Dental Casts for Fixed Dental Prostheses Printed with SLA Technology: Influence of External Shell Thickness and Printing Orientation
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- For casts printed using an SLA 3D printer intended for fixed dental prostheses, print orientation did not appear to influence the overall accuracy (trueness and precision) of the casts under the conditions described.
- The shell thickness of the master casts, as tested with the SLA printer, did not affect the overall accuracy. However, when analyzing specific reference points, casts with a 2 mm shell thickness demonstrated better trueness than those with a 4 mm thickness.
- All printed casts achieved trueness values ranging from 73.9 µm to 193.4 µm, which is considered clinically acceptable.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mangano, F.G.; Hauschild, U.; Veronesi, G.; Imburgia, M.; Mangano, C.; Admakin, O. Trueness and precision of 5 intraoral scanners in the impressions of single and multiple implants: A comparative in vitro study. BMC Oral Health 2019, 19, 101. [Google Scholar] [CrossRef] [PubMed]
- Albdour, E.A.; Shaheen, E.; Vranckx, M.; Mangano, F.G.; Politis, C.; Jacobs, R. A novel in vivo method to evaluate trueness of digital impressions. BMC Oral Health 2018, 18, 117. [Google Scholar] [CrossRef] [PubMed]
- Nowak, R.; Wesemann, C.; Robben, J.; Muallah, J.; Bumann, A. An in-vitro study comparing the accuracy of full-arch casts digitized with desktop scanners. Quintessence Int. 2017, 48, 667–676. [Google Scholar]
- van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef]
- Revilla-León, M.; Sadeghpour, M.; Özcan, M. An update on applications of 3D printing technologies used for processing polymers used in implant dentistry. Odontology 2020, 108, 331–338. [Google Scholar] [CrossRef]
- Rutkūnas, V.; Gedrimienė, A.; Auškalnis, L.; Admakin, O.; Mangano, F. Accuracy of fixed implant-supported dental prostheses additively manufactured by metal, ceramic, or polymer: A systematic review. J. Prosthodont. 2022, 31 (Suppl. 1), 70–87. [Google Scholar] [CrossRef]
- Horn, T.J.; Harrysson, O.L.A. Overview of current additive manufacturing technologies and selected applications. Sci. Prog. 2012, 95, 255–282. [Google Scholar] [CrossRef]
- Martelli, N.; Serrano, C.; van den Brink, H.; Pineau, J.; Prognon, P.; Borget, I.; El Batti, S. Advantages and disadvantages of 3-dimensional printing in surgery: A systematic review. Surgery 2016, 159, 1485–1500. [Google Scholar] [CrossRef]
- Oberoi, G.; Nitsch, S.; Edelmayer, M.; Janjić, K.; Müller, A.S.; Agis, H. 3D printing—Encompassing the facets of dentistry. Front. Bioeng. Biotechnol. 2018, 6, 172. [Google Scholar] [CrossRef]
- Barazanchi, A.; Li, K.C.; Al-Amleh, B.; Lyons, K.; Waddell, J.N. Additive technology: Update on current materials and applications in dentistry. J. Prosthodont. 2017, 26, 156–163. [Google Scholar] [CrossRef]
- Revilla-León, M.; Meyer, M.J.; Özcan, M. Metal additive manufacturing technologies: Literature review of current status and prosthodontic applications. Int. J. Comput. Dent. 2019, 22, 55–67. [Google Scholar] [PubMed]
- Pradíes, G.; Morón-Conejo, B.; Martínez-Rus, F.; Salido, M.P.; Berrendero, S. Current applications of 3D printing in dental implantology: A scoping review mapping the evidence. Clin. Oral Implant. Res. 2023, 35, 1011–1032. [Google Scholar] [CrossRef] [PubMed]
- Alexander, A.E.; Wake, N.; Chepelev, L.; Brantner, P.; Ryan, J.; Wang, K.C. A guideline for 3D printing terminology in biomedical research utilizing ISO/ASTM standards. 3D Print. Med. 2021, 7, 8. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Özcan, M. Additive manufacturing technologies used for processing polymers: Current status and potential application in prosthetic dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef]
- Alharbi, N.; Wismeijer, D.; Osman, R.B. Additive manufacturing techniques in prosthodontics: Where do we currently stand? A critical review. Int. J. Prosthodont. 2017, 30, 474–484. [Google Scholar] [CrossRef]
- Beguma, Z.; Chhedat, P. Rapid prototyping—When virtual meets reality. Int. J. Comput. Dent. 2014, 17, 297–306. [Google Scholar]
- Dawood, A.; Marti Marti, B.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]
- Ide, Y.; Nayar, S.; Logan, H.; Gallagher, B.; Wolfaardt, J. The effect of the angle of acuteness of additive manufactured models and the direction of printing on the dimensional fidelity: Clinical implications. Odontology 2017, 105, 108–115. [Google Scholar] [CrossRef]
- Wu, D.; Zhao, Z.; Zhang, Q.; Qi, H.J.; Fang, D. Mechanics of shape distortion of DLP 3D printed structures during UV post-curing. Soft Matter 2019, 15, 6151–6159. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef]
- ISO/ASTM 52900:2021; Additive Manufacturing—General Principles—Fundamentals and Vocabulary. International Organization for Standardization: Geneva, Switzerland; ASTM, Committee F42 on Additive Manufacturing Technologies: West Conshohocken, PA, USA, 2021. Available online: https://www.iso.org/standard/74514.html (accessed on 20 July 2024).
- ISO 5725-1:2023; Accuracy (Trueness and Precision) of Measurement Methods and Results—Part 1: General Principles and Definitions. International Organization for Standardization: Geneva, Switzerland, 2023. Available online: https://www.iso.org/standard/69418.html (accessed on 20 July 2024).
- ISO 20896-1:2019; Dentistry—Digital Impression Devices—Part 1: Methods for Assessing Accuracy. International Organization for Standardization: Geneva, Switzerland, 2019. Available online: https://www.iso.org/standard/69402.html (accessed on 20 July 2024).
- Bartkowiak, T.; Peta, K.; Królczyk, J.B.; Niesłony, P.; Bogdan-Chudy, M.; Przeszłowski, Ł.; Trych-Wildner, A.; Wojciechowska, N.; Królczyk, G.M.; Wieczorowski, M. Wetting properties of polymer additively manufactured surfaces—Multiscale and multi-technique study into the surface-measurement-function interactions. Tribol. Int. 2025, 202, 110394. [Google Scholar] [CrossRef]
- García-Gil, I.; Rodríguez Alonso, V.; Suárez, C.L.; Mosaddad, S.A.; Peláez, J.; Suárez, M.J. Influence of the print orientation and cast thickness on the accuracy of DLP master casts for fixed dental prostheses. BMC Oral Health 2025, 25, 532. [Google Scholar] [CrossRef] [PubMed]
- Paranna, S.; Thosar, N.; Kanitkar, A. Effect of build orientation on mechanical and physical properties of additively manufactured resins using digital light processing technology in dentistry: A systematic review. J. Contemp. Dent. Pract. 2024, 25, 891–903. [Google Scholar]
- Horoz, S.; Palaz, C.H.; Meric, G. Mechanical properties of 3D-printed resin with various printing orientation. Int. Dent. J. 2024, 74, S7. [Google Scholar] [CrossRef]
- Alghauli, M.A.; Almuzaini, S.A.; Aljohani, R.; Alqutaibi, A.Y. Impact of 3D printing orientation on accuracy, properties, cost, and time efficiency of additively manufactured dental models: A systematic review. BMC Oral Health 2024, 24, 1550. [Google Scholar] [CrossRef]
- Piedra-Cascón, W.; Pérez-López, J.; Veiga-López, B.; Oteo-Morilla, C.; Pose-Rodriguez, J.M.; Gallas-Torreira, M. Influence of base designs on the manufacturing accuracy of vat-polymerized diagnostic casts using two different technologies. J. Prosthet. Dent. 2024, 132, 453.e1–453.e9. [Google Scholar] [CrossRef]
- Bennett, G.W.; DiGiovanni, T. Effect of wall thickness of 3D-printed models on resisting deformation from thermal forming in-office aligners. Clin. Exp. Dent. Res. 2024, 10, e827. [Google Scholar] [CrossRef]
- Vincze, Z.É.; Kovács, Z.I.; Vass, A.F.; Borbély, J.; Márton, K. Evaluation of the dimensional stability of 3D-printed dental casts. J. Dent. 2024, 151, 105431. [Google Scholar] [CrossRef]
- Shin, S.-H.; Kwon, J.-S.; Shim, J.-S.; Kim, J.-E. Evaluating the three-dimensional printing accuracy of partial-arch models according to outer wall thickness: An in vitro study. Materials 2021, 14, 6734. [Google Scholar] [CrossRef]
- Perlea, P.; Stefanescu, C.; Dalaban, M.G.; Petre, A.E. Experimental study on dimensional variations of 3D printed dental models based on printing orientation. Clin. Case Rep. 2024, 12, e8630. [Google Scholar] [CrossRef]
- ElShebiny, T.; Matthaios, S.; Menezes, L.M.; Tsolakis, I.A.; Palomo, J.M. Effect of printing technology, layer height, and orientation on assessment of 3D-printed models. J. World Fed. Orthod. 2024, 13, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Demirel, M.; Diken Türksayar, A.A.; Donmez, M.B.; Yilmaz, B. Effect of 3D printing technology and print orientation on the trueness of additively manufactured definitive casts with different tooth preparations. J. Dent. 2024, 148, 105244. [Google Scholar] [CrossRef] [PubMed]
- Short, M.M.; Favero, C.S.; English, J.D.; Kasper, F.K. Impact of orientation on dimensional accuracy of 3D-printed orthodontic models. J. Clin. Orthod. 2018, 52, 13–20. [Google Scholar] [PubMed]
- Favero, C.S.; English, J.D.; Cozad, B.E.; Wirthlin, J.O.; Short, M.M.; Kasper, F.K. Effect of print layer height and printer type on the accuracy of 3-dimensional printed orthodontic models. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 557–565. [Google Scholar] [CrossRef]
- Yang, M.S.; Kim, S.K.; Heo, S.J.; Koak, J.Y.; Park, J.M. Investigation of the marginal fit of a 3D-printed three-unit resin prosthesis with different build orientations and layer thicknesses. J. Adv. Prosthodont. 2022, 14, 250–261. [Google Scholar] [CrossRef]
- Park, M.E.; Shin, S.Y. Three-dimensional comparative study on the accuracy and reproducibility of dental casts fabricated by 3D printers. J. Prosthet. Dent. 2018, 119, 861.e1–861.e7. [Google Scholar] [CrossRef]
- Mangano, F.G.; Admakin, O.; Bonacina, M.; Biaggini, F.; Farronato, D.; Lerner, H. Accuracy of 6 desktop 3D printers in dentistry: A comparative in vitro study. Eur. J. Prosthodont. Restor. Dent. 2020, 28, 75–85. [Google Scholar]
- Joda, T.; Matthisson, L.; Zitzmann, N.U. Impact of aging on the accuracy of 3D-printed dental models: An in vitro investigation. J. Clin. Med. 2020, 9, 1436. [Google Scholar] [CrossRef]
- Hazeveld, A.; Huddleston Slater, J.J.R.; Ren, Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 108–115. [Google Scholar] [CrossRef]
- Park, J.M.; Jeon, J.; Koak, J.Y.; Kim, S.K.; Heo, S.J. Dimensional accuracy and surface characteristics of 3D-printed dental casts. J. Prosthet. Dent. 2021, 126, 427–437. [Google Scholar] [CrossRef]
- Keating, A.P.; Knox, J.; Bibb, R.; Zhurov, A.I. A comparison of plaster, digital and reconstructed study model accuracy. J. Orthod. 2008, 35, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Meyers, M.J.; Zandinejad, A.; Özcan, M. A review on chemical composition, mechanical properties, and manufacturing work flow of additively manufactured current polymers for interim dental restorations. J. Esthet. Restor. Dent. 2019, 31, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Osman, R.B.; Wismeijer, D. Factors influencing the dimensional accuracy of 3D-printed full-coverage dental restorations using stereolithography technology. Int. J. Prosthodont. 2016, 29, 503–510. [Google Scholar] [CrossRef] [PubMed]
- W, P.C.; Vr, K.; W, A.; M, R.L. 3D printing parameters, supporting structures, slicing, and post-processing procedures of vat-polymerization additive manufacturing technologies: A narrative review. J. Dent. 2021, 109, 103630. [Google Scholar]
- Maneiro Lojo, J.; Alonso Pérez-Barquero, J.; García-Sala Bonmatí, F.; Agustín-Panadero, R.; Yilmaz, B.; Revilla-León, M. Influence of print orientation on the accuracy (trueness and precision) of diagnostic casts manufactured with a daylight polymer printer. J. Prosthet. Dent. 2023, 132, 1314–1322. [Google Scholar] [CrossRef]
- Revilla-León, M.; Piedra-Cascón, W.; Methani, M.M.; Barmak, B.A.; Att, W. Influence of the base design on the accuracy of additive manufactured casts measured using a coordinate measuring machine. J. Prosthodont. Res. 2022, 66, 68–74. [Google Scholar] [CrossRef]
- Morón-Conejo, B.; López-Vilagran, J.; Cáceres, D.; Berrendero, S.; Pradíes, G. Accuracy of five different 3D printing workflows for dental models comparing industrial and dental desktop printers. Clin. Oral Investig. 2023, 27, 2521–2532. [Google Scholar] [CrossRef]
- Kim, S.Y.; Shin, Y.S.; Jung, H.D.; Hwang, C.J.; Baik, H.S.; Cha, J.Y. Precision and trueness of dental models manufactured with different 3-dimensional printing techniques. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 144–153. [Google Scholar] [CrossRef]
- Brown, G.B.; Currier, G.F.; Kadioglu, O.; Kierl, J.P. Accuracy of 3-dimensional printed dental models reconstructed from digital intraoral impressions. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 733–739. [Google Scholar] [CrossRef]
- Jin, S.J.; Jeong, I.D.; Kim, J.H.; Kim, W.C. Accuracy (trueness and precision) of dental models fabricated using additive manufacturing methods. Int. J. Comput. Dent. 2018, 21, 107–113. [Google Scholar]
- Rebong, R.E.; Stewart, K.T.; Utreja, A.; Ghoneima, A.A. Accuracy of three-dimensional dental resin models created by fused deposition modeling, stereolithography, and Polyjet prototype technologies: A comparative study. Angle Orthod. 2018, 88, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.A.; Ender, A.; Baumgartner, S.; Mehl, A. A validation study of reconstructed rapid prototyping models produced by two technologies. Angle Orthod. 2017, 87, 782–787. [Google Scholar] [CrossRef] [PubMed]
- Camardella, L.T.; de Vasconcellos Vilella, O.; Breuning, H. Accuracy of printed dental models made with 2 prototype technologies and different designs of model bases. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1178–1187. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Diagnostic accuracy and measurement sensitivity of digital models for orthodontic purposes: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 161–170. [Google Scholar] [CrossRef]
- De Luca Canto, G.; Pachêco-Pereira, C.; Lagravere, M.O.; Flores-Mir, C.; Major, P.W. Intra-arch dimensional measurement validity of laser-scanned digital dental models compared with the original plaster models: A systematic review. Orthod. Craniofac. Res. 2015, 18, 65–76. [Google Scholar] [CrossRef]



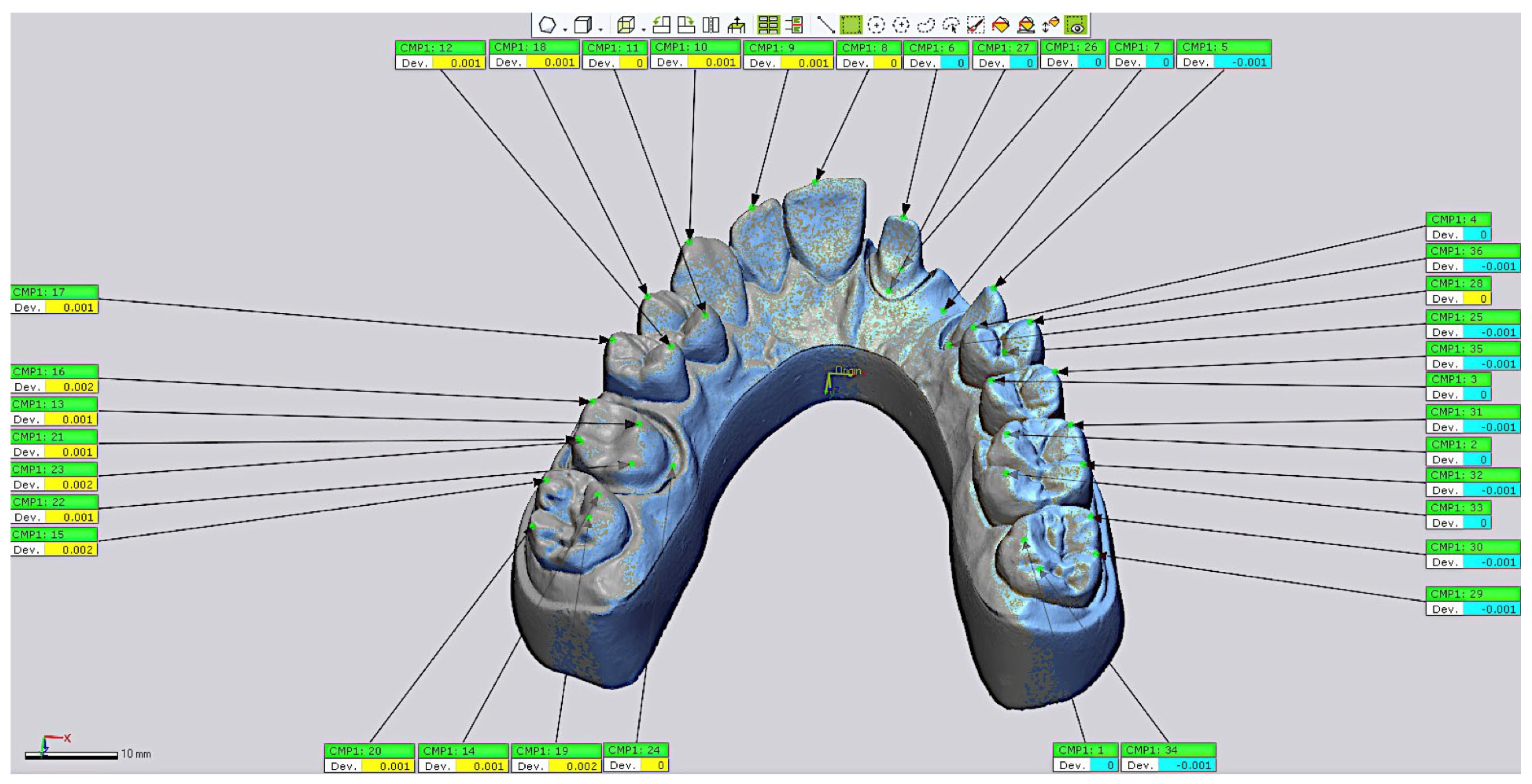

| Tooth | Points |
|---|---|
| 17 | 14 (palatal cusp), 15 (buccal cusp), 19 (palatal cusp), 20 (buccal cusp) |
| 16 | 13 (palatal mesial cusp), 16 (buccal mesial cusp), 21 (buccal distal cusp), 22 (palatal mesial cusp), 23 (buccal finish line), 24 (palatal finish line) |
| 15 | 12 (palatal cusp), 17 (buccal cusp) |
| 14 | 11 (palatal cusp), 18 (buccal cusp) |
| 13 | 10 |
| 12 | 9 |
| 11 | 8 |
| 21 | 6 (incisal edge), 26 (buccal finish line), 27 (palatal finish line) |
| 22 | 7 |
| 23 | 5 (incisal edge), 25 (buccal finish line), 28 (palatal finish line) |
| 24 | 4 (palatal cusp), 36 (buccal cusp) |
| 25 | 3 (palatal cusp), 35 (buccal cusp) |
| 26 | 2 (palatal cusp), 31 (buccal cusp), 32 (buccal cusp), 33 (palatal cusp) |
| 27 | 1 (palatal cusp), 29 (buccal cusp), 30 (buccal cusp), 34 (palatal cusp) |
| Groups | minDV | maxDV | RMS |
|---|---|---|---|
| Group 1 | (−0.342 ± 0.0741) | (0.23 ± 0.0904) | (0.133 ± 0.0383) |
| Group 2 | (−0.29 ± 0.0996) | (0.168 ± 0.079) | (0.116 ± 0.0421) |
| Group 3 | (−0.324 ± 0.074) | (0.189 ± 0.0468) | (0.126 ± 0.0273) |
| Group 4 | (−0.299 ± 0.0566) | (0.195 ± 0.0681) | (0.127 ± 0.0236) |
| Group 5 | (−0.31 ± 0.0545) | (0.187 ± 0.0592) | (0.133 ± 0.0191) |
| Group 6 | (−0.375 ± 0.0994) | (0.273 ± 0.137) | (0.151 ± 0.0424) |
| Groups | RMS (p-Value) |
|---|---|
| G1 > G4 | TDabs2 (p = 0.0209), TDabs3 (p = 0.0120), TDabs5 (p = 0.0005), TDabs6 (p = 0.0061), TDabs7 (p = 0.0047), TDabs8 (p = 0.0463), TDabs12 (p = 0.0061), TDabs35 (p = 0.0327) |
| G1 < G4 | TDabs1 (p = 0.0130) |
| G2 > G5 | TDabs2 (p = 0.0008), TDabs3 (p = 0.0004), TDabs5 (p < 0.0001), TDabs6 (p = 0.0012), TDabs8 (p = 0.0165), TDabs12 (p < 0.0001), TDab35 (p = 0.0039), TDab36 (p = 0.0350) |
| G2 < G5 | TDabs25 (p = 0.0042) |
| G3 > G6 | TDabs2 (p = 0.0350), TDabs3 (p = 0.0079), TDabs5 (p = 0.0032), TDabs6 (p = 0.0047), TDabs7 (p = 0.0032), TDabs8 (p = 0.0209), TDabs11 (p = 0.0012), TDabs12 (p = 0.0043), TDabs13 (p = 0.0032), TDabs24 (p = 0.0403), TDab35 (p = 0.0282) |
| G3 < G6 | TDabs1 (p = 0.0079), TDabs25 (p = 0.0350) |
| G3 > G5 > G6 | TDabs2 (p = 0.0357) |
| Groups | RMS | X axis | Y Axis | Z Axis |
|---|---|---|---|---|
| G1 > G4 | TDabs5 (p = 0.0005), TDabs6 (p = 0.0061) | Xabs5 (p = 0.0003), Xabs6 (p = 0.0078), | Yabs5 (p = 0.0003), Yabs6 (p = 0.0066) Yabs7 (p = 0.0046) Yabs13 (p = 0.0395) Yabs28 (p = 0.037) | Zabs5 (p = 0.0003), Zabs6 (p = 0.0066) Zabs7 (p < 0.001) Zabs13 (p = 0.0376) |
| G1 < G4 | TDabs7 (p = 0.006) | Xabs7 (p = 0.0038) Xabs13 (p = 0.0293) Xabs28 (p = 0.049) | Zabs28 (p = 0.047) | |
| G2 > G5 | TDabs5 (p < 0.001), TDabs6 (p < 0.001) | Xabs5 (p < 0.001), Xabs6 (p < 0.001) | Yabs5 (p < 0.001), Yabs6 (p < 0.001) | Zabs5 (p < 0.001), Zabs6 (p < 0.001) |
| G2 < G5 | TDabs25 (p < 0.001) | Xabs25 (p < 0.001) | Yabs25 (p < 0.001) | Zabs25 (p < 0.001) |
| G3 > G6 | TDabs5 (p < 0.001), TDabs6 (p < 0.001) TDabs7 (p < 0.001) TDabs13 (p < 0.001) TDabs24 (p = 0.0403) | Xabs5 (p < 0.001), Xabs6 (p < 0.001) Xabs7 (p < 0.001) Xabs13 (p < 0.01) Xabs24 (p = 0.0403) | Yabs5(p < 0.001), Yabs6 (p < 0.001) Yabs7 (p < 0.001) Yabs13 (p < 0.001) Yabs24 (p = 0.0403) Yabs25 (p = 0.035) | Zabs5 (p < 0.001), Zabs6 (p < 0.001) Zabs13 (p < 0.001) Zabs24 (p = 0.0403) |
| G3 < G6 | TDabs25 (p = 0.035) | Xabs25 (p = 0.035) | Zabs25 (p = 0.035) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Gil, I.; Rodríguez Alonso, V.; Tobar Arribas, C.; Mosaddad, S.A.; Peláez, J.; Suárez, M.J. Dental Casts for Fixed Dental Prostheses Printed with SLA Technology: Influence of External Shell Thickness and Printing Orientation. Materials 2025, 18, 2246. https://doi.org/10.3390/ma18102246
García-Gil I, Rodríguez Alonso V, Tobar Arribas C, Mosaddad SA, Peláez J, Suárez MJ. Dental Casts for Fixed Dental Prostheses Printed with SLA Technology: Influence of External Shell Thickness and Printing Orientation. Materials. 2025; 18(10):2246. https://doi.org/10.3390/ma18102246
Chicago/Turabian StyleGarcía-Gil, Ignacio, Verónica Rodríguez Alonso, Celia Tobar Arribas, Seyed Ali Mosaddad, Jesús Peláez, and María J. Suárez. 2025. "Dental Casts for Fixed Dental Prostheses Printed with SLA Technology: Influence of External Shell Thickness and Printing Orientation" Materials 18, no. 10: 2246. https://doi.org/10.3390/ma18102246
APA StyleGarcía-Gil, I., Rodríguez Alonso, V., Tobar Arribas, C., Mosaddad, S. A., Peláez, J., & Suárez, M. J. (2025). Dental Casts for Fixed Dental Prostheses Printed with SLA Technology: Influence of External Shell Thickness and Printing Orientation. Materials, 18(10), 2246. https://doi.org/10.3390/ma18102246







