The Effect of Number and Distribution of Mini Dental Implants on Overdenture Stability: An In Vitro Study
Abstract
:1. Introduction
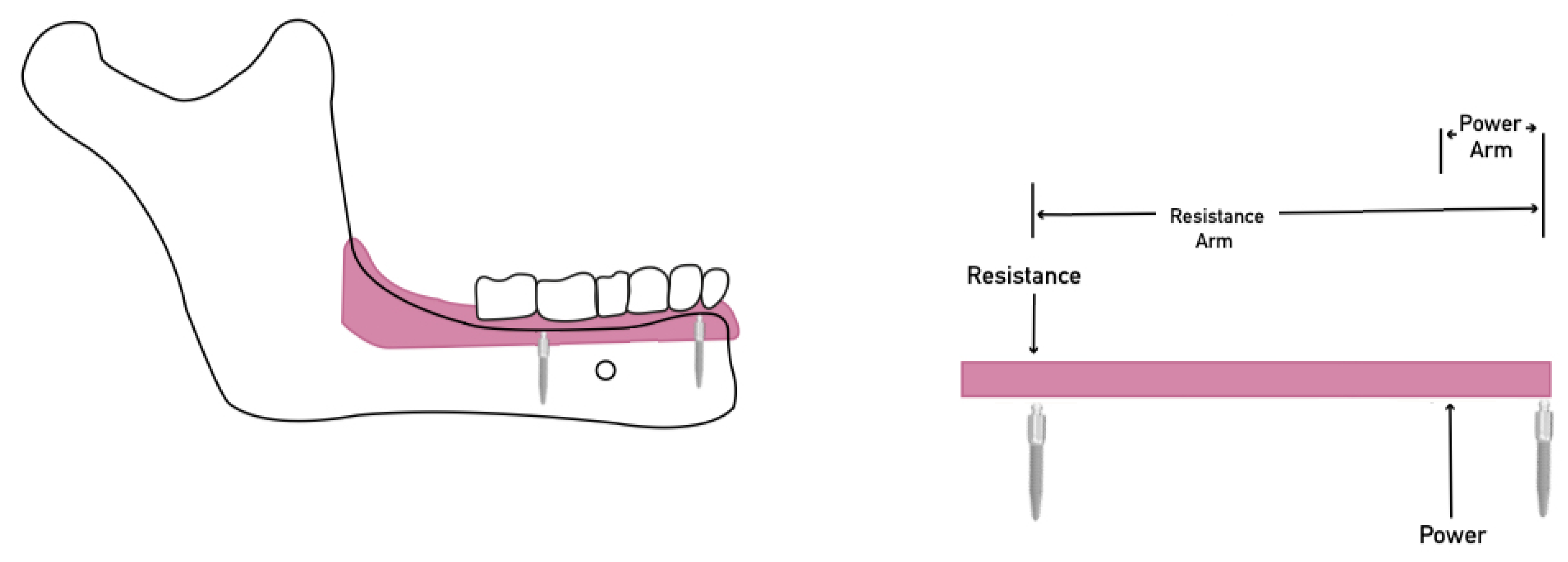
2. Materials and Methods
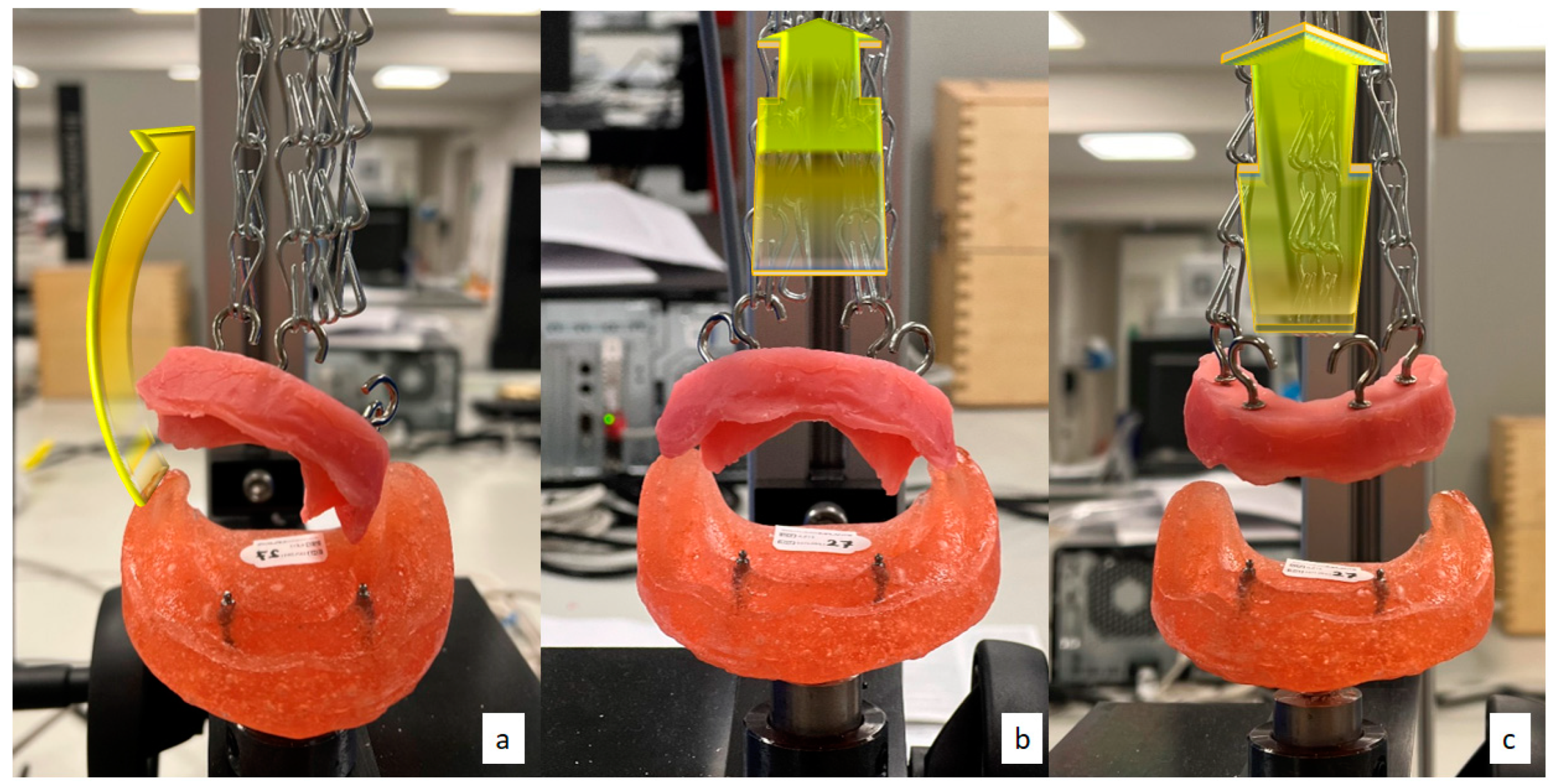
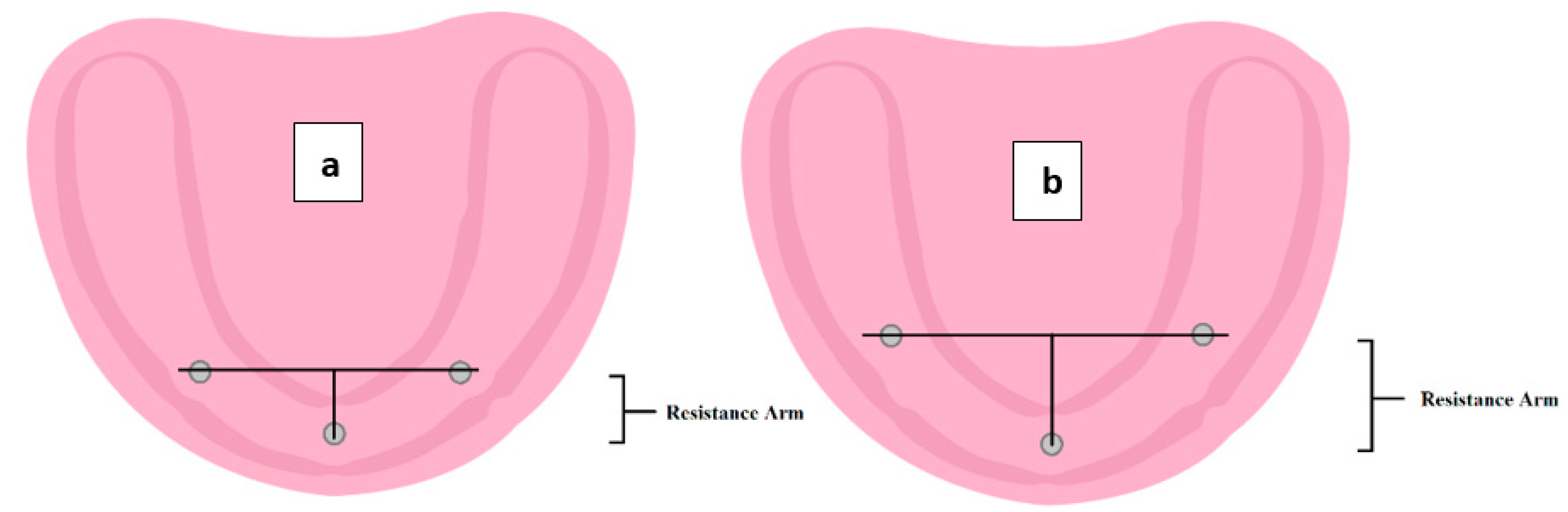
- Lateral (oblique) dislodgment: connecting two chains on the hooks at the right side and disconnecting the left side chains (Figure 2a). In addition, the left side dislodgment test was also carried out, but values were excluded to reduce data analysis.
- Anterior rotational dislodgment: connecting two chains on the hooks placed anteriorly and disconnecting the posterior side chains (Figure 2b).
- Posterior rotational dislodgment: connecting two chains on the hooks at the posterior at both sides and disconnecting the anterior chains (Figure 2c).
3. Results and Discussion
3.1. Initial Dislodgment Forces
3.2. Dislodgment Forces Following Six Months of Simulated Placement/Removal
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jacobson, T.E.; Krol, A.J. A contemporary review of the factors involved in complete dentures. Part II: Stability. J. Prosthet. Dent. 1983, 49, 165–172. [Google Scholar] [CrossRef]
- The Glossary of Prosthodontic Terms. J. Prosthet. Dent. 2005, 94, 10–92. [CrossRef] [PubMed]
- Mericske-Stern, R.; Geering, A.H.; Bürgin, W.B.; Graf, H.; Implants, M. Three-Dimensional Force Measurements on Mandibular Implants Supporting Overdentures. Int. J. Oral Maxillofac. Implant. 1992, 7, 7. [Google Scholar]
- Delucchi, F.; De Giovanni, E.; Pesce, P.; Bagnasco, F.; Pera, F.; Baldi, D.; Menini, M. Framework Materials for Full-Arch Implant-Supported Rehabilitations: A Systematic Review of Clinical Studies. Materials 2021, 14, 3251. [Google Scholar] [CrossRef] [PubMed]
- Marin, M.; Tandara, A.; Preoteasa, E.J.I.J.M.D. Correlations Between Inter-Implant Distance and Clinical Aspects in Two Implant Mandibular Overdentures. Int. J. Med. Dent. 2011, 1, 304–309. [Google Scholar]
- Türk, P.E.; Geckili, O.; Türk, Y.; Günay, V.; Bilgin, T. In vitro comparison of the retentive properties of ball and locator attachments for implant overdentures. Int. J. Oral Maxillofac. Implant. 2014, 29, 1106–1113. [Google Scholar] [CrossRef]
- Federick, D.R.; Caputo, A.A. Effects of overdenture retention designs and implant orientations on load transfer characteristics. J. Prosthet. Dent. 1996, 76, 624–632. [Google Scholar] [CrossRef]
- Meijer, H.J.A.; Raghoebar, G.M.; Batenburg, R.H.K.; Visser, A.; Vissink, A. Mandibular overdentures supported by two or four endosseous implants: A 10-year clinical trial. Clin. Oral Implant. Res. 2009, 20, 722–728. [Google Scholar] [CrossRef]
- Jawad, S.; Barclay, C.; Whittaker, W.; Tickle, M.; Walsh, T. A pilot randomised controlled trial evaluating mini and conventional implant retained dentures on the function and quality of life of patients with an edentulous mandible. BMC Oral Health 2017, 17, 53. [Google Scholar] [CrossRef] [Green Version]
- De Souza, R.F.; Ribeiro, A.B.; Della Vecchia, M.P.; Costa, L.; Cunha, T.R.; Reis, A.C.; Albuquerque, R.F. Mini vs. standard implants for mandibular overdentures: A randomized trial. J. Dent. Res. 2015, 94, 1376–1384. [Google Scholar] [CrossRef]
- Barclay, C.W.; Jawad, S.; Foster, E. Mini Dental Implants in the Management of The Atrophic Maxilla and Mandible: A New Implant Design and Preliminary Results. Eur. J. Prosthodont. Restor. Dent. 2018, 26, 190–196. [Google Scholar]
- Singh, R.; Ramashanker, P.C. Management of atrophic mandibular ridge with mini dental implant system. Natl. J. Maxillofac. Surg. 2010, 1, 176. [Google Scholar] [CrossRef] [PubMed]
- Chieruzzi, M.; Pagano, S.; Cianetti, S.; Lombardo, G.; Kenny, J.M.; Torre, L. Effect of fibre posts, bone losses and fibre content on the biomechanical behaviour of endodontically treated teeth: 3D-finite element analysis. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 74, 334–346. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Pan, S.; Dong, J.; Mo, Z.; Fan, Y.; Feng, H. Influence of implant number on the biomechanical behaviour of mandibular implant-retained/supported overdentures: A three-dimensional finite element analysis. J. Dent. 2013, 41, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Pisani, M.X.; Presotto, A.G.C.; Mesquita, M.F.; Barão, V.A.R.; Kemmoku, D.T.; Cury, A.A.D.B. Biomechanical behavior of 2-implant–and single-implant–retained mandibular overdentures with conventional or mini implants. J. Prosthet. Dent. 2018, 120, 421–430. [Google Scholar] [CrossRef]
- Warin, P.; Rungsiyakull, P.; Rungsiyakull, C.; Khongkhunthian, P. Effects of different numbers of mini-dental implants on alveolar ridge strain distribution under mandibular implant-retained overdentures. J. Prosthodont. Res. 2018, 62, 35–43. [Google Scholar] [CrossRef]
- Keirns, C.C.; Goold, S.D. Patient-centered care and preference-sensitive decision making. JAMA 2009, 302, 1805–1806. [Google Scholar] [CrossRef]
- Alshenaiber, R.; Cowan, C.; Barclay, C.; Silikas, N. Analysis of Residual Ridge Morphology in a Group of Edentulous Patients Seeking NHS Dental Implant Provision—A Retrospective Observational Lateral Cephalometric Study. Diagnostics 2021, 11, 2348. [Google Scholar] [CrossRef]
- Worthington, P.; Rubenstein, J.E. Problems associated with the atrophic mandible. Dent. Clin. N. Am. 1998, 42, 129–160. [Google Scholar]
- Misch, C.E. Chapter 10—Force Factors Related to Patient Conditions (A Determinant for Implant Number and Size). In Dental Implant Prosthetics, 2nd ed.; Misch, C.E., Ed.; Mosby: St. Louis, MO, USA, 2015; pp. 206–236. [Google Scholar] [CrossRef]
- Barclay, C.; Williams, R. The tensile and shear bond strength of a conventional and a 4-META self-cure acrylic resin to various surface finishes of Co-Cr alloy. Eur. J. Prosthodont. Restor. Dent. 1994, 3, 5–9. [Google Scholar]
- Timmerman, R.; Stoker, G.T.; Wismeijer, D.; Oosterveld, P.; Vermeeren, J.I.; van Waas, M.A. An eight-year follow-up to a randomized clinical trial of participant satisfaction with three types of mandibular implant-retained overdentures. J. Dent. Res. 2004, 83, 630–633. [Google Scholar] [CrossRef] [PubMed]
- Kimoto, S.; Pan, S.; Drolet, N.; Feine, J.S. Rotational movements of mandibular two-implant overdentures. Clin. Oral Implant. Res. 2009, 20, 838–843. [Google Scholar] [CrossRef] [PubMed]
- Petropoulos, V.C.; Smith, P.W.; Kousvelari, E. Comparison of retention and release periods for implant overdenture attachments. Int. J. Oral Maxillofac. Implant. 1997, 12, 176–185. [Google Scholar]
- Petropoulos, V.C.; Mante, F.K. Comparison of Retention and Strain Energies of Stud Attachments for Implant Overdentures. J. Prosthodont. 2011, 20, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Petropoulos, V.C.; Smith, W. Maximum dislodging forces of implant overdenture stud attachments. Int. J. Oral Maxillofac. Implant. 2002, 17, 526–535. [Google Scholar]
- Chung, K.-H.; Chung, C.-Y.; Cagna, D.R.; Cronin, R.J., Jr. Retention Characteristics of Attachment Systems for Implant Overdentures. J. Prosthodont. 2004, 13, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Setz, J.; Lee, S.H.; Engel, E. Retention of prefabricated attachments for implant stabilized overdentures in the edentulous mandible: An in vitro study. J. Prosthet. Dent. 1998, 80, 323–329. [Google Scholar] [CrossRef]
- Lee, E.; Shin, S.-Y. The influence of the number and the type of magnetic attachment on the retention of mandibular mini implant overdenture. J. Adv. Prosthodont. 2017, 9, 14–21. [Google Scholar] [CrossRef] [Green Version]
- Rutkunas, V.; Mizutani, H.; Takahashi, H. Influence of attachment wear on retention of mandibular overdenture. J. Oral Rehabil. 2007, 34, 41–51. [Google Scholar] [CrossRef]
- Al-Ghafli, S.A.; Michalakis, K.X.; Hirayama, H.; Kang, K. The in Vitro Effect of Different Implant Angulations and Cyclic Dislodgement on the Retentive Properties of an Overdenture Attachment System. J. Prosthet. Dent. 2009, 102, 140–147. [Google Scholar] [CrossRef]
- Sadig, W. A comparative in vitro study on the retention and stability of implant-supported overdentures. Quintessence Int. 2009, 40, 313–319. [Google Scholar] [PubMed]
- Avant, W.E. Indirect retention in partial denture design. J. Prosthet. Dent. 1966, 16, 1103–1110. [Google Scholar] [CrossRef]
- Scherer, M.D.; McGlumphy, E.A.; Seghi, R.R.; Campagni, W.V. Comparison of retention and stability of two implant-retained overdentures based on implant location. J. Prosthet Dent. 2014, 112, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Doukas, D.; Michelinakis, G.; Smith, P.W.; Barclay, C.W. The influence of interimplant distance and attachment type on the retention characteristics of mandibular overdentures on 2 implants: 6-month fatigue retention values. Int. J. Prosthodont. 2008, 21, 152–154. [Google Scholar]
- Michelinakis, G.; Barclay, C.; Smith, P. The influence of interimplant distance and attachment type on the retention characteristics of mandibular overdentures on 2 implants: Initial retention values. Int. J. Prosthodont. 2006, 19, 507–512. [Google Scholar]
- Beresin, V.E.; Schiesser, F.J. The neutral zone in complete dentures. J. Prosthet. Dent. 1976, 36, 356–367. [Google Scholar] [CrossRef]
- Elsyad, M.; Elhaddad, A.; Khirallah, A. Retentive Properties of O-Ring and Locator Attachments for Implant-Retained Maxillary Overdentures: An In Vitro Study. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2018, 27, 568–576. [Google Scholar] [CrossRef]
- Rendell, J.; Grasso, J.E.; Gay, T. Retention and stability of the maxillary denture during function. J. Prosthet. Dent. 1995, 73, 344–347. [Google Scholar] [CrossRef]
- CH/106/2. BS EN ISO 13017:2020 Dentistry; Magnetic Attachments. BSI: Brussels, Belgium, 2020.
- Barão, V.A.; Assunção, W.G.; Tabata, L.F.; de Sousa, E.A.; Rocha, E.P. Effect of different mucosa thickness and resiliency on stress distribution of implant-retained overdentures-2D FEA. Comput. Methods Programs Biomed. 2008, 92, 213–223. [Google Scholar] [CrossRef]
- Guo, Y.; Kono, K.; Suzuki, Y.; Ohkubo, C.; Zeng, J.-Y.; Zhang, J. Influence of marginal bone resorption on two mini implant-retained mandibular overdenture: An in vitro study. J. Adv. Prosthodont. 2021, 13, 55–64. [Google Scholar] [CrossRef]
- Boulos, P.J.; Akiki, L.A.; Makzoumé, J.E.; Fakhoury, J.; Tohmé, H.; El Hage, F.S. Retentive force variations of stud attachments for implant overdentures. Gen. Dent. 2018, 66, 41–45. [Google Scholar] [PubMed]
- Botega, D.M.; Mesquita, M.F.; Henriques, G.E.P.; Vaz, L.G. Retention force and fatigue strength of overdenture attachment systems. J. Oral Rehabil. 2004, 31, 884–889. [Google Scholar] [CrossRef] [PubMed]
- Rutkunas, V.; Mizutani, H.; Takahashi, H. Evaluation of stable retentive properties of overdenture attachments. Stomatologija 2005, 7, 115–120. [Google Scholar] [PubMed]
- Mumcu, E.; Bilhan, H.; Geckili, O. The effect of attachment type and implant number on satisfaction and quality of life of mandibular implant-retained overdenture wearers. Gerodontology 2012, 29, e618–e623. [Google Scholar] [CrossRef] [PubMed]

| Force to Dislodgment (N) ± SD | One Way ANOVA p Value | |||||||
|---|---|---|---|---|---|---|---|---|
| Dislodgment Force Direction | 2MDIs-19 | 2MDIs-23 | 2MDIs-27 | 3MDIs-1 | 3MDIs-2 | 4MDIs-1 | 4MDIs-2 | |
| Right lateral oblique | 22.20 ± 0.30 | 22.84 ± 0.76 | 22.20 ± 0.61 | 27.83 ± 0.49 | 27.99 ± 0.62 | 34.72 ± 0.28 | 34.98 ± 0.28 | 0.00 * |
| Anterior rotational | 27.91 ± 0.68 | 28.16 ± 0.43 | 28.20 ± 0.68 | 32.02 ± 0.45 | 34.81 ± 0.35 | 38.04 ± 0.16 | 39.17 ± 0.27 | 0.00 * |
| Posterior rotational | 25.92 ± 0.57 | 26.72 ± 0.65 | 28.79 ± 0.68 | 36.99 ± 0.49 | 38.03 ± 0.31 | 38.84 ± 0.63 | 39.69 ± 0.33 | 0.00 * |
| The Inter-Implant Distances Groups | p Value at Lateral Dislodgment | p Value at Anterior Dislodgment |
|---|---|---|
| 19 mm vs. 23 mm | 0.44 | 0.98 |
| 19 mm vs. 27 mm | 1.00 | 0.95 |
| 23 mm vs. 27 mm | 0.45 | 1.00 |
| Force to Dislodgment (N) ± SD | One Way ANOVA p Value | |||||||
|---|---|---|---|---|---|---|---|---|
| Dislodgment Force Direction | 2MDIs-19 | 2MDIs-23 | 2MDIs-27 | 3MDIs-1 | 3MDIs-2 | 4MDIs-1 | 4MDIs-2 | |
| Right lateral oblique | 17.87 ± 0.31 | 18.42 ± 0.34 | 17.92 ± 0.66 | 22.70 ± 0.55 | 22.76 ± 0.39 | 28.43 ± 0.35 | 28.44 ± 0.58 | 0.00 * |
| Anterior rotational | 28.11 ± 0.49 | 27.82 ± 0.33 | 27.72 ± 0.39 | 29.54 ± 0.33 | 30.24 ± 0.45 | 34.70 ± 0.25 | 36.70 ± 0.34 | 0.00 * |
| Posterior rotational | 22.56 ± 0.31 | 22.87 ± 0.18 | 23.90 ± 0.31 | 31.65 ± 1.36 | 33.66 ± 0.27 | 35.85 ± 0.27 | 37.29 ± 0.79 | 0.00 * |
| The Inter-Implant Distances Groups | p Value at Lateral Dislodgment | p Value at Anterior Dislodgment |
|---|---|---|
| 19 mm vs. 23 mm | 0.53 | 0.88 |
| 19 mm vs. 27 mm | 1.00 | 0.67 |
| 23 mm vs. 27 mm | 0.63 | 1.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshenaiber, R.; Barclay, C.; Silikas, N. The Effect of Number and Distribution of Mini Dental Implants on Overdenture Stability: An In Vitro Study. Materials 2022, 15, 2988. https://doi.org/10.3390/ma15092988
Alshenaiber R, Barclay C, Silikas N. The Effect of Number and Distribution of Mini Dental Implants on Overdenture Stability: An In Vitro Study. Materials. 2022; 15(9):2988. https://doi.org/10.3390/ma15092988
Chicago/Turabian StyleAlshenaiber, Rafif, Craig Barclay, and Nick Silikas. 2022. "The Effect of Number and Distribution of Mini Dental Implants on Overdenture Stability: An In Vitro Study" Materials 15, no. 9: 2988. https://doi.org/10.3390/ma15092988
APA StyleAlshenaiber, R., Barclay, C., & Silikas, N. (2022). The Effect of Number and Distribution of Mini Dental Implants on Overdenture Stability: An In Vitro Study. Materials, 15(9), 2988. https://doi.org/10.3390/ma15092988







