Appendix A. Scripts to Be Read to Patients
Script for Health Care Clinicians to Offer the Opportunity to Participate in the Research Project
“Based on recommendations from the Centers for Disease Control and other organizations, I am prescribing that you exercise an average of 30 min daily over five days each week (total of 2 h and 30 min per week). Your exercise can include any activity you enjoy, including walking, hiking, biking, yoga, stretching, games, swimming and strength conditioning. I am giving you this prescription because exercise can provide important physical and mental health benefits.
I am partnering with university and scientists to study the effects of regular exercise in people with chronic conditions. The study will take place between July and October 2024. Participation is completely voluntary and participants will receive a $100 Visa or comparable gift card for participating. Would you like the learn more about this study and what you would need to do as a participant? [PLEASE CONTINUE ONLY IF PATIENT WOULD LIKE TO LEARN MORE] Would it be okay if I shared your telephone number and/or email address with the research team so they can reach out to you?”
Participant Recruitment Script
(To Be Read to Potential Participants by Senior Student Researcher)
“Based on recommendations from the Centers for Disease Control, and other organizations, your health care provider has prescribed that you exercise an average of 30 min daily over five days each week (total of 2 h and 30 min per week). Your provider is giving you this prescription because exercise can provide important physical and mental health benefits.
Your provider is partnering with university and scientists to study the effects of regular exercise in people with chronic conditions. The study will take place between July and October 2024. Participation is voluntary. If you choose to participate in this study, you will be asked to keep a daily log of your exercise activities, which we will provide to you. The log form will either by online or on paper, depending on your preference. It will include information on where you exercised, your sleep habits, your heart rate immediately after exercising, and how you feel physically and mentally. Completing the log form is expected to take about 5 min per day. If you keep your log on paper, once per week for eight weeks, university researchers will call and ask you to report the data from your log form. Each week, they will anonymously record these data on a password-protected data sheet.
You will also be asked to complete short questionnaires at the beginning of the study, after eight weeks, and after six months. These questionnaires will focus on your exercise activities, time spent in nature, and your personal characteristics.
Approximately 84 people will participate in this study. university and will seek to publish the study’s results to increase knowledge about the effects of exercise. No personally identifying information will appear in any publications.
To offset the participation costs and as a small token of appreciation for your time, you will receive cash or a gift card of $100. Once you receive this gift, it is yours to keep, and even if you decide to leave the study, it does not need to be returned.
Would you be willing to participate in this study? If yes, I will send you a document that answers questions about use of your information, privacy and who to contact during the study. I will then follow up to ask if you have any questions. I will also ask if you voluntarily consent to participate in the study.”
Script For Participants Who Have Given Informed Consent and Are Randomized into the Treatment Group (To Be Read to Participants by Senior Student Researcher)
“Thank you for agreeing to participate in this study conducted by university and scientists. As a reminder, the focus of the study is to understand the effects of regular exercise in people with chronic health conditions. The study will take place between July and October 2024.”
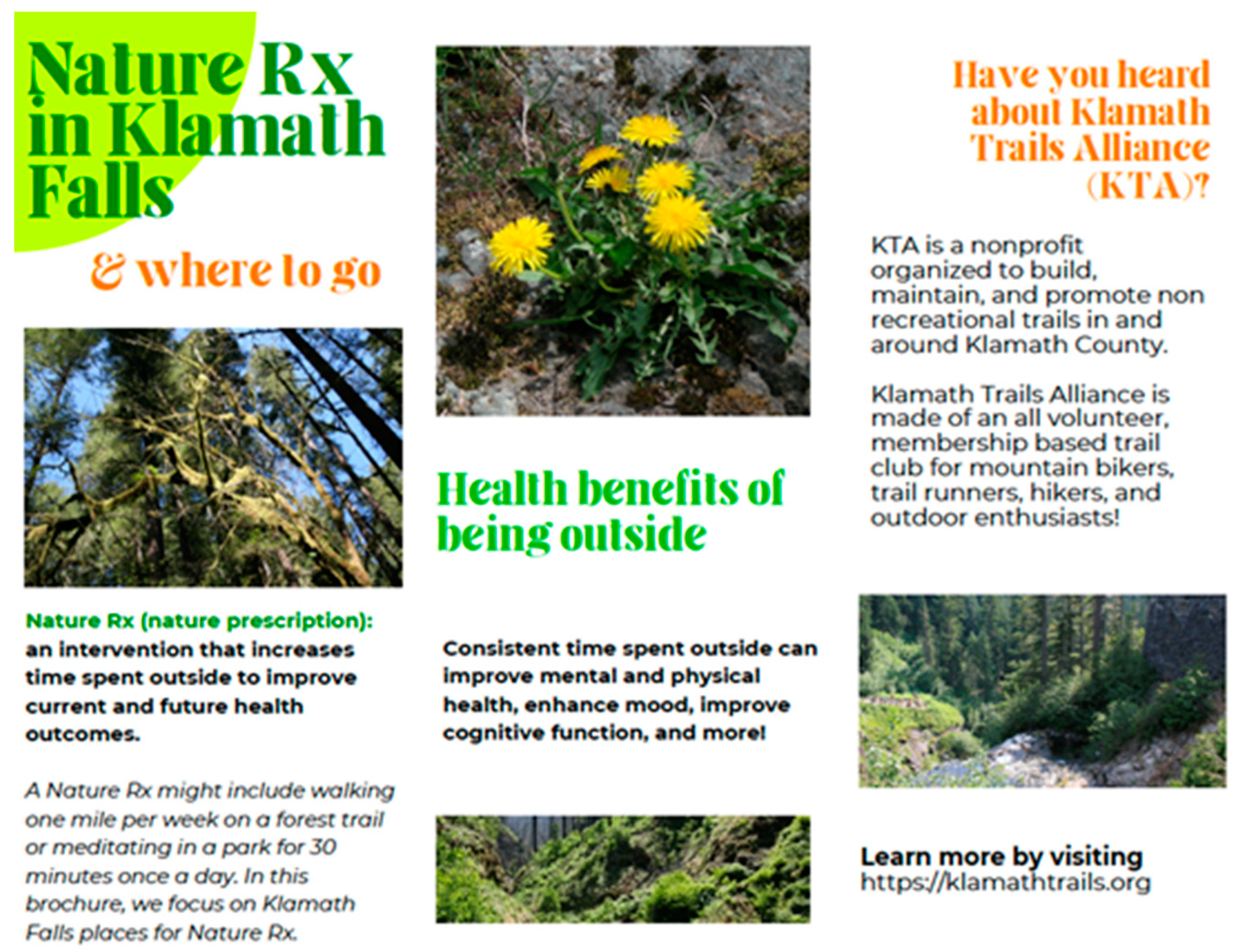
“Your exercise can consist of any activity you enjoy doing, including walking, hiking, biking, yoga, stretching, games, swimming, and strength conditioning. Your health care provider is prescribing that you conduct exercise as much as possible, in natural areas within approximately 15 min of your home for an average of 30 min daily over five days each week (total of 2 h and 30 min per week). Your provider is giving you this prescription to exercise to the extent possible in natural areas because exercising in nature–or spending any time in nature – may provide important physical and mental health benefits above-and-beyond any benefits from exercise.
These natural areas should be green and have significant plant coverage Your provider is making this recommendation, because exposure to green natural areas can especially offer health benefits. Ideally, there should be trees in your places of exercise that cover at least 50% of the sky. When you look up, at least some of the time, tree canopy should cover half the sky. Please think of this recommendation as a prescription about where you might like to do your exercise. Do you have any questions so far?
I will be sending you information about natural areas where you may want to exercise. I can send this information by email or post. Which would be better for you? [Note to research assistant: please take note of the participant’s preferred delivery method and send the information by that method.] I will also be connecting you with a university undergraduate student who will be working with you throughout the study [Note to research assistant: If you will be working with this participant yourself, please let them know] and who will send you daily log forms each week and the first of three surveys. These can be made available via an online Google Form or as a document. If you would like these as documents, the student or I will telephone you weekly at a mutually agreeable time to get your responses. Which method would you prefer? [Note to research assistant: If using Google Forms, please request the email address to send the link. If by paper, please ask if the participant would like the form emailed or sent by post. Please ask the patient for the relevant addresses]. I will also send your $100 gift card [Note to research assistant: Please discuss whether the participant would like a physical or electronic Visa gift card]. Do you have any questions?”
Script For Participants Who Have Given Informed Consent and Are Randomized into the Control Group (To Be Read to Participants by Senior Student Researcher)
“Thank you for agreeing to participate in this study conducted by university and scientists. As a reminder, the focus of the study is to understand the effects of regular exercise in people with chronic health conditions. The study will take place between July and October 2024.”
“Your exercise can consist of any activity you enjoy doing, including walking, hiking, biking, yoga, stretching, games, swimming, and strength conditioning. Your health care provider is prescribing that you exercise indoors or outside for an average of 30 min daily over five days each week (total of 2 h and 30 min per week). Your provider is giving you this prescription because exercise can provide important physical and mental health benefits. Do you have any questions so far?
I will be connecting you with a university undergraduate student who will be working with you throughout the study and [Note to graduate research assistant: If you will be working with this participant yourself, please let them know] who will be sending you the daily log form and the first of three surveys. These can be made available via an online Google Form or as a document. If you would like these as documents, the student or I will telephone you weekly at a mutually agreeable time to get your responses. Which method would you prefer? [Note to graduate research assistant: If using Google Forms, please request the email address to send the link. If by paper, please ask if the participant would like the form emailed or sent by post. Please ask the patient for the relevant addresses]. I will also send your $100 gift card [Note to research assistant: Please discuss whether the participant would like a physical or electronic Visa gift card]. Do you have any questions?”
Daily Log form
Please complete approximately at the same time each day. At the end of each day, please upload your responses via Google Forms. If you are not using Google Forms, at the end of the week a university researcher will call you to collect this information.| | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
| Your Sleep-Please Answer Approximately at the Same Time Each Day |
| 1 | How many hours did you sleep last night? | | | | | | | |
| | Approximately how many min did it take for you to fall asleep? | | | | | | | |
| 2 | How was the quality of your sleep? (poor, okay, good, excellent) | | | | | | | |
| Your Exercise-Please Answer Approximately at the Same Time Each Day |
| 3 | Did you exercise today? | | | | | | | |
| Your first time exercising today (if applicable) |
| 4 | What exercise activity did you do? | | | | | | | |
| 5 | What time did you start? | | | | | | | |
| 6 | What time did you stop? | | | | | | | |
| 7 | Was exercise done outside? (yes, no) | | | | | | | |
| 8 | How would you rate the intensity of exercise? (Low, moderate, high) | | | | | | | |
| | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
| 9 | What was the location? (place name or home) | | | | | | | |
| 10 | What was your heart rate immediately after exercising(beats/minute) | | | | | | | |
| Your second time exercising today (if applicable) |
| 11 | What exercise activity did you do? | | | | | | | |
| 12 | What time did you start? | | | | | | | |
| 13 | What time did you stop? | | | | | | | |
| 14 | Was exercise done outside? | | | | | | | |
| 15 | How would you rate the intensity of exercise? (Low, moderate, high) | | | | | | | |
| 16 | What was the location? (place name or home) | | | | | | | |
| 17 | What was your heart rate immediately after exercising(beats/minute) | | | | | | | |
| | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
| Your Physical Health-Please Answer Approximately at the Same Time Each Day |
| 18 | What was your blood pressure? | | | | | | | |
| 19 | How was your physical flexibility today? (poor, okay, good, excellent) | | | | | | | |
| 20 | How was your physical strength today? (poor, okay, good, excellent) | | | | | | | |
| Your Mental Health-Please Answer Approximately at the Same Time Each Day |
| 21 | Did you feel down, depressed or hopeless at all? (yes, no, somewhat) | | | | | | | |
| 22 | Did you have little interest or pleasure in doing things? (yes, no, somewhat) | | | | | | | |
| 23 | Did you feel nervous, anxious or on edge? (yes, no, somewhat) | | | | | | | |
| 24 | Were you unable to control worrying? (yes, no, somewhat) | | | | | | | |
Table A1.
Review of Recent Quantitative Studies on Enhancing Physical Activity and Reducing Obesity.
Table A1.
Review of Recent Quantitative Studies on Enhancing Physical Activity and Reducing Obesity.
| Literature | Study Area | Data Source | Dependent Variable Examined | Major Findings |
|---|
| [1]-(Ulmer et al., 2016) | Sacramento, California | California Health Interview Survey (CHIS). | General Health is assessed in relation to tree canopy near participants’ homes, with mediating factors including obesity, social cohesion, and physical activity. | Higher tree cover was linked to better health, mainly through reduced obesity and enhanced social cohesion. |
| [33]-(Reuben et al., 2020) | United States | National Survey of Children’s Health (NSCH), 2016. | Child Health: focusing on outcomes like physical activity, screen time, sleep, obesity, anxiety, depression, and ADHD in relation to the presence of neighborhood parks. | Children with access to parks showed higher physical activity, better sleep, lower obesity, and reduced ADHD symptoms. |
| [31]-(Wolch et al., 2011) | Southern California | Southern California Children’s Health Study (CHS) (longitudinal study). | BMI index Growth: assessed how access to park space and recreational programs influenced children’s BMI levels over time. | Proximity to parks and availability of programs were associated with reduced BMI growth by age 18, with recreation programs showing more substantial impacts than park space. |
| [32]-(Persson et al., 2018) | Stockholm County, Sweden | Stockholm Diabetes Prevention Program (SDsPP) cohort. | BMI, waist circumference, and weight gain: used to assess adiposity and risks of overweight, obesity, and central obesity with residential greenness. | Greater residential greenness was linked to reduced waist circumference and central obesity in women, not men. Exposure to low greenness, traffic pollution, and noise increased waist circumference in both sexes. |
| [34]-(Tesler et al., 2022) | Israel | Urban Forest Health Intervention Program Survey. | Physical activity, healthy eating habits, self-efficacy, and life satisfaction (LS). | Participation in the program significantly improved physical activity, healthy eating, self-efficacy, and life satisfaction among at-risk youth. |
Table A2.
Review of Recent Quantitative Studies on Reducing Heart Disease.
Table A2.
Review of Recent Quantitative Studies on Reducing Heart Disease.
| Literature | Study Area | Data Source | Dependent Variable Examined | Major Findings |
|---|
| [45]-(Giacinto et al., 2021) | California | California Department of Public Health covering 2010-2018. | Cardiovascular mortality rates for heart disease and stroke are measured per 100,000 individuals. | Greater urban forest biodiversity was linked to a 13% reduction in heart disease mortality and a 16% reduction in stroke mortality, highlighting the health benefits of a diverse tree population. |
| [3]-(Lee et al., 2014) | Japan | Observational field experiment: 48 young Japanese adult males were recruited to examine the short-term physiological and psychological effects of forest walking versus urban walking. | Heart rate variability (HRV), heart rate, blood pressure, and mood states. | Forest walking increased parasympathetic activity, reduced sympathetic activity, lowered heart rate, and improved mood, promoting both physiological and psychological relaxation compared to urban walking. |
| [40]-(Grazuleviciene et al., 2015) | Kaunas, Lithuania | Randomized controlled trial: 20 coronary artery disease (CAD) patients were recruited and randomly assigned to walk 30 min daily for seven consecutive days. | Heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate recovery, and exercise capacity. | Green walking improved heart rate variability, indicating better autonomic function and relaxation, while both green and suburban walking reduced systolic blood pressure without significant differences between environments. |
| [43]-(Brito et al., 2020) | St-Paul Minneapolis, MN metropolitan area | Crossover trial: 24 middle-aged adults participating in both green and suburban walking conditions. The study, lasting for 9 weeks, included two treatments: green walking on nature trails and suburban walking on residential sidewalks. | Heart rate variability (HRV) and blood Pressure. They were measured before, during, and after walking session. | Greater residential greenness was linked to reduced waist circumference and central obesity in women, not men. Exposure to low greenness, traffic pollution, and noise increased waist circumference in both sexes. |
| [12]-(Mao et al., 2017) | Zhejiang Province, China | Randomized controlled trial: 45 CHF patients from Hangzhou City, with 36 completing the study. | Cardiovascular biomarkers include BNP and NT-pro BNP, as well as inflammatory cytokines, oxidative stress markers, and cardiovascular disease-related factors like endothelin-1(ET-1) and renin–angiotensin system components. | Forest bathing improved health in elderly heart failure patients, reducing BNP ET-1, inflammatory markers, and oxidative stress while enhancing mood and reducing tension, anxiety, and depression. |
| [62]-(Seo et al., 2019) | Korea | Korean National Health Insurance Service National Sample Cohort (NHIS-NSC), which includes data from 351,409 participants aged over 20 years from seven Korean metropolitan areas. | Cardiovascular disease (CVD) events include coronary heart disease, acute myocardial infarction, total stroke, ischemic stroke, and hemorrhagic stroke. | Living in areas with higher green space coverage significantly reduced the risk of cardiovascular disease, including coronary heart disease and stroke, especially for individuals aged 40 and older. |
| [39]-(Paul et al., 2020) | Ontario, Canada | Ontario Population Health and Environment Cohort (ONPHEC), which includes all Canadian-born Ontario residents aged 35–100 who were registered with provincial health insurance. | Risk of dementia and stroke. | Increased urban green space was linked to a 3% reduced risk of dementia and a 4% reduced risk of stroke, indicating its protective effect on neurological health. |
| [44] (Mao et al., 2012) | Hangzhou, China | Randomized controlled trial: 24 elderly patients with essential hypertension we recruited. | Blood pressure (systolic and diastolic), cardiovascular disease-related biomarkers, pro-inflammatory cytokines, and mood states. | Forest bathing significantly reduced blood pressure and improved cardiovascular health in elderly hypertensive patients, with lower levels of endothelin-1, homocysteine, and pro-inflammatory cytokines. |
Table A3.
Review of Recent Quantitative Studies on the Mental Health Effects of Nature Therapies.
Table A3.
Review of Recent Quantitative Studies on the Mental Health Effects of Nature Therapies.
| Literature | Study Area | Data Source | Dependent Variable Examined | Major Findings |
| [50]-(Koselka et al., 2019) | Greater Chicago, Illinois | Randomized controlled trial (RCT): participants from Northwestern University and nearby communities. | Positive and negative affect, state anxiety, perceived stress, and working memory (visual backward digit span). | Forest walking improved positive affect, reduced anxiety, and lowered perceived stress compared to road sidewalk and daily activities. |
| [63]-(Razani et al., 2018) | Oakland, California | Randomized controlled trial: Primary Care Clinic (PCC), a federally qualified health center in Oakland, California. | Stress: Using PSS10, other secondary variables include park visits, loneliness, physical activity, physiologic stress (salivary cortisol), and nature affinity. | Park prescription reduced stress in low-income parents, with increased park visits significantly linked to lower stress. |
| [41]-(Song et al., 2015) | Japan | Twenty Japanese men; participants walked in a coniferous forest and an urban area on consecutive days. | Heart rate variability (HRV) and heart rate, psychological responses (measured by semantic differential and POMS) to assess autonomic nervous system and mood changes. | Forest walking significantly increased parasympathetic activity, lowered heart rate, and improved mood, reducing anxiety and fatigue in middle-aged hypertensive individuals compared to urban walking. |
| [47]-(Berman et al., 2012) | Ann Arbor, Michigan | Participants with major depressive disorder were recruited and assessed using SCID and PANAS. | Working memory capacity and affective states. These were measured before and after participants took a walk in a natural or urban setting. | Nature walks improved memory and had more positive effects on individuals with depression than urban walks. |
| [64]-(Sia et al., 2020) | Singapore | Field experimental design: data from 47 elderly participants in Singapore’s senior care centers were measured using various scales (happiness, cognitive function, sleep hygiene), before, during, and after a 24-week therapeutic horticulture program. | Momentary affect, cognitive function (measured by MMSE), functional outcomes, and psychosocial health. | The program improved cognitive function, reduced anxiety, and enhanced positive affect in older adults with sustained benefits up to size months post-intervention. |
| [42]-(Yu et al., 2017) | Taiwan | One-group pre-test–post-test field experimental design. | Autonomic nervous system activity measured through HRV, pulse rate, and diastolic blood pressure, and psychological states assessed using POMS and STAI. | Forest bathing reduced pulse rate and systolic and diastolic blood pressure, improved mood, and increased positive emotions in middle-aged and elderly participants. |
| [51]-(Orstad et al., 2020) | New York City | New York City’s Physical Activity and Transit (PAT) survey conducted between 2010 and 2011. | Mental distress and other variables include park proximity and frequency of park use for physical activity. | Park proximity was linked to fewer days of mental distress through increased park-based physical activity. |
| [49]-Beute & De Kort, 2018) | Eindhoven, Netherlands | Ecological Momentary Assessment (EMA) in an intensive longitudinal design. Fifty-nine participants were recruited for the study from the mental health institutes and a local participant database. | Stress levels as measured by momentary assessment throughout the day. Other variables include mood, psychosomatic complaints, and rumination. | Nature and daylight exposure improved mood and reduced stress, with nature being particularly beneficial for individuals with depressive symptoms, while daylight had consistent positive effects across all participants. |
| [65]-(Razani et al., 2019) | Oakland, California | Prospective cohort design, observing individuals for three months. Data were collected from the clinical trial at a federally qualified health center. | Child resilience is measured using the Brief Resiliency Scale (BRS), and child stress is measured using the PSQ 8-11 scale. | Park prescriptions increased resilience in low-income children, with more weekly park visits linked to greater improvements. |
| [66]-(Chun et al., 2017) | Gyenggi-do, Republic of Korea | Cross-sectional study: 59 patients with chronic stroke were recruited from a stroke welfare center in South Korea. | Depression and anxiety in patients with chronic stroke. | Forest therapy significantly reduced depression and anxiety in chronic stroke patients with increased antioxidant capacity. |