Bonding Strength of Various Luting Agents between Zirconium Dioxide Crowns and Titanium Bonding Bases after Long-Term Artificial Chewing
Abstract
:1. Introduction
2. Materials and Methods
- SpeedCEM Plus (Ivoclar Vivadent AG, Schaan, Liechtenstein)
- Panavia SA Cement Universal (Kuraray Noritake Dental, Inc., Okayama, Japan)
- Panavia V5 (Kuraray Noritake Dental, Inc.)
- RelyX Unicem 2 Automix (3M Espe, Seefeld, Germany)
- VITA ADIVA IA-Cem (VITA Zahnfabrik, Bad Säckingen, Germany)
- Ketac CEM (Aplicap) (3M Espe, Seefeld, Germany)
- Hoffmann’s Phosphate Cement (Hoffman Dental Manufaktur GmbH, Berlin, Germany)
3. Results
4. Discussion
5. Conclusions
- Most of the luting agents tested in the current investigation are suitable for “cementation” of a zirconium dioxide hybrid abutment crown onto a titanium bonding base since the debonding forces are above a recommended value (159 N).
- The use of self-adhesive cements yielded the highest bonding strength for bonding a zirconium dioxide hybrid abutment crown onto a titanium bonding base after long-term artificial fatigue and aging.
- The adhesive bond to zirconium dioxide is more vulnerable than the adhesive bond to titanium.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pjetursson, B.E.; Sailer, I.; Latyshev, A.; Rabel, K.; Kohal, R.; Karasan, D. A Systematic Review and Meta-analysis Evaluating the Survival, the Failure, and the Complication Rates of Veneered and Monolithic All-ceramic Implant-supported Single Crowns. Clin. Oral Implant. Res. 2021, 32, 254–288. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Lai, Y.; Qian, S.; Qiao, S.; Tonetti, M.S.; Lai, H. Clinical, Radiographic and Economic Evaluation of Short-6-mm Implants and Longer Implants Combined with Osteotome Sinus Floor Elevation in Moderately Atrophic Maxillae: A 3-year Randomized Clinical Trial. J. Clin. Periodontol. 2021, 48, 695–704. [Google Scholar] [CrossRef] [PubMed]
- Mazza, L.C.; Lemos, C.A.A.; Pesqueira, A.A.; Pellizzer, E.P. Survival and Complications of Monolithic Ceramic for Tooth-Supported Fixed Dental Prostheses: A Systematic Review and Meta-Analysis. J. Prosthet. Dent. 2022, 128, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Korsch, M.; Marten, S.-M.; Walther, W.; Vital, M.; Pieper, D.H.; Dötsch, A. Impact of Dental Cement on the Peri-Implant Biofilm-Microbial Comparison of Two Different Cements in an in Vivo Observational Study. Clin. Implant Dent. Relat. Res. 2018, 20, 806–813. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T.G., Jr. The Positive Relationship Between Excess Cement and Peri-Implant Disease: A Prospective Clinical Endoscopic Study. J. Periodontol. 2009, 80, 1388–1392. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Polo, M.; Ortega, R.; Gómez-Polo, C.; Celemin, A.; Del Rio Highsmith, J. Factors Affecting the Decision to Use Cemented or Screw-Retained Fixed Implant-Supported Prostheses: A Critical Review. Int. J. Prosthodont. 2018, 31, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Hahnel, S. Vollkeramische implantatgetragene Versorgungen: State of the Art? Wissen Kompakt 2017, 11, 55–64. [Google Scholar] [CrossRef]
- Alsahhaf, A.; Spies, B.C.; Vach, K.; Kohal, R.-J. Fracture Resistance of Zirconium Dioxide-Based Implant Abutments after Artificial Long-Term Aging. J. Mech. Behav. Biomed. Mater. 2017, 66, 224–232. [Google Scholar] [CrossRef]
- Stimmelmayr, M.; Edelhoff, D.; Güth, J.-F.; Erdelt, K.; Happe, A.; Beuer, F. Wear at the Titanium–Titanium and the Titanium–Zirconium dioxide Implant–Abutment Interface: A Comparative in Vitro Study. Dent. Mater. 2012, 28, 1215–1220. [Google Scholar] [CrossRef]
- Edelhoff, D.; Schweiger, J.; Prandtner, O.; Stimmelmayr, M.; Güth, J.-F. Metal-Free Implant-Supported Single-Tooth Restorations. Part II: Hybrid Abutment Crowns and Material Selection. Quintessence Int. 2019, 50, 260–269. [Google Scholar] [CrossRef]
- Matos, J.D.; Arcila, L.V.; Ortiz, L.P.; Lopes, G.R.; Anami, L.C.; Ramos, N.C.; Saavedra, G.S.; Tribst, J.P.; Bottino, M.A. Hybrid Abutment during Prosthetic Planning and Oral Rehabilitation. Minerva Dent. Oral Sci. 2022, 71, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Nouh, I.; Kern, M.; Sabet, A.E.; Aboelfadl, A.K.; Hamdy, A.M.; Chaar, M.S. Mechanical Behavior of Posterior All-Ceramic Hybrid-Abutment-Crowns versus Hybrid-Abutments with Separate Crowns-A Laboratory Study. Clin. Oral Implant. Res. 2019, 30, 90–98. [Google Scholar] [CrossRef]
- Naumann, M.; Scholz, P.; Krois, J.; Schwendicke, F.; Sterzenbach, G.; Happe, A. Monolithic Hybrid Abutment Crowns (Screw-Retained) versus Monolithic Hybrid Abutments with Adhesively Cemented Monolithic Crowns. Three-Year Data of a Randomized Prospective Clinical Pilot Study. Clin. Oral Implant. Res. 2023, 34, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Brägger, U. Complete Digital Workflow for the Production of Implant-Supported Single-Unit Monolithic Crowns. Clin. Oral Implant. Res. 2014, 25, 1304–1306. [Google Scholar] [CrossRef] [PubMed]
- Guncu, M.; Aktas, G.; Guncu, G.; Anıl, D.; Turkyilmaz, I.; Antonoff, L. Clinical, Technical, and Radiologic Outcomes of 182 Implant-Supported Zirconium Dioxide Single Crowns Using Titanium-Base Abutments: A Retrospective Study. Int. J. Prosthodont. 2022, 35, 553–559. [Google Scholar] [CrossRef] [PubMed]
- Karasan, D.; Sailer, I.; Demir, F.; Akca, K. Screw-retained Monolithic Zirconium dioxide Implant Restorations Supported by Titanium Base Abutments Produced with Complete Digital Work-flow: A Retrospective Cohort up-to 4-year Follow-up. Clin. Oral Implant. Res. 2020, 31, 211. [Google Scholar] [CrossRef]
- Takano, R.; Honda, J.; Kobayashi, T.; Kubochi, K.; Takata, H.; Komine, F. Fracture Strength of Implant-Supported Hybrid Abutment Crowns in Premolar Region Fabricated Using Different Restorative CAD/CAM Materials. Dent. Mater. J. 2023, 42, 187–192. [Google Scholar] [CrossRef]
- Schweiger, J.; Edelhoff, D.; Beuer, F.; Stimmelmayr, M. Part 1: The Road to Implant Abutments. IDT Inside Dent. Technol. 2014, 5. Available online: https://www.aegisdentalnetwork.com/idt/2014/06/part-1-the-road-to-implant-abutments (accessed on 16 November 2023).
- Beuer, F.; Groesser, J.; Schweiger, J.; Hey, J.; Güth, J.-F.; Stimmelmayr, M. The Digital One-Abutment/One-Time Concept. A Clinical Report: Digital One-Abutment/One-Time. J. Prosthodont. 2015, 24, 580–585. [Google Scholar] [CrossRef]
- Beuer, F.; Herklotz, I.; Schweiger, J.; Stimmelmayr, M. Update Zu CAD/CAM-Gefertigten Suprakonstruktionen. Implantologie 2018, 25, 35–40. [Google Scholar]
- Adolfi, D.; Tribst, J.; Borges, A.; Bottino, M. Torque Maintenance Capacity, Vertical Misfit, Load to Failure, and Stress Concentration of Zirconium dioxide Restorations Cemented or Notched to Titanium Bases. Int. J. Oral Maxillofac. Implant. 2020, 35, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Bömicke, W. Befestigungsmaterialien in der restaurativen Zahnheilkunde. Wissen Kompakt 2015, 9, 163–178. [Google Scholar] [CrossRef]
- Behr, M.; Belli, R.; Boccaccini, A.R.; Forstreuter, J.; Frankenberger, R.; Gbureck, U. Werkstoffkunde in der Zahnmedizin: Moderne Materialien und Technologien: 442 Abbildungen; Rosentritt, M., Ilie, N., Lohbauer, U., Eds.; Georg Thieme Verlag: Stuttgart, Germany; New York, NY, USA, 2018; ISBN 978-3-13-240108-2. [Google Scholar]
- Smith, D.C. Development of Glass-Ionomer Cement Systems. Biomaterials 1998, 19, 467–478. [Google Scholar] [CrossRef] [PubMed]
- Lad, P.P.; Kamath, M.; Tarale, K.; Kusugal, P.B. Practical Clinical Considerations of Luting Cements: A Review. J. Int. Oral Health 2014, 6, 116–120. [Google Scholar] [PubMed]
- Agar, J.R.; Cameron, S.M.; Hughbanks, J.C.; Parker, M.H. Cement Removal from Restorations Luted to Titanium Abutments with Simulated Subgingival Margins. J. Prosthet. Dent. 1997, 78, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Gehrt, M.; Wolfart, S.; Rafai, N.; Reich, S.; Edelhoff, D. Clinical Results of Lithium-Disilicate Crowns after up to 9 Years of Service. Clin. Oral Investig. 2013, 17, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Donovan, T.; Simonsen, R.J.; Guertin, G.; Tucker, R.V. Retrospective clinical evaluation of 1314 cast gold restorations in service from 1 to 52 years. J. Esthet. Restor. Dent. 2004, 16, 194–204. [Google Scholar] [CrossRef]
- Rohr, N.; Fischer, J. Effect of Aging and Curing Mode on the Compressive and Indirect Tensile Strength of Resin Composite Cements. Head Face Med. 2017, 13, 22. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Keul, C.; Eichberger, M.; Figge, D.; Edelhoff, D.; Lümkemann, N. Three Generations of Zirconium dioxide: From Veneered to Monolithic. Part II. Quintessence Int. 2017, 48, 441–450. [Google Scholar] [CrossRef]
- Cadenaro, M.; Josic, U.; Maravić, T.; Mazzitelli, C.; Marchesi, G.; Mancuso, E.; Breschi, L.; Mazzoni, A. Progress in Dental Adhesive Materials. J. Dent. Res 2023, 102, 254–262. [Google Scholar] [CrossRef]
- de Matos, J.D.M.; Gomes, L.S.; de Carvalho Ramos, N.; Queiroz, D.A.; Tribst, J.P.M.; Campos, T.M.B.; Borges, A.L.S.; da Rocha Scalzer Lopes, G.; Bottino, M.A.; Paes Junior, T.J.A. Influence of CAD/CAM Abutment Heights on the Biomechanical Behavior of Zirconium dioxide Single Crowns. Metals 2022, 12, 2025. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Liebermann, A.; Kieschnick, A. Befestigung “Step-by-Step” Zirkonoxid. 2017. Available online: https://eadt.de/downloads/befestigung-step-step-zirkonoxid (accessed on 16 November 2023).
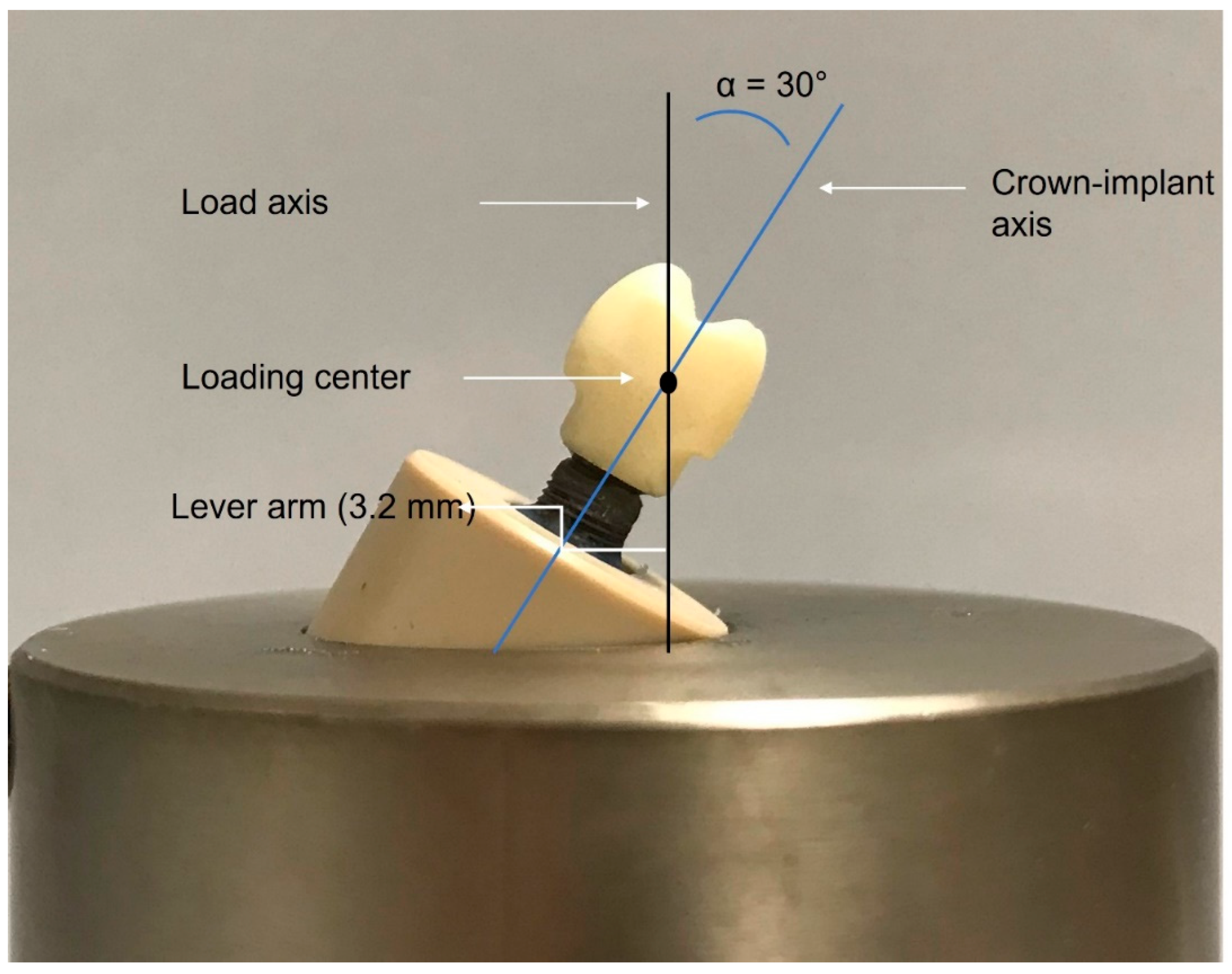
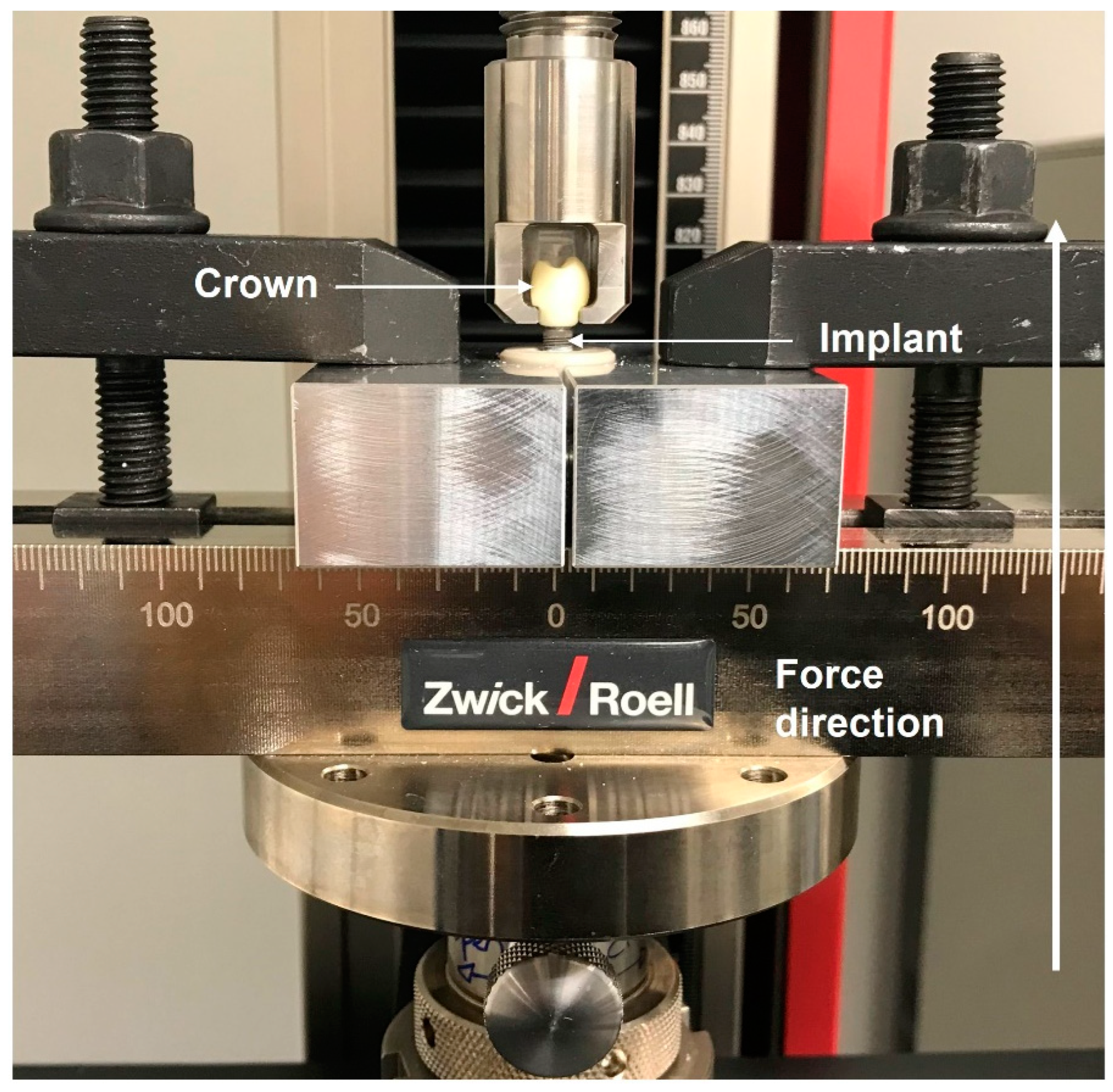
- ISO 14801:2016; Dentistry—Implants—Dynamic Loading Test for Endosseous Dental Implants. ISO: Geneva, Switzerland, 2016. Available online: https://www.iso.org/standard/61997.html (accessed on 16 November 2023).
- Bitter, K.; Schubert, A.; Neumann, K.; Blunck, U.; Sterzenbach, G.; Rüttermann, S. Are Self-Adhesive Resin Cements Suitable as Core Build-up Materials? Analyses of Maximum Load Capability, Margin Integrity, and Physical Properties. Clin. Oral Investig. 2016, 20, 1337–1345. [Google Scholar] [CrossRef] [PubMed]
- Bagegni, A.; Weihrauch, V.; Vach, K.; Kohal, R. The Mechanical Behavior of a Screwless Morse Taper Implant–Abutment Connection: An In Vitro Study. Materials 2022, 15, 3381. [Google Scholar] [CrossRef] [PubMed]
- Outhwaite, W.C.; Twiggs, S.W.; Fairhurst, C.W.; King, G.E. Slots vs. pins: A comparison of retention under simulated chewing stresses. J. Dent. Res. 1982, 61, 400–402. [Google Scholar] [CrossRef] [PubMed]
- White, S.N.; Yu, Z. Compressive and Diametral Tensile Strengths of Current Adhesive Luting Agents. J. Prosthet. Dent. 1993, 69, 568–572. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Beuer, F.; Ender, A.; Roos, M.; Edelhoff, D.; Wimmer, T. Influence of Cementation and Cement Type on the Fracture Load Testing Methodology of Anterior Crowns Made of Different Materials. Dent. Mater. J. 2013, 32, 888–895. [Google Scholar] [CrossRef] [PubMed]
- Rohr, N.; Märtin, S.; Fischer, J. Correlations between Fracture Load of Zirconium dioxide Implant Supported Single Crowns and Mechanical Properties of Restorative Material and Cement. Dent. Mater. J. 2018, 37, 222–228. [Google Scholar] [CrossRef]
- Raju, S.; Nair, V.; Karunakaran, H.; Manjuran, N. Management of Perishing Implants with Abutment Screw Fracture—A Systematic Review. J. Indian Prosthodont. Soc. 2021, 21, 229–239. [Google Scholar] [CrossRef]
- Katsavochristou, A.; Koumoulis, D. Incidence of Abutment Screw Failure of Single or Splinted Implant Prostheses: A Review and Update on Current Clinical Status. J. Oral Rehabil. 2019, 46, 776–786. [Google Scholar] [CrossRef]
- Winkler, S.; Ring, K.; Ring, J.D.; Boberick, K.G. Implant Screw Mechanics and the Settling Effect: Overview. J. Oral Implantol. 2003, 29, 242–245. [Google Scholar] [CrossRef]
- Mehta, S.; Kalra, T.; Kumar, M.; Bansal, A.; Avasthi, A.; Malik, S.S. To Evaluate the Solubility of Different Permanent and Temporary Dental Luting Cements in Artificial Saliva of Different PH Values at Different Time Intervals—An In Vitro Study. Dent. J. Adv. Stud. 2020, 8, 92–101. [Google Scholar] [CrossRef]
- Chang, J.C.; Hart, D.A.; Estey, A.W.; Chan, J.T. Tensile Bond Strengths of Five Luting Agents to Two CAD-CAM Restorative Materials and Enamel. J. Prosthet. Dent. 2003, 90, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Arce, C.; Lawson, N.; Liu, P.-R.; Lin, C.; Givan, D. Retentive Force of Zirconium dioxide Implant Crowns on Titanium Bases Following Different Surface Treatments. Int. J. Oral Maxillofac. Implant. 2018, 33, 530–535. [Google Scholar] [CrossRef] [PubMed]
- Güngör, M.; Nemli, S. The Effect of Resin Cement Type and Thermomechanical Aging on the Retentive Strength of Custom Zirconium dioxide Abutments Bonded to Titanium Inserts. Int. J. Oral Maxillofac. Implant. 2018, 33, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Mehl, C.; Zhang, Q.; Lehmann, F.; Kern, M. Retention of Zirconium dioxide on Titanium in Two-Piece Abutments with Self-Adhesive Resin Cements. J. Prosthet. Dent. 2018, 120, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Freifrau von Maltzahn, N.; Bernard, S.; Kohorst, P. Two-part Implant Abutments with Titanium and Ceramic Components: Surface Modification Affects Retention Forces—An In-Vitro Study. Clin. Oral Implant. Res. 2019, 30, 903–909. [Google Scholar] [CrossRef]
- Wiedenmann, F.; Liebermann, A.; Spintzyk, S.; Eichberger, M.; Stawarczyk, B. Influence of Different Cleaning Procedures on Tensile Bond Strength between Zirconium Dioxide Abutment and Titanium Base. Int. J. Oral Maxillofac. Implant. 2019, 34, 1318–1327. [Google Scholar] [CrossRef]
- Hansen, N.A.; Wille, S.; Kern, M. Effect of Reduced Airborne-Particle Abrasion Pressure on the Retention of Zirconium dioxide Copings Resin Bonded to Titanium Abutments. J. Prosthet. Dent. 2020, 124, 60–67. [Google Scholar] [CrossRef]
- Oddbratt, E.; Hua, L.; Chrcanovic, B.R.; Papia, E. Bond Strength of Zirconium dioxide- or Polymer-Based Copings Cemented on Implant-Supported Titanium Bases—An in Vitro Study. Biomater. Investig. Dent. 2021, 8, 129–136. [Google Scholar] [CrossRef]
- Gehrke, P.; Alius, J.; Fischer, C.; Erdelt, K.J.; Beuer, F. Retentive Strength of Two-Piece CAD/CAM Zirconium dioxide Implant Abutments: Retentive Strength Two-Piece CAD/CAM Abutments. Clin. Implant Dent. Relat. Res. 2014, 16, 920–925. [Google Scholar] [CrossRef]
- Alvarez-Arenal, A.; Gonzalez-Gonzalez, I.; deLlanos-Lanchares, H.; Brizuela-Velasco, A.; Ellacuria-Echebarria, J. The Selection Criteria of Temporary or Permanent Luting Agents in Implant-Supported Prostheses: In Vitro Study. J. Adv. Prosthodont. 2016, 8, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Mehl, C.; Ali, S.; El Bahra, S.; Harder, S.; Vollrath, O.; Kern, M. Is There a Correlation between Tensile Strength and Retrievability of Cemented Implant-Retained Crowns Using Artificial Aging? Int. J. Prosthodont. 2016, 29, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Veselinović, V.; Marin, S.; Trtić, Z.; Trtić, N.; Dolić, O.; Adamović, T.; Arbutina, R.; Šćepanović, M.; Todorović, A. Application of Semipermanent Cements and Conventional Cement with Modified Cementing Technique in Dental Implantology. Acta Stomatol. Croat. 2021, 55, 367–379. [Google Scholar] [CrossRef] [PubMed]
- Schiessl, C.; Schaefer, L.; Winter, C.; Fuerst, J.; Rosentritt, M.; Zeman, F.; Behr, M. Factors Determining the Retentiveness of Luting Agents Used with Metal- and Ceramic-Based Implant Components. Clin. Oral Investig. 2013, 17, 1179–1190. [Google Scholar] [CrossRef] [PubMed]
- Rab, J.; Rzanny, A.; Göbel, R.; Welker, D. Experimentell–vergleichende Untersuchungen an Befestigungswerkstoffen unter besonderer Berücksichtigung von Kompositen. ZWR Dtsch. Zahnärzteblatt 2009, 118, 408–419. [Google Scholar] [CrossRef]
- Tzanakakis, E.C.; Beketova, A.; Papadopoulou, L.; Kontonasaki, E.; Tzoutzas, I.G. Novel Femto Laser Patterning of High Translucent Zirconia as an Alternative to Conventional Particle Abrasion. Dent. J. 2021, 9, 20. [Google Scholar] [CrossRef] [PubMed]
- Burkhardt, F.; Sailer, I.; Fehmer, V.; Mojon, P.; Pitta, J. Retention and Marginal Integrity of CAD/CAM Fabricated Crowns Adhesively Cemented to Titanium Base Abutments—Influence of Bonding System and Restorative Material. Int. J. Prosthodont. 2023, 36, 651. [Google Scholar] [CrossRef]
- Lennartz, A.; Dohmen, A.; Bishti, S.; Fischer, H.; Wolfart, S. Retrievability of Implant-Supported Zirconium dioxide Restorations Cemented on Zirconium dioxide Abutments. J. Prosthet. Dent. 2018, 120, 740–746. [Google Scholar] [CrossRef]
- Eldafrawy, M.; Bekaert, S.; Nguyen, J.; Sadoun, M.; Mainjot, A. Bonding Properties of Third-Generation Zirconia Cad-Cam Blocks for Monolithic Restorations to Composite and Resin-Modified Glass-Ionomer Cements. J. Prosthodont. Res. 2022, 30, 466–475. [Google Scholar] [CrossRef]
- Ebert, A.; Hedderich, J.; Kern, M. Retention of Zirconium dioxide Ceramic Copings Bonded to Titanium Abutments. Int. J. Oral Maxillofac. Implant. 2007, 22, 921–927. [Google Scholar]
- von Maltzahn, N.F.; Holstermann, J.; Kohorst, P. Retention Forces between Titanium and Zirconia Components of Two-Part Implant Abutments with Different Techniques of Surface Modification: Retention Forces of Two-Part Implant Abutments. Clin. Implant Dent. Relat. Res. 2016, 18, 735–744. [Google Scholar] [CrossRef]
- Chevalier, J.; Gremillard, L.; Virkar, A.V.; Clarke, D.R. The Tetragonal-Monoclinic Transformation in Zirconium dioxide: Lessons Learned and Future Trends. J. Am. Ceram. Soc. 2009, 92, 1901–1920. [Google Scholar] [CrossRef]
- De Souza, G.M.; Zykus, A.; Ghahnavyeh, R.R.; Lawrence, S.K.; Bahr, D.F. Effect of Accelerated Aging on Dental Zirconium dioxide-Based Materials. J. Mech. Behav. Biomed. Mater. 2017, 65, 256–263. [Google Scholar] [CrossRef]





| Components | Amount (in %) |
|---|---|
| ZrO2 + HfO2 + Y2O3 | ≥99.0 |
| Y2O3 | >4.5–≤ 6.0 |
| HfO2 | ≤5 |
| Al2O3 | ≤0.5 |
| Fe2O3 | ≤0.3 |
| Density | 6.05 ± 0.2 g cm−3 |
| Fracture toughness KIC | 5.8 MPa m1/2 |
| Thermal expansion coefficient (20–500 °C) | 11 × 10−6 K−1 |
| Bending strength | 1200 MPa |
| Cement | Air Abrasion Pressure |
|---|---|
| SpeedCEM Plus | 2 bar |
| Panavia SA Cement Universal | 2 bar |
| Panavia V5 | 2 bar |
| RelyX Unicem 2 Automix | 2 bar |
| VITA ADIVA IA-Cem | 1.5 bar |
| Ketac CEM (Aplicap) | 1 bar |
| Hoffmann’s Phosphate Cement | 1 bar |
| Group (Number of Samples) | Cement Type | Type and Chemical Components | Special Features, Preparation, Processing |
|---|---|---|---|
| Group 1 (n = 8) | SpeedCEM Plus | Resin cement: long-chain methacrylate with a phosphoric acid monomer (MDP), barium glass, ytterbium trifluoride, co-polymer, and highly dispersed silicon dioxide |
|
| Group 2 (n = 8) | Panavia SA Cement Universal | Resin cement: 10-methacryloyloxydecyl dihydrogen phosphate (MDP), bisphenol A diglycidylmethacrylate (Bis-GMA), triethyleneglycol dimethacrylate (TEGDMA), hydrophobic aromatic dimethacrylate, 2-hydroxymethacrylate (HEMA), silanated barium glass filler, silanated colloidal silica, dl-camphorquinone, peroxide, catalysts, and pigments |
|
| Group 3 (n = 8) | Panavia V5 | Resin cement: Paste A: bisphenol A diglycidylmethacrylate (Bis-GMA), triethyleneglycol dimethacrylate (TEGDMA), hydrophobic aromatic dimethacrylate, hydrophilic aliphatic dimethacrylate, initiators, accelerators, silanated barium glass filler, silanated fluoroalminosilicate glass filler, and colloidal silica Paste B: bisphenol A diglycidylmethacrylate (Bis-GMA), hydrophobic aromatic dimethacrylate, hydrophilic aliphatic dimethacrylate, silanated barium glass filler, silanated aluminum oxide filler, accelerators, dl-camphorquinone, and pigments |
|
| Group 4 (n = 8) | RelyX Unicem 2 Automix | Resin cement: Base paste: methacrylate monomers containing phosphoric acid groups, methacrylate monomers, silanated fillers, initiator components, stabilizers, and rheological additives Catalyst paste: methacrylate monomers, alkaline (basic) fillers, silanated fillers, stabilizers, pigments, and rheological additives |
|
| Group 5 (n = 8) | VITA ADIVA IA-Cem | Ultra-opaque resin cement: mixture of resin based on Bis-GMA, catalyst, stabilizer, and pigments |
|
| Group 6 (control) (n = 8) | Ketac CEM (Aplicap) | Glass ionomer cement: Powder: glass powder (CaAlFsilicate) and pigments Liquid: polycarboxylic acid, tartaric acid, water, and conservation agents |
|
| Group 7 (control) (n = 8) | Hoffmann‘s Phosphate Cement | Zinc phosphate cement: Powder: zinc oxide and magnesium oxide Liquid: ortho-phosphoric acid |
|
| Group (n Samples) | Mean | Standard Deviation | Minimum | Maximum | Shear Bond Strength |
|---|---|---|---|---|---|
| 1 (8) | 550 N | 85 N | 437 N | 661 N | 11 MPa |
| 2 (8) | 762 N | 476 N | 55 N | 1265 N | 15 MPa |
| 3 (8) | 318 N | 345 N | 74 N | 1136 N | 6 MPa |
| 4 (7) a | 508 N | 255 N | 244 N | 956 N | 10 MPa |
| 5 (8) | 126 N | 86 N | 18 N | 277 N | 3 MPa |
| 6 (8) | 55 N | 34 N | 8 N | 108 N | 1 MPa |
| 7 (8) | 214 N | 259 N | 0 N b | 698 N | 4 MPa |
| Category | A | B | C | D | E |
|---|---|---|---|---|---|
| Group 1 | 0 | 5 | 0 | 3 | 0 |
| Group 2 | 1 | 2 | 2 | 3 | 0 |
| Group 3 | 5 | 0 | 0 | 3 | 0 |
| Group 4 | 7 | 0 | 0 | 0 | 0 |
| Group 5 | 8 | 0 | 0 | 0 | 0 |
| Group 6 | 0 | 0 | 0 | 6 | 2 |
| Group 7 | 0 | 2 | 0 | 4 | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bagegni, A.; Borchers, J.; Beisel, S.; Patzelt, S.B.M.; Vach, K.; Kohal, R. Bonding Strength of Various Luting Agents between Zirconium Dioxide Crowns and Titanium Bonding Bases after Long-Term Artificial Chewing. Materials 2023, 16, 7314. https://doi.org/10.3390/ma16237314
Bagegni A, Borchers J, Beisel S, Patzelt SBM, Vach K, Kohal R. Bonding Strength of Various Luting Agents between Zirconium Dioxide Crowns and Titanium Bonding Bases after Long-Term Artificial Chewing. Materials. 2023; 16(23):7314. https://doi.org/10.3390/ma16237314
Chicago/Turabian StyleBagegni, Aimen, Justus Borchers, Samuel Beisel, Sebastian B. M. Patzelt, Kirstin Vach, and Ralf Kohal. 2023. "Bonding Strength of Various Luting Agents between Zirconium Dioxide Crowns and Titanium Bonding Bases after Long-Term Artificial Chewing" Materials 16, no. 23: 7314. https://doi.org/10.3390/ma16237314
APA StyleBagegni, A., Borchers, J., Beisel, S., Patzelt, S. B. M., Vach, K., & Kohal, R. (2023). Bonding Strength of Various Luting Agents between Zirconium Dioxide Crowns and Titanium Bonding Bases after Long-Term Artificial Chewing. Materials, 16(23), 7314. https://doi.org/10.3390/ma16237314









