Bacteriophage Rescue Therapy of a Vancomycin-Resistant Enterococcus faecium Infection in a One-Year-Old Child following a Third Liver Transplantation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Phage Susceptibility Testing
2.2. Phage DNA Analysis and Lysogeny
2.3. Production of Phage Active Pharmaceutical Ingredients (APIs)
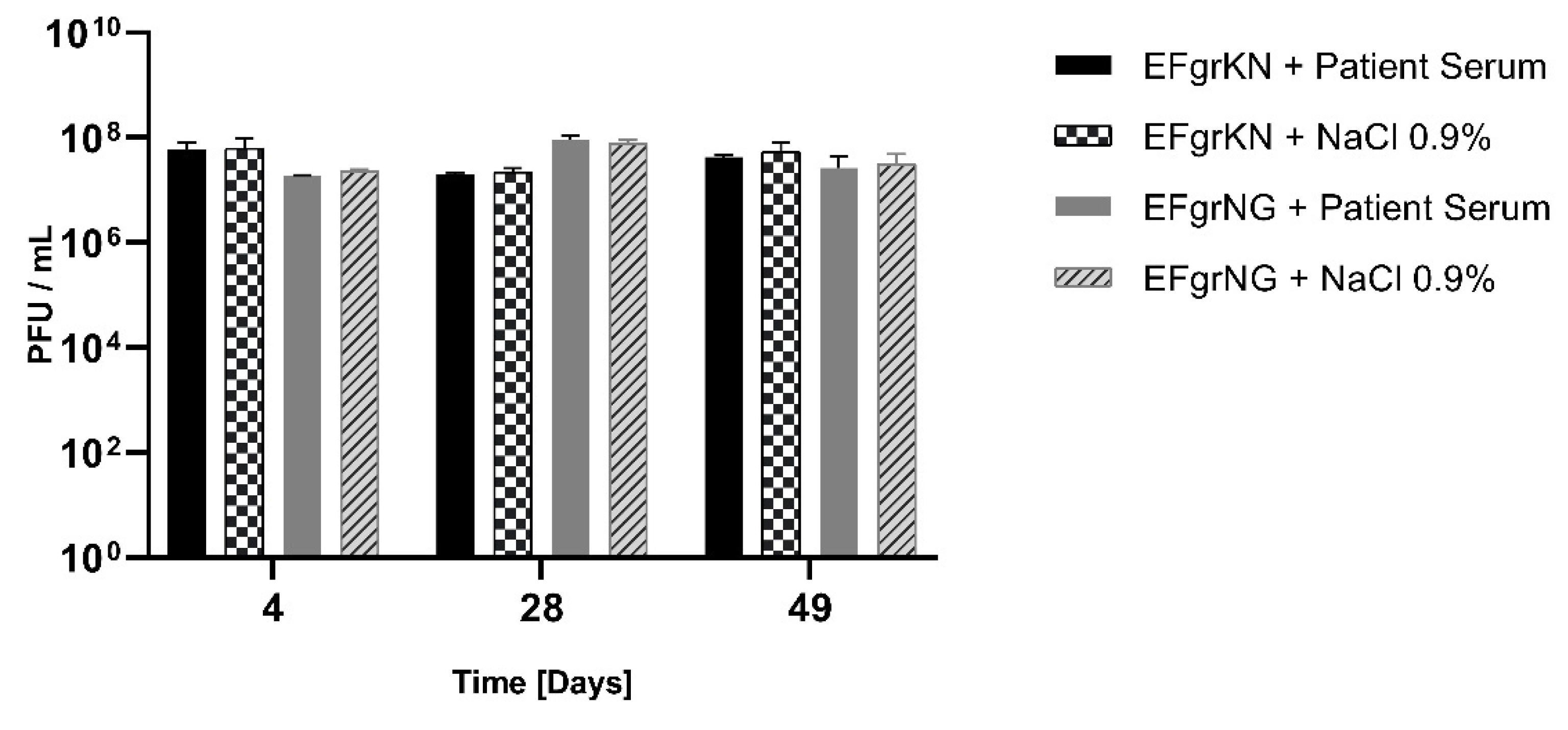
2.4. Stability of the Phages
2.5. Phage Neutralization Assay
2.6. Microbiological Methods and Whole Genome Sequencing of E. faecium Isolates
3. Results
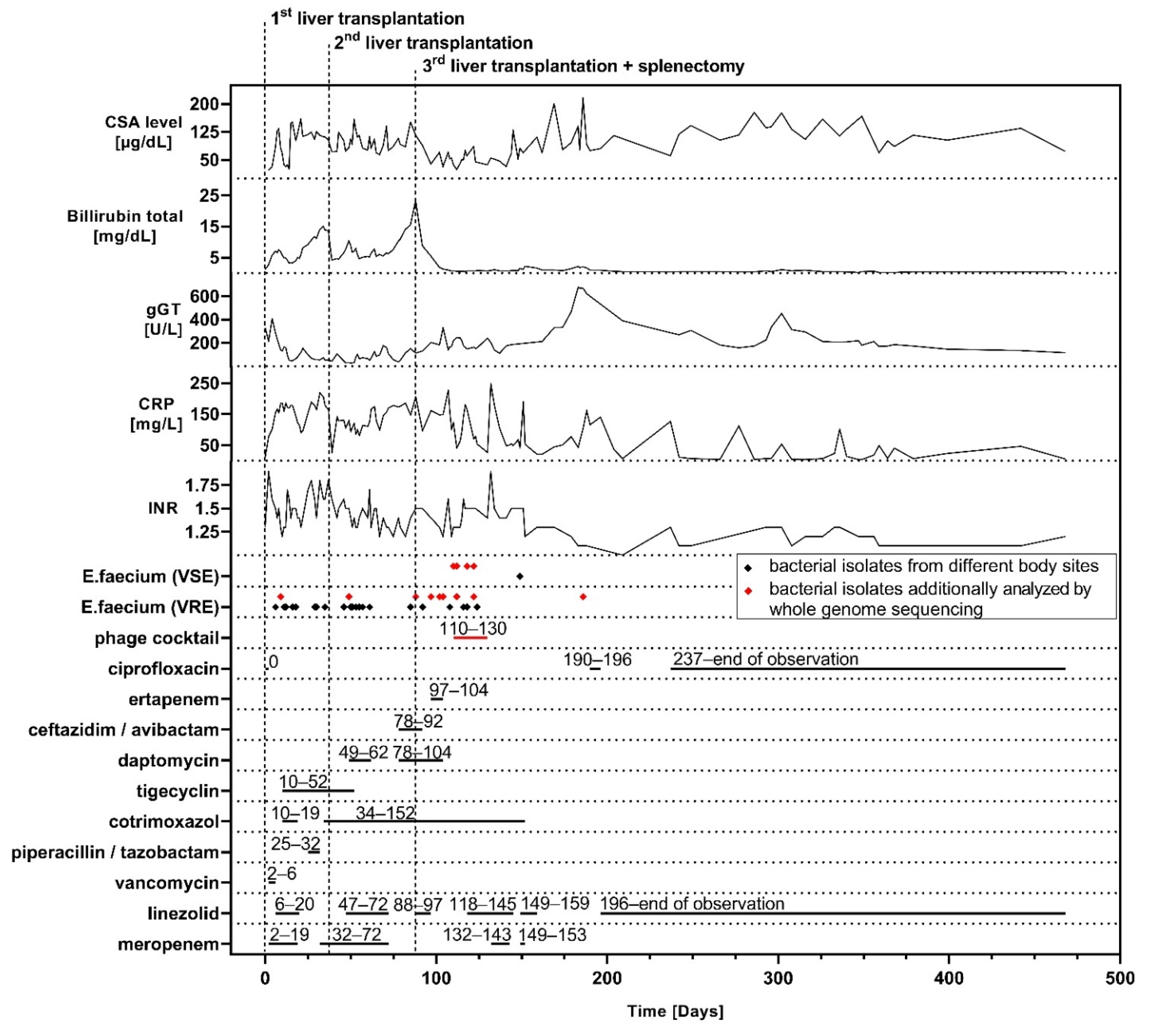
3.1. Case Presentation
3.2. Phage Procurement and Quality Standards
3.3. Humoral Immune Response
3.4. Genetic Characterization of E. faecium Isolates
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lakshminarayanan, B.; Davenport, M. Biliary atresia: A comprehensive review. J. Autoimmun. 2016, 73, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Cuenca, A.G.; Kim, H.B.; Vakili, K. Pediatric liver transplantation. Semin. Pediatr. Surg. 2017, 26, 217–223. [Google Scholar] [CrossRef]
- Baek, S.H.; Kang, J.M.; Ihn, K.; Han, S.J.; Koh, H.; Ahn, J.G. The Epidemiology and Etiology of Cholangitis After Kasai Portoenterostomy in Patients With Biliary Atresia. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Reid, G.E.; Grim, S.A.; Sankary, H.; Benedetti, E.; Oberholzer, J.; Clark, N.M. Early intra-abdominal infections associated with orthotopic liver transplantation. Transplantation 2009, 87, 1706–1711. [Google Scholar] [CrossRef]
- Viehman, J.A.; Clancy, C.J.; Clarke, L.; Shields, R.K.; Silveira, F.P.; Kwak, E.J.; Vergidis, P.; Hughes, C.; Humar, A.; Nguyen, M.H. Surgical Site Infections after Liver Transplantation: Emergence of Multidrug-Resistant Bacteria and Implications for Prophylaxis and Treatment Strategies. Transplantation 2016, 100, 2107–2114. [Google Scholar] [CrossRef] [PubMed]
- Yao, S.; Yagi, S.; Nagao, M.; Uozumi, R.; Iida, T.; Iwamura, S.; Miyachi, Y.; Shirai, H.; Kobayashi, A.; Okumura, S.; et al. Etiologies, risk factors, and outcomes of bacterial cholangitis after living donor liver transplantation. Eur. J. Clin. Microbiol. Infect. Dis. 2018, 37, 1973–1982. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, D.M.P.; Forde, B.M.; Kidd, T.J.; Harris, P.N.A.; Schembri, M.A.; Beatson, S.A.; Paterson, D.L.; Walker, M.J. Antimicrobial resistance in ESKAPE pathogens. Clin. Microbiol. Rev. 2020, 33, e00181-19. [Google Scholar] [CrossRef]
- Sulakvelidze, A.; Alavidze, Z.; Morris, G.J. Minireview Bacteriophage Therapy. Antimicrob. Agents Chemother. 2001, 45, 649–659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aslam, S.; Courtwright, A.M.; Koval, C.; Lehman, S.M.; Morales, S.; Furr, C.L.L.; Rosas, F.; Brownstein, M.J.; Fackler, J.R.; Sisson, B.M.; et al. Early clinical experience of bacteriophage therapy in 3 lung transplant recipients. Am. J. Transplant. 2019, 19, 2631–2639. [Google Scholar] [CrossRef]
- Aslam, S.; Lampley, E.; Wooten, D.; Karris, M.; Benson, C.; Strathdee, S.; Schooley, R.T. Lessons learned from the first 10 consecutive cases of intravenous bacteriophage therapy to treat multidrug-resistant bacterial infections at a single center in the United States. Open Forum Infect. Dis. 2020, 7, ofaa389. [Google Scholar] [CrossRef]
- Dedrick, R.M.; Guerrero-Bustamante, C.A.; Garlena, R.A.; Russell, D.A.; Ford, K.; Harris, K.; Gilmour, K.C.; Soothill, J.; Jacobs-Sera, D.; Schooley, R.T.; et al. Engineered bacteriophages for treatment of a patient with a disseminated drug-resistant Mycobacterium abscessus. Nat. Med. 2019, 25, 730–733. [Google Scholar] [CrossRef]
- Nir-Paz, R.; Gelman, D.; Khouri, A.; Sisson, B.M.; Fackler, J.; Alkalay-Oren, S.; Khalifa, L.; Rimon, A.; Yerushalmy, O.; Bader, R.; et al. Successful Treatment of Antibiotic-resistant, Poly-microbial Bone Infection with Bacteriophages and Antibiotics Combination. Clin. Infect. Dis. 2019, 69, 2015–2018. [Google Scholar] [CrossRef]
- Theuretzbacher, U.; Piddock, L.J.V. Non-traditional Antibacterial Therapeutic Options and Challenges. Cell Host Microbe 2019, 26, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Pirnay, J.P.; De Vos, D.; Verbeken, G. Clinical application of bacteriophages in Europe. Microbiol. Aust. 2019, 40, 8–15. [Google Scholar] [CrossRef] [Green Version]
- Merabishvili, M.; Pirnay, J.P.; Verbeken, G.; Chanishvili, N.; Tediashvili, M.; Lashkhi, N.; Glonti, T.; Krylov, V.; Mast, J.; Van Parys, L.; et al. Quality-controlled small-scale production of a well-defined bacteriophage cocktail for use in human clinical trials. PLoS ONE 2009, 4, e4944. [Google Scholar] [CrossRef] [PubMed]
- Yerushalmy, O.; Khalifa, L.; Gold, N.; Rakov, C.; Alkalay-Oren, S.; Adler, K.; Ben-Porat, S.; Kraitman, R.; Gronovich, N.; Ginat, K.S.; et al. The israeli phage bank (IPB). Antibiotics 2020, 9, 269. [Google Scholar] [CrossRef] [PubMed]
- Alkalay-Oren, S.; Gold, N.; Khalifa, L.; Yerushalmy, O.; Coppenhagen-Glazer, S.; Nir-Paz, R.; Hazan, R. Complete Genome Sequences of Two Enterococcus faecalis Bacteriophages, EFGrKN and EFGrNG, Targeted to Phage Therapy. Microbiol. Resour. Announc. 2021, 10, 20–22. [Google Scholar] [CrossRef]
- Gelman, D.; Yerushalmy, O.; Ben-Porat, S.; Rakov, C.; Alkalay-Oren, S.; Adler, K.; Khalifa, L.; Abdalrhman, M.; Coppenhagen-Glazer, S.; Aslam, S. Clinical Phage Microbiology: A suggested framework and recommendations for the in-vitro matching steps of phage therapy. Lancet Microbe bioRxiv 2021. [Google Scholar] [CrossRef]
- Yerushalmy, O.; Coppenhagen-Glazer, S.; Nir-Paz, R.; Tuomala, H.; Skurnik, M.; Kiljunen, S.; Hazan, R. Complete Genome Sequences of Two Klebsiella pneumoniae Phages Isolated as Part of an International Effort. Microbiol. Resour. Announc. 2019, 8, 1–3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pirnay, J.P.; Verbeken, G.; Ceyssens, P.J.; Huys, I.; de Vos, D.; Ameloot, C.; Fauconnier, A. The magistral phage. Viruses 2018, 10, 64. [Google Scholar] [CrossRef] [Green Version]
- Adams, M.H. Methods of study of bacterial viruses. In Bacteriophages; Interscience Publishers, Inc.: New York, NY, USA, 1959; pp. 443–523. [Google Scholar]
- Olearo, F.; Both, A.; Belmar Campos, C.; Hilgarth, H.; Klupp, E.M.; Hansen, J.L.; Maurer, F.P.; Christner, M.; Aepfelbacher, M.; Rohde, H. Emergence of linezolid-resistance in vancomycin-resistant Enterococcus faecium ST117 associated with increased linezolid-consumption. Int. J. Med. Microbiol. 2021, 311, 151477. [Google Scholar] [CrossRef] [PubMed]
- Tritt, A.; Eisen, J.A.; Facciotti, M.T.; Darling, A.E. An Integrated Pipeline for de Novo Assembly of Microbial Genomes. PLoS ONE 2012, 7, e42304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merabishvili, M. Production of bacteriophages using bacterial suspension cultures for phage-therapy. In Industrial Scale Suspension Culture of Living Cells; Meyer, H.P., Schmidhalter, D.R., Eds.; Wiley-VCH Verlag: Weinheim, Germany, 2014; pp. 537–543. [Google Scholar]
- Chacko, K.I.; Sullivan, M.J.; Beckford, C.; Altman, D.R.; Ciferri, B.; Pak, T.R.; Sebra, R.; Kasarskis, A.; Hamula, C.L.; Van Bakel, H. Genetic basis of emerging vancomycin, linezolid, and daptomycin heteroresistance in a case of persistent Enterococcus faecium bacteremia. Antimicrob. Agents Chemother. 2018, 62, e02007-17. [Google Scholar] [CrossRef] [Green Version]
- Belga, S.; Chiang, D.; Kabbani, D.; Abraldes, J.G.; Cervera, C. The direct and indirect effects of vancomycin-resistant enterococci colonization in liver transplant candidates and recipients. Expert Rev. Anti. Infect. Ther. 2019, 17, 363–373. [Google Scholar] [CrossRef] [PubMed]
- Gelman, D.; Beyth, S.; Lerer, V.; Adler, K.; Poradosu-Cohen, R.; Coppenhagen-Glazer, S.; Hazan, R. Combined bacteriophages and antibiotics as an efficient therapy against VRE Enterococcus faecalis in a mouse model. Res. Microbiol. 2018, 169, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Cheng, M.; Liang, J.; Zhang, Y.; Hu, L.; Gong, P.; Cai, R.; Zhang, L.; Zhang, H.; Ge, J.; Ji, Y.; et al. The bacteriophage EF-P29 efficiently protects against lethal vancomycin-resistant enterococcus faecalis and alleviates gut microbiota imbalance in a murine bacteremia model. Front. Microbiol. 2017, 8, 837. [Google Scholar] [CrossRef]
- Biswas, B.; Adhya, S.; Washart, P.; Paul, B.; Trostel, A.N.; Powell, B.; Carlton, R.; Merril, C.R. Erratum: Bacteriophage therapy rescues mice bacteremic from a clinical isolate of vancomycin-resistant Enterococcus faecium (Infection and Immunity (2002) 70:1 (204–210)). Infect. Immun. 2002, 70, 1664. [Google Scholar] [CrossRef] [Green Version]
- Rakhuba, D.V.; Kolomiets, E.I.; Szwajcer Dey, E.; Novik, G.I. Bacteriophage receptors, mechanisms of phage adsorption and penetration into host cell. Pol. J. Microbiol. 2010, 59, 145–155. [Google Scholar] [CrossRef]
- Huh, H.; Wong, S.; St. Jean, J.; Slavcev, R. Bacteriophage interactions with mammalian tissue: Therapeutic applications. Adv. Drug Deliv. Rev. 2019, 145, 4–17. [Google Scholar] [CrossRef]
| Isolate ID | Isolation Site | Isolation Relative to Phage Application (Days) | MIC 1 | MLST 2 |
|---|---|---|---|---|
| Vancomycin (mg/L) | Sequence Type | |||
| VREfm_1 | Blood culture | −101 | >256 | 1299 |
| VREfm_2 | Central venous | −61 | >256 | 1299 |
| catheter | ||||
| VREfm_3 | Abdominal swab | −21 | >256 | 1299 |
| VREfm_4 | Abdominal swab | −12 | >256 | 1299 |
| VREfm_5 | Abdominal drainage | −7 | >256 | 1299 |
| VREfm_6 | Upper respiratory tract swab | −7 | >256 | 1299 |
| VREfm_7 | Intraoperative swab | −5 | >256 | 1299 |
| E. faecium_1 | Abdominal drainage | 0 | 2 | 1299 |
| E. faecium _2 | Abdominal drainage | 2 | 2 | 1299 |
| E. faecium_3 | Abdominal drainage | 8 | 2 | 1299 |
| E. faecium _4 | Abdominal drainage | 10 | 2 | 1299 |
| VREfm_8 | Abdominal drainage | 10 | >256 | 1299 |
| VREfm_9 | Inguinal swab | 76 | >256 | 1299 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paul, K.; Merabishvili, M.; Hazan, R.; Christner, M.; Herden, U.; Gelman, D.; Khalifa, L.; Yerushalmy, O.; Coppenhagen-Glazer, S.; Harbauer, T.; et al. Bacteriophage Rescue Therapy of a Vancomycin-Resistant Enterococcus faecium Infection in a One-Year-Old Child following a Third Liver Transplantation. Viruses 2021, 13, 1785. https://doi.org/10.3390/v13091785
Paul K, Merabishvili M, Hazan R, Christner M, Herden U, Gelman D, Khalifa L, Yerushalmy O, Coppenhagen-Glazer S, Harbauer T, et al. Bacteriophage Rescue Therapy of a Vancomycin-Resistant Enterococcus faecium Infection in a One-Year-Old Child following a Third Liver Transplantation. Viruses. 2021; 13(9):1785. https://doi.org/10.3390/v13091785
Chicago/Turabian StylePaul, Kevin, Maya Merabishvili, Ronen Hazan, Martin Christner, Uta Herden, Daniel Gelman, Leron Khalifa, Ortal Yerushalmy, Shunit Coppenhagen-Glazer, Theresa Harbauer, and et al. 2021. "Bacteriophage Rescue Therapy of a Vancomycin-Resistant Enterococcus faecium Infection in a One-Year-Old Child following a Third Liver Transplantation" Viruses 13, no. 9: 1785. https://doi.org/10.3390/v13091785
APA StylePaul, K., Merabishvili, M., Hazan, R., Christner, M., Herden, U., Gelman, D., Khalifa, L., Yerushalmy, O., Coppenhagen-Glazer, S., Harbauer, T., Schulz-Jürgensen, S., Rohde, H., Fischer, L., Aslam, S., Rohde, C., Nir-Paz, R., Pirnay, J.-P., Singer, D., & Muntau, A. C. (2021). Bacteriophage Rescue Therapy of a Vancomycin-Resistant Enterococcus faecium Infection in a One-Year-Old Child following a Third Liver Transplantation. Viruses, 13(9), 1785. https://doi.org/10.3390/v13091785







