Stress Distribution on Various Implant-Retained Bar Overdentures
Abstract
1. Introduction
2. Materials and Methods
2.1. Preparation of the Solid Models
2.2. Loading Conditions
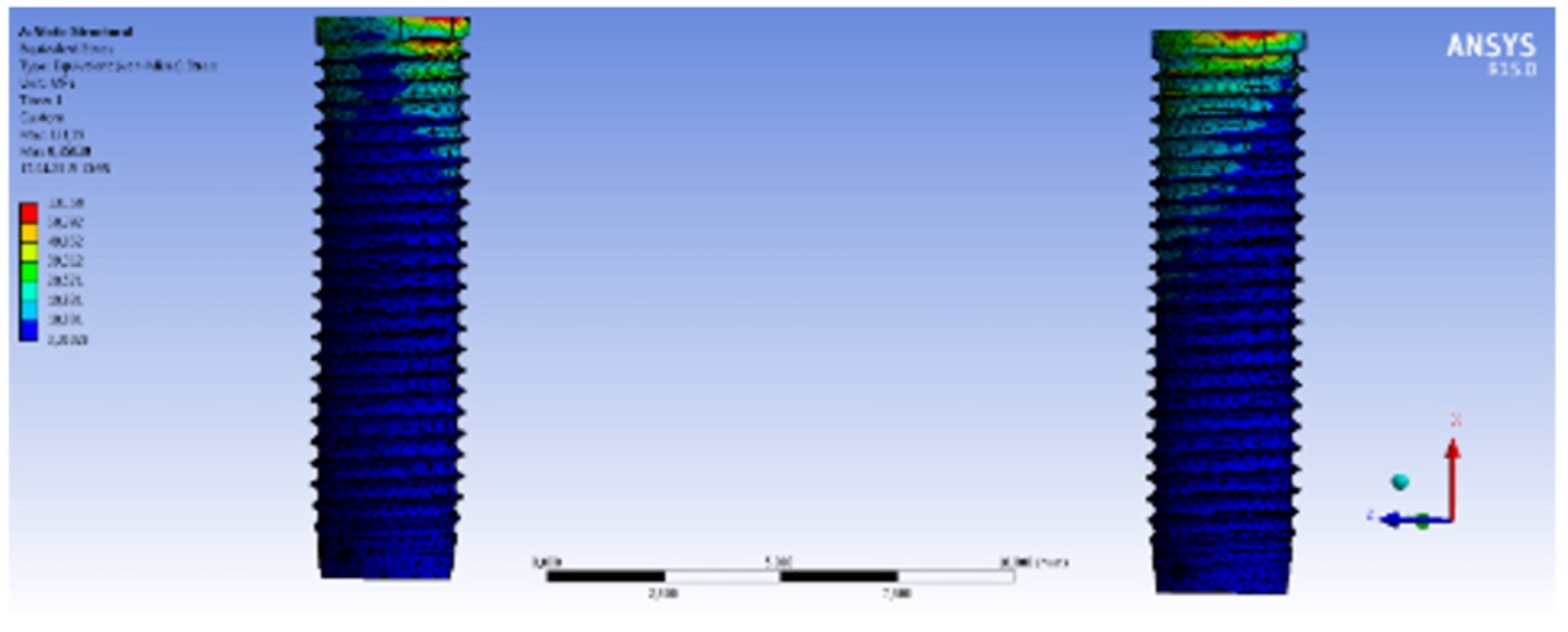
3. Results
3.1. Application of 100 N Static Load
3.2. Vertical Loading
3.3. Horizontal Loading
3.4. Oblique Loading
3.5. The Minimum and Maximum Principal Stress on the Cortical Bone
4. Discussion
5. Conclusions
- -
- The highest Von Mises stress on the implants and the bone tissue was observed in all models after 100 N of horizontal loading. The horizontal loading stress values were higher than the vertical and oblique loading stress values.
- -
- In all loading conditions, the highest Von Mises stress on the implants and the cortical bone was observed in Model 1, which was constructed with no multi-unit abutment. Using multi-unit abutments in bar-retentive overdenture systems provides stress absorption, and this results in low tensile stress values in the implants and the bone.
- -
- The elasticity modulus of the bar material did not have a significant effect on stress occurrence in implants and bone.
- -
- After the horizontal, vertical and oblique loading, the stress on the implants, and on the cortical and trabecular bone in the Co-Cr bar system with multi-unit abutments, was nearer to, or lower than, the values of the Ti Grade 5 (Ti-6Al-4V) bar system. This is connected to the use of the manufacturer’s original implant multi-unit abutments.
- -
- After the implementation of static load in three different directions, the maximum principal stress in the cortical bone was lower than the tensile and the compressive strength values of the bone. The stress occurrence on the trabecular bone was lower than the stress occurrence on the cortical bone.
6. Clinical Implication
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Misch, C.E. Dental Implant Prosthetics, 2nd ed.; Elsevier Mosby Inc.: St. Louis, MO, USA, 2005. [Google Scholar]
- Davis, D.M.; Zarb, G.A.; Chao, Y. Studies on frameworks for osseointegrated prostheses: Part I. The effect of varying the number of supporting abutments. Int. J. Oral. Maxillofac. Implant. 1988, 3, 197–201. [Google Scholar]
- Epstein, D.D.; Epstein, P.L.; Cohen, B.I.; Pagnillo, M.K. Comparison of the retentive properties of six prefabricated post overdenture attachment systems. J. Prosthet. Dent. 1999, 82, 579–584. [Google Scholar] [CrossRef]
- Heckmann, S.M.; Winter, W.; Meyer, M.; Weber, H.P.; Wichmann, M.G. Overdenture attachment selection and the loading of implant and denture-bearing area. Part I: In vivo verification of stereolithographic model. Clin. Oral. Implants. Res. 2001, 12, 617–623. [Google Scholar] [CrossRef]
- Feine, J.S.; Carlsson, G.E.; Awad, M.A.; Chehade, A.; Duncan, W.J.; Gizani, S.; Head, T.; Lund, J.P.; MacEntee, M.; Mericske-Stern, R.; et al. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Int. J. Oral. Maxillofac. Implant. 2002, 17, 601–602. [Google Scholar]
- Shafie, H. Principles of attachment selection. In Clinical and Laboratory Manual of Implant Overdentures, 1st ed.; Blackwell Publishing Inc.: Oxford, UK, 2007; pp. 31–36. [Google Scholar]
- Williams, B.H.; Ochiai, K.T.; Hojo, S.; Nishimura, R.; Caputo, A.A. Retention of maxillary implant overdenture bars of different designs. J. Prosthet. Dent. 2001, 86, 603–607. [Google Scholar] [CrossRef]
- Batenburg, R.; Meijer, H.; Raghoebar, G.; Vissink, A. Treatment concept for mandibular overdentures supported by endosseous implants: A literature review. Int. J. Oral. Maxillofac. Implant. 1998, 13, 539–545. [Google Scholar]
- Jemt, T.; Book, K.; Karlsson, S. Occlusal force and mandibular movements in patients with removable overdentures and fixed prostheses supported by implants in the maxilla. Int. J. Oral. Maxillofac. Implant. 1993, 8, 301–308. [Google Scholar]
- Davodi, A.; Nishimura, R.; Beumer, J. An implant-supported fixed-removable prosthesis with a milled tissue bar and Hader clip retention as a restorative option for the edentulous maxilla. J. Prosthet. Dent. 1997, 78, 212–217. [Google Scholar] [CrossRef]
- Phillips, K.; Wong, K.M. Space requirements for implant-retained bar-and-clip overdentures. Compend. Contin. Educ. Dent. 2001, 22, 516–522. [Google Scholar]
- Zitzmann, N.; Marinello, C. Implant-supported removable overdentures in the edentulous maxilla: Clinical and technical aspects. Int. J. Prosthodont. 1999, 12, 385–390. [Google Scholar]
- Abreu, R.T.; Spazzin, A.O.; Noritomi, P.Y.; Consani, R.L.X.; Mesquita, M.F. Influence of material of overdenture-retaining bar with vertical misfit on three-dimensional stress distribution. J. Prosthodont. 2010, 19, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Mochalski, J.; Fröhls, C.; Keilig, L.; Bourauel, C.; Dörsam, I. Experimental and numerical investigations of fracture and fatigue behaviour of implant-supported bars with distal extension made of three different materials. Biomed. Eng. Biomed. Tech. 2020, 66, 305–316. [Google Scholar] [CrossRef]
- Jaros, O.L.; De Carvalho, G.P.; Franco, A.G.; Kreve, S.; Lopes, P.B.; Dias, S. Biomechanical behavior of an implant system using polyether ether ketone bar: Finite element analysis. J. Int. Soc. Prev. Community Dent. 2018, 8, 446–450. [Google Scholar] [PubMed]
- Zaparolli, D.; Peixoto, R.F.; Pupim, D.; Macedo, A.P.; Toniollo, M.B.; Mattos, M.; de Mattos, M.D.G.C. Photoelastic analysis of mandibular full-arch implant-supported fixed dentures made with different bar materials and manufacturing techniques. Mater. Sci. Eng. C 2017, 81, 144–147. [Google Scholar] [CrossRef] [PubMed]
- Carr, A. A comparison of impression techniques for a five-implant mandibular model. Int. J. Oral. Maxillofac. Implant. 1991, 6, 448–455. [Google Scholar] [CrossRef]
- Carr, A.B.; Stewart, R.B. Full-Arch Implant Framework Casting Accuracy: Preliminary In Vitro Observation for In Vivo Testing. J. Prosthodont. 1993, 2, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Linke, B.A.; Nicholls, J.I.; Faucher, R.R. Distortion analysis of stone casts made from impression materials. J. Prosthet. Dent. 1985, 54, 794–802. [Google Scholar] [CrossRef]
- Inturregui, J.A.; Aquilino, S.A.; Ryther, J.S.; Lund, P.S. Evaluation of three impression techniques for osseointegrated oral implants. J. Prosthet. Dent. 1993, 69, 503–509. [Google Scholar] [CrossRef]
- Assif, D.; Marshak, B.; Schmidt, A. Accuracy of implant impression techniques. Int. J. Oral. Maxillofac. Implant. 1996, 11, 216–222. [Google Scholar] [CrossRef]
- Humphries, R.M.; Yaman, P.; Bloem, T.J. The accuracy of implant master casts constructed from transfer impressions. Int. J. Oral. Maxillofac. Implant. 1990, 5, 331–336. [Google Scholar]
- Strong, S. Improved Fit with a CAD/CAM Titanium Bar Overdenture An efficient, cost-effective approach for long-term success. Insid. Dent. 2013, 9, 46–54. [Google Scholar]
- Goo, C.L.; Tan, K.B.C. Fabricating CAD/CAM Implant-Retained Mandibular Bar Overdentures: A Clinical and Technical Overview. Case. Rep. Dent. 2017, 2017, 9373818. [Google Scholar] [CrossRef]
- Janev, E.; Redzep, E.; Janeva, N.; Mindova, S. Multi Unit Abutments Recommended in Prosthetic and Surgical Implantology Treatment (Case Report). J. Morphol. Sci. 2020, 3, 65–72. [Google Scholar]
- Van Kampen, F.; Cune, M.; Van Der Bilt, A.; Bosman, F. Retention and postinsertion maintenance of bar-clip, ball and magnet attachments in mandibular implant overdenture treatment: An in vivo comparison after 3 months of function. Clin. Oral. Implants. Res. 2003, 14, 720–726. [Google Scholar] [CrossRef]
- Rho, J.Y.; Ashman, R.B.; Turner, C.H. Young’s modulus of trabecular and cortical bone material: Ultrasonic and microtensile measurements. J. Biomech. 1993, 26, 111–119. [Google Scholar] [CrossRef]
- Kordatzis, K.; Wright, P.; Meijer, H. Posterior mandibular residual ridge resorption in patients with conventional dentures and implant overdentures. Int. J. Oral. Maxillofac. Implant. 2003, 18, 447–452. [Google Scholar]
- Schmitt, A.; Zarb, G.A. The notion of implant-supported overdentures. J. Prosthet. Dent. 1998, 79, 60–65. [Google Scholar] [CrossRef]
- Meijer, H.J.A.; Kuiper, J.H.; Starmans, F.J.M.; Bosman, F. Stress distribution around dental implants: Influence of superstructure, length of implants, and height of mandible. J. Prosthet. Dent. 1992, 68, 96–102. [Google Scholar] [CrossRef]
- Meijer, H.J.A.; Starmans, F.J.M.; Steen, W.H.A.; Bosman, F. A three-dimensional, finite-element analysis of bone around dental implants in an edentulous human mandible. Arch. Oral. Biol. 1993, 38, 491–496. [Google Scholar] [CrossRef]
- Kenney, R.; Richards, M.W. Photoelastic stress patterns produced by implant-retained overdentures. J. Prosthet. Dent. 1998, 80, 559–564. [Google Scholar] [CrossRef]
- Chiapasco, M. Early and immediate restoration and loading of implants in completely edentulous patients. Int. J. Oral. Maxillofac. Implant. 2004, 19, 76–91. [Google Scholar]
- Satpathy, S.; Satish Babu, C.L.; Shetty, S.; Raj, B. Stress distribution patterns of implant supported overdentures-analog versus finite element analysis: A comparative in-vitro study. J. Indian. Prosthodont. Soc. 2015, 15, 250–256. [Google Scholar] [CrossRef]
- Memari, Y.; Fattahi, P.; Fattahi, A.; Eskandarion, S.; Rakhshan, V. Finite element analysis of stress distribution around short and long implants in mandibular overdenture treatment. Dent. Res. J. 2019, 17, 25–33. [Google Scholar]
- Joshi, S.; Kumar, S.; Jain, S.; Aggarwal, R.; Choudhary, S.; Reddy, N.K. 3D finite element analysis to assess the stress distribution pattern in mandibular implant-supported overdenture with different bar heights. J. Contemp. Dent. Pract. 2019, 20, 794–800. [Google Scholar] [CrossRef]
- Geramy, A.; Habibzadeh, S. Stress distribution in splinted and unsplinted implant-supported maxillary overdentures: A 3D finite element analysis. Implant. Dent. 2018, 27, 56–61. [Google Scholar] [CrossRef]
- Ebadian, B.; Farzin, M.; Talebi, S.; Khodaeian, N. Evaluation of stress distribution of implant-retained mandibular overdenture with different vertical restorative spaces: A finite element analysis. Dent. Res. J. 2012, 9, 741–747. [Google Scholar]
- Misch, C.E. Contemporary Implant Dentistry, 2nd ed.; Mosby Inc.: Philadelphia, PA, USA, 1999. [Google Scholar]
- Satheesh Kumar, P.; Satheesh, K.K.S.; John, J.; Patil, G.; Patel, R. Force Transfer and Stress Distribution in an Implant-Supported Overdenture Retained with a Hader Bar Attachment: A Finite Element Analysis. ISRN Dent. 2013, 2013, 369147. [Google Scholar] [CrossRef]
- Menicucci, G.; Lorenzetti, M.; Pera, P.; Preti, G. Mandibular implant-retained overdenture: Finite element analysis of two anchorage systems. Int. J. Oral. Maxillofac. Implant. 1998, 13, 369–376. [Google Scholar]
- Daas, M.; Dubois, G.; Bonnet, A.S.; Lipinski, P.; Rignon-Bret, C. A complete finite element model of a mandibular implant-retained overdenture with two implants: Comparison between rigid and resilient attachment configurations. Med. Eng. Phys. 2008, 30, 218–225. [Google Scholar] [CrossRef]
- Spazzin, A.O.; Abreu, R.T.; Noritomi, P.Y.; Consani, R.L.X.; Mesquita, M.F. Evaluation of Stress Distribution in Overdenture-Retaining Bar with Different Levels of Vertical Misfit. J. Prosthodont. 2011, 20, 280–285. [Google Scholar] [CrossRef]
- Spazzin, A.O.; dos Santos, M.B.F.; Sobrinho, L.C.; Consani, R.L.X.; Mesquita, M.F. Effects of horizontal misfit and bar framework material on the stress distribution of an overdenture-retaining bar system: A 3D finite element analysis. J. Prosthodont. 2011, 20, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Sertgöz, A.; Güvener, S. Finite element analysis of the effect of cantilever and implant length on stress distribution in an implant-supported fixed prosthesis. J. Prosthet. Dent. 1996, 76, 165–169. [Google Scholar] [CrossRef]
- Barão, V.A.R.; Delben, J.A.; Lima, J.; Cabral, T.; Assunção, W.G. Comparison of different designs of implant-retained overdentures and fixed full-arch implant-supported prosthesis on stress distribution in edentulous mandible—A computed tomography-based three-dimensional finite element analysis. J. Biomech. 2013, 46, 1312–1320. [Google Scholar] [CrossRef]
- Product Catalogue. 2012. Available online: www.straumann.us (accessed on 2 March 2022).
- Mericske-Stern, R.; Hofmann, J.; Wedig, A.; Geering, A.H. In vivo measurements of maximal occlusal force and minimal pressure threshold on overdentures supported by implants or natural roots: A comparative study, Part 1. Int. J. Oral. Maxillofac. Implant. 1993, 8, 641–649. [Google Scholar]
- Prakash, V.; D’Souza, M.; Adhikari, R. A comparison of stress distribution and flexion among various designs of bar attachments for implant overdentures: A three dimensional finite element analysis. Indian J. Dent. Res. 2009, 20, 31–36. [Google Scholar] [CrossRef]
- Göçer, B. Dişsel İmplant Sistemlerinin Gerilme Analizi; Dokuz Eylul University: Izmir, Turkey, 2010. [Google Scholar]
- Geng, J.P.A.; Tan, K.B.C.; Liu, G.R. Application of finite element analysis in implant dentistry: A review of the literature. J. Prosthet. Dent. 2001, 85, 585–598. [Google Scholar] [CrossRef] [PubMed]
- Sevimay, M.; Usumez, A.; Eskitascioglu, G. The influence of various occlusal materials on stresses transferred to implant-supported prostheses and supporting bone: A three-dimensional finite-element study. J. Biomed. Mater. Res. Part B Appl. Biomater. 2005, 73, 140–147. [Google Scholar] [CrossRef]
- van Staden, R.C.; Guan, H.; Loo, Y.C. Application of the finite element method in dental implant research. Comput. Methods. Biomech. Biomed. Engin. 2006, 9, 257–270. [Google Scholar] [CrossRef]
- Saito, M.; Kanazawa, M.; Takahashi, H.; Uo, M.; Minakuchi, S. Trend of change in retentive force for bar attachments with different materials. J. Prosthet. Dent. 2014, 112, 1545–1552. [Google Scholar] [CrossRef]
- Cheng, W.W.; Ju, C.P.; Chern Lin, J.H. Structure, castability and mechanical properties of commercially pure and alloyed titanium cast in graphite mould. J. Oral. Rehabil. 2007, 34, 528–540. [Google Scholar] [CrossRef]
- Anthony, A.; Echeverri, D.; Parra, M.; Castro, I.J.; Garzón, H.; Valencia, C.H.; Olave, G. Caracterización metalográfica de barras para sobredentaduras, elaboradas por sobrecolado de pilares para implantes dentales. Rev. Fac. Odontol. Univ. Antioq. 2013, 25, 26–43. [Google Scholar]
- de la Rosa Castolo, G.; Guevara Perez, S.V.; Arnoux, P.J.; Badih, L.; Bonnet, F.; Behr, M. Implant-supported overdentures with different clinical configurations: Mechanical resistance using a numerical approach. J. Prosthet. Dent. 2019, 121, e1–e546. [Google Scholar] [CrossRef] [PubMed]
- Caetano, C.R.; Mesquita, M.F.; Consani, R.L.X.; Correr-Sobrinho, L.; Dos Santos, M.B.F. Overdenture retaining bar stress distribution: A finite-element analysis. Acta. Odontol. Scand. 2015, 73, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Tabata, L.F.; Assunção, W.G.; Barão, V.A.R.; Alves Gomes, E.; Aparecida Delben, J.; Capello De Sousa, E.A.; Rocha, E.P. Comparison of single-standing or connected implants on stress distribution in bone of mandibular overdentures: A two-dimensional finite element analysis. J. Craniofac. Surg. 2010, 21, 696–702. [Google Scholar] [CrossRef]
- Zampelis, A.; Rangert, B.; Heijl, L. Tilting of splinted implants for improved prosthodontic support: A two-dimensional finite element analysis. J. Prosthet. Dent. 2007, 97, 35–43. [Google Scholar] [CrossRef]
- Menicucci, G.; Mossolov, A.; Mozzati, M.; Lorenzetti, M.; Preti, G. Tooth-implant connection: Some biomechanical aspects based on finite element analyses. Clin. Oral. Implants. Res. 2002, 13, 334–341. [Google Scholar] [CrossRef]
- Mericske-Stern, R. Treatment outcomes with implant-supported overdentures: Clinical considerations. J. Prosthet. Dent. 1998, 79, 66–73. [Google Scholar] [CrossRef]
- Wirz, J.; Jäger, K. Pin anchored implant supported hybrid prostheses. Quintessenz 1991, 42, 2007–2014. [Google Scholar]
- Andersson, M.; Carlsson, L.; Persson, M.; Bergman, B. Accuracy of machine milling and spark erosion with a CAD/CAM system. J. Prosthet. Dent. 1996, 76, 187–193. [Google Scholar] [CrossRef]
- Liu, J.; Watanabe, I.; Yoshida, K.; Atsuta, M. Joint strength of laser-welded titanium. Dent. Mater. 2002, 18, 143–148. [Google Scholar] [CrossRef]
- Örtorp, A.; Jemt, T.; Back, T.; Jalevik, T. Comparisons of precision of fit between cast and CNC-milled titanium implant frameworks for the edentulous mandible. Int. J. Prosthodont. 2003, 16, 194–200. [Google Scholar] [PubMed]
- Helldén, L.; Ericson, G.; Elliot, A.; Fornell, J.; Holmgren, K.; Nilner, K.; Olsson, C.O. A prospective 5-year multicenter study of the cresco implantology concept. Int. J. Prosthodont. 2003, 16, 554–562. [Google Scholar] [PubMed]
- Al-Fadda, S.; Zarb, G.; Finer, Y. A comparison of the accuracy of fit of 2 methods for fabricating implant-prosthodontic frameworks. Int. J. Prosthodont. 2007, 20, 125–131. [Google Scholar]
- Katsoulis, J.; Mericske-Stern, R.; Yates, D.M.; Izutani, N.; Enkling, N.; Blatz, M.B. In vitro precision of fit of computer-aided design and computer-aided manufacturing titanium and zirconium dioxide bars. Dent. Mater. 2013, 29, 945–953. [Google Scholar] [CrossRef] [PubMed]
- Aloise, J.P.; Curcio, R.; Laporta, M.Z.; Rossi, L.; da Silva, A.M.Á.; Rapoport, A. Microbial leakage through the implant-abutment interface of morse taper implants in vitro. Clin. Oral. Implants. Res. 2010, 21, 328–335. [Google Scholar] [CrossRef]
- Montanini, R.; Scafidi, M.; Staiti, G.; Marcianò, A.; D’Acquisto, L.; Oteri, G. Misfit evaluation of dental implant-supported metal frameworks manufactured with different techniques: Photoelastic and strain gauge measurements. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2016, 230, 1106–1116. [Google Scholar] [CrossRef]
- Natali, A.N.; Pavan, P.G.; Ruggero, A.L. Evaluation of stress induced in peri-implant bone tissue by misfit in multi-implant prosthesis. Dent. Mater. 2006, 22, 388–395. [Google Scholar] [CrossRef]
- Meijer HJ, A.; Starmans FJ, M.; Bosman, F.; Steen, W.H.A. A comparison of three finite element models of an edentulous mandible provided with implants. J. Oral. Rehabil. 1993, 20, 147–157. [Google Scholar] [CrossRef]
- Meijer, H.J.A.; Starmans, F.J.M.; Steen, W.H.A.; Bosman, F. Loading conditions of endosseous implants in an edentulous human mandible: A three-dimensional, finite-element study. J. Oral. Rehabil. 1996, 23, 757–763. [Google Scholar] [CrossRef]
- Miyaura, K.; Morita, M.; Matsuka, Y.; Yamashita, A.; Watanabe, T. Rehabilitation of biting abilities in patients with different types of dental prostheses. J. Oral. Rehabil. 2000, 27, 1073–1076. [Google Scholar] [CrossRef]
- Sharma, A.J.; Nagrath, R.; Lahori, M. A comparative evaluation of chewing efficiency, masticatory bite force, and patient satisfaction between conventional denture and implant-supported mandibular overdenture: An in vivo study. J Indian Prosthodont Soc 2017, 17, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Helmy, M.A.; Kothayer, M. Effect of two different overdenture attachments on the biting force and occlusal force distribution. Egypt. Dent. J. 2019, 65, 1723–1732. [Google Scholar] [CrossRef][Green Version]
- Hu, F.; Gong, Y.; Bian, Z.; Zhang, X.; Xu, B.; Zhang, J.; Shi, X.; Yu, Y.; Song, L. Comparison of three different types of two-implant-supported magnetic attachments on the stress distribution in edentulous mandible. Comput. Math. Methods Med. 2019, 2019, 6839517. [Google Scholar] [CrossRef] [PubMed]
- Sivrikaya, E.C.; Güler, M.S.; Bekçi, M.L. Stress Distribution of Dental Implants in Lateral or Canine Areas: A Three-Dimensional Finite Element Analysis. EUDFD 2019, 40, 141–146. [Google Scholar] [CrossRef]







| Material | Poisson Ratio (V) | Elasticity Modulus (MPa) |
|---|---|---|
| Cortical Bone [41,42,43,44] | 0.3 | 13,700 |
| Trabecular Bone [41,42,43,44] | 0.3 | 1370 |
| Mucosa [41,42] | 0.37 | 1 |
| İmplant [33,43] | 0.33 | 110,000 |
| Screw [43,44] | 0.28 | 110,000 |
| Bar (Ti Grade 5/Ti-6Al-4V) [45,46] | 0.35 | 103,400 |
| Bar (Co-Cr alloy) [44] | 0.33 | 218,000 |
| Multi-unit abutment (Ti-6Al-7Nb) [46,47] | 0.28 | 110,000 |
| Yield Strength (MPa) | Tensile Strength (MPa) | |
|---|---|---|
| Ti [50] | 680 | 760 |
| Ti-6Al-4V (Ti Grade 5) [50] | 760 | 930 |
| Cortical Bone [50] | -- | 88–164 |
| Trabecular Bone [50] | -- | 23 |
| 100 N | ||||
|---|---|---|---|---|
| Model | Loading Direction | Stress Values (MPa) | ||
| Implant | Cortical Bone | Trabecular Bone | ||
| Model 1 | Horizontal | 419.42 | 119.60 | 2.84 |
| Vertical | 148.24 | 19.92 | 1.62 | |
| Oblique | 131.59 | 32.21 | 1.68 | |
| Model 2 | Horizontal | 312.24 | 72.10 | 3.27 |
| Vertical | 87.49 | 20.09 | 1.75 | |
| Oblique | 105.10 | 20.44 | 1.57 | |
| Model 3 | Horizontal | 316.68 | 72.14 | 3.26 |
| Vertical | 86.86 | 19.95 | 1.75 | |
| Oblique | 87.66 | 19.10 | 1.45 | |
| 100 N | |||
|---|---|---|---|
| Model | Loading Direction | Principal Stress Values (MPa) | |
| Maximum Principal Stress | Minimum Principal Stress | ||
| Model 1 | Horizontal | 141.69 | −114.75 |
| Vertical | 9.77 | −23.73 | |
| Oblique | 31.34 | −36.33 | |
| Model 2 | Horizontal | 61.50 | −84.47 |
| Vertical | 12.99 | −20.74 | |
| Oblique | 7.30 | −20.14 | |
| Model 3 | Horizontal | 61.97 | −83.95 |
| Vertical | 12.93 | −20.60 | |
| Oblique | 6.98 | −19.00 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kümbüloğlu, Ö.; Koyuncu, B.; Yerlioğlu, G.; Al-Haj Husain, N.; Özcan, M. Stress Distribution on Various Implant-Retained Bar Overdentures. Materials 2022, 15, 3248. https://doi.org/10.3390/ma15093248
Kümbüloğlu Ö, Koyuncu B, Yerlioğlu G, Al-Haj Husain N, Özcan M. Stress Distribution on Various Implant-Retained Bar Overdentures. Materials. 2022; 15(9):3248. https://doi.org/10.3390/ma15093248
Chicago/Turabian StyleKümbüloğlu, Övül, Beril Koyuncu, Gözde Yerlioğlu, Nadin Al-Haj Husain, and Mutlu Özcan. 2022. "Stress Distribution on Various Implant-Retained Bar Overdentures" Materials 15, no. 9: 3248. https://doi.org/10.3390/ma15093248
APA StyleKümbüloğlu, Ö., Koyuncu, B., Yerlioğlu, G., Al-Haj Husain, N., & Özcan, M. (2022). Stress Distribution on Various Implant-Retained Bar Overdentures. Materials, 15(9), 3248. https://doi.org/10.3390/ma15093248







