Biomechanical Influence of Placement Angle and Loading Direction of Orthodontic Miniscrews on Orthotropic Mandible
Abstract
1. Introduction
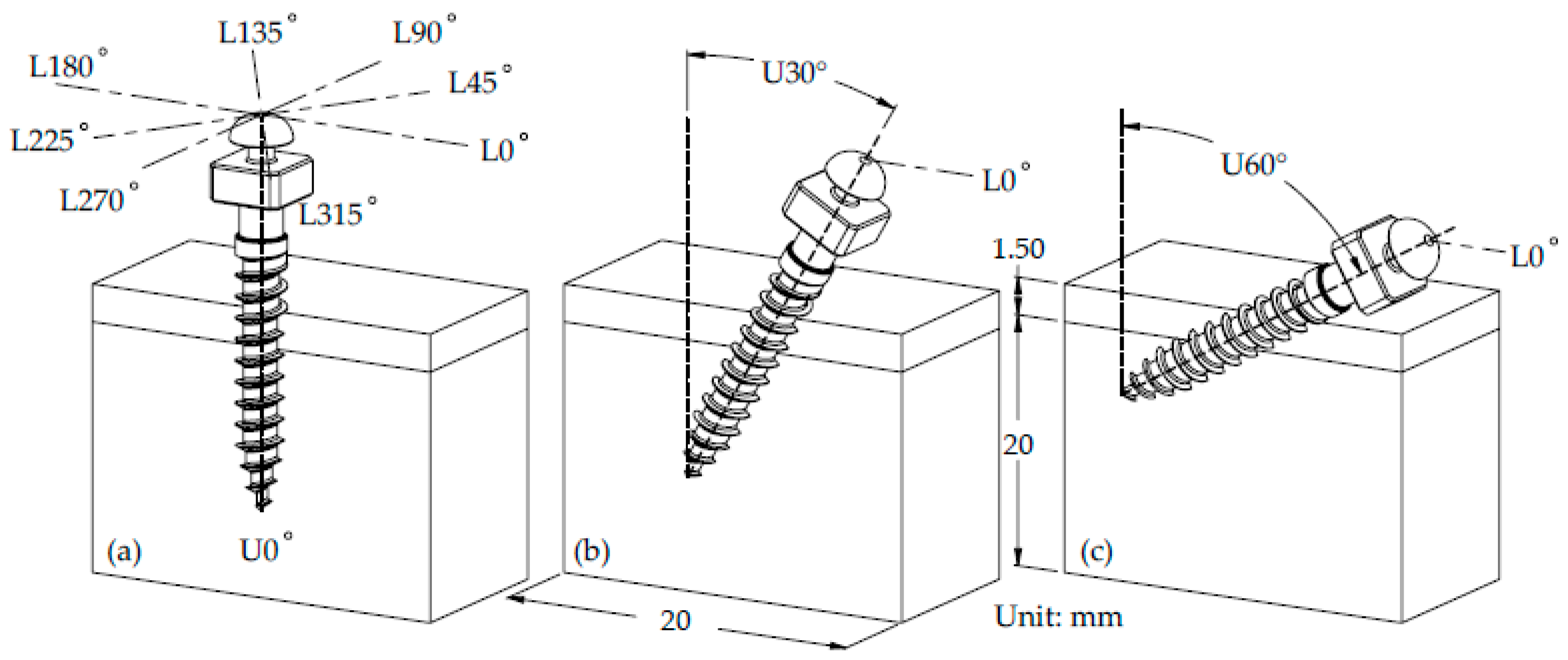
2. Materials and Methods
2.1. Three-Dimensional Model Preparation
2.2. Material Property
2.3. Finite Element Analysis
2.4. Biomechanical Parameters for Evaluation
3. Results
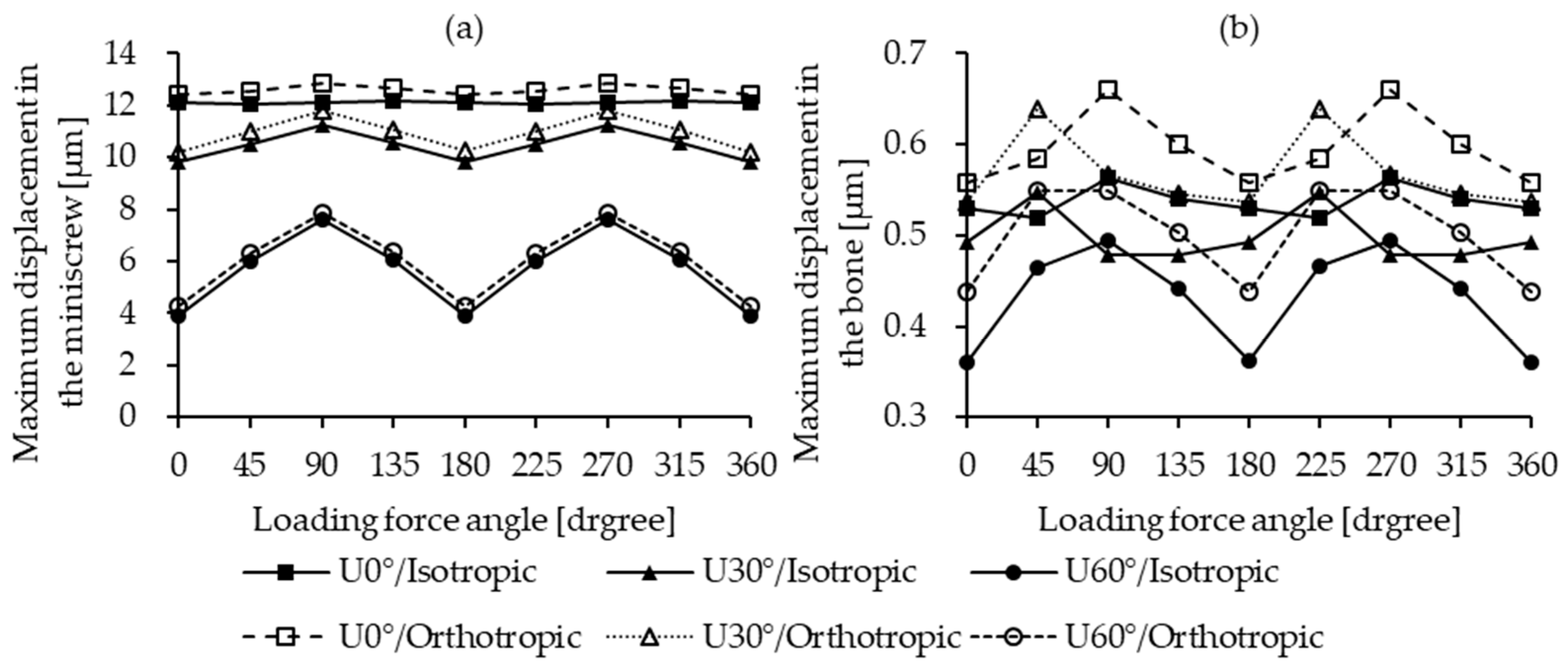
3.1. Maximum Displacement in the Miniscrew and the Bone
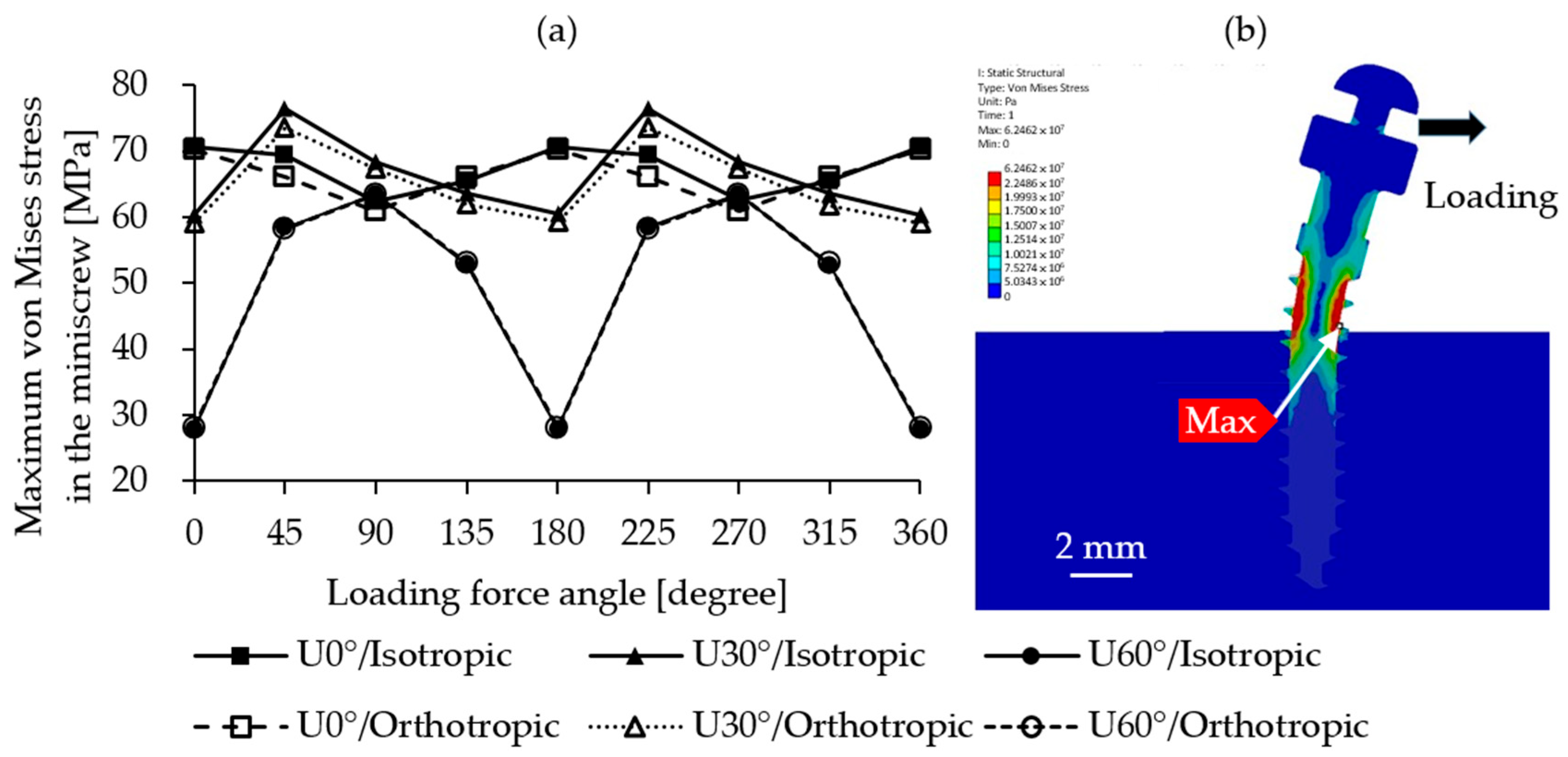
3.2. Maximum Von Mises Stress in the Miniscrew
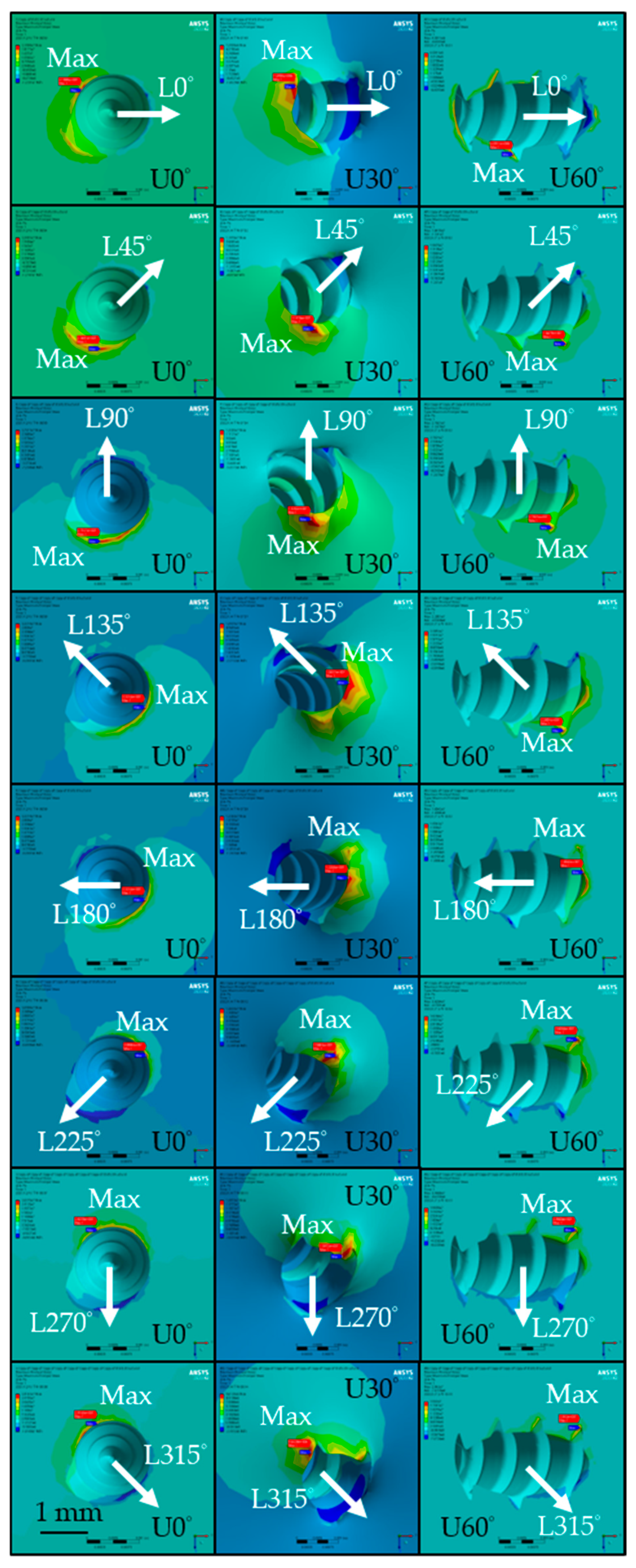
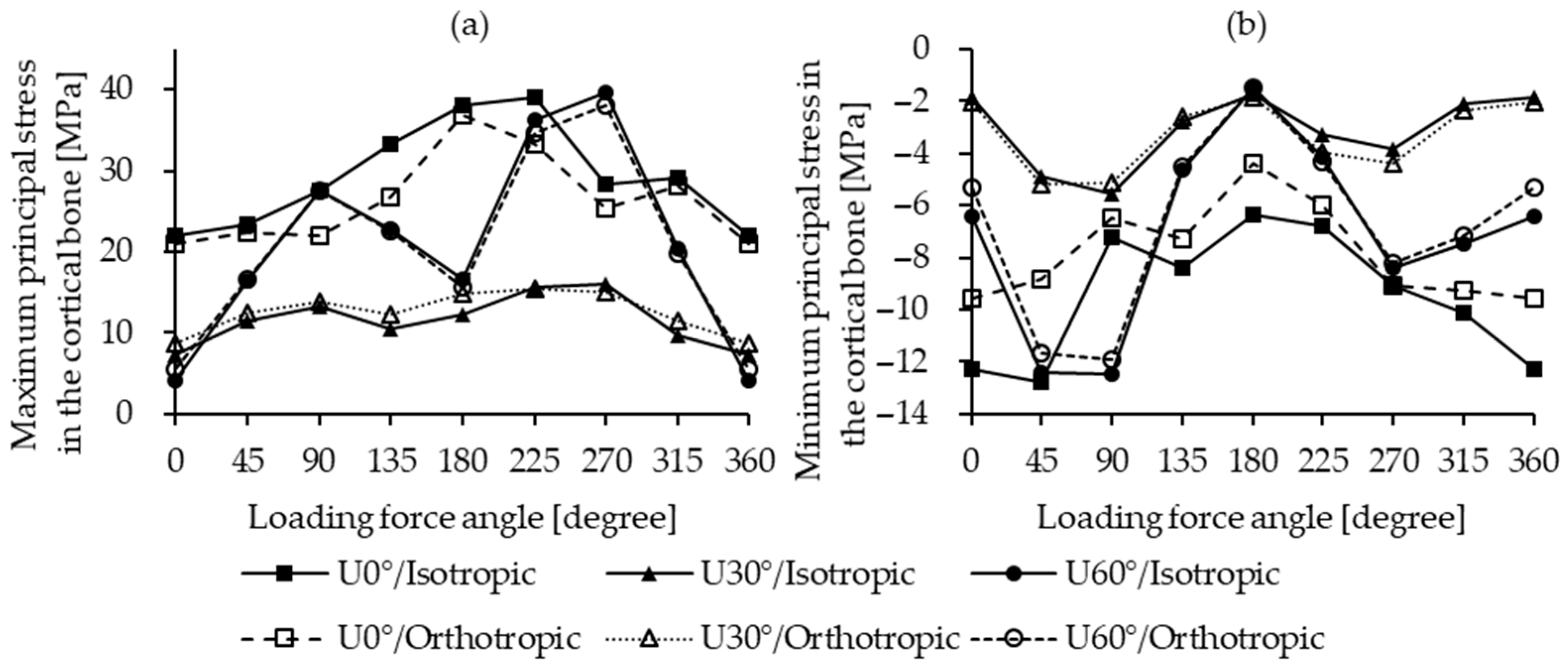
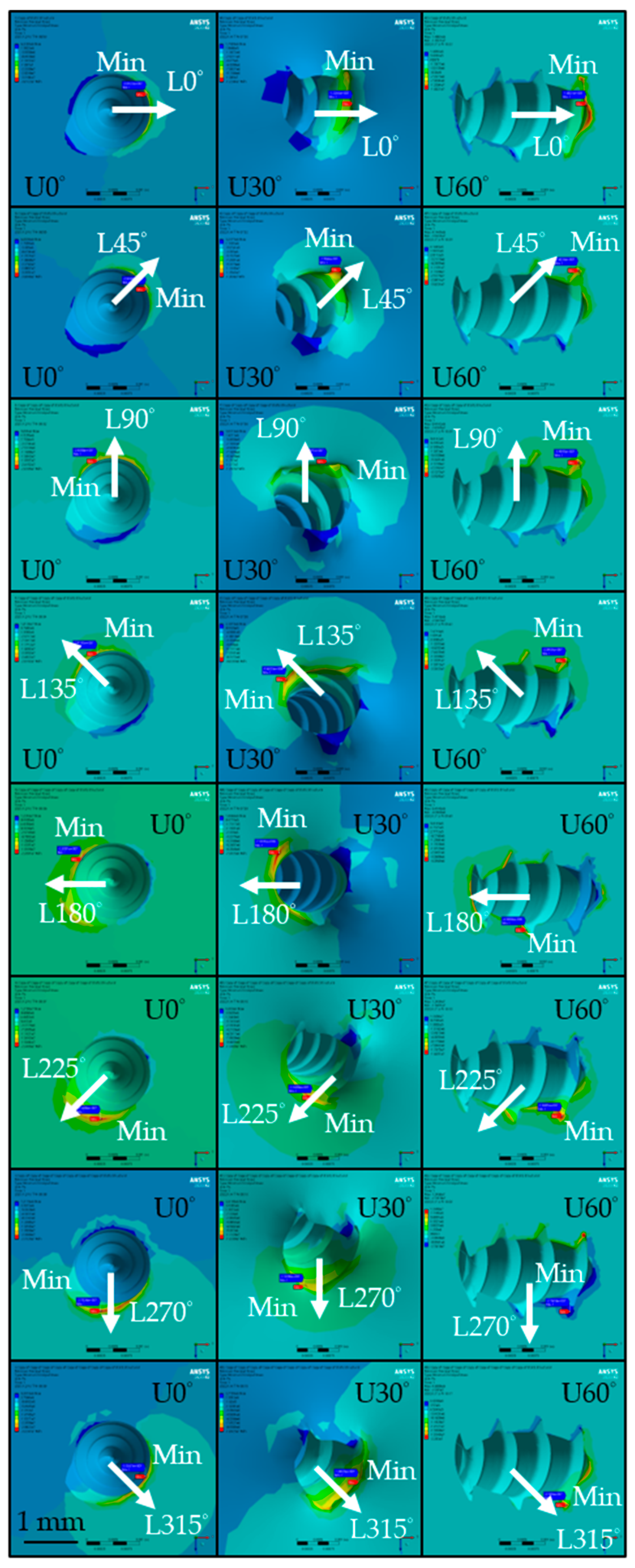
3.3. Maximum/Minimum Principal Stress in the Cortical Bone
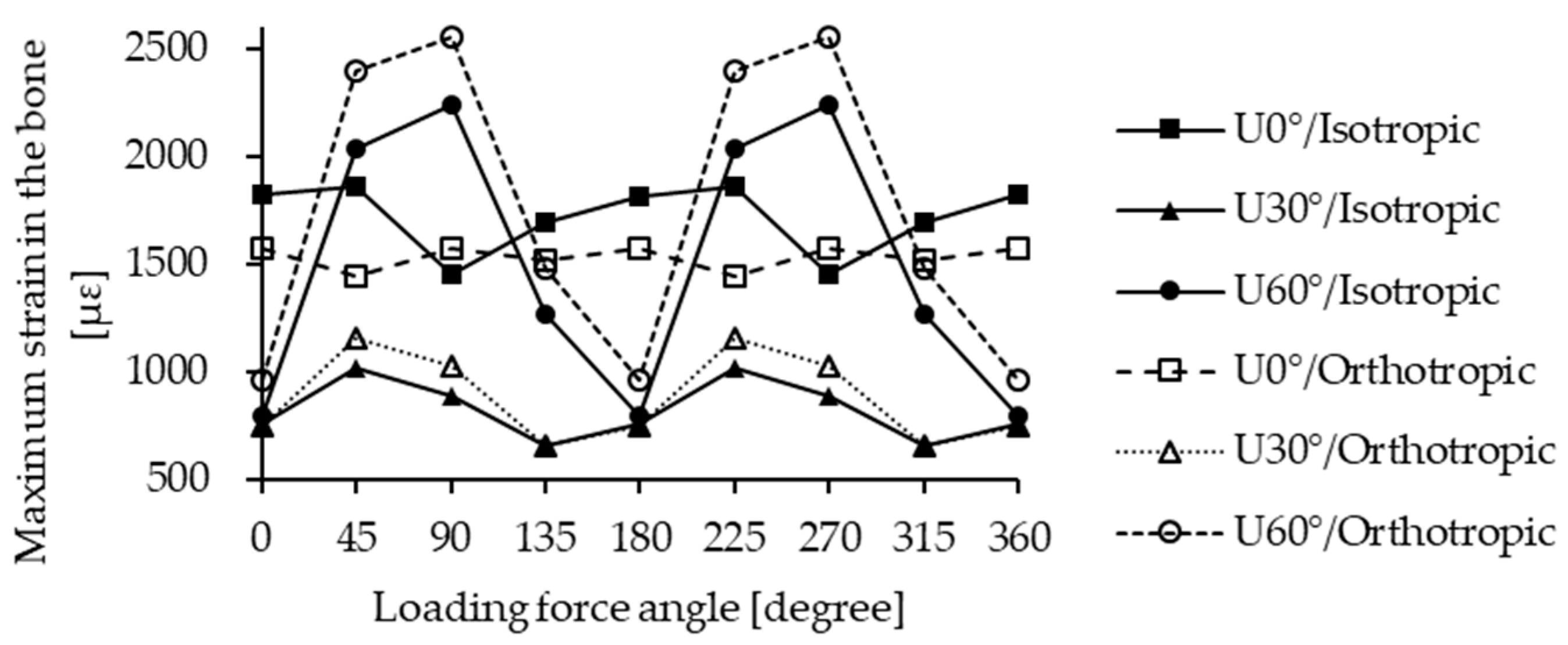
3.4. Maximum Strain in the Bone
4. Discussion
4.1. Anisotropic Bone Models
4.2. Safety of Minscrew Design
4.3. Influence of Loading Direction and Insertion Angle
4.4. Strain Distribution in the Bone
4.5. Principal Stresses in the Cortical Bone
5. Conclusions
- Assuming isotropic bone properties leads to unrealistic predictions, underestimating miniscrew displacement and stability risk; orthotropic properties reflecting true bone anisotropy are therefore recommended.
- Increasing the miniscrew insertion angle reduces stability, particularly affecting bone strain and osseointegration potential, which vary with loading direction.
- Oblique miniscrew insertion may reduce stability, but aligning the load parallel to the insertion plane can mitigate adverse effects.
- For vertical insertion, thread design has minimal impact on displacement, von Mises stress, and bone strain; its influence increases at larger insertion angles.
- Certain biomechanical indicators (displacement, maximum von Mises stress, maximum strain) are symmetric across loading directions, allowing for an analysis of only half the directions.
- The current miniscrew design does not cause direct mechanical failure under clinical loading; most reported failures are likely due to biological factors, such as bone resorption or inflammation.
6. Limitations
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alharbi, F.; Almuzian, M.; Bearn, D. Anchorage effectiveness of orthodontic miniscrews compared to headgear and transpalatal arches: A systematic review and meta-analysis. Acta Odontol. Scand. 2019, 77, 88–98. [Google Scholar] [CrossRef]
- Papageorgiou, S.N.; Kutschera, E.; Memmert, S.; Gölz, L.; Jäger, A.; Bourauel, C.; Eliades, T. Effectiveness of early orthopaedic treatment with headgear: A systematic review and meta-analysis. Eur. J. Orthod. 2017, 39, 176–187. [Google Scholar] [CrossRef]
- Becker, K.; Unland, J.; Wilmes, B.; Tarraf, N.E.; Drescher, D. Is there an ideal insertion angle and position for orthodontic mini-implants in the anterior palate? A CBCT study in humans. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 345–354. [Google Scholar] [CrossRef]
- Costa, A.; Raffainl, M.; Melsen, B. Miniscrews as orthodontic anchorage: A preliminary report. Int. J. Adult Orthodon. Orthognath. Surg. 1998, 13, 201–209. [Google Scholar]
- Meher, A.H.; Shrivastav, S.S.; Vibhute, P.J.; Hazarey, P.V. Deflection and stress distribution around mini-screw implants: A finite element investigation into the effect of cortical bone thickness, force magnitude and direction. J. Orthod. 2012, 39, 249–255. [Google Scholar] [CrossRef]
- Lee, J.; Kim, J.Y.; Choi, Y.J.; Kim, K.H.; Chung, C.J. Effects of placement angle and direction of orthopedic force application on the stability of orthodontic miniscrews. Angle Orthod. 2013, 83, 667–673. [Google Scholar] [CrossRef]
- Rodríguez-Rimachi, M.E.; Malpartida-Pacheco, M.I.; Olazábal-Martínez, W.C. Success rate of infrazygomatic miniscrews considering their design and insertion techniques: A review. Rev. Cient. Odontol. 2022, 10, e117. [Google Scholar] [CrossRef]
- Xin, Y.; Wu, Y.; Chen, C.; Wang, C.; Zhao, L. Miniscrews for orthodontic anchorage: Analysis of risk factors correlated with the progressive susceptibility to failure. Am. J. Orthod. Dentofac. Orthop. 2022, 162, e192–e202. [Google Scholar] [CrossRef]
- Zheng, J.; Wu, Y.; Jiang, W.; Zhao, L.; Jing, D.; Zhang, N.; Cao, X.; Xu, Z.; Zhao, Z. Factors affecting the clinical success rate of miniscrew implants for orthodontic treatment. Int. J. Oral Maxillofac. Implant. 2016, 31, 835–841. [Google Scholar] [CrossRef]
- Wilmes, B.; Su, Y.Y.; Drescher, D. Insertion angle impact on primary stability of orthodontic mini-implants. Angle Orthod. 2008, 78, 1065–1070. [Google Scholar] [CrossRef]
- Araghbidikashani, M.; Golshah, A.; Nikkerdar, N.; Rezaei, M. In-vitro impact of insertion angle on primary stability of miniscrews. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 436–443. [Google Scholar] [CrossRef]
- Perillo, L.; Jamilian, A.; Shafieyoon, A.; Karimi, H.; Cozzani, M. Finite element analysis of miniscrew placement in mandibular alveolar bone. Eur. J. Orthod. 2015, 37, 56–59. [Google Scholar] [CrossRef][Green Version]
- Tatli, U.; Alraawi, M.; Toroğlu, M.S. Effects of size and insertion angle of orthodontic mini-implants on skeletal anchorage. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 220–228. [Google Scholar] [CrossRef]
- Cozzani, M.; Nucci, L.; Lupini, D.; Dolatshahizand, H.; Fazeli, D.; Barzkar, E.; Naeini, E.; Jamilian, A. The ideal insertion angle after immediate loading in Jeil, Storm, and Thunder miniscrews: A 3D-FEM study. Int. Orthod. 2020, 18, 503–508. [Google Scholar] [CrossRef]
- Li, S.; Demirci, E.; Silberschmidt, V.V. Variability and anisotropy of mechanical behavior of cortical bone in tension and compression. J. Mech. Behav. Biomed. Mater. 2013, 21, 109–120. [Google Scholar] [CrossRef]
- Schwartz-Dabney, C.L.; Dechow, P.C. Variations in cortical material properties throughout the human dentate mandible. Am. J. Phys. Anthropol. 2003, 120, 252–277. [Google Scholar] [CrossRef]
- Castaño, M.C.; Zapata, U.; Pedroza, A.; Jaramillo, J.D.; Roldán, S. Creation of a three-dimensional model of the mandible and the TMJ in vivo by means of the finite element method. Int. J. Comput. Dent. 2002, 5, 87–99. [Google Scholar]
- Wolfram, U.; Schwiedrzik, J. Post-yield and failure properties of cortical bone. Bonekey Rep. 2016, 5, 829. [Google Scholar] [CrossRef]
- Baca, V.; Horak, Z.; Mikulenka, P.; Dzupa, V. Comparison of an inhomogeneous orthotropic and isotropic material models used for FE analyses. Med. Eng. Phys. 2008, 30, 924–930. [Google Scholar] [CrossRef]
- Baca, V.; Horak, Z. Comparison of isotropic and orthotropic material property assignments on femoral finite element models under two loading conditions. Med. Eng. Phys. 2007, 29, 935. [Google Scholar] [CrossRef]
- Yang, H.; Ma, X.; Guo, T. Some factors that affect the comparison between isotropic and orthotropic inhomogeneous finite element material models of femur. Med. Eng. Phys. 2010, 32, 553–560. [Google Scholar] [CrossRef]
- Boggio, A.; Jamilian, A.; Manni, A.; Gastaldi, G.; Farjaminejad, R.; Hasani, M.; Cozzani, M. The effect of a Manni telescopic Herbst appliance with four miniscrews (STM4) on the treatment of a Class II Division I malocclusion: A 3D finite element study. Oral 2025, 5, 27. [Google Scholar] [CrossRef]
- Nazeri, A.; Castillo, J.A.; Ghaffari-Rafi, A. Impact of molar distalization with clear aligners on periodontal ligament stress and root resorption risk: A systematic review of 3D finite element analysis studies. Dent. J. 2025, 13, 65. [Google Scholar] [CrossRef]
- Hwang, J.B.; Mo, S.S. Finite element analysis of maxillary teeth movement with time during en masse retraction using orthodontic mini-screw. Appl. Sci. 2023, 13, 3579. [Google Scholar] [CrossRef]
- Kim, J.H.; Hyeok, J.J.; Woo, J.H.; Kim, S.M. Correlation analysis of suture anchor pull-out strength with cortical bone thickness and cancellous bone density on a finite element model. Bioengineering 2025, 12, 863. [Google Scholar] [CrossRef] [PubMed]
- Pimentel-Mendoza, A.B.; Rico-Pérez, L.; Rosel-Solis, M.J.; Villarreal-Gómez, L.J.; Vega, Y.; Dávalos-Ramírez, J.O. Application of inverse neural networks for optimal pretension of absorbable mini plate and screw system. Appl. Sci. 2021, 11, 1350. [Google Scholar] [CrossRef]
- Sunagawa-Kojima, H.; Ohtani, J.; Kaku, M.; Tsubamoto, N.; Ishikawa, E.; Tanne, K.; Tanimoto, K. Histomorphometric evaluation of cortical bone surrounding miniscrew: Why is the insertion torque critical for primary stability? Biomed. Res. 2018, 29, 3028–3033. [Google Scholar]
- Deguchi, T.; Nasu, M.; Murakami, K.; Yabuuchi, T.; Kamioka, H.; Takano-Yamamoto, T. Quantitative evaluation of cortical bone thickness with computed tomographic scanning for orthodontic implants. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 721–732. [Google Scholar] [CrossRef] [PubMed]
- Gracco, A.; Luca, L.; Cozzani, M.; Siciliani, G. Assessment of palatal bone thickness in adults with cone beam computerized tomography. Aust. Orthod. J. 2007, 23, 109–113. [Google Scholar]
- Parmar, R.; Reddy, V.; Reddy, S.K.; Reddy, D. Determination of soft tissue thickness at orthodontic miniscrew placement sites using ultrasonography for customizing screw selection. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 651–658. [Google Scholar] [CrossRef]
- Javiya, P.; Bhattu, B.K.; Chitumalla, R.; Mahantshetty, M.; Dave, M.; Pattnaik, N.; Ghadage, M.; Patil, D. In Vitro Evaluation of Stress Distribution around Implants with Different Designs. J. Pharm. Bioallied Sci. 2025, 17 (Suppl. 2), S1478–S1480. [Google Scholar] [CrossRef]
- ASM International. Medical Applications of Stainless Steels; ASM International: Materials Park, OH, USA, 2012; p. 12. [Google Scholar]
- Vande Vannet, B.; Moradi Sabzevar, M.; Wehrbein, H.; Asscherickx, K. Osseointegration of miniscrews: A histomorphometric evaluation. Eur. J. Orthod. 2007, 29, 437–442. [Google Scholar] [CrossRef]
- Choi, S.-H.; Kim, S.-J.; Lee, K.-J.; Sung, S.-J.; Chun, Y.-S.; Hwang, C.-J. Stress distributions in peri-miniscrew areas from cylindrical and tapered miniscrews inserted at different angles. Korean J. Orthod. 2016, 46, 189–198. [Google Scholar] [CrossRef][Green Version]
- Tokuyama-Toda, R.; Umeki, H.; Ide, S.; Kobayashi, F.; Tooyama, S.; Umehara, M.; Tadokoro, S.; Tomonari, H.; Satomura, K. A new implantation method for orthodontic anchor screws: Basic research for clinical applications. Biomedicines 2023, 11, 665. [Google Scholar] [CrossRef]
- Abdul Wahab, A.H.; Abdul Kadir, M.R.; Harun, M.N.; Syahrom, A.; Ramlee, M.H. Different material properties of cancellous bone influence analysis of glenoid component loosening: A finite element study. Malays. J. Fundam. Appl. Sci. 2017, 13, 483–488. [Google Scholar] [CrossRef]
- Taheri, R.A.; Jarrahi, A.; Farnoosh, G.; Karimi, A. A comparative finite element simulation of stress in dental implant–bone interface using isotropic and orthotropic material models in three mastication cycles. J. Braz. Soc. Mech. Sci. Eng. 2018, 40, 10. [Google Scholar] [CrossRef]
- Do, V.; Hsu, Q.C.; Chen, P.H.; Chen, Y.L. Study on the performance of orthodontic self-drilling correction screw of Ti6Al4V and stainless 316L. Mater. Sci. Forum 2016, 872, 276–280. [Google Scholar] [CrossRef]
- Tepedino, M.; Masedu, F.; Chimenti, C. Comparative evaluation of insertion torque and mechanical stability for self-tapping and self-drilling orthodontic miniscrews: An in vitro study. Head Face Med. 2017, 13, 10. [Google Scholar] [CrossRef]
- Ebacher, V.; Tang, C.; McKay, H.; Oxland, T.R.; Guy, P.; Wang, R. Strain redistribution and cracking behavior of human bone during bending. Bone 2007, 40, 1265–1275. [Google Scholar] [CrossRef]
- Singh, S.; Mogra, S.; Shetty, V.S.; Shetty, S.; Philip, P. Three-dimensional finite element analysis of strength, stability, and stress distribution in orthodontic anchorage: A conical, self-drilling miniscrew implant system. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 327–336. [Google Scholar] [CrossRef]
- Teekavanich, C.; Uezono, M.; Takakuda, K.; Ogasawara, T.; Techalertpaisarn, P.; Moriyama, K. Evaluation of cortical bone microdamage and primary stability of orthodontic miniscrew using a human bone analogue. Materials 2021, 14, 1825. [Google Scholar] [CrossRef]
- Kuroda, S.; Inoue, M.; Kyung, H.M.; Koolstra, J.H.; Tanaka, E. Stress distribution in obliquely inserted orthodontic miniscrews evaluated by three-dimensional finite-element analysis. Int. J. Oral Maxillofac. Implant. 2017, 32, 344–349. [Google Scholar] [CrossRef]
- Motoyoshi, M.; Inaba, M.; Ono, A.; Ueno, S.; Shimizu, N. The effect of cortical bone thickness on the stability of orthodontic mini-implants and on the stress distribution in surrounding bone. Int. J. Oral Maxillofac. Surg. 2009, 38, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Dissaux, C.; Wagner, D.; George, D.; Spingarn, C.; Remond, Y. Mechanical impairment on alveolar bone graft: A literature review. J. Craniomaxillofac. Surg. 2019, 47, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Duaibis, R.; Kusnoto, B.; Natarajan, R.; Zhao, L.; Evans, C. Factors affecting stresses in cortical bone around miniscrew implants: A three-dimensional finite element study. Angle Orthod. 2012, 82, 875–880. [Google Scholar] [CrossRef] [PubMed]



| Material | Young’s Modulus, E [MPa] | Poisson’s Ratio, ν |
|---|---|---|
| Cortical bone | 13,700 | 0.3 |
| Cancellous bone | 1370 | 0.3 |
| Miniscrew | 200,000 | 0.33 |
| Material | Young’s Modulus, E [MPa] | Poisson’s Ratio, ν | Shear Modulus, G [MPa] | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Direction | X | Y | Z | XY | YZ | XZ | XY | YZ | XZ |
| Cortical bone | 19,600 | 13,800 | 10,600 | 0.38 | 0.23 | 0.47 | 6200 | 4100 | 5400 |
| Cancellous bone | 960 | 390 | 320 | 0.3 | 0.3 | 0.3 | 170 | 130 | 90 |
| Insert Angle | Nodes | Elements |
|---|---|---|
| U0° | 207,663 | 148,023 |
| U30° | 200,084 | 137,417 |
| U60° | 187,787 | 122,500 |
| L0° | L45° | L90° | L135° | L180° | L225° | L270° | L315° | L360° | |
|---|---|---|---|---|---|---|---|---|---|
| Maximum displacement in the miniscrew [%] | |||||||||
| U0° | 2.5 | 4.4 | 6.1 | 4.2 | 2.5 | 4.4 | 6.1 | 4.2 | 2.5 |
| U30° | 4.2 | 5.0 | 5.3 | 4.7 | 4.2 | 5.0 | 5.3 | 4.7 | 4.2 |
| U60° | 8.9 | 4.8 | 3.6 | 4.7 | 8.9 | 4.8 | 3.6 | 4.7 | 8.9 |
| Maximum von Mises stress in the miniscrew [%] | |||||||||
| U0° | −0.6 | −4.7 | −2.6 | 0.9 | −0.6 | −4.7 | −2.6 | 0.9 | −0.6 |
| U30° | −2.1 | −3.9 | −1.5 | −2.6 | −2.1 | −3.9 | −1.5 | −2.8 | −2.1 |
| U60° | 0.4 | −0.5 | −0.1 | 0.3 | 0.4 | −0.5 | −0.1 | 0.3 | 0.4 |
| Maximum principal stress in the cortical bone [%] | |||||||||
| U0° | −4.8 | −4.9 | −20.1 | −19.2 | −3.1 | −14.4 | −10.1 | −3.8 | −4.8 |
| U30° | 19.8 | 9.4 | 5.6 | 16.6 | 21.5 | −1.2 | −5.7 | 18.5 | 19.8 |
| U60° | 34.3 | 1.2 | −0.1 | −1.0 | −5.8 | −4.6 | −3.9 | −2.9 | 34.3 |
| Minimum principal stress in the cortical bone [%] | |||||||||
| U0° | −22.2 | −30.7 | −10.8 | −13.0 | −31.0 | −12.1 | 0.0 | −8.8 | −22.2 |
| U30° | 10.4 | 5.9 | −7.3 | −5.6 | 5.6 | 21.8 | 14.4 | 11.3 | 10.4 |
| U60° | −16.8 | −6.0 | −4.7 | −2.0 | 0.3 | 3.6 | −2.4 | −4.3 | −16.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.-C.; Hwang, J.-R.; Fung, C.-P.; Chung, C.-Y. Biomechanical Influence of Placement Angle and Loading Direction of Orthodontic Miniscrews on Orthotropic Mandible. Materials 2025, 18, 4963. https://doi.org/10.3390/ma18214963
Li Y-C, Hwang J-R, Fung C-P, Chung C-Y. Biomechanical Influence of Placement Angle and Loading Direction of Orthodontic Miniscrews on Orthotropic Mandible. Materials. 2025; 18(21):4963. https://doi.org/10.3390/ma18214963
Chicago/Turabian StyleLi, Yu-Ching, Jiun-Ren Hwang, Chin-Ping Fung, and Chen-Yuan Chung. 2025. "Biomechanical Influence of Placement Angle and Loading Direction of Orthodontic Miniscrews on Orthotropic Mandible" Materials 18, no. 21: 4963. https://doi.org/10.3390/ma18214963
APA StyleLi, Y.-C., Hwang, J.-R., Fung, C.-P., & Chung, C.-Y. (2025). Biomechanical Influence of Placement Angle and Loading Direction of Orthodontic Miniscrews on Orthotropic Mandible. Materials, 18(21), 4963. https://doi.org/10.3390/ma18214963






