Marginal Fit, Mechanical Properties, and Esthetic Outcomes of CAD/CAM Interim Fixed Dental Prostheses (FDPs): A Systematic Review
Abstract
1. Introduction
2. Material and Methods
3. Results
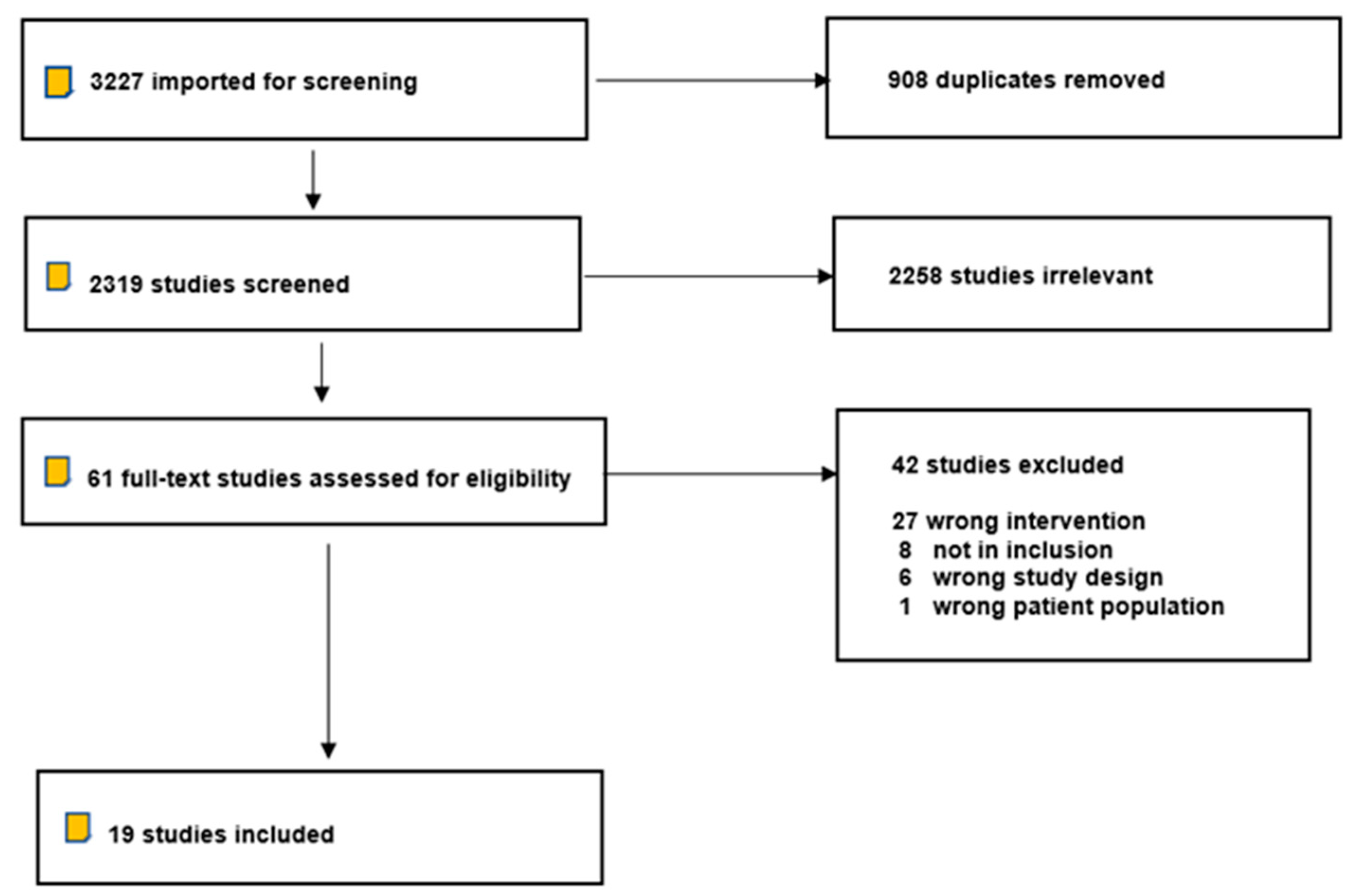
3.1. Study Screening and Selection
3.2. Data Quality Assessment
3.3. Data Extraction and Analysis
3.4. Marginal Fit
3.5. Mechanical Properties
3.5.1. Surface Roughness
3.5.2. Mechanical Strengths
3.5.3. Esthetic Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Reeponmaha, T.; Angwaravong, O.; Angwarawong, T. Comparison of fracture strength after thermo-mechanical aging between provisional crowns made with CAD/CAM and conventional method. J. Adv. Prosthodont. 2020, 12, 218–224. [Google Scholar] [CrossRef]
- Rayyan, M.M.; Aboushelib, M.; Sayed, N.M.; Ibrahim, A.; Jimbo, R. Comparison of interim restorations fabricated by CAD/CAM with those fabricated manually. J. Prosthet. Dent. 2015, 114, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Rayyan, M.M.; Aboushelib, M.; Sayed, N.M.; Ibrahim, A.; Jimbo, R. Comparative in vitro evaluation of CAD/CAM vs conventional provisional crowns. J. Appl. Oral. Sci. 2016, 24, 258–263. [Google Scholar]
- Christensen, G.J. Provisional restorations for fixed prosthodontics. J. Am. Dent. Assoc. 1996, 127, 249–252. [Google Scholar] [CrossRef] [PubMed]
- Christensen, G.J. The fastest and best provisional restorations. J. Am. Dent. Assoc. 2003, 134, 637–639. [Google Scholar] [CrossRef] [PubMed]
- Yao, J.; Li, J.; Wang, Y.; Huang, H. Comparison of the flexural strength and marginal accuracy of traditional and CAD/CAM interim materials before and after thermal cycling. J. Prosthet. Dent. 2014, 112, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L. Characterization of the mechanical properties of CAD/CAM polymers for interim fixed restorations. Dent. Mater. J. 2020, 39, 319–325. [Google Scholar] [CrossRef]
- Regish, K.M.; Sharma, D.; Prithviraj, D.R. Techniques of fabrication of provisional restoration: An overview. Int. J. Dent. 2011, 2011, 134659. [Google Scholar] [CrossRef]
- Fehling, A.W.; Neitzke, C. A direct provisional restoration for decreased occlusal wear and improved marginal integrity: A hybrid technique. J. Prosthodont. 1994, 3, 256–260. [Google Scholar] [CrossRef]
- Small, B.W. Indirect provisional restorations. Gen. Dent. 1999, 47, 140–142. [Google Scholar]
- Benli, M.; Eker-Gümüş, B.; Kahraman, Y.; Huck, O.; Özcan, M. Can polylactic acid be a CAD/CAM material for provisional crown restorations in terms of fit and fracture strength? Dent. Mater. J. 2021, 40, 772–780. [Google Scholar] [CrossRef]
- Strassler, H.E.; Lowe, R.A. Chairside resin-based provisional restorative materials for fixed prosthodontics. Compend. Contin. Educ. Dent. 2011, 32, 10–12. [Google Scholar]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- F42 Committee. ISO/ASTM52900 Additive Manufacturing–General Principles–Terminology [Internet]; ASTM International: West Conshohocken, PA, USA, 2015. Available online: https://www.astm.org/Standards/ISOASTM52900.htm (accessed on 19 February 2023).
- Papadiochou, S.; Pissiotis, A.L. Marginal adaptation and CAD-CAM technology: A systematic review of restorative material and fabrication techniques. J. Prosthet. Dent. 2018, 119, 545–551. [Google Scholar] [CrossRef]
- Yadav, B.; Dureja, I.; Malhotra, P.; Dabas, N.; Bhargava, A.; Pahwa, R. A comparative evaluation of vertical marginal fit of provisional crowns fabricated by computer-aided design/computer-aided manufacturing technique and direct (intraoral technique) and flexural strength of the materials: An in vitro study. J. Indian Prosthodont. Soc. 2018, 18, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Güth, J.F.; e Silva, J.A.; Edelhoff, D. Enhancing the predictability of complex rehabilitation with a removable CAD/CAM-fabricated long-term provisional prosthesis: A clinical report. J. Prosthet. Dent. 2012, 107, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Güth, J.F.; Dent, M. CAD/CAM-generated high-density polymer restorations for the pretreatment of complex cases: A case report. Quintessence Int. 2012, 43, 457–467. [Google Scholar]
- Jokstad, A.; Gokce, M.; Hjortsjo, C. A systematic review of the scientific documentation of fixed partial dentures made from fiber- reinforced polymer to replace missing teeth. J. Prosthet. Dent. 2005, 18, 489–496. [Google Scholar] [CrossRef]
- Hamza, T.A.; Johnston, W.M.; Schricker, S.R. Effect of polyhedral silsesquioxane (POSS) on the flexural strength and color of interim materials. J. Prosthet. Dent. 2014, 112, 228–234. [Google Scholar] [CrossRef]
- Alp, G.; Murat, S.; Yilmaz, B. Comparison of flexural strength of different CAD/CAM PMMA-based polymers. J. Prosthodontics. 2019, 28, e491–e495. [Google Scholar] [CrossRef]
- Ozcelik, T.B.; Yilmaz, B.; Seker, E.; Shah, K. Marginal Adaptation of Provisional CAD/CAM Restorations Fabricated Using Various Simulated Digital Cement Space Settings. Int. J. Oral. Maxillofac. Implants 2018, 33, 1064–1069. [Google Scholar] [CrossRef] [PubMed]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inf. Decis Mak. 2007, 15, 16. [Google Scholar] [CrossRef] [PubMed]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 18, 343. [Google Scholar]
- Cheng, C.W.; Ye, S.Y.; Chien, C.H.; Chen, C.J.; Papaspyridakos, P.; Ko, C.-C. Randomized clinical trial of a conventional and a digital workflow for the fabrication of interim crowns: An evaluation of treatment efficiency, fit, and the effect of clinician experience. J. Prosthet. Dent. 2021, 125, 73–81. [Google Scholar] [CrossRef]
- Wu, J.; Xie, H.; Sadr, A.; Chung, K.H. Evaluation of Internal Fit and Marginal Adaptation of Provisional Crowns Fabricated with Three Different Techniques. Sensors 2021, 22, 740. [Google Scholar] [CrossRef]
- Angwarawong, T.; Reeponmaha, T.; Angwaravong, O. Influence of thermomechanical aging on marginal gap of CAD-CAM and conventional interim restorations. J. Prosthet. Dent. 2020, 124, 566.e1–566.e6. [Google Scholar] [CrossRef]
- Kelvin Khng, K.Y.; Ettinger, R.L.; Armstrong, S.R.; Lindquist, T.; Gratton, D.G.; Qian, F. In vitro evaluation of the marginal integrity of CAD/CAM interim crowns. J. Prosthet. Dent. 2016, 115, 617–623. [Google Scholar] [CrossRef]
- Ahmadzadeh, A.; Beheshti, B.; Haghighizadeh, M.H. Comparing Fracture Resistance of Provisional Restorations of 3-Unit Fixed Partial Dentures: An in Vitro Study of CAD/CAM versus Indirect Technique. Indian J. Forensic Med. Toxicol. 2021, 1, 15. [Google Scholar]
- Coelho, C.; Calamote, C.; Pinto, A.C.; Esteves, J.L.; Ramos, A.; Escuin, T.; Souza, J.C.M. Comparison of CAD-CAM and traditional chairside processing of 4-unit interim prostheses with and without cantilevers: Mechanics, fracture behavior, and finite element analysis. J. Prosthet. Dent. 2021, 125, 543.e1–543.e10. [Google Scholar] [CrossRef]
- Myagmar, G.; Lee, J.H.; Ahn, J.S.; Yeo, I.S.; Yoon, H.I.; Han, J.S. Wear of 3D printed and CAD/CAM milled interim resin materials after chewing simulation. J. Adv. Prosthodont. 2021, 13, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Çakmak, G.; Yilmaz, H.; Aydoğ, Ö.; Yilmaz, B. Flexural strength of CAD-CAM and conventional interim resin materials with a surface sealant. J. Prosthet. Dent. 2020, 124, 800.e1–800.e7. [Google Scholar] [CrossRef] [PubMed]
- Jeong, K.W.; Kim, S.H. Influence of surface treatments and repair materials on the shear bond strength of CAD/CAM provisional restorations. J. Adv. Prosthodont. 2019, 11, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Karaokutan, I.; Sayin, G.; Kara, O. In vitro study of fracture strength of provisional crown materials. J. Adv. Prosthodont. 2015, 7, 27–31. [Google Scholar] [CrossRef]
- Vally, Z.; Sykes, L.M.; Aspeling, M.E.; Van de Merwe, J.; Ballyram, R. In vitro comparison of the compressive strengths of seven different provisional crown materials. SADJ. 2013, 68, 64–67. [Google Scholar]
- Alt, V.; Hannig, M.; Wöstmann, B.; Balkenhol, M. Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent. Mater. 2011, 27, 339–347. [Google Scholar] [CrossRef]
- Aldahian, N.; Khan, R.; Mustafa, M.; Vohra, F.; Alrahlah, A. Influence of Conventional, CAD-CAM, and 3D Printing Fabrication Techniques on the Marginal Integrity and Surface Roughness and Wear of Interim Crowns. Appl. Sci. 2021, 11, 8964. [Google Scholar] [CrossRef]
- Al Deeb, L.; Al Ahdal, K.; Alotaibi, G.; Alshehri, A.; Alotaibi, B.; Alabdulwahab, F.; Al Deeb, M.; AlFawaz, Y.F.; Vohra, F.; Abduljabbar, T. Marginal integrity, internal adaptation and compressive strength of 3D printed, Computer Aided Design and computer aided manufacture and conventional interim fixed partial dentures. J. Biomater. Tissue Eng. 2019, 9, 1745–1750. [Google Scholar] [CrossRef]
- Abdullah, A.O.; Pollington, S.; Liu, Y. Comparison between direct chairside and digitally fabricated temporary crowns. Dent. Mater. J. 2018, 37, 957–963. [Google Scholar] [CrossRef]
- Atria, P.J.; Lagos, I.; Sampaio, C.S. In vitro evaluation of surface roughness, color stability, and color masking of provisional restoration materials for veneers and crowns. Int. J. Comput. Dent. 2020, 23, 343–350. [Google Scholar]
- Neppelenbroek, K.H. The clinical challenge of achieving marginal adaptation in direct and indirect restorations. J. Appl. Oral Sci. 2015, 23, 448–449. [Google Scholar] [CrossRef]
- Sailer, I.; Fehér, A.; Filser, F.; Lüthy, H.; Gauckler, L.J.; Schärer, P.; Hämmerle, C.H.F. Prospective clinical study of zirconia posterior fixed partial dentures: 3 years follow-up. Quintessence Int. 2006, 37, 685–693. [Google Scholar] [PubMed]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef]
- Tan, K.; Pjetursson, B.E.; Lang, N.P.; Chan, E.S.Y. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin. Oral. Implant. Res. 2004, 15, 654–666. [Google Scholar] [CrossRef]
- Abduo, J.; Lyons, K.; Swain, M. Fit of zirconia fixed partial denture: A systematic review. J. Oral. Rehabil. 2010, 37, 866–876. [Google Scholar] [CrossRef] [PubMed]
- Raut, A.; Rao, P.L.; Ravindranath, T. Zirconium for esthetic rehabilitation: An overview. Indian J. Dent. Res. Publ. Indian Soc. Dent. Res. 2011, 22, 140–143. [Google Scholar] [CrossRef]
- Qualtrough, A.J.; Piddock, V. Fitting accuracy of indirect restorations: A review of methods of assessment. Eur. J. Prosthodont. Restor. Dent. 1992, 1, 57–61. [Google Scholar] [PubMed]
- ANS/ADA. Specification n 8; American Dental Association: Chicago, IL, USA, 1977. [Google Scholar]
- Mohajeri, M.; Khazaei, S.; Vafaee, F.; Firouz, F.; Ghorbani Gholiabad, S.; Shisheian, A. Marginal Fit of Temporary Restorations Fabricated by the Conventional Chairside Method, 3D Printing, and Milling. Front. Dent. 2021, 18, 31. [Google Scholar] [CrossRef]
| Focus Question | In Natural Teeth, what Are the Outcomes of CAD-CAM Interim FDPs Compared to the Conventionally Manufactured Ones Regarding Marginal Fit, Mechanical Properties, Esthetics, and Color Stability? |
|---|---|
| Population | 1. Teeth [MeSH Terms]: tooth OR dentate OR dentulous. 2. Provisional restoration [MeSH Terms]: temporary dental restoration OR dental restoration, temporary, OR tooth crown, denture, partial, temporary, provisional OR interim and dental restoration OR temporary dental restoration OR provisional crown OR temporary crown OR interim crown OR provisional fixed partial OR interim fixed partial OR temporary fixed partial. |
| Intervention or Exposure | 3. CAD/CAM [MeSH Terms]: computer-aided design [MeSh] OR computer aided manufacturing OR CAD/CAM OR computer dentistry OR computer milled prosthesis OR digital dentistry. |
| Comparison | 4. Conventional provisional restoration [MeSH Terms]: conventional interim restoration OR conventional temporary restoration OR conventional provisional crown OR conventional provisional bridge OR conventional provisional prosthesis OR traditional provisional restoration. |
| Outcome | 5. Marginal fit [MeSH Terms]: Marginal fit OR fit OR gap OR internal OR marginal OR adaptation OR accuracy OR precision OR trueness OR Esthetic OR strength OR superiority OR clinician preference OR clinical efficacy. 6. Mechanical properties [MeSH Terms]: mechanical phenomena OR mechanical processes OR mechanical phenomena OR mechanical processes OR dental restoration wear OR mechanical properties OR fracture toughness OR flexural strength OR surface wear OR compressive strength OR Brittleness OR ductility OR elastic modulus OR fatigue OR hardness OR impact strength OR malleability OR elongation OR proportional limit OR shear strength OR tensile strength OR yield strength OR Young’s modulus. 7. Esthetics [MeSH Terms]: esthetic OR dental esthetic OR cosmetic OR appearance OR color stability OR shade OR value OR hue OR chroma. |
| Search combination | (1 OR 2 OR 3) AND 4 AND (5 OR 6 OR 7) |
| Language | English |
| Electronic databases | PubMed (MEDLINE) Cochrane Central Register of Controlled Trials (CENTRAL) EMBASE Web of Science |
| Manual journal searches | Journal of Prosthetic Dentistry, Journal of Prosthodontics, International Journal of Prosthodontics, Journal of Dentistry, Journal of the American Dental Association, Journal of Operative Dentistry, personal communications in the New York Academy of Medicine Grey Literature Report, and Dental Materials. |
| Inclusion criteria | In vitro and in vivo studies Articles published 2000–2022 |
| Exclusion criteria | Case reports with fewer than six patients Studies without comparative methodology Methodology, technique, or review article Multiple publications on the same patient population Non-English language |
| Selection | Comparability | Outcome | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Authors, Year | Was the Study Definition Adequate? (1) | Sample Size (1) | Selection of Controls (1) | Definition of Controls (1) | Comparability of Samples and Controls (2) | Assessment of Outcome (1) | Same Method of Ascertainment for All Samples (1) | Statics (1) | Total Quality Score (9) |
| Aldahian et al., 2021 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | |
| Ahmadzadeh et al., 2021 | 1 | 1 | 2 | 1 | 1 | 1 | 7 | ||
| Coelho et al., 2021 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Myagmar et al., 2021 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | |
| Wu et al., 2021 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | |
| Çakmak et al., 2020 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 8 | |
| Angwarawong et al., 2020 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Atria et al., 2020 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Jeong et al., 2019 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Aldeeb et al., 2019 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | |
| Abdullah et al., 2018 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | |
| Abdullah et al., 2016 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | |
| Kelvin Khng et al., 2016 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Karaokutan et al., 2015 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Rayyan et al., 2015 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Yao et al., 2014 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | |
| Vally et al., 2013 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 8 | |
| Alt et al., 2011 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Author, Year | Sequence Generation | Allocation Concealment | Blinding of Participants and Personnel | Blinding of Outcome Assessment | Final Decision |
|---|---|---|---|---|---|
| Cheng, 2021 | Low | Low | Low | Low | Low risk of bias |
| Author | Year | Sample Size | Study Type | Material | Fabrication Method | Marginal (M, G, F, I, A, MIF, IN) | Mechanical Properties (FS, CS, FLS, KC, Wear, Rs, EM, PS, FL) | Esthetics/Color | Comments |
|---|---|---|---|---|---|---|---|---|---|
| Aldahian et al. | 2021 | 30 | In Vitro | Jet Tooth Shade (PMMA) | Conventional | (M). (A) 269.94 μm (M.MIF) 395.89 μm | (Rs) 4.17 (Wear) 17.79 | Freeprint Temp resin 3D-printed interim (samples showed better fit with the smallest discrepancies (211 μm), adaptation (197.82 μm), and least wear (Rs) (10.81) properties compared to other groups. However, surface roughness was the highest in the 3D-printed samples. (Rs) 3.28. | |
| Cercon base PMMA blocks | CAD/CAM (milled) | (M). (A) 269.52 μm (MIF) 244.95 μm | (Rs) 3.28 (Wear) 13.63 | ||||||
| Freeprint Temp resin | CAD/CAM (3D-printed) | (M). (A) 197.82 μm (MIF) 211.87 μm | (Rs) 5.61 (Wear) 10.81 | ||||||
| Ahmadzadeh et al. | 2021 | 30 | In Vitro | Protemp 4 (Bis-acryl) | Conventional | (FS) 1326.6 ± 101.7 N | PMMA block showed higher fracture resistance (1494.3 ± 117.1 N) in comparison to the conventional material. | ||
| PMMA | Conventional | (FS) 1179.1 ± 133.5 N | |||||||
| PMMA block | CAD/CAM (milled) | (FS) 1494.3 ± 117.1 N | |||||||
| Coelho et al. | 2021 | 40 | In Vitro | Protemp4 (Bis-acryl) | Conventional | (FS) 1287 N (cantilever) 1954 N | Provisional fixed partial prostheses produced by Vita CADTemp (FS) 3136 N, Telio CA PMMA (cantilever) 2649 N (CAD/CAM) had higher strength than those fabricated by traditional chairside polymerization. | ||
| Telio CA (PMMA) | CAD/CAM (milled) | (FS) 3126 N (cantilever) 2649 N | |||||||
| Dentalon Plus (PMMA) | Conventional | (FS) 1390 N (cantilever) 1268 N | |||||||
| Vita CADTemp (acrylate polymer) | CAD/CAM (milled) | (FS) 3136 N (cantilever) 1634 N | |||||||
| Myagmar et al. | 2021 | 48 | In Vitro | NextDent C&B | CAD/CAM (3D-printed) | (Rs) (before) 0.13 ± 0.01 nm (Rs) (30k c) 0.48 ± 0.07nm (Rs) (60k c) 0.59 ± 0.06nm | The 3D printed resin (NextDent C&B) and milled resin Yamahachi PMMA Disk showed greater wear resistance than the conventional interim resin after simulation of the clinical chewing period equivalent to a duration of 1.5 and 3 months. | ||
| Yamahachi PMMA Disk | CAD/CAM (milled) | (Rs) (before) 0.19 ± 0.03nm (Rs) (30k c) 0.88 ± 0.05nm (Rs) (60k c) 1.27 ± 0.49nm | |||||||
| Jet (PMMA) | Conventional | (Rs) (before) 0.26 ± 0.02 nm (Rs) (30k c) 0.92 ± 0.10 nm (Rs) (60k c) 1.64 ± 0.44 nm | |||||||
| Cheng et al. | 2021 | 40 | RCT | PMMA Disk; Yamahachi Dental | CAD/CAM (milled) | (M.F) 1.15 ± 0.37 | Interim crowns fabricated with the digital workflow (PMMA Disk; Yamahachi Dental) resulted in smaller gap (MF) 1.15 ± 0.37, which resulted in a better fit then the conventional. | ||
| MMA materials (ALIKE; GC (PMMA) | Conventional | (M.F) 1.50 ± 0.69 | |||||||
| Wu et al. | 2021 | 48 | In Vitro | LuxaCrown (bis-acryl) | Conventional | Polyvinyl siloxane-replica method (M. discrepancy absolute) 71.3 ± 64.9 Optical coherence tomographic scanning technique (M. discrepancy absolute) 82.7 ± 65.8 | The conventionally fabricated provisional crowns using resin-based composite material LuxaCrown presented a lower gap distance (71.3 ± 64.9, 82.7 ± 65.8), which meant a better internal fit and a smaller absolute marginal discrepancy. | ||
| Lava Ultimate (Nano-ceramic) | CAD/CAM (milled) | Polyvinyl siloxane-replica method (M. discrepancy absolute) 96.9 ± 60.2 Optical coherence tomographic scanning technique (M. discrepancy absolute) 99.6 ± 54.6 | |||||||
| Dima PrintDenture Teeth | CAD/CAM (3D-printed) | Polyvinyl siloxane-replica method (M. discrepancy absolute) 120.8 ± 70.9 Optical coherence tomographic scanning technique (M. discrepancy absolute) 143.1 ± 39.9 | |||||||
| Çakmak et al. | 2020 | 14 | In Vitro | M-PM-Disc (PMMA) | CAD/CAM (milled) | (FL) 34.80 ± 6.61 | The flexural strength of milled PMMA-based polymers (M-PM-Disc PMMA) (FL) 34.80 ± 6.61 was higher than the flexural strength of conventional bisacrylate composite resin and PEMA IR materials. | ||
| Polident- (PMMA) | CAD/CAM (milled) | (FL) 31.11 ± 6.56A | |||||||
| Telio CA (PMMA) | CAD/CAM (milled) | (FL) 32.84 ± 7.83 | |||||||
| Acrytemp (Bis-acryl) | Conventional | (FL) 15.92 ± 3.95 | |||||||
| Bosworth Trim (PEMA) | Conventional | (FL)15.79 ± 9.78B | |||||||
| Angwarawong et al. | 2020 | 40 | In Vitro | Unifast Trad (PMMA) | Conventional | (M.G) (before aging) 85 ± 23 (M.G) (after aging) 114 ± 29 | The Brylic Solid and Freeprint Temp groups (CAD/ CAM fabricated interim restorations) showed a smaller marginal gap, which resulted in better marginal adaptability than the Unifast Trad and Protemp 4 groups (conventionally fabricated restorations) both before and after artificial aging. | ||
| Protemp 4 (Bis-acryl) | Conventional | (M.G) (before aging) 88 ± 17 (M.G) (after aging) 109 ± 15 | |||||||
| Brylic Solid (PMMA) | CAD/CAM (milled) | (M.G) (before aging) 54 ± 8 (M.G) (after aging) 74 ± 9 | |||||||
| Freeprint Temp | CAD/CAM (3D-printed) | (M.G) (before aging) 56 ± 7 (M.G) (after aging) 71 ± 7 | |||||||
| Atria et al. | 2020 | 40 | In Vitro | Acrylic resin (Marche 66 shade (PMMA) | Conventional | 1.3 mm Thickness Before (TC) (Rs) 0.22 After (TC) (Rs) 0.31 0.6 mm Thickness Before (TC) (Rs) 0.26 After (TC) (Rs) 0.31 | 1.3mm Thickness Translucency Before (TC) 9.59(0.10) C* After (TC) 9.97 (0.10) D* 0.6 mm Thickness Translucency Before (TC) 17.70 (0.33) c After (TC) 16.81 (0.15) c | The PMMA milled (TelioCAD) material had the least effect after thermal cycling for both roughness and translucency in comparison to the other materials in the study. | |
| Protemp (Bis-acryl) | Conventional | 1.3 mm Thickness Before (TC) (Rs) 0.18 After (TC) (Rs) 0.23 0.6 mm Thickness Before (TC) (Rs) 0.20 After (TC) (Rs) 0.25 | 1.3 mm Thickness Translucency Before (TC) 11.07 (0.12) B* After (TC) 10.59 (0.05) C* 0.6 mm Thickness Translucency Before (TC) 17.33 (0.49) c After (TC) 14.76 (0.22) d | ||||||
| TelioCAD (PMMA) | CAD/CAM (milled) | 1.3 mm Thickness Before (TC) (Rs) 0.20 After (TC) (Rs) 0.19 0.6 mm Thickness Before (TC) (Rs) 0.20 After (TC) (Rs) 0.20 | 1.3 mm Thickness Translucency Before (TC) 11.75 (0.02) B* After (TC) 12.11 (0.03) B* 0.6 mm Thickness Translucency Before (TC) 20.07 (0.10) b After (TC) 20.59 (0.04) b | ||||||
| Raydent C&B for temporary crown and bridge | CAD/CAM (3D-printed) | 1.3 mm Thickness (Rs) 0.26 (after TC) 0.54 0.6 mm Thickness Before (TC) (Rs) 0.21 After (TC) (Rs) 0.60 | 1.3 mm Thickness Translucency Before (TC) 17.51 (0.10) A* After (TC) 14.85 (0.21) A* 0.6 mm Thickness Translucency Before (TC) 24.60 (0.07) a After (TC) 23.19 (0.10) a | ||||||
| Jeong et al. | 2019 | 80 | In Vitro | Nextdent C&B | CAD/CAM (3D-printed) | (KC) 1.5(0.24) MPa·m1/2) | Yamahachi PMMA disk milled material showed the highest fracture toughness value ((KC) 3.08(0.16) Mpa·m1/2) in comparison to the other materials in the study. | ||
| ZMD-1000B Temporary | CAD/CAM (3D-printed)) | (KC) 1.52(0.19) MPa·m1/2 | |||||||
| Yamahachi PMMA disk | CAD/CAM (milled) | (KC) 3.08(0.16) Mpa·m1/2 | |||||||
| Huge PMMA block | CAD/CAM (milled) | (KC) 2.67(0.12) Mpa·m1/2 | |||||||
| Jet PMMA | Conventional | (KC) 1.91(0.23) Mpa·m1/2 | |||||||
| Alike PMMA | Conventional | (KC) 1.62(0.22) Mpa·m1/2 | |||||||
| Luxatemp (Bis-acryl) | Conventional | (KC) 1.60(0.09) Mpa·m1/2 | |||||||
| Protemp 4 (Bis-acryl) | Conventional | (KC) 2.00(0.23) Mpa·m1/2 | |||||||
| Al Deeb et al. | 2019 | 30 | In Vitro | CAD-CAM blocks Ceramill TEMP, (PMMA) | CAD/CAM (Milled) | (M.MIF) 68.2 ± 18.1 nm | (FL) 687.86 ± 46.72 N (CS) 2.44 ± 0.27 MPa | Ceramill TEMP (PMMA) milled materials showed superior marginal fit, internal adaptation, fracture load and compressive strength than the conventional material. | |
| TrimPlus, (PMMA) | Conventional | (M.MIF) 283.3 ± 98.6 nm | (FL) 492.7 ± 61.8 N (CS) 1.65 ± 0.20 MPa | ||||||
| Form 2, Formlabs, (PMMA) | CAD/CAM (3D-printed) | (M.MIF) 84.7 ± 27.5 nm | (FL) 534.8 ± 46.1 N (CS) 1.80 ± 0.15 MPa | ||||||
| Abdullah et al. | 2018 | 40 | In Vitro | VITA CAD-Temp (Acrylate polymer) | CAD/CAM (milled) | (M.G)59.97 ± 11.1 μm, (IN. F) 117.8 ± 15.58 μm | (FS) 347 ± 30.71 N | The milled PMMA samples showed a smaller marginal gap and internal fit with the smallest ArtBloc® Temp (45.58 ± 9.99 μm, 109.27 ± 19.21 μm); the milled PMMA samples also showed a higher fracture strength with the highest ArtBloc® Temp (375.04 ± 36.97 N); the milled PMMA showed smaller marginal gap and internal fit with a superior fracture strength in comparison to the conventional. | |
| ArtBloc® Temp (PMMA) | CAD/CAM (milled) | (M.G) 45.58 ± 9.99 μm, (IN. F) 109.27 ± 19.21 μm | (FS) 375.04 ± 36.97 N | ||||||
| PMMA DISK | CAD/CAM (milled) | (M.G) 62.19 ± 12.9 μm, (IN.F) 123.16 ± 23.97 μm | (FS) 361.52 ± 27.76 N | ||||||
| Acrytemp (Bis-acryl) | Conventional | (M.G) 138.6 ± 10.1 μm (IN. F) 140.1 ± 26.53 μm | (FS) 284.9 ± 49.07 N | ||||||
| Abdullah et al. | 2016 | 40 | In Vitro | VITA CAD-Temp (Acrylate polymer) | CAD/CAM (milled) | (M.G)60.61 ± 9.99 um, (IN.F) 124.94 ± 22.96 um | (FS) 361.01 ± 21.61 N | All of the milled samples showed a smaller marginal gap and internal fit with the smallest marginal gap PEEK (46.75 ± 8.26um), and Telio CAD-Temp had the smallest internal fit (110.95 ± 11.64um); milled samples also showed a higher fracture strength with the highest PEEK (802.23 ± 111.29 N) except vita cap-temp, which was lower than the conventional protemp. Milled materials showed a smaller marginal gap and internal fit with superior fracture strength in comparison to the conventional. | |
| PEEK | CAD/CAM (milled) | (M.G) 46.75 ± 8.26 um, (IN.F) 113.14 ± 23.55 um | (FS) 802.23 ± 111.29 N | ||||||
| Telio CAD-Temp (PMMA) | CAD/CAM (milled) | (M.G) 56.10 ± 5.65 um, (IN.F) 110.95 ± 11.64 um | (FS) 719.24 ± 95.17 N | ||||||
| ProtempTM4 (Bis-GMA) | Conventional | (M.G) 193.07 ± 35.96 um, (IN.F) 143.48 ± 26.74 um | (FS) 416.40 ± 69.14 N | ||||||
| Kelvin Khng et al. | 2016 | 60 | In Vitro | Telio CAD-CE (PMMA) | CAD/CAM (milled) | (M.I) (Vertical) (Facial) 0.18 mm (Lingual) 0.09 mm (M.I) (Horizontal) (Facial) 0.18 (0.05) (Lingual) 0.03 mm | The Paradigm MZ100-E4D (milled provisional crown) showed a smaller vertical marginal discrepancy in comparison to the conventionally fabricated crowns. However, there was no significant difference in the horizontal component. | ||
| Paradigm MZ100-E4D (Composite) | CAD/CAM (milled) | (M.I) (V) F 0.13 mm L 0.09 mm (M.I) (H) F 0.10 (0.05) L 0.02 (0.03) mm | |||||||
| Caulk (Composite) | Conventional | (M.I) (V) F 0.29 (0.14) L 0.13 (0.07) mm (M.I) (H) F 0.10 (0.08) L 0.16 (0.18) mm | |||||||
| Jet (PMMA) | Conventional | (M.I) (V) F 0.15 (0.06) L 0.11 (0.06) mm (M.I) (H) F 0.02 (0.04) mm L 0.13 (0.09) mm | |||||||
| Karaokutan et al. | 2015 | 60 | In Vitro | Imident (PMMA) | Conventional | (FS) 843.71 ± 83.46 N | Structur Premium (bis-acryl) conventional material showed ((FS) 1392.1 ± 344.11 N) a higher fracture strength in comparison to the other groups (including milled materials, which came in second). | ||
| Structur Premium (Bis-acryl) | Conventional | (FS) 1392.1 ± 344.11 N | |||||||
| Systemp c&b ll Polyurethane polymethacrylate | Conventional | (FS) 1009.0 ± 84.50 N | |||||||
| Acrytemp (Bis-acryl) | Conventional | (FS) 910.05 ± 77.09 N | |||||||
| Takilon BBF (PMMA) | Conventional | (FS) 711.09 ± 179.18 N | |||||||
| Temdent Classic (PMMA) | CAD/CAM (milled) | (FS) 745.23 ± 94.75 N | |||||||
| Cercon Base (PMMA) | CAD/CAM (milled) | (FS) 1106 ± 134.65 N |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-humood, H.; Alfaraj, A.; Yang, C.-C.; Levon, J.; Chu, T.-M.G.; Lin, W.-S. Marginal Fit, Mechanical Properties, and Esthetic Outcomes of CAD/CAM Interim Fixed Dental Prostheses (FDPs): A Systematic Review. Materials 2023, 16, 1996. https://doi.org/10.3390/ma16051996
Al-humood H, Alfaraj A, Yang C-C, Levon J, Chu T-MG, Lin W-S. Marginal Fit, Mechanical Properties, and Esthetic Outcomes of CAD/CAM Interim Fixed Dental Prostheses (FDPs): A Systematic Review. Materials. 2023; 16(5):1996. https://doi.org/10.3390/ma16051996
Chicago/Turabian StyleAl-humood, Hussain, Amal Alfaraj, Chao-Chieh Yang, John Levon, Tien-Min Gabriel Chu, and Wei-Shao Lin. 2023. "Marginal Fit, Mechanical Properties, and Esthetic Outcomes of CAD/CAM Interim Fixed Dental Prostheses (FDPs): A Systematic Review" Materials 16, no. 5: 1996. https://doi.org/10.3390/ma16051996
APA StyleAl-humood, H., Alfaraj, A., Yang, C.-C., Levon, J., Chu, T.-M. G., & Lin, W.-S. (2023). Marginal Fit, Mechanical Properties, and Esthetic Outcomes of CAD/CAM Interim Fixed Dental Prostheses (FDPs): A Systematic Review. Materials, 16(5), 1996. https://doi.org/10.3390/ma16051996








