021304. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J. Environment and Birth Defects; Academic Press: New York, NY, USA, 1973. [Google Scholar]
- Cavalheiro, S.; Lopez, A.; Serra, S.; Da Cunha, A.; Da Costa, M.D.S.; Moron, A.; Lederman, H.M. Microcephaly and Zika virus: Neonatal neuroradiological aspects. Child’s Nerv. Syst. 2016, 32, 1057–1060. [Google Scholar] [CrossRef][Green Version]
- Kattuoa, M.L.M.; Das, J. Lissencephaly; Stat Pearls: Treasure Island, FL, USA, 2021. [Google Scholar]
- Brasil, P.; Pereira, J.P.; Gabaglia, C.R.; Damasceno, L.; Wakimoto, M.; Nogueira, R.M.R.; De Sequeira, P.C.; Siqueira, A.; De Carvalho, L.M.A.; Da Cunha, D.C.; et al. Zika virus Infection in Pregnant Women in Rio de Janeiro-Preliminary Report. Obs. Gynecol. Surv. 2016, 71, 331–333. [Google Scholar] [CrossRef]
- Peçanha, P.M.; Gomes Junior, S.C.; Pone, S.M.; da Silva Pone, M.V.; Vasconcelos, Z.; Zin, A.; Vilibor, R.H.H.; Costa, R.P.; Meio, M.D.B.B.; Nielsen-Saines, K.; et al. Neurodevelopment of children exposed intra-uterus by Zika virus: A case series. PLoS ONE 2020, 15, e0229434. [Google Scholar] [CrossRef] [PubMed]
- Moreira, M.E.L.; Nielsen-Saines, K.; Brasil, P.; Kerin, T.; Damasceno, L.; Pone, M.; Carvalho, L.M.; Pone, S.M.; Vasconcelos, Z.; Ribeiro, I.P.; et al. Neurodevelopment in infants exposed to Zika virus in utero. N. Engl. J. Med. Massachussetts Med. Soc. 2018, 379, 2377–2379. [Google Scholar] [CrossRef] [PubMed]
- Ximenes, R.A.D.A.; Miranda-Filho, D.D.B.; Montarroyos, U.R.; Martelli, C.M.T.; de Araújo, T.V.B.; Brickley, E.; Albuquerque, M.D.F.P.M.D.; Souza, W.V.; Ventura, L.O.; Ventura, C.V.; et al. Zika-related adverse outcomes in a cohort of pregnant women with rash in Pernambuco, Brazil. PLoS Negl. Trop. Dis. 2021, 15, e0009216. [Google Scholar] [CrossRef]
- Aragao, M.F.V.V.; Holanda, A.C.; Brainer-Lima, A.M.; Petribu, N.C.L.; Castillo, M.; van der Linden, V.; Serpa, S.C.; Tenório, A.G.; Travassos, P.T.C.; Cordeiro, M.T.; et al. Nonmicrocephalic Infants with Congenital Zika Syndrome Suspected Only after Neuroimaging Evaluation Compared with Those with Microcephaly at Birth and Postnatally: How Large Is the Zika virus “Iceberg”? AJNR Am. J. Neuroradiol. 2017, 38, 1427–1434. [Google Scholar] [CrossRef]
- Ospina, M.L.; Tong, V.T.; Gonzalez, M.; Valencia, D.; Mercado, M.; Gilboa, S.M.; Rodriguez, A.J.; Tinker, S.C.; Rico, A.; Winfield, C.M.; et al. Zika virus Disease and Pregnancy Outcomes in Colombia. N. Engl. J. Med. 2020, 383, 537–545. [Google Scholar] [CrossRef]
- Reynolds, M.R.; Jones, A.M.; Petersen, E.E.; Lee, E.H.; Rice, M.E.; Bingham, A.; Ellington, S.R.; Evert, N.; Reagan-Steiner, S.; Oduyebo, T.; et al. Vital Signs: Update on Zika virus-Associated Birth Defects and Evaluation of All U.S. Infants with Congenital Zika virus Exposure—U.S. Zika Pregnancy Registry, 2016. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 366–373. Available online: http://www.cdc.gov/mmwr/volumes/66/wr/mm6613e1.htm%0Apapers3://publication/doi/10.15585/mmwr.mm6613e1 (accessed on 11 June 2019). [CrossRef]
- Hoen, B.; Schaub, B.; Funk, A.L.; Ardillon, V.; Boullard, M.; Cabié, A.; Callier, C.; Carles, G.; Cassadou, S.; Césaire, R.; et al. Pregnancy Outcomes after ZIKV Infection in French Territories in the Americas. N. Engl. J. Med. 2018, 378, 985–994. [Google Scholar] [CrossRef]
- Van der Linden, V.; Pessoa, A.; Dobyns, W.; Barkovich, A.J.; van der Júnior, H.L.; Filho, E.L.R.; Ribeiro, E.M.; Leal, M.D.; Coimbra, P.P.D.; Aragão, M.D.V.V.; et al. Description of 13 Infants Born during October 2015–January 2016 with Congenital Zika virus Infection without Microcephaly at Birth—Brazil. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 1343–1348. [Google Scholar] [CrossRef] [PubMed]
- Shapiro-Mendoza, C.K.; Rice, M.E.; Galang, R.R.; Fulton, A.C.; VanMaldeghem, K.; Prado, M.V.; Ellis, E.; Anesi, M.S.; Simeone, R.M.; Petersen, E.E.; et al. Pregnancy Outcomes after Maternal Zika virus Infection during Pregnancy—U.S. Territories, January 1, 2016–April 25, 2017. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 615–621. Available online: http://www.mendeley.com/research/pregnancy-outcomes-after-maternal-zika-virus-infection-during-pregnancy-2 (accessed on 6 April 2019). [CrossRef] [PubMed]
- Winden, K.D.; Yuskaitis, C.J.; Poduri, A. Megalencephaly and macrocephaly. Semin. Neurol. 2015, 35, 277–287. [Google Scholar] [CrossRef]
- Swaiman, K.F.; Ashwal, S.; Ferriero, D.M.; Schor, N.F. Swaiman’s Pediatric Neurology: Principles and Practice; Swaiman, K., Ashwal, S., Shevell, M., Eds.; Elsevier Saunders: Edinburgh, UK, 2012; 173p. [Google Scholar]
- Vianna, P.; Gomes, J.D.A.; Boquett, J.A.; Fraga, L.R.; Schuch, J.B.; Vianna, F.S.L.; Schuler-Faccini, L. Zika virus as a possible risk factor for autism spectrum disorder: Neuroimmunological aspects. Neuroimmunomodulation 2019, 25, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.; Sharifi-Hannauer, P.; Martinez-Agosto, J.A. Macrocephaly as a clinical indicator of genetic subtypes in autism. Autism Res. 2013, 6, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Krogh, K.; Green, M.; Thayer, S. HIV-1 Tat-Induced Changes in Synaptically-Driven Network Activity Adapt During Prolonged Exposure. Curr. HIV Res. 2015, 12, 406–414. [Google Scholar] [CrossRef][Green Version]
- Abu-Raya, B.; Kollmann, T.R.; Marchant, A.; MacGillivray, D.M. The immune system of HIV-exposed uninfected infants. Front. Immunol. 2016, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Wedderburn, C.J.; Evans, C.; Yeung, S.; Gibb, D.M.; Donald, K.A.; Prendergast, A.J. Growth and Neurodevelopment of HIV-Exposed Uninfected Children: A Conceptual Framework. Curr. HIV/AIDS Rep. 2019, 16, 501–513. [Google Scholar] [CrossRef]
| Baseline Characteristics | Microcephaly n/Total | Normocephaly n/Total | Macrocephaly n/Total | n/Total (%) |
|---|---|---|---|---|
| Age (average ± SD) | 22.5 ± 6.6 | 28 ± 6.4 | 27.7 ± 6.3 | 27.8 ± 6.3 |
| ≤19 years, n(%) | 0/4 (0%) | 6/65 (9.3%) | 0/8 (0%) | 6/77 (7.8%) |
| 20–34 years, n(%) | 4/4 (100%) | 47/65 (72.1%) | 6/8 (75%) | 57/77 (74%) |
| ≥35 years, n(%) | 0/4 (0%) | 12/65 (18.6%) | 2/8 (25%) | 14/77 (18.2%) |
| Years of schooling | ||||
| 0–8, n(%) | 2/3 (66.7%) | 8/62 (12.9%) | 2/8 (25%) | 12/73 (16.5%) |
| 9–11, n(%) | 1/3 (33.3%) | 36/62 (58.1%) | 2/8 (25%) | 39/73 (53.4%) |
| >12 years, n(%) | 0/3 (0%) | 18/62 (29%) | 4/8 (50%) | 22/73 (30.1%) |
| Hypertensive disease, n(%) | 1/4 (25%) | 10/65 (15.4%) | 0/8 (0%) | 11/77 (14.3%) |
| Gestational diabetes, n(%) | 0/4 (0%) | 1/65 (1.5%) | 2/8 (25%) | 3/77 (3.9%) |
| Tobacco intake, n(%) | 0/4 (0%) | 1/65 (1.5%) | 0/8 (0%) | 1/77 (1.3%) |
| Alcohol intake, n(%) | 0/4 (0%) | 2/65 (3%) | 0/8 (0%) | 2/77 (2.6%) |
| Illicit drugs intake, n(%) | 0/4 (0%) | 0/65 (0%) | 0/8 (0%) | 0/77 (0%) |
| Gestational bleeding, n(%) | 0/4 (0%) | 3/65 (4.6%) | 1/8 (12.5%) | 4/77 (5.2%) |
| Depression, n(%) | 0/4 (0%) | 1/65 (1.5%) | 0/8 (0%) | 1/77 (1.3%) |
| Trimester of ZIKV infection | ||||
| 1st trimester, n(%) | 4/4 (100%) | 13/65 (20.1%) | 2/8 (25%) | 19/77 (24.6%) |
| 2nd trimester, n(%) | 0/4 (0%) | 24/65 (36.9%) | 5/8 (62.5%) | 29/77 (37.7%) |
| 3rd trimester, n(%) | 0/4 (0%) | 28/65 (43%) | 1/8 (12.5%) | 29/77 (37.7%) |
| Coinfection occurrence, n (%) | 0/4 (0%) | 13/65 (20.1%) * | 2/8 (25%) * | 15/77 (19.5%) * |
| Herpes simplex type 1 and 2, n(%) | 0/4 (0%) | 4/65 (6.1%) | 1/8 (12.5%) | 5/77 (6.5%) |
| Parvovirus B19, n(%) | 0/4 (0%) | 1/65 (1.5%) | 1/8 (12.5%) | 2/77 (2.6%) |
| HIV, n(%) | 0/4 (0%) | 1/65 (1.5%) | 1/8 (12.5%) | 2/77 (2.6%) |
| Epistein-Barr, n(%) | 0/4 (0%) | 1/65 (1.5%) | 0/8 (0%) | 1/77 (1.3%) |
| Hepatitis B, n(%) | 0/4 (0%) | 1/65 (1.5%) | 0/8 (0%) | 1/77 (1.3%) |
| Dengue, n(%) | 0/4 (0%) | 4/65 (6.1%) | 0/8 (0%) | 4/77 (5.2%) |
| Toxoplasmosis, n(%) | 0/4 (0%) | 2/65 (3%) | 0/8 (0%) | 2/77 (2.6%) |
| Malaria, n(%) | 0/4 (0%) | 1/65 (1.5%) | 0/8 (0%) | 1/77 (1.3%) |
| Birth and Neonatal Variables | Microcephaly n/Total | Normocephaly n/Total | Macrocephaly n/Total | Total |
|---|---|---|---|---|
| Type of delivery | ||||
| Vaginal | 1/4 (25%) | 33/65 (50.8%) | 1/8 (12.5%) | 35/77 (45.5%) |
| C-section | 3/4 (75 %) | 32/65 (49.2%) | 7/8 (87.5%) | 42/77 (54.5%) |
| Gender | ||||
| Male | 3/4 (75 %) | 26/65 (40%) | 7/8 (87.5%) | 36/77 (46.7%) |
| Female | 1/4 (25%) | 39/65 (60%) | 1/8 (12.5%) | 41/77 (53.3%) |
| Apgar at 5th min < 7 | 0/4 (0%) | 1/64 (1.6%) | 0/7 (0%) | 1/75 (1.3%) |
| Gestational age, (average ± SD) | 39.2 ± 0.9 | 39 ± 0.9 | 39 ± 1 | 39 ± 0.96 |
| Prematurity | 0/4 (0%) | 5/65 (7.7%) | 0/8 (0%) | 5/77 (6.5%) |
| Intracranial bleeding | ||||
| Grades I and II | 0/4 (0%) | 3/65 (4.6%) | 0/8 (0%) | 3/77 (3.9 %) |
| Grades III and IV | 1/4 (25%) | 0/65 (0%) | 0/8 (0%) | 1/77 (1.3%) |
| Neonatal sepsis | 0/4 (0%) | 5/65 (7.7%) | 0/8 (0%) | 5/77 (6.5%) |
| Neonatal jaundice | 1/4 (25%) | 15/65 (23%) | 2/8 (25%) | 18/77 (23.4%) |
| Neonatal crises | 3/4 (75 %) | 0/65 (0%) | 0/8 (0%) | 3/77 (3.9 %) |
| Hyaline membrane disease | 0/4 (0%) | 1/65 (1.5%) | 0/8 (0%) | 1/77 (1.3%) |
| Pulmonary Bronchodysplasia | 0/4 (0%) | 1/65 (1.5%) | 0/8 (0%) | 1/77 (1.3%) |
| Neurological Findings | N (%) | IC (95%) |
|---|---|---|
| Head circumference | ||
| Normocephaly | 71 (92.2%) | 83.5–96.5 |
| Microcephaly | 4 (5.2%) | 1.9–13.3 |
| Macrocephaly | 2 (2.6%) | 0.6–10.1 |
| Neurologic examination with at least one abnormality | 25 (32.5%) | 22.8–43.9 |
| Hemiparesis * | 3 (3.9%) | 1.2–11.7 |
| Tetraparesis | 5 (6.5%) | 2.7–14.9 |
| Hypotonia | 1 (1.3%) | 0.2–9.0 |
| Spastic hypertonia | 7 (9.1%) | 4.3–18.1 |
| Osteotendinous hyperreflexia | 9 (11.7%) | 6.1–21.2 |
| Cranial nerves abnormalities | 7 (9.1%) | 4.3–18.1 |
| Neuropsychomotor development | 26 (33.8%) | 23.9–45.2 |
| Cognitive skills | 9 (11.7%) | 6.1–21.2 |
| Language skills | 23 (29.9%) | 20.5–41.2 |
| Motor skills | 14 (18.2%) | 10.9–28.7 |
| Psychosocial skills | 11 (14.3%) | 8.0–24.2 |
| Autism | 4 (5.2%) | 1.9–13.3 |
| Epilepsy | 6 (7.8%) | 3.5–16.5 |
| Dysphagia | 7 (9.1%) | 4.3–18.1 |
| Neurological Findings | Normocephaly (n = 71) | Microcephaly (n = 4) | Macrocephaly (n = 2) | p-Valor |
|---|---|---|---|---|
| Neurologic examination with at least one abnormality | 19 (26.7%) | 4 (100%) | 2 (100%) | 0.001 |
| Deficits in social interaction | 6 (8.4%) | 4 (100%) | 0 (0%) | 0.001 |
| Deficit of muscle strength | 4 (5.6%) | 4 (100%) | 0 (0%) | <0.001 |
| Muscle-tonus abnormalities | 4 (5.6%) | 4 (100%) | 0 (0%) | <0.001 |
| Osteotendinous Hyperreflexia | 5 (7.0%) | 4 (100%) | 0 (0%) | <0.001 |
| Cranial-nerves abnormalities | 3 (4.2%) | 4 (100%) | 0 (0%) | <0.001 |
| Epilepsy | 1 (1.4%) | 4 (100%) | 1 (50%) | <0.001 |
| Neurodevelopment delay | 21 (29.6%) | 4 (100%) | 1 (50%) | 0.006 |
| Cognitive skills | 5 (7.0%) | 4 (100%) | 0 (0%) | <0.001 |
| Language skills | 18 (25.3%) | 4 (100%) | 1 (50%) | 0.022 |
| Motor skills | 9 (12.7%) | 4 (100%) | 1 (50%) | <0.001 |
| Psychosocial skills | 7 (9.9%) | 4 (100%) | 0 (0%) | <0.001 |
| Dysmorphisms | 9 (12.7%) | 4 (100%) | 1 (50%) | <0.001 |
| Autism | 4 (5.6%) | 0 (0%) | 0 (0%) | 1.000 |
| Neuroimaging Features | Microcephaly (n = 4) | Normocephaly (n = 20) | Macrocephaly (n = 5) | n/Total (%) (n = 29) | IC (95%) |
|---|---|---|---|---|---|
| Abnormal Neuroimaging | 4/4 (100%) | 3/20 (15%) | 1/5 (20%) | 8/29 (27.6%) | 13.8–47.5 |
| Cerebral calcifications | 4/4 (100%) | 1/20 (5%) | 0/5 (0%) | 5/29 (17.2%) | 7.0–37.7 |
| Ventricular dilatation | 4/4 (100%) | 1/20 (5%) | 0/5 (0%) | 6/29 (20.7%) | 9.1–40.4 |
| Lissencephaly/ pachygyria | 4/4 (100%) | 1/20 (5%) | 0/5 (0%) | 5/29 (17.2%) | 7.0–37.7 |
| Cortico-subcortical atrophy | 4/4 (100%) | 2/20 (10%) | 0/5 (0%) | 6/29 (20.7%) | 9.1–40.4 |
| Megacisterna magna | 0/4 (0%) | 0/20 (0%) | 1/5 (20%) | 1/29 (3.4%) | 0.4–23.0 |
| Periventricular leukomalacia | 0/4 (0%) | 2/20 (10%) | 0/5 (0%) | 2/29 (6.9%) | 1.6–25.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abtibol-Bernardino, M.R.; Peixoto, L.d.F.A.d.A.; Castilho, M.d.C.; Bôtto-Menezes, C.H.A.; Benzecry, S.G.; Otani, R.H.; Rodrigues, G.R.I.; Chaves, B.C.S.; Oliveira, G.A.d.; Rodrigues, C.d.S.; et al. Would Zika virus Infection in Pregnancy Be a Sentence of Poor Neurological Prognosis for Exposed Children? Neurodevelopmental Outcomes in a Cohort from Brazilian Amazon. Viruses 2022, 14, 2659. https://doi.org/10.3390/v14122659
Abtibol-Bernardino MR, Peixoto LdFAdA, Castilho MdC, Bôtto-Menezes CHA, Benzecry SG, Otani RH, Rodrigues GRI, Chaves BCS, Oliveira GAd, Rodrigues CdS, et al. Would Zika virus Infection in Pregnancy Be a Sentence of Poor Neurological Prognosis for Exposed Children? Neurodevelopmental Outcomes in a Cohort from Brazilian Amazon. Viruses. 2022; 14(12):2659. https://doi.org/10.3390/v14122659
Chicago/Turabian StyleAbtibol-Bernardino, Marília Rosa, Lucíola de Fátima Albuquerque de Almeida Peixoto, Marcia da Costa Castilho, Camila Helena Aguiar Bôtto-Menezes, Silvana Gomes Benzecry, Rodrigo Haruo Otani, Gabriela Ribeiro Ivo Rodrigues, Beatriz Caroline Soares Chaves, Geruza Alfaia de Oliveira, Cristina de Souza Rodrigues, and et al. 2022. "Would Zika virus Infection in Pregnancy Be a Sentence of Poor Neurological Prognosis for Exposed Children? Neurodevelopmental Outcomes in a Cohort from Brazilian Amazon" Viruses 14, no. 12: 2659. https://doi.org/10.3390/v14122659
APA StyleAbtibol-Bernardino, M. R., Peixoto, L. d. F. A. d. A., Castilho, M. d. C., Bôtto-Menezes, C. H. A., Benzecry, S. G., Otani, R. H., Rodrigues, G. R. I., Chaves, B. C. S., Oliveira, G. A. d., Rodrigues, C. d. S., Martinez-Espinosa, F. E., & Alecrim, M. d. G. C. (2022). Would Zika virus Infection in Pregnancy Be a Sentence of Poor Neurological Prognosis for Exposed Children? Neurodevelopmental Outcomes in a Cohort from Brazilian Amazon. Viruses, 14(12), 2659. https://doi.org/10.3390/v14122659





