The Interplay between Bluetongue Virus Infections and Adaptive Immunity
Abstract
1. Introduction
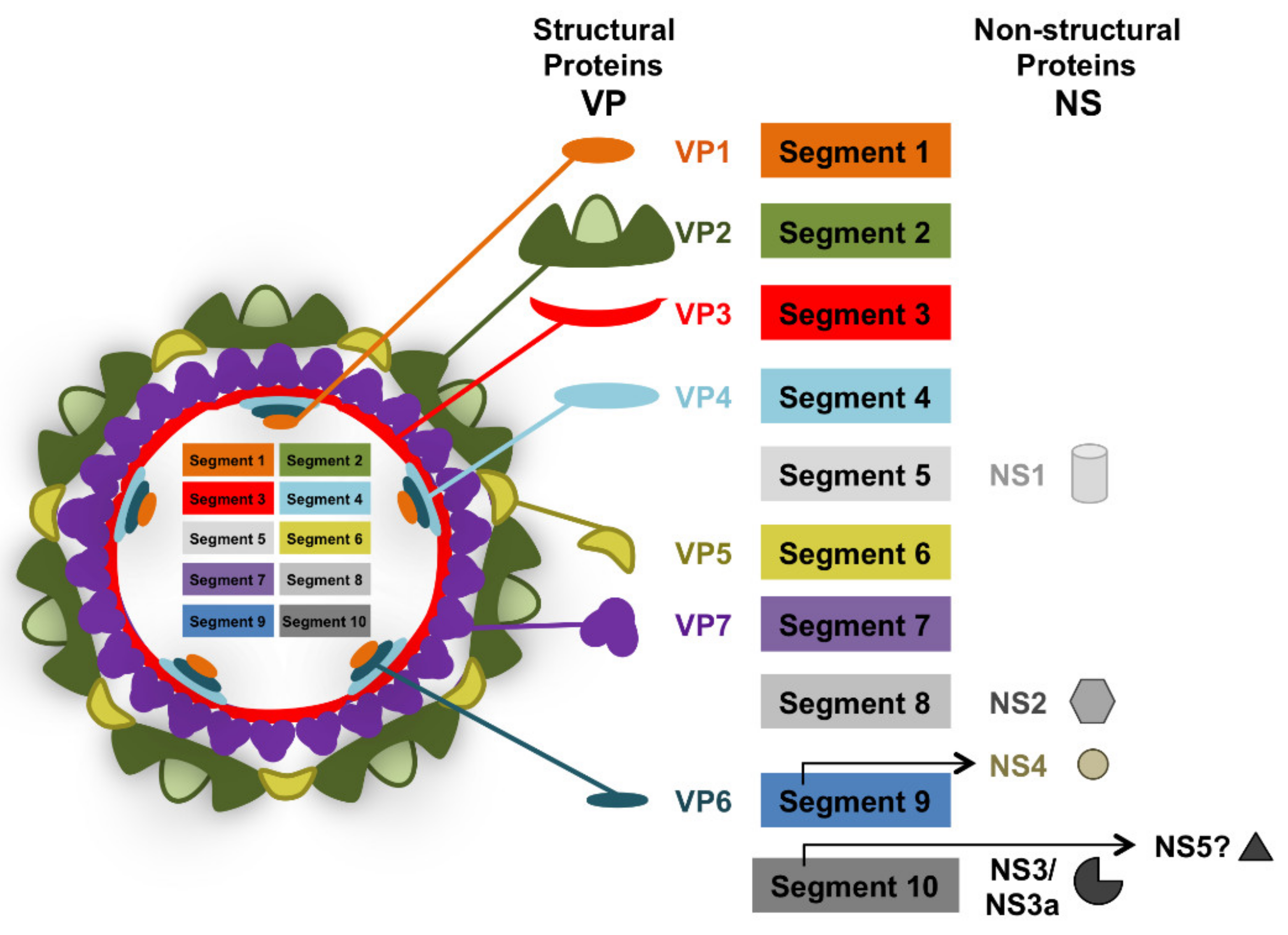
2. Bluetongue Virus: The Prototypical Orbivirus
3. The Control of BTV by Host Immunity
4. Experimental BTV Infections of Natural Hosts and Prolonged Viremia
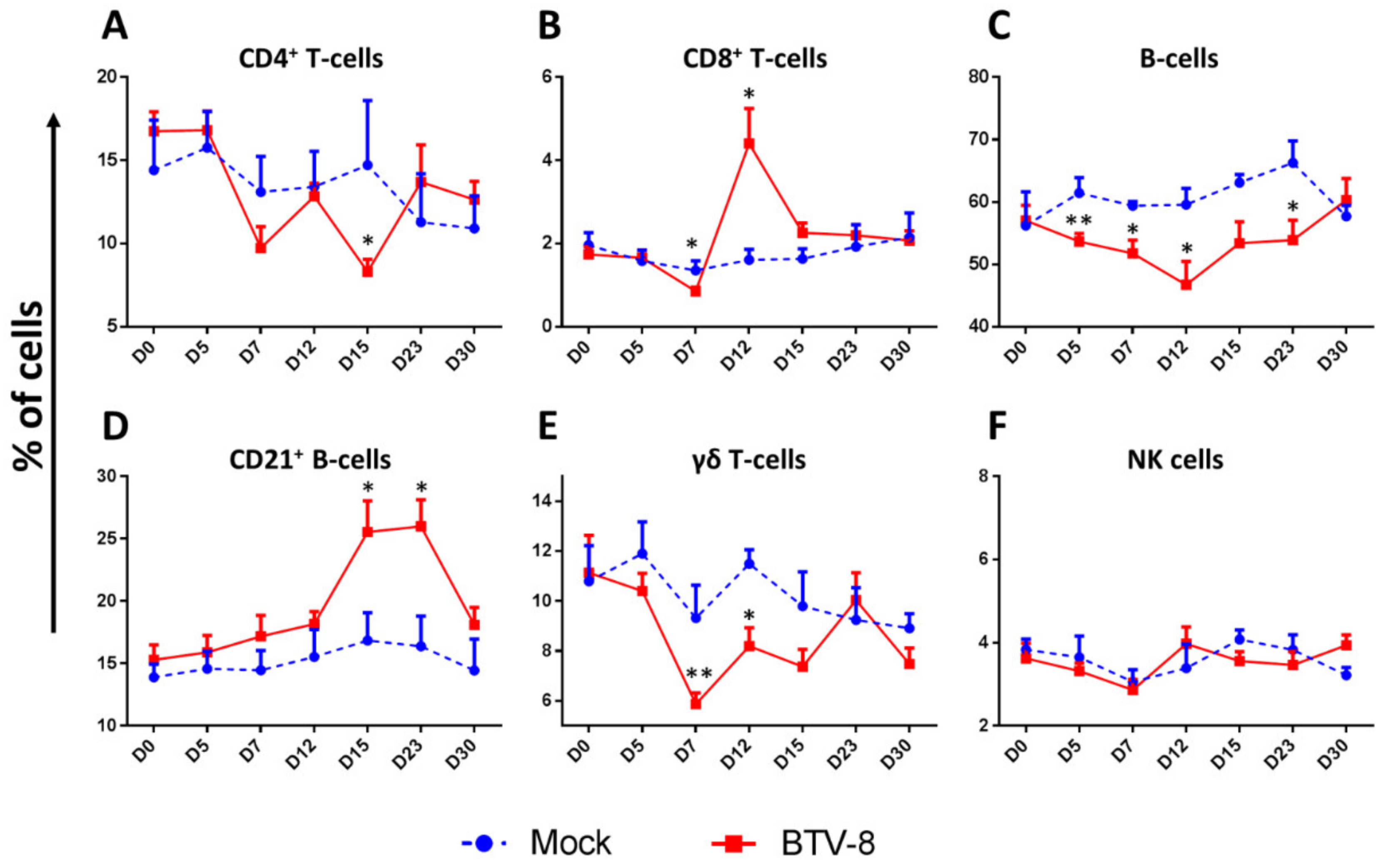
5. Effects of BTV Infection on Peripheral Lymphoid Cells Populations
5.1. BTV Infections Produce Leucopenia
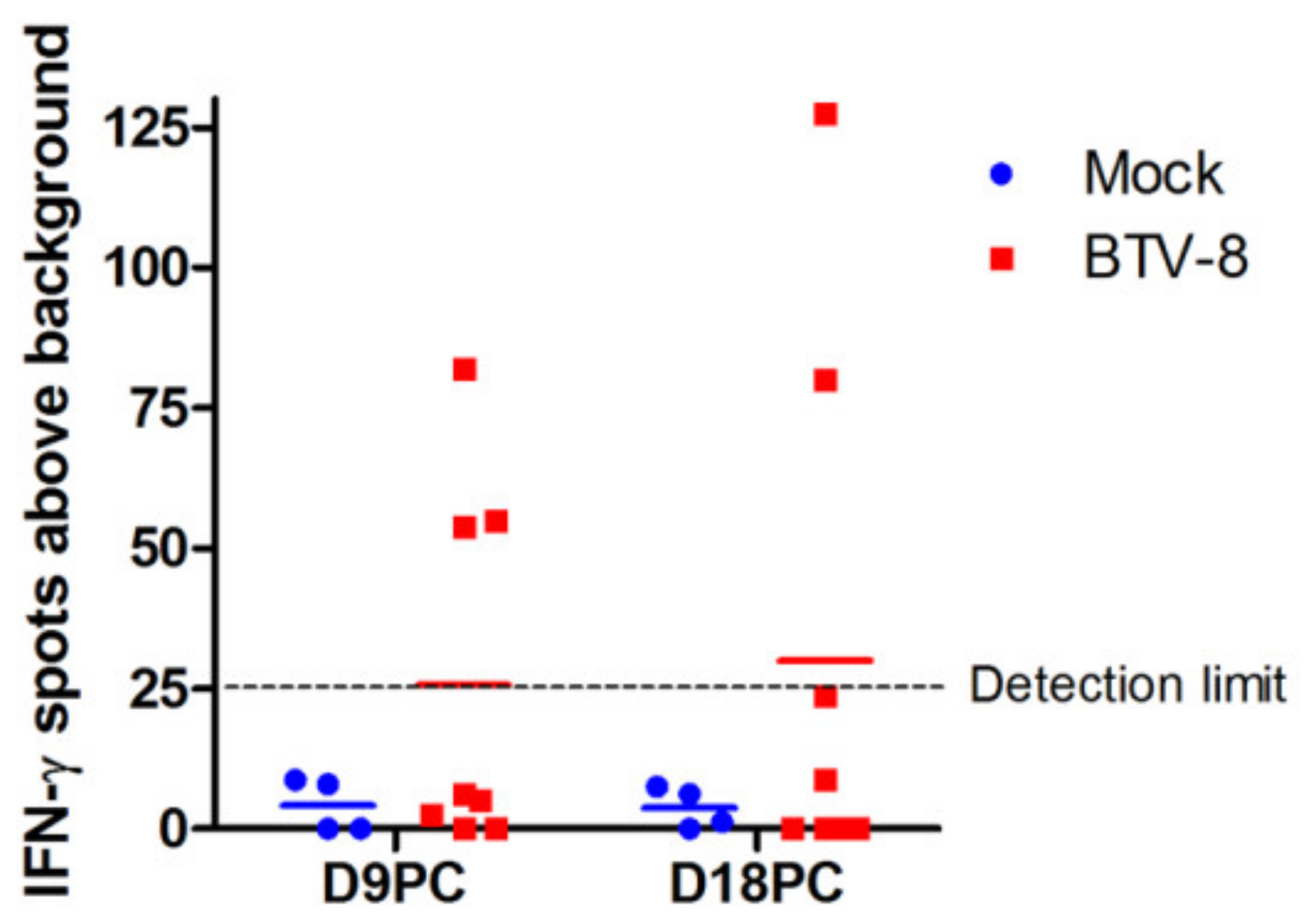
5.2. BTV Infections Trigger Cellular and Humoral Immunity
6. BTV Disruption of Adaptive Immunity
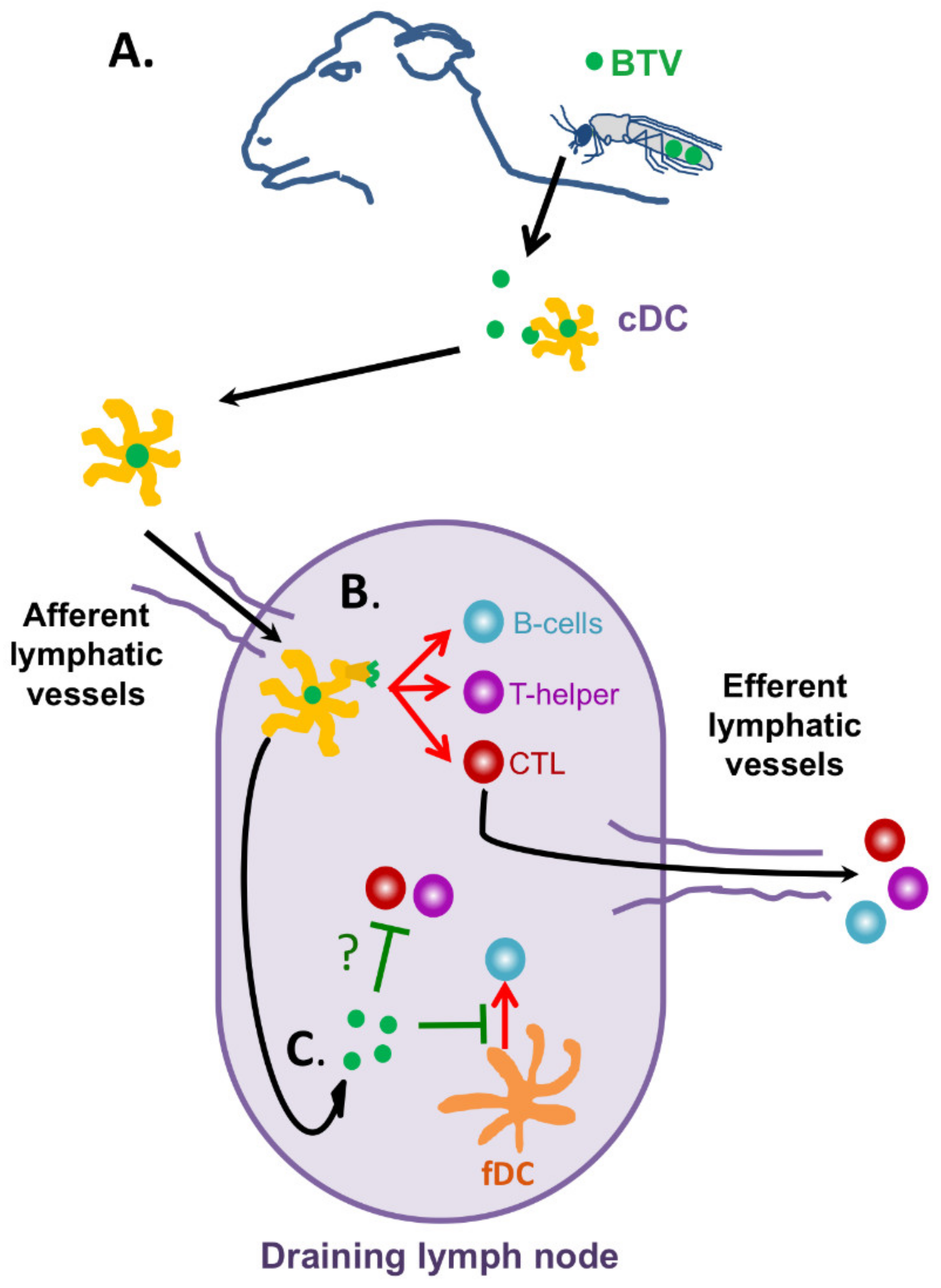
6.1. BTV Effects on Dendritic Cells
6.2. BTV Effects on Humoral Immunity
6.3. BTV Effects on Cellular Immunity
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Riedel, S. Edward Jenner and the history of smallpox and vaccination. Bayl. Univ. Med. Cent. Proc. 2005, 18, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.A. Louis Pasteur, the father of immunology? Front. Immunol. 2012, 3, 68. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Hakeem, M.S. Viruses Teaching Immunology: Role of LCMV Model and Human Viral Infections in Immunological Discoveries. Viruses 2019, 11, 106. [Google Scholar] [CrossRef] [PubMed]
- Oldstone, M.B. Biology and pathogenesis of lymphocytic choriomeningitis virus infection. Curr. Top. Microbiol. Immunol. 2002, 263, 83–117. [Google Scholar] [PubMed]
- Zinkernagel, R.M. Lymphocytic choriomeningitis virus and immunology. Curr. Top. Microbiol. Immunol. 2002, 263, 1–5. [Google Scholar]
- Zhou, X.; Ramachandran, S.; Mann, M.; Popkin, D.L. Role of lymphocytic choriomeningitis virus (LCMV) in understanding viral immunology: Past, present and future. Viruses 2012, 4, 2650–2669. [Google Scholar] [CrossRef] [PubMed]
- Oldstone, M.B.A. Anatomy of Viral Persistence. PLoS Pathog. 2009, 5, e1000523. [Google Scholar] [CrossRef] [PubMed]
- Zinkernagel, R.M.; Doherty, P.C. Restriction of in vitro T cell-mediated cytotoxicity in lymphocytic choriomeningitis within a syngeneic or semiallogeneic system. Nature 1974, 248, 701–702. [Google Scholar] [CrossRef]
- Doherty, P.C.; Zinkernagel, R.M. H-2 compatibility is required for T-cell-mediated lysis of target cells infected with lymphocytic choriomeningitis virus. J. Exp. Med. 1975, 141, 502–507. [Google Scholar] [CrossRef] [PubMed]
- Zinkernagel, R.M.; Doherty, P.C. H-2 compatability requirement for T-cell-mediated lysis of target cells infected with lymphocytic choriomeningitis virus. Different cytotoxic T-cell specificities are associated with structures coded for in H-2K or H-2D. J. Exp. Med. 1975, 141, 1427–1436. [Google Scholar] [CrossRef]
- Lau, L.L.; Jamieson, B.D.; Somasundaram, T.; Ahmed, R. Cytotoxic T-cell memory without antigen. Nature 1994, 369, 648–652. [Google Scholar] [CrossRef] [PubMed]
- Murali-Krishna, K.; Lau, L.L.; Sambhara, S.; Lemonnier, F.; Altman, J.; Ahmed, R. Persistence of memory CD8 T cells in MHC class I-deficient mice. Science 1999, 286, 1377–1381. [Google Scholar] [CrossRef]
- Sevilla, N.; Kunz, S.; Holz, A.; Lewicki, H.; Homann, D.; Yamada, H.; Campbell, K.P.; de La Torre, J.C.; Oldstone, M.B. Immunosuppression and resultant viral persistence by specific viral targeting of dendritic cells. J. Exp. Med. 2000, 192, 1249–1260. [Google Scholar] [CrossRef]
- Kunz, S.; Sevilla, N.; McGavern, D.B.; Campbell, K.P.; Oldstone, M.B. Molecular analysis of the interaction of LCMV with its cellular receptor [alpha]-dystroglycan. J. Cell Biol. 2001, 155, 301–310. [Google Scholar] [CrossRef] [PubMed]
- Moskophidis, D.; Lechner, F.; Pircher, H.; Zinkernagel, R.M. Virus persistence in acutely infected immunocompetent mice by exhaustion of antiviral cytotoxic effector T cells. Nature 1993, 362, 758–761. [Google Scholar] [CrossRef] [PubMed]
- Baylis, M.; O’Connell, L.; Mellor, P.S. Rates of bluetongue virus transmission between Culicoides sonorensis and sheep. Med. Vet. Entomol. 2008, 22, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Baylis, M.; Caminade, C.; Turner, J.; Jones, A.E. The role of climate change in a developing threat: The case of bluetongue in Europe. Rev. Sci. Tech. 2017, 36, 467–478. [Google Scholar] [CrossRef]
- Rushton, J.; Lyons, N. Economic impact of Bluetongue: A review of the effects on production. Vet. Ital 2015, 51, 401–406. [Google Scholar]
- Roy, P. Bluetongue virus structure and assembly. Curr. Opin. Virol. 2017, 24, 115–123. [Google Scholar] [CrossRef]
- Maan, S.; Maan, N.S.; Belaganahalli, M.N.; Potgieter, A.C.; Kumar, V.; Batra, K.; Wright, I.M.; Kirkland, P.D.; Mertens, P.P.C. Development and Evaluation of Real Time RT-PCR Assays for Detection and Typing of Bluetongue Virus. PLoS ONE 2016, 11, e0163014. [Google Scholar] [CrossRef]
- Zientara, S.; Sanchez-Vizcaino, J.M. Control of bluetongue in Europe. Vet. Microbiol. 2013, 165, 33–37. [Google Scholar] [CrossRef]
- Breard, E.; Belbis, G.; Viarouge, C.; Nomikou, K.; Haegeman, A.; De Clercq, K.; Hudelet, P.; Hamers, C.; Moreau, F.; Lilin, T.; et al. Evaluation of adaptive immune responses and heterologous protection induced by inactivated bluetongue virus vaccines. Vaccine 2015, 33, 512–518. [Google Scholar] [CrossRef]
- Shaw, A.E.; Ratinier, M.; Nunes, S.F.; Nomikou, K.; Caporale, M.; Golder, M.; Allan, K.; Hamers, C.; Hudelet, P.; Zientara, S.; et al. Reassortment between two serologically unrelated bluetongue virus strains is flexible and can involve any genome segment. J. Virol. 2013, 87, 543–557. [Google Scholar] [CrossRef]
- Rojas, J.M.; Rodríguez-Martín, D.; Martín, V.; Sevilla, N. Diagnosing bluetongue virus in domestic ruminants: Current perspectives. Vet. Med. 2019, 10, 17–27. [Google Scholar] [CrossRef]
- Boyce, M.; Celma, C.C.; Roy, P. Bluetongue virus non-structural protein 1 is a positive regulator of viral protein synthesis. Virol. J. 2012, 9, 178. [Google Scholar] [CrossRef] [PubMed]
- Kar, A.K.; Bhattacharya, B.; Roy, P. Bluetongue virus RNA binding protein NS2 is a modulator of viral replication and assembly. BMC Mol. Biol. 2007, 8, 4. [Google Scholar] [CrossRef] [PubMed]
- Wirblich, C.; Bhattacharya, B.; Roy, P. Nonstructural protein 3 of bluetongue virus assists virus release by recruiting ESCRT-I protein Tsg101. J. Virol. 2006, 80, 460–473. [Google Scholar] [CrossRef] [PubMed]
- Celma, C.C.; Roy, P. A viral nonstructural protein regulates bluetongue virus trafficking and release. J. Virol. 2009, 83, 6806–6816. [Google Scholar] [CrossRef]
- Labadie, T.; Jegouic, S.; Roy, P. Bluetongue Virus Nonstructural Protein 3 Orchestrates Virus Maturation and Drives Non-Lytic Egress via Two Polybasic Motifs. Viruses 2019, 11, 1107. [Google Scholar] [CrossRef] [PubMed]
- Chauveau, E.; Doceul, V.; Lara, E.; Breard, E.; Sailleau, C.; Vidalain, P.O.; Meurs, E.F.; Dabo, S.; Schwartz-Cornil, I.; Zientara, S.; et al. NS3 of bluetongue virus interferes with the induction of type I interferon. J. Virol. 2013, 87, 8241–8246. [Google Scholar] [CrossRef]
- Avia, M.; Rojas, J.M.; Miorin, L.; Pascual, E.; Van Rijn, P.A.; Martín, V.; García-Sastre, A.; Sevilla, N. Virus-induced autophagic degradation of STAT2 as a mechanism for interferon signaling blockade. EMBO Rep. 2019, 20, e48766. [Google Scholar] [CrossRef] [PubMed]
- Ratinier, M.; Shaw, A.E.; Barry, G.; Gu, Q.; Di Gialleonardo, L.; Janowicz, A.; Varela, M.; Randall, R.E.; Caporale, M.; Palmarini, M. Bluetongue Virus NS4 Protein Is an Interferon Antagonist and a Determinant of Virus Virulence. J. Virol. 2016, 90, 5427–5439. [Google Scholar] [CrossRef]
- Stewart, M.; Hardy, A.; Barry, G.; Pinto, R.M.; Caporale, M.; Melzi, E.; Hughes, J.; Taggart, A.; Janowicz, A.; Varela, M.; et al. Characterization of a second open reading frame in genome segment 10 of bluetongue virus. J. Gen. Virol. 2015, 96, 3280–3293. [Google Scholar] [CrossRef] [PubMed]
- Rojas, J.M.; Avia, M.; Martín, V.; Sevilla, N. Inhibition of the IFN Response by Bluetongue Virus: The Story So Far. Front. Microbiol. 2021, 12, 692069. [Google Scholar] [CrossRef]
- Pourcelot, M.; Amaral Moraes, R.; Fablet, A.; Bréard, E.; Sailleau, C.; Viarouge, C.; Postic, L.; Zientara, S.; Caignard, G.; Vitour, D. The VP3 Protein of Bluetongue Virus Associates with the MAVS Complex and Interferes with the RIG-I-Signaling Pathway. Viruses 2021, 13, 230. [Google Scholar] [CrossRef] [PubMed]
- MacLachlan, N.J.; Thompson, J. Bluetongue virus-induced interferon in cattle. Am. J. Vet. Res. 1985, 46, 1238–1241. [Google Scholar] [PubMed]
- Foster, N.M.; Luedke, A.J.; Parsonson, I.M.; Walton, T.E. Temporal relationships of viremia, interferon activity, and antibody responses of sheep infected with several bluetongue virus strains. Am. J. Vet. Res. 1991, 52, 192–196. [Google Scholar]
- Barratt-Boyes, S.M.; MacLachlan, N.J. Dynamics of viral spread in bluetongue virus infected calves. Vet. Microbiol. 1994, 40, 361–371. [Google Scholar] [CrossRef]
- Takamatsu, H.; Mellor, P.S.; Mertens, P.P.C.; Kirkham, P.A.; Burroughs, J.N.; Parkhouse, R.M.E. A possible overwintering mechanism for bluetongue virus in the absence of the insect vector. J. Gen. Virol. 2003, 84 Pt 1, 227–235. [Google Scholar] [CrossRef]
- Jeggo, M.H.; Wardley, R.C.; Taylor, W.P. Role of neutralising antibody in passive immunity to bluetongue infection. Res. Vet. Sci. 1984, 36, 81–86. [Google Scholar] [CrossRef]
- Jeggo, M.H.; Wardley, R.C.; Brownlie, J. A study of the role of cell-mediated immunity in bluetongue virus infection in sheep, using cellular adoptive transfer techniques. Immunology 1984, 52, 403–410. [Google Scholar]
- Zulu, G.B.; Venter, E.H. Evaluation of cross-protection of bluetongue virus serotype 4 with other serotypes in sheep. J. S. Afr. Vet. Assoc. 2014, 85, 1041. [Google Scholar] [CrossRef] [PubMed]
- Martin, V.; Pascual, E.; Avia, M.; Pena, L.; Valcarcel, F.; Sevilla, N. Protective Efficacy in Sheep of Adenovirus-Vectored Vaccines against Bluetongue Virus Is Associated with Specific T Cell Responses. PLoS ONE 2015, 10, e0143273. [Google Scholar] [CrossRef]
- Rojas, J.M.; Barba-Moreno, D.; Avia, M.; Sevilla, N.; Martín, V. Vaccination With Recombinant Adenoviruses Expressing the Bluetongue Virus Subunits VP7 and VP2 Provides Protection Against Heterologous Virus Challenge. Front. Vet. Sci. 2021, 8, 645561. [Google Scholar] [CrossRef] [PubMed]
- Rojas, J.M.; Pena, L.; Martin, V.; Sevilla, N. Ovine and murine T cell epitopes from the non-structural protein 1 (NS1) of bluetongue virus serotype 8 (BTV-8) are shared among viral serotypes. Vet. Res. 2014, 45, 30. [Google Scholar] [CrossRef]
- Marín-López, A.; Calvo-Pinilla, E.; Barriales, D.; Lorenzo, G.; Brun, A.; Anguita, J.; Ortego, J. CD8 T Cell Responses to an Immunodominant Epitope within the Nonstructural Protein NS1 Provide Wide Immunoprotection against Bluetongue Virus in IFNAR(-/-) Mice. J. Virol. 2018, 92, e00938-18. [Google Scholar] [CrossRef]
- Umeshappa, C.S.; Singh, K.P.; Pandey, A.B.; Singh, R.P.; Nanjundappa, R.H. Cell-mediated immune response and cross-protective efficacy of binary ethylenimine-inactivated bluetongue virus serotype-1 vaccine in sheep. Vaccine 2010, 28, 2522–2531. [Google Scholar] [CrossRef]
- Anderson, J.; Hägglund, S.; Bréard, E.; Riou, M.; Zohari, S.; Comtet, L.; Olofson, A.S.; Gélineau, R.; Martin, G.; Elvander, M.; et al. Strong protection induced by an experimental DIVA subunit vaccine against bluetongue virus serotype 8 in cattle. Vaccine 2014, 32, 6614–6621. [Google Scholar] [CrossRef] [PubMed]
- Jeggo, M.H.; Wardley, R.C.; Brownlie, J.; Corteyn, A.H. Serial inoculation of sheep with two bluetongue virus types. Res. Vet. Sci. 1986, 40, 386–392. [Google Scholar] [CrossRef]
- Maclachlan, N.J.; Drew, C.P.; Darpel, K.E.; Worwa, G. The pathology and pathogenesis of bluetongue. J. Comp. Pathol. 2009, 141, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Gerdes, G.H. A South African overview of the virus, vectors, surveillance and unique features of bluetongue. Vet. Ital. 2004, 40, 39–42. [Google Scholar]
- Stallknecht, D.E.; Howerth, E.W. Epidemiology of bluetongue and epizootic haemorrhagic disease in wildlife: Surveillance methods. Vet. Ital. 2004, 40, 203–207. [Google Scholar] [PubMed]
- García-Bocanegra, I.; Arenas-Montes, A.; Lorca-Oró, C.; Pujols, J.; González, M.Á.; Napp, S.; Gómez-Guillamón, F.; Zorrilla, I.; Miguel, E.S.; Arenas, A. Role of wild ruminants in the epidemiology of bluetongue virus serotypes 1, 4 and 8 in Spain. Vet. Res. 2011, 42, 88. [Google Scholar] [CrossRef] [PubMed]
- Lorca-Oró, C.; López-Olvera, J.R.; Ruiz-Fons, F.; Acevedo, P.; García-Bocanegra, I.; Oleaga, Á.; Gortázar, C.; Pujols, J. Long-Term Dynamics of Bluetongue Virus in Wild Ruminants: Relationship with Outbreaks in Livestock in Spain, 2006–2011. PLoS ONE 2014, 9, e100027. [Google Scholar] [CrossRef] [PubMed]
- Elbers, A.R.; Backx, A.; Meroc, E.; Gerbier, G.; Staubach, C.; Hendrickx, G.; van der Spek, A.; Mintiens, K. Field observations during the bluetongue serotype 8 epidemic in 2006. I. Detection of first outbreaks and clinical signs in sheep and cattle in Belgium, France and the Netherlands. Prev. Vet. Med. 2008, 87, 21–30. [Google Scholar] [CrossRef]
- Perrin, A.; Albina, E.; Bréard, E.; Sailleau, C.; Promé, S.; Grillet, C.; Kwiatek, O.; Russo, P.; Thiéry, R.; Zientara, S.; et al. Recombinant capripoxviruses expressing proteins of bluetongue virus: Evaluation of immune responses and protection in small ruminants. Vaccine 2007, 25, 6774–6783. [Google Scholar] [CrossRef]
- Caporale, M.; Di Gialleonorado, L.; Janowicz, A.; Wilkie, G.; Shaw, A.; Savini, G.; Van Rijn, P.A.; Mertens, P.; Di Ventura, M.; Palmarini, M. Virus and host factors affecting the clinical outcome of bluetongue virus infection. J. Virol. 2014, 88, 10399–10411. [Google Scholar] [CrossRef] [PubMed]
- Van Gennip, R.G.P.; van de Water, S.G.P.; Maris-Veldhuis, M.; van Rijn, P.A. Bluetongue viruses based on modified-live vaccine serotype 6 with exchanged outer shell proteins confer full protection in sheep against virulent BTV8. PLoS ONE 2012, 7, e44619. [Google Scholar]
- Huismans, H.; van der Walt, N.T.; Cloete, M.; Erasmus, B.J. Isolation of a capsid protein of bluetongue virus that induces a protective immune response in sheep. Virology 1987, 157, 172–179. [Google Scholar] [CrossRef]
- Sánchez-Cordón, P.J.; Pleguezuelos, F.J.; Pérez de Diego, A.C.; Gómez-Villamandos, J.C.; Sánchez-Vizcaíno, J.M.; Cerón, J.J.; Tecles, F.; Garfia, B.; Pedrera, M. Comparative study of clinical courses, gross lesions, acute phase response and coagulation disorders in sheep inoculated with bluetongue virus serotype 1 and 8. Vet. Microbiol. 2013, 166, 184–194. [Google Scholar] [CrossRef]
- Rojas, J.M.; Rodriguez-Calvo, T.; Pena, L.; Sevilla, N. T cell responses to bluetongue virus are directed against multiple and identical CD4+ and CD8+ T cell epitopes from the VP7 core protein in mouse and sheep. Vaccine 2011, 29, 6848–6857. [Google Scholar] [CrossRef]
- Toussaint, J.F.; Sailleau, C.; Breard, E.; Zientara, S.; De Clercq, K. Bluetongue virus detection by two real-time RT-qPCRs targeting two different genomic segments. J. Virol. Methods 2007, 140, 115–123. [Google Scholar] [CrossRef]
- Chaignat, V.; Worwa, G.; Scherrer, N.; Hilbe, M.; Ehrensperger, F.; Batten, C.; Cortyen, M.; Hofmann, M.; Thuer, B. Toggenburg Orbivirus, a new bluetongue virus: Initial detection, first observations in field and experimental infection of goats and sheep. Vet. Microbiol. 2009, 138, 11–19. [Google Scholar] [CrossRef]
- Maan, S.; Maan, N.S.; Nomikou, K.; Batten, C.; Antony, F.; Belaganahalli, M.N.; Samy, A.M.; Reda, A.A.; Al-Rashid, S.A.; El Batel, M.; et al. Novel bluetongue virus serotype from Kuwait. Emerg. Infect. Dis. 2011, 17, 886–889. [Google Scholar] [CrossRef] [PubMed]
- Zientara, S.; Sailleau, C.; Viarouge, C.; Höper, D.; Beer, M.; Jenckel, M.; Hoffmann, B.; Romey, A.; Bakkali-Kassimi, L.; Fablet, A.; et al. Novel bluetongue virus in goats, Corsica, France, 2014. Emerg. Infect. Dis. 2014, 20, 2123–2125. [Google Scholar] [CrossRef]
- World Organization for Animal Health (OIE). Terrestrial Manual. Chapter 3.1.3. Bluetongue (Infection with Bluetongue Virus). In Manual of Diagnostic Tests and Vaccines for Terrestrial Animals; International Office of Epizootics: Paris, France, 2018. [Google Scholar]
- Ries, C.; Domes, U.; Janowetz, B.; Böttcher, J.; Burkhardt, K.; Miller, T.; Beer, M.; Hoffmann, B. Isolation and Cultivation of a New Isolate of BTV-25 and Presumptive Evidence for a Potential Persistent Infection in Healthy Goats. Viruses 2020, 12, 983. [Google Scholar] [CrossRef] [PubMed]
- Lunt, R.A.; Melville, L.; Hunt, N.; Davis, S.; Rootes, C.L.; Newberry, K.M.; Pritchard, L.I.; Middleton, D.; Bingham, J.; Daniels, P.W.; et al. Cultured skin fibroblast cells derived from bluetongue virus-inoculated sheep and field-infected cattle are not a source of late and protracted recoverable virus. J. Gen. Virol. 2006, 87 Pt 12, 3661–3666. [Google Scholar] [CrossRef]
- Maclachlan, N.J.; Henderson, C.; Schwartz-Cornil, I.; Zientara, S. The immune response of ruminant livestock to bluetongue virus: From type I interferon to antibody. Virus Res. 2014, 182, 71–77. [Google Scholar] [CrossRef]
- Bonneau, K.R.; DeMaula, C.D.; Mullens, B.A.; MacLachlan, N.J. Duration of viraemia infectious to Culicoides sonorensis in bluetongue virus-infected cattle and sheep. Vet. Microbiol. 2002, 88, 115–125. [Google Scholar] [CrossRef]
- Wang, L.F.; Kattenbelt, J.A.; Gould, A.R.; Pritchard, L.I.; Crameri, G.S.; Eaton, B.T. Major core protein VP7 of Australian bluetongue virus serotype 15: Sequence and antigenicity divergence from other BTV serotypes. J. Gen. Virol. 1994, 75 Pt 9, 2421–2425. [Google Scholar] [CrossRef]
- Martinelle, L.; Dal Pozzo, F.; Sarradin, P.; Van Campe, W.; De Leeuw, I.; De Clercq, K.; Thys, C.; Thiry, E.; Saegerman, C. Experimental bluetongue virus superinfection in calves previously immunized with bluetongue virus serotype 8. Vet. Res. 2016, 47, 73. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rojas, J.M.; Rodriguez-Calvo, T.; Sevilla, N. Recall T cell responses to bluetongue virus produce a narrowing of the T cell repertoire. Vet. Res. 2017, 48, 38. [Google Scholar] [CrossRef] [PubMed]
- Ellis, J.A.; Luedke, A.J.; Davis, W.C.; Wechsler, S.J.; Mecham, J.O.; Pratt, D.L.; Elliott, J.D. T Lymphocyte Subset Alterations Following Bluetongue Virus Infection in Sheep and Cattle. Vet. Immunol. Immunopathol. 1990, 24, 49–67. [Google Scholar] [CrossRef]
- Mahrt, C.R.; Osburn, B.I. Experimental bluetongue virus infection of sheep; effect of previous vaccination: Clinical and immunologic studies. Am. J. Vet. Res. 1986, 47, 1191–1197. [Google Scholar]
- Umeshappa, C.S.; Singh, K.P.; Nanjundappa, R.H.; Pandey, A.B. Apoptosis and immuno-suppression in sheep infected with bluetongue virus serotype-23. Vet. Microbiol. 2010, 144, 310–318. [Google Scholar] [CrossRef]
- Parsonson, I.M. Pathology and pathogenesis of bluetongue infections. Curr. Top. Microbiol. Immunol. 1990, 162, 119–141. [Google Scholar]
- Barratt-Boyes, S.M.; Rossitto, P.V.; Taylor, B.C.; Ellis, J.A.; MacLachlan, N.J. Response of the regional lymph node to bluetongue virus infection in calves. Vet. Immunol. Immunopathol. 1995, 45, 73–84. [Google Scholar] [CrossRef]
- Hemati, B.; Contreras, V.; Urien, C.; Bonneau, M.; Takamatsu, H.H.; Mertens, P.P.; Bréard, E.; Sailleau, C.; Zientara, S.; Schwartz-Cornil, I. Bluetongue virus targets conventional dendritic cells in skin lymph. J. Virol. 2009, 83, 8789–8799. [Google Scholar] [CrossRef]
- Russell, H.; O’Toole, D.T.; Bardsley, K.; Davis, W.C.; Ellis, J.A. Comparative effects of bluetongue virus infection of ovine and bovine endothelial cells. Vet. Pathol. 1996, 33, 319–331. [Google Scholar] [CrossRef]
- Barratt-Boyes, S.M.; Rossitto, P.V.; Stott, J.L.; MacLachlan, N.J. Flow cytometric analysis of in vitro bluetongue virus infection of bovine blood mononuclear cells. J. Gen. Virol. 1992, 73 Pt 8, 1953–1960. [Google Scholar] [CrossRef]
- Ellis, J.A.; Coen, M.L.; MacLachlan, N.J.; Wilson, W.C.; Williams, E.S.; Leudke, A.J. Prevalence of bluetongue virus expression in leukocytes from experimentally infected ruminants. Am. J. Vet. Res. 1993, 54, 1452–1456. [Google Scholar]
- Howerth, E.W. Cytokine release and endothelial dysfunction: A perfect storm in orbivirus pathogenesis. Vet. Ital. 2015, 51, 275–281. [Google Scholar]
- Diniz Matos, A.C.; Alvarez Balaro, M.F.; Maldonado Coelho Guedes, M.I.; Costa, E.A.; Ca Mara Rosa, J.L.; Costa, A.T.; Branda, O.F.; Portela Lobato, Z.L. Epidemiology of a Bluetongue outbreak in a sheep flock in Brazil. Vet. Ital. 2016, 52, 325–331. [Google Scholar]
- Rojas, J.M.; Moreno, H.; Valcarcel, F.; Pena, L.; Sevilla, N.; Martin, V. Vaccination with recombinant adenoviruses expressing the peste des petits ruminants virus F or H proteins overcomes viral immunosuppression and induces protective immunity against PPRV challenge in sheep. PLoS ONE 2014, 9, e101226. [Google Scholar] [CrossRef]
- Kumar, N.; Maherchandani, S.; Kashyap, S.K.; Singh, S.V.; Sharma, S.; Chaubey, K.K.; Ly, H. Peste des petits ruminants virus infection of small ruminants: A comprehensive review. Viruses 2014, 6, 2287–2327. [Google Scholar] [CrossRef]
- Sanchez-Cordon, P.J.; Perez de Diego, A.C.; Gomez-Villamandos, J.C.; Sanchez-Vizcaino, J.M.; Pleguezuelos, F.J.; Garfia, B.; del Carmen, P.; Pedrera, M. Comparative analysis of cellular immune responses and cytokine levels in sheep experimentally infected with bluetongue virus serotype 1 and 8. Vet. Microbiol. 2015, 177, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Pérez de Diego, A.C.; Sánchez-Cordón, P.J.; de las Heras, A.I.; Sánchez-Vizcaíno, J.M. Characterization of the immune response induced by a commercially available inactivated bluetongue virus serotype 1 vaccine in sheep. Sci. World J. 2012, 2012, 147158. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, C.L.; Yirsaw, A.; Gillespie, A.; Le Page, L.; Zhang, F.; Damani-Yokota, P.; Telfer, J.C. γδ T cells in livestock: Responses to pathogens and vaccine potential. Transbound. Emerg. Dis. 2020, 67 (Suppl. 2), 119–128. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.W.; Lund, B.T.; McConnell, I.; Bujdoso, R. Antigen recognition and activation of ovine gamma delta T cells. Immunology 1994, 82, 229–237. [Google Scholar]
- Vesosky, B.; Turner, O.C.; Turner, J.; Orme, I.M. Gamma interferon production by bovine gamma delta T cells following stimulation with mycobacterial mycolylarabinogalactan peptidoglycan. Infect. Immun. 2004, 72, 4612–4618. [Google Scholar] [CrossRef]
- Endsley, J.J.; Quade, M.J.; Terhaar, B.; Roth, J.A. Bovine viral diarrhea virus type 1- and type 2-specific bovine T lymphocyte-subset responses following modified-live virus vaccination. Vet. Ther. 2002, 3, 364–372. [Google Scholar]
- Luján, L.; Begara, I.; Collie, D.D.; Watt, N.J. CD8+ lymphocytes in bronchoalveolar lavage and blood: In vivo indicators of lung pathology caused by maedi-visna virus. Vet. Immunol. Immunopathol. 1995, 49, 89–100. [Google Scholar] [CrossRef]
- Melzi, E.; Caporale, M.; Rocchi, M.; Martin, V.; Gamino, V.; di Provvido, A.; Marruchella, G.; Entrican, G.; Sevilla, N.; Palmarini, M. Follicular dendritic cell disruption as a novel mechanism of virus-induced immunosuppression. Proc. Natl. Acad. Sci. USA 2016, 113, E6238–E6247. [Google Scholar] [CrossRef]
- Sun, J.C.; Lanier, L.L. NK cell development, homeostasis and function: Parallels with CD8⁺ T cells. Nat. Rev. Immunol. 2011, 11, 645–657. [Google Scholar] [CrossRef] [PubMed]
- Roozendaal, R.; Carroll, M.C. Complement receptors CD21 and CD35 in humoral immunity. Immunol. Rev. 2007, 219, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Bitew, M.; Ravishankar, C.; Chakravarti, S.; Kumar Sharma, G.; Nandi, S. Comparative Evaluation of T-Cell Immune Response to BTV Infection in Sheep Vaccinated with Pentavalent BTV Vaccine When Compared to Un-Vaccinated Animals. Vet. Med. Int. 2019, 2019, 8762780. [Google Scholar] [CrossRef] [PubMed]
- Coetzee, P.; van Vuuren, M.; Venter, E.H.; Stokstad, M. A review of experimental infections with bluetongue virus in the mammalian host. Virus Res. 2014, 182, 21–34. [Google Scholar] [CrossRef]
- Eisenbarth, S.C. Dendritic cell subsets in T cell programming: Location dictates function. Nat. Rev. Immunol. 2019, 19, 89–103. [Google Scholar] [CrossRef] [PubMed]
- Kranich, J.; Krautler, N.J. How Follicular Dendritic Cells Shape the B-Cell Antigenome. Front. Immunol. 2016, 7, 225. [Google Scholar] [CrossRef]
- Heesters, B.A.; Myers, R.C.; Carroll, M.C. Follicular dendritic cells: Dynamic antigen libraries. Nat. Rev. Immunol. 2014, 14, 495–504. [Google Scholar] [CrossRef] [PubMed]
- Sevilla, N.; McGavern, D.B.; Teng, C.; Kunz, S.; Oldstone, M.B. Viral targeting of hematopoietic progenitors and inhibition of DC maturation as a dual strategy for immune subversion. J. Clin. Investig. 2004, 113, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Schneider-Schaulies, S.; Klagge, I.M.; ter Meulen, V. Dendritic cells and measles virus infection. Curr. Top. Microbiol. Immunol. 2003, 276, 77–101. [Google Scholar]
- Rodriguez-Calvo, T.; Rojas, J.M.; Martin, V.; Sevilla, N. Type I interferon limits the capacity of bluetongue virus to infect hematopoietic precursors and dendritic cells in vitro and in vivo. J. Virol. 2014, 88, 859–867. [Google Scholar] [CrossRef] [PubMed]
- Hilke, J.; Strobel, H.; Woelke, S.; Stoeter, M.; Voigt, K.; Moeller, B.; Bastian, M.; Ganter, M. Presence of Antibodies against Bluetongue Virus (BTV) in Sheep 5 to 7.5 Years after Vaccination with Inactivated BTV-8 Vaccines. Viruses 2019, 11, 533. [Google Scholar] [CrossRef]
- Ries, C.; Beer, M.; Hoffmann, B. BTV antibody longevity in cattle five to eight years post BTV-8 vaccination. Vaccine 2019, 37, 2656–2660. [Google Scholar] [CrossRef] [PubMed]
- Rojas, J.M.; Avia, M.; Martín, V.; Sevilla, N. IL-10: A Multifunctional Cytokine in Viral Infections. J. Immunol. Res. 2017, 2017, 6104054. [Google Scholar] [CrossRef]
- Schoenborn, J.R.; Wilson, C.B. Regulation of interferon-gamma during innate and adaptive immune responses. Adv. Immunol. 2007, 96, 41–101. [Google Scholar]
- Hu, X.; Ivashkiv, L.B. Cross-regulation of Signaling Pathways by Interferon-γ: Implications for Immune Responses and Autoimmune Diseases. Immunity 2009, 31, 539–550. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Martín, D.; Louloudes-Lázaro, A.; Avia, M.; Martín, V.; Rojas, J.M.; Sevilla, N. The Interplay between Bluetongue Virus Infections and Adaptive Immunity. Viruses 2021, 13, 1511. https://doi.org/10.3390/v13081511
Rodríguez-Martín D, Louloudes-Lázaro A, Avia M, Martín V, Rojas JM, Sevilla N. The Interplay between Bluetongue Virus Infections and Adaptive Immunity. Viruses. 2021; 13(8):1511. https://doi.org/10.3390/v13081511
Chicago/Turabian StyleRodríguez-Martín, Daniel, Andrés Louloudes-Lázaro, Miguel Avia, Verónica Martín, José M. Rojas, and Noemí Sevilla. 2021. "The Interplay between Bluetongue Virus Infections and Adaptive Immunity" Viruses 13, no. 8: 1511. https://doi.org/10.3390/v13081511
APA StyleRodríguez-Martín, D., Louloudes-Lázaro, A., Avia, M., Martín, V., Rojas, J. M., & Sevilla, N. (2021). The Interplay between Bluetongue Virus Infections and Adaptive Immunity. Viruses, 13(8), 1511. https://doi.org/10.3390/v13081511





