Influence of the Phase Composition of Titanium Alloys on Cell Adhesion and Surface Colonization
Abstract
1. Introduction
2. Experimental
2.1. Alloys Preparation and Structure Analysis
2.2. Cytotoxicity Studies
2.3. Studies of Cell Adhesion and Colonization of the Surface of Titanium Alloys
3. Results and Discussion
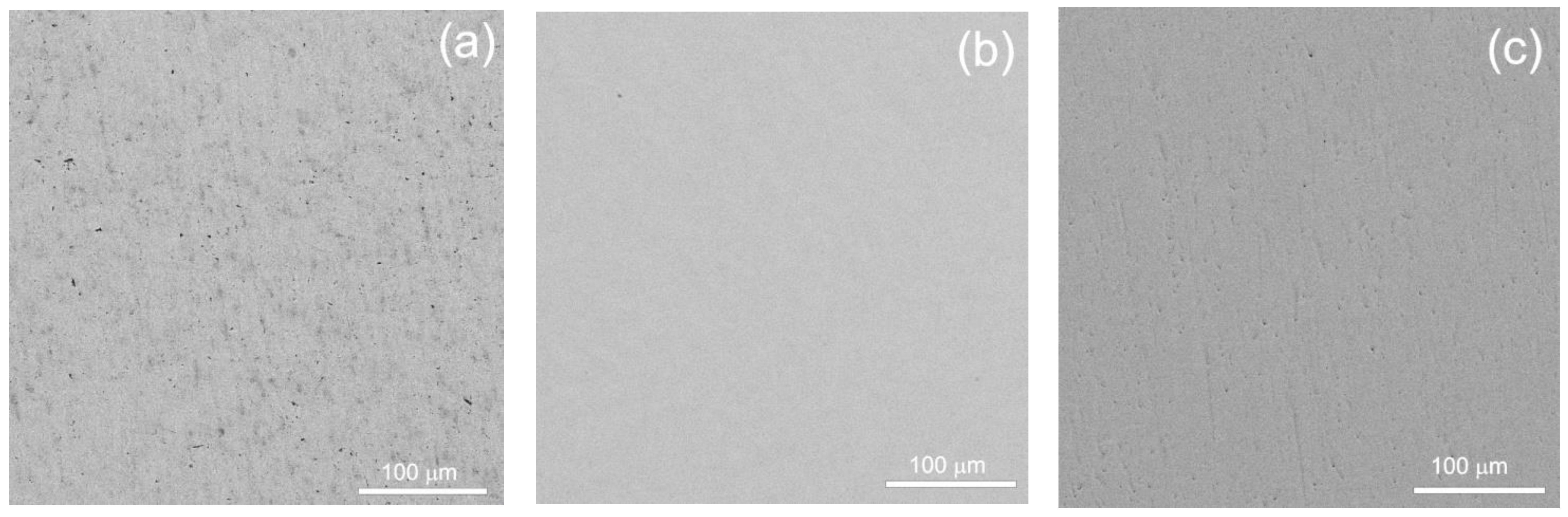
3.1. Studies of Microstructure
3.2. Studies of the Hemolysis Induced by Titanium Alloy Samples in the In Vitro Experiments
3.3. Cytotoxicity Studies
3.4. Study of the Influence of Titanium Alloy Surface Features on Human MHMSCs Colonization
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Geetha, M.; Singh, A.K.; Asokamani, R.; Gogia, A.K. Ti based biomaterials, the ultimate choice for orthopaedic implants—A review. Prog. Mater. Sci. 2009, 54, 397–425. [Google Scholar] [CrossRef]
- Spataru, M.C.; Butnaru, M.; Sandu, A.V.; Vulpe, V.; Vlad, M.D.; Baltatu, M.S.; Geanta, V.; Voiculescu, I.; Vizureanu, P.; Solcan, C. In-depth assessment of new Ti-based biocompatible materials. Mater. Chem. Phys. 2021, 258, 123959. [Google Scholar] [CrossRef]
- Bălţatu, M.S.; Vizureanu, P.; Ţierean, M.H.; Minciună, M.G.; Achiţei, D.C. Ti–Mo alloys used in medical applications. Adv. Mater. Res. 2015, 1128, 105–111. [Google Scholar] [CrossRef]
- Istrate, B.; Mareci, D.; Munteanu, C.; Stanciu, S.; Luca, D.; Crimu, C.I.; Kamel, E. In vitro electrochemical properties of biodegradable ZrO2-CaO coated MgCa alloy using atmospheric plasma spraying. J. Optoel. Adv. Mater. 2015, 17, 1186–1192. [Google Scholar]
- Baltatu, M.S.; Vizureanu, P.; Sandu, A.V.; Munteanu, C.; Istrate, B. Microstructural analysis and tribological behavior of Ti-based alloys with a ceramic layer using the thermal spray method. Coatings 2020, 10, 1216. [Google Scholar] [CrossRef]
- Creteanu, A.; Stefanache, A.; Vieriu, M.; Tantaru, G.; Ochiuz, L. Study on the formulation and pharmacotechnical characterization of hydrophilic matrix tables with amiodarone chlorhydrate. Rev. Chim. 2019, 70, 1–5. [Google Scholar] [CrossRef]
- Kawahara, H. Cytotoxicity of implantable metals and alloys. Bull. Jap. Inst. Met. Mater. 1992, 31, 1033–1039. [Google Scholar] [CrossRef][Green Version]
- Okazaki, Y.; Ito, Y.; Ito, A.; Tateishi, T. Effect of alloying elements on mechanical properties of titanium alloys for medical implants. J. Jap. Inst. Met. Mater. 1993, 57, 332–337. [Google Scholar] [CrossRef]
- Yamamoto, A.; Honma, R.; Sumita, M. Cytotoxicity evaluation of 43 metal salts using murine fibroblasts and osteoblastic cells. J. Biomed. Mater. Res. 1998, 39, 331–340. [Google Scholar] [CrossRef]
- Verestiuc, L.; Spataru, M.C.; Baltatu, M.S.; Butnaru, M.; Solcan, C.; Sandu, A.V.; Voiculescu, I.; Geanta, V.; Vizureanu, P. New Ti–Mo–Si materials for bone prosthesis applications. J. Mech. Behav. Biomed. Mater. 2021, 113, 104198. [Google Scholar] [CrossRef]
- Song, Y.; Xu, D.S.; Yang, R.; Li, D.; Wu, W.T.; Guo, Z.X. Theoretical study of the effects of alloying elements on the strength and modulus of -type bio-titanium alloys. Mater. Sci. Eng. A 1999, 260, 269–274. [Google Scholar] [CrossRef]
- Yamamuro, T. Patterns of osteogenesis in relation to various biomaterials. J. Jpn. Soc. Biomater. 1989, 7, 19–23. [Google Scholar]
- Istrate, B.; Munteanu, C.; Chelariu, R.; Mihai, D.; Cimpoesu, R.; Tudose, F.S.V. Electrochemical evaluation of some Mg-Ca-Mn-Zr biodegradable alloys. Rev. Chim. 2019, 70, 3435–3440. [Google Scholar] [CrossRef]
- Steinemann, S.G. Corrosion of surgical implants—In vivo and in vitro tests. In Evaluation of Biomaterials; Winter, G.D., Leray, J.L., de Groot, K., Eds.; John Wiley and Sons: New York, NY, USA, 1980; pp. 1–34. [Google Scholar]
- Baltatu, M.S.; Vizureanu, P.; Cimpoesu, R.; Abdullah, M.M.A.; Sandu, A.V. The corrosion behavior of TiMoZrTa alloys used for medical applications. Rev. Chim. 2016, 67, 2100–2102. [Google Scholar]
- Niinomi, M. Development of high biocompatible titanium alloys. Func. Mater. 2000, 20, 36–44. [Google Scholar]
- Nawaz, M.H.; Aizaz, A.; Shafique, H.; Ropari, A.Q.; bin Imran, O.; Abbas, M.; Rehman, M.A.U. Rosemary loaded Xanthan coatings on surgical grade stainless steel for potential orthopedic applications. Prog. Org. Coat. 2024, 186, 107987. [Google Scholar] [CrossRef]
- Yoo, S.-Y.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y.; Park, J.-M.; Chung, S.H. Comparison of fit and stability between 3D-printed and milled implant abutments with titanium-6Al-4V and Co-Cr metal alloys. Int. J. Oral Maxillofac. Implant. 2023, 38, 1014–1024. [Google Scholar] [CrossRef]
- Achitei, D.C.; Baltatu, M.S.; Vizureanu, P.; Sandu, A.V.; Benchea, M.; Istrate, B. Ni-Cr alloys assessment for dental implants suitability. Appl. Sci. 2022, 12, 12814. [Google Scholar] [CrossRef]
- Zhang, H.; Saberi, A.; Heydari, Z.; Baltatu, M.S. Bredigite-CNTs Reinforced Mg-Zn bio-composites to enhance the mechanical and biological properties for biomedical applications. Materials 2023, 16, 1681. [Google Scholar] [CrossRef]
- Anisimova, N.; Martynenko, N.; Novruzov, K.; Rybalchenko, O.; Kiselevskiy, M.; Rybalchenko, G.; Straumal, B.; Salishchev, G.; Mansharipova, A.; Kabiyeva, A.; et al. Modification of biocorrosion and cellular response of magnesium alloy WE43 by multiaxial deformation. Metals 2022, 12, 105. [Google Scholar] [CrossRef]
- Kong, L.; Heydari, Z.; Lami, G.H.; Saberi, A.; Baltatu, M.S.; Vizureanu, P. A Comprehensive review of the current research status of biodegradable zinc alloys and composites for biomedical applications. Materials 2023, 16, 4797. [Google Scholar] [CrossRef] [PubMed]
- Il’in, A.A.; Kolachev, B.A.; Pol’kin, I.S. Titanium alloys. In Composition, Structure, Properties; VILS-MATIL: Moscow, Russia, 2009. (In Russian) [Google Scholar]
- Kolachev, B.A. Physical Metallurgy of Titanium; Metallurgiya: Moscow, Russia, 1976. (In Russian) [Google Scholar]
- Kolachev, B.A.; Eliseev, Y.S.; Bratukhin, A.G.; Talalaev, V.D. Titanium Alloys in the Design and Manufacture of Aircraft Engines and Aerospace Technology; MAI: Moscow, Russia, 2001. (In Russian) [Google Scholar]
- Kolachev, B.A.; Betsofen, S.Y.; Bunin, L.A.; Volodin, V.A. Physico-Mechanical Properties of Light Structural Alloys; Metallurgia Publishing House: Moscow, Russia, 1995. (In Russian) [Google Scholar]
- Kolachev, B.A.; Lyasotskaya, V.S. Correlation between diagrams of isothermal and anisothermal transformations and phase composition diagram of hardened titanium alloys. Met. Sci. Heat Treat. 2003, 45, 119–126. [Google Scholar] [CrossRef]
- Egorova, Y.B.; Il’in, A.A.; Kolachev, B.A.; Nosov, V.K.; Mamonov, A.M. Effect of the structure on the cutability of titanium alloys. Met. Sci. Heat Treat. 2003, 45, 134–139. [Google Scholar] [CrossRef]
- Kolachev, B.A.; Veitsman, M.G.; Gus’kova, L.N. Structure and mechanical properties of annealed α+β titanium alloys. Met. Sci. Heat Treat. 1983, 25, 626–631. [Google Scholar] [CrossRef]
- Fishgoit, A.V.; Maistrov, V.M.; Rozanov, M.A. Interaction of short cracks with the structure of metals. Sov. Mater. Sci. 1988, 24, 247–251. [Google Scholar] [CrossRef]
- Bălțatu, M.S.; Vizureanu, P.; Bălan, T.; Lohan, M.; Țugui, C.A. Preliminary tests for Ti-Mo-Zr-Ta alloys as potential biomaterials. IOP Conf. Ser. Mater. Sci. Eng. 2018, 374, 012023. [Google Scholar] [CrossRef]
- Spataru, M.-C.; Cojocaru, F.D.; Sandu, A.V.; Solcan, C.; Duceac, I.A.; Baltatu, M.S.; Voiculescu, I.; Geanta, V.; Vizureanu, P. Assessment of the effects of Si addition to a new TiMoZrTa system. Materials 2021, 14, 7610. [Google Scholar] [CrossRef]
- Gornakova, A.; Straumal, B.; Kuzmin, A.; Tyurin, A.; Chernyaeva, E.; Druzhinin, A.; Afonikova, N.; Davdian, G. Influence of heat treatment and high-pressure torsion on phase transformations in TiZrHfMoCr high-entropy alloy. Metals 2023, 13, 1030. [Google Scholar] [CrossRef]
- Ishimoto, T.; Ozasa, R.; Nakano, K.; Weinmann, M.; Schnitter, C.; Stenzel, M.; Matsugaki, A.; Nagase, T.; Matsuzaka, T.; Todai, M.; et al. Development of TiNbTaZrMo bio-high entropy alloy (BioHEA) super-solid solution by selective laser melting, and its improved mechanical property and biocompatibility. Scr. Mater. 2021, 194, 113658. [Google Scholar] [CrossRef]
- Okazaki, Y.; Gotoh, E. Comparison of metal release from various metallic biomaterials in vitro. Biomaterials 2005, 26, 11–21. [Google Scholar] [CrossRef]
- Teoh, S.H. Fatigue of biomaterials: A review. Int. J. Fatigue 2000, 22, 825–837. [Google Scholar] [CrossRef]
- Niinomi, M. Deformation of NiTiCu shape memory single crystals in compression. Met. Mater. Trans. A 2001, 32, 477–486. [Google Scholar] [CrossRef]
- Niinomi, M. Mechanical properties of biomedical titanium alloys. Mater. Sci. Eng. A 1998, 243, 231–236. [Google Scholar] [CrossRef]
- Machara, K.; Doi, K.; Matsushita, T.; Susaki, Y. Application of vanadium-free titanium alloys to artificial hip joints. Mater. Trans. 2002, 43, 2936–2942. [Google Scholar] [CrossRef][Green Version]
- Akahori, T.; Niinomi, M.; Fukui, H.; Ogawa, M.; Toda, H. Improvement in fatigue characteristics of newly developed beta type titanium alloy for biomedical applications by thermo-mechanical treatments. Mater. Sci. Eng. C 2005, 25, 247–252. [Google Scholar] [CrossRef]
- Kirby, R.S.; Heard, S.R.; Miller, P.; Eardley, I.; Holmes, S.; Vale, J.; Bryan, J.; Liu, B.S. Use of the ASI titanium stent in the management of bladder outflow obstruction due to benign prostatic hyperplasia. J. Urol. 1992, 148, 1195–1197. [Google Scholar] [CrossRef]
- Nag, S.; Banerjee, R.; Fraser, H.L. Microstructural evolution and strengthening mechanisms in Ti–Nb–Zr–Ta, Ti–Mo–Zr–Fe and Ti–15Mo biocompatible alloys. Mater. Sci. Eng. C 2005, 25, 357–362. [Google Scholar] [CrossRef]
- Wapner, K.L. Implications of metallic corrosion in total knee arthroplasty. Clin. Orthop. Relat. Res. 1991, 271, 12–20. [Google Scholar] [CrossRef]
- Eisenbarth, E.; Velten, D.; Müller, M.; Thull, R.; Breme, J. Biocompatibility of beta-stabilizing elements of titanium alloys. Biomaterials 2004, 25, 5705–5713. [Google Scholar] [CrossRef] [PubMed]
- Miller, P.D.; Holladay, J.W. Friction and wear properties of titanium. Wear 1958, 2, 133–140. [Google Scholar] [CrossRef]
- Liang, G., Jr.; Ferguson, E.S., Jr.; Hodge, E.S. Tissue reaction in rabbit muscle exposed to metallic implants. J. Biomed. Mater. Res. 1967, 1, 135–149. [Google Scholar] [CrossRef] [PubMed]
- Kuan, T.S.; Ahrens, R.R.; Sass, S.L. The stress-induced omega phase transformation in Ti–V alloys. Met. Trans. A 1975, 6, 1767–1774. [Google Scholar] [CrossRef]
- Zhao, X.F.; Niinomi, M.; Nakai, M.; Hieda, J.; Ishimoto, T.; Nakano, T. Optimization of Cr content of metastable β-type Ti–Cr alloys with changeable Young’s modulus for spinal fixation applications. Acta Biomater. 2012, 8, 2392–2400. [Google Scholar] [CrossRef]
- Gornakova, A.S.; Korneva, A.; Tyurin, A.I.; Afonikova, N.S.; Kilmametov, A.R.; Straumal, B.B. Omega phase formation and mechanical properties of Ti-1.5 wt.% Mo and Ti-15 wt.% Mo alloys after high pressure torsion. Processes 2023, 11, 221. [Google Scholar] [CrossRef]
- Kilmametov, A.; Ivanisenko, Y.; Mazilkin, A.A.; Straumal, B.B.; Gornakova, A.S.; Fabrichnaya, O.B.; Kriegel, M.J.; Rafaja, D.; Hahn, H. The α→ω and β→ω phase transformations in Ti–Fe alloys under high-pressure torsion. Acta Mater. 2018, 144, 337–351. [Google Scholar] [CrossRef]
- Straumal, B.B.; Kilmametov, A.R.; Ivanisenko, Y.; Gornakova, A.S.; Mazilkin, A.A.; Kriegel, M.J.; Fabrichnaya, O.B.; Baretzky, B.; Hahn, H. Phase transformations in Ti-Fe alloys induced by high pressure torsion. Adv. Eng. Mater. 2015, 17, 1835–1841. [Google Scholar] [CrossRef]
- Kriegel, M.J.; Kilmametov, A.; Klemm, V.; Schimpf, C.; Straumal, B.B.; Gornakova, A.S.; Ivanisenko, Y.; Fabrichnaya, O.; Hahn, H.; Rafaja, D. Thermal stability of athermal ω-Ti(Fe) produced upon quenching of β-Ti(Fe). Adv. Eng. Mater. 2019, 21, 1800158. [Google Scholar] [CrossRef]
- Kilmametov, A.R.; Ivanisenko, Y.; Straumal, B.B.; Gornakova, A.S.; Mazilkin, A.A.; Hahn, H. The α → ω transformation in titanium-cobalt alloys under high-pressure torsion. Metals 2018, 8, 1. [Google Scholar] [CrossRef]
- Niinomi, M.; Nakai, M.; Hieda, J. Development of new metallic alloys for biomedical applications. Acta Biomater. 2012, 8, 3888–3903. [Google Scholar] [CrossRef]
- Sakaguchi, N.; Niinomi, M.; Akahori, T.; Takeda, J.; Toda, H. Relationships between tensile deformation behaviour and microstructure in Ti–Nb–Ta–Zr system alloys. Mater. Sci. Eng. C 2005, 25, 363–369. [Google Scholar] [CrossRef]
- Hanada, S.; Ozaki, T.; Takahashi, E.; Watanabe, T.S.; Yoshimi, K.; Abumiya, T. Composition dependence of Young’s modulus in beta titanium binary alloys. Mater. Sci. Forum 2003, 426–432, 3103–3108. [Google Scholar] [CrossRef]
- Li, S.J.; Yang, R.; Li, S.; Hao, Y.L.; Cui, Y.Y.; Niinomi, M.; Guo, Z.X. Wear characteristics of Ti–Nb–Ta–Zr and Ti–6Al–4V alloys for biomedical applications. Wear 2004, 257, 869–876. [Google Scholar] [CrossRef]
- Long, M.; Rack, H.J. Titanium alloys in total joint replacement—A materials science perspective. Biomaterials 1998, 19, 1621–1639. [Google Scholar] [CrossRef]
- Tang, X.; Ahmed, T.; Rack, H.J. Phase transformations in Ti–Nb–Ta and Ti–Nb–Ta–Zr alloys. J. Mater. Sci. 2000, 35, 1805–1811. [Google Scholar] [CrossRef]
- Lábár, J.L. Electron diffraction based analysis of phase fractions and texture in nanocrystalline thin films, Part I: Principles. Microsc. Microanal. 2008, 14, 287–295. [Google Scholar] [CrossRef]
- Martynenko, N.S.; Anisimova, N.Y.; Rybalchenko, O.V.; Kiselevskiy, M.V.; Rybalchenko, G.; Straumal, B.; Temralieva, D.; Mansharipova, A.T.; Kabiyeva, A.O.; Gabdullin, M.T.; et al. Rationale for processing of a Mg-Zn-Ca alloy by equal-channel angular pressing for use in biodegradable implants for osteoreconstruction. Crystals 2021, 11, 1381. [Google Scholar] [CrossRef]
- Kriegel, M.J.; Kilmametov, A.; Rudolph, M.; Straumal, B.B.; Gornakova, A.S.; Stöcker, H.; Ivanisenko, Y.; Fabrichnaya, O.; Hahn, H.; Rafaja, D. Transformation pathway upon heating of Ti–Fe alloys deformed by high-pressure torsion. Adv. Eng. Mater. 2018, 20, 1700933. [Google Scholar] [CrossRef]

















| Sample Denomination | Composition, wt.% | Conditions of Annealing and Postprocessing |
|---|---|---|
| 1a | Ti-4% Fe | 950 °C, 124 h |
| 2a | Ti-4% Fe | 950 °C, 152 h |
| 3a | Ti-4% Fe | 900 °C, 40 h |
| 4b | Ti-4% Fe | 800 °C, 100 h + HPT |
| 41a | Ti-0.5% Fe | 570 °C, 1300 h |
| 41b | Ti-1% Fe | 470 °C, 673 h + HPT |
| 63a | Ti-5% Nb | 800 °C, 91 h |
| 64a | Ti-10% Nb | 800 °C, 91 h |
| 65a | Ti-20% Nb | 800 °C, 91 h |
| 63b | Ti-5% Nb | 800 °C, 91 h + HPT |
| 61b | Ti-6% Nb | 1000 °C, 24 h + HPT |
| 62b | Ti-10% Nb | 1000 °C, 24 h + HPT |
| 66b | Ti-30% Nb | 600 °C, 768 h + HPT |
| Sample Denomination | Composition, wt.% | Conditions of Annealing and Postprocessing | Phases in the Sample |
|---|---|---|---|
| 1a | Ti-4% Fe | 950 °C, 124 h | α + β, 80% β, 20% α |
| 2a | Ti-4% Fe | 950 °C, 152 h | α + β, 50% β, 50% α |
| 3a | Ti-4% Fe | 900 °C, 40 h | α + β, 20% β, 80% α |
| 4b | Ti-4% Fe | 800 °C, 100 h + HPT | 100% ω phase |
| 41a | Ti-0.5% Fe | 570 °C, 1300 h | α phase v + TiFe, large grains |
| 41b | Ti-1% Fe | 470 °C, 673 h + HPT | α phase + TiFe, fine grains |
| 63a | Ti-5% Nb | 800 °C, 91 h | α + β, 20% β, 80% α |
| 64a | Ti-10% Nb | 800 °C, 91 h | α + β, 50% β, 50% α |
| 65a | Ti-20% Nb | 800 °C, 91 h | α + β, 80% β, 20% α |
| 63b | Ti-5% Nb | 800 °C, 91 h + HPT | 50% α + 50% ω |
| 61b | Ti-6% Nb | 1000 °C, 24 h + HPT | α + α’, no ω |
| 62b | Ti-10% Nb | 1000 °C, 24 h + HPT | 10% α + 90% ω |
| 66b | Ti-30% Nb | 600 °C, 768 h + HPT | 100% ω |
| Sample | Optical Density | p | ||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | M | SD | ||
| 1a | 0.093 | 0.126 | 0.12 | 0.113 | 0.017578 | 0.896 |
| 2a | 0.12 | 0.261 | 0.132 | 0.171 | 0.078173 | 0.941 |
| 3a | 0.13 | 0.138 | 0.118 | 0.128667 | 0.010066 | 0.918 |
| 4a | 0.168 | 0.135 | 0.118 | 0.140333 | 0.025423 | 0.931 |
| 4b | 0.128 | 0.124 | 0.13 | 0.127333 | 0.003055 | 0.917 |
| 41a | 0.131 | 0.119 | 0.122 | 0.124 | 0.006245 | 0.912 |
| 41 b | 0.131 | 0.132 | 0.128 | 0.130333 | 0.002082 | 0.921 |
| 63a | 0.119 | 0.128 | 0.141 | 0.129333 | 0.01106 | 0.919 |
| 64a | 0.129 | 0.114 | 0.116 | 0.119667 | 0.008145 | 0.906 |
| 65a | 0.156 | 0.115 | 0.125 | 0.132 | 0.021378 | 0.921 |
| 63b | 0.11 | 0.142 | 0.128 | 0.126667 | 0.016042 | 0.915 |
| 61b | 0.159 | 0.109 | 0.106 | 0.124667 | 0.029771 | 0.910 |
| 62b | 0.128 | 0.145 | 0.159 | 0.144 | 0.015524 | 0.937 |
| 66b | 0.115 | 0.114 | 0.142 | 0.123667 | 0.015885 | 0.911 |
| Spontaneous control | 0.127 | 0.126 | 0.131 | 0.128 | 0.002646 | - |
| Intact control (0% hemolysis) | 0.092 | 0.097 | 0.091 | 0.093333 | 0.003215 | - |
| Control with Triton-X (100% hemolysis) | 2.145 | 2.221 | 2.174 | 2.18 | 0.038354 | - |
| Sample | M | SD | p vs. Control |
|---|---|---|---|
| 1a | 1.9 | 0.9 | 0.110 |
| 2a | 0.8 | 0.7 | 0.380 |
| 3a | 1.5 | 1.4 | 0.070 |
| 4a | 0.7 | 1.1 | 0.384 |
| 4b | 0.5 | 0.8 | 0.363 |
| 41a | 0.0 | 0.0 | 0.156 |
| 41 b | 0.6 | 1.0 | 0.185 |
| 63a | 0.6 | 1.0 | 0.185 |
| 64a | 0.0 | 0.0 | 0.155 |
| 65a | 0.5 | 0.9 | 0.211 |
| 63b | 0.7 | 1.2 | 0.370 |
| 61b | 0.8 | 0.7 | 0.529 |
| 62b | 1.2 | 1.0 | 0.486 |
| 66b | 1.4 | 1.3 | 0.432 |
| Control | 1.3 | 0.5 | - |
| Sample | M | SD | p vs. Control |
|---|---|---|---|
| 1a | 0.232 | 0.018 | 0.997 |
| 2a | 0.290 | 0.078 | 0.963 |
| 3a | 0.248 | 0.010 | 0.999 |
| 4a | 0.259 | 0.025 | 0.996 |
| 4b | 0.246 | 0.003 | 1.000 |
| 41a | 0.243 | 0.006 | 1.000 |
| 41b | 0.249 | 0.002 | 1.000 |
| 63a | 0.248 | 0.011 | 1.000 |
| 64a | 0.239 | 0.008 | 0.999 |
| 65a | 0.251 | 0.021 | 0.998 |
| 63b | 0.246 | 0.016 | 0.999 |
| 61b | 0.244 | 0.030 | 0.996 |
| 62b | 0.263 | 0.016 | 0.998 |
| 66b | 0.243 | 0.016 | 0.999 |
| Control | 0.247 | 0.003 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Straumal, B.B.; Anisimova, N.Y.; Kiselevskiy, M.V.; Novruzov, K.M.; Korneva, A.; Gornakova, A.S.; Kilmametov, A.R.; Sommadossi, S.; Davdian, G. Influence of the Phase Composition of Titanium Alloys on Cell Adhesion and Surface Colonization. Materials 2023, 16, 7130. https://doi.org/10.3390/ma16227130
Straumal BB, Anisimova NY, Kiselevskiy MV, Novruzov KM, Korneva A, Gornakova AS, Kilmametov AR, Sommadossi S, Davdian G. Influence of the Phase Composition of Titanium Alloys on Cell Adhesion and Surface Colonization. Materials. 2023; 16(22):7130. https://doi.org/10.3390/ma16227130
Chicago/Turabian StyleStraumal, Boris B., Natalia Yu. Anisimova, Mikhail V. Kiselevskiy, Keryam M. Novruzov, Anna Korneva, Alena S. Gornakova, Askar R. Kilmametov, Silvana Sommadossi, and Gregory Davdian. 2023. "Influence of the Phase Composition of Titanium Alloys on Cell Adhesion and Surface Colonization" Materials 16, no. 22: 7130. https://doi.org/10.3390/ma16227130
APA StyleStraumal, B. B., Anisimova, N. Y., Kiselevskiy, M. V., Novruzov, K. M., Korneva, A., Gornakova, A. S., Kilmametov, A. R., Sommadossi, S., & Davdian, G. (2023). Influence of the Phase Composition of Titanium Alloys on Cell Adhesion and Surface Colonization. Materials, 16(22), 7130. https://doi.org/10.3390/ma16227130










