Micro-CT Assessment of Internal and External Void Formation in Class II Restorations of Primary Molars Using Bulk-Fill Composites
Abstract
1. Introduction
2. Materials and Methods
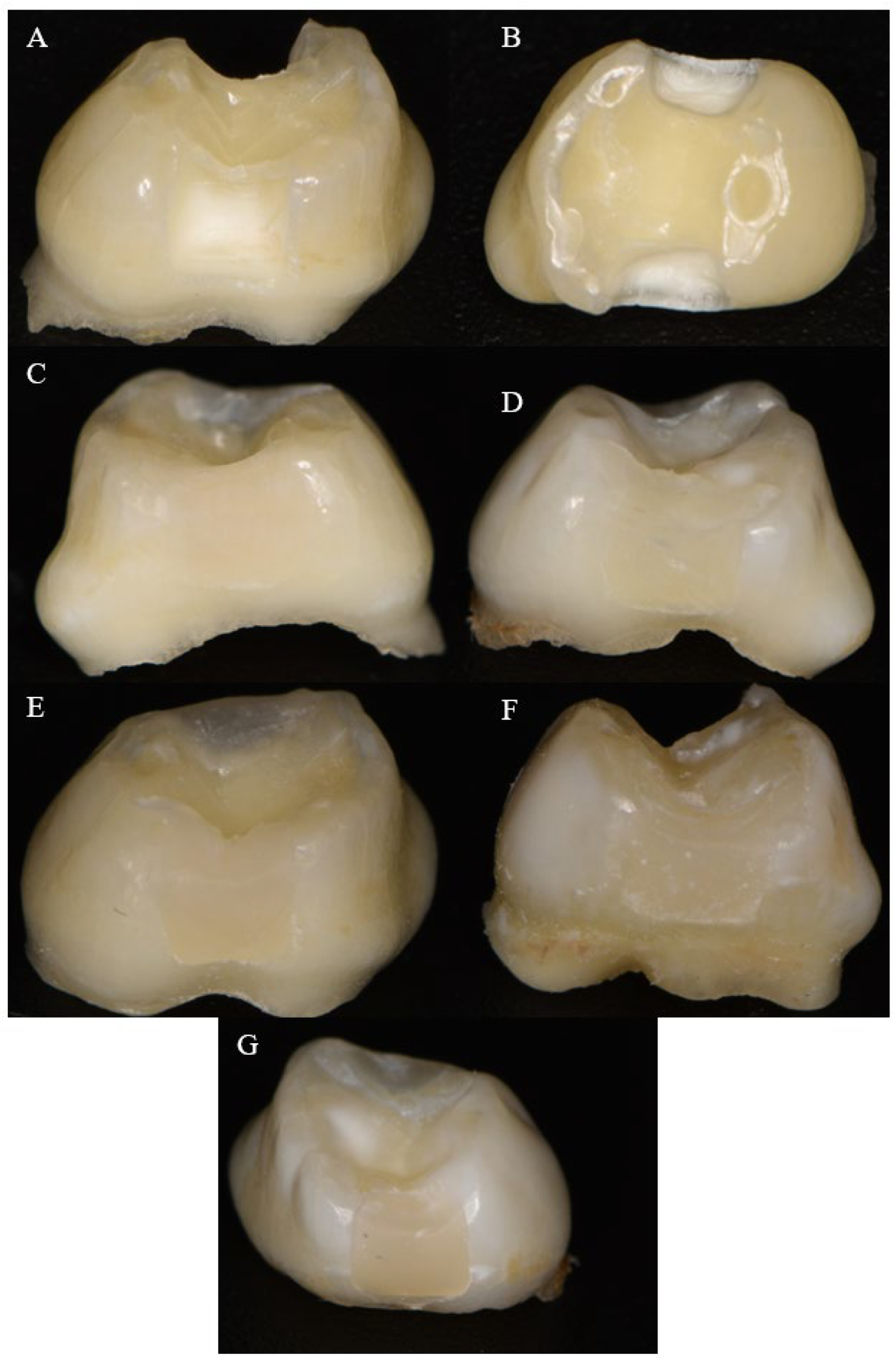
2.1. Sample Preparation
2.2. Restorative Technique
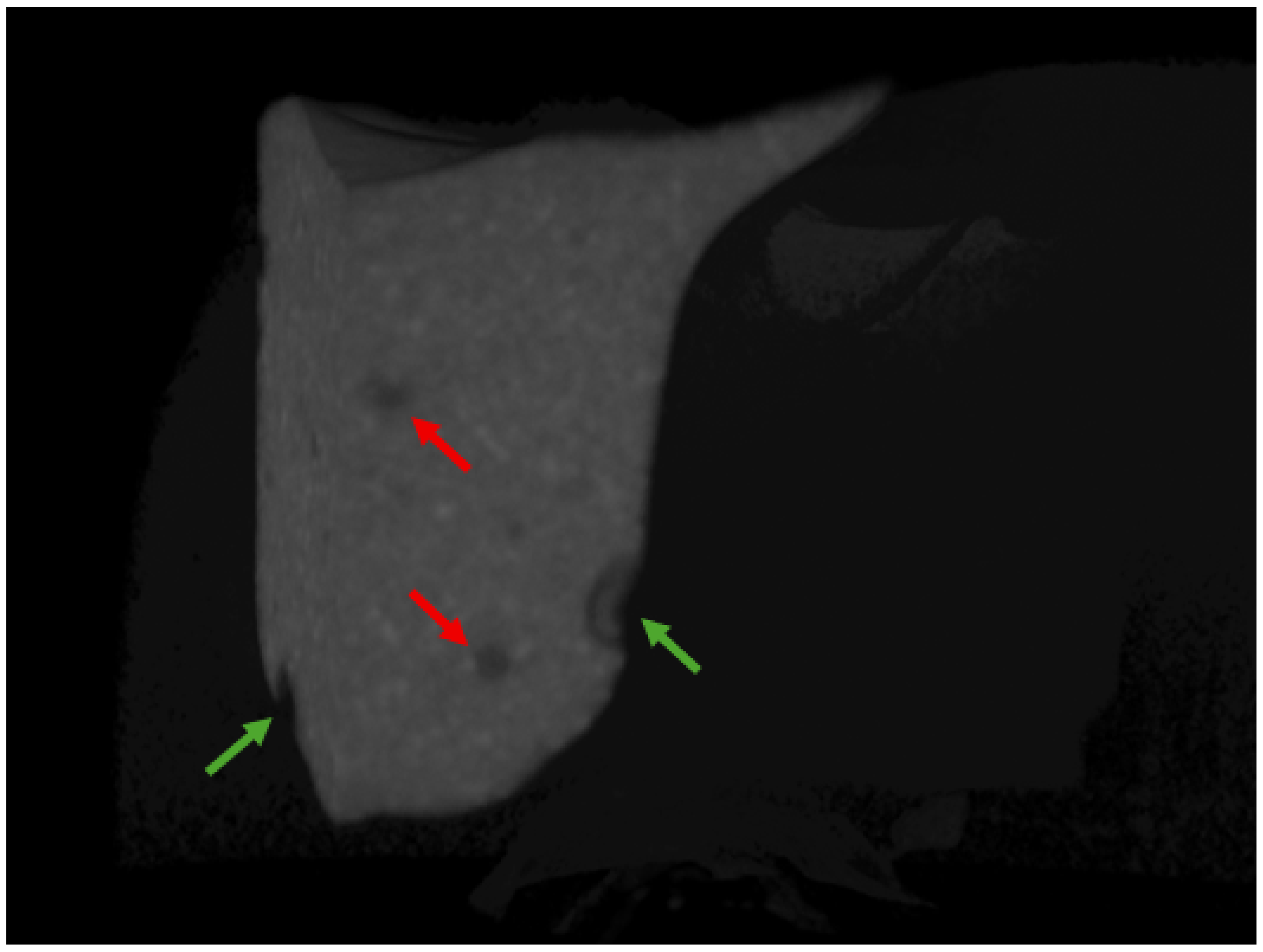
2.3. Scanning Procedure
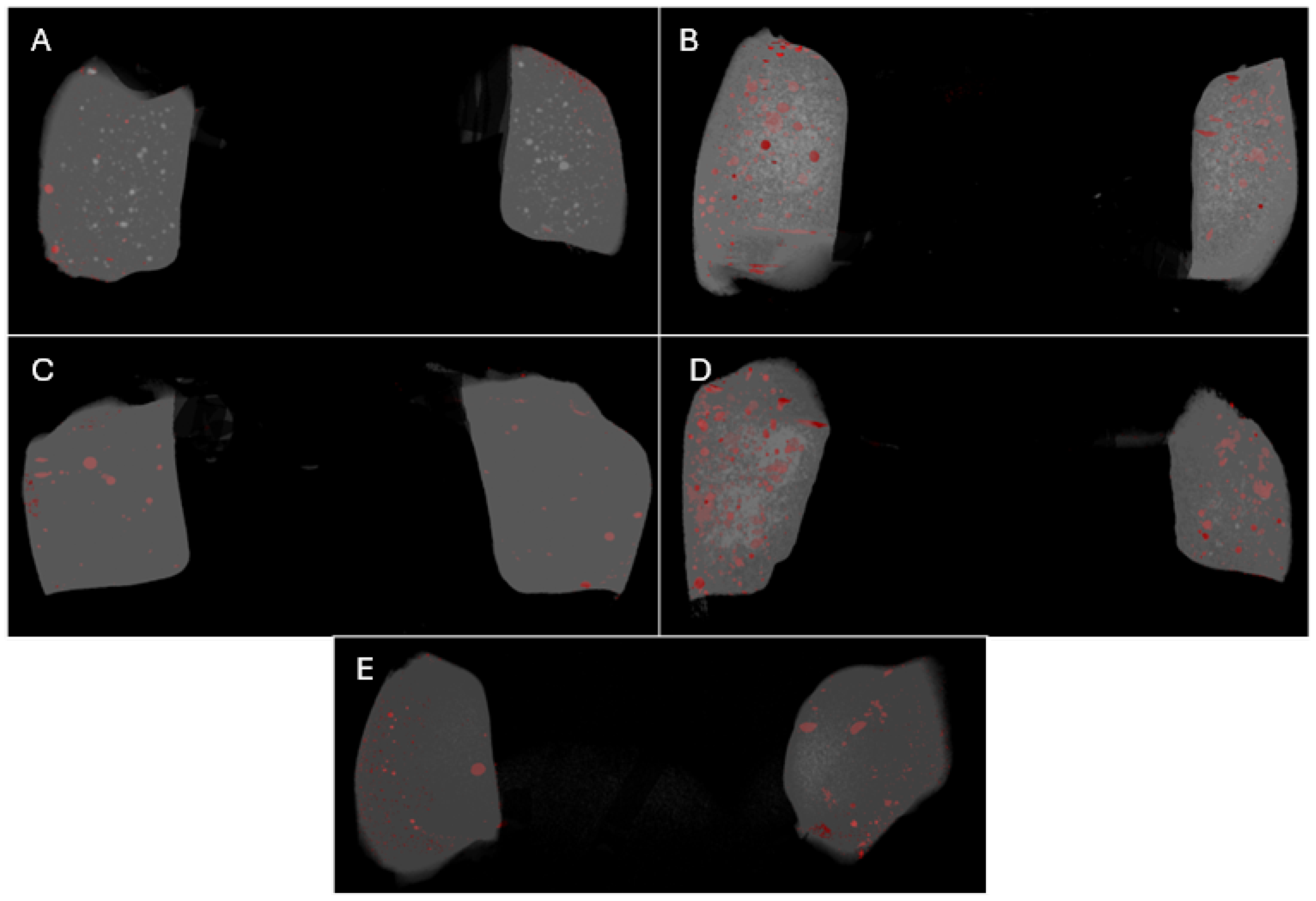
2.4. Void Analysis
2.5. Sample Size Calculation, Statistical Methods, and Data Processing
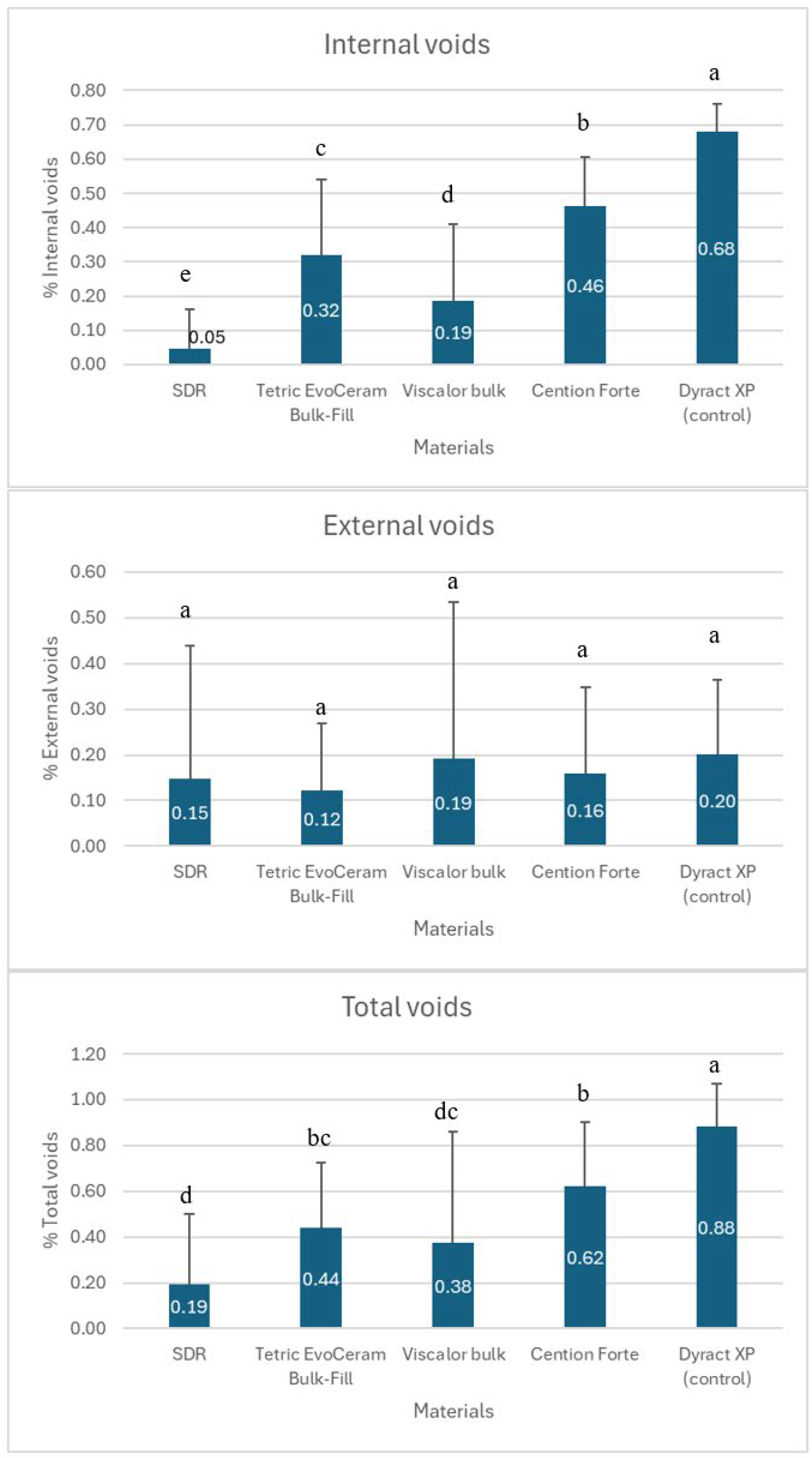
3. Results
4. Discussion
5. Conclusions
- Key Points:
- -
- The SDR bulk-fill composite exhibited the fewest internal voids, suggesting superior adaptation within the restoration bulk in primary molars.
- -
- External void formation was comparable across all tested bulk-fill materials, indicating that no single material offers a significant advantage in interfacial adaptation.
- -
- The low overall void percentages (expressed as the percentage of the total restoration volume) support the clinical viability of bulk-fill composites for class II restorations in pediatric dentistry, offering efficiency and reduced technique sensitivity.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arbildo-Vega, H.I.; Lapinska, B.; Panda, S.; Lamas-Lara, C.; Khan, A.S.; Lukomska-Szymanska, M. Clinical Effectiveness of Bulk-Fill and Conventional Resin Composite Restorations: Systematic Review and Meta-Analysis. Polymers 2020, 12, 1786. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekhar, V.; Rudrapati, L.; Badami, V.; Tummala, M. Incremental techniques in direct composite restoration. J. Conserv. Dent. 2017, 20, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Aminian, A.; Leven, A.J.; Ashley, M.P. Clinical considerations in the application of direct composite for tooth wear. Br. Dent. J. 2023, 234, 400–405. [Google Scholar] [CrossRef]
- Yadav, R.; Sonwal, S.; Sharma, R.P.; Saini, S.; Huh, Y.S.; Brambilla, E.; Ionescu, A.C. Ranking Analysis of Tribological, Mechanical, and Thermal Properties of Nano Hydroxyapatite Filled Dental Restorative Composite Materials Using the R-Method. Polym. Adv. Technol. 2024, 35, e70010. [Google Scholar] [CrossRef]
- Park, J.; Chang, J.; Ferracane, J.; Lee, I.B. How should composite be layered to reduce shrinkage stress: Incremental or bulk filling? Dent. Mater. 2008, 24, 1501–1505. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.; AlKhalefah, A.; Alsaghirat, A.; Alburayh, R.; Alabdullah, N. Comparison between Different Bulk-Fill and Incremental Composite Materials Used for Class II Restorations in Primary and Permanent Teeth: In Vitro Assessments. Materials 2023, 16, 6674. [Google Scholar] [CrossRef]
- Kwon, Y.; Ferracane, J.; Lee, I.B. Effect of layering methods, composite type, and flowable liner on the polymerization shrinkage stress of light cured composites. Dent. Mater. 2012, 28, 801–809. [Google Scholar] [CrossRef]
- Parra Gatica, E.; Duran Ojeda, G.; Wendler, M. Contemporary flowable bulk-fill resin-based composites: A systematic review. Biomater. Investig. Dent. 2023, 10, 8–19. [Google Scholar] [CrossRef]
- Benetti, A.R.; Havndrup-Pedersen, C.; Honoré, D.; Pedersen, M.K.; Pallesen, U. Bulk-fill resin composites: Polymerization contraction, depth of cure, and gap formation. Oper. Dent. 2015, 40, 190–200. [Google Scholar] [CrossRef]
- Van Ende, A.; De Munck, J.; Lise, D.P.; Van Meerbeek, B. Bulk-Fill Composites: A Review of the Current Literature. J. Adhes. Dent. 2017, 19, 95–109. [Google Scholar] [CrossRef]
- Lalovic, M.; Kolak, V.; Melih, I.; Nikitovic, A.; Trajkovic, I.; Milosevic, M.; Pejanovic, D.; Pesic, D. Mechanical properties of ion-releasing restorative materials. Am. J. Dent. 2024, 37, 13–18. [Google Scholar] [PubMed]
- Abouelleil, H.; Attik, N.; Chiriac, R.; Toche, F.; Ory, A.; Zayakh, A.; Grosgogeat, B.; Pradelle-Plasse, N. Comparative study of two bioactive dental materials. Dent. Mater. 2024, 40, 297–306. [Google Scholar] [CrossRef]
- Niem, T.; Frankenberger, R.; Amend, S.; Wöstmann, B.; Krämer, N. Damping Behaviour and Mechanical Properties of Restorative Materials for Primary Teeth. Materials 2022, 15, 7698. [Google Scholar] [CrossRef] [PubMed]
- Gjorgievska, E.; Oh, D.S.; Haam, D.; Gabric, D.; Coleman, N.J. Evaluation of Efficiency of Polymerization, Surface Roughness, Porosity and Adaptation of Flowable and Sculptable Bulk Fill Composite Resins. Molecules 2021, 26, 5202. [Google Scholar] [CrossRef] [PubMed]
- Paganini, A.; Attin, T.; Tauböck, T.T. Margin Integrity of Bulk-Fill Composite Restorations in Primary Teeth. Materials 2020, 13, 3802. [Google Scholar] [CrossRef]
- Al-Zain, A.O.; Baeesa, L.; Jassoma, E.; Alghilan, M.A.; Hariri, M.; Ismail, E.H.; Münchow, E.A. Assessment of internal porosities for different placement techniques of bulk-fill resin-based composites: A micro-computed tomography study. Clin. Oral. Investig. 2023, 27, 7489–7499. [Google Scholar] [CrossRef]
- Soares, B.M.; Barbosa, M.P.; de Almeida, R.V.; Jardim, R.N.; da Silva, E.M. Marginal integrity and physicomechanical properties of a thermoviscous and regular bulk-fill resin composites. Clin. Oral. Investig. 2024, 28, 496. [Google Scholar] [CrossRef]
- Sá, V.A.; Bittencourt, H.R.; Burnett Júnior, L.H.; Spohr, A.M. Preheated and Injected Bulk-Fill Resin Composites: A Micro-CT Analysis of Internal Voids and Marginal Adaptation in Class II Restorations. Materials 2025, 18, 327. [Google Scholar] [CrossRef]
- Pascon, F.M.; Kantovitz, K.R.; Caldo-Teixeira, A.S.; Borges, A.F.; Silva, T.N.; Puppin-Rontani, R.M.; Garcia-Godoy, F. Clinical evaluation of composite and compomer restorations in primary teeth: 24-month results. J. Dent. 2006, 34, 381–388. [Google Scholar] [CrossRef]
- Krämer, N.; Frankenberger, R. Compomers in restorative therapy of children: A literature review. Int. J. Paediatr. Dent. 2007, 17, 2–9. [Google Scholar] [CrossRef]
- Papagiannoulis, L.; Kakaboura, A.; Pantaleon, F.; Kavvadia, K. Clinical evaluation of a polyacid-modified resin composite (compomer) in Class II restorations of primary teeth: A two-year follow-up study. Pediatr. Dent. 1999, 21, 231–234. [Google Scholar] [PubMed]
- Hamza, B.; Zimmerman, M.; Attin, T.; Tauböck, T.T. Marginal integrity of classical and bulk-fill composite restorations in permanent and primary molars. Sci. Rep. 2022, 12, 13670. [Google Scholar] [CrossRef]
- Gaintantzopoulou, M.D.; Gopinath, V.K.; Zinelis, S. Evaluation of cavity wall adaptation of bulk esthetic materials to restore class II cavities in primary molars. Clin. Oral Investig. 2017, 21, 1063–1070. [Google Scholar] [CrossRef]
- Pardo Díaz, C.A.; Shimokawa, C.; Sampaio, C.S.; Freitas, A.Z.; Turbino, M.L. Characterization and Comparative Analysis of Voids in Class II Composite Resin Restorations by Optical Coherence Tomography. Oper. Dent. 2020, 45, 71–79. [Google Scholar] [CrossRef]
- Osiewicz, M.A.; Werner, A.; Roeters, F.J.M.; Kleverlaan, C.J. Wear of bulk-fill resin composites. Dent. Mater. 2022, 38, 549–553. [Google Scholar] [CrossRef]
- Miletic, V.; Pongprueksa, P.; De Munck, J.; Brooks, N.R.; Van Meerbeek, B. Curing characteristics of flowable and sculptable bulk-fill composites. Clin. Oral Investig. 2017, 21, 1201–1212. [Google Scholar] [CrossRef] [PubMed]
- Schulze, K.A.; Zaman, A.A.; Söderholm, K.J. Effect of filler fraction on strength, viscosity and porosity of experimental compomer materials. J. Dent. 2003, 31, 373–382. [Google Scholar] [CrossRef]
- Loumprinis, N.; Maier, E.; Belli, R.; Petschelt, A.; Eliades, G.; Lohbauer, U. Viscosity and stickiness of dental resin composites at elevated temperatures. Dent. Mater. 2021, 37, 413–422. [Google Scholar] [CrossRef]
- Lee, J.H.; Um, C.M.; Lee, I.B. Rheological properties of resin composites according to variations in monomer and filler composition. Dent. Mater. 2006, 22, 515–526. [Google Scholar] [CrossRef]
- Tosco, V.; Vitiello, F.; Furlani, M.; Gatto, M.L.; Monterubbianesi, R.; Giuliani, A.; Orsini, G.; Putignano, A. Microleakage Analysis of Different Bulk-Filling Techniques for Class II Restorations: µ-CT, SEM and EDS Evaluations. Materials 2020, 14, 31. [Google Scholar] [CrossRef]
- Sampaio, C.S.; Fernández Arias, J.; Atria, P.J.; Cáceres, E.; Pardo Díaz, C.; Freitas, A.Z.; Hirata, R. Volumetric polymerization shrinkage and its comparison to internal adaptation in bulk fill and conventional composites: A μCT and OCT in vitro analysis. Dent. Mater. 2019, 35, 1568–1575. [Google Scholar] [CrossRef] [PubMed]
- Bolding, K.H.; Hill, A.E.; Tantbirojn, D.; Versluis, A. Prewarming effect on adaptation, porosities, and strength of a composite resin. J. Mech. Behav. Biomed. Mater. 2023, 143, 105913. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatric Dentistry; Clinical Affairs Committee—Restorative Dentistry Subcommittee. Guideline on pediatric restorative dentistry. Pediatr. Dent. 2012, 34, 173–180. [Google Scholar]
- Demirel, G.; Orhan, A.I.; Irmak, Ö.; Aydin, F.; Buyuksungur, A.; Bilecenoğlu, B.; Orhan, K. Micro-computed tomographic evaluation of the effects of pre-heating and sonic delivery on the internal void formation of bulk-fill composites. Dent. Mater. J. 2021, 40, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Fronza, B.M.; Rueggeberg, F.A.; Braga, R.R.; Mogilevych, B.; Soares, L.E.; Martin, A.A.; Ambrosano, G.; Giannini, M. Monomer conversion, microhardness, internal marginal adaptation, and shrinkage stress of bulk-fill resin composites. Dent. Mater. 2015, 31, 1542–1551. [Google Scholar] [CrossRef]
- Rummani, G.; Ide, K.; Hosaka, K.; Tichy, A.; Abdou, A.; Otsuki, M.; Nakajima, M. Regional ultimate tensile strength and water sorption/solubility of bulk-fill and conventional resin composites: The effect of long-term water storage. Dent. Mater. J. 2021, 40, 1394–1402. [Google Scholar] [CrossRef]
| Groups | Manufacturer | Restorative Technique | Viscosity | Composition |
|---|---|---|---|---|
| Group 1 SDR | Dentsply Sirona, Konstanz, Germany | The material was injected directly into the cavity from the compule at room temperature. The tip of the compule was placed in contact with the gingival base, and the material was extruded using the bulk-fill technique. | Low-viscosity bulk-fill resin composite | Modified UDMA, TEGDMA, dimethacrylate and trimethacrylate resin, silanated bariumalumino-fluoroborosilicate glass, silanated strontium alumino-fluoro-silicate glass, surface treated fume silicas, ytterbium fluoride, synthetic inorganic iron oxide pigments, and titanium dioxide |
| Group 2 Tetric EvoCeram bulk-fill | Ivoclar Vivadent, Schaan, Liechtenstein | The material was applied in one portion with the bulk-fill technique and condensed and shaped using modeling instruments (OptraSculpt & OptraSculpt Pad System Kit, Ivoclar Vivadent, Schaan, Liechtenstein). | High-viscosity bulk-fill resin composite | Bisphenol-A-glycidylmethacrylat (Bis-GMA), Bis-EMA, and barium glass filler |
| Group 3 Viscalor bulk | VOCO, Cuxhaven, Germany | The composite was preheated using its specialized heating gun and injected directly from the compule into the cavity using bulk-fill technique. | Thermoviscous bulk-fill resin composite | Bis-GMA, aliphatic dimethacrylate, and inorganic filler |
| Group 4 Cention Forte | Ivoclar Vivadent, Schaan, Liechtenstein | The material was prepared in a capsule mixer for 15 s and applied directly from the capsule with a capsule gun using the bulk-fill technique. Then, it was shaped with an Optrasculpt modeling instrument. | Moderate-viscosity alkasite material | Calcium-fluoro-silicate glass, barium-aluminosilicate glass, ytterbium trifluoride, copper salt and thiocarbamide-self cure initiator (Ivocerin), acyl phosphine oxidephotoinitiator, pigment, urethane dimethacrylate (UDMA), tetramethyl xylylendiurethane dimethacrylate, tricyclodecandimethanol dimethacrylate (DCP), polyethylene glycol 400 dimethacrylate (PEG400 DMA), initiator (hydroperoxide—self-curing), and stabilizer |
| Group 5 Dyract XP (control) | Dentsply Sirona, Konstanz, Germany | The material was applied from the compule in two layers of 2 mm, condensed and shaped with Optrasculpt modeling instrument. | High-viscosity compomer material | UDMA, carboxylic acid modified dimethacrylate, TEGDMA, trimethacrylate resin (TMPTMA), dimethacrylate resins, camphorquinone, ethyl-4 (dimethylamino) benzoate, butylated hydroxy toluene (BHT), strontium-alumino-sodium-fluoro phosphor-silicate glass, highly dispersed silicon dioxide, strontium fluoride, iron oxide pigments, and titanium oxide pigments |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gigova, R.; Hristov, K. Micro-CT Assessment of Internal and External Void Formation in Class II Restorations of Primary Molars Using Bulk-Fill Composites. Materials 2025, 18, 2621. https://doi.org/10.3390/ma18112621
Gigova R, Hristov K. Micro-CT Assessment of Internal and External Void Formation in Class II Restorations of Primary Molars Using Bulk-Fill Composites. Materials. 2025; 18(11):2621. https://doi.org/10.3390/ma18112621
Chicago/Turabian StyleGigova, Ralitsa, and Krasimir Hristov. 2025. "Micro-CT Assessment of Internal and External Void Formation in Class II Restorations of Primary Molars Using Bulk-Fill Composites" Materials 18, no. 11: 2621. https://doi.org/10.3390/ma18112621
APA StyleGigova, R., & Hristov, K. (2025). Micro-CT Assessment of Internal and External Void Formation in Class II Restorations of Primary Molars Using Bulk-Fill Composites. Materials, 18(11), 2621. https://doi.org/10.3390/ma18112621





