Aesthetic Restorations: The Role of The Dental Hygienist in Professional Maintenance: In Vitro Microbiological Study
Abstract
:1. Introduction
2. Materials and Methods
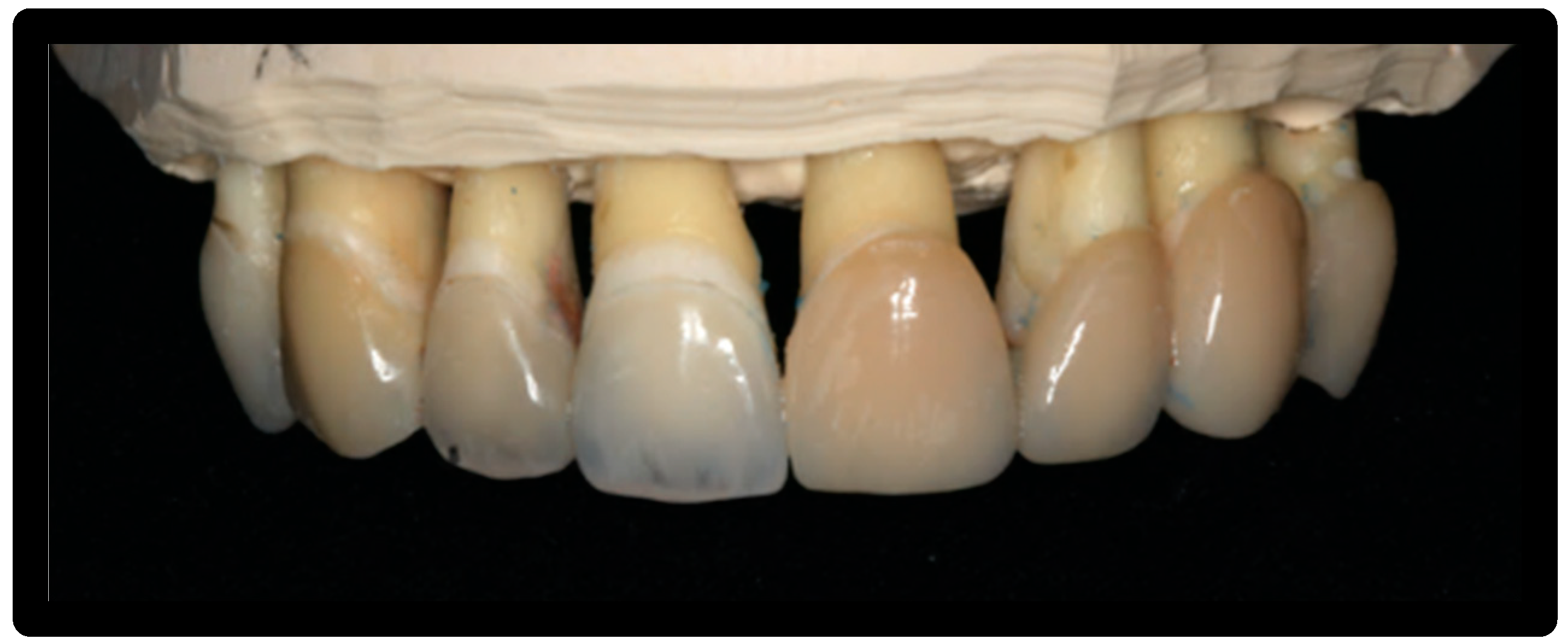
2.1. Dental Veneers
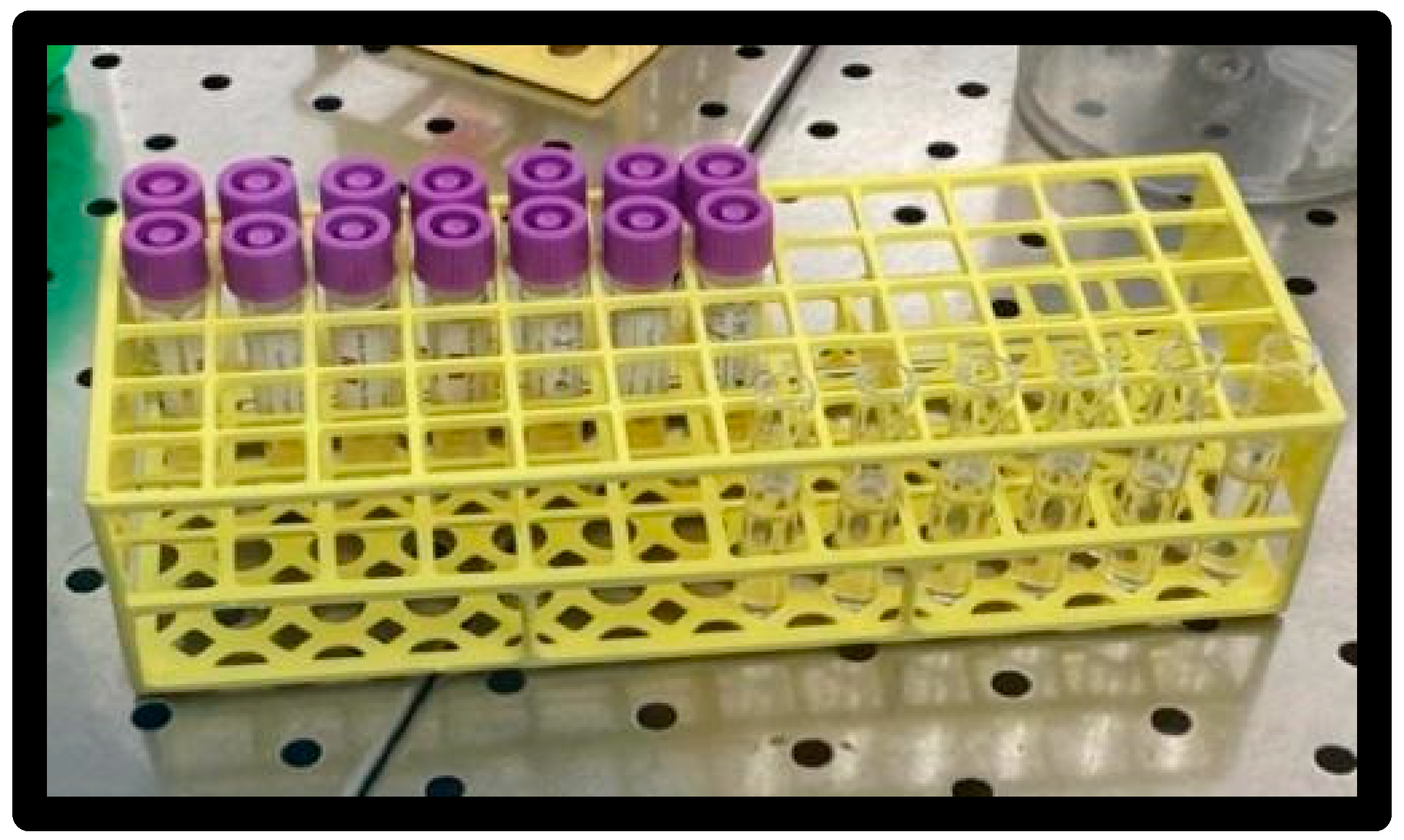
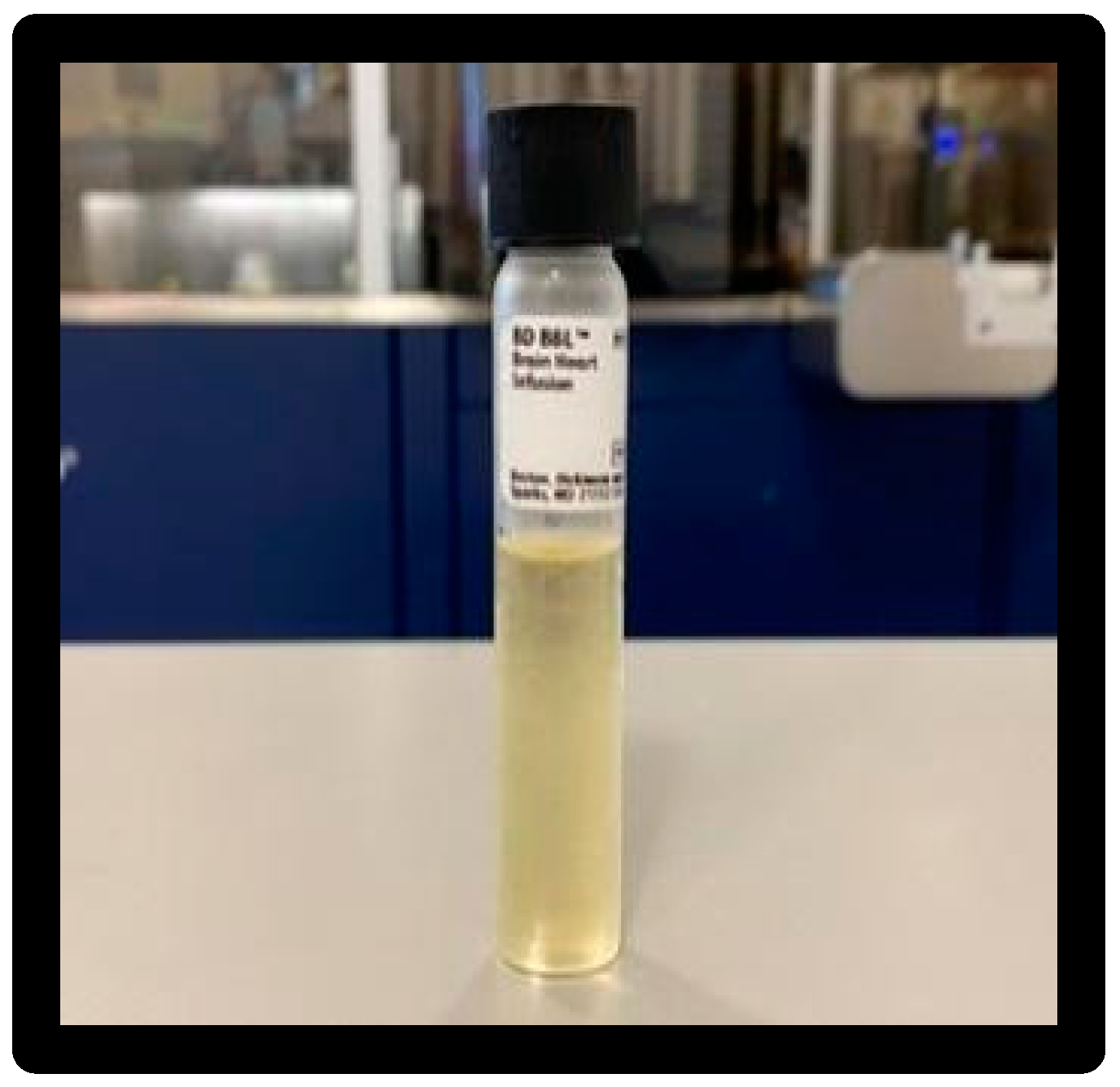
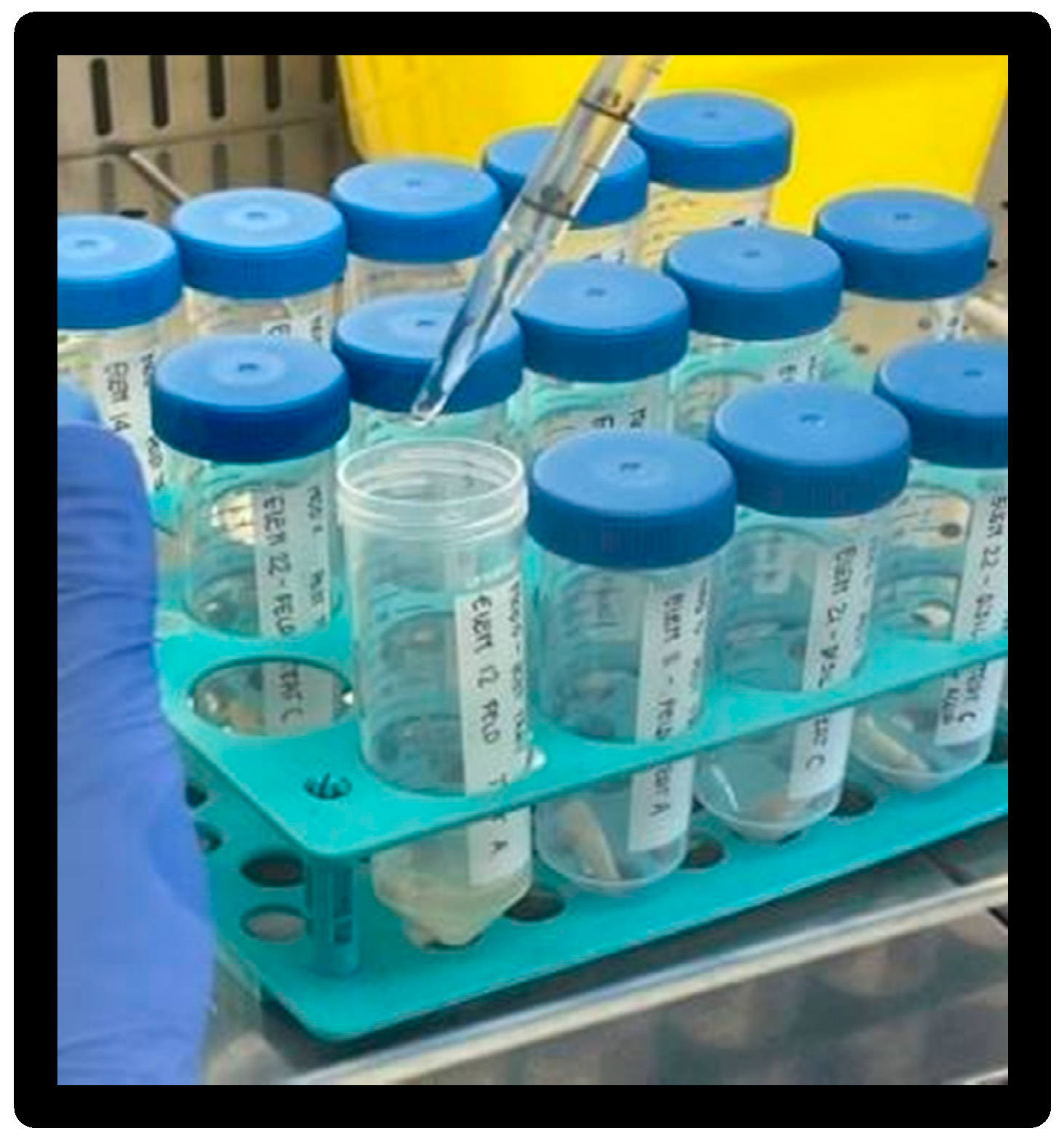
2.2. Microbiology
2.3. Consumables
2.4. Instrumentation Products
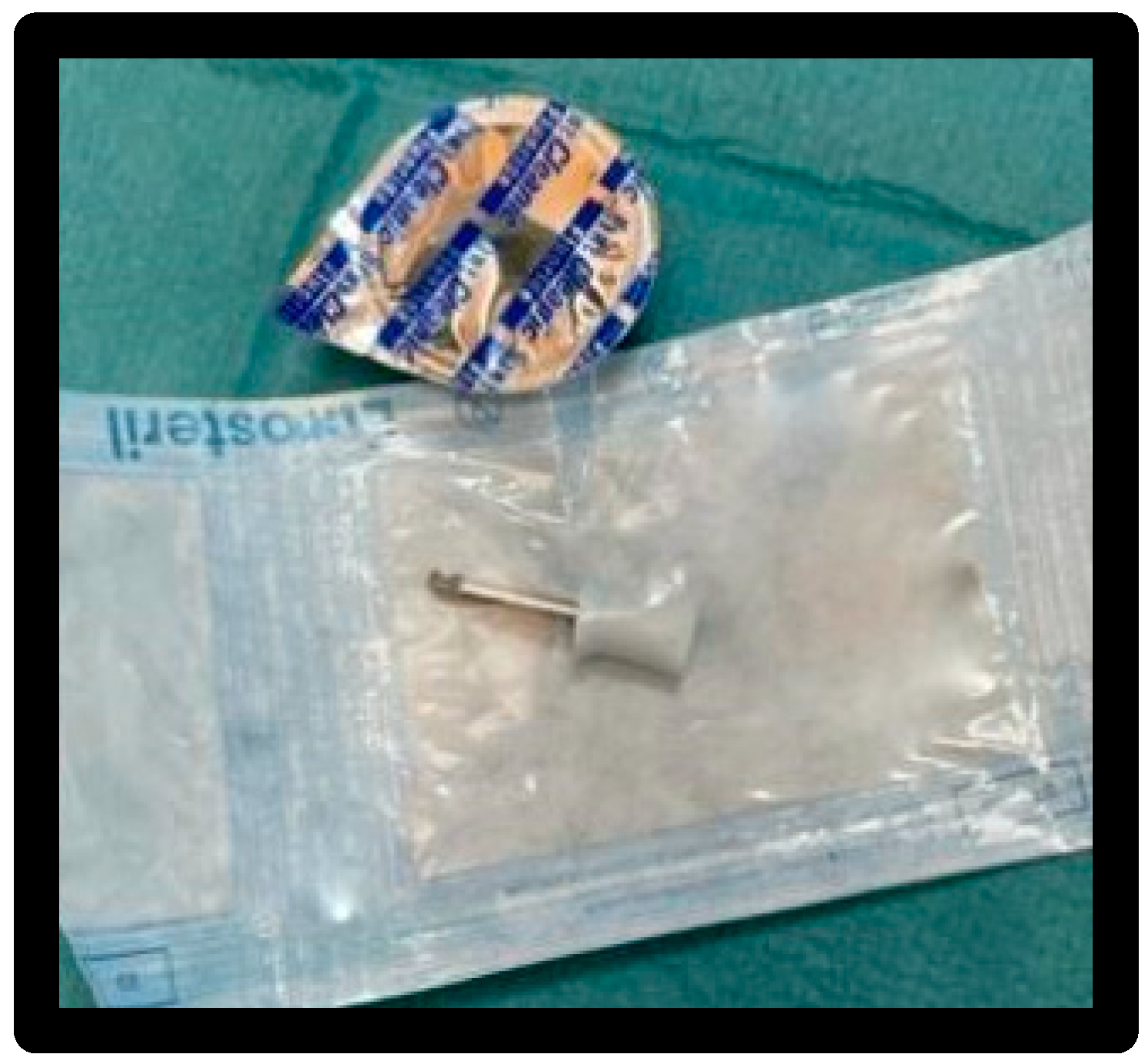
- White prophy cup
- Cleanic® prophy paste based on perlite (Figure 7)
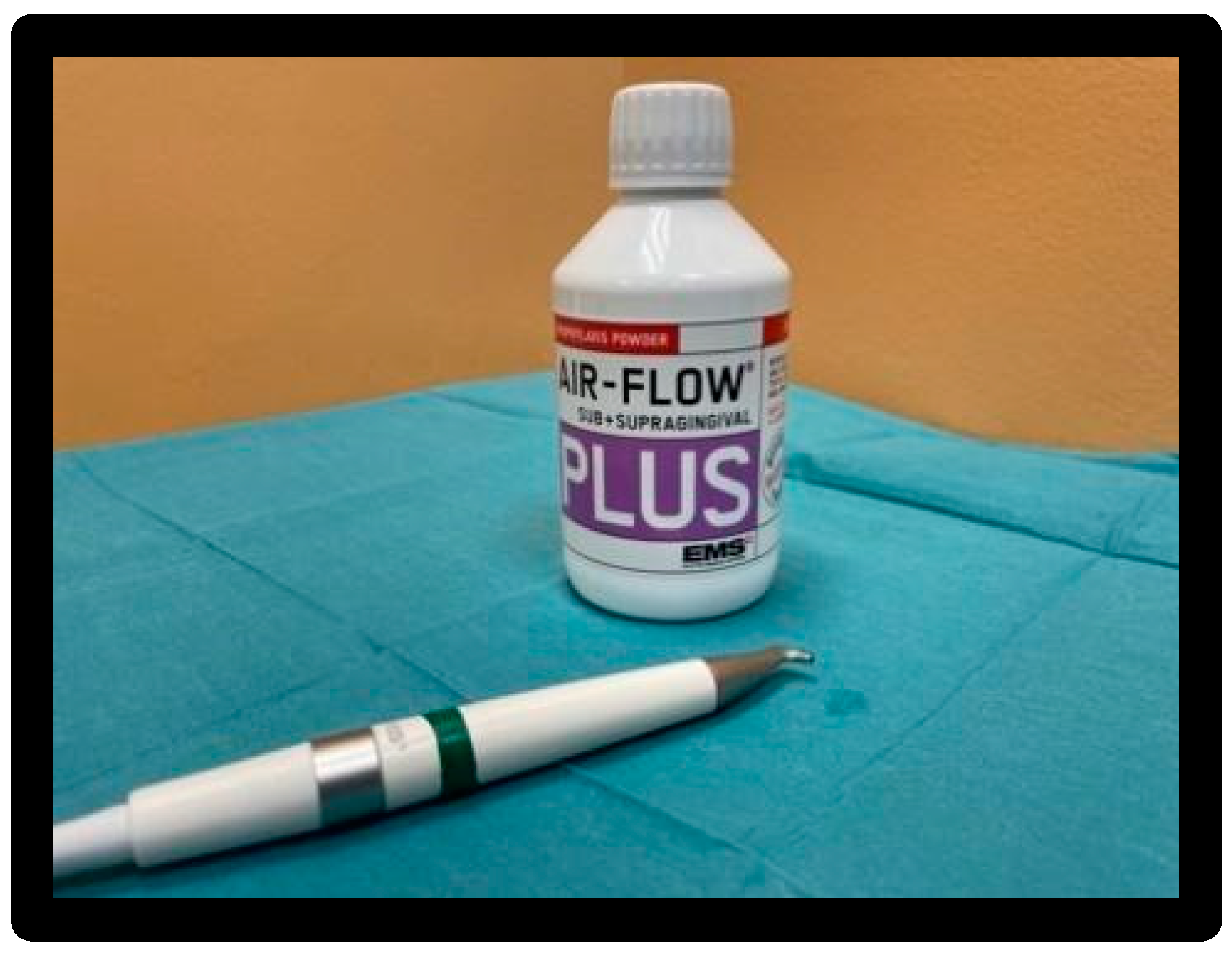
- Air-Flow Master Piezon® EMS:
- EMS Air-Flow Plus® powder, based on erythritol, with Chlorhexidine (0.3%) average grain size 14 µm (Figure 8).
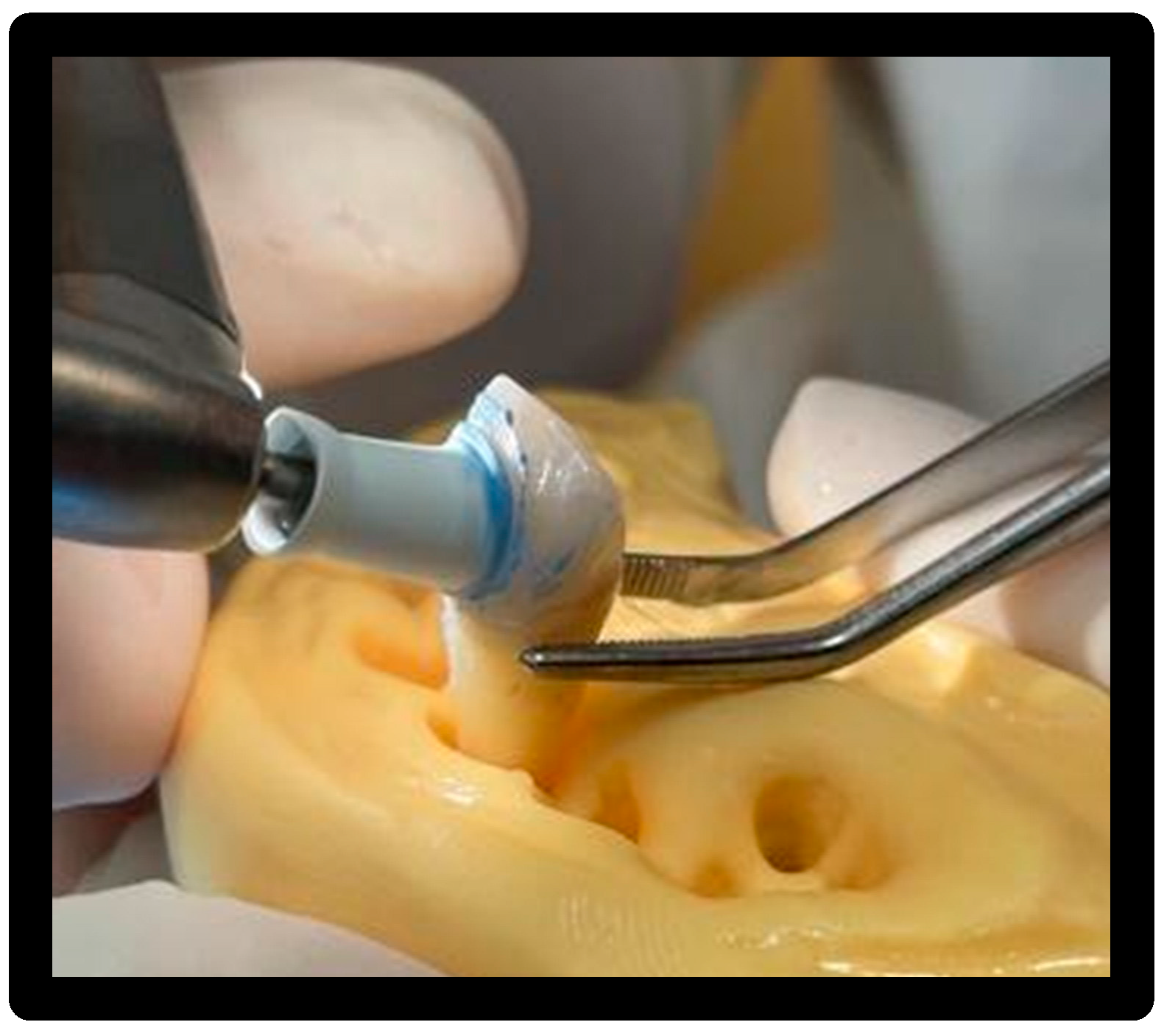
- Clearfil Twist DIA polishers in two grain sizes, dark blue and light blue (Figure 9).
2.5. Types of Treatments
- Treatment 1: prophy cup + Cleanic paste, 15′/surface at 1200 rpm.
- Treatment 2: Air-Flow with Plus powder (erythritol with CHX) with tip angle of 30 °—60 °, 5 sec/surface at 5 mm distance from the surface.
- Treatment 3: Clearfil Twist DIA rubber pads.
- 1 pass DARK BLUE 15 sec/surface with 10,000 rpm speed.
- 2 pass LIGHT BLUE 30 sec/surface with 10,000 rpm speed.
- Treatment 4: Clearfil Twist DIA rubber pads + irrigation.
- 1 pass DARK BLUE 15 sec/surface with 10,000 rpm speed.
- 2 pass LIGHT BLUE 30 sec/surface with 10,000 rpm speed.
3. Methods
3.1. Preliminary Phase
3.2. Operational Phase
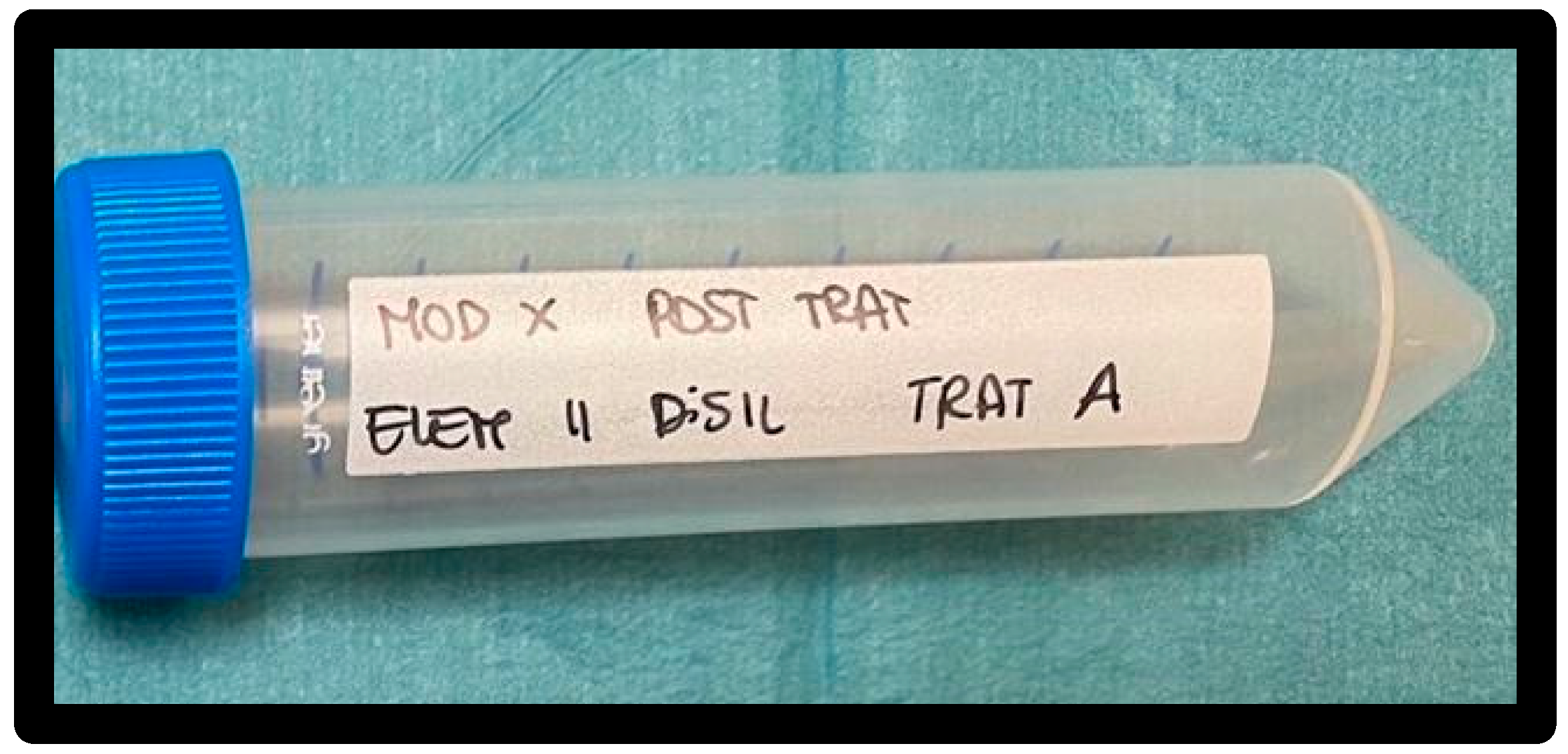
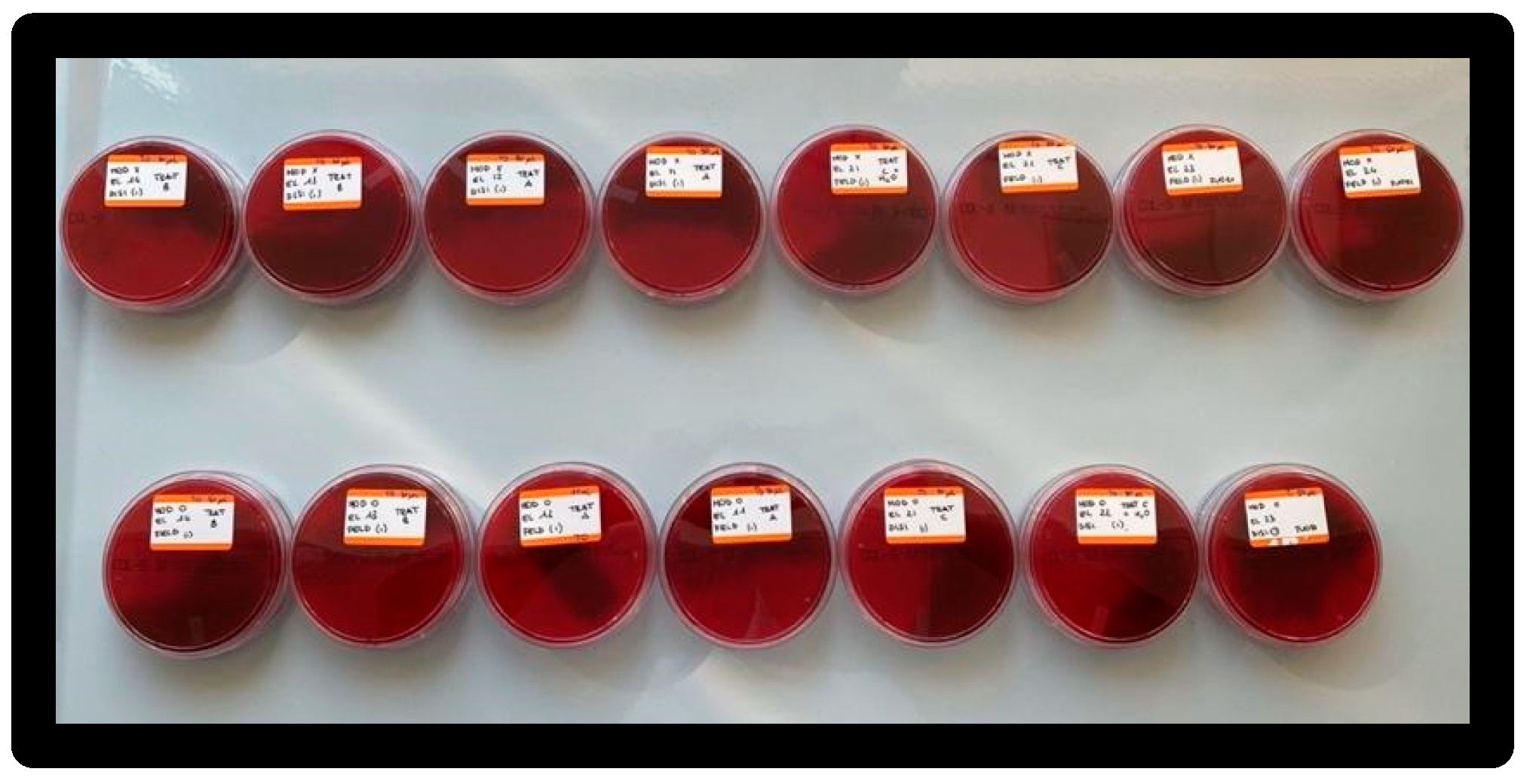
3.3. Working Groups
- GROUP A: Treatment 1—Cup with Cleanic prophy paste.
- GROUP B Treatment 2—Air-Flow with Plus powder.
- GROUP C: Treatment 3—Clearfil Twist DIA rubber pads.
- GROUP D: Treatment 4—Clearfil Twist DIA rubber pads + irrigation.
- GROUP E: Positive control.
3.4. Professional Instrumentation Techniques
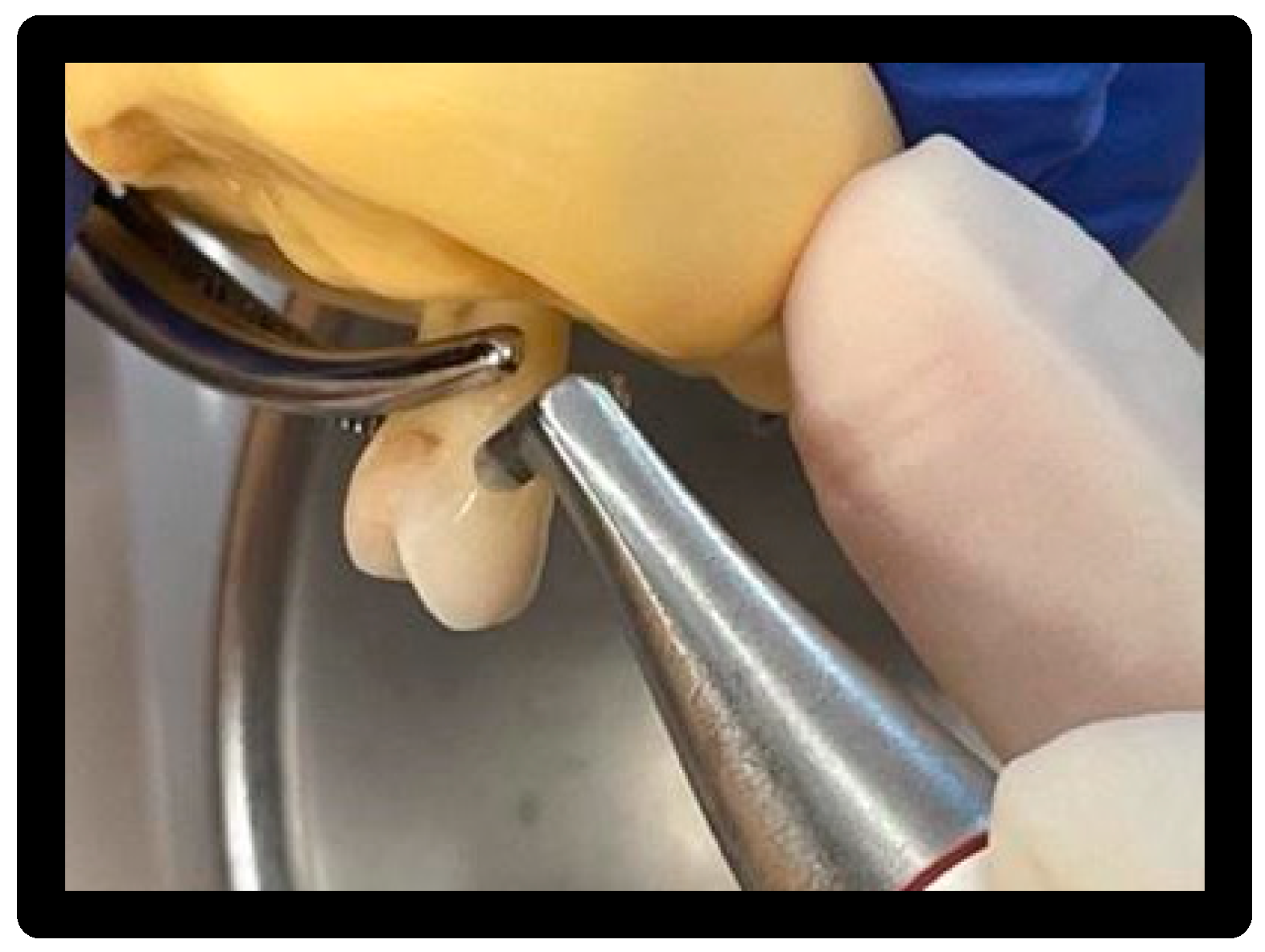
3.5. Treatment 1
- White prophy cup (WIEDER) with Cleanic® prophy paste based on perlite:
3.6. Treatment 2
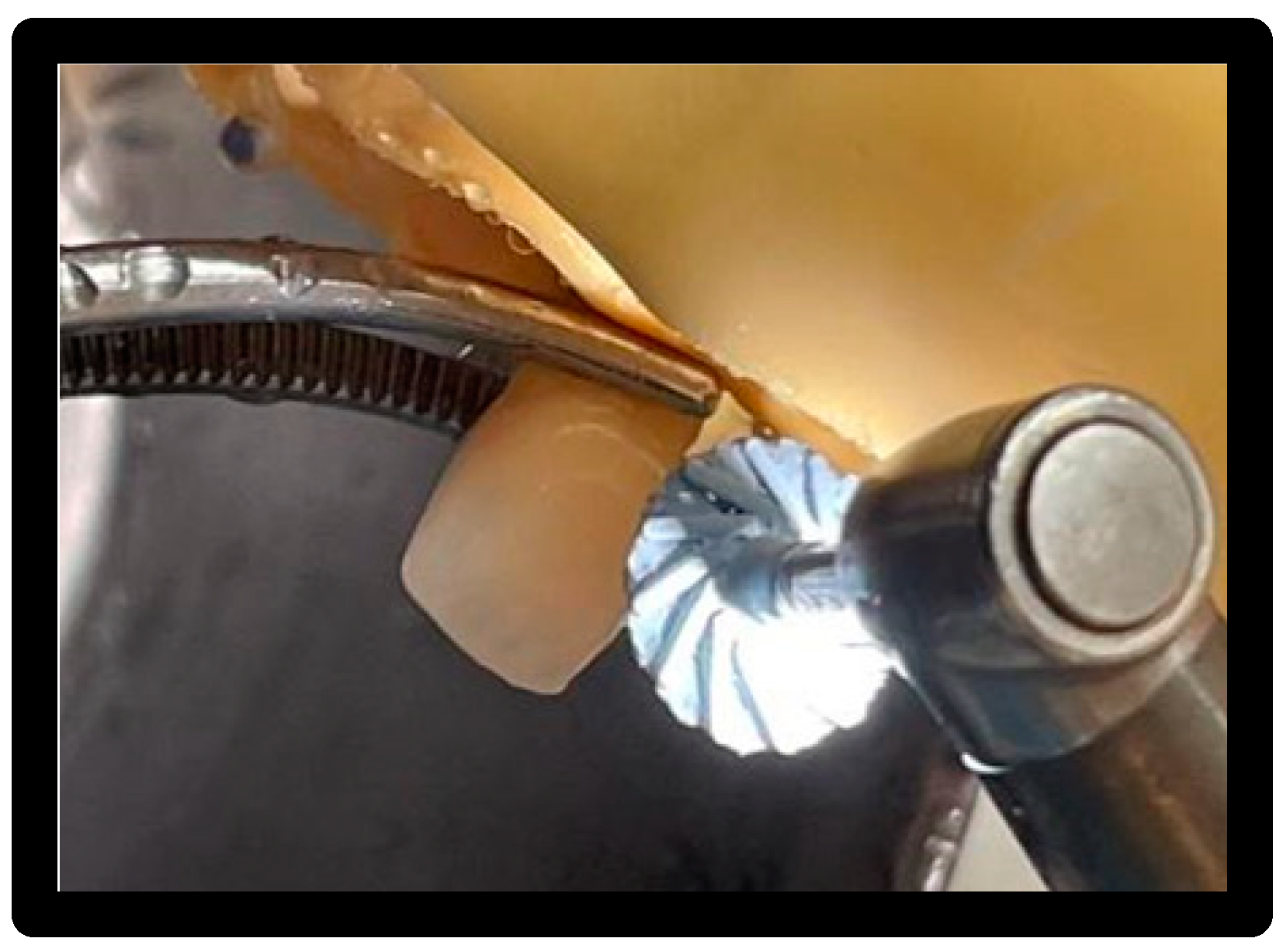
- Air-Flow Master Piezon® EMS:
3.7. Treatment 3
- Clearfil Twist DIA—dark blue and light blue:
3.8. Treatment 4
- Clearfil Twist DIA—dark blue and light blue with irrigation:
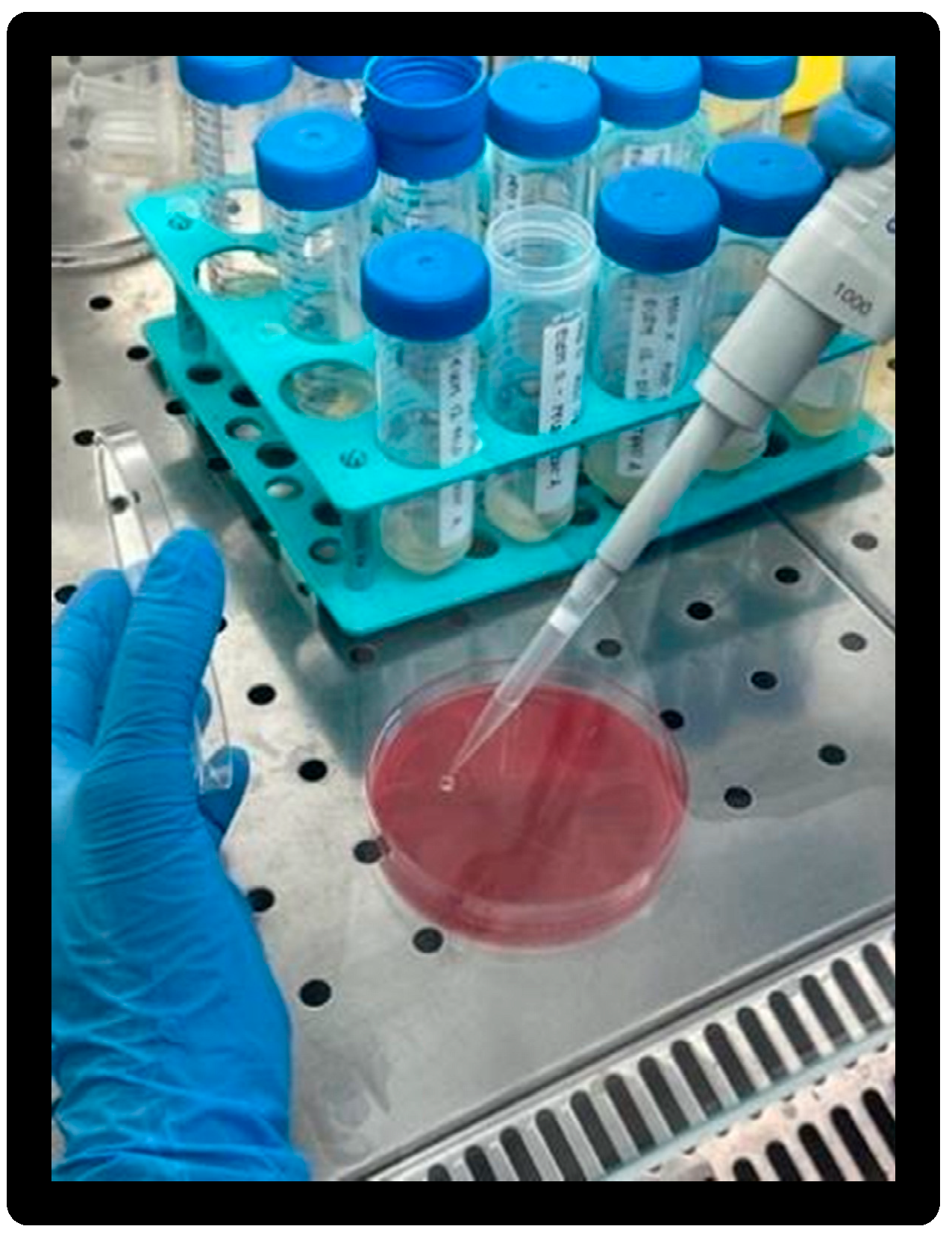
3.9. Microbiological Phase
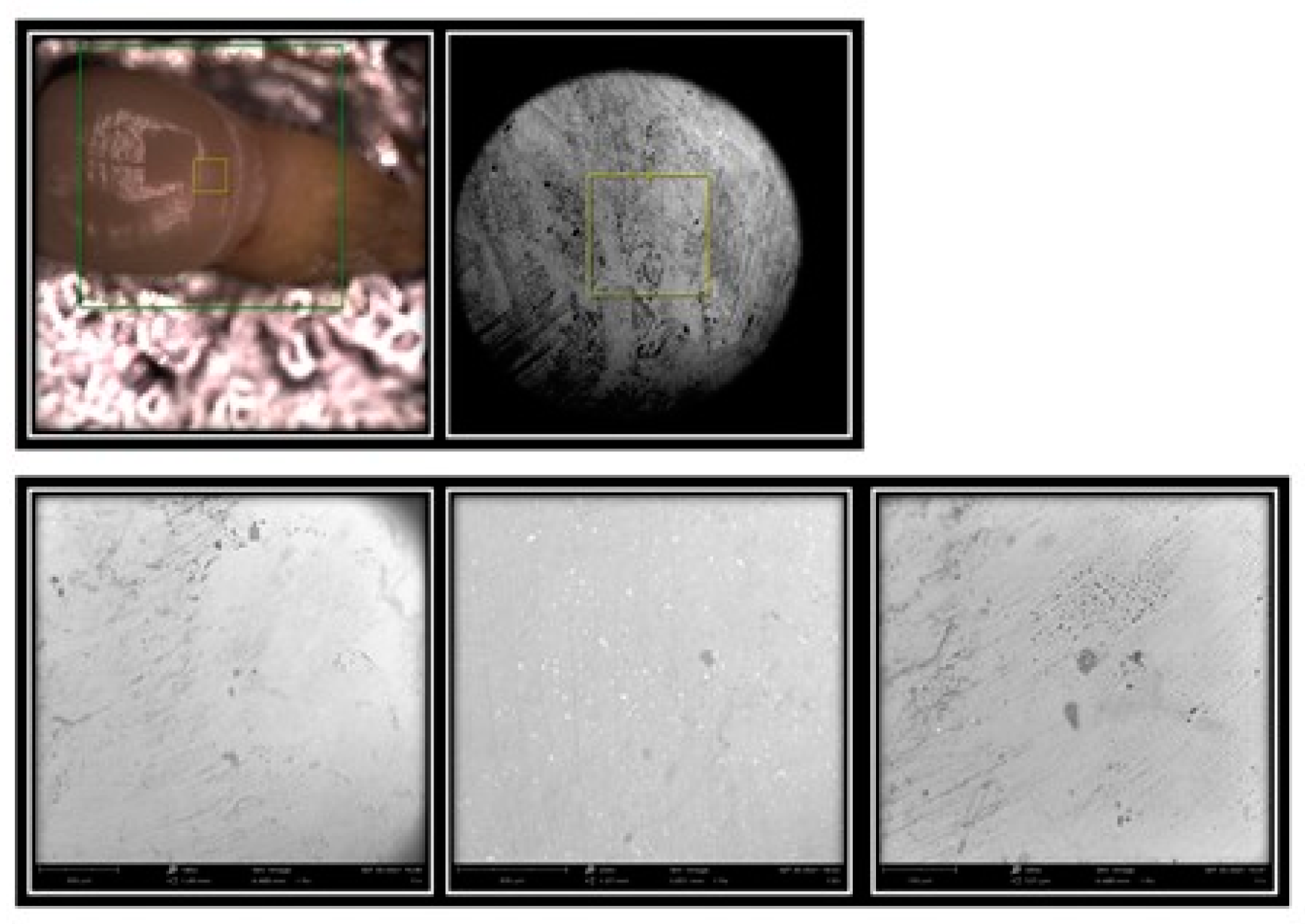
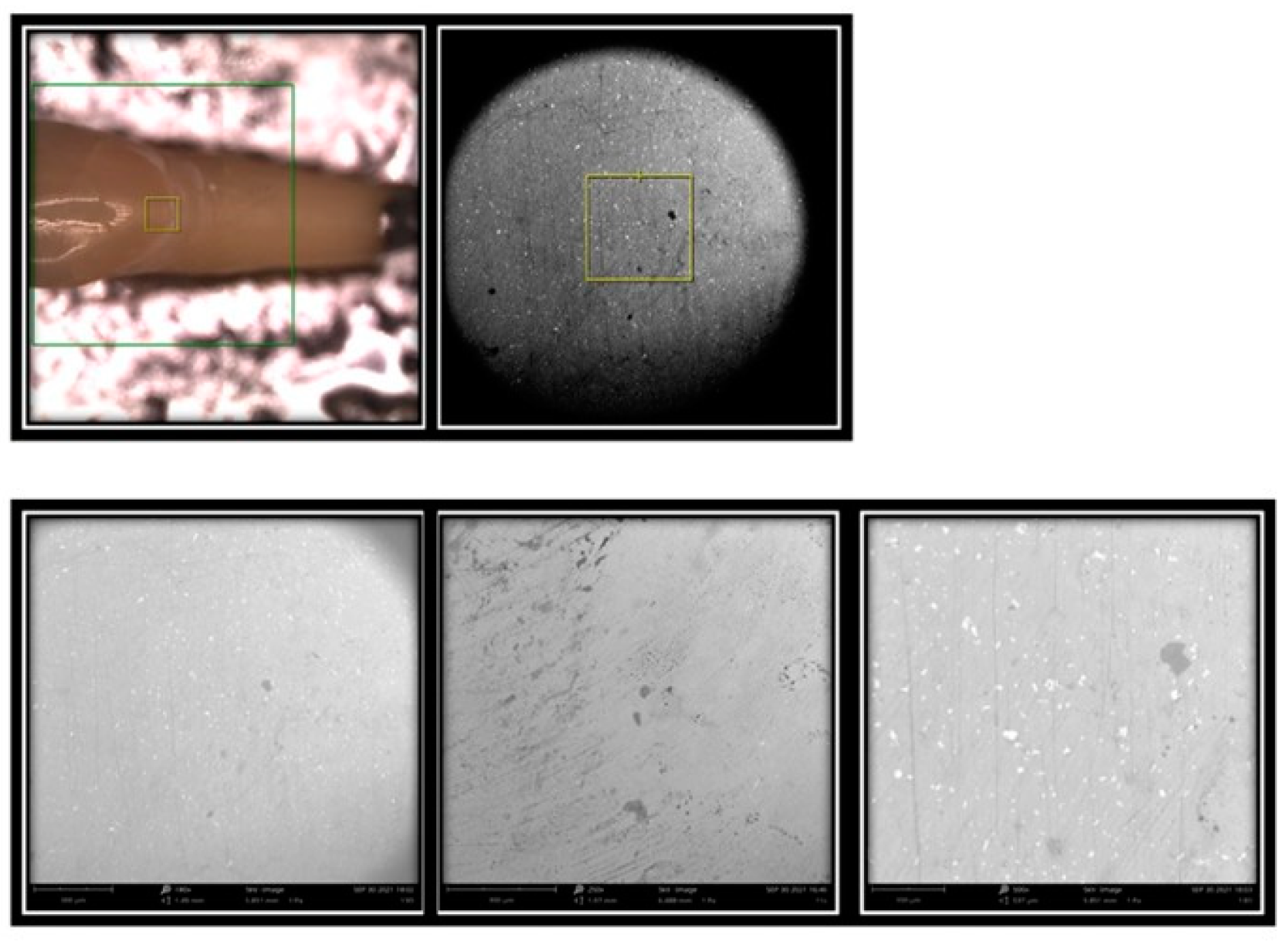
3.10. Microscopic Analysis with SEM (Scanning Electron Microscope)
4. Results
4.1. Microbiological Results
4.2. Micromorphostructural Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Capparè, P.; D’ambrosio, R.; De Cunto, R.; Darvizeh, A.; Nagni, M.; Gherlone, E. The usage of an air purifier device with HEPA 14 filter during dental procedures in COVID-19 pandemic: A randomized clinical trial. Int. J. Environ. Res. Public Health 2022, 19, 5139. [Google Scholar] [CrossRef]
- Polizzi, E.; Tetè, G. Manual vs Mechanical Oral Hygiene Procedures: Has the Role of the Dental Hygienist in Phase 2 Post-lockdown Really Changed? Oral Health Prev Dent. 2020, 18, 1031–1037. [Google Scholar] [CrossRef]
- Cattoni, F.; Teté, G.; Calloni, A.M.; Manazza, F.; Gastaldi, G.; Capparè, P. Milled versus moulded mock-ups based on the superimposition of 3D meshes from digital oral impressions: A comparative in vitro study in the aesthetic area. BMC Oral Health. 2019, 19, 230. [Google Scholar] [CrossRef]
- Tetè, G.; Polizzi, E.; D’orto, B.; Carinci, G.; Capparè, P. How to consider implant-prosthetic rehabilitation in elderly patients: A narrative review. J. Biol. Regul. Homeost. Agents 2021, 35, 119–126. [Google Scholar] [CrossRef]
- Cattoni, F.; Mastrangelo, F.; Gherlone, E.F.; Gastaldi, G. A New Total Digital Smile Planning Technique (3D-DSP) to Fabricate CAD-CAM Mockups for Esthetic Crowns and Veneers. Int. J. Dent. 2016, 2016, 6282587. [Google Scholar] [CrossRef]
- Ferrari Cagidiaco, E.; Carboncini, F.; Parrini, S.; Doldo, T.; Nagni, M.; Nuti, N.; Ferrari, M. Functional implant prosthodontic score of a one-year prospective study on three different connections for single-implant restorations. J. Osseointegration 2018, 10, 130–135. [Google Scholar] [CrossRef]
- Tecco, S.; Cattoni, F.; Darvizeh, A.; Bosco, F.; Sanci, V.; Nota, A.; Gastaldi, G.; Gherlone, E.F. Evaluation of Masticatory Muscle Function Using Digital versus Traditional Techniques for Mockup Fabrication: A Controlled Prospective Study. Appl. Sci. 2020, 10, 6013. [Google Scholar] [CrossRef]
- Cattoni, F.; Tetè, G.; Uccioli, R.; Manazza, F.; Gastaldi, G.; Perani, D. An fMRI Study on Self-Perception of Patients after Aesthetic Implant-Prosthetic Rehabilitation. Int. J. Environ. Res. Public Health 2020, 17, 588. [Google Scholar] [CrossRef]
- Crespi, R.; Capparè, P.; Polizzi, E.; Gherlone, E. Fresh-Socket Implants of Different Collar Length: Clinical Evaluation in the Aesthetic Zone. Clin. Implant. Dent. Relat. Res. 2015, 17, 871–878. [Google Scholar] [CrossRef]
- Crespi, R.; Capparè, P.; Polizzi, E.M.; Gherlone, E.F. Tissue remodeling after bone expansion in grafted and ungrafted sockets. Int. J. Oral Maxillofac. Implant. 2014, 29, 699–704. [Google Scholar] [CrossRef]
- Gastaldi, G.; Gherlone, E.; Manacorda, M.; Ferrini, F.; Bova, F.; Vinci, R.; Cattoni, F. A 3-D CAD/CAM technique in full-arch implant supported rehabilitations: The Virtual Implant-Prosthetic Procedure (VIPP Technique). A prospective longitudinal study. J. Osseointegration 2018, 10, 2–10. [Google Scholar]
- Manacorda, M.; Poletti de Chaurand, B.; Merlone, A.; Tetè, G.; Mottola, F.; Vinci, R. Virtual Implant Rehabilitation of the Severely Atrophic Maxilla: A Radiographic Study. Dent. J. 2020, 8, 14. [Google Scholar] [CrossRef]
- Cattoni, F.; Chirico, L.; Merlone, A.; Manacorda, M.; Vinci, R.; Gherlone, E.F. Digital Smile Designed Computer-Aided Surgery versus Traditional Workflow in “All on Four” Rehabilitations: A Randomized Clinical Trial with 4-Years Follow-Up. Int. J. Environ. Res. Public Health 2021, 18, 3449. [Google Scholar] [CrossRef]
- Manazza, F.; La Rocca, S.; Nagni, M.; Chirico, L.; Cattoni, F. A simplified digital workflow for the prosthetic finishing of implant rehabilitations: A case report. J. Biol. Regul. Homeost. Agents 2021, 35, 87–97. [Google Scholar] [CrossRef]
- Rebba, B.; Merlone, A.; Cantile, N.; Manazza, F.; Cattoni, F. Digital smile planning technique applied to prosthetic rehabilitation of dental esthetic area: A case report. J. Biol. Regul. Homeost. Agents 2021, 35, 1–9. [Google Scholar] [CrossRef]
- Lazetera, A.; Cattoni, F. Manual manufacturing of zirconia. Dent. Cadmos 2010, 78, 51–56. [Google Scholar]
- Gherlone, E.; Bollero, R.; Dolci, A.; Cattoni, F. The preparation of abutment-teeth with subgingival crown technique|La tecnica dei solchi guida nella preparazione dei denti pilastro. PROtech 2008, 9, 7–16. [Google Scholar]
- Cattoni, F.; Tetè, G.; D’orto, B.; Bergamaschi, A.; Polizzi, E.; Gastaldi, G. Comparison of hygiene levels in metal-ceramic and stratified zirconia in prosthetic rehabilitation on teeth and implants: A retrospective clinical study of a three-year follow-up. J. Biol. Regul. Homeost. Agents 2021, 35, 41–49. [Google Scholar] [CrossRef]
- Cappare, P.; Ferrini, F.; Mariani, G.; Nagni, M.; Cattoni, F. Implant rehabilitation of edentulous jaws with predominantly monolithic zirconia compared to metal-acrylic prostheses: A 2-year retrospective clinical study. J. Biol. Regul. Homeost. Agents 2021, 35, 99–112. [Google Scholar] [CrossRef]
- Cattoni, F.; Merlone, A.; Broggi, R.; Manacorda, M.; Vinci, R. Computer-assisted prosthetic planning and implant design with integrated digital bite registration: A treatment protocol. J. Biol. Regul. Homeost. Agents 2021, 35, 11–29. [Google Scholar] [CrossRef]
- Cattoni, F.; Chirico, L.; Cantile, N.; Merlone, A. Traditional prosthetic workflow for implant rehabilitations with a reduced number of fixtures: Proposal of a protocol. J. Biol. Regul. Homeost. Agents 2021, 35, 31–40. [Google Scholar] [CrossRef]
- Siadat, H.; Alikhasi, M.; Beyabanaki, E. Interim Prosthesis Options for Dental Implants. J Prosthodont. 2017, 26, 331–338. [Google Scholar] [CrossRef]
- Peumans, M.; Van Meerbeek, B.; Lambrechts, P.; Vanherle, G. Porcelain veneers: A review of the literature. J. Dent. 2000, 28, 163–177. [Google Scholar] [CrossRef]
- Tetè, G.; D’orto, B.; Ferrante, L.; Polizzi, E.; Cattoni, F. Role of mast cells in oral inflammation. J. Biol. Regul. Homeost. Agents 2021, 35, 65–70. [Google Scholar] [CrossRef]
- Merlone, A.; Tetè, G.; Cantile, N.; Manacorda, M.; Cattoni, F. Minimally invasive digital implant-prosthetic procedure in “all on 4” rehabilitation in patients with special needs: A three-year follow-up. J. Biol. Regul. Homeost. Agents 2021, 35, 71–85. [Google Scholar] [CrossRef]
- Tetè, G.; Cattoni, F.; Polizzi, E. Anti-discoloration system: A new chlorhexidine mouthwash. J. Biol. Regul. Homeost. Agents 2021, 35, 113–118. [Google Scholar] [CrossRef]
- Polizzi, E.; D’orto, B.; Tomasi, S.; Tetè, G. A micromorphological/microbiological pilot study assessing three methods for the maintenance of the implant patient. Clin. Exp. Dent. Res. 2021, 7, 156–162. [Google Scholar] [CrossRef]
- Angiero, F.; Ugolini, A.; Cattoni, F.; Bova, F.; Blasi, S.; Gallo, F.; Cossellu, G.; Gherlone, E. Evaluation of bradykinin, VEGF, and EGF biomarkers in gingival crevicular fluid and comparison of PhotoBioModulation with conventional techniques in periodontitis: A split-mouth randomized clinical trial. Lasers Med. Sci. 2020, 35, 965–970. [Google Scholar] [CrossRef]
- Mastrangelo, F.; Dedola, A.; Cattoni, F.; Ferrini, F.; Bova, F.; Tatullo, M.; Gherlone, E.; Lo Muzio, L. Etiological periodontal treatment with and without low-level laser therapy on IL-1β level in gingival crevicular fluid: An in vivo multicentric pilot study. J. Biol. Regul. Homeost. Agents 2018, 32, 425–431. [Google Scholar]
- Cattoni, F.; Pappalardo, S.; Vettese, P.; Santoro, G.; Gherlone, E. The laser technology in impression-taking technique and soft tissues management La tecnologia laser nel rilievo delle impronte in protesi fissa e nella gestione dei tessuti molli. PROtech 2007, 8, 17–27. [Google Scholar]
- Polizzi, E.; Tetè, G.; Targa, C.; Salviato, B.; Ferrini, F.; Gastaldi, G. Evaluation of the Effectiveness of the Use of the Diode Laser in the Reduction of the Volume of the Edematous Gingival Tissue after Causal Therapy. Int. J. Environ. Res. Public Health 2020, 17, 6192. [Google Scholar] [CrossRef]
- Tetè, G.; Sacchi, L.; Camerano, C.; Nagni, M.; Capelli, O.; Giuntoli Vercellin, S.; La Rocca, G.; Polizzi, E. Management of the delicate phase of the temporary crown: An in vitro study. J. Biol. Regul. Homeost. Agents 2020, 34, 69–80. [Google Scholar]
- Gresnigt, M.M.M.; Cune, M.S.; Jansen, K.; van der Made, S.A.M.; Özcan, M. Randomized clinical trial on indirect resin composite and ceramic laminate veneers: Up to 10-year findings. J. Dent. 2019, 86, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Menini, M.; Delucchi, F.; Bagnasco, F.; Pera, F.; Di Tullio, N.; Pesce, P. Efficacy of air-polishing devices without removal of implant-supported full-arch prostheses. Int. J. Oral Implantol. 2021, 14, 401–416. [Google Scholar]
- Park, C.; Vang, M.S.; Park, S.W.; Lim, H.P. Effect of various polishing systems on the surface roughness and phase transformation of zirconia and the durability of the polishing systems. J. Prosthet. Dent. 2017, 117, 430–437. [Google Scholar] [CrossRef] [PubMed]








| Tooth Element | T0 | T1 | T2 |
|---|---|---|---|
| X 11 disilicate- PROC.1CUP | 1.5 × 108 | 4 × 105 | 8 × 105 |
| X 12 disilicate- PROC.1CUP | 1.5 × 108 | 1.6 × 105 | 3.2 × 105 |
| X13 disilicate- PROC. 2 AIR FLOW | 1.5 × 108 | 2.4 × 105 | 7.2 × 105 |
| X14 disilicate- PROC. 2 AIR FLOW | 1.5 × 108 | 9 × 104 | 2.7 × 105 |
| 021 disilicate- PROC.3 gum | 1.5 × 108 | 1.54 × 105 | 6.16 × 105 |
| 022 disilicate- PROC.3 gum + H2o | 1.5 × 108 | 2.1 × 105 | 8.4 × 105 |
| 023 disilicate- ctr. | 1.5 × 108 | 3.5 × 105 | 1.4 × 104 |
| Tooth Element | T0 | T1 | T2 |
|---|---|---|---|
| O 11 feldspathic- PROC.1CUP | 1.5 × 108 | 1.8 × 105 | 5.2 × 105 |
| O 12 feldspathic- PROC.1CUP | 1.5 × 108 | 1.5 × 105 | 6 × 105 |
| 0 13 feldspathic- PROC. 2 AIR FLOW | 1.5 × 108 | 1.5 × 105 | 6 × 105 |
| 0 14 feldspathic- PROC. 2 AIR FLOW | 1.5 × 108 | 1.5 × 104 | 4.5 × 105 |
| X 22 feldspathic- PROC.3 gum | 1.5 × 108 | 1.8 × 105 | 5.4 × 105 |
| X 21 feldspathic- PROC.3 gum + H2o | 1.5 × 108 | 1.5 × 105 | 4.5 × 105 |
| X 23 feldspathic- ctr. | 1.5 × 108 | 5 × 105 | 1.5 × 106 |
| X 24 feldspathic- ctr. | 1.5 × 108 | 6 × 105 | 1.8 × 106 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Petto, L.F.; Tetè, G.; Hera, M.; Polizzi, E. Aesthetic Restorations: The Role of The Dental Hygienist in Professional Maintenance: In Vitro Microbiological Study. Materials 2023, 16, 1373. https://doi.org/10.3390/ma16041373
Di Petto LF, Tetè G, Hera M, Polizzi E. Aesthetic Restorations: The Role of The Dental Hygienist in Professional Maintenance: In Vitro Microbiological Study. Materials. 2023; 16(4):1373. https://doi.org/10.3390/ma16041373
Chicago/Turabian StyleDi Petto, Lorenza Francesca, Giulia Tetè, Mara Hera, and Elisabetta Polizzi. 2023. "Aesthetic Restorations: The Role of The Dental Hygienist in Professional Maintenance: In Vitro Microbiological Study" Materials 16, no. 4: 1373. https://doi.org/10.3390/ma16041373
APA StyleDi Petto, L. F., Tetè, G., Hera, M., & Polizzi, E. (2023). Aesthetic Restorations: The Role of The Dental Hygienist in Professional Maintenance: In Vitro Microbiological Study. Materials, 16(4), 1373. https://doi.org/10.3390/ma16041373







