Brief Narrative Review on Commercial Dental Sealants—Comparison with Respect to Their Composition and Potential Modifications
Abstract
1. Introduction
2. Methods
3. Results
3.1. Comparison of Composition of Commercially Used Materials
| Product Name | Abbr. | Manufacturer | Composition | Fluoride Presence | Shear Bond Strength [MPa] | Hardness [HK] or [HV] | Shrinkage [%] | Light Curing | Material Classification | Ref. |
|---|---|---|---|---|---|---|---|---|---|---|
| Helioseal F | HF | Ivoclar Vivadent, Lichtenstein | bisphenol A-glycidyl methacrylate (Bis-GMA), dimethacrylates fluorosilicate glass, silica, titanium dioxide, initiators, and stabilizers | Yes | 13.7 ± 7.0 | 19.3 HV | 3.98 | Yes | Sealant | [19,20] |
| Helioseal | HS | Ivoclar Vivadent, Lichtenstein | Bis-GMA, triethylene glycol dimethacrylate (TEGDMA), titanium dioxide, stabilizers, and catalysts | No | 12 ± 1.0 | - | - | Yes | Sealant | [21,22] |
| Fissure Sealant | FS | Arkona | Bis-GMA, TEGDMA, Urethane dimethacrylate (UDMA), barium- aluminum-silicon glass, barium- aluminum-boron-fluorine glass, fire silica, photoinitiators (CQ:DMAEMA-camphorquinone:ethyl-4-dimethylaminobenzoate), stabilizers, pigments | Yes | - | - | - | Yes | Sealant | [23] |
| Embrace Wetbond | EW | Pulpdent, United States | Uncured acrylate ester monomers 55–60%, amorphous silica 5%, sodium fluoride < 2% | Yes | 21.7 ± 2.0 | 23.9 HV | 3.45 | Yes | Sealant | [19,24,25] |
| Fuji Triage | FT | GC Cooperation, Japan | Glass-ionomer, aluminofluorosilicate glass, polyacrylic acid, distilled water, polybase carboxylic acid | Yes | 3.5 ± 0.8 | 52.0 ± 1.0 HV * | - | Yes/No *** | Glass-ionomer | [26,27] |
| Smart Seal loc F | SSLF | Detax, Germany | bis(methacryloxyethyl) hydrogen phosphate, 2-propenoic acid, 2-methyl-2-hydroxyethyl ester, phosphate, 2-dimethylaminoethyl methacrylate | Yes | 9.5 ± 1.4 | - | 5.06 ± 1.20 | Yes | Sealant | [28,29] |
| Fuji VII EP | F7E | GC Cooperation, Japan | Fluoroaluminosilicate glass, casein phosphopeptide-amorphous calcium phosphate (CPP-ACP), pigment, distilled water, polyacrylic acid, polybase carboxylic acid | Yes | 5.0 ± 1.7 | 47.1 ± 6.0 HV | - | No | Glass-ionomer cement | [26,30] |
| GCP Glass Seal | GCP | GCP Dental, Netherlands | Nanoparticles glass ionomer-based material | Yes | - | 50.0 ± 1.5 HV | - | Yes/Nos | Glass-ionomer sealant | [27,31] |
| Ketac Molar | KM | 3M ESPE, Germany | Al-Ca-La fluorosilicate glass, 5%, copolymer of acrylic acid and maleic acid, polyacrylic acid, tartaric acid, water | Yes | 4.8 ± 1.0 | 89.9 ± 4.2 HV | - | No | Glass-ionomer | [32,33] |
| Voco Ionofil Molar AC Quick | IMAC | Voco, Germany | Water, polyacrylic acid, (+)-tartaric acid, aluminofluorosilicate glass, and pigments | Yes | 5.3 ± 0.6 | 79.9 ± 2.1 HV | - | No | Glass-ionomer | [32,34,35] |
| Equia Fil | EQF | GC Cooperation, Japan | Polyacrylic acid, aluminosilicate glass, distilled water | No | - | 99.3 ± 4.5 HV | - | No | Glass-ionomer | [32] |
| UltraSeal XT plus | USXT | Ultradent, USA | TEGDMA 10–25%, diurethane dimethacrylate 2.5–10%, aluminium oxide 2.5–10%, 2-hydroxyethyl methacrylate < 2.5%, amine methacrylate < 2.5%, organophosphine oxide < 2.5%, sodium monofluorophosphate < 0.1% | Yes | 42.7 | 27.6 HK | 5.98 | Yes | Sealant | [36,37] |
| Conseal F | CF | SDI, Australia | UDMA base 7% filled with a submicron filler size of 0.04 µm | No | 14.0 ± 0.9 | - | - | Yes | Sealant | [28] |
| Tetric Flow | TF | Vivadent | Bis-GMA (10–25%), UDMA (10–25%), ytterbium trifluoride, 1,10-decandiol dimethacrylate (2.5–10%), diphenyl(2,4,6- trimethylbenzoyl)phosphine oxide (0.1–2.5%), 2-(2-Hydroxy-5-methylphenyl)-benzotriazol; 2-(2H-Benzotriazol-2-yl)-p-kresol (0.1–1.0%) | Yes | 16.8 ± 2.7 | 34.0 HV ** | - | Yes | Flow composite | [20,38,39] |
| Tetric Evo Ceram | TEC | Vivadent | Dimethacrylate co-monomers (17–18 wt.%), barium glass, ytterbium trifluoride, mixed oxides and prepolymers (82–83 wt.%) | Yes | 20.7 ± 7.2 | 51.0 HV ** | 1.95 ± 0.03 | Yes | composite | [38,40,41] |
| Wave | WV | SDI, Australia | UDMA, strontium glass | No | 24.6 ± 1.5 | - | 5.00 | Yes | Flow composite | [42,43] |
| Clinpro Sealant | CS | 3M ESPE, Germany | TEGDMA, bisphenol A digilycidyl ether dimethacrylate, tetrabuttylammonium tetrafluoroborate, silane-treated silica | Yes | 12.8 ± 8.3 | 21.5 ± 0.2 HV | 6.60 ± 1.54 | Yes | Sealant | [29,44,45] |
| Grandio Seal | GS | Voco, Germany | TEGDMA (10–25%), fumed silica (5–10%), Bis-GMA (2.5–5%) | No | 42.6 ± 3.2 | 75.1 ± 2.0 HV | - | Yes | Sealant | [45,46,47] |
| Fissurit FX | FFX | Voco, Germany | TEGDMA (15–25%), Bis-GMA (5–10%), sodium fluoride (≤2.5%) | Yes | 6.2 ± 0.7 | - | 4.30 ± 1.15 | Yes | Sealant | [29,48,49] |
| Dyract Seal | DS | Dentsply, Germany | Patented macromonomers (AP and M-1A-BSA), strontium-aluminium, fluorosilicate glass, Diethylene glycol dimethacrylate DGDMA, dispersed silicon oxide (Aerosil), initiators, inhibitor | Yes | 8.3 ± 0.3 | - | 5.38 ± 1.30 | Yes | Sealant | [29,50] |
| Teethmate F-1 | TF1 | Kuraray, Japan | 2-hydroxyethyl methacrylate, TEGDMA, 10-methacryloyloxydecyl dihydrogen phosphate, methacryloylfluoride-methyl methacrylate copolymer, hydrophobic aromatic dimethacrylate, d,l-camphorquinone, initiators, accelerators, dyes | Yes | - | 26.7 ± 1.3 HV * | 7.40 ± 1.17 | [27,29] |
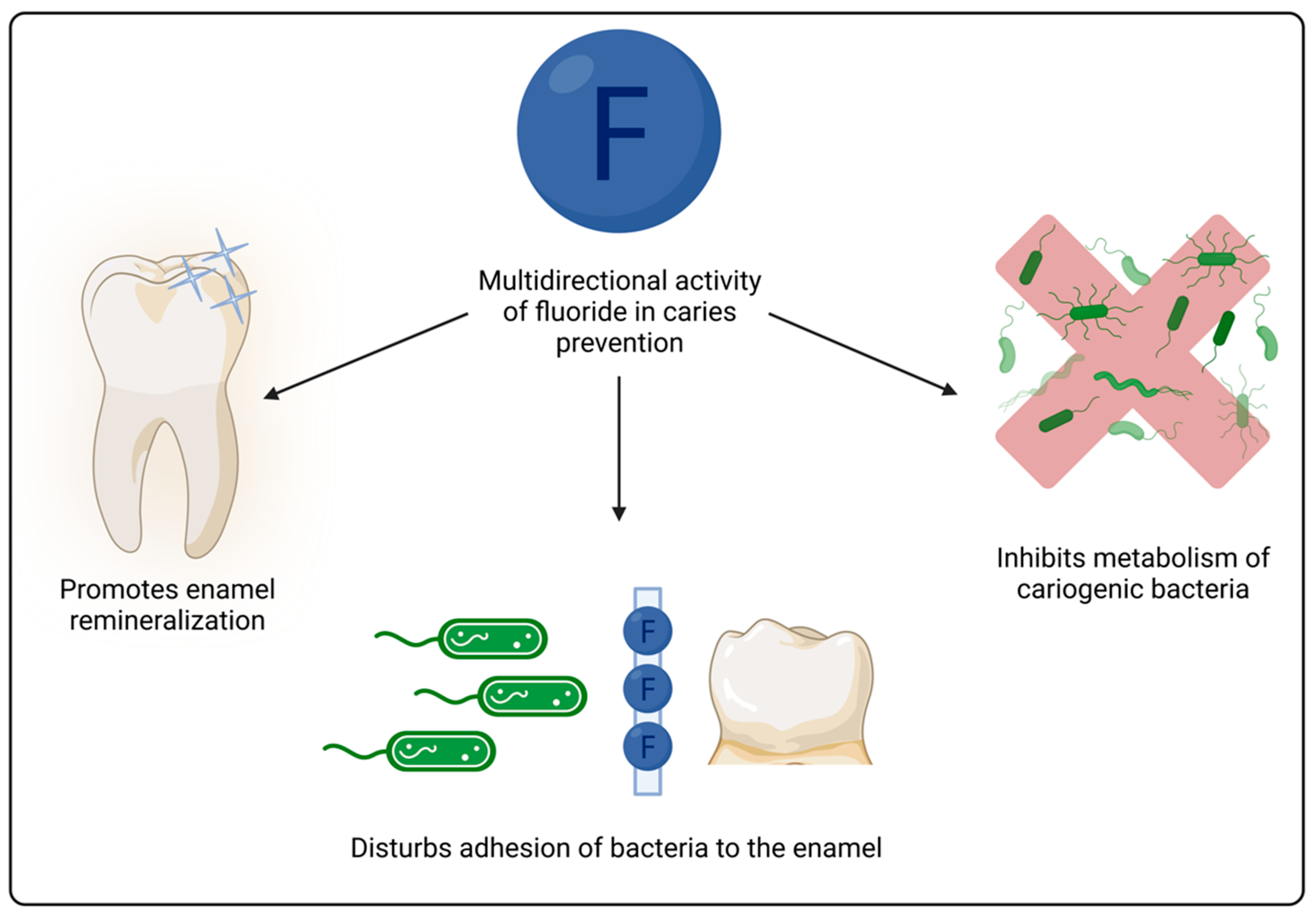
3.2. Modifications in Composition
3.3. Indications for Use
3.4. Microleakage and Adhesion
3.5. Effectiveness of Sealing and Future Perspectives
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Sugars and Dental Caries. Available online: https://www.who.int/news-room/fact-sheets/detail/sugars-and-dental-caries (accessed on 1 June 2023).
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.L.; Marcenes, W. Global Burden of Untreated Caries: A Systematic Review and Metaregression. J. Dent. Res. 2015, 94, 650–658. [Google Scholar] [CrossRef]
- Naaman, R.; El-Housseiny, A.A.; Alamoudi, N. The Use of Pit and Fissure Sealants—A Literature Review. Dent. J. 2017, 5, 34. [Google Scholar] [CrossRef] [PubMed]
- Nebu, P. State of the Art Enamel Remineralization Systems: The Next Frontier in Caries Management. Caries Res. 2019, 53, 284–295. [Google Scholar] [CrossRef]
- Nouri, M.-R.; Titley, K.C. Paediatrics: A Review of the Antibacterial Effect of Fluoride. Available online: https://www.oralhealthgroup.com/features/paediatrics-a-review-of-the-antibacterial-effect-of-fluoride/ (accessed on 23 August 2023).
- Bijle, M.N.A.; Ekambaram, M.; Lo, E.C.M.; Yiu, C.K.Y. The Combined Antimicrobial Effect of Arginine and Fluoride Toothpaste. Sci. Rep. 2019, 9, 8405. [Google Scholar] [CrossRef]
- Lubojanski, A.; Dobrzynski, M.; Nowak, N.; Rewak-Soroczynska, J.; Sztyler, K.; Zakrzewski, W.; Dobrzynski, W.; Szymonowicz, M.; Rybak, Z.; Wiglusz, K.; et al. Application of Selected Nanomaterials and Ozone in Modern Clinical Dentistry. Nanomaterials 2021, 11, 259. [Google Scholar] [CrossRef] [PubMed]
- Rošin-Grget, K.; Peroš, K.; Sutej, I.; Bašić, K. The Cariostatic Mechanisms of Fluoride. Acta Med. Acad. 2013, 42, 179–188. [Google Scholar] [CrossRef]
- Llena-Puy, C. The Rôle of Saliva in Maintaining Oral Health and as an Aid to Diagnosis. Med. Oral Patol. Oral Cir. Bucal 2006, 11, E449–E455. [Google Scholar]
- Hicks, J.; Garcia-Godoy, F.; Flaitz, C. Biological Factors in Dental Caries: Role of Saliva and Dental Plaque in the Dynamic Process of Demineralization and Remineralization (Part 1). J. Clin. Pediatr. Dent. 2004, 28, 47–52. [Google Scholar] [CrossRef]
- Millsop, J.W.; Wang, E.A.; Fazel, N. Etiology, Evaluation, and Management of Xerostomia. Clin. Dermatol. 2017, 35, 468–476. [Google Scholar] [CrossRef]
- Fox, P.C.; Busch, K.A.; Baum, B.J. Subjective Reports of Xerostomia and Objective Measures of Salivary Gland Performance. J. Am. Dent. Assoc. 1987, 115, 581–584. [Google Scholar] [CrossRef]
- Hopcraft, M.S.; Tan, C. Xerostomia: An Update for Clinicians. Aust. Dent. J. 2010, 55, 238–244. [Google Scholar] [CrossRef]
- Villa, A.; Polimeni, A.; Strohmenger, L.; Cicciù, D.; Gherlone, E.; Abati, S. Dental Patients’ Self-Reports of Xerostomia and Associated Risk Factors. J. Am. Dent. Assoc. 2011, 142, 811–816. [Google Scholar] [CrossRef]
- Ahovuo-Saloranta, A.; Forss, H.; Walsh, T.; Nordblad, A.; Mäkelä, M.; Worthington, H.V. Pit and Fissure Sealants for Preventing Dental Decay in Permanent Teeth. Cochrane Database Syst. Rev. 2017, 2017, CD001830. [Google Scholar] [CrossRef]
- Wright, J.T.; Crall, J.J.; Fontana, M.; Gillette, E.J.; Nový, B.B.; Dhar, V.; Donly, K.; Hewlett, E.R.; Quinonez, R.B.; Chaffin, J.; et al. Evidence-Based Clinical Practice Guideline for the Use of Pit-and-Fissure Sealants: A Report of the American Dental Association and the American Academy of Pediatric Dentistry. J. Am. Dent. Assoc. 2016, 147, 672–682.e12. [Google Scholar] [CrossRef]
- Meereis, C.T.W.; Münchow, E.A.; de Oliveira da Rosa, W.L.; da Silva, A.F.; Piva, E. Polymerization Shrinkage Stress of Resin-Based Dental Materials: A Systematic Review and Meta-Analyses of Composition Strategies. J. Mech. Behav. Biomed. Mater. 2018, 82, 268–281. [Google Scholar] [CrossRef]
- Braga, R.R.; Ballester, R.Y.; Ferracane, J.L. Factors Involved in the Development of Polymerization Shrinkage Stress in Resin-Composites: A Systematic Review. Dent. Mater. 2005, 21, 962–970. [Google Scholar] [CrossRef]
- Arumugam, P. Comparative Evaluation of the Effect of Variation in Light-Curing Cycle with a Time Gap and Its Effect on Polymerization Shrinkage and Microhardness of Conventional Hydrophobic Sealants and Moisture-Tolerant Resin-Based Sealants: An in Vitro Study. Indian J. Multidiscip. Dent. 2018, 8, 13. [Google Scholar] [CrossRef]
- Babaji, P.; Vaid, S.; Deep, S.; Mishra, S.; Srivastava, M.; Manjooran, T. In Vitro Evaluation of Shear Bond Strength and Microleakage of Different Pit and Fissure Sealants. J. Int. Soc. Prev. Community Dent. 2016, 6, S111. [Google Scholar] [CrossRef] [PubMed]
- Ivoclar Vivadent. Helioseal; Ivoclar Vivadent: Schaan, Liechtenstein, 2019. [Google Scholar]
- Lekka, M.P.; Papagiannoulis, L.; Eliades, G.C.; Caputo, A.A. A Comparative in Vitro Study of Visible Light-cured Sealants. J. Oral Rehabil. 1989, 16, 287–299. [Google Scholar] [CrossRef] [PubMed]
- Arkona. Arkona Fissure Sealant Brochure. Available online: https://arkonadent.com/wp-content/uploads/2020/10/arkonadent-lak-szczelinowy-kompendium-wiedzy.pdf (accessed on 8 August 2023).
- Pulpdent Corporation. Embrace WetBond Safety Data Sheet. Available online: https://www.pulpdent.com/wp-content/uploads/2021/03/GHS-SDS-EMS.pdf (accessed on 23 July 2023).
- Panigrahi, A. Microtensile Bond Strength of Embrace Wetbond Hydrophilic Sealant in Different Moisture Contamination: An In-Vitro Study. J. Clin. Diagn. Res. 2015, 9, ZC23. [Google Scholar] [CrossRef] [PubMed]
- Kucukyilmaz, E.; Savas, S. Evaluation of Shear Bond Strength, Penetration Ability, Microleakage and Remineralisation Capacity of Glass Ionomer-Based Fissure Sealants. Eur. J. Paediatr. Dent. 2016, 17, 17–23. [Google Scholar] [PubMed]
- Arslanoğlu, Z.; Altan, H.; Kale, E.; Bılgıç, F.; Şahin, O. Nanomechanical Behaviour and Surface Roughness of New Generation Dental Fissure Sealants. Acta Phys. Pol. A 2016, 130, 388–393. [Google Scholar] [CrossRef]
- Muwaffaq Attash, Z.; Sami Gasgoos, Z. Shear Bond Strength of Four Types of Pit and Fissure Sealants (In Vitro Study). Int. J. Enhanc. Res. Sci. Technol. Eng. 2018, 7, 1–7. [Google Scholar]
- Kucukyilmaz, E.; Savas, S.; Sener, Y.; Tosun, G.; Botsali, M. Polymerization Shrinkage of Six Different Fissure Sealants. J. Restor. Dent. 2014, 2, 88. [Google Scholar] [CrossRef]
- Zalizniak, I.; Palamara, J.E.A.; Wong, R.H.K.; Cochrane, N.J.; Burrow, M.F.; Reynolds, E.C. Ion Release and Physical Properties of CPP–ACP Modified GIC in Acid Solutions. J. Dent. 2013, 41, 449–454. [Google Scholar] [CrossRef]
- Elkwatehy, W.M.A.; Bukhari, O.M. The Efficacy of Different Sealant Modalities for Prevention of Pits and Fissures Caries: A Randomized Clinical Trial. J. Int. Soc. Prev. Community Dent. 2019, 9, 119. [Google Scholar] [CrossRef]
- Gavic, L.; Gorseta, K.; Borzabadi-Farahani, A.; Tadin, A.; Glavina, D.; van Duinen, R.; Lynch, E. Influence of Thermo-Light Curing with Dental Light-Curing Units on the Microhardness of Glass-Ionomer Cements. Int. J. Periodontics Restor. Dent. 2016, 36, 425–430. [Google Scholar] [CrossRef]
- Murthy, S.S.; Murthy, G.S. Comparative Evaluation of Shear Bond Strength of Three Commercially Available Glass Ionomer Cements in Primary Teeth. J. Int. Oral Health 2015, 7, 103. [Google Scholar]
- VOCO. Ionofil Safety Data Sheet. Available online: https://www.voco.dental/en/portaldata/1/resources/products/safety-data-sheets/gb/voco-ionofil-molar-ac_sds_gb.pdf (accessed on 23 August 2022).
- Shebl, E.A.; Etman, W.M.; Genaid, T.M.; Shalaby, M.E. Durability of Bond Strength of Glass-Ionomers to Enamel. Tanta Dent. J. 2015, 12, 16–27. [Google Scholar] [CrossRef]
- Ultradent. Ultraseal XT Brochure. Available online: https://assets.ctfassets.net/wfptrcrbtkd0/6CDOVq0rW3Ia1bBseRnDYG/5de0b1fac706906d9c3577d36589e1ad/UltraSeal-XT-Sealant-Family-Sales-Sheet-1007280AR03.pdf (accessed on 1 May 2023).
- Ultradent. UltraSeal XT Plus Safety Data Sheet. Available online: https://optident.co.uk/app/uploads/2018/03/UltraSeal-XT%C2%AE-plus-SDS-English.pdf (accessed on 8 August 2023).
- Hannig, C.; Duong, S.; Becker, K.; Brunner, E.; Kahler, E.; Attin, T. Effect of Bleaching on Subsurface Micro-Hardness of Composite and a Polyacid Modified Composite. Dent. Mater. 2007, 23, 198–203. [Google Scholar] [CrossRef]
- Ivoclar Vivadent. Tetric EvoFlow Safety Data Sheet. Available online: https://www.ivoclar.com/pl_pl/eifu?document-id=36624&show-detail=1 (accessed on 27 September 2023).
- Oglakci, B.; Arhun, N. The Shear Bond Strength of Repaired High-Viscosity Bulk-Fill Resin Composites with Different Adhesive Systems and Resin Composite Types. J. Adhes. Sci. Technol. 2019, 33, 1584–1597. [Google Scholar] [CrossRef]
- Salem, H.; Hefnawy, S.; Nagi, S. Degree of Conversion and Polymerization Shrinkage of Low Shrinkage Bulk-Fill Resin Composites. Contemp. Clin. Dent. 2019, 10, 465. [Google Scholar] [CrossRef] [PubMed]
- Najafi-Abrandabadi, A.; Najafi-Abrandabadi, S.; Ghasemi, A.; Kotick, P.G. Microshear Bond Strength of Composite Resins to Enamel and Porcelain Substrates Utilizing Unfilled versus Filled Resins. Dent. Res. J. 2014, 11, 636. [Google Scholar]
- Deb, S.; Di Silvio, L.; MacKler, H.E.; Millar, B.J. Pre-Warming of Dental Composites. Dent. Mater. 2011, 27, e51–e59. [Google Scholar] [CrossRef]
- Alonso, R.C.B.; Correr, G.M.; Borges, A.F.S.; Kantovitz, K.R.; Rontani, R.M.P. Minimally Invasive Dentistry: Bond Strength of Different Sealant and Filling Materials to Enamel. Oral Health Prev. Dent. 2005, 3, 87–95. [Google Scholar]
- Kuşgöz, A.; Tüzüner, T.; Ülker, M.; Kemer, B.; Saray, O. Conversion Degree, Microhardness, Microleakage and Fluoride Release of Different Fissure Sealants. J. Mech. Behav. Biomed. Mater. 2010, 3, 594–599. [Google Scholar] [CrossRef]
- Simsek Derelioglu, S.; Yilmaz, Y.; Celik, P.; Carikcioglu, B.; Keles, S. Bond Strength and Microleakage of Self-Adhesive and Conventional Fissure Sealants. Dent. Mater. J. 2014, 33, 530–538. [Google Scholar] [CrossRef][Green Version]
- VOCO. Grandio Seal Safety Data Sheet. Available online: https://www.voco.dental/us/portaldata/1/resources/products/safety-data-sheets/us/grandio-seal_sds_us.pdf (accessed on 8 August 2023).
- Bayrak, G.D.; Gurdogan-Guler, E.B.; Yildirim, Y.; Ozturk, D.; Selvi-Kuvvetli, S. Assessment of Shear Bond Strength and Microleakage of Fissure Sealant Following Enamel Deproteinization: An in Vitro Study. J. Clin. Exp. Dent. 2020, 12, e220. [Google Scholar] [CrossRef]
- VOCO. Fissurit FX Safety Data Sheet. Available online: https://www.voco.dental/au/portaldata/1/resources/products/safety-data-sheets/au/fissurit-fx_sds_au.pdf (accessed on 8 August 2023).
- Güngör, Ö.E.; Erdogan, Y.; Yalçin-Güngör, A.; Alkiş, H. Comparative Evaluation of Shear Bond Strength of Three Flowable Compomers on Enamel of Primary Teeth: An in-Vitro Study. J. Clin. Exp. Dent. 2016, 8, e322. [Google Scholar] [CrossRef]
- Garcia, I.M.; Leitune, V.C.B.; Rücker, V.B.; Nunes, J.; Visioli, F.; Collares, F.M. Physicochemical and Biological Evaluation of a Triazine-Methacrylate Monomer into a Dental Resin. J. Dent. 2021, 114, 103818. [Google Scholar] [CrossRef]
- Li, F.; Li, F.; Wu, D.; Ma, S.; Gao, J.; Li, Y.; Xiao, Y.; Chen, J. The Effect of an Antibacterial Monomer on the Antibacterial Activity and Mechanical Properties of a Pit-and-Fissure Sealant. J. Am. Dent. Assoc. 2011, 142, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Mori, D.I.; Powell, A.; Kehe, G.M.; Schurr, M.J.; Nair, D.P.; Puranik, C.P. Acrylated Hydroxyazobenzene Copolymers in Composite-Resin Matrix Inhibits Streptococcus mutans Biofilms In Vitro. Pediatr. Dent. 2021, 43, 484–491. [Google Scholar] [PubMed]
- Mori, D.I.; Schurr, M.J.; Nair, D.P. Selective Inhibition of Streptococci Biofilm Growth via a Hydroxylated Azobenzene Coating. Adv. Mater. Interfaces 2020, 7, 1902149. [Google Scholar] [CrossRef] [PubMed]
- Kantovitz, K.R.; Pascon, F.M.; Nociti, F.H.; Tabchoury, C.P.M.H.; Puppin-Rontani, R.M. Inhibition of Enamel Mineral Loss by Fissure Sealant: An in Situ Study. J. Dent. 2013, 41, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Mejàre, I. Indications for Fissure Sealants and Their Role in Children and Adolescents. Dent. Update 2011, 38, 699–703. [Google Scholar] [CrossRef]
- Lupi-Pégurier, L.; Bertrand, M.F.; Genovese, O.; Rocca, J.P.; Muller-Bolla, M. Microleakage of Resin-Based Sealants after Er:YAG Laser Conditioning. Lasers Med. Sci. 2007, 22, 183–188. [Google Scholar] [CrossRef]
- Summitt, J.B.; Robbins, J.W.; Hilton, T.J.; Schwartz, R.S. Fundamentals of Operative Dentistry: A Contemporary Approach; Quintessence Publishing Co., Inc.: Batavia, IL, USA, 2006; Volume 5, ISBN 9781119130536. [Google Scholar]
- Cardoso, M.V.; De Almeida Neves, A.; Mine, A.; Coutinho, E.; Van Landuyt, K.; De Munck, J.; Van Meerbeek, B. Current Aspects on Bonding Effectiveness and Stability in Adhesive Dentistry. Aust. Dent. J. 2011, 56, 31–44. [Google Scholar] [CrossRef]
- Ivoclar Vivadent. Helioseal F Instruction of Use. Available online: https://www.dentaltix.com/en/sites/default/files/helioseal_1.pdf (accessed on 8 August 2023).
- SDI. Conseal F Brochure. Available online: https://www.sdi.com.au/pdfs/brochures/au/conseal%20f_sdi_brochures_au.pdf (accessed on 8 August 2023).
- Bishayi, D.; Srinivasan, A.; Mahabala, K.Y.; Natarajan, S.; Rao, A.; Nayak, A.P. A Novel Application of a Bioactive Material as a Pit and Fissure Sealant: In Vitro Pilot Study Evaluating the Sealing Ability and Penetration. Eur. Arch. Paediatr. Dent. 2023, 24, 195–201. [Google Scholar] [CrossRef]
- Rahimian-Imam, S.; Ramazani, N.; Fayazi, M.R.; Ramazani, N. Marginal Microleakage of Conventional Fissure Sealants and Self-Adhering Flowable Composite as Fissure Sealant in Permanent Teeth. J. Dent. 2015, 12, 430. [Google Scholar]
- Unal, M.; Hubbezoglu, I.; Zan, R.; Kapdan, A.; Hurmuzlu, F. Effect of Acid Etching and Different Er:YAG Laser Procedures on Microleakage of Three Different Fissure Sealants in Primary Teeth after Aging. Dent. Mater. J. 2013, 32, 557–563. [Google Scholar] [CrossRef]
- Güçlü, Z.A.; Dönmez, N.; Tüzüner, T.; Odabaş, M.E.; Hurt, A.P.; Coleman, N.J. The Impact of Er:YAG Laser Enamel Conditioning on the Microleakage of a New Hydrophilic Sealant—UltraSeal XT® HydroTM. Lasers Med. Sci. 2016, 31, 705–711. [Google Scholar] [CrossRef]
- Karaman, E.; Yazici, A.R.; Baseren, M.; Gorucu, J. Comparison of Acid versus Laser Etching on the Clinical Performance of a Fissure Sealant: 24-Month Results. Oper. Dent. 2013, 38, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Güçlü, Z.A.; Hurt, A.P.; Dönmez, N.; Coleman, N.J. Effect of Er:YAG Laser Enamel Conditioning and Moisture on the Microleakage of a Hydrophilic Sealant. Odontology 2018, 106, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Ferrazzano, G.F.; Ingenito, A.; Alcidi, B.; Sangianantoni, G.; Schiavone, M.G.; Cantile, T. In Vitro Performance of Ultrasound Enamel Preparation Compared with Classical Bur Preparation on Pit and Fissure Sealing. Eur. J. Paediatr. Dent. 2017, 18, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Memarpour, M.; Shafiei, F. The Effect of Antibacterial Agents on Fissure Sealant Microleakage: A 6-Month in Vitro Study. Oral Health Prev. Dent. 2014, 12, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Mézquita-Rodrigo, I.; Scougall-Vilchis, R.J.; Moyaho-Bernal, M.A.; Rodríguez-Vilchis, L.E.; Rubio-Rosas, E.; Contreras-Bulnes, R. Using Self-Etch Adhesive Agents with Pit and Fissure Sealants. In Vitro Analysis of Shear Bond Strength, Adhesive Remnant Index and Enamel Etching Patterns. Eur. Arch. Paediatr. Dent. 2022, 23, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Rotta, M.; Bresciani, P.; Moura, S.K.; Grande, R.H.; Hilgert, L.A.; Baratieri, L.N.; Loguercio, A.D.; Reis, A. Effects of Phosphoric Acid Pretreatment and Substitution of Bonding Resin on Bonding Effectiveness of Self-Etching Systems to Enamel. J. Adhes. Dent. 2007, 9, 537–545. [Google Scholar] [CrossRef]
- Tsujimoto, A.; Barkmeier, W.; Takamizawa, T.; Latta, M.; Miyazaki, M. The Effect of Phosphoric Acid Pre-Etching Times on Bonding Performance and Surface Free Energy with Single-Step Self-Etch Adhesives. Oper. Dent. 2016, 41, 441–449. [Google Scholar] [CrossRef]
- Eltoukhy, R.I.; Elkaffas, A.A.; Ali, A.I.; Mahmoud, S.H. Indirect Resin Composite Inlays Cemented with a Self-Adhesive, Self-Etch or a Conventional Resin Cement Luting Agent: A 5 Years Prospective Clinical Evaluation. J. Dent. 2021, 112, 103740. [Google Scholar] [CrossRef]
- Yun, X.; Li, W.; Ling, C.; Fok, A. Effect of Artificial Aging on the Bond Durability of Fissure Sealants. J. Adhes. Dent. 2013, 15, 251–258. [Google Scholar] [CrossRef]
- McCafferty, J.; O’Connell, A.C. A Randomised Clinical Trial on the Use of Intermediate Bonding on the Retention of Fissure Sealants in Children. Int. J. Paediatr. Dent. 2016, 26, 110–115. [Google Scholar] [CrossRef]
- Sreedevi, A.; Brizuela, M.; Mohamed, S. Pit and Fissure Sealants. Available online: https://www.ncbi.nlm.nih.gov/books/NBK448116/ (accessed on 20 May 2023).
- Cooley, R.L.; McCourt, J.W.; Huddleston, A.M.; Casmedes, H.P. Evaluation of a Fluoride-Containing Sealant by SEM, Microleakage, and Fluoride Release. Pediatr. Dent. 1990, 12, 38–42. [Google Scholar] [PubMed]
- Lygidakis, N.A.; Oulis, K.I.; Christodoulidis, A. Evaluation of Fissure Sealants Retention Following Four Different Isolation and Surface Preparation Techniques: Four Years Clinical Trial. J. Clin. Pediatr. Dent. 1994, 19, 23–25. [Google Scholar] [PubMed]
- Zhang, Y.; Wang, Y.; Chen, Y.; Chen, Y.; Zhang, Q.; Zou, J. The Clinical Effects of Laser Preparation of Tooth Surfaces for Fissure Sealants Placement: A Systematic Review and Meta-Analysis. BMC Oral Health 2019, 19, 203. [Google Scholar] [CrossRef] [PubMed]
- Colombo, S.; Paglia, L. Dental Sealants. Part 1: Prevention First. Eur. J. Paediatr. Dent. 2018, 19, 80–82. [Google Scholar] [CrossRef]
- Olczak-Kowalczyk, D.; Szczepańska, J.; Kaczmarek, U. Współczesna Stomatologia Wieku Rozwojowego, 1st ed.; Med Tour Press: Otwock, Poland, 2017; ISBN 978-83-87717-26-1. [Google Scholar]
- Lubojanski, A.; Piesiak-Panczyszyn, D.; Zakrzewski, W.; Dobrzynski, W.; Szymonowicz, M.; Rybak, Z.; Mielan, B.; Wiglusz, R.J.; Watras, A.; Dobrzynski, M. The Safety of Fluoride Compounds and Their Effect on the Human Body—A Narrative Review. Materials 2023, 16, 1242. [Google Scholar] [CrossRef]
- Wright, J.T.; Tampi, M.P.; Graham, L.; Estrich, C.; Crall, J.J.; Fontana, M.; Gillette, E.J.; Nový, B.B.; Dhar, V.; Donly, K.; et al. Sealants for Preventing and Arresting Pit-and-Fissure Occlusal Caries in Primary and Permanent Molars: A Systematic Review of Randomized Controlled Trials—A Report of the American Dental Association and the American Academy of Pediatric Dentistry. Pediatr. Dent. 2016, 38, 282–294. [Google Scholar] [CrossRef]
- Liu, W.; Xiong, L.; Li, J.; Guo, C.; Fan, W.; Huang, S. The Anticaries Effects of Pit and Fissure Sealant in the First Permanent Molars of School-Age Children from Guangzhou: A Population-Based Cohort Study. BMC Oral Health 2019, 19, 156. [Google Scholar] [CrossRef]
- Fernández-Barrera, M.Á.; De Jesús Saucedo-Molina, T.; Scougall-Vilchis, R.J.; De Lourdes Márquez-Corona, M.; Medina-Solís, C.E.; Maupomé, G. Comparison of Two Types of Pit and Fissure Sealants in Reducing the Incidence of Dental Caries Using a Split-Mouth Design. Acta Stomatol. Croat. 2021, 55, 137–146. [Google Scholar] [CrossRef]
- Kosior, P.; Dobrzyński, M.; Korczyński, M.; Herman, K.; Czajczyńska-Waszkiewicz, A.; Kowalczyk-Zając, M.; Piesiak-Pańczyszyn, D.; Fita, K.; Janeczek, M. Long-Term Release of Fluoride from Fissure Sealants—In Vitro Study. J. Trace Elem. Med. Biol. 2017, 41, 107–110. [Google Scholar] [CrossRef]
- Horst, J.A.; Tanzer, J.M.; Milgrom, P.M. Fluorides and Other Preventive Strategies for Tooth Decay. Dent. Clin. N. Am. 2018, 62, 207–234. [Google Scholar] [CrossRef] [PubMed]
- Muller-Bolla, M.; Courson, F.; Lupi-Pégurier, L.; Tardieu, C.; Mohit, S.; Staccini, P.; Velly, A.M. Effectiveness of Resin-Based Sealants with and without Fluoride Placed in a High Caries Risk Population: Multicentric 2-Year Randomized Clinical Trial. Caries Res. 2018, 52, 312–322. [Google Scholar] [CrossRef] [PubMed]
- Chestnutt, I.G. Are Fluoride-Containing Sealants More Effective than Non-Fluoride Sealants? Evid. Based Dent. 2019, 20, 12–13. [Google Scholar] [CrossRef]
- Zawaideh, F.I.; Owais, A.I.; Kawaja, W. Ability of Pit and Fissure Sealant-Containing Amorphous Calcium Phosphate to Inhibit Enamel Demineralization. Int. J. Clin. Pediatr. Dent. 2016, 9, 10–14. [Google Scholar] [CrossRef]
- Silva, K.G.; Pedrini, D.; Delbem, A.C.B.; Ferreira, L.; Cannon, M. In Situ Evaluation of the Remineralizing Capacity of Pit and Fissure Sealants Containing Amorphous Calcium Phosphate and/or Fluoride. Acta Odontol. Scand. 2010, 68, 11–18. [Google Scholar] [CrossRef]
- Borges, B.C.D.; Catelan, A.; Sasaki, R.T.; Ambrosano, G.M.B.; Reis, A.F.; Aguiar, F.H.B. Effect of the Application of a Casein Phosphopeptide-Amorphous Calcium Phosphate (CPP-ACP) Paste and Adhesive Systems on Bond Durability of a Fissure Sealant. Odontology 2013, 101, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Memarpour, M.; Baghdadabadi, N.A.; Rafiee, A.; Vossoughi, M. Ion Release and Recharge from a Fissure Sealant Containing Amorphous Calcium Phosphate. PLoS ONE 2020, 15, e0241272. [Google Scholar] [CrossRef]
- Ogawa, Y.; Sayed, M.; Hiraishi, N.; Al-Haj Husain, N.; Tagami, J.; Özcan, M.; Shimada, Y. Effect of Surface Pre-Reacted Glass Ionomer Containing Dental Sealant on the Inhibition of Enamel Demineralization. J. Funct. Biomater. 2022, 13, 189. [Google Scholar] [CrossRef]
- Rashed, T.; Alkhalefa, N.; Adam, A.; Alkheraif, A. Pit and Fissure Sealant versus Fluoride Varnish for the Prevention of Dental Caries in School Children: A Systematic Review and Meta-Analysis. Int. J. Clin. Pract. 2022, 2022, 8635254. [Google Scholar] [CrossRef]
- Ahovuo-Saloranta, A.; Forss, H.; Hiiri, A.; Nordblad, A.; Mäkelä, M. Pit and Fissure Sealants versus Fluoride Varnishes for Preventing Dental Decay in the Permanent Teeth of Children and Adolescents (Review). Cochrane Database Syst. Rev. 2020, 2020, CD003067. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piszko, A.; Piszko, P.J.; Lubojański, A.; Grzebieluch, W.; Szymonowicz, M.; Dobrzyński, M. Brief Narrative Review on Commercial Dental Sealants—Comparison with Respect to Their Composition and Potential Modifications. Materials 2023, 16, 6453. https://doi.org/10.3390/ma16196453
Piszko A, Piszko PJ, Lubojański A, Grzebieluch W, Szymonowicz M, Dobrzyński M. Brief Narrative Review on Commercial Dental Sealants—Comparison with Respect to Their Composition and Potential Modifications. Materials. 2023; 16(19):6453. https://doi.org/10.3390/ma16196453
Chicago/Turabian StylePiszko, Aleksandra, Paweł J. Piszko, Adam Lubojański, Wojciech Grzebieluch, Maria Szymonowicz, and Maciej Dobrzyński. 2023. "Brief Narrative Review on Commercial Dental Sealants—Comparison with Respect to Their Composition and Potential Modifications" Materials 16, no. 19: 6453. https://doi.org/10.3390/ma16196453
APA StylePiszko, A., Piszko, P. J., Lubojański, A., Grzebieluch, W., Szymonowicz, M., & Dobrzyński, M. (2023). Brief Narrative Review on Commercial Dental Sealants—Comparison with Respect to Their Composition and Potential Modifications. Materials, 16(19), 6453. https://doi.org/10.3390/ma16196453








