Compressive and Flexural Strength of 3D-Printed and Conventional Resins Designated for Interim Fixed Dental Prostheses: An In Vitro Comparison
Abstract
:1. Introduction
2. Materials and Methods
2.1. Fabrication of Resin Samples
- -
- 3DCS: The 3D-printed resin samples made from NextDent C&B MFH, NextDent by 3D Systems, Vertex B.V., Soesterberg, The Netherlands.
- -
- 3DOS: The 3D-printed resin samples made from HARZ Labs Dental Sand, HARZ Labs, Riga, Latvia;
- -
- CAP: The conventional auto-polymerized resin samples made from Duracyl, SpofaDental a.s., Jicin, Czech Republic, KaVo Kerr Group;
- -
- CHP: The conventional pressure/heat-cured acrylic resin samples made from Superpont C+B, SpofaDental a.s., Jicin, Czech Republic, KaVo Kerr Group.
2.2. Mechanical Tests
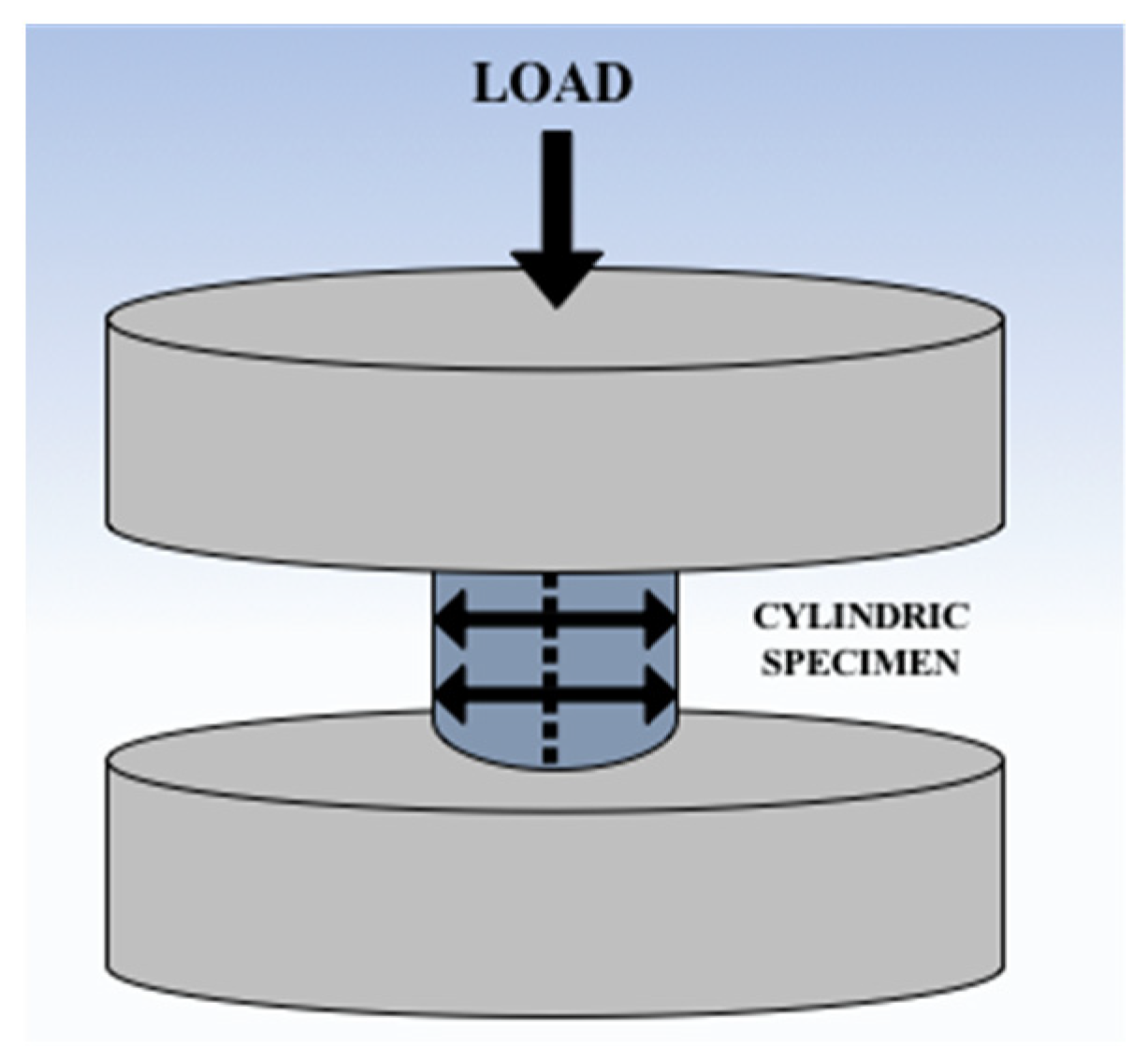
2.2.1. Compression Tests
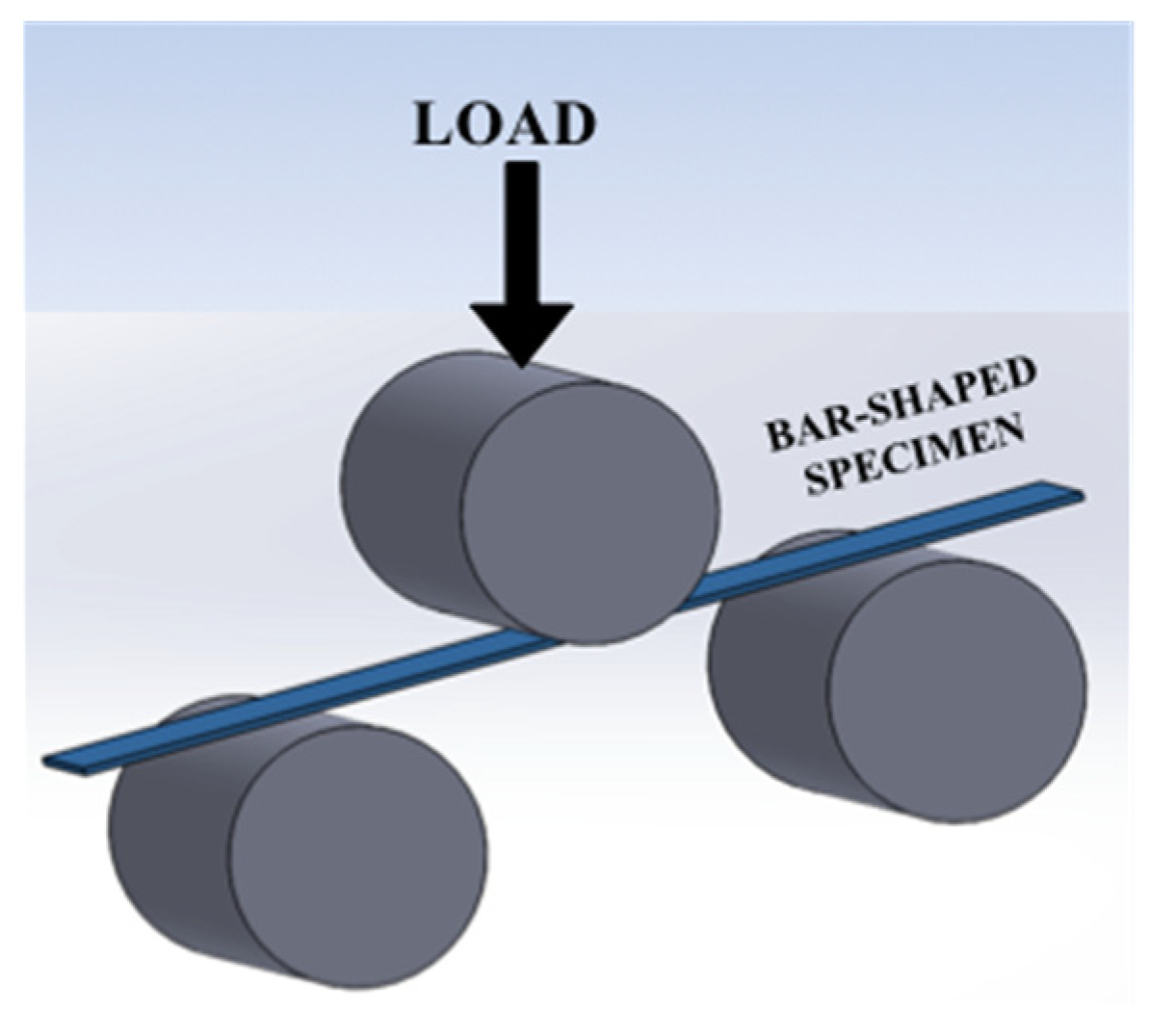
2.2.2. Flexural Tests (Three-Point Bending Tests)
2.2.3. Fractographic Analysis of Samples That Failed the Flexural Tests
3. Results
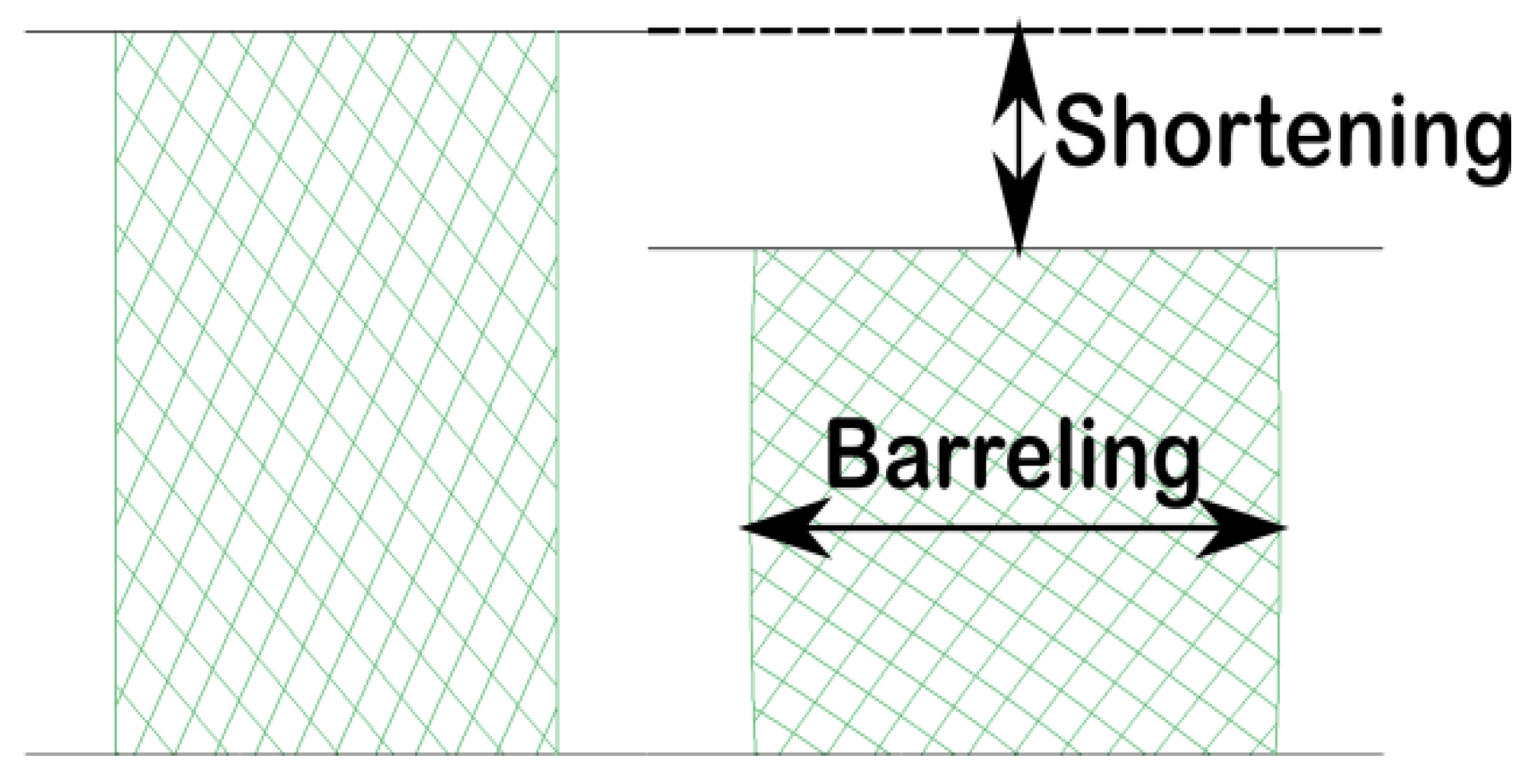
3.1. Compression Tests
3.2. Flexural Tests
3.3. Fractographic Analysis of Samples That Failed the Flexure Tests
4. Discussion
5. Conclusions
- The tested 3D-printed interim resins obtained better results than the conventional resins in both the compression and flexure tests;
- The 3D-printed resin coded 3DCS demonstrated the best mechanical behavior during the performed tests;
- From a structural point of view, the tested 3D-printed materials presented a better homogeneity than the conventional materials.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rosenstiel, S.F.; Land, M.F.; Fujimoto, J. Contemporary Fixed Prosthodontics, 4th ed.; Mosby: St. Louis, MO, USA, 2006; pp. 401, 466–467, 469–470, 482–489. [Google Scholar]
- Abad-Coronel, C.; Carrera, E.; Mena Córdova, N.; Fajardo, J.I.; Aliaga, P. Comparative Analysis of Fracture Resistance between CAD/CAM Materials for Interim Fixed Prosthesis. Materials 2021, 14, 7791. [Google Scholar] [CrossRef] [PubMed]
- Miura, S.; Fujisawa, M.; Komine, F.; Maseki, T.; Ogawa, T.; Takebe, J.; Nara, Y. Importance of interim restorations in the molar region. J. Oral Sci. 2019, 61, 195–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mousavi Nejad, Z.; Zamanian, A.; Saeidifar, M.; Vanaei, H.R.; Salar Amoli, M. 3D Bioprinting of Polycaprolactone-Based Scaffolds for Pulp-Dentin Regeneration: Investigation of Physicochemical and Biological Behavior. Polymers 2021, 13, 4442. [Google Scholar] [CrossRef] [PubMed]
- Piedra-Cascón, W.; Krishnamurthy, V.R.; Att, W.; Revilla-León, M. 3D printing parameters, supporting structures, slicing, and post-processing procedures of vat-polymerization additive manufacturing technologies: A narrative review. J. Dent. 2021, 109, 103630. [Google Scholar] [CrossRef] [PubMed]
- Mostafavi, D.; Methani, M.M.; Piedra-Cascón, W.; Zandinejad, A.; Revilla-León, M. Influence of the Rinsing Postprocessing Procedures on the Manufacturing Accuracy of Vat-Polymerized Dental Model Material. J. Prosthodont. 2021, 30, 610–616. [Google Scholar] [CrossRef]
- Campaner, M.; Takamiya, A.S.; Bitencourt, S.B.; Mazzaa, L.C.; Penha de Oliveira, S.H.; Shibayama, R.; Barãof, V.A.R.; Sukotjoe, C.; Alves Pesqueira, A. Cytotoxicity and inflammatory response of different types of provisional restorative materials. Arch. Oral Biol. 2020, 111, 104643. [Google Scholar] [CrossRef] [PubMed]
- Engler, M.L.P.D.; Güth, J.; Keul, C.; Erdelt, K.; Edelho, D.; Liebermann, A. Residual monomer elution from different conventional and CAD/CAM dental polymers during artificial aging. Clin. Oral Investig. 2020, 24, 277–284. [Google Scholar] [CrossRef]
- Pagano, S.; Lombardo, G.; Costanzi, E.; Balloni, S.; Bruscoli, S.; Flamini, S.; Coniglio, M.; Valenti, C.; Cianetti, S.; Marinucci, L. Morpho-functional effects of different universal dental adhesives on human gingival fibroblasts: An in vitro study. Odontology 2021, 109, 524–539. [Google Scholar] [CrossRef]
- Williams, D. Essential Biomaterials Science. In Cambridge Texts in Biomedical Engineering; Cambridge University Press: Cambridge, UK, 2014; pp. 130–132. [Google Scholar]
- Taşın, S.; Ismatullaev, A. Comparative evaluation of the effect of thermocycling on the mechanical properties of conventionally polymerized, CAD-CAM milled, and 3D-printed interim materials. J. Prosthet. Dent. 2022, 127, 173.e1–173.e8. [Google Scholar] [CrossRef]
- Reymus, M.; Lümkemann, N.; Stawarczyk, B. 3D-printed material for temporary restorations: Impact of print layer thickness and post-curing method on degree of conversion. Int. J. Comput. Dent. 2019, 22, 231–237. [Google Scholar]
- Firlej, M.; Pieniak, D.; Niewczas, A.M.; Walczak, A.; Domagała, I.; Borucka, A.; Przystupa, K.; Igielska-Kalwat, J.; Jarosz, W.; Biedziak, B. Effect of Artificial Aging on Mechanical and Tribological Properties of CAD/CAM Composite Materials Used in Dentistry. Materials 2021, 14, 4678. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Meyers, M.J.; Zandinejad, A.; Özcan, M. A review on chemical composition, mechanical properties, and manufacturing workflow of additively manufactured current polymers for interim dental restorations. J. Esthet. Restor. Dent. 2019, 31, 51–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jockusch, J.; Özcan, M. Additive manufacturing of dental polymers: An overview on processes, materials and applications. Dent. Mater. J. 2020, 39, 345–354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D printing restorative materials using a stereolithographic technique: A systematic review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef] [PubMed]
- Lim, N.K.; Shin, S.Y. Bonding of conventional interim resin to 3D-printed resin: The role of surface treatments and type of repair resins. J. Adv. Prosthodont. 2020, 12, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Nam, N.-E.; Shin, S.-H.; Lim, J.-H.; Shim, J.-S.; Kim, J.-E. Effects of Artificial Tooth Brushing and Hydrothermal Aging on The Mechanical Properties and Color Stability of Dental 3D-printed and CAD/CAM Materials. Materials 2021, 14, 6207. [Google Scholar] [CrossRef] [PubMed]
- Gantz, L.; Fauxpoint, G.; Arntz, Y.; Pelletier, H.; Etienne, O. In vitro comparison of the surface roughness of polymethyl methacrylate and bis-acrylic resins for interim restorations before and after polishing. J. Prosthet. Dent. 2021, 125, 833.e1. [Google Scholar] [CrossRef]
- Zhang, A.P.; Qu, X.; Soman, P.; Hribar, K.C.; Lee, J.W.; Chen, S.; He, S. Rapid fabrication of complex 3D extracellular microenvironments by dynamic optical projection stereolithography. Adv. Mater. 2012, 24, 4266–4270. [Google Scholar] [CrossRef] [Green Version]
- Lambert, H.; Durand, J.C.; Jacquot, B.; Fages, M. Dental biomaterials for chairside CAD/CAM: State of the art. Korean Acad. Prosthodont. 2017, 9, 486–495. [Google Scholar] [CrossRef] [Green Version]
- Al Jabbari, Y.S.; Al-Rasheed, A.; Smith, J.W.; Iacopino, A.M. An indirect technique for assuring simplicity and marginal integrity of provisional restorations during full mouth rehabilitation. Saudi Dent. J. 2013, 25, 39–42. [Google Scholar] [CrossRef] [Green Version]
- Pituru, S.M.; Greabu, M.; Totan, A.; Imre, M.; Pantea, M.; Spinu, T.; Tancu, A.M.C.; Popoviciu, N.O.; Stanescu, I.-I.; Ionescu, E. A Review on the biocompatibility of PMMA-based dental materials for interim prosthetic restorations with a glimpse into their modern manufacturing techniques. Materials 2020, 13, 2894. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Özcan, M. Additive Manufacturing Technologies Used for Processing Polymers: Current Status and Potential Application in Prosthetic Dentistry. J. Prosthodont. 2018, 28, 146–158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dong, T.; Wang, X.; Xia, L.; Yuan, L.; Ye, N.; Fang, B. Accuracy of different tooth surfaces on 3D printed dental models: Orthodontic perspective. BMC Oral Health 2020, 20, 340. [Google Scholar] [CrossRef] [PubMed]
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]
- Attaran, M. The rise of 3-D printing: The advantages of additive manufacturing over traditional manufacturing. Bus. Horiz. 2017, 60, 677–688. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Ilie, N. In vitro investigation of the influence of printing direction on the flexural strength, flexural modulus and fractographic analysis of 3D-printed temporary materials. Dent. Mater. J. 2021, 40, 641–649. [Google Scholar] [CrossRef]
- Park, S.M.; Park, J.M.; Kim, S.K.; Heo, S.J.; Koak, J.Y. Comparison of flexural strength of three-dimensional printed three-unit provisional fixed dental prostheses according to build directions. J. Korean Dent. Sci. 2019, 12, 13–19. [Google Scholar]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef]
- Unkovskiy, A.; Bui, P.H.B.; Schille, C.; Geis-Gerstorfer, J.; Huettig, F.; Spintzyk, S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent. Mater. 2018, 34, e324–e333. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.B.; Wismeijer, D. Factors Influencing the Dimensional Accuracy of 3D-Printed Full-Coverage Dental Restorations Using Stereolithography Technology. Int. J. Prosthodont. 2016, 29, 503–510. [Google Scholar] [CrossRef] [Green Version]
- Vanaei, S.; Parizi, M.S.; Vanaei, S.; Salemizadehparizi, F.; Vanaei, H.R. An Overview on Materials and Techniques in 3D Bioprinting Toward Biomedical Application. Eng. Regen. 2021, 2, 1–18. [Google Scholar] [CrossRef]
- Abdullah, A.O.; Pollington, S.; Liu, Y. Comparison between direct chairside and digitally fabricated temporary crowns. Dent. Mater. J. 2018, 37, 957–963. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alt, V.; Hannig, M.; Wöstmann, B.; Balkenhol, M. Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent. Mater. 2011, 27, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Manzon, L.; Vozza, I.; Poli, O. Bite Force in Elderly with Full Natural Dentition and Different Rehabilitation Prosthesis. Int. J. Environ. Res. Public Health 2021, 18, 1424. [Google Scholar] [CrossRef] [PubMed]
- Poli, O.; Manzon, L.; Niglio, T.; Ettorre, E.; Vozza, I. Masticatory force in relation with age in subjects with full permanent dentition: A cross-sectional study. Healthcare 2021, 9, 700. [Google Scholar] [CrossRef] [PubMed]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D-printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Simoneti, D.M.; Pereira-Cenci, T.; Dos Santos, M.B.F. Comparison of material properties and biofilm formation in interim single crowns obtained by 3D printing and conventional methods. J. Prosthet. Dent. 2020, 127, 168–172. [Google Scholar] [CrossRef]
- Reeponmaha, T.; Angwaravong, O.; Angwarawong, T. Comparison of fracture strength after thermo-mechanical aging between provisional crowns made with CAD/CAM and conventional method. J. Adv. Prosthodont. 2020, 12, 218. [Google Scholar] [CrossRef]
- Al-Halabi, M.N.; Bshara, N.; Comisi, J.C.; Abou Nassar, J. Evaluation of Fracture Resistance Force in Three Types of Primary Molar Crowns: Milled by CAD\CAM, 3D Dental Printed, and Composite Celluloid Crowns. Eur. Dent. Res. Biomater. J. 2020, 1, 33–39. [Google Scholar] [CrossRef]
- Park, S.-M.; Park, J.-M.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y. Flexural Strength of 3D-Printing Resin Materials for Provisional Fixed Dental Prostheses. Materials 2020, 13, 3970. [Google Scholar] [CrossRef]
- Al-Qahtani, A.S.; Tulbah, H.I.; Binhasan, M.; Abbasi, M.S.; Ahmed, N.; Shabib, S.; Farooq, I.; Aldahian, N.; Nisar, S.S.; Tanveer, S.A.; et al. Surface Properties of Polymer Resins Fabricated with Subtractive and Additive Manufacturing Techniques. Polymers 2021, 13, 4077. [Google Scholar] [CrossRef] [PubMed]
- Puebla, K.; Arcaute, K.; Quintana, R.; Wicker, R.B. Effects of environmental conditions, aging, and build orientations on the mechanical properties of ASTM type I specimens manufactured via stereolithography. Rapid Prototyp. J. 2012, 18, 374–388. [Google Scholar] [CrossRef]
- Arnold, C.; Monsees, D.; Hey, J.; Schweyen, R. Surface quality of 3D-printed models as a function of various printing parameters. Materials 2019, 12, 1970. [Google Scholar] [CrossRef] [Green Version]
- Ide, Y.; Nayar, S.; Logan, H.; Gallagher, B.; Wolfaardt, J. The effect of the angle of acuteness of additive manufactured models and the direction of printing on the dimensional fidelity: Clinical implications. Odontology 2017, 105, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Nold, J.; Wesemann, C.; Rieg, L.; Binder, L.; Witkowski, S.; Spies, B.C.; Kohal, R.J. Does printing orientation matter? In-vitro fracture strength of temporary fixed dental prostheses after a 1-year simulation in the artificial mouth. Materials 2021, 14, 259. [Google Scholar] [CrossRef] [PubMed]
- Reymus, M.; Fabritius, R.; Keßler, A.; Hickel, R.; Edelhoff, D.; Stawarczyk, B. Fracture load of 3D-printed fixed dental prostheses compared with milled and conventionally fabricated ones: The impact of resin material, build direction, post-curing, and artificial aging-an in vitro study. Clin. Oral Investig. 2020, 24, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Zhao, Z.; Zhang, Q.; Qi, H.J.; Fang, D. Mechanics of shape distortion of DLP 3D printed structures during UV post-curing. Soft Matter 2019, 15, 6151–6159. [Google Scholar] [CrossRef]
- Nayar, S.; Bhuminathan, S.; Bhat, W.M. Rapid prototyping and stereolithography in dentistry. J. Pharm. Bioallied Sci. 2015, 7, S216. [Google Scholar] [CrossRef]
- Skorulska, A.; Piszko, P.; Rybak, Z.; Szymonowicz, M.; Dobrzynski, M. Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry - Application, Mechanical Characteristics and Comparison. Materials 2021, 14, 1592. [Google Scholar] [CrossRef]
- Martín-Ortega, N.; Sallorenzo, A.; Casajús, J.; Cervera, A.; Revilla-León, M.; Gómez-Polo, M. Fracture resistance of additive manufactured and milled implant-supported interim crowns. J. Prosthet. Dent. 2022, 127, 267–274. [Google Scholar] [CrossRef]
- Tamini, F.; Hirayama, H. Digital Restorative Dentistry. A Guide to Materials, Equipment, and Clinical Procedures; Springer: Cham, Switzerland, 2019; Volume 57, pp. 63–64. [Google Scholar] [CrossRef]
- Alghazzawi, T.F. Advancements in CAD/CAM technology: Options for practical implementation. J. Prosthodont. Res. 2016, 60, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Patel, N. Contemporary dental CAD/CAM: Modern chairside/lab applications and the future of computerized dentistry. Compend. Contin. Educ. Dent. 2014, 35, 739–746. [Google Scholar] [PubMed]
- Iliescu, A.A.; Perlea, P.; Iliescu, M.G.; Gorea, V.; Nicolau, G. Printarea 3D în tehnologia dentara-statusul actual. Med. Stomatol. 2017, 45, 9–13. [Google Scholar]
- Stansbury, J.W.; Idacavage, M.J. 3D-printing with polymers: Challenges among expanding options and opportunities. Dent. Mater. 2016, 32, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-C.; Chen, T.; Lin, Y.-C. A Collaborative and Ubiquitous System for Fabricating Dental Parts Using 3D-printing Technologies. Healthcare 2019, 7, 103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Revilla-León, M.; Sadeghpour, M.; Özcan, M. An update on applications of 3D printing technologies used for processing polymers used in implant dentistry. Odontology 2020, 108, 331–338. [Google Scholar] [CrossRef]
- Reyes, M.G.; Torras, A.B.; Carrillo, J.A.C.; García, J.M.V.; Aguilar, J.J.C. A study of tensile and bending properties of 3D-printed biocompatible materials used in dental appliances. J. Mater. Sci. 2022, 57, 2953–2968. [Google Scholar] [CrossRef]
- Salmi, M. Additive Manufacturing Processes in Medical Applications. Materials 2021, 14, 191. [Google Scholar] [CrossRef]
- Patras, M.; Naka, O.; Doukoudakis, S.; Pissiotis, A. Management of provisional restorations’ deficiencies: A literature review. J. Esthet. Restor. Dent. 2012, 24, 26–38. [Google Scholar] [CrossRef]
- Murakami, N.; Wakabayashi, N.; Matsushima, R.; Kishida, A.; Igarashi, Y. Effect of high-pressure polymerization on mechanical properties of PMMA denture base resin. J. Mech. Behav. Biomed. Mater. 2013, 20, 98–104. [Google Scholar] [CrossRef]
- Lee, J.; Clark, S.R.; Tantbirojn, D.; Korioth, T.V.P.; Hill, A.E.; Versluis, A. Strength and stiffness of interim materials and interim fixed dental prostheses when tested at different loading rates. J. Prosthet. Dent. 2020, 127, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Peñate, L.; Basilio, J.; Roig, M.; Mercadé, M. Comparative study of interim materials for direct fixed dental prostheses and their fabrication with CAD/CAM technique. J. Prosthet. Dent. 2015, 114, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, A.; Baydas, S. Fracture resistance of various temporary crown materials. J. Contemp. Dent. Pract. 2007, 8, 44–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Digholkar, S.; Madhav, V.N.V.; Palaskar, J. Evaluation of the flexural strength and microhardness of provisional crown and bridge materials fabricated by different methods. J. Indian Prosthodont. Soc. 2016, 16, 328. [Google Scholar] [PubMed]
- Berge, M.; Hegdahl, T. Porosity of resin veneer materials. Acta Odontol. Scand. 1987, 45, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Bauer, R.; Zacher, J.; Strasser, T.; Rosentritt, M. In vitro performance and fracture resistance of interim conventional or CAD-CAM implant-supported screw-or cement-retained anterior fixed partial dentures. J. Prosthet. Dent. 2021, 126, 575–580. [Google Scholar] [CrossRef]







| Material Name | Manufacturer | Material (Resin) Type | Chemical Composition |
|---|---|---|---|
| NextDent C&B MFH | NextDent by 3D Systems, Vertex B.V., Soesterberg, The Netherlands | 3D-printed resin/DLP Microfilled hybrid material PMMA (poly (methyl methacrylate))-based resin Lot: NDCMN101000_1 | NP a |
| HARZ Labs Dental Sand | HARZ Labs, Riga, Latvia | 3D-printed resin/LCD PMMA (poly (methyl methacrylate))-like Microfilled composite resin Lot: 4603740518543 | NP a |
| Duracyl | SpofaDental a.s., Jicin, Czech Republic, KaVo Kerr Group | Auto-polymerized acrylic resin PMMA (poly (methyl methacrylate))-based Lot: 7169865 | Powder: poly (methyl methacrylate), BPO (benzoyl peroxide), pigments, initiator, plasticizers, gelatin, talc, mineral and organic dyes Liquid: methyl methacrylate, DMTP (dimethyl terephthalate), polymerization activator |
| Superpont C+B | SpofaDental a.s., Jicin, Czech Republic, KaVo Kerr Group | Pressure/heat-cured acrylic resin PMMA (poly (methyl methacrylate))-based Lot: 6766480 | - Powder: poly (methyl methacrylate), BPO (benzoyl peroxide), pigments, initiator, plasticizers, gelatin, talc, mineral and organic dyes Liquid: methyl methacrylate, triethylene glycol dimethacrylate, hydroquinone (polymerization inhibitor) |
| Sample Set | Elastic Modulus [MPa] | Elastic Limit [MPa] | Yield Strength [MPa] | Shortening [%] | Barreling [%] |
|---|---|---|---|---|---|
| CAP | 1315 ± 186 | 43 ± 10 | 73 ± 8 | 16 ± 1.0 | 34 ± 5.0 |
| CHP | 1346 ± 379 | 46 ± 9 | 64 ± 15 | NA | NA |
| 3DOS | 2419 ± 16 | 63 ± 3 | 97 ± 2 | 11 ± 1.0 | 19 ± 1.6 |
| 3DCS | 2615 ± 183 | 75 ± 3 | 110 ± 9 | 13 ± 0.7 | 23 ± 1.0 |
| Sample Set | Elastic Modulus [MPa] | Bending Strength [MPa] | Strain at Failure [%] |
|---|---|---|---|
| CAP | 4124 ± 333 | 88 ± 10 | 1.5 ± 0.01 |
| CHP | 4022 ± 1167 | 76 ± 7 | 1.1 ± 0.33 |
| 3DOS | 6329 ± 79 | 141 ± 17 | 1.34 ± 0.20 |
| 3DCS | 6402 ± 69 | 143 ± 15 | 1.38 ± 0.19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pantea, M.; Ciocoiu, R.C.; Greabu, M.; Ripszky Totan, A.; Imre, M.; Țâncu, A.M.C.; Sfeatcu, R.; Spînu, T.C.; Ilinca, R.; Petre, A.E. Compressive and Flexural Strength of 3D-Printed and Conventional Resins Designated for Interim Fixed Dental Prostheses: An In Vitro Comparison. Materials 2022, 15, 3075. https://doi.org/10.3390/ma15093075
Pantea M, Ciocoiu RC, Greabu M, Ripszky Totan A, Imre M, Țâncu AMC, Sfeatcu R, Spînu TC, Ilinca R, Petre AE. Compressive and Flexural Strength of 3D-Printed and Conventional Resins Designated for Interim Fixed Dental Prostheses: An In Vitro Comparison. Materials. 2022; 15(9):3075. https://doi.org/10.3390/ma15093075
Chicago/Turabian StylePantea, Mihaela, Robert Cătălin Ciocoiu, Maria Greabu, Alexandra Ripszky Totan, Marina Imre, Ana Maria Cristina Țâncu, Ruxandra Sfeatcu, Tudor Claudiu Spînu, Radu Ilinca, and Alexandru Eugen Petre. 2022. "Compressive and Flexural Strength of 3D-Printed and Conventional Resins Designated for Interim Fixed Dental Prostheses: An In Vitro Comparison" Materials 15, no. 9: 3075. https://doi.org/10.3390/ma15093075
APA StylePantea, M., Ciocoiu, R. C., Greabu, M., Ripszky Totan, A., Imre, M., Țâncu, A. M. C., Sfeatcu, R., Spînu, T. C., Ilinca, R., & Petre, A. E. (2022). Compressive and Flexural Strength of 3D-Printed and Conventional Resins Designated for Interim Fixed Dental Prostheses: An In Vitro Comparison. Materials, 15(9), 3075. https://doi.org/10.3390/ma15093075










