Wear Behavior and Water Sorption of Additively Manufactured Resin-Based Splint Materials
Abstract
1. Introduction
2. Materials and Methods
2.1. Printing—Wear Behavior/Water Sorption
2.2. Cleaning—Wear Behavior/Water Sorption
2.3. Post-Polymerization—Wear Behavior/Water Sorption
2.4. Processing
2.4.1. Processing—Wear Behavior
2.4.2. Processing—Water Sorption
2.5. Storage
2.5.1. Storage—Wear Behavior
2.5.2. Storage—Water Sorption
2.6. Testing
2.6.1. Testing—Wear Behavior
2.6.2. Testing—Water Sorption and Solubility
2.7. Statistics
3. Results
3.1. Wear Behavior
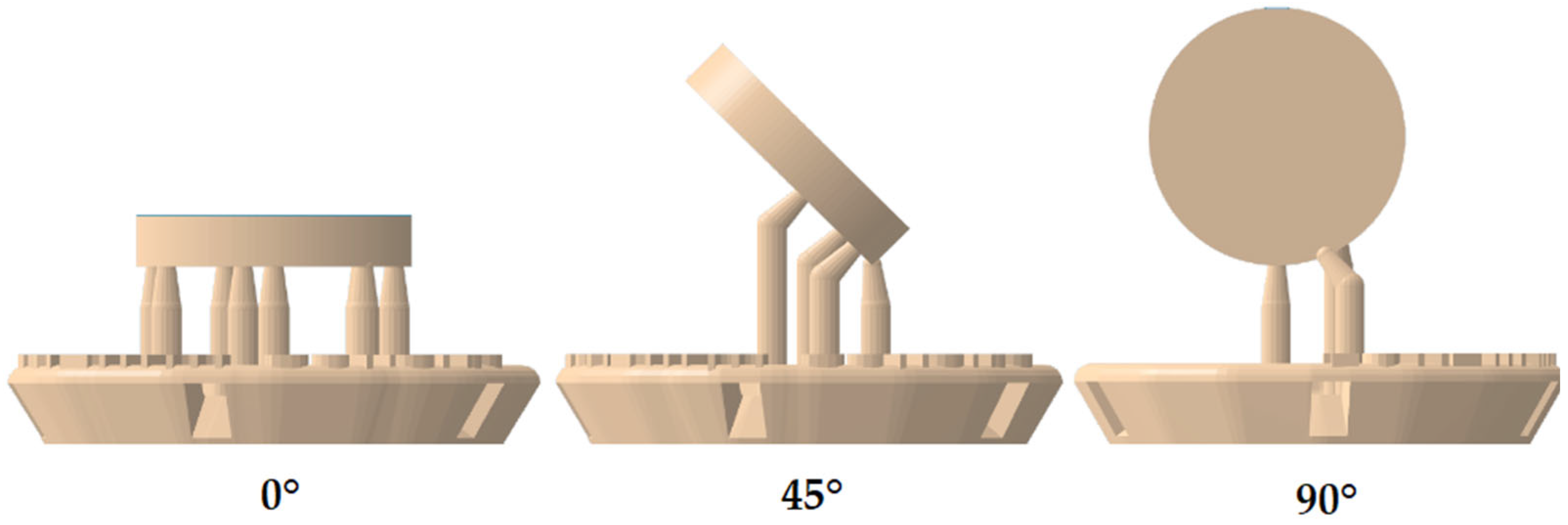
3.1.1. Building Orientation
3.1.2. Cleaning
3.1.3. Post-Polymerization
3.1.4. Storage
3.2. Water Sorption
3.2.1. Building Orientation
3.2.2. Cleaning
3.2.3. Post-Polymerization
| Wear | Water Sorption | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 24 h | 60 d | ||||||||
| Orientation to Building Platform | Material | Cleaning | Post- Polymerization | Mean [µm] | SD | Mean [µm] | SD | Mean [µm] | SD |
| 90° | 1 | WA | LED | −635.5 | 227.1 | −647.0 | 166.8 | 18.1 | 0.3 |
| XEN | −594.6 | 212.7 | −503.4 | 237.9 | 16.7 | 0.3 | |||
| WM | LED | −481.6 | 136.5 | −523.0 | 217.4 | 17.7 | 0.5 | ||
| XEN | −418.6 | 50.3 | −421.8 | 140.4 | 17.0 | 1.3 | |||
| 2 | WA | LED | −637.6 | 105.6 | −453.4 | 150.5 | 21.9 | 2.8 | |
| XEN | −579.8 | 191.1 | −556.5 | 159.0 | 23.3 | 0.4 | |||
| WM | LED | −711.3 | 326.1 | −548.8 | 185.0 | 21.7 | 0.3 | ||
| XEN | −620.8 | 160.8 | −506.1 | 161.1 | 24.0 | 0.7 | |||
| 45° | 1 | WA | LED | −697.0 | 174.0 | −526.3 | 152.2 | 18.2 | 2.6 |
| XEN | −676.6 | 128.0 | −527.5 | 107.7 | 16.2 | 0.3 | |||
| WM | LED | −645.9 | 189.4 | −603.3 | 122.4 | 13.8 | 6.3 | ||
| XEN | −713.0 | 149.0 | −592.2 | 174.1 | 16.7 | 0.3 | |||
| 2 | WA | LED | −657.5 | 184.3 | −524.7 | 162.3 | 22.1 | 1.2 | |
| XEN | −651.8 | 158.7 | −633.1 | 238.3 | 22.1 | 0.5 | |||
| WM | LED | −597.5 | 156.5 | −667.5 | 210.2 | 27.5 | 0.8 | ||
| XEN | −583.6 | 196.1 | −507.9 | 77.1 | 28.3 | 0.7 | |||
| 0° | 1 | WA | LED | −476.0 | 141.1 | −576.0 | 182.6 | 16.3 | 0.5 |
| XEN | −469.0 | 113.2 | −533.1 | 124.4 | 17.3 | 0.4 | |||
| WM | LED | −634.1 | 158.4 | −425.6 | 74.0 | 13.8 | 0.6 | ||
| XEN | −637.3 | 192.8 | −612.2 | 169.4 | 13.8 | 0.6 | |||
| 2 | WA | LED | −628.9 | 113.8 | −485.2 | 60.5 | 30.3 | 0.6 | |
| XEN | −440.0 | 181.9 | −492.2 | 99.6 | 29.4 | 0.5 | |||
| WM | LED | −559.0 | 109.1 | −520.3 | 188.8 | 29.1 | 0.6 | ||
| XEN | −537.2 | 79.8 | −568.6 | 240.8 | 29.2 | 0.5 | |||
4. Discussion
4.1. Wear Behavior
4.1.1. Building Orientation
4.1.2. Cleaning
4.1.3. Post-Polymerization
4.1.4. Storage
4.2. Water Sorption
4.2.1. Building Orientation
4.2.2. Cleaning
4.2.3. Post-Polymerization
4.2.4. Material
5. Conclusions
- (1)
- The building orientation of additively manufactured materials has a significant effect on wear behavior and water sorption.
- (2)
- The cleaning procedure after printing does not have a significant influence on either of the tested parameters.
- (3)
- The type of post-polymerization does not have a significant influence on either of the tested parameters.
- (4)
- The storage of the samples has a significant influence on the wear behavior.
- (5)
- The water sorption is different between various additively manufactured materials.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bartlett, D.; O’Toole, S. Tooth Wear: Best Evidence Consensus Statement. J. Prosthodont. 2020, 30, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Schlueter, N.; Luka, B. Erosive tooth wear—A review on global prevalence and on its prevalence in risk groups. Br. Dent. J. 2018, 224, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Lobbezoo, F.; Ahlberg, J.; Glaros, A.G.; Kato, T.; Koyano, K.; Lavigne, G.J.; de Leeuw, R.; Manfredini, D.; Svensson, P.; Winocur, E. Bruxism defined and graded: An international consensus. J. Oral Rehabil. 2013, 40, 2–4. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Lobbezoo, F. Relationship between bruxism and temporomandibular disorders: A systematic review of literature from 1998 to 2008. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, e26–e50. [Google Scholar] [CrossRef] [PubMed]
- Klasser, G.D.; Rei, N.; Lavigne, G.J. Sleep bruxism etiology: The evolution of a changing paradigm. J. Can. Dent. Assoc. 2015, 81, f2. [Google Scholar]
- Lobbezoo, F.; van der Zaag, J.; van Selms, M.K.A.; Hamburger, H.L.; Naeije, M. Principles for the management of bruxism. J. Oral Rehabil. 2008, 35, 509–523. [Google Scholar] [CrossRef]
- Manfredini, D.; Ahlberg, J.; Winocur, E.; Lobbezoo, F. Management of sleep bruxism in adults: A qualitative systematic literature review. J. Oral Rehabil. 2015, 42, 862–874. [Google Scholar] [CrossRef]
- Berli, C.; Thieringer, F.M.; Sharma, N.; Müller, J.A.; Dedem, P.; Fischer, J.; Rohr, N. Comparing the mechanical properties of pressed, milled, and 3D-printed resins for occlusal devices. J. Prosthet. Dent. 2020, 124, 780–786. [Google Scholar] [CrossRef]
- Ainoosah, S.; Farghal, A.E.; Alzemei, M.S.; Saini, R.S.; Gurumurthy, V.; Quadri, S.A.; Okshah, A.; Mosaddad, S.A.; Heboyan, A. Comparative analysis of different types of occlusal splints for the management of sleep bruxism: A systematic review. BMC Oral Health 2024, 24, 29. [Google Scholar] [CrossRef]
- Kass, C.A.; Tregaskes, J.N. Occlusal splint fabrication. J. Prosthet. Dent. 1978, 40, 461–463. [Google Scholar] [CrossRef]
- Bohnenkamp, D.M. Dimensional stability of occlusal splints. J. Prosthet. Dent. 1996, 75, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Leib, A.M. Patient preference for light-cured composite bite splint compared to heat-cured acrylic bite splint. J. Periodontol. 2001, 72, 1108–1112. [Google Scholar] [CrossRef] [PubMed]
- Dedem, P.; Türp, J.C. Digital Michigan splint—From intraoral scanning to plasterless manufacturing. Int. J. Comput. Dent. 2016, 19, 63–76. [Google Scholar]
- van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Salmi, M.; Paloheimo, K.-S.; Tuomi, J.; Ingman, T.; Mäkitie, A. A digital process for additive manufacturing of occlusal splints: A clinical pilot study. J. R. Soc. Interface 2013, 10, 20130203. [Google Scholar] [CrossRef] [PubMed]
- Nassif, M.; Haddad, C.; Habli, L.; Zoghby, A. Materials and manufacturing techniques for occlusal splints: A literature review. J. Oral Rehabil. 2023, 50, 1348–1354. [Google Scholar] [CrossRef]
- Lutz, A.-M.; Hampe, R.; Roos, M.; Lümkemann, N.; Eichberger, M.; Stawarczyk, B. Fracture resistance and 2-body wear of 3-dimensional-printed occlusal devices. J. Prosthet. Dent. 2019, 121, 166–172. [Google Scholar] [CrossRef]
- Wesemann, C.; Spies, B.C.; Sterzenbach, G.; Beuer, F.; Kohal, R.; Wemken, G.; Krügel, M.; Pieralli, S. Polymers for conventional, subtractive, and additive manufacturing of occlusal devices differ in hardness and flexural properties but not in wear resistance. Dent. Mater. 2021, 37, 432–442. [Google Scholar] [CrossRef]
- de Paula Lopez, V.; Dias Corpa Tardelli, J.; Botelho, A.L.; Marcondes Agnelli, J.A.; Cândido Dos Reis, A. Mechanical performance of 3-dimensionally printed resins compared with conventional and milled resins for the manufacture of occlusal devices: A systematic review. J. Prosthet. Dent. 2023. [Google Scholar] [CrossRef]
- Lin, R.; Yu, C.-H.; Sun, J. Mechanical properties and cytotoxicity of three-dimensional printing polycarbonate for occlusal splints. Shanghai Kou Qiang Yi Xue 2019, 28, 467–471. [Google Scholar]
- Rosentritt, M.; Behr, M.; Strasser, T.; Schmid, A. Pilot in-vitro study on insertion/removal performance of hand-cast, milled and 3D printed splints. J. Mech. Behav. Biomed. Mater. 2021, 121, 104612. [Google Scholar] [CrossRef] [PubMed]
- Benli, M.; Al-Haj Husain, N.; Ozcan, M. Mechanical and chemical characterization of contemporary occlusal splint materials fabricated with different methods: A systematic review. Clin. Oral Investig. 2023, 27, 7115–7141. [Google Scholar] [CrossRef] [PubMed]
- Grymak, A.; Aarts, J.M.; Ma, S.; Waddell, J.N.; Choi, J.J.E. Wear Behavior of Occlusal Splint Materials Manufactured By Various Methods: A Systematic Review. J. Prosthodont. 2022, 31, 472–487. [Google Scholar] [CrossRef] [PubMed]
- Wulff, J.; Rauch, A.; Schmidt, M.B.; Rosentritt, M. Biaxial Flexural Strength of Printed Splint Materials. Materials 2024, 17, 1112. [Google Scholar] [CrossRef]
- Hada, T.; Kanazawa, M.; Iwaki, M.; Arakida, T.; Minakuchi, S. Effect of printing direction on stress distortion of three-dimensional printed dentures using stereolithography technology. J. Mech. Behav. Biomed. Mater. 2020, 110, 103949. [Google Scholar] [CrossRef]
- Nold, J.; Wesemann, C.; Rieg, L.; Binder, L.; Witkowski, S.; Spies, B.C.; Kohal, R.J. Does Printing Orientation Matter? In-Vitro Fracture Strength of Temporary Fixed Dental Prostheses after a 1-Year Simulation in the Artificial Mouth. Materials 2021, 14, 259. [Google Scholar] [CrossRef]
- Shim, J.S.; Kim, J.-E.; Jeong, S.H.; Choi, Y.J.; Ryu, J.J. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. J. Prosthet. Dent. 2020, 124, 468–475. [Google Scholar] [CrossRef]
- Hada, T.; Kanazawa, M.; Iwaki, M.; Katheng, A.; Minakuchi, S. Comparison of Mechanical Properties of PMMA Disks for Digitally Designed Dentures. Polymers 2021, 13, 1745. [Google Scholar] [CrossRef]
- Maleki, T.; Meinen, J.; Coldea, A.; Reymus, M.; Edelhoff, D.; Stawarczyk, B. Mechanical and physical properties of splint materials for oral appliances produced by additive, subtractive and conventional manufacturing. Dent. Mater. 2024, 40, 1171–1183. [Google Scholar] [CrossRef]
- Tian, J.; Qi, X.; Xian, G. Effect of hygrothermal aging on the friction behavior and wear mechanism of the multi-filler reinforced epoxy composites for coated steel. J. Mater. Res. Technol. 2024, 32, 140–151. [Google Scholar] [CrossRef]
- Xian, G.; Bai, Y.; Qi, X.; Wang, J.; Tian, J.; Xiao, H. Hygrothermal aging on the mechanical property and degradation mechanism of carbon fiber reinforced epoxy composites modified by nylon 6. J. Mater. Res. Technol. 2024, 33, 6297–6306. [Google Scholar] [CrossRef]
- ISO/TR 14569-1:2007-05; Zahnärztliche Werkstoffe—Anleitung zur Prüfung der Abriebsfestigkeit—Teil 1: Abrieb durch Zähneputzen. DIN Media GmbH: Berlin, Germany, 2007.
- DIN EN ISO 10477:2021-02; Zahnheilkunde—Polymerbasierte Kronen- und Verblendwerkstoffe (ISO 10477:2020). Deutsche Fassung EN ISO 10477:2020; DIN Media GmbH: Berlin, Germany, 2021.
- Federici, M.; Straffelini, G.; Gialanella, S. Pin-on-Disc Testing of Low-Metallic Friction Material Sliding Against HVOF Coated Cast Iron: Modelling of the Contact Temperature Evolution. Tribol. Lett. 2017, 65, 121. [Google Scholar] [CrossRef]
- Hutchings, I.M.; Shipway, P. Tribology: Friction and Wear of Engineering Materials, 2nd ed.; Butterworth-Heinemann: Oxford, UK, 2017; ISBN 9780081009512. [Google Scholar]
- Grymak, A.; Waddell, J.N.; Aarts, J.M.; Ma, S.; Choi, J.J.E. Evaluation of wear behaviour of various occlusal splint materials and manufacturing processes. J. Mech. Behav. Biomed. Mater. 2022, 126, 105053. [Google Scholar] [CrossRef] [PubMed]
- Zohdi, N.; Yang, R.C. Material Anisotropy in Additively Manufactured Polymers and Polymer Composites: A Review. Polymers 2021, 13, 3368. [Google Scholar] [CrossRef]
- Dizon, J.R.C.; Espera, A.H.; Chen, Q.; Advincula, R.C. Mechanical characterization of 3D-printed polymers. Addit. Manuf. 2018, 20, 44–67. [Google Scholar] [CrossRef]
- Hwangbo, N.-K.; Nam, N.-E.; Choi, J.-H.; Kim, J.-E. Effects of the Washing Time and Washing Solution on the Biocompatibility and Mechanical Properties of 3D Printed Dental Resin Materials. Polymers 2021, 13, 4410. [Google Scholar] [CrossRef]
- Wulff, J.; Schmid, A.; Huber, C.; Rosentritt, M. Dynamic fatigue of 3D-printed splint materials. J. Mech. Behav. Biomed. Mater. 2021, 124, 104885. [Google Scholar] [CrossRef]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L. Evaluation of the mechanical properties and degree of conversion of 3D printed splint material. J. Mech. Behav. Biomed. Mater. 2021, 115, 104254. [Google Scholar] [CrossRef]
- Franz, A.; König, F.; Lucas, T.; Watts, D.C.; Schedle, A. Cytotoxic effects of dental bonding substances as a function of degree of conversion. Dent. Mater. 2009, 25, 232–239. [Google Scholar] [CrossRef]
- Wulff, J.; Schweikl, H.; Rosentritt, M. Cytotoxicity of printed resin-based splint materials. J. Dent. 2022, 120, 104097. [Google Scholar] [CrossRef]
- Bayarsaikhan, E.; Lim, J.-H.; Shin, S.-H.; Park, K.-H.; Park, Y.-B.; Lee, J.-H.; Kim, J.-E. Effects of Postcuring Temperature on the Mechanical Properties and Biocompatibility of Three-Dimensional Printed Dental Resin Material. Polymers 2021, 13, 1180. [Google Scholar] [CrossRef] [PubMed]
- Oh, R.; Lim, J.-H.; Lee, C.-G.; Lee, K.-W.; Kim, S.-Y.; Kim, J.-E. Effects of washing solution temperature on the biocompatibility and mechanical properties of 3D-Printed dental resin material. J. Mech. Behav. Biomed. Mater. 2023, 143, 105906. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Cascos-Sánchez, R.; Zeitler, J.M.; Barmak, A.B.; Kois, J.C.; Gómez-Polo, M. Influence of print orientation and wet-dry storage time on the intaglio accuracy of additively manufactured occlusal devices. J. Prosthet. Dent. 2024, 131, 1226–1234. [Google Scholar] [CrossRef]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L.V. 3D-Printed vs. Heat-Polymerizing and Autopolymerizing Denture Base Acrylic Resins. Materials 2021, 14, 5781. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Alshehri, S.Z.; Alhamid, S.A.; Albarrak, A.; Khan, S.Q.; Alshahrani, F.A.; Alqarawi, F.K. Water Sorption, Solubility, and Translucency of 3D-Printed Denture Base Resins. Dent. J. 2022, 10, 42. [Google Scholar] [CrossRef]
- Barsby, M.J. A denture base resin with low water absorption. J. Dent. 1992, 20, 240–244. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Abualsaud, R.; Alshahrani, F.A.; Al-Thobity, A.M.; Khan, S.Q.; Akhtar, S.; Ateeq, I.S.; Helal, M.A.; Al-Harbi, F.A. Strength and Surface Properties of a 3D-Printed Denture Base Polymer. J. Prosthodont. 2022, 31, 412–418. [Google Scholar] [CrossRef]
- Vallittu, P.K.; Ruyter, I.E.; Nat, R. The swelling phenomenon of acrylic resin polymer teeth at the interface with denture base polymers. J. Prosthet. Dent. 1997, 78, 194–199. [Google Scholar] [CrossRef]
- Liu, Y.; Jin, G.; Lim, J.-H.; Kim, J.-E. Effects of washing agents on the mechanical and biocompatibility properties of water-washable 3D printing crown and bridge resin. Sci. Rep. 2024, 14, 9909. [Google Scholar] [CrossRef]
- Luo, K.; Liu, Q.; Alhotan, A.; Dai, J.; Li, A.; Xu, S.; Li, P. Effect of post-curing conditions on surface characteristics, physico-mechanical properties, and cytotoxicity of a 3D-printed denture base polymer. Dent. Mater. 2024, 40, 500–507. [Google Scholar] [CrossRef]


| Abbr. Text | Device/Material Protocol | Manufacturer LOT | |
|---|---|---|---|
| Printer | P30+ (digital light processing) | Straumann, Basel, Switzerland | |
| Orientation | 0° | ||
| 45° | |||
| 90° | |||
| Cleaning | AUTO | P Wash (isopropanol): pre-cleaning 3:10 min, cleaning 2:20 min, drying 1:30 min | Straumann, Basel, Switzerland |
| MAN | Pre-/Main-Clean (isopropanol): pre-cleaning 3:00 min, ultrasonic: 2:00 min, air-drying: 1:00 min | VOCO, Cuxhaven, Germany | |
| Post-polymerization | LED | P Cure: LED, 10 min, vacuum, UV–A: 400–315 nm; UV-B: 315–280 nm, heating | Straumann, Basel, Switzerland |
| XEN | Otoflash G171: 2 × 2000 Xenon flashes, 280–700 nm, maximum between 400 and 500 nm | NK-OPTIK, Baierbrunn, Germany | |
| Materials | M1 | Luxaprint OrthoPlus: >90% bisphenol A dimethacrylate, 385/405 nm, flexural strength ≥ 70 MPa, flexural modulus ≥ 1 GPa, Shore D ≥ 60 | DMG, Hamburg, Germany LOT 218479 |
| M2 | V-Print Splint: acrylate, Bis-EMA, TEGDMA, hydroxypropyl methacrylate, butylated hydroxytoluene, diphenyl(2,4,6-trimethylbenzoyl) phosphine oxide, 385 nm, flexural strength 75 MPa, flexural modulus ≥ 2.1 GPa, sorption 27.7 μg/mm3, solubility < 0.1 μg/mm3 | VOCO, Cuxhaven, Germany LOT 2023138 |
| F | p-Value | |
|---|---|---|
| aging | 10.483 | 0.001 |
| position | 7.302 | 0.001 |
| material | 0.058 | 0.810 |
| cleaning | 0.007 | 0.933 |
| polymerization | 1.406 | 0.237 |
| aging ∗ position | 1.071 | 0.344 |
| aging ∗ material | 0.139 | 0.710 |
| aging ∗ cleaning | 0.011 | 0.916 |
| aging ∗ polymerization | 0.917 | 0.339 |
| position ∗ material | 1.696 | 0.185 |
| position ∗ cleaning | 2.638 | 0.073 |
| position ∗ polymerization | 1.010 | 0.365 |
| material ∗ cleaning | 0.692 | 0.406 |
| material ∗ polymerization | 0.120 | 0.729 |
| cleaning ∗ polymerization | 0.047 | 0.829 |
| aging ∗ position ∗ material | 2.687 | 0.070 |
| aging ∗ position ∗ cleaning | 1.711 | 0.182 |
| aging ∗ position ∗ polymerization | 1.174 | 0.310 |
| aging ∗ material ∗ cleaning | 0.456 | 0.500 |
| aging ∗ material ∗ polymerization | 1.442 | 0.231 |
| aging ∗ cleaning ∗ polymerization | 0.587 | 0.444 |
| position ∗ material ∗ cleaning | 4.583 | 0.011 |
| position ∗ material ∗ polymerization | 1.426 | 0.242 |
| position ∗ cleaning ∗ polymerization | 2.348 | 0.097 |
| material ∗ cleaning ∗ polymerization | 2.006 | 0.158 |
| aging ∗ position ∗ material ∗ cleaning | 2.178 | 0.115 |
| aging ∗ position ∗ material ∗ polymerization | 0.497 | 0.609 |
| aging ∗ position ∗ cleaning ∗ polymerization | 0.959 | 0.384 |
| aging ∗ material ∗ cleaning ∗ polymerization | 2.766 | 0.097 |
| position ∗ material ∗ cleaning ∗ polymerization | 0.457 | 0.634 |
| aging ∗ position ∗ material ∗ cleaning ∗ polymerization | 0.186 | 0.830 |
| F | p-Value | |
|---|---|---|
| position | 23.273 | <0.001 |
| material | 988.122 | <0.001 |
| cleaning | 0.049 | 0.826 |
| polymerization | 0.907 | 0.343 |
| position ∗ material | 74.666 | <0.001 |
| position ∗ cleaning | 13.298 | <0.001 |
| position ∗ polymerization | 0.179 | 0.836 |
| material ∗ cleaning | 32.759 | <0.001 |
| material ∗ polymerization | 1.245 | 0.267 |
| cleaning ∗ polymerization | 3.950 | 0.050 |
| position ∗ material ∗ cleaning | 13.732 | <0.001 |
| position ∗ material ∗ polymerization | 3.657 | 0.030 |
| position ∗ cleaning ∗ polymerization | 1.974 | 0.145 |
| material ∗ cleaning ∗ polymerization | 0.230 | 0.632 |
| position ∗ material ∗ cleaning ∗ polymerization | 2.228 | 0.113 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wulff, J.; Merle, C.L.; Hahnel, S.; Rosentritt, M. Wear Behavior and Water Sorption of Additively Manufactured Resin-Based Splint Materials. Materials 2024, 17, 5880. https://doi.org/10.3390/ma17235880
Wulff J, Merle CL, Hahnel S, Rosentritt M. Wear Behavior and Water Sorption of Additively Manufactured Resin-Based Splint Materials. Materials. 2024; 17(23):5880. https://doi.org/10.3390/ma17235880
Chicago/Turabian StyleWulff, Johann, Cordula Leonie Merle, Sebastian Hahnel, and Martin Rosentritt. 2024. "Wear Behavior and Water Sorption of Additively Manufactured Resin-Based Splint Materials" Materials 17, no. 23: 5880. https://doi.org/10.3390/ma17235880
APA StyleWulff, J., Merle, C. L., Hahnel, S., & Rosentritt, M. (2024). Wear Behavior and Water Sorption of Additively Manufactured Resin-Based Splint Materials. Materials, 17(23), 5880. https://doi.org/10.3390/ma17235880







