Biomechanical Analysis of Palateless Splinted and Unsplinted Maxillary Implant-Supported Overdentures: A Three-Dimensional Finite Element Analysis
Abstract
1. Introduction
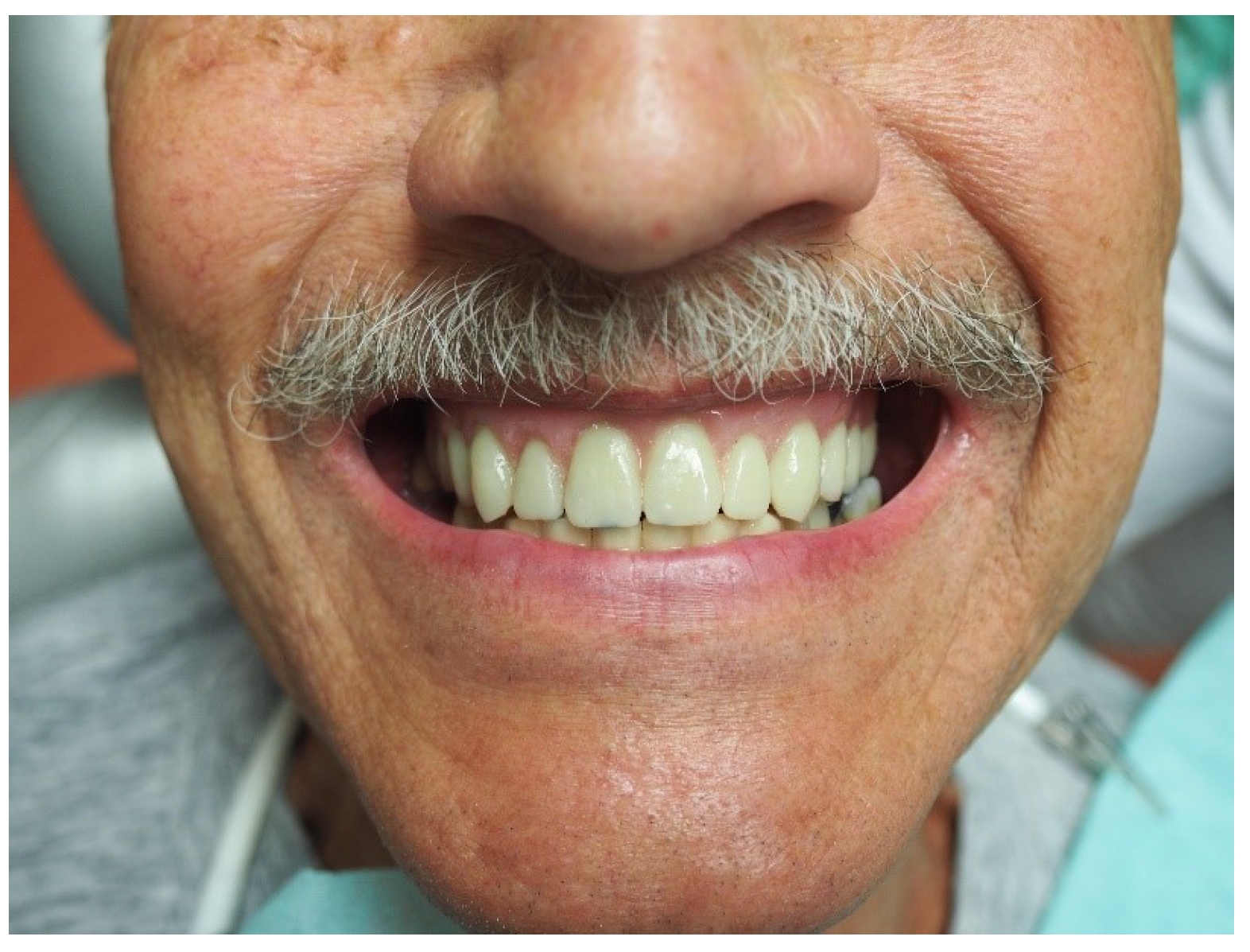
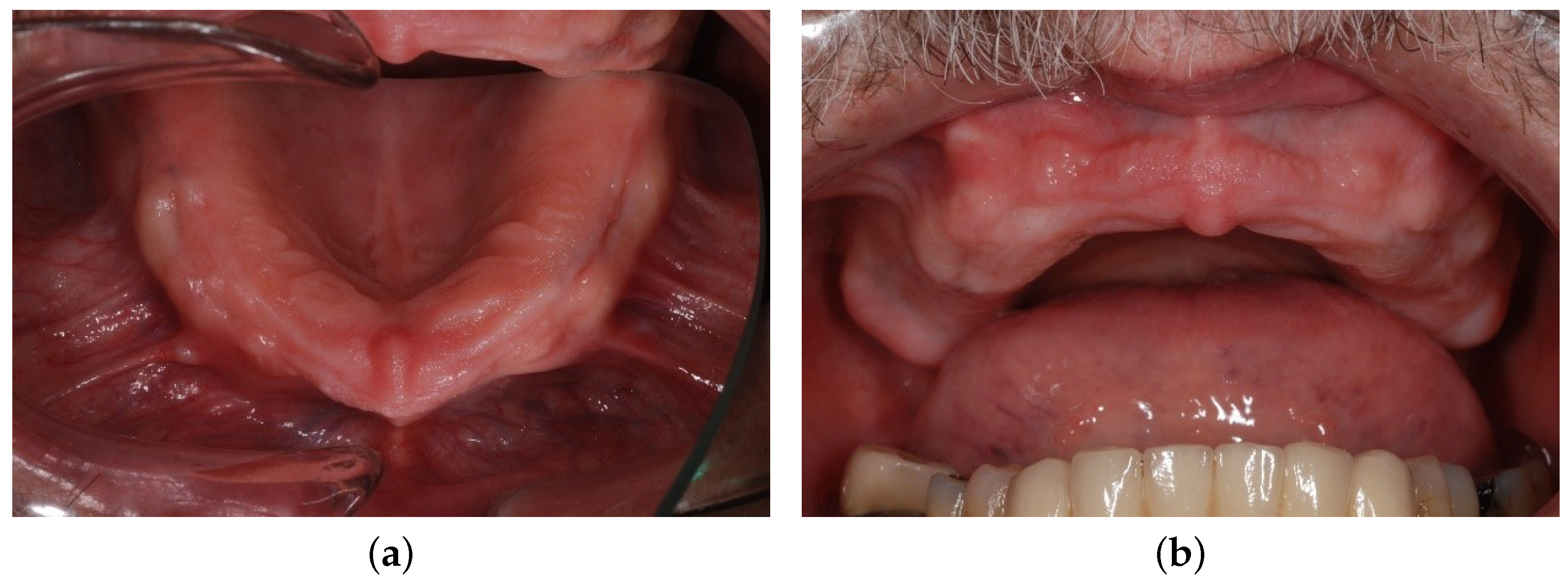
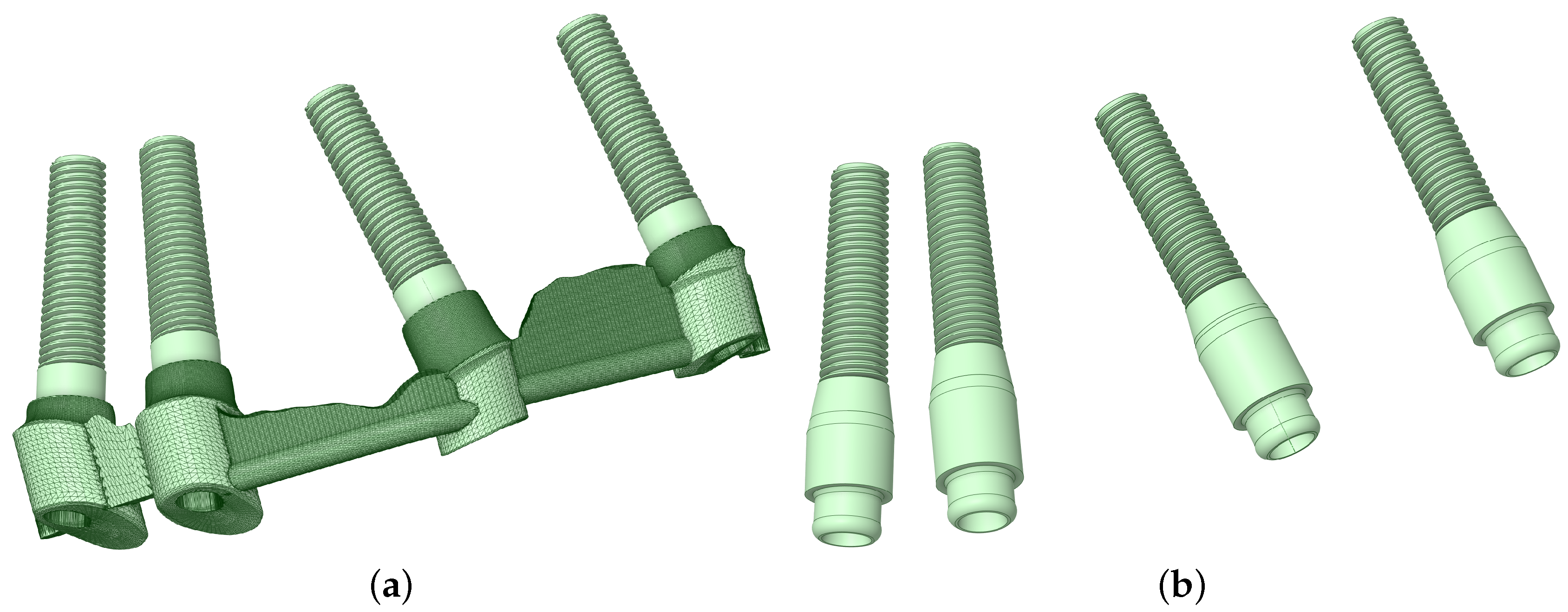
2. Materials and Methods
2.1. Methodology
2.2. Mesh, Loads, and Boundary Conditions
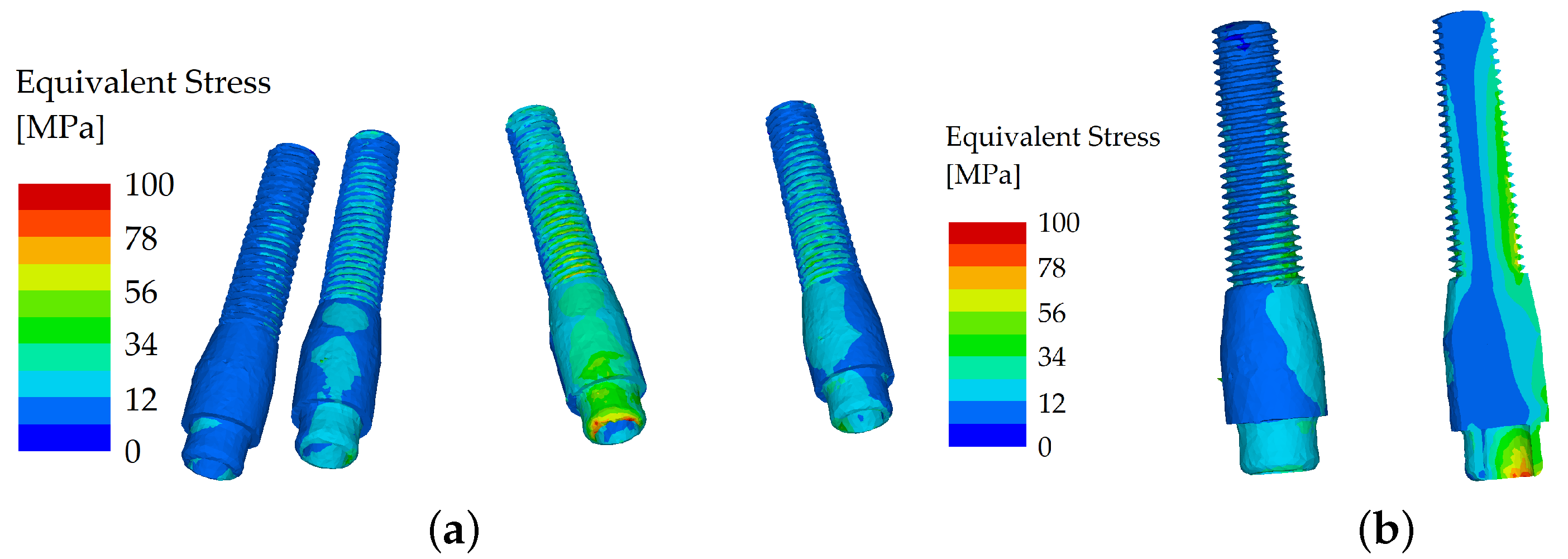
3. Results
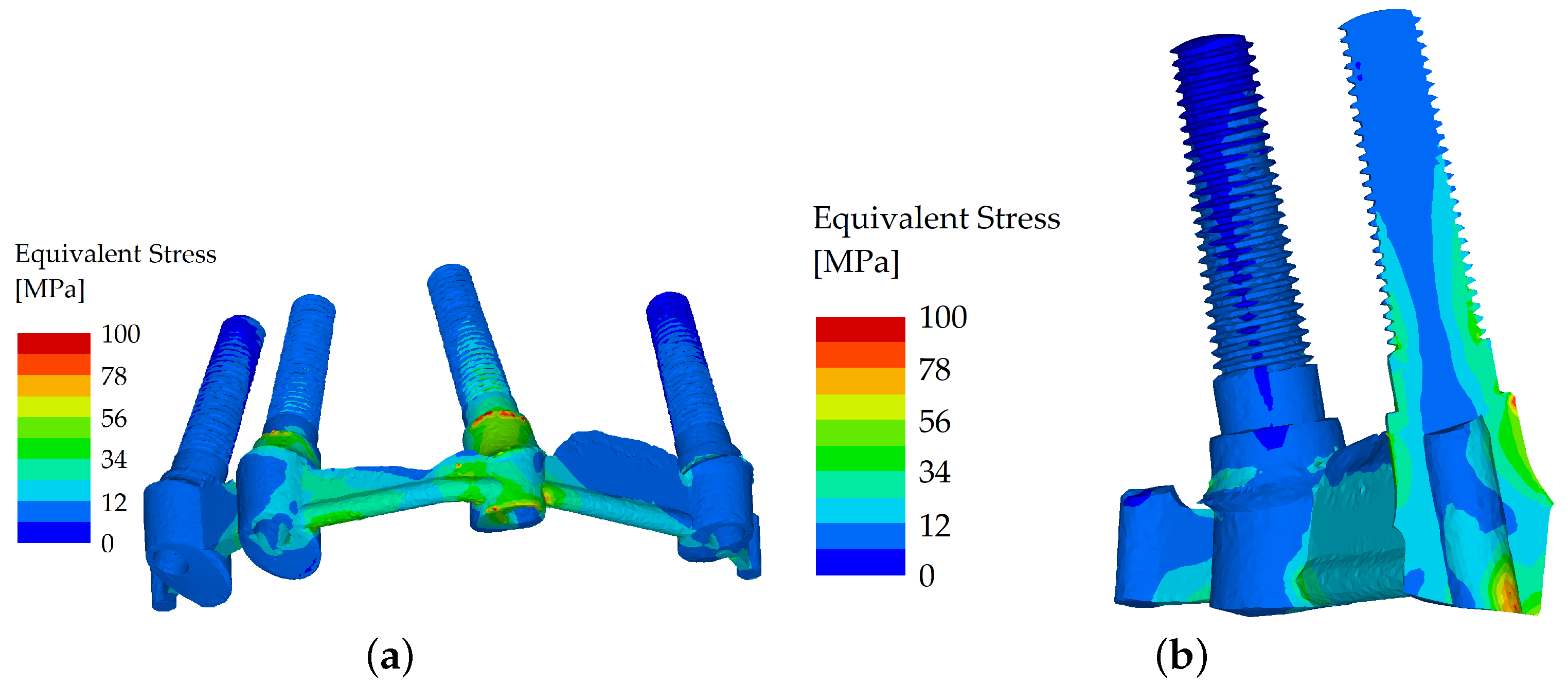
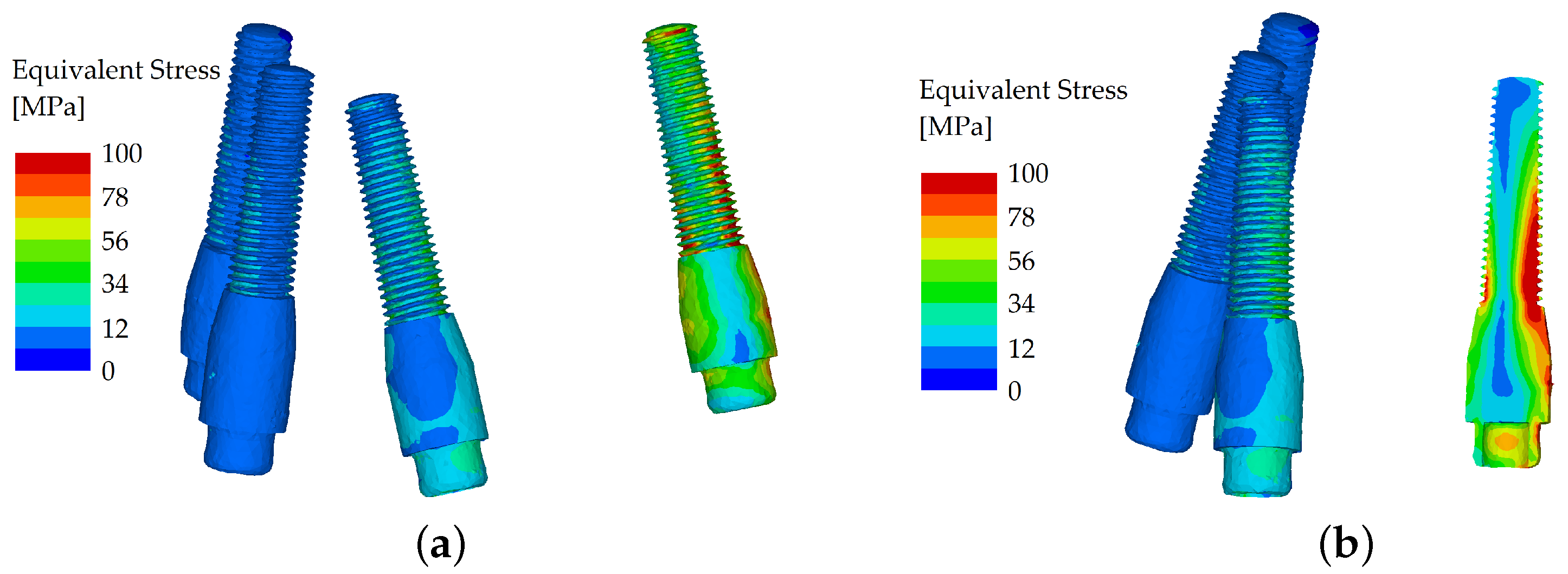
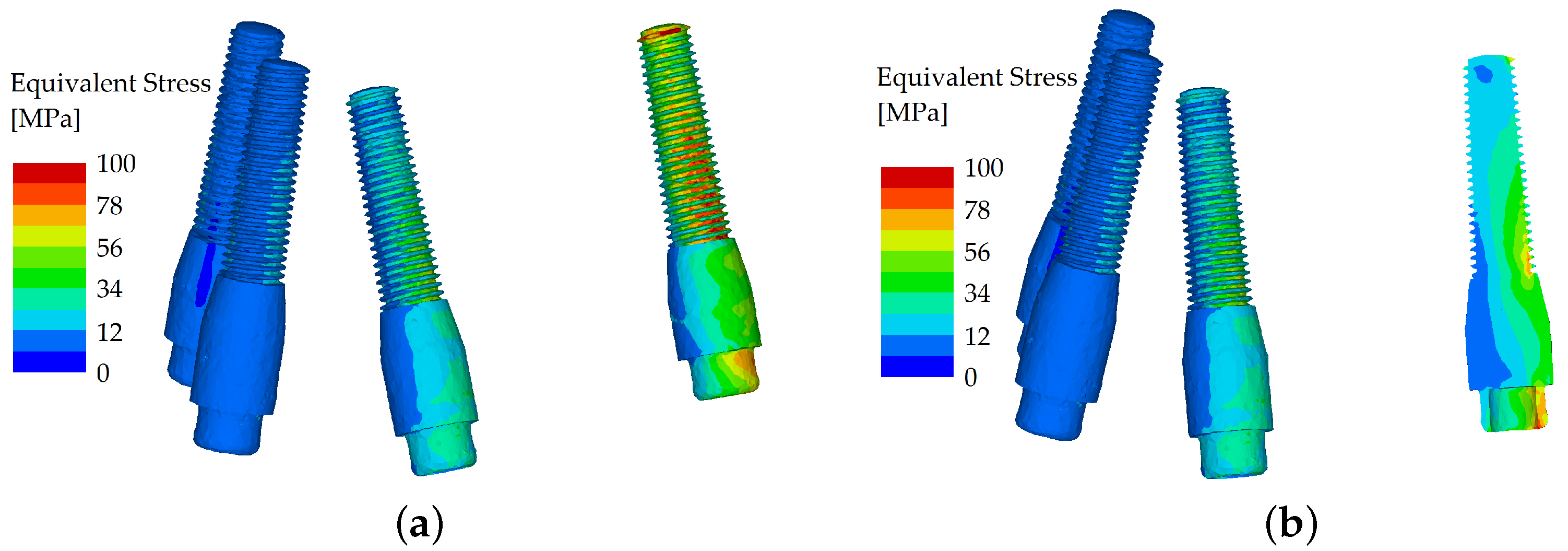
3.1. Comparison of Stress Distribution between Splinted and Unsplinted Models in Implants
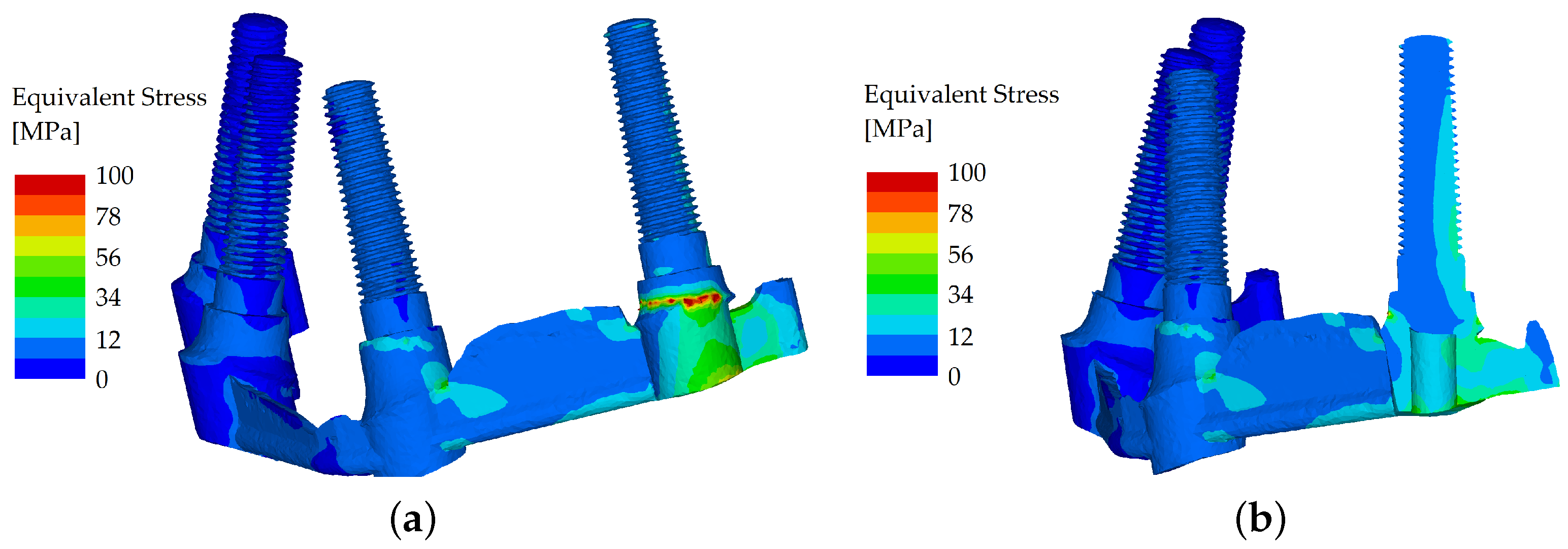
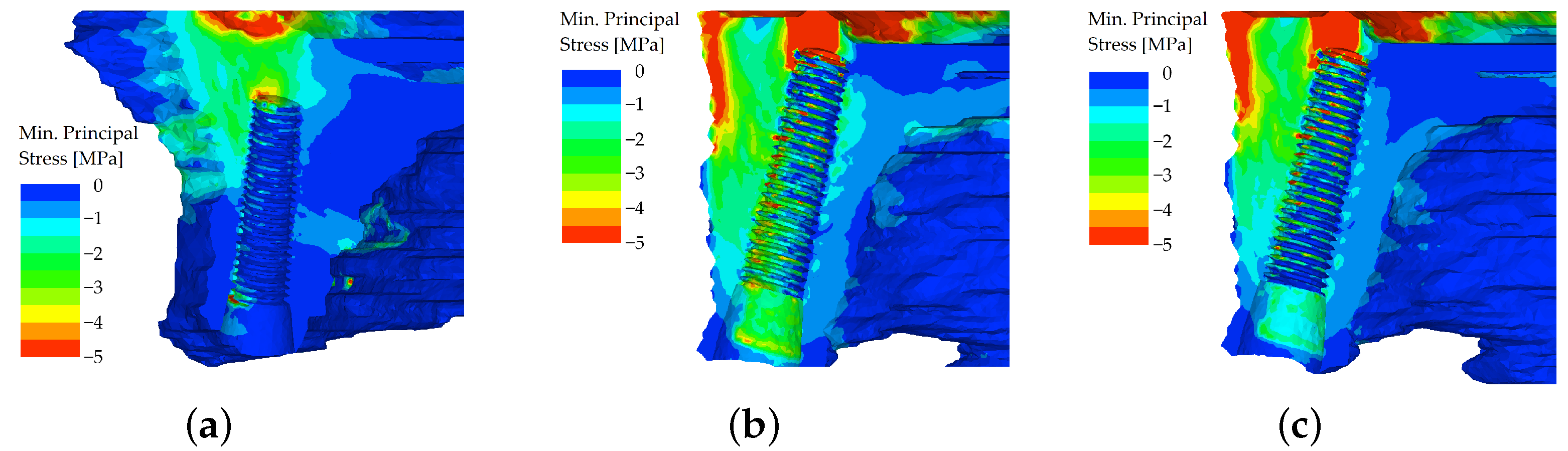
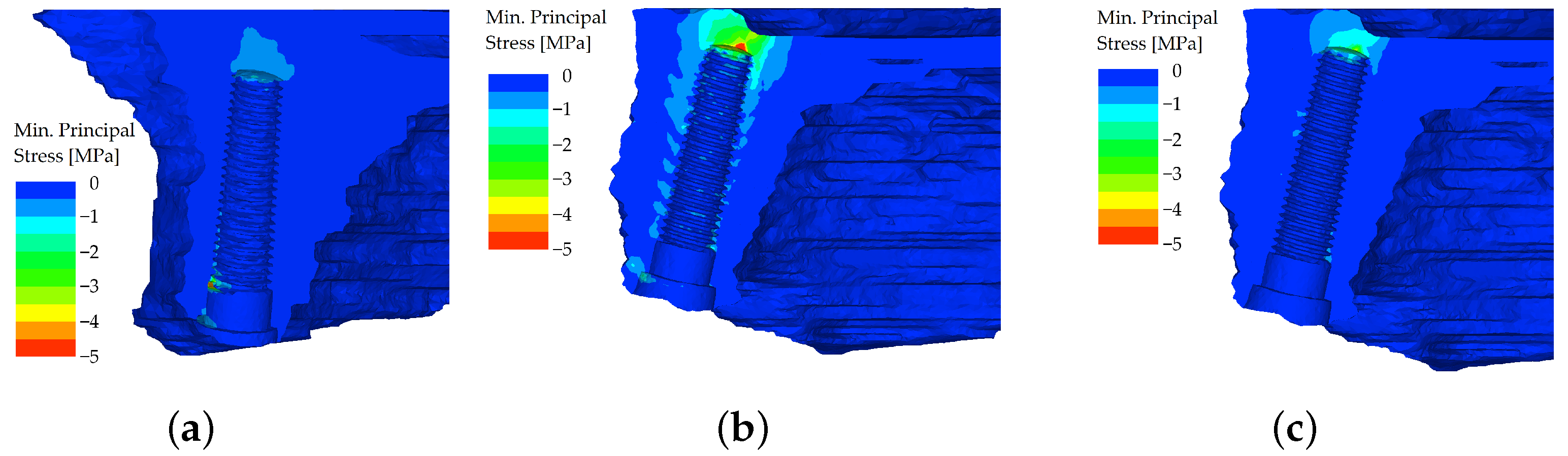
3.2. Comparison of Stress Distribution between Splinted and Unsplinted Models in the Maxilla
4. Discussion
- When analyzing stress distribution in the implants with a frontal load (force applied to both incisors), the stress distribution in analyzed implants was similar, and the equivalent stress did not show many differences between the two variants.
- When analyzing the stress distribution in the implants with a distal load (force applied to the first premolar), the differences in stress distribution between the unsplinted and splinted variant were not remarkable. The load was transferred right into the body of the implant positioned directly under the first premolar.
- When analyzing stress distribution in the implants with a distal load (force applied to both molars), the splinted variant transferred the loads with less flexion, whereas in the unsplinted variant, most of the load was localized to the outermost implant.
- When analyzing the stress distribution in the maxilla, localized peaks of compressive stress were created in the unsplinted variant. This effect was more pronounced in the distal region, where loading was applied to the premolar and molars of the denture.
- When analyzing the stress distribution in the maxilla in the splinted variant, the bar prevented excessive implant displacement. The compressive stresses are noticeably smaller in all regions where the load was applied.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thalji, G.; Bryington, M.; De Kok, I.J.; Cooper, L.F. Prosthodontic management of implant therapy. Dent. Clin. N. Am. 2014, 58, 207–225. [Google Scholar] [CrossRef]
- Sadowsky, S.J. Treatment considerations for maxillary implant overdentures: A systematic review. J. Prosthet. Dent. 2007, 97, 340–348. [Google Scholar] [CrossRef]
- Mericske-Stern, R.D.; Taylor, T.D.; Belser, U. Management of the edentulous patient. Clin. Oral. Implants Res. 2000, 11, 108–125. [Google Scholar] [CrossRef] [PubMed]
- Aldhohrah, T.; Mashrah, M.A.; Wang, Y. Effect of 2-implant mandibular overdenture with different attachments and loading protocols on peri-implant health and prosthetic complications: A systematic review and network meta-analysis. J. Prosthet. Dent. 2022, 127, 832–844. [Google Scholar] [CrossRef]
- Ceraulo, S.; Leonida, A.; Lauritano, D.; Baldoni, A.; Longoni, S.; Baldoni, M.; Caccianiga, G. Proposal for a clinical approach to geriatric patients with anchor need on implant for removable denture: New technique. Prosthesis 2020, 2, 185–195. [Google Scholar] [CrossRef]
- Amornvit, P.; Rokaya, D.; Bajracharya, S.; Keawcharoen, K.; Supavanich, W. Management of obstructive sleep apnea with implant retained mandibular advancement device. World J. Dent. 2014, 5, 184–189. [Google Scholar] [CrossRef]
- Al Amri, M.D. Crestal bone loss around submerged and nonsubmerged dental implants: A systematic review. J. Prosthet. Dent. 2016, 115, 564–570. [Google Scholar] [CrossRef]
- Trakas, T.; Michalakis, K.; Kang, K.; Hirayama, H. Attachment systems for implant retained overdentures: A literature review. Implant Dent. 2006, 15, 24–34. [Google Scholar] [CrossRef]
- Heckmann, S.M.; Winter, W.; Meyer, M.; Weber, H.P. Overdenture attachment selection and the loading of implant and denture-bearing area. Part 2: A methodical study using five types of attachment. Clin. Oral Implants Res. 2001, 12, 640–647. [Google Scholar] [CrossRef] [PubMed]
- Elsyad, M.A.; Alokda, M.M.; Gebreel, A.A.; Hammouda, N.I.; Habib, A.A. Effect of two designs of implant-supported overdentures on peri-implant and posterior mandibular bone resorptions: A 5-year prospective radiographic study. Clin. Oral Implants Res. 2017, 28, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Lage-Azorín, J.F.; Segura-Andrés, G.; Faus-López, J.; Agustín-Panadero, R. Rehabilitation with implant-supported overdentures in total edentulous patients: A review. J. Clin. Exp. Dent. 2013, 5, 267–272. [Google Scholar] [CrossRef]
- Barão, V.A.; Assunção, W.G.; Tabata, L.F.; de Sousa, E.A.C.; Rocha, E.P. Effect of different mucosa thickness and resiliency on stress distribution of implant-retained overdentures-2D FEA. Comput. Methods Programs Biomed. 2008, 92, 213–223. [Google Scholar] [CrossRef]
- Roccuzzo, M.; Bonino, F.; Gaudioso, L.; Zwahlen, M.; Meijer, H.J. What is the optimal number of implants for removable reconstructions? A systematic review on implant-supported overdentures. Clin. Oral Implants Res. 2012, 23, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Cavallaro, J.S., Jr.; Tarnow, D.P. Unsplinted implants retaining maxillary overdentures with partial palatal coverage: Report of 5 consecutive cases. Int. J. Oral Maxillofac. Implants 2007, 22, 808–814. [Google Scholar] [PubMed]
- Raghoebar, G.M.; Meijer, H.J.; Slot, W.; Slater, J.J.; Vissink, A. A systematic review of implant-supported overdentures in the edentulous maxilla, compared to the mandible: How many implants? Eur. J. Oral Implantol. 2014, 7, 191–201. [Google Scholar]
- Di Francesco, F.; De Marco, G.; Sommella, A.; Lanza, A. Splinting vs Not Splinting Four Implants Supporting a Maxillary Overdenture: A Systematic Review. Int. J. Prosthodont. 2019, 32, 509–518. [Google Scholar] [CrossRef]
- Jagota, V.; Sethi, A.P.S.; Kumar, K. Finite Element Method: An Overview. Walailak J. Sci. Tech. 2013, 10, 1–8. [Google Scholar]
- Geng, J.P.; Tan, K.B.; Liu, G.R. Application of finite element analysis in implant dentistry: A review of the literature. J. Prosthet. Dent. 2001, 85, 585–598. [Google Scholar] [CrossRef]
- Brunski, J.B. Biomechanical Aspects of the Optimal Number of Implants to Carry a Cross-Arch Full Restoration. Eur. J. Oral Implantol. 2014, 7, 111–131. [Google Scholar]
- Prado, M.; Khosla, S.; Chaput, C.; Giambini, H. Opportunistic application of phantom-less calibration methods for fracture risk prediction using QCT/FEA. Eur Radiol. 2021, 31, 9428–9435. [Google Scholar] [CrossRef]
- Mechanical Finder. Available online: https://mechanical-finder.com/ (accessed on 4 May 2023).
- Keyak, J.H.; Rossi, S.A.; Jones, K.A.; Skinner, H.B. Prediction of femoral fracture load using automated finite element modeling. J. Biomech. 1998, 31, 125–133. [Google Scholar] [CrossRef] [PubMed]
- CoprApeek. Available online: https://www.white-peaks-dental.com/en/produkt-details/coprapeek (accessed on 4 May 2023).
- Misch, C.E. Dental Implant Prosthetics, 2nd ed.; Mosby: St. Louis, MO, USA, 2014. [Google Scholar]
- Bergkvist, G.; Simonsson, K.; Rydberg, K.; Johansson, F.; Dérand, T. A finite element analysis of stress distribution in bone tissue surrounding uncoupled or splinted dental implants. Clin. Implant Dent. Relat. Res. 2008, 10, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.M.; Leu, L.J.; Wang, J.; Lin, L.D. Effects of prosthesis materials and prosthesis splinting on peri-implant bone stress around implants in poor-quality bone: A numeric analysis. Int. J. Oral Maxillofac. Implants 2002, 17, 231–237. [Google Scholar] [PubMed]
- Tabata, L.F.; Assunção, W.G.; Barão, V.A.; Gomes, E.A.; Delben, J.A.; de Sousa, E.A.C.; Rocha, E.P. Comparison of single-standing or connected implants on stress distribution in bone of mandibular overdentures: A two-dimensional finite element analysis. J. Craniofac. Surg. 2010, 21, 696–702. [Google Scholar] [CrossRef]
- Vafaei, F.; Khoshhal, M.; Bayat-Movahed, S.; Ahangary, A.H.; Firooz, F.; Izady, A.; Rakhshan, V. Comparative stress distribution of implant-retained mandibular ball-supported and bar-supported overlay dentures: A finite element analysis. J. Oral. Implantol. 2011, 37, 421–429. [Google Scholar] [CrossRef]
- Jofre, J.; Cendoya, P.; Munoz, P. Effect of splinting mini-implants on marginal bone loss: A biomechanical model and clinical randomized study with mandibular overdentures. Int. J. Oral Maxillofac Implants. 2010, 25, 1137–1144. [Google Scholar]
- Assunção, W.G.; Tabata, L.F.; Barão, V.A.; Rocha, E.P. Comparison of stress distribution between complete denture and implant-retained overdenture-2D FEA. J. Oral Rehabil. 2008, 35, 766–774. [Google Scholar] [CrossRef]
- Barão, V.A.R.; Assunção, W.G.; Tabata, L.F.; Delben, J.A.; Gomes, É.A.; de Sousa, E.A.C.; Rocha, E.P. Finite element analysis to compare complete denture and implant-retained overdentures with different attachment systems. J. Craniofac. Surg. 2009, 20, 1066–1071. [Google Scholar] [CrossRef]
- Menicucci, G.; Lorenzetti, M.; Pera, P.; Preti, G. Mandibular implant-retained overdenture: Finite element analysis of two anchorage systems. Int. J. Oral Maxillofac. Implants 1998, 13, 369–376. [Google Scholar]
- Geramy, A.; Habibzadeh, S. Stress Distribution in Splinted and Unsplinted Implant-Supported Maxillary Overdentures: A 3D Finite Element Analysis. Implant Dent. 2018, 27, 56–62. [Google Scholar] [CrossRef]
- Aquib, J.; Tarun, K.; Manjit, K.; Ajay, B.; Udey, S.W. A Finite Element Analysis on Stress Distribution in Overdenture Implants and Implant Abutment Interface Using Different Attachment Systems: An In Vitro Study. Dent. J. Adv. Stud. 2020, 8, 22–31. [Google Scholar]
- Kim, M.J.; Hong, S.O. Finite element analysis on stress distribution of maxillary implant-retained overdentures depending on the Bar attachment design and palatal coverage. J. Adv. Prosthodont. 2016, 8, 85–93. [Google Scholar] [CrossRef]
- Fernandez, M.A.; Subramanian, N.; Nawrocki, M.; Nawrocki, A.; Craighead, J.; Clark, A.; O’Neill, E.; Esquivel-Upshaw, J. Finite element analysis (FEA) of palatal coverage on implant retained maxillary overdentures. Appl. Sci. 2020, 10, 6635. [Google Scholar] [CrossRef]
- Slot, W.; Raghoebar, G.M.; Vissink, A.; Huddleston Slater, J.J.; Meijer, H.J. A systematic review of implant-supporteded maxillary overdentures after a mean observation period of at least 1 year. J. Clin. Periodontol. 2010, 37, 98–110. [Google Scholar] [CrossRef] [PubMed]
- Leão, R.S.; Moraes, S.L.D.; Vasconcelos, B.C.E.; Lemos, C.A.A.; Pellizzer, E.P. Splinted and unsplinted overdenture attachment systems: A systematic review and meta-analysis. J. Oral Rehabil. 2018, 45, 647–656. [Google Scholar] [CrossRef]
- Ahmed, K. Splinted versus unsplinted overdenture attachment systems—No difference in clinical outcomes. Evid. Based Dent. 2019, 20, 28–29. [Google Scholar] [CrossRef] [PubMed]
- Stoumpis, C.; Kohal, R.J. To splint or not to splint oral implants in the implant-supported overdenture therapy? A systematic literature review. J. Oral Rehabil. 2011, 38, 857–869. [Google Scholar] [CrossRef] [PubMed]
- Chaware, S.H.; Thakkar, S.T. A systematic review and meta-analysis of the attachments used in implant-supported overdentures. J. Indian Prosthodont. Soc. 2020, 20, 255–268. [Google Scholar] [CrossRef] [PubMed]



| Material | Young Modulus [MPa] | Poisson’s Ratio | References |
|---|---|---|---|
| Dental implants, locators, bar superstructure | 108,854 | 0.28 | [21] |
| Cortical and cancellous bone | QCT/FEA | 0.4 | [22] |
| Overdenture (PEEK) | 3727 | 0.4 | [23] |
| Splinted Model | Unsplinted Model | |
|---|---|---|
| No. of Nodes | 897,377 | 739,654 |
| No. of Shells | 358,648 | 290,490 |
| No. of Solids | 4,923,388 | 4,038,705 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frolo, M.; Řehounek, L.; Jíra, A.; Pošta, P.; Hauer, L. Biomechanical Analysis of Palateless Splinted and Unsplinted Maxillary Implant-Supported Overdentures: A Three-Dimensional Finite Element Analysis. Materials 2023, 16, 5248. https://doi.org/10.3390/ma16155248
Frolo M, Řehounek L, Jíra A, Pošta P, Hauer L. Biomechanical Analysis of Palateless Splinted and Unsplinted Maxillary Implant-Supported Overdentures: A Three-Dimensional Finite Element Analysis. Materials. 2023; 16(15):5248. https://doi.org/10.3390/ma16155248
Chicago/Turabian StyleFrolo, Mária, Luboš Řehounek, Aleš Jíra, Petr Pošta, and Lukáš Hauer. 2023. "Biomechanical Analysis of Palateless Splinted and Unsplinted Maxillary Implant-Supported Overdentures: A Three-Dimensional Finite Element Analysis" Materials 16, no. 15: 5248. https://doi.org/10.3390/ma16155248
APA StyleFrolo, M., Řehounek, L., Jíra, A., Pošta, P., & Hauer, L. (2023). Biomechanical Analysis of Palateless Splinted and Unsplinted Maxillary Implant-Supported Overdentures: A Three-Dimensional Finite Element Analysis. Materials, 16(15), 5248. https://doi.org/10.3390/ma16155248






