In Vivo Study of Aerosol, Droplets and Splatter Reduction in Dentistry
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Setup
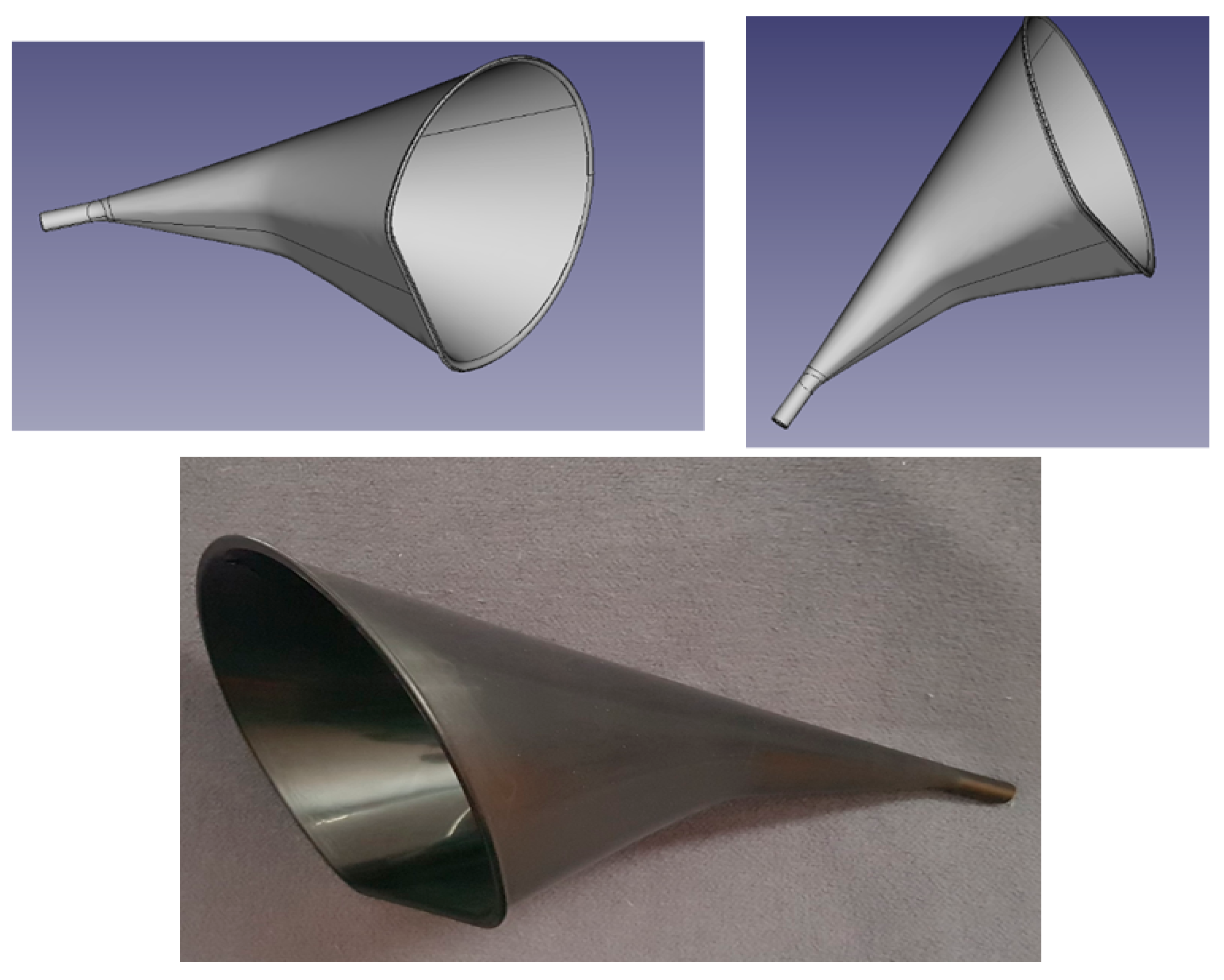
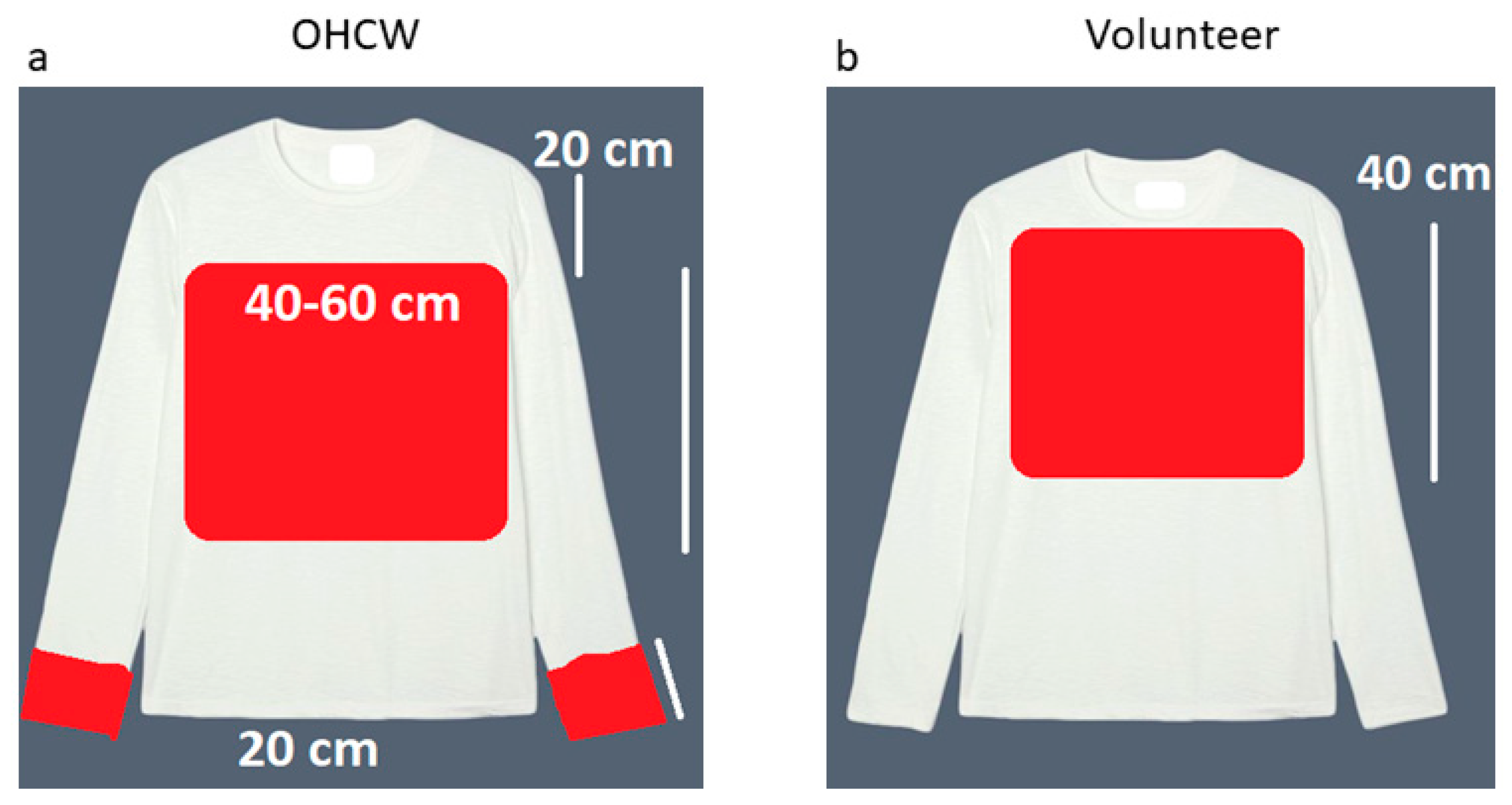
2.2. Equipment Used
2.3. Measurement Method
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Singla, D.; Singh, A.; Shiva Manjunath, R.; Bhattacharya, H.; Sarkar, A.; Chandra, N. Aerosol, a health hazard during ultrasonic scaling: A clinico-microbiological study. Indian J. Dent. Res. 2016, 27, 160–162. [Google Scholar] [CrossRef]
- Szymańska, J. Dental bioaerosol as an occupational hazard in a dentist’s workplace. Ann. Agric. Environ. Med. 2007, 14, 203–207. [Google Scholar]
- Kampf, G.; Todt, D.; Pfaender, S.; Steinmann, E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020, 104, 246–251. [Google Scholar] [CrossRef]
- Laheij, A.; Kistler, J.; Belibasakis, G.; Välimaa, H.; de Soet, J. Healthcare-associated viral and bacterial infections in dentistry. J. Oral. Microbiol. 2012, 4, 17659. [Google Scholar] [CrossRef]
- Matys, J.; Grzech-Leśniak, K. Dental Aerosol as a Hazard Risk for Dental Workers. Materials 2020, 13, 5109. [Google Scholar] [CrossRef]
- Zemouri, C.; Volgenant, C.; Buijs, M.; Crielaard, W.; Rosema, N.; Brandt, B.; Laheij, A.; De Soet, J. Dental aerosols: Microbial composition and spatial distribution. J. Oral. Microbiol. 2020, 12, 1762040. [Google Scholar] [CrossRef]
- Han, P.; Li, H.; Walsh, L.; Ivanovski, S. Splatters and Aerosols Contamination in Dental Aerosol Generating Procedures. Appl. Sci. 2020, 11, 1914. [Google Scholar] [CrossRef]
- Senpuku, H.; Fukumoto, M.; Uchiyama, T.; Taguchi, C.; Suzuki, I.; Arikawa, K. Effects of Extraoral Suction on Droplets and Aerosols for Infection Control Practices. Dent. J. 2021, 9, 80. [Google Scholar] [CrossRef]
- Veena, H.; Mahantesha, S.; Joseph, P.; Patil, S.; Patil, S. Dissemination of aerosol and splatter during ultrasonic scaling: A pilot study. J. Infect. Public Health 2015, 8, 260–265. [Google Scholar] [CrossRef]
- Prospero, E.; Savini, S.; Annino, I. Microbial Aerosol Contamination of Dental Healthcare Workers’ Faces and Other Surfaces in Dental Practice. Infect. Control Hosp. Epidemiol. 2003, 24, 139–141. [Google Scholar] [CrossRef]
- Convissar, R. Principles and Practice of Laser Dentistry, 2nd ed.; Mosby Elsevier: St. Louis, MO, USA, 2015; pp. 1–328. [Google Scholar]
- Wei, J.; Li, Y. Airborne spread of infectious agents in the indoor environment. Am. J. Infect. Control 2016, 44, S102–S108. [Google Scholar] [CrossRef]
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020, 12, 1–6. [Google Scholar] [CrossRef]
- Singh, T.; Mabe, O. Occupational exposure to endotoxin from contaminated dental unit waterlines. SADJ 2009, 64, 10–12. [Google Scholar]
- Liljeroos, L.; Huiskonen, J.; Ora, A.; Susi, P.; Butcher, S. Electron cryotomography of measles virus reveals how matrix protein coats the ribonucleocapsid within intact virions. Proc. Natl. Acad. Sci. USA 2011, 108, 18085–18090. [Google Scholar] [CrossRef]
- Rossman, J.; Lamb, R. Influenza virus assembly and budding. Virology 2011, 411, 229–236. [Google Scholar] [CrossRef]
- Makhsous, S.; Segovia, J.; He, J.; Chan, D.; Lee, L.; Novosselov, I.; Mamishev, A. Methodology for Addressing Infectious Aerosol Persistence in Real-Time Using Sensor Network. Sensors 2021, 21, 3928. [Google Scholar] [CrossRef]
- Sinjari, B.; Rexhepi, I.; Santilli, M.; D′Addazio, G.; Chiacchiaretta, P.; Di Carlo, P.; Caputi, S. The Impact of COVID-19 Related Lockdown on Dental Practice in Central Italy—Outcomes of A Survey. Int. J. Environ. Res. Public Health 2020, 17, 5780. [Google Scholar] [CrossRef]
- Chang, D.; Mo, G.; Yuan, X.; Tao, Y.; Peng, X.; Wang, F.; Xie, L.; Sharma, L.; Dela Cruz, C.; Qin, E. Time Kinetics of Viral Clearance and Resolution of Symptoms in Novel Coronavirus Infection. Am. J. Respir. Crit. Care Med. 2020, 201, 1150–1152. [Google Scholar] [CrossRef]
- Zou, L.; Ruan, F.; Huang, M.; Liang, L.; Huang, H.; Hong, Z.; Yu, J.; Kang, M.; Song, Y.; Xia, J.; et al. SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. N. Eng. J. Med. 2020, 382, 1177–1179. [Google Scholar] [CrossRef]
- Balanta-Melo, J.; Gutiérrez, A.; Sinisterra, G.; Díaz-Posso, M.; Gallego, D.; Villavicencio, J.; Contreras, A. Rubber Dam Isolation and High-Volume Suction Reduce Ultrafine Dental Aerosol Particles: An Experiment in a Simulated Patient. Appl. Sci. 2020, 10, 6345. [Google Scholar] [CrossRef]
- Zemouri, C.; De Soet, H.; Crielaard, W.; Laheij, A. A scoping review on bio-aerosols in healthcare and the dental environment. PLoS ONE 2017, 12, e0178007. [Google Scholar] [CrossRef]
- Alberta Federation of Labour. Available online: https://www.afl.org/as_albertans_return_to_work_who_is_at_the_highest_risk_of_exposure_to_the_novel_coronavirus (accessed on 5 September 2021).
- Cochran, M.; Miller, C.; Sheldrake, M. The efficacy of the rubber dam as a barrier to the spread of microorganisms during dental treatment. JADA 1989, 119, 141–144. [Google Scholar] [CrossRef]
- Al-Amad, S.; Awad, M.; Edher, F.; Shahramian, K.; Omran, T. The effect of rubber dam on atmospheric bacterial aerosols during restorative dentistry. J. Infect. Public Health 2017, 10, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Shahdad, S.; Patel, T.; Hindocha, A.; Cagney, N.; Mueller, J.-D.; Sedoudi, N.; Morgan, C.; Din, A. The efficacy of an extraoral scavenging device on reduction of splatter contamination during dental aerosol generating procedures: An exploratory study. Br. Dent. J. 2020, 11, 1–10. [Google Scholar] [CrossRef]
- Chavis, S.E.; Hines, S.E.; Dyalram, D.; Wilken, N.C.; Dalby, R.N. Can extraoral suction units minimize droplet spatter during a simulated dental procedure? JADA 2021, 152, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Holloman, J.; Mauriello, S.; Pimenta, L.; Arnold, R. Comparison of suction device with saliva ejector for aerosol and spatter reduction during ultrasonic scaling. JADA 2015, 146, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Rexhepi, I.; Mangifesta, R.; Santilli, M.; Guri, S.; Di Carlo, P.; D’Addazio, G.; Caputi, S.; Sinjari, B. Effects of Natural Ventilation and Saliva Standard Ejectors during the COVID-19 Pandemic: A Quantitative Analysis of Aerosol Produced during Dental Procedures. Int. J. Environ. Res. Public Health 2021, 18, 7472. [Google Scholar] [CrossRef]
- Horsophonphong, S.; Chestsuttayangkul, Y.; Surarit, R.; Lertsooksawat, W. Efficacy of extraoral suction devices in aerosol and splatter reduction during ultrasonic scaling: A laboratory investigation. J. Dent. Res. Dent. Clin. Dent. Prospects 2021, 15, 197–202. [Google Scholar]
- Leung, N.; Chu, D.; Shiu, E.; Chan, K.; McDevitt, J.; Hau, B.; Yen, H.; Li, Y.; Ip, D.; Peiris, J.; et al. Author Correction: Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020, 26, 981. [Google Scholar] [CrossRef]
- Di Carlo, P.; Falasca, K.; Ucciferri, C.; Sinjari, B.; Aruffo, E.; Antonucci, I.; Di Serafino, A.; Pompilio, A.; Damiani, V.; Mandatori, D.; et al. Normal breathing releases SARS-CoV-2 into the air. J. Med. Microbiol. 2021, 70, 001328. [Google Scholar] [CrossRef]

| Device Assessed | Volunteer Chest (cm2) | OHCW Chest below Shield (cm2) | OHCW Wrists (cm2) |
|---|---|---|---|
| LV only | 105 (±6.02) | 357 (±4) | 118 (±4) |
| HV + LV | 55 (±5) | 192 (±4.58) | 71 (±2.64) |
| DASD + LV | 25 (±2) * | 133 (±2) * | 35 (±1) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noordien, N.; Mulder-van Staden, S.; Mulder, R. In Vivo Study of Aerosol, Droplets and Splatter Reduction in Dentistry. Viruses 2021, 13, 1928. https://doi.org/10.3390/v13101928
Noordien N, Mulder-van Staden S, Mulder R. In Vivo Study of Aerosol, Droplets and Splatter Reduction in Dentistry. Viruses. 2021; 13(10):1928. https://doi.org/10.3390/v13101928
Chicago/Turabian StyleNoordien, Naeemah, Suné Mulder-van Staden, and Riaan Mulder. 2021. "In Vivo Study of Aerosol, Droplets and Splatter Reduction in Dentistry" Viruses 13, no. 10: 1928. https://doi.org/10.3390/v13101928
APA StyleNoordien, N., Mulder-van Staden, S., & Mulder, R. (2021). In Vivo Study of Aerosol, Droplets and Splatter Reduction in Dentistry. Viruses, 13(10), 1928. https://doi.org/10.3390/v13101928







