Use of Monocyte-Derived Macrophage Culture Increases Zika Virus Isolation Rate from Human Plasma
Abstract
:1. Introduction
2. Materials and Methods
2.1. Specimens
2.2. Infectivity Studies
2.2.1. In Vero, C6/36 and JEG-3 Cell Line Culture Systems
2.2.2. In Monocyte-Derived Macrophages (MDM) Primary Cell Culture System
2.3. ZIKV TaqMan RT-PCR
2.4. Quantification of ZIKV by FFA
3. Results
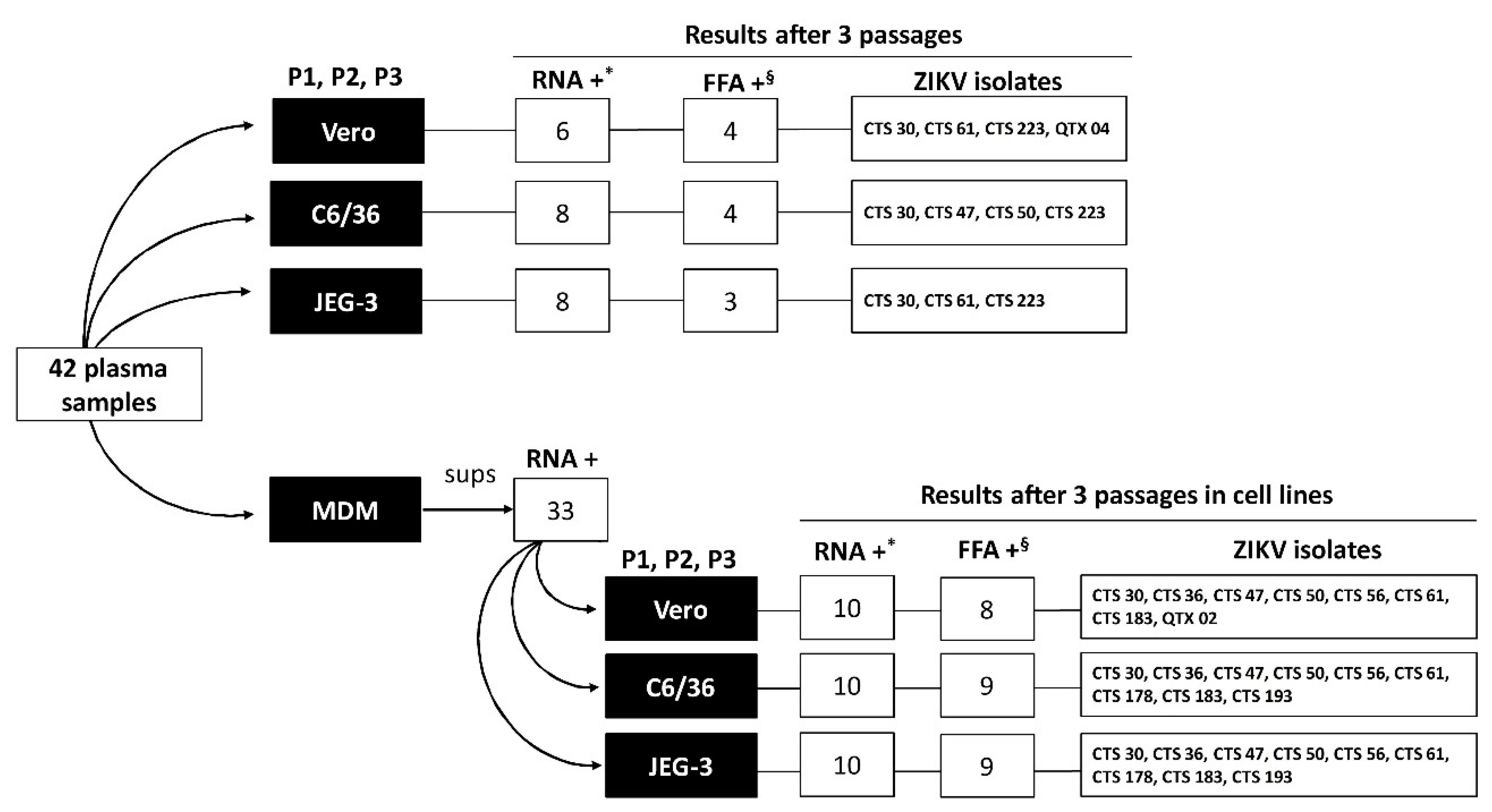
3.1. ZIKV Isolation Using Cell Lines: Vero, C6/36 and JEG-3
3.2. ZIKV Isolation Using MDM
3.3. Antibody Status Plays A Role in Viral Isolation
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Dick, G.W.; Kitchen, S.F.; Haddow, A.J. Zika virus. I. Isolations and serological specificity. Trans. R. Soc. Trop. Med. Hyg. 1952, 46, 509–520. [Google Scholar] [CrossRef]
- Duffy, M.R.; Chen, T.H.; Hancock, W.T.; Powers, A.M.; Kool, J.L.; Lanciotti, R.S.; Pretrick, M.; Marfel, M.; Holzbauer, S.; Dubray, C.; et al. Zika virus outbreak on Yap Island, Federated States of Micronesia. N. Engl. J. Med. 2009, 360, 2536–2543. [Google Scholar] [CrossRef] [PubMed]
- Lanciotti, R.S.; Kosoy, O.L.; Laven, J.J.; Velez, J.O.; Lambert, A.J.; Johnson, A.J.; Stanfield, S.M.; Duffy, M.R. Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg. Infect. Dis. 2008, 14, 1232–1239. [Google Scholar] [CrossRef] [PubMed]
- Cao-Lormeau, V.M.; Roche, C.; Teissier, A.; Robin, E.; Berry, A.L.; Mallet, H.P.; Sall, A.A.; Musso, D. Zika virus, French polynesia, South pacific, 2013. Emerg. Infect. Dis. 2014, 20, 1085–1086. [Google Scholar] [CrossRef] [PubMed]
- Faria, N.R.; Azevedo, R.; Kraemer, M.U.G.; Souza, R.; Cunha, M.S.; Hill, S.C.; Theze, J.; Bonsall, M.B.; Bowden, T.A.; Rissanen, I.; et al. Zika virus in the Americas: Early epidemiological and genetic findings. Science 2016, 352, 345–349. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Rapid Risk Assessment: Zika Virus Infection Outbreak, Brazil and the Pacific Region. Stockholm: ECDC. 25 May 2015. Available online: https://www.basg.gv.at/fileadmin/user_upload/ECDC_RRA-Zika_virus-South_America_Brazil_25-05-15.pdf (accessed on 7 July 2019).
- World Heath Organization (WHO). WHO Statement on the First Meeting of the International Health Regulations (2005) (IHR 2005) Emergency Committee on Zika Virus and Observed Increase in Neurological Disorders and Neonatal Malformations. Available online: https://www.who.int/en/news-room/detail/01-02-2016-who-statement-on-the-first-meeting-of-the-international-health-regulations-(2005)-(ihr-2005)-emergency-committee-on-zika-virus-and-observed-increase-in-neurological-disorders-and-neonatal-malformations (accessed on 13 November 2019).
- Brasil, P.; Pereira, J.P., Jr.; Moreira, M.E.; Ribeiro Nogueira, R.M.; Damasceno, L.; Wakimoto, M.; Rabello, R.S.; Valderramos, S.G.; Halai, U.A.; Salles, T.S.; et al. Zika Virus Infection in Pregnant Women in Rio de Janeiro. N. Engl. J. Med. 2016, 375, 2321–2334. [Google Scholar] [CrossRef]
- Calvet, G.; Aguiar, R.S.; Melo, A.S.O.; Sampaio, S.A.; de Filippis, I.; Fabri, A.; Araujo, E.S.M.; de Sequeira, P.C.; de Mendonca, M.C.L.; de Oliveira, L.; et al. Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: A case study. Lancet Infect. Dis. 2016, 16, 653–660. [Google Scholar] [CrossRef]
- D’Ortenzio, E.; Matheron, S.; Yazdanpanah, Y.; de Lamballerie, X.; Hubert, B.; Piorkowski, G.; Maquart, M.; Descamps, D.; Damond, F.; Leparc-Goffart, I. Evidence of Sexual Transmission of Zika Virus. N. Engl. J. Med. 2016, 374, 2195–2198. [Google Scholar] [CrossRef]
- Hastings, A.K.; Fikrig, E. Zika Virus and Sexual Transmission: A New Route of Transmission for Mosquito-borne Flaviviruses. Yale J. Biol. Med. 2017, 90, 325–330. [Google Scholar]
- Barjas-Castro, M.L.; Angerami, R.N.; Cunha, M.S.; Suzuki, A.; Nogueira, J.S.; Rocco, I.M.; Maeda, A.Y.; Vasami, F.G.; Katz, G.; Boin, I.F.; et al. Probable transfusion-transmitted Zika virus in Brazil. Transfusion 2016, 56, 1684–1688. [Google Scholar] [CrossRef]
- Motta, I.J.; Spencer, B.R.; Cordeiro da Silva, S.G.; Arruda, M.B.; Dobbin, J.A.; Gonzaga, Y.B.; Arcuri, I.P.; Tavares, R.C.; Atta, E.H.; Fernandes, R.F.; et al. Evidence for Transmission of Zika Virus by Platelet Transfusion. N. Engl. J. Med. 2016, 375, 1101–1103. [Google Scholar] [CrossRef] [PubMed]
- Bonaldo, M.C.; Ribeiro, I.P.; Lima, N.S.; Dos Santos, A.A.; Menezes, L.S.; da Cruz, S.O.; de Mello, I.S.; Furtado, N.D.; de Moura, E.E.; Damasceno, L.; et al. Isolation of Infective Zika Virus from Urine and Saliva of Patients in Brazil. PLoS Negl. Trop. Dis. 2016, 10, e0004816. [Google Scholar] [CrossRef] [PubMed]
- Musso, D.; Roche, C.; Robin, E.; Nhan, T.; Teissier, A.; Cao-Lormeau, V.M. Potential sexual transmission of Zika virus. Emerg. Infect. Dis. 2015, 21, 359–361. [Google Scholar] [CrossRef] [PubMed]
- Dupont-Rouzeyrol, M.; Biron, A.; O’Connor, O.; Huguon, E.; Descloux, E. Infectious Zika viral particles in breastmilk. Lancet 2016, 387, 1051. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention (CDC). Zika and Blood Transfusion. Available online: https://www.cdc.gov/zika/transmission/blood-transfusion.html (accessed on 9 October 2019).
- Landry, M.L.; St George, K. Laboratory Diagnosis of Zika Virus Infection. Arch. Pathol. Lab. Med. 2017, 141, 60–67. [Google Scholar] [CrossRef]
- Chan, J.F.; Yip, C.C.; Tsang, J.O.; Tee, K.M.; Cai, J.P.; Chik, K.K.; Zhu, Z.; Chan, C.C.; Choi, G.K.; Sridhar, S.; et al. Differential cell line susceptibility to the emerging Zika virus: Implications for disease pathogenesis, non-vector-borne human transmission and animal reservoirs. Emerg. Microbes Infect. 2016, 5, e93. [Google Scholar] [CrossRef]
- Himmelsbach, K.; Hildt, E. Identification of various cell culture models for the study of Zika virus. World J. Virol. 2018, 7, 10–20. [Google Scholar] [CrossRef]
- Nikolay, A.; Castilho, L.R.; Reichl, U.; Genzel, Y. Propagation of Brazilian Zika virus strains in static and suspension cultures using Vero and BHK cells. Vaccine 2018, 36, 3140–3145. [Google Scholar] [CrossRef]
- Moser, L.A.; Boylan, B.T.; Moreira, F.R.; Myers, L.J.; Svenson, E.L.; Fedorova, N.B.; Pickett, B.E.; Bernard, K.A. Growth and adaptation of Zika virus in mammalian and mosquito cells. PLoS Negl. Trop. Dis. 2018, 12, e0006880. [Google Scholar] [CrossRef]
- Foo, S.S.; Chen, W.; Chan, Y.; Bowman, J.W.; Chang, L.C.; Choi, Y.; Yoo, J.S.; Ge, J.; Cheng, G.; Bonnin, A.; et al. Asian Zika virus strains target CD14(+) blood monocytes and induce M2-skewed immunosuppression during pregnancy. Nat. Microbiol. 2017, 2, 1558–1570. [Google Scholar] [CrossRef]
- Michlmayr, D.; Andrade, P.; Gonzalez, K.; Balmaseda, A.; Harris, E. CD14(+)CD16(+) monocytes are the main target of Zika virus infection in peripheral blood mononuclear cells in a paediatric study in Nicaragua. Nat. Microbiol. 2017, 2, 1462–1470. [Google Scholar] [CrossRef] [PubMed]
- Lum, F.M.; Lee, D.; Chua, T.K.; Tan, J.J.L.; Lee, C.Y.P.; Liu, X.; Fang, Y.; Lee, B.; Yee, W.X.; Rickett, N.Y.; et al. Zika Virus Infection Preferentially Counterbalances Human Peripheral Monocyte and/or NK Cell Activity. mSphere 2018, 3. [Google Scholar] [CrossRef] [PubMed]
- Rios, M.; Zhang, M.J.; Grinev, A.; Srinivasan, K.; Daniel, S.; Wood, O.; Hewlett, I.K.; Dayton, A.I. Monocytes-macrophages are a potential target in human infection with West Nile virus through blood transfusion. Transfusion 2006, 46, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Fares-Gusmao, R.; Chancey, C.; Volkova, E.; Grinev, A.; Sippert, E.; Jiang, Z.; Rios, M. Production and characterization of Zika virus RNA reference reagents as a response to a public health emergency. Transfusion 2018, 58, 2171–2174. [Google Scholar] [CrossRef] [PubMed]
- Bol, S.M.; van Remmerden, Y.; Sietzema, J.G.; Kootstra, N.A.; Schuitemaker, H.; van’t Wout, A.B. Donor variation in in vitro HIV-1 susceptibility of monocyte-derived macrophages. Virology 2009, 390, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Jarman, R.G.; Nisalak, A.; Anderson, K.B.; Klungthong, C.; Thaisomboonsuk, B.; Kaneechit, W.; Kalayanarooj, S.; Gibbons, R.V. Factors influencing dengue virus isolation by C6/36 cell culture and mosquito inoculation of nested PCR-positive clinical samples. Am. J. Trop. Med. Hyg. 2011, 84, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Rios, M.; Daniel, S.; Dayton, A.I.; Wood, O.; Hewlett, I.K.; Epstein, J.S.; Caglioti, S.; Stramer, S.L. In vitro evaluation of the protective role of human antibodies to West Nile virus (WNV) produced during natural WNV infection. J. Infect. Dis. 2008, 198, 1300–1308. [Google Scholar] [CrossRef]
- Singh, R.K.; Dhama, K.; Karthik, K.; Tiwari, R.; Khandia, R.; Munjal, A.; Iqbal, H.M.N.; Malik, Y.S.; Bueno-Mari, R. Advances in Diagnosis, Surveillance, and Monitoring of Zika Virus: An Update. Front. Microbiol. 2017, 8, 2677. [Google Scholar] [CrossRef]
- Martinez Viedma, M.D.P.; Pickett, B.E. Characterizing the Different Effects of Zika Virus Infection in Placenta and Microglia Cells. Viruses 2018, 10, 649. [Google Scholar] [CrossRef]
- Shim, B.S.; Kwon, Y.C.; Ricciardi, M.J.; Stone, M.; Otsuka, Y.; Berri, F.; Kwal, J.M.; Magnani, D.M.; Jackson, C.B.; Richard, A.S.; et al. Zika Virus-Immune Plasmas from Symptomatic and Asymptomatic Individuals Enhance Zika Pathogenesis in Adult and Pregnant Mice. MBio 2019, 10, e00758-19. [Google Scholar] [CrossRef]
- Taylor, A.; Foo, S.S.; Bruzzone, R.; Dinh, L.V.; King, N.J.; Mahalingam, S. Fc receptors in antibody-dependent enhancement of viral infections. Immunol. Rev. 2015, 268, 340–364. [Google Scholar] [CrossRef] [PubMed]
- Crill, W.D.; Roehrig, J.T. Monoclonal antibodies that bind to domain III of dengue virus E glycoprotein are the most efficient blockers of virus adsorption to Vero cells. J. Virol. 2001, 75, 7769–7773. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Antibody Test Result | Copies/mL * | FFU/mL † | ||||||
|---|---|---|---|---|---|---|---|---|
| Isolate | IgM | IgG | Vero | C6/36 | JEG-3 | Vero | C6/36 | JEG-3 |
| CTS 30 | ̶ | ̶ | 1.71 × 104 | 1.67 × 109 | 1.09 × 106 | 1.00 × 101 | 1.00 × 107 | 6.00 × 102 |
| CTS 36 | ̶ | ̶ | 0 | 0 | 1.21 × 102 | |||
| CTS 47 | ̶ | ̶ | 2.96 × 102 | 1.30 × 109 | 0 | 3.00 × 106 | ||
| CTS 50 | ̶ | ̶ | 0 | 1.74 × 109 | 1.55 × 102 | 9.00 × 106 | ||
| CTS 56 | + | + | 0 | 2.20 × 102 | 4.19 × 101 | |||
| CTS 61 | ̶ | ̶ | 9.58 × 108 | 7.43 × 101 | 6.09 × 105 | 4.00 × 106 | 3.00 × 102 | |
| CTS 178 | ̶ | + | 0 | 2.03 × 102 | 0 | |||
| CTS 183 | ̶ | ̶ | 7.34 × 101 | 0 | 0 | |||
| CTS 193 | + | ̶ | 0 | 4.44 × 101 | 1.05 × 102 | |||
| CTS 223 | ̶ | ̶ | 3.44 × 108 | 1.89 × 109 | 8.72 × 108 | 9.50 × 105 | 1.70 × 106 | 3.00 × 105 |
| QTX 04 | ̶ | ̶ | 2.12 × 109 | 0 | 4.81 × 101 | 7.50 × 106 | ||
| Sample ID | Antibody Test Result | MDM Positive Cultures * | Average of ZIKV (copies/mL) in MDM Cultures † | FFA in Cell Lines Supernatant from P3 after Inoculated with MDM Supernatants | Average of Infectious Particle Concentration (FFU/mL) in P3 Supernatants § | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| IgM | IgG | Vero | C6/36 | JEG-3 | Vero | C6/36 | JEG-3 | |||
| CTS 30 | ̶ | ̶ | 3/4 | 6.71 × 107 | Pos (1/3) | Pos (2/3) | Pos (2/3) | 5.00 × 102 | 8.75 × 106 | 2.10 × 106 |
| CTS 36 | ̶ | ̶ | 4/7 | 5.35 × 106 | Pos (1/4) | Pos (1/4) | Pos (1/4) | 4.50 × 105 | 3.50 × 106 | 2.10 × 105 |
| CTS 47 | ̶ | ̶ | 3/4 | 6.85 × 107 | Pos (2/3) | Pos (3/3) | Pos (3/3) | 4.65 × 105 | 1.37 × 107 | 2.67 × 106 |
| CTS 50 | ̶ | ̶ | 3/4 | 7.65 × 107 | Pos (2/3) | Pos (2/3) | Pos (2/3) | 1.43 × 106 | 2.28 × 107 | 2.00 × 106 |
| CTS 61 | ̶ | ̶ | 4/4 | 2.59 × 105 | Pos (2/4) | Pos (3/4) | Pos (3/4) | 5.50 × 104 | 2.08 × 107 | 1.43 × 107 |
| CTS 183 | ̶ | ̶ | 2/4 | 3.10 × 107 | Pos (2/2) | Pos (2/2) | Pos (2/2) | 1.76 × 105 | 9.25 × 106 | 2.05 × 106 |
| QTX 02 | ̶ | ̶ | 1/7 | 4.31 × 104 | Pos (1/1) | Neg | Neg | 1.00 × 107 | ||
| QTX 04 | ̶ | ̶ | 1/1 | 7.77 × 103 | Neg | Neg | Neg | |||
| CTS 223 | ̶ | ̶ | 6/6 | 1.80 × 104 | Neg | Neg | Neg | |||
| CTS 56 | + | + | 1/4 | 1.95 × 108 | Pos (1/1) | Pos (1/1) | Pos (1/1) | 1.40 × 107 | 6.00 × 107 | 1.50 × 106 |
| CTS 178 | ̶ | + | 4/4 | 2.67 × 107 | Neg | Pos (2/4) | Pos (1/4) | 4.00 × 107 | 1.10 × 105 | |
| CTS 193 | + | ̶ | 1/4 | 1.31 × 107 | Neg | Pos (1/4) | Pos (1/4) | 1.00 × 107 | 6.50 × 105 | |
| ZIKV Antibody Status | Total | Isolation Rate Direct in Cell Lines | MDM * | Isolation Rate in Cell Lines after MDM Rescue | ||||
|---|---|---|---|---|---|---|---|---|
| Vero | C6/36 | JEG-3 | Vero | C6/36 | JEG-3 | |||
| Pos (%) | Pos (%) | Pos (%) | Pos (%) | Pos (%) | Pos (%) | Pos (%) | ||
| IgM‒, IgG‒ | 18 | 4 (22.22) | 4 (22.22) | 3 (16.66) | 17 (94.44) | 7 (41.18) | 6 (35.29) | 6 (35.29) |
| IgM+, IgG+ | 11 | 0 (0) | 0 (0) | 0 (0) | 7 (63.63) | 1 (14.29) | 1 (14.29) | 1 (14.29) |
| IgM‒, IgG+ | 5 | 0 (0) | 0 (0) | 0 (0) | 3 (60) | 0 (0) | 1 (33.33) | 1 (33.33) |
| IgM+, IgG‒ or IgM+, IgG Eq | 3 | 0 (0) | 0 (0) | 0 (0) | 2 (100) | 0 (0) | 1 (50) | 1 (50) |
| IgM‒, IgG Eq or IgM Eq, IgG‒ | 5 | 0 (0) | 0 (0) | 0 (0) | 4 (66.66) | 0 (0) | 0 (0) | 0 (0) |
| 42 | 4 (9.52) | 4 (9.52) | 3 (7.14) | 33 (78.57) | 8 (24.24) | 9 (27.27) | 9 (27.27) | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sippert, E.; Rocha, B.C.; Assis, F.L.; Ok, S.; Rios, M. Use of Monocyte-Derived Macrophage Culture Increases Zika Virus Isolation Rate from Human Plasma. Viruses 2019, 11, 1058. https://doi.org/10.3390/v11111058
Sippert E, Rocha BC, Assis FL, Ok S, Rios M. Use of Monocyte-Derived Macrophage Culture Increases Zika Virus Isolation Rate from Human Plasma. Viruses. 2019; 11(11):1058. https://doi.org/10.3390/v11111058
Chicago/Turabian StyleSippert, Emilia, Bruno C. Rocha, Felipe L. Assis, Suzan Ok, and Maria Rios. 2019. "Use of Monocyte-Derived Macrophage Culture Increases Zika Virus Isolation Rate from Human Plasma" Viruses 11, no. 11: 1058. https://doi.org/10.3390/v11111058
APA StyleSippert, E., Rocha, B. C., Assis, F. L., Ok, S., & Rios, M. (2019). Use of Monocyte-Derived Macrophage Culture Increases Zika Virus Isolation Rate from Human Plasma. Viruses, 11(11), 1058. https://doi.org/10.3390/v11111058





