Abstract
The aging population in developed countries has increased the number of edentulous patients and, therefore, the need for prosthetic rehabilitation to improve their quality of life. Complete dentures are the main treatment option in these cases. The use of CAD/CAM (Computer Aided Design/Computer Aided Manufacturing) in dentistry has improved clinical protocols and outcomes, achieving a reduction in work time and economic costs for the patients. The main objective of this review was to compare the characteristics of conventional and digital dentures, attempting to determine whether the use of new technologies represents an improvement in the properties of removable complete dentures. A bibliographic review was carried out in the PubMed/MEDLINE, Cochrane Library, Scielo, and Embase databases. With the initial search, 157 articles were obtained. After applying the inclusion and exclusion criteria, 64 publications were selected for this bibliographic review. The different conclusions of the studies consulted were compared regarding fit and retention, fracture resistance, surface roughness, biocompatibility, and aesthetics, taking into account the different methods of prostheses fabrication. In general, digital prostheses have shown better mechanical properties and, consequently, better biocompatibility and aesthetics than conventional prostheses. However, the obtained results were very heterogeneous, preventing a supported conclusion.
1. Introduction
Currently, developed countries are facing significant population aging, leading to an increase in the prevalence of partially or completely edentulous patients, resulting in the need for prosthetic treatments [1,2,3]. The conventional complete denture is considered the primary treatment option for these patients. Implant-supported or implant-retained prostheses are good alternatives, but they might be contraindicated or inaccessible for some patients, due to economic reasons, systemic conditions that contraindicate surgery, a complete lack of oral hygiene by the patient, anatomical constraints such as insufficient bone quantity or quality, or head and neck radiation therapy or chemotherapy, among others [4,5]. These situations make conventional complete dentures a valid option for most edentulous patients [2,3]. Over the past decades, with the rapid advancement of science and new technologies, the use of digital methods in dentistry, including the field of complete dentures, has significantly increased [6].
The conventional protocol for fabricating a mucosa-supported prosthesis involves a lengthy sequence of clinical and laboratory steps, which can result in a relatively long time period for completion. The polymerization shrinkage of polymethyl methacrylate (PMMA) and the difficulty in duplicating the prosthesis in case of a need to revert to earlier manufacturing stages can be considered the main drawbacks of the technique [7,8,9,10,11].
The use of CAD/CAM (computer-aided design/computer-aided manufacturing) in dentistry began in the early 1980s [3]. Currently, CAD/CAM is more advanced compared to conventional techniques [12]. The implementation of CAD/CAM in dental prosthesis has resulted in easier clinical protocols, the use of material with better properties, improved fit and retention of prostheses, a reduction in chairside and laboratory working time, and overall cost reduction. However, adopting this technology requires a learning curve and the digitalization of clinical procedures. The combined use of optical scanner and conventional techniques has shown success, while fully digital workflows still require further studies [13,14,15,16,17]. Within digital fabrication of complete prostheses and other elements, two techniques can be distinguished [3,7,18]:
- Subtractive or milling technique. It utilizes pre-polymerized PMMA discs that are milled under high pressure and controlled conditions. Recent research has shown that milled resins have better mechanical and surface properties (greater color stability, reduced bacterial colonization, and lower monomer release) than thermopolymerizable resins [19]. It is commonly used for fabricating fixed dental prostheses, inlays, onlays, veneers, or crowns [20,21,22].
- Additive or 3D printing technique. The additive manufacturing involves layer-by-layer deposition of liquid resins on a support structure, followed by curing with visible light, ultraviolet light, heat, or laser. This process is repeated until the complete prosthesis takes the shape specified in the digital design software. The use of this technique is increasing in dentistry as it allows fabrication not only of complete dentures but also fixed prostheses, surgical guides, occlusal splints, and more [20].
Initially, most manufacturers use milling for producing complete dentures, while the additive manufacturing is mainly used for fabricating provisional prostheses, but this has been changing as the materials used in 3D printing have evolved [23,24].
Some advantages of CAD/CAM include the possibility to store patient anatomical data and prosthesis design, making it feasible to reproduce the prosthesis in case of loss or damage without repeating patient records. Additionally, CAD/CAM eliminates the polymerization shrinkage of the prosthetic base, reduces the clinician’s workload, and results in a higher strength and density of the material used [25,26,27]. The digital fabrication technique of complete dentures differs from the conventional technique, mainly in the need for impressions that capture both the internal and external surface of the prosthesis, as well as functional impressions [12]. Currently, using an intraoral scanner on completely edentulous arches does not achieve the same precision as conventional impressions, as scanning accuracy decreases with an increasing number of missing teeth. Several factors, such as the characteristics of the scanned surface, oral cavity conditions, or patient movements, can negatively impact the quality of the impression. Anatomical deviations such a high-arched palate, wide edentulous gaps, or the patient´s inability to open their mouth can also become limitations of the intraoral scanner [28,29]. Digital complete dentures can be manufactured from scratch or copying a previous denture. If the patient does not have existing dentures, irreversible hydrocolloid impressions will be taken to obtain plaster models, on which thermopolymerizable trays will be adapted. The vertical dimension (VD) will be obtained with phonetic registrations, mainly using bilabial sounds, and the occlusal vertical dimension (OVD) will be calculated from it [3,30]. The digital fabrication technique depends on the system being used.
In milling manufacturing, the prostheses are manufactured from a cylinder of acrylic resin produced under high pressure and temperature, preventing the shrinkage of the final milled prosthesis. As a result of compressing this resin, there is a decrease in monomer release, reduced porosity compared to conventional prostheses, and a reduction in Candida albicans adhesion to the prosthetic base. The teeth used in milled prostheses are not milled; instead, they are the same as those used in conventional prostheses [12,14,31]. The design software positions the teeth according to the desired occlusion, using a transparent guide to place the maxillary anterior teeth. At this point, the preliminary prosthesis design in sent to the dentist, who can modify it if necessary. Some design software, like the 3Shape Dental System 2013, can simulate mandibular movements (laterotrusions, protrusions, and retrusions), allowing the occlusion to be adjusted based on the registered mandibular movements. However, this step should not replace the final occlusion adjustment once the prostheses are placed in the patient´s mouth [3]. Once the teeth design is approved by the dentist, the prosthesis base and tooth sockets (simulating alveoli) are milled. Finally, the artificial teeth are chemically bonded to the base using a bonding technique that involves heat and pressure. In the conventional method, the bonding between teeth and denture base occurs during the polymerization process, while in digital prostheses, the bonding takes place after the polymerization of the base. The release of the monomer that occurs during polymerization reduces the bonding capacity of the resin. This requires the use of techniques that modify the surfaces, primarily airborne-particle abrasion or sandblasting, to strengthen the chemical bond formed through the use of appropriate adhesives [32,33,34].
To assess the quality of a removable prosthesis, studies rely on the following criteria: aesthetics (lip support and smile line), retention, stability, support, and balanced occlusion. However, patient satisfaction with the prosthesis is also crucial and remains essential in evaluating its quality [1,25].
In milled prostheses, a decrease in stability-related problems has been observed because the prosthesis is milled from a pre-polymerized acrylic resin disc [14,35]. This improvement results not only in enhanced stability but also in better retention, leading to reduced trauma and a decreased need for adjustments after insertion [14,35]. In conventional techniques, the deformation of the thermopolymerizable resin can decrease the degree of adaptation of the prosthetic base, which can be compensated by sealing the posterior part of the palate [30]. Complete dentures made from materials with low surface hardness can suffer damage from aggressive brushing, leading to plaque retention and discoloration, thereby reducing the prosthesis´ lifespan [30,36]. Surface roughness is one of the most critical factors influencing bacterial colonization of material, as well as color stability. In CAD/CAM-fabricated dentures, the bases are milled from resin discs subjected to high pressure during polymerization. This milling process produces smoother surfaces, resulting in reduced microbial adhesion compared to conventional fabrication methods [18,30]. Biocompatibility is one of the most crucial qualities to consider when selecting a material. Oral mucosa in contact with a foreign material may experience adverse reactions such as pain, hypersensitivity reactions or a burning sensation in the mouth. Therefore, assessing the material´s biocompatibility before initiating treatment is essential to ensure patient satisfaction [18]. Regarding aesthetics, dentists prefer the aesthetics of conventional dentures [35]. The aesthetics of CAD/CAM-fabricated dentures remains a limitation. Additionally, one of the advantages of conventional dentures is the prosthetist´s ability to work collaboratively with the dentist and patient, considering their preferences in the fabrication process [30].
This literature review was conducted to compare the properties of conventional and digital prostheses, aiming to determine whether the new manufacturing techniques using advances technologies result in improvements nor only in terms of cost-effectiveness and time saving but also in treatment quality and patient satisfaction. The review focused on digitally manufactured prosthetics produced mainly through milling, primarily due to a larger amount of available research in the literature. So, the results, despite including both manufacturing techniques, are primarily applicable to the subtractive technique. The specific objectives proposed were as follows:
- A comparison of the properties of the final prosthesis, as well as the advantages and disadvantages between both conventional and CAD/CAM methods of fabricating complete mucosa-supported dentures.
- A comparison of the fit, retention, fracture resistance, surface roughness, biocompatibility, and aesthetics of the base in conventional dentures and CAD/CAM-fabricated dentures.
The null hypothesis is that digital dentures show better results in all the investigated variables.
2. Materials and Methods
A search was conducted for articles related to the fabrication of both conventional and digital complete mucosa-supported dental prostheses and their mechanical and aesthetic properties. The databases used were PubMed/MEDLINE, Cochrane Library, Scielo and Embase, with the keywords digital, removable complete dental prostheses, CAD/CAM, and complete denture. Additionally, the Boolean operator OR was used in the search equation [(Removable complete dental prostheses) OR (digital)]. The inclusion and exclusion criteria used were as follows (Table 1):

Table 1.
Inclusion and exclusion criteria.
3. Results
In the following flowchart (Figure 1), the conducted search and its outcomes are depicted:
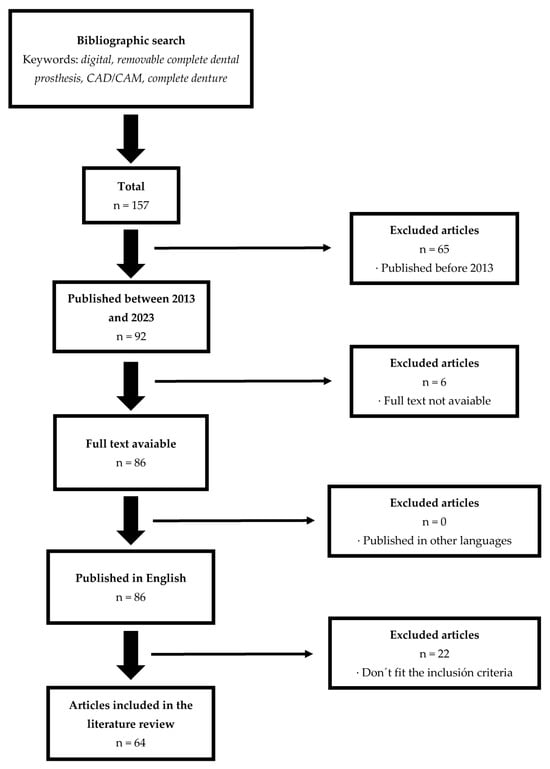
Figure 1.
Flowchart of the search performed.
A total of 40 articles were analyzed in the conducted review. All articles were published after 2017, and they were all clinical trials (in vitro or in vivo). Among these, nine publications focused on analyzing base fit, four discussed retention, and two addressed dimensional stability. Regarding material properties, six articles discussed flexural strength, three covered material hardness, three discussed the modulus of elasticity, and seven articles examined material roughness and porosity. Finally, six publications discussed material biocompatibility, and four of them explored topics related to aesthetics and color stability. Among the analyzed articles, 40 of them discussed milled prosthetics, and 10 discussed printed prosthetics (comparing them with prosthetics manufactured using conventional methods) (Figure 2).
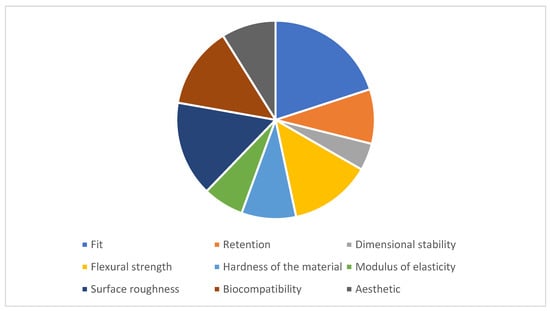
Figure 2.
Analyzed variables.
4. Discussion
In most cases, patients prefer digital complete dentures over the conventional dentures they had previously. One of the main factors influencing this preference is the reduced treatment time, which decreases from five appointments to two appointments [20,37]. However, according to Ohara et al. [11], patient satisfaction with conventional dentures is significantly higher than with digital dentures, and within the digital dentures category, patients prefer milled dentures over those manufactures using 3D printing technology. This is partly because printed dentures require a minimum thickness of 2.5 mm to ensure base strength, while milled and conventional dentures only require a thickness of 1.4 mm, resulting in greater comfort for patients during speech. Additionally, the teeth used in milled and conventional dentures are made of a harder resin compared to the resin used in 3D printers, resulting in fewer color changes, better resemblance to natural teeth, and easier maintenance. However, teeth used in conventional dentures still exhibit better color stability than milled dentures. Another advantage of conventional dentures is the ease of placing teeth in different axes, especially in the anterior region. In milled dentures, as the teeth are milled from a single piece, it is more challenging to change the angulation of each tooth individually. Patients also prefer conventional dentures due to their better stability, which can be attributed to the peripheral seal of the denture and stable occlusal contacts, which are not as effective in digital dentures [11].
Some researchers attribute patient dissatisfaction to psychological factors and even differences in perspective between the clinician and the patient. In cases where a patient has complex oral characteristics, the professional may assess a prosthesis as adequate, which under normal circumstances may not meet the patient´s expectations. Consequently, the patient may end up with an unsatisfactory prosthesis. Alfadda S. [1], after studying all the aforementioned variables, concludes that the lack of stability and retention in mandibular dentures has the most significant impact on the acceptance of complete dentures. Several studies have shown that the lack of stability in the lower denture leads to difficulties in chewing and an increase in the mobility of the upper denture [1].
Numerous studies (Table 2) have demonstrated better retention in digital dentures compared to conventional dentures, which exhibit less dimensional stability mainly due to the absence of polymerization shrinkage in the denture base [25,30,35,38,39,40,41].

Table 2.
Analysis of prosthetic fit and retention.
The shrinkage of PMMA can cause volumetric distortion in the denture base, which has traditionally been counteracted by hydrating the denture with water. The expansion resulting from this hydration offsets the polymerization shrinkage, depending on the amount of free monomer. In the study by AlHelal et al. [25], both conventional and digital dentures were fabricated, and both were immediately immersed in water after their fabrication. The results showed a significant increase in retention in the digital dentures compared to the conventional ones. Thus, hydration may not be sufficient to compensate for the polymerization shrinkage that occurs in conventional dentures. This difference between the two groups could be explained by the higher density of the milled denture bases, resulting in greater dimensional stability and reducing the influence of hydration on retention [25]. However, in the research by Srinivasan et al. [44], which compared the fit of dentures fabricated using two conventional techniques (flasking and injection molding of resin) and milling, all three techniques demonstrated clinically acceptable fit with no significant differences prior to hydration. After hydration with artificial saliva, the dentures fabricated using flasking improved their fit significantly, contrary to the findings of the study by AlHelal et al. [25,44].
It is believed that 3D printing resins, which are applied in liquid from to the model, may lead to a better fit, but currently, there is not enough evidence to support this. However, the need to polymerize these resins after their conformation can be a disadvantage in terms of fit, due to the polymerization shrinkage these resins undergo, leading to detachment of the palate. This compromises the suction effect of the denture. This phenomenon also occurs in conventional complete dentures made of thermopolymerizable resin and can be compensated for by creating a post-dam in the denture or hydrating the denture base with water; the resulting expansion due to hydration can counteract the deformation produced via polymerization, depending on the amount of free monomer [18,25]. In milled dentures, on the other hand, polymerization takes place before the denture is formed. However, more research is needed to determine if, in this case, a post-dam would also be necessary to achieve this suction effect [18]. The additive manufacturing uses resins that, once processed, require a final photopolymerization. Until this photopolymerization is performed, the resins may undergo polymerization shrinkage and compromise their mechanical properties. Additionally, the removal of the denture from the 3D printer occurs before the final polymerization, which can result in denture deformation. Invariably, an unpolymerized resin layer, the inhibited layer, remains in the finished denture, which must be removed with an appropriate solvent. Although all these situations may result in less fit and dimensional stability of the printed dentures compared to the milled ones, the additive manufacturing has many advantages such as precision, less material waste, and more economical machinery. Today, 3D printers are cheaper and easier to transport than milling machines, making them more accessible for private clinics and dental laboratories, eliminating the time and costs of shipping [18,47]. However, some authors such as Lee et al. [46] or Hwang et al. [43] obtained results in their studies showing that printed dentures had better fit than milled dentures and conventional dentures [42,43].
Faty et al. [7] concluded that PMMA pre-polymerized denture bases showed better adaptation to the supporting tissues tan those made of conventionally polymerized PMMA, similar to the findings of Goodacre et al. [26] and Hsu et al. [48], who determined that digital dentures exhibit superior adaptation compared to dentures fabricated via any conventional method [7,26,48]. This is attributed to the reduced occurrence of dimensional changes during polymerization in the case of digital dentures. Additionally, pre-polymerized PMMA provides better retention due to its lower polymerization shrinkage. However, a disadvantage could be its higher cost and increased material waste. Faty et al. [7] also found significant differences in the retention of the three types of dentures analyzed: conventional, milled, and printed dentures. Furthermore, they demonstrated that milled dentures had higher retention than conventional dentures [7].
The fit of the denture base to the supporting tissues is essential for proper retention, stability, and support of complete dentures. Minimal distortion during the denture fabrication process is crucial to achieve a correct adaptation to the mucosa. The degree of distortion depends on both the thickness and material used, as well as the fabrication technique. In the milling of denture bases, dimensional deformation due to polymerization is avoided, and a smoother surface, meaning lower surface roughness, is achieved. In the study by Faty et al. [7], milled dentures showed better fit, greater adaptation, fewer dimensional changes, and higher precision during the fabrication process. In the case of conventional dentures, the complexity of the procedure, the required time, and the deformation due to PMMA polymerization may reduce the degree of adaptation of the denture base [6,7].
The quality of the impression, whether obtained conventionally with materials like hydrocolloids or polyvinyl siloxanes or digitally trough scanning, is a determining factor in the final fit of the denture base. Information for CAD/CAM processing can be acquired either extraorally by scanning an impression or a model of the dental arch, or intraorally, by directly scanning the dental arch. There are different systems: mechanical digitalization, based on touch, and optical digitalization, which utilizes CBCT, laser, or light-emitting diode scanners [14]. In 2007, Quaas et al. [49] studied the measurement uncertainty and accuracy of data obtained from mechanical digitalization and concluded that the measurement uncertainty was low, while the accuracy was high. However, they ruled out this method for scanning impressions with flexible materials, as the physical contact of the scanner with the impression could deform it and increase imprecision [14,49]. In 2012, Goodacre et al. [12] introduced a technique to obtain definitive impressions of edentulous maxillary and mandibular arches, which would later be scanned. They also described how to record the neutral zona, the position of the maxillary and mandibular anterior teeth, palatal morphology, VDO, and interocclusal relationship, and added this data to the scanned impressions to fabricate the denture base trough milling. Additionally, it is essential to consider that saliva on soft tissues and their movements can influence the quality of digital impressions [7,12,14].
Flexural strength (Table 3) is considered a reflection of the resistance and stiffness of the studied material and serves to evaluate the quality of material polymerization [50]. Although PMMA acrylic resins are the most used materials in the fabrication of both digital and conventional dentures, they are susceptible to fractures due to the material´s brittleness when subjected to impacts. Thermopolymerizable resins used in the fabrication of conventional dentures exhibit good physical and mechanical properties, although some drawbacks related to polymerization have been described, such as high porosity, potential for cracking, and volumetric and linear shrinkage [51]. On the other hand, pre-polymerized resins used in milled dentures exhibit higher flexural strength. These resin discs are polymerized under high temperature and pressure, leading to the formation of longer polymer chains, resulting in lower residual monomer values and minimal porosity. Additionally, the polymerization process leads to a reduction in the intermolecular distance of the resin, which could explain the improved mechanical behavior of pre-polymerized PMMA [51].

Table 3.
Analysis of the flexural strength, modulus of elasticity, and hardness of the prosthetic base.
Materials with a high modulus of elasticity are more resistant to elastic deformation, allowing the fabrication of thinner denture bases. Becerra et al. [54] and Iwaki et al. [55] determined that digital dentures exhibited a higher modulus of elasticity compared to conventional dentures [54,55]. The main advantage of this is that a denture base resistant to plastic deformation provides greater occlusal stability [51]. In several studies by Al-Dwairi et al. [50,52] (2019 and 2020), digital dentures showed higher flexural strength and greater surface hardness, indicating a higher modulus of elasticity than conventional dentures, which was also confirmed in the study by Alp et al. This could be attributed to a lower monomer content in digital dentures, reducing the plasticity of PMMA [50,52,53]. However, in the study by Perea-Lowery et al. [51], no significant differences in hardness were found between the two groups [6,51]. Prpić V et al. [36] confirmed the results of Perea-Lowery et al. [51], but pointed out that the different results were not solely due to different polymerization methods, but could also be influenced by the use of different materials from different manufacturers [6,36,51].
Many authors such as Angelara et al. [56] and Arslan et al. [16] state that the flexural strength of pre-polymerized PMMA (used in milled dentures) is higher than conventionally polymerized PMMA due to conditions under which polymerization occurs (for pre-polymerized PMMA, high pressures and temperatures), the homogeneity of the denture base and its higher density, minimal contraction that takes place, and the reduced amount of pores and free monomer [16,56]. Choi et al. [57] and Srinivasan et al. [13] reported that conventionally polymerized PMMA had higher toughness than pre-polymerized PMMA, meaning it could absorb more force before fracturing, attributed to the amount of free monomer in the material: higher monomer content resulted in greater material plasticity and, therefore, higher toughness [6,18,36,57]. Over time, pre-polymerized PMMA exhibits less swelling and deterioration than conventional PMMA due to lower water absorption and less difference in thermal expansion between the denture base and artificial teeth, resulting in minimal differences in terms of toughness [6].
Prosthetic stomatitis is an inflammation of the palatal mucosa covered by the denture caused by the accumulation of Candida albicans. A smooth surface is important in any restoration to reduce the formation of a biofilm. Milled denture bases have lower porosity, while conventional dentures, even after final polishing, are associated with a higher presence of Candida [37]. Numerous researchers such as Al-Dwairi et al. [52], Klaiber et al. [34], Chang et al. [58], Murat et al. [59], or Al-Fouzan et al. [60] (Table 4) found that the surface roughness of PMMA denture bases in conventional dentures was higher than in milled PMMA. The reduced number and size of pores are mainly due to a lower amount of residual monomer and the polymerization technique, which gives digital dentures better properties, such as reduced microbial adhesion to the surface, less plaque retention, and fewer surface alterations. However, other authors like Arslan et al. [16] did not find significant differences in surface roughness between both types of dentures. This discrepancy in the results may be due to factors such as different water solubility, hardness, microstructure, and chemical configuration of the studied materials [6,16,34,52,58,59,60]. In the case of printed dentures, Srinivasan et al. [13] determined that the degree of surface roughness was similar to milled dentures. However, using resins and 3D printers not recommended by the manufacturer may negatively influence this aspect, significantly increasing the roughness of the denture base [18].

Table 4.
Analysis of the surface roughness of the prosthetic base.
The biocompatibility (Table 5) of dentures largely depends on the amount of residual free monomer released by the resin after polymerization. Ayman et al. [17] observed that the release of free monomer was higher in the thermopolymerizable resins used in the fabrication of conventional dentures, mainly due to the pre-polymerization of the discs used for milling the dentures [17]. According to Engler et al. [61], the monomer release depends on the material used, so it will be different depending on the manufacturing method used. In the case of conventional dentures, the initial monomer release is considerably higher than in digital dentures but remains more stable over time, while pre-polymerized PMMA increases the monomer release over the days [61]. However, other authors such as Steinmassl et al. [45] concluded that although digital dentures had a lower amount of free monomer than conventional dentures, the differences were not significant [45].

Table 5.
Analysis of the biocompatibility of the prosthetic base.
Another influential factor in the biocompatibility of dentures is microbial adhesion (Table 5), closely related to the previously mentioned surface roughness. Both Al-Fouzan et al. [60] and Murat et al. [59] found that microbial adhesion, mainly by Candida albicans, was higher in conventional dentures due to increased surface roughness [59,60]. In terms of overall biocompatibility, both milled and 3D-printed dentures showed good compatibility with oral tissues, with no significant differences between them [1].
Regarding aesthetics (Table 6), the most decisive factor is the color stability of both the denture base and the used teeth. This variable is inversely related to surface roughness: the higher the surface roughness, the lower the color stability. Authors such as Dayan et al. [62] and Iwaki et al. [55] concluded that the resins used in milled dentures showed fewer color changes compared to other resins [37,50]. Gruber et al. [63] found no significant differences between conventional dentures and milled dentures, with the 3D-printed resins showing the most color changes [51]. However, some studies, like the one by Alp et al. [53], confirmed that the color changes observed in any type of denture were within clinically acceptable ranges [39].

Table 6.
Aesthetic analysis of the prostheses.
The null hypothesis was accepted, as digital prosthetics demonstrated better performance than conventional prosthetics. However, the review presents numerous limitations such as the different manufacturing methods, the small sample size used in the consulted studies, or the need to consult more articles.
The future of dentistry is being explored through the possibilities offered by digital systems. The advances made possible by these systems are evident today. Concerning the topic of complete prosthetics produced using digital systems, there is still a long way to go, largely due to the need to research improvements in materials and the necessity to enhance and reduce the cost of the equipment that facilitates their fabrication. The use of digital systems for prostheses allows the dentist to intervene and modify parameters to meet the patient´s needs. Furthermore, it constitutes an important marketing tool for convincing the patient (previews and smile design). However, it comes with certain drawbacks, such as a higher production cost, the need for equipment investment, and a steep learning curve to achieve satisfactory results. Undoubtedly, the future of prosthodontics lies in applying all the technological advancements at our disposal, which are already demonstrating their ability to address the issues associated with conventional methods.
5. Conclusions
As a result of the conducted review and in accordance with the specific objectives outlined, the following conclusions were drawn:
- Regarding fit, retention, fracture resistance, surface roughness, biocompatibility, and aesthetics, digital prostheses, particularly the milled ones, have demonstrated superior performance.
- The planning process of digital prostheses, with its advantage of preserving all data and prosthetic designs, except anatomical registers, facilitates quick retrieval at any time.
Author Contributions
Conceptualization, S.D.Z. and A.D.; methodology, S.D.Z.; validation, A.D., Y.G. and J.M.; formal analysis, J.D.Z.; investigation, S.D.Z.; resources, J.D.Z.; writing—original draft preparation, S.D.Z.; writing—review and editing, J.D.Z. and J.M.; visualization, Y.G.; supervision, A.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Alfadda, S.A. The relationship between various parameters of complete denture quality and patients’ satisfaction. J. Am. Dent. Assoc. 2014, 145, 941–948. [Google Scholar] [CrossRef]
- Sanjeevan, V.; Rajagopal, P.; Venkitachalam, R.; Aras, M. Efficiency of simplified versus traditional denture fabrication methods: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, 126, 377–385. [Google Scholar] [CrossRef]
- Han, W.; Li, Y.; Zhang, Y.; Lv, Y.; Zhang, Y.; Hu, P.; Liu, H.; Ma, Z.; Shen, Y. Design and fabrication of complete dentures using CAD/CAM technology. Medicine 2017, 96, e5435. [Google Scholar] [CrossRef]
- Jokstad, A.; Ganeles, J. Systematic review of clinical and patient-reported outcomes following oral rehabilitation on dental implants with a tapered compared to a non-tapered implant design. Clin. Oral. Implants Res. 2018, 29, 41–54. [Google Scholar] [CrossRef]
- Romanos, G.E.; Delgado-Ruiz, R.; Sculean, A. Concepts for prevention of complications in implant therapy. Periodontology 2000 2019, 81, 7–17. [Google Scholar] [CrossRef]
- Jasiūnaitė, A.; Verenis, A.M.; Ivanauskienė, E.; Zilinskas, J. A comparison of mechanic properties regarding complete removable dentures, which were made from polymethylmetacrilate (PMMA) during conventional and CAD/CAM processes. Systemic literature review. Stomatologija 2022, 24, 3–12. [Google Scholar]
- Faty, M.; Sabet, M.; Thabet, Y. A Comparison of Denture Base Retention and Adaptation between CAD-CAM and Conventional Fabrication Techniques. Int. J. Prosthodont. 2023, 36, 469–478. Available online: http://quintpub.com/journals/ijp/abstract.php?iss2_id=1453&article_id=21203 (accessed on 18 May 2023). [CrossRef]
- de Villa Camargos, G.; Armenine, T.E.; Paleari, A.G.; Nascimento, G.M.O.; Munhoz, M.F.V. Teaching Complete Denture Procedures to Dental Students by Conventional or Simplified Methods: A Randomized Clinical Trial. J. Dent. Educ. 2019, 83, 303–313. [Google Scholar] [CrossRef]
- Emera, R.M.K.; Shady, M.; Alnajih, M.A. Comparison of retention and denture base adaptation between conventional and 3D-printed complete dentures. J. Dent. Res. Dent. Clin. Dent. Prospects 2022, 16, 179–185. [Google Scholar] [CrossRef]
- Vecchia, M.P.D.; Regis, R.R.; Cunha, T.R.; de Andrade, I.M.; da Matta, J.C.S.; de Souza, R.F. A Randomized Trial on Simplified and Conventional Methods for Complete Denture Fabrication: Cost Analysis: Cost of Simplified Complete Dentures. J. Prosthodont. 2014, 23, 182–191. [Google Scholar] [CrossRef]
- Ohara, K.; Isshiki, Y.; Hoshi, N.; Ohno, A.; Kawanishi, N.; Nagashima, S.; Inoue, M.; Kubo, D.; Yamaya, K.; Inoue, E.; et al. Patient satisfaction with conventional dentures vs. digital dentures fabricated using 3D-printing: A randomized crossover trial. J. Prosthodont. Res. 2022, 66, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Goodacre, C.J.; Garbacea, A.; Naylor, W.P.; Daher, T.; Marchack, C.B.; Lowry, J. CAD/CAM fabricated complete dentures: Concepts and clinical methods of obtaining required morphological data. J. Prosthet. Dent. 2012, 107, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.; Kalberer, N.; Naharro, M.; Marchand, L.; Lee, H.; Müller, F. CAD-CAM milled dentures: The Geneva protocols for digital dentures. J. Prosthet. Dent. 2020, 123, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Infante, L.; Yilmaz, B.; McGlumphy, E.; Finger, I. Fabricating complete dentures with CAD/CAM technology. J. Prosthet. Dent. 2014, 111, 351–355. [Google Scholar] [CrossRef]
- Yilmaz, B.; Azak, A.N.; Alp, G.; Ekşi, H. Use of CAD-CAM technology for the fabrication of complete dentures: An alternative technique. J. Prosthet. Dent. 2017, 118, 140–143. [Google Scholar] [CrossRef]
- Arslan, M.; Murat, S.; Alp, G.; Zaimoglu, A. Evaluation of flexural strength and surface properties of prepolymerized CAD/CAM PMMA-based polymers used for digital 3D complete dentures. Int. J. Comput. Dent. 2018, 21, 31–40. [Google Scholar]
- Ayman, A.D. The residual monomer content and mechanical properties of CAD\CAM resins used in the fabrication of complete dentures as compared to heat cured resins. Electron. Physician 2017, 9, 4766–4772. [Google Scholar] [CrossRef]
- Srinivasan, M.; Kalberer, N.; Kamnoedboon, P.; Mekki, M.; Durual, S.; Özcan, M.; Müller, F. CAD-CAM complete denture resins: An evaluation of biocompatibility, mechanical properties, and surface characteristics. J. Dent. 2021, 114, 103785. [Google Scholar] [CrossRef]
- Paolone, G.; Mandurino, M.; De Palma, F.; Mazzitelli, C.; Scotti, N.; Breschi, L.; Gherlone, E.; Cantatore, G.; Vichi, A. Color Stability of Polymer-Based Composite CAD/CAM Blocks: A Systematic Review. Polymers 2023, 15, 464. [Google Scholar] [CrossRef]
- Clark, W.A.; Brazile, B.; Matthews, D.; Solares, J.; De Kok, I.J. A Comparison of Conventionally Versus Digitally Fabricated Denture Outcomes in a University Dental Clinic. J. Prosthodont. 2021, 30, 47–50. [Google Scholar] [CrossRef]
- Wang, C.; Shi, Y.F.; Xie, P.J.; Wu, J.H. Accuracy of digital complete dentures: A systematic review of in vitro studies. J. Prosthet. Dent. 2021, 125, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Kattadiyil, M.T.; AlHelal, A. An update on computer-engineered complete dentures: A systematic review on clinical outcomes. J. Prosthet. Dent. 2017, 117, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.; Kalberer, N.; Fankhauser, N.; Naharro, M.; Maniewicz, S.; Müller, F. CAD-CAM complete removable dental prostheses: A double-blind, randomized, crossover clinical trial evaluating milled and 3D-printed dentures. J. Dent. 2021, 115, 103842. [Google Scholar] [CrossRef]
- Stansbury, J.W.; Idacavage, M.J. 3D printing with polymers: Challenges among expanding options and opportunities. Dent. Mater. 2016, 32, 54–64. [Google Scholar] [CrossRef] [PubMed]
- AlHelal, A.; AlRumaih, H.S.; Kattadiyil, M.T.; Baba, N.Z.; Goodacre, C.J. Comparison of retention between maxillary milled and conventional denture bases: A clinical study. J. Prosthet. Dent. 2017, 117, 233–238. [Google Scholar] [CrossRef]
- Goodacre, B.J.; Goodacre, C.J.; Baba, N.Z.; Kattadiyil, M.T. Comparison of denture base adaptation between CAD-CAM and conventional fabrication techniques. J. Prosthet. Dent. 2016, 116, 249–256. [Google Scholar] [CrossRef]
- Lozado, J.; Garbacea, A.; Goodacre, C.; Kattadiyil, M. Use of a Digitally Planned and Fabricated Mandibular Complete Denture for Easy Conversion to an Immediately Loaded Provisional Fixed Complete Denture. Part 1. Planning and Surgical Phase. Int. J. Prosthodont. 2014, 27, 417–421. [Google Scholar] [CrossRef]
- Fueki, K.; Inamochi, Y.; Wada, J.; Arai, Y.; Takaichi, A.; Murakami, N.; Ueno, T.; Wakabayashi, N. A systematic review of digital removable partial dentures. Part I: Clinical evidence, digital impression, and maxillomandibular relationship record. J. Prosthodont. Res. 2022, 66, 40–52. [Google Scholar] [CrossRef]
- Ender, A.; Zimmermann, M.; Mehl, A. Accuracy of Complete- and Partial-Arch Impressions of Actual Intraoral Scanning Systems In Vitro. 2019. Available online: https://www.zora.uzh.ch/id/eprint/180700 (accessed on 7 February 2023).
- Srinivasan, M.; Kamnoedboon, P.; McKenna, G.; Angst, L.; Schimmel, M.; Özcan, M.; Müller, F. CAD-CAM removable complete dentures: A systematic review and meta-analysis of trueness of fit, biocompatibility, mechanical properties, surface characteristics, color stability, time-cost analysis, clinical and patient-reported outcomes. J. Dent. 2021, 113, 103777. [Google Scholar] [CrossRef]
- Paulino, M.R.; Alves, L.R.; Gurgel, B.C.V.; Calderon, P.S. Simplified versus traditional techniques for complete denture fabrication: A systematic review. J. Prosthet. Dent. 2015, 113, 12–16. [Google Scholar] [CrossRef]
- Bidra, A.S.; Taylor, T.D.; Agar, J.R. Computer-aided technology for fabricating complete dentures: Systematic review of historical background, current status, and future perspectives. J. Prosthet. Dent. 2013, 109, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, S.; Kanazawa, M.; Iwaki, M.; Jokanovic, A.; Minakuchi, S. Effects of offset values for artificial teeth positions in CAD/CAM complete denture. Comput. Biol. Med. 2014, 52, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Klaiber, D.; Spintzyk, S.; Geis-Gerstorfer, J.; Klink, A.; Unkovskiy, A.; Huettig, F. Bonding Behavior of Conventional PMMA towards Industrial CAD/CAM PMMA and Artificial Resin Teeth for Complete Denture Manufacturing in a Digital Workflow. Materials 2021, 14, 3822. [Google Scholar] [CrossRef] [PubMed]
- Kattadiyil, M.T.; Jekki, R.; Goodacre, C.J.; Baba, N.Z. Comparison of treatment outcomes in digital and conventional complete removable dental prosthesis fabrications in a predoctoral setting. J. Prosthet. Dent. 2015, 114, 818–825. [Google Scholar] [CrossRef]
- Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; Čimić, S. Comparison of Mechanical Properties of 3D-Printed, CAD/CAM, and Conventional Denture Base Materials. J. Prosthodont. 2020, 29, 524–528. [Google Scholar] [CrossRef]
- Mubaraki, M.Q.; Al Moaleem, M.M.; Alzahrani, A.H.; Shariff, M.; Alqahtani, S.M.; Porwal, A.; Al-Sanabani, F.A.; Bhandi, S.; Tribst, J.P.M.; Heboyan, A.; et al. Assessment of Conventionally and Digitally Fabricated Complete Dentures: A Comprehensive Review. Materials 2022, 15, 3868. [Google Scholar] [CrossRef]
- AlRumaih, H.S.; AlHelal, A.; Baba, N.Z.; Goodacre, C.J.; Al-Qahtani, A.; Kattadiyil, M.T. Effects of denture adhesive on the retention of milled and heat-activated maxillary denture bases: A clinical study. J. Prosthet. Dent. 2018, 120, 361–366. [Google Scholar] [CrossRef]
- Einarsdottir, E.R.; Geminiani, A.; Chochlidakis, K.; Feng, C.; Tsigarida, A.; Ercoli, C. Dimensional stability of double-processed complete denture bases fabricated with compression molding, injection molding, and CAD-CAM subtraction milling. J. Prosthet. Dent. 2020, 124, 116–121. [Google Scholar] [CrossRef]
- McLaughlin, J.B.; Ramos, V.; Dickinson, D.P. Comparison of Fit of Dentures Fabricated by Traditional Techniques Versus CAD/CAM Technology. J. Prosthodont. 2019, 28, 428–435. [Google Scholar] [CrossRef]
- Steinmassl, O.; Dumfahrt, H.; Grunert, I.; Steinmassl, P.A. CAD/CAM produces dentures with improved fit. Clin. Oral. Investig. 2018, 22, 2829–2835. [Google Scholar] [CrossRef]
- Tasaka, A.; Matsunaga, S.; Odaka, K.; Ishizaki, K.; Ueda, T.; Abe, S.; Yoshinari, M.; Yamashita, S.; Sakurai, K. Accuracy and retention of denture base fabricated by heat curing and additive manufacturing. J. Prosthodont. Res. 2019, 63, 85–89. [Google Scholar] [CrossRef]
- Hwang, H.J.; Lee, S.J.; Park, E.J.; Yoon, H.I. Assessment of the trueness and tissue surface adaptation of CAD-CAM maxillary denture bases manufactured using digital light processing. J. Prosthet. Dent. 2019, 121, 110–117. [Google Scholar] [CrossRef]
- Srinivasan, M.; Cantin, Y.; Mehl, A.; Gjengedal, H.; Müller, F.; Schimmel, M. CAD/CAM milled removable complete dentures: An in vitro evaluation of trueness. Clin. Oral. Investig. 2017, 21, 2007–2019. [Google Scholar] [CrossRef]
- Steinmassl, P.A.; Wiedemair, V.; Huck, C.; Klaunzer, F.; Steinmassl, O.; Grunert, I.; Dumfahrt, H. Do CAD/CAM dentures really release less monomer than conventional dentures? Clin. Oral. Investig. 2017, 21, 1697–1705. [Google Scholar] [CrossRef]
- Lee, S.; Hong, S.J.; Paek, J.; Pae, A.; Kwon, K.R.; Noh, K. Comparing accuracy of denture bases fabricated by injection molding, CAD/CAM milling, and rapid prototyping method. J. Adv. Prosthodont. 2019, 11, 55. [Google Scholar] [CrossRef]
- Wemken, G.; Spies, B.C.; Pieralli, S.; Adali, U.; Beuer, F.; Wesemann, C. Do hydrothermal aging and microwave sterilization affect the trueness of milled, additive manufactured and injection molded denture bases? J. Mech. Behav. Biomed. Mater. 2020, 111, 103975. [Google Scholar] [CrossRef]
- Hsu, C.Y.; Yang, T.C.; Wang, T.M.; Lin, L.D. Effects of fabrication techniques on denture base adaptation: An in vitro study. J. Prosthet. Dent. 2020, 124, 740–747. [Google Scholar] [CrossRef]
- Quaas, S.; Rudolph, H.; Luthardt, R.G. Direct mechanical data acquisition of dental impressions for the manufacturing of CAD/CAM restorations. J. Dent. 2007, 35, 903–908. [Google Scholar] [CrossRef]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J. A Comparison of the Flexural and Impact Strengths and Flexural Modulus of CAD/CAM and Conventional Heat-Cured Polymethyl Methacrylate (PMMA). J. Prosthodont. 2020, 29, 341–349. [Google Scholar] [CrossRef]
- Perea-Lowery, L.; Minja, I.K.; Lassila, L.; Ramakrishnaiah, R.; Vallittu, P.K. Assessment of CAD-CAM polymers for digitally fabricated complete dentures. J. Prosthet. Dent. 2021, 125, 175–181. [Google Scholar] [CrossRef]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J.; Özcan, M. A Comparison of the Surface Properties of CAD/CAM and Conventional Polymethylmethacrylate (PMMA). J. Prosthodont. 2019, 28, 452–457. [Google Scholar] [CrossRef]
- Alp, G.; Murat, S.; Yilmaz, B. Comparison of Flexural Strength of Different CAD/CAM PMMA-Based Polymers: Comparison of Flexural Strength of Interim Resin Materials. J. Prosthodont. 2019, 28, e491–e495. [Google Scholar] [CrossRef]
- Becerra, J.; Mainjot, A.; Hüe, O.; Sadoun, M.; Nguyen, J. Influence of High-Pressure Polymerization on Mechanical Properties of Denture Base Resins. J. Prosthodont. 2021, 30, 128–134. [Google Scholar] [CrossRef]
- Iwaki, M.; Kanazawa, M.; Arakida, T.; Minakuchi, S. Mechanical properties of a polymethyl methacrylate block for CAD/CAM dentures. J. Oral. Sci. 2020, 62, 420–422. [Google Scholar] [CrossRef]
- Angelara, K.; Bratos, M.; Sorensen, J.A. Comparison of strength of milled and conventionally processed PMMA complete-arch implant-supported immediate interim fixed dental prostheses. J. Prosthet. Dent. 2023, 129, 221–227. [Google Scholar] [CrossRef]
- Choi, J.J.E.; Uy, C.E.; Plaksina, P.; Ramani, R.S.; Ganjigatti, R.; Waddell, J.N. Bond Strength of Denture Teeth to Heat-Cured, CAD/CAM and 3D Printed Denture Acrylics. J. Prosthodont. 2020, 29, 415–421. [Google Scholar] [CrossRef]
- Chang, Y.H.; Lee, C.Y.; Hsu, M.S.; Du, J.K.; Chen, K.K.; Wu, J.H. Effect of toothbrush/dentifrice abrasion on weight variation, surface roughness, surface morphology and hardness of conventional and CAD/CAM denture base materials. Dent. Mater. J. 2021, 40, 220–227. [Google Scholar] [CrossRef]
- Murat, S.; Alp, G.; Alatalı, C.; Uzun, M. In Vitro Evaluation of Adhesion of Candida albicans on CAD/CAM PMMA-Based Polymers: Adhesion of C. albicans on CAD/CAM PMMA-Based Polymers. J. Prosthodont. 2019, 28, e873–e879. [Google Scholar] [CrossRef]
- Al-Fouzan, A.F.; Al-mejrad, L.A.; Albarrag, A.M. Adherence of Candida to complete denture surfaces in vitro: A comparison of conventional and CAD/CAM complete dentures. J. Adv. Prosthodont. 2017, 9, 402. [Google Scholar] [CrossRef]
- Engler, M.L.P.D.; Güth, J.F.; Keul, C.; Erdelt, K.; Edelhoff, D.; Liebermann, A. Residual monomer elution from different conventional and CAD/CAM dental polymers during artificial aging. Clin. Oral. Investig. 2020, 24, 277–284. [Google Scholar] [CrossRef]
- Dayan, C.; Celik Guven, M.; Gencel, B.; Bural, C. A Color Stability Comparison of Conventional and CAD/CAM Polymethyl Methacrylate Denture Base Materials. Acta Stomatol. Croat. 2019, 53, 158–167. [Google Scholar] [CrossRef]
- Gruber, S.; Kamnoedboon, P.; Özcan, M.; Srinivasan, M. CAD/CAM Complete Denture Resins: An In Vitro Evaluation of Color Stability. J. Prosthodont. 2021, 30, 430–439. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).