Analysis of the Effect of Component Ratio Imbalances on Selected Mechanical Properties of Seasoned, Medium Viscosity Bone Cements
Abstract
:1. Introduction
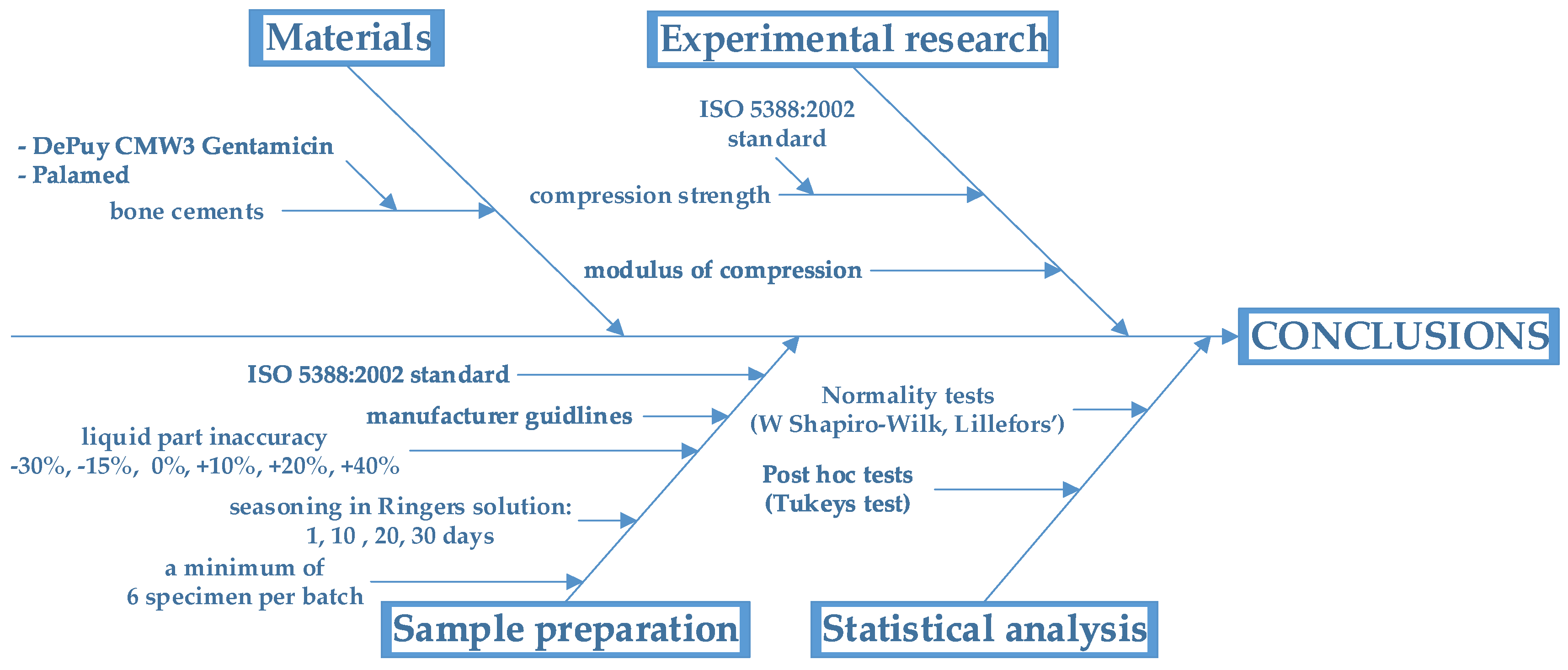
2. Materials and Methods
2.1. Materials and Sample Preparation
- polymethyl methacrylate (PMMA) and benzoyl peroxide (as initiator),
- radiopaque agent: barium sulphate (in CMW3), zirconium dioxide (in Palamed);
- antibiotic: gentamicin sulphate (in CMW3),
- colourant: E141—chlorophyllin (in Palamed).
- methyl methacrylate (MMA),
- N,N-dimethyl-ptoluidine (DMPT) (as accelerator),
- hydroquinone (as stabiliser),
- colorant: E141—chlorophyllin (in Palamed, as colorant).
2.2. Mechanical Testing
2.3. Statistical Analysis
3. Results and Discussion
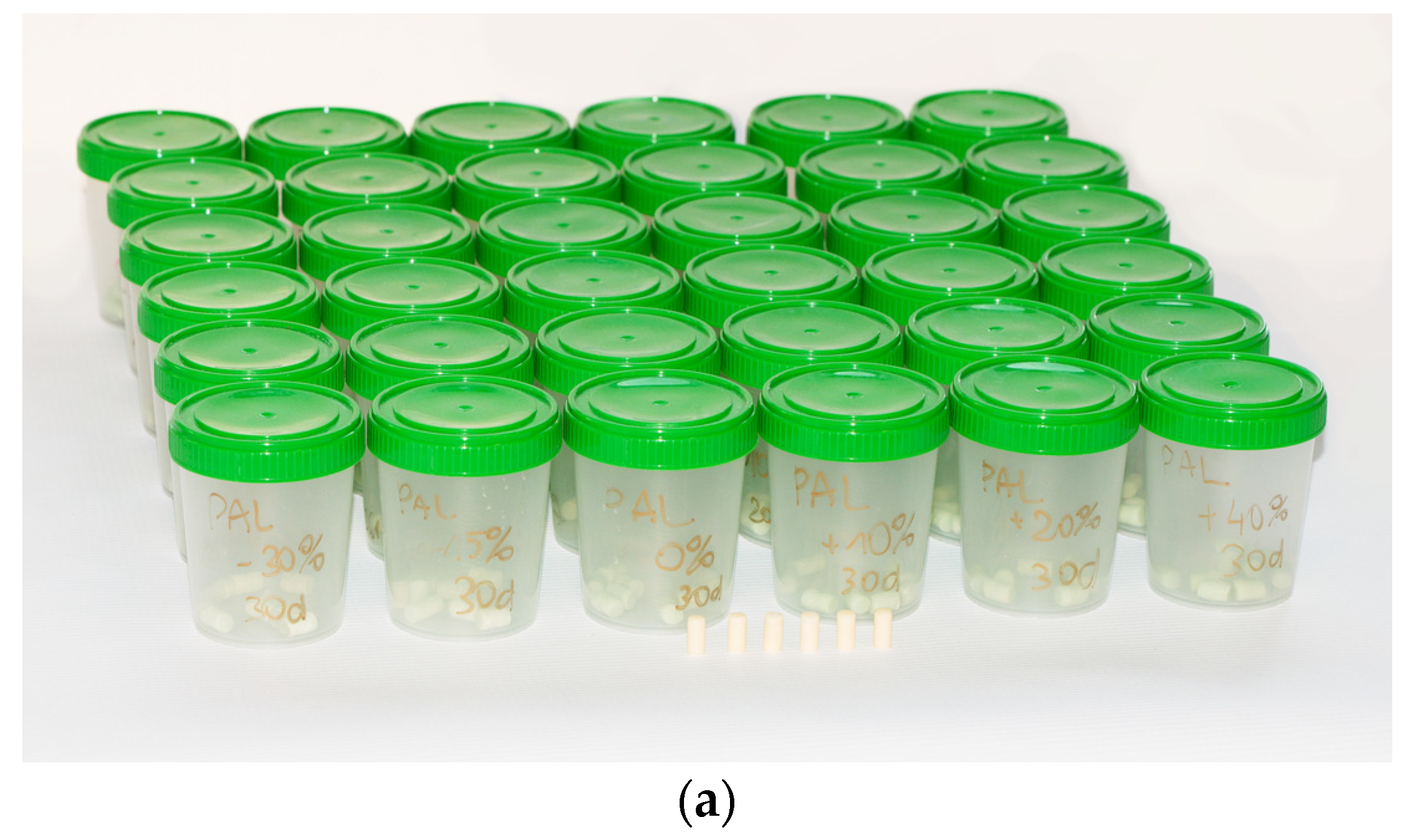
3.1. Moisture Uptake
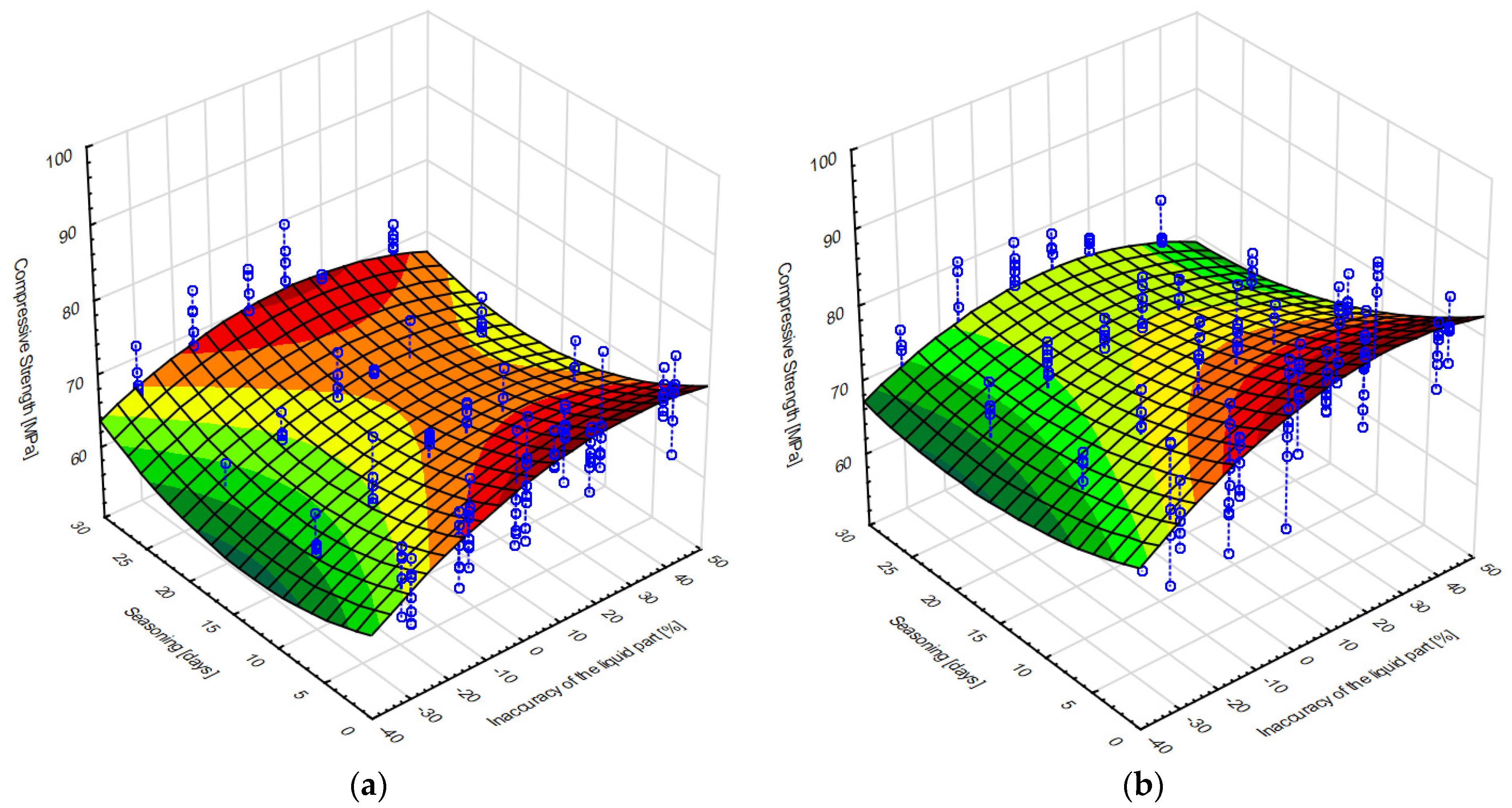
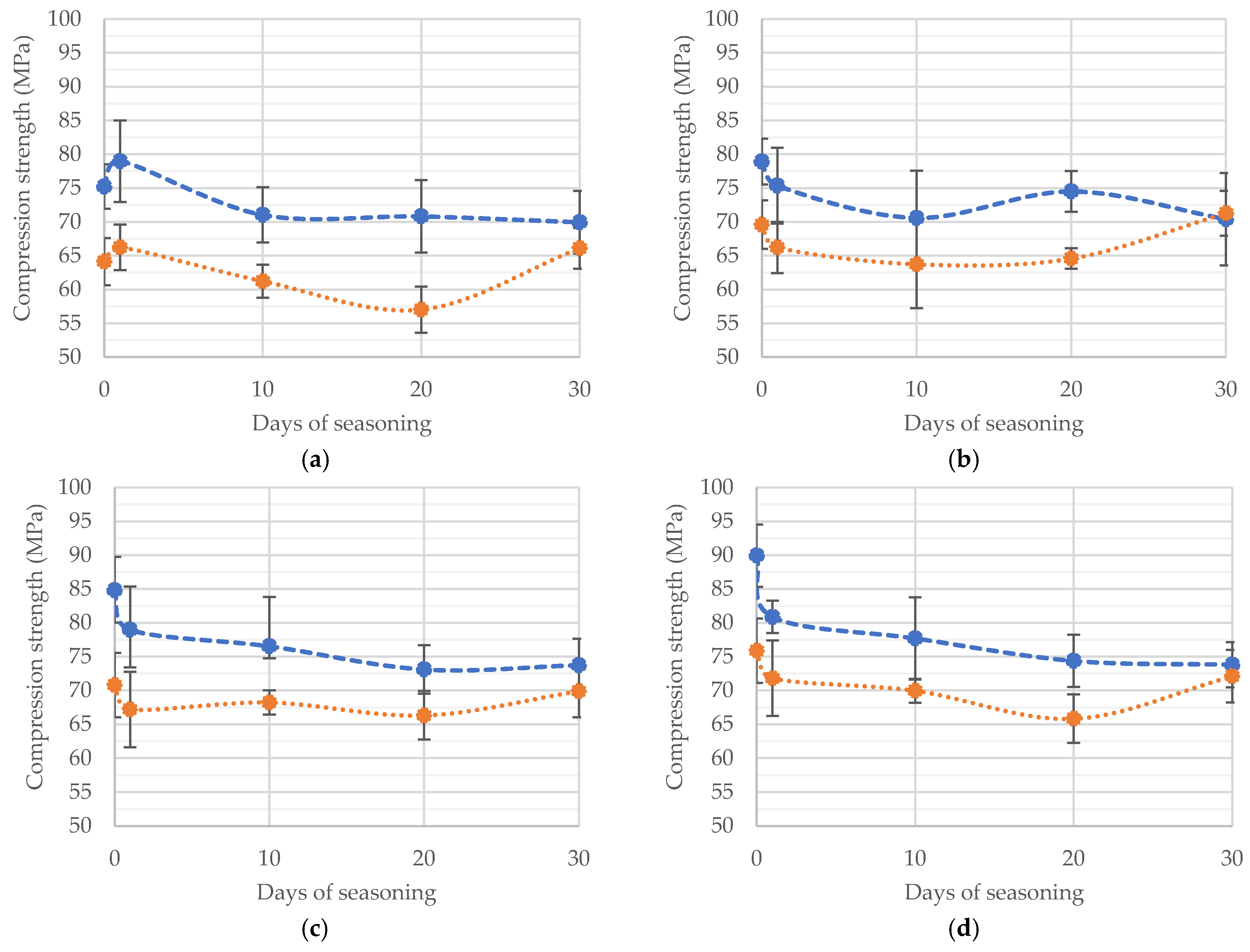
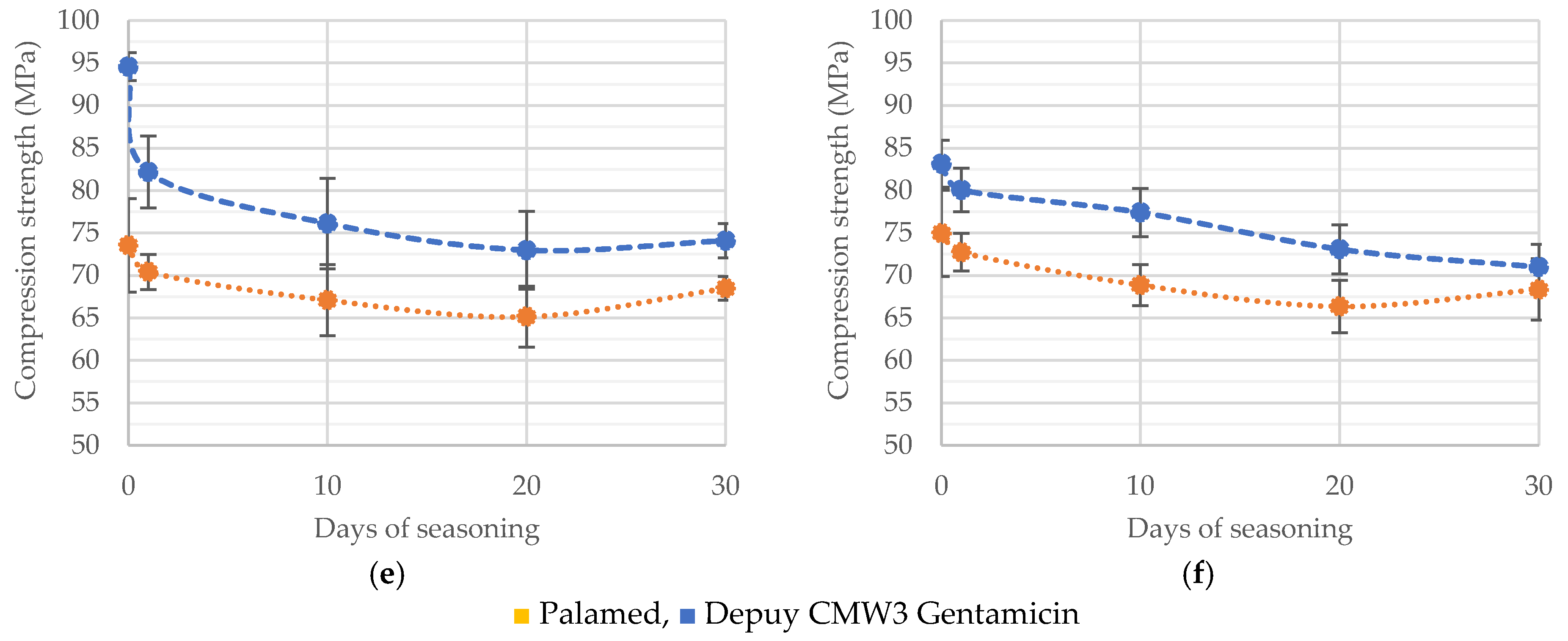
3.2. Compressive Strength
- b1—free expression,
- b2–b6—coefficients at individual components,
- v1—liquid component inaccuracy (%),
- v2—seasoning time (days).
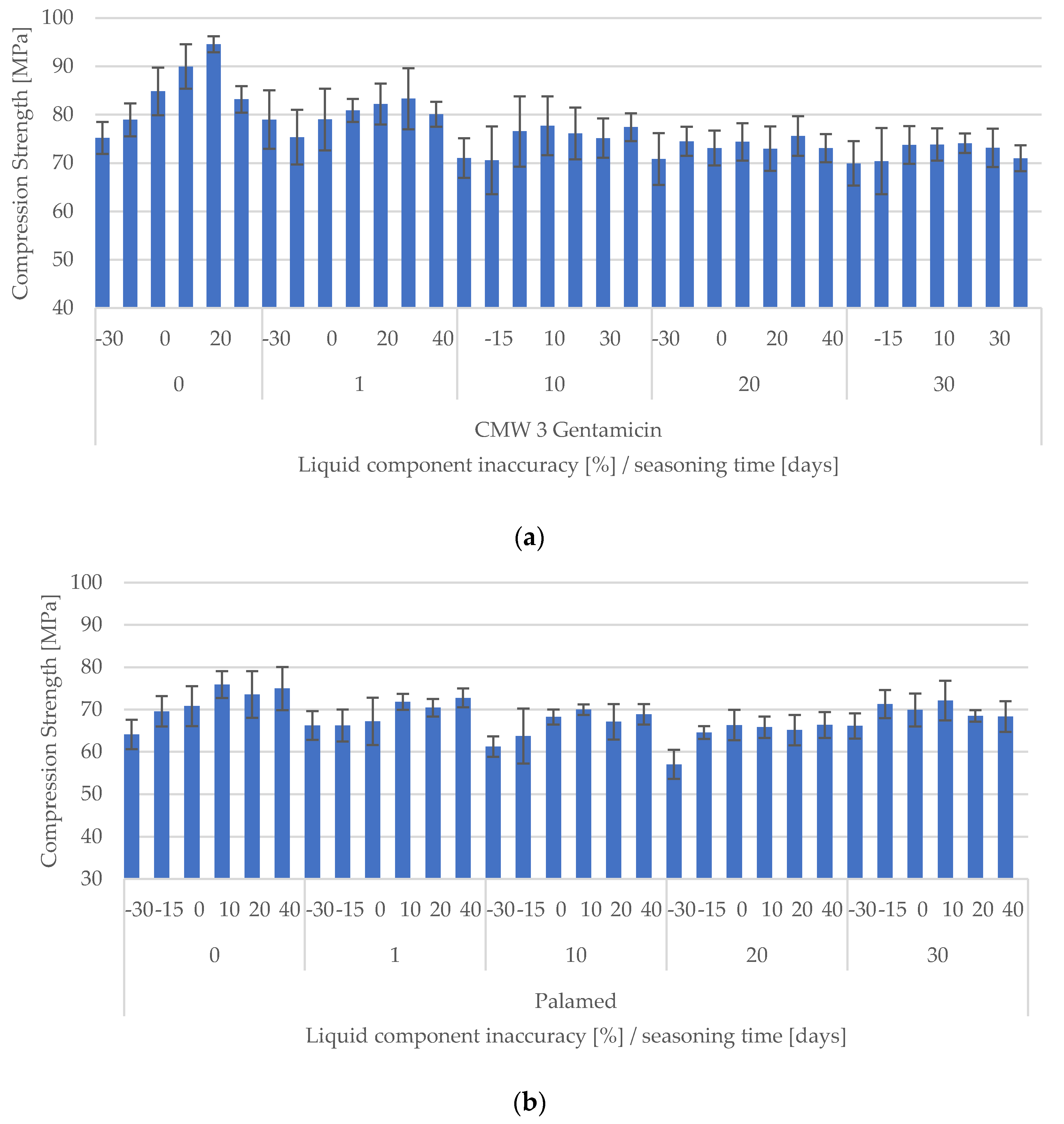
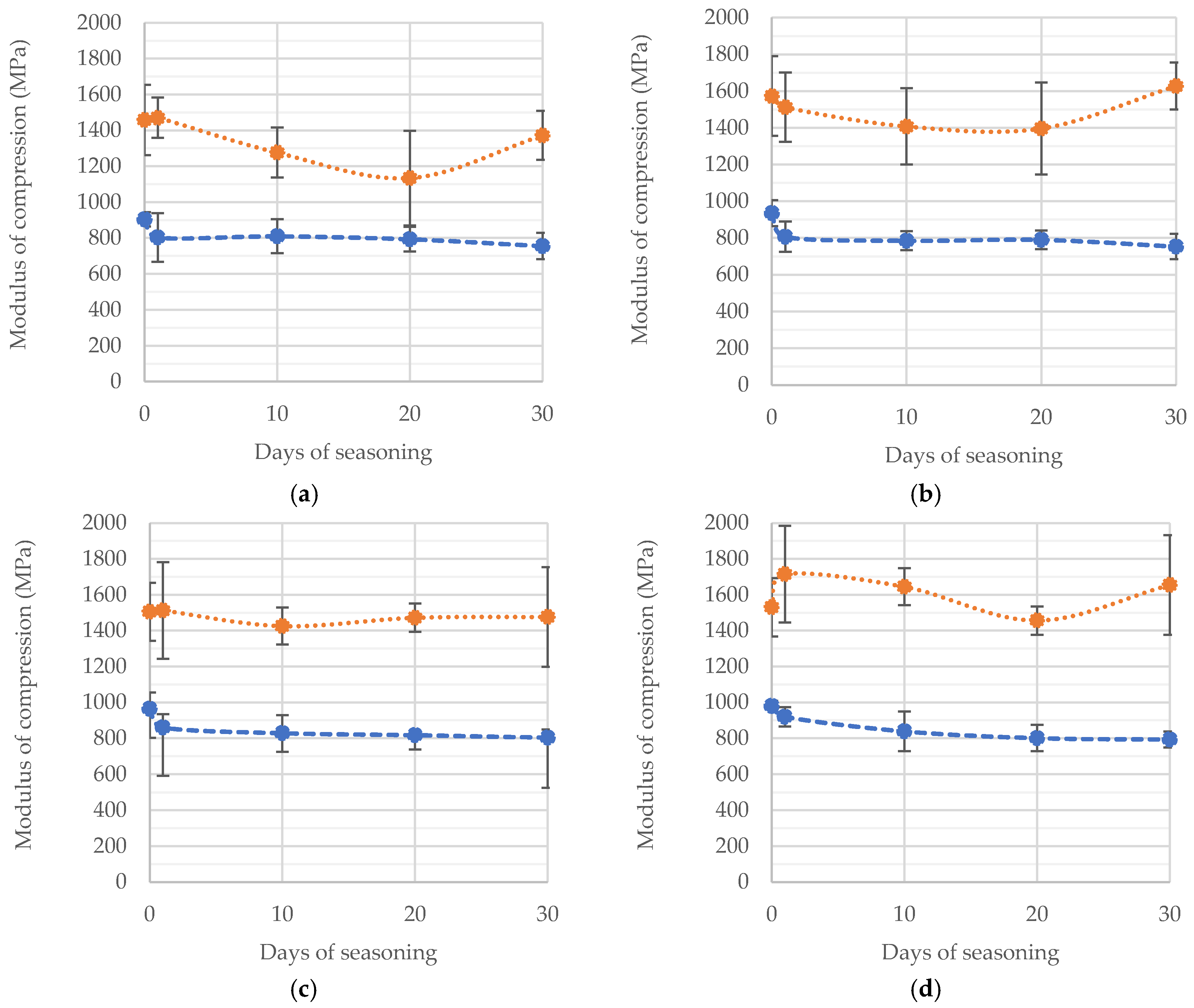
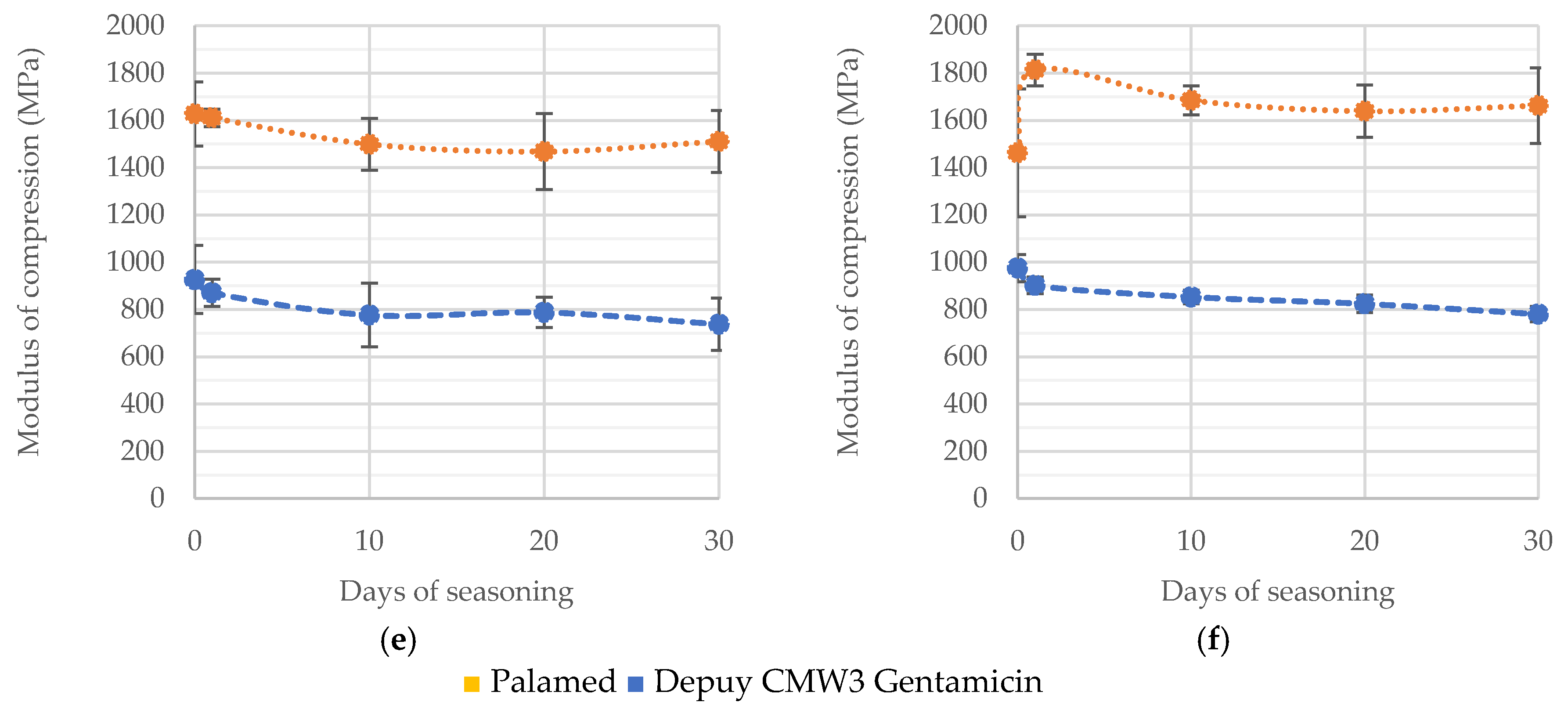
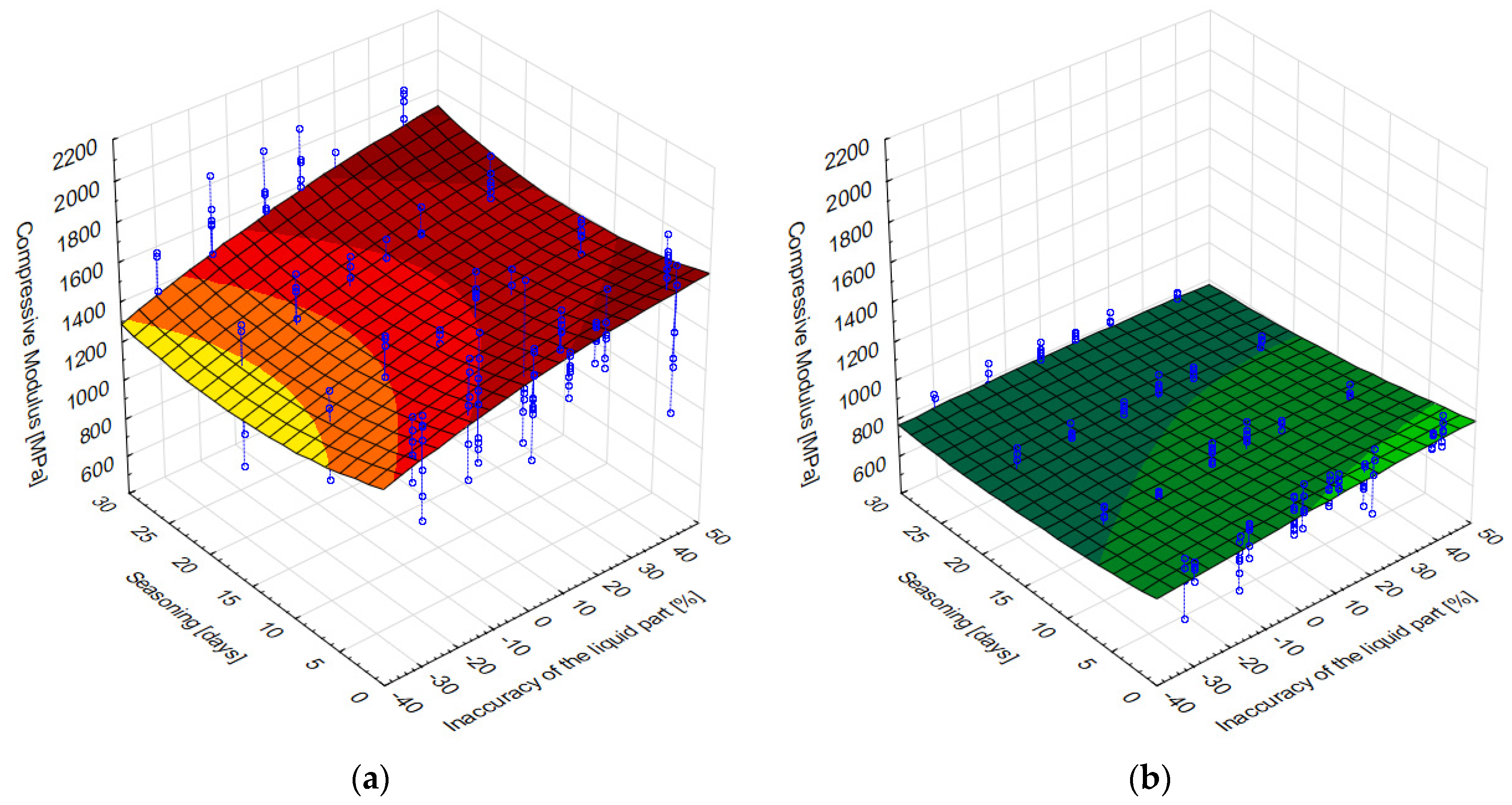
3.3. Compressive Modulus of Elasticity
4. Discussion
Limitations of the Study and General Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Australian Orthopaedic Association. National Joint Replacement Registry. Annual Report; AOA: Adelaide, Australia, 2015. [Google Scholar]
- Singh, J.A.; Yu, S.; Chen, L.; Cleveland, J.D. Rates of Total Joint Replacement in the United States: Future Projections to 2020–2040 Using the National Inpatient Sample. J. Rheumatol. 2019, 46, 1134–1140. [Google Scholar] [CrossRef] [PubMed]
- Kontis, V.; Bennett, J.E.; Mathers, C.D.; Li, G.; Foreman, K.; Ezzati, M. Future Life Expectancy in 35 Industrialised Countries: Projections with a Bayesian Model Ensemble. Lancet 2017, 389, 1323–1335. [Google Scholar] [CrossRef]
- Neogi, T.; Zhang, Y. Epidemiology of Osteoarthritis. Rheum. Dis. Clin. N. Am. 2013, 39, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Krakowski, P.; Nogalski, A.; Jurkiewicz, A.; Karpiński, R.; Maciejewski, R.; Jonak, J. Comparison of Diagnostic Accuracy of Physical Examination and MRI in the Most Common Knee Injuries. Appl. Sci. 2019, 9, 4102. [Google Scholar] [CrossRef]
- Karpiński, R.; Krakowski, P.; Jonak, J.; Machrowska, A.; Maciejewski, M.; Nogalski, A. Diagnostics of Articular Cartilage Damage Based on Generated Acoustic Signals Using ANN—Part I: Femoral-Tibial Joint. Sensors 2022, 22, 2176. [Google Scholar] [CrossRef] [PubMed]
- Karpiński, R.; Krakowski, P.; Jonak, J.; Machrowska, A.; Maciejewski, M.; Nogalski, A. Diagnostics of Articular Cartilage Damage Based on Generated Acoustic Signals Using ANN—Part II: Patellofemoral Joint. Sensors 2022, 22, 3765. [Google Scholar] [CrossRef] [PubMed]
- Reyes, C.; Garcia-Gil, M.; Elorza, J.; Mendez-Boo, L.; Hermosilla, E.; Javaid, M.; Cooper, C.; Diez-Perez, A.; Arden, N.; Bolibar, B.; et al. Socio-Economic Status and the Risk of Developing Hand, Hip or Knee Osteoarthritis: A Region-Wide Ecological Study. Osteoarthr. Cartil. 2015, 23, 1323–1329. [Google Scholar] [CrossRef]
- Johnson, V.; Hunter, D. The Epidemiology of Osteoarhtritis. Best Pract. Res. Clin. Rheumatol 2014, 28, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Krakowski, P.; Karpiński, R.; Jojczuk, M.; Nogalska, A.; Jonak, J. Knee MRI Underestimates the Grade of Cartilage Lesions. Appl. Sci. 2021, 11, 1552. [Google Scholar] [CrossRef]
- Cibere, J.; Sayre, E.C.; Guermazi, A.; Nicolaou, S.; Kopec, J.A.; Esdaile, J.M.; Thorne, A.; Singer, J.; Wong, H. Natural History of Cartilage Damage and Osteoarthritis Progression on Magnetic Resonance Imaging in a Population-Based Cohort with Knee Pain. Osteoarthr. Cartil. 2011, 19, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Krakowski, P.; Karpiński, R.; Maciejewski, R.; Jonak, J.; Jurkiewicz, A. Short-Term Effects of Arthroscopic Microfracturation of Knee Chondral Defects in Osteoarthritis. Appl. Sci. 2020, 10, 8312. [Google Scholar] [CrossRef]
- Jenny, J.-Y. Minimally Invasive Unicompartmental Knee Arthroplasty. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 793–797. [Google Scholar] [CrossRef] [PubMed]
- Mistry, H.; Connock, M.; Pink, J.; Shyangdan, D.; Clar, C.; Royle, P.; Court, R.; Biant, L.C.; Metcalfe, A.; Waugh, N. Autologous Chondrocyte Implantation in the Knee: Systematic Review and Economic Evaluation. Health Technol. Assess. 2017, 21, 1–294. [Google Scholar] [CrossRef] [PubMed]
- Castagnini, F.; Sudanese, A.; Bordini, B.; Tassinari, E.; Stea, S.; Toni, A. Total Knee Replacement in Young Patients: Survival and Causes of Revision in a Registry Population. J. Arthroplast. 2017, 32, 3368–3372. [Google Scholar] [CrossRef]
- Gwam, C.U.; Mistry, J.B.; Mohamed, N.S.; Thomas, M.; Bigart, K.C.; Mont, M.A.; Delanois, R.E. Current Epidemiology of Revision Total Hip Arthroplasty in the United States: National Inpatient Sample 2009 to 2013. J. Arthroplast. 2017, 32, 2088–2092. [Google Scholar] [CrossRef]
- Learmonth, I.D.; Young, C.; Rorabeck, C. The Operation of the Century: Total Hip Replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef]
- Klasan, A.; Bäumlein, M.; Bliemel, C.; Putnis, S.E.; Neri, T.; Schofer, M.D.; Heyse, T.J. Cementing of the Hip Arthroplasty Stem Increases Load-to-Failure Force: A Cadaveric Study. Acta Orthop. 2019, 90, 445–449. [Google Scholar] [CrossRef]
- Polkowski, G.G.; Clohisy, J.C. Hip Biomechanics. Sports Med. Arthrosc. Rev. 2010, 18, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Vaishya, R.; Chauhan, M.; Vaish, A. Bone Cement. J. Clin. Orthop. Trauma 2013, 4, 157–163. [Google Scholar] [CrossRef]
- Sundfeldt, M.; Carlsson, L.V.; Johansson, C.B.; Thomsen, P.; Gretzer, C. Aseptic Loosening, Not Only a Question of Wear: A Review of Different Theories. Acta Orthop. 2006, 77, 177–197. [Google Scholar] [CrossRef]
- Wooley, P.; Schwarz, E. Aseptic Loosening. Gene Ther. 2004, 11, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Lewis, G. Properties of Acrylic Bone Cement: State of the Art Review. J. Biomed. Mater. Res. 1997, 38, 155–182. [Google Scholar] [CrossRef]
- Willert, H.G.; Bertram, H.; Buchhorn, G.H. Osteolysis in Alloarthroplasty of the Hip. The Role of Bone Cement Fragmentation. Clin. Orthop. 1990, 258, 108–121. [Google Scholar] [CrossRef]
- Mjöberg, B. Theories of Wear and Loosening in Hip Prostheses: Wear-Induced Loosening vs. Loosening-Induced Wear–a Review. Acta Orthop. Scand. 1994, 65, 361–371. [Google Scholar] [CrossRef]
- Norton, M.R.; Eyres, K.S. Irrigation and Suction Technique to Ensure Reliable Cement Penetration for Total Knee Arthroplasty. J. Arthroplast. 2000, 15, 468–474. [Google Scholar] [CrossRef]
- Phillips, A.M.; Goddard, N.J.; Tomlinson, J.E. Current Techniques in Total Knee Replacement: Results of a National Survey. Ann. R. Coll. Surg. Engl. 1996, 78, 515–520. [Google Scholar]
- Karpiński, R.; Szabelski, J.; Krakowski, P.; Jonak, J. Effect of Physiological Saline Solution Contamination on Selected Mechanical Properties of Seasoned Acrylic Bone Cements of Medium and High Viscosity. Materials 2020, 14, 110. [Google Scholar] [CrossRef]
- Mousa, W.F.; Kobayashi, M.; Shinzato, S.; Kamimura, M.; Neo, M.; Yoshihara, S.; Nakamura, T. Biological and Mechanical Properties of PMMA-Based Bioactive Bone Cements. Biomaterials 2000, 21, 2137–2146. [Google Scholar] [CrossRef]
- Lelovics, H.; Liptáková, T. Time and Mixing Technique-Dependent Changes in Bone Cement SmartSet® HV. Acta Bioeng. Biomech. 2010, 12, 63–67. [Google Scholar]
- Eyerer, P.; Jin, R. Influence of Mixing Technique on Some Properties of PMMA Bone Cement. J. Biomed. Mater. Res. 1986, 20, 1057–1094. [Google Scholar] [CrossRef]
- Dunne, N.J.; Orr, J.F. Influence of Mixing Techniques on the Physical Properties of Acrylic Bone Cement. Biomaterials 2001, 22, 1819–1826. [Google Scholar] [CrossRef]
- Karpinski, R.; Szabelski, J.; Maksymiuk, J. Analysis of the Properties of Bone Cement with Respect to Its Manufacturing and Typical Service Lifetime Conditions. MATEC Web Conf. 2018, 244, 01004. [Google Scholar] [CrossRef]
- Karpiński, R.; Szabelski, J.; Maksymiuk, J. Seasoning Polymethyl Methacrylate (PMMA) Bone Cements with Incorrect Mix Ratio. Materials 2019, 12, 3073. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Koh, B.T.; Ramruttun, A.; Wang, W. Compression and Flexural Strength of Bone Cement Mixed with Blood. J. Orthop. Surg. 2016, 24, 240–244. [Google Scholar] [CrossRef]
- Karpiński, R.; Szabelski, J.; Maksymiuk, J. Effect of Physiological Fluids Contamination on Selected Mechanical Properties of Acrylate Bone Cement. Materials 2019, 12, 3963. [Google Scholar] [CrossRef] [PubMed]
- Szabelski, J.; Karpiński, R.; Krakowski, P.; Jonak, J. The Impact of Contaminating Poly (Methyl Methacrylate) (PMMA) Bone Cements on Their Compressive Strength. Materials 2021, 14, 2555. [Google Scholar] [CrossRef]
- Machrowska, A.; Karpiński, R.; Jonak, J.; Szabelski, J.; Krakowski, P. Numerical Prediction of the Component-Ratio-Dependent Compressive Strength of Bone Cement. Appl. Comput. Sci. 2020, 16, 87–101. [Google Scholar] [CrossRef]
- Machrowska, A.; Szabelski, J.; Karpiński, R.; Krakowski, P.; Jonak, J.; Jonak, K. Use of Deep Learning Networks and Statistical Modeling to Predict Changes in Mechanical Parameters of Contaminated Bone Cements. Materials 2020, 13, 5419. [Google Scholar] [CrossRef]
- Karpiński, R.; Szabelski, J.; Krakowski, P.; Jojczuk, M.; Jonak, J.; Nogalski, A. Evaluation of the Effect of Selected Physiological Fluid Contaminants on the Mechanical Properties of Selected Medium-Viscosity PMMA Bone Cements. Materials 2022, 15, 2197. [Google Scholar] [CrossRef]
- Boehm, A.; Meininger, S.; Tesch, A.; Gbureck, U.; Müller, F. The Mechanical Properties of Biocompatible Apatite Bone Cement Reinforced with Chemically Activated Carbon Fibers. Materials 2018, 11, 192. [Google Scholar] [CrossRef]
- Soleymani Eil Bakhtiari, S.; Bakhsheshi-Rad, H.R.; Karbasi, S.; Tavakoli, M.; Razzaghi, M.; Ismail, A.F.; RamaKrishna, S.; Berto, F. Polymethyl Methacrylate-Based Bone Cements Containing Carbon Nanotubes and Graphene Oxide: An Overview of Physical, Mechanical, and Biological Properties. Polymers 2020, 12, 1469. [Google Scholar] [CrossRef]
- Kane, R.J.; Yue, W.; Mason, J.J.; Roeder, R.K. Improved Fatigue Life of Acrylic Bone Cements Reinforced with Zirconia Fibers. J. Mech. Behav. Biomed. Mater. 2010, 3, 504–511. [Google Scholar] [CrossRef]
- Kotha, S.; Li, C.; Schmid, S.; Mason, J. Reinforcement of Bone Cement Using Zirconia Fibers with and without Acrylic Coating. J. Biomed. Mater. Res. A 2009, 88, 898–906. [Google Scholar] [CrossRef] [PubMed]
- Khaled, S.M.Z.; Charpentier, P.A.; Rizkalla, A.S. Physical and Mechanical Properties of PMMA Bone Cement Reinforced with Nano-Sized Titania Fibers. J. Biomater. Appl. 2011, 25, 515–537. [Google Scholar] [CrossRef] [PubMed]
- Kotha, S.P.; Li, C.; McGinn, P.; Schmid, S.R.; Mason, J.J. Improved Mechanical Properties of Acrylic Bone Cement with Short Titanium Fiber Reinforcement. J. Mater. Sci. Mater. Med. 2006, 17, 743–748. [Google Scholar] [CrossRef] [PubMed]
- Kotha, S.P.; Li, C.; McGinn, P.; Schmid, S.R.; Mason, J.J. Improved Mechanical Properties of Acrylic Bone Cement with Short Titanium Fiber Reinforcement. J. Mater. Sci. Mater. Med. 2006, 17, 1403–1409. [Google Scholar] [CrossRef]
- Knoell, A.; Maxwell, H.; Bechtol, C. Graphite Fiber Reinforced Bone Cement: An Experimental Feasibility Investigation. Ann. Biomed. Eng. 1975, 3, 225–229. [Google Scholar] [CrossRef]
- Gonçalves, G.; Cruz, S.M.A.; Ramalho, A.; Grácio, J.; Marques, P.A.A.P. Graphene Oxide versus Functionalized Carbon Nanotubes as a Reinforcing Agent in a PMMA/HA Bone Cement. Nanoscale 2012, 4, 2937. [Google Scholar] [CrossRef]
- Paz, E.; Ballesteros, Y.; Abenojar, J.; del Real, J.C.; Dunne, N.J. Graphene Oxide and Graphene Reinforced PMMA Bone Cements: Evaluation of Thermal Properties and Biocompatibility. Materials 2019, 12, 3146. [Google Scholar] [CrossRef]
- Paz, E.; Ballesteros, Y.; Forriol, F.; Dunne, N.J.; del Real, J.C. Graphene and Graphene Oxide Functionalisation with Silanes for Advanced Dispersion and Reinforcement of PMMA-Based Bone Cements. Mater. Sci. Eng. C 2019, 104, 109946. [Google Scholar] [CrossRef]
- Wekwejt, M.; Chen, S.; Kaczmarek-Szczepańska, B.; Nadolska, M.; Łukowicz, K.; Pałubicka, A.; Michno, A.; Osyczka, A.M.; Michálek, M.; Zieliński, A. Nanosilver-Loaded PMMA Bone Cement Doped with Different Bioactive Glasses—Evaluation of Cytocompatibility, Antibacterial Activity, and Mechanical Properties. Biomater. Sci. 2021, 9, 3112–3126. [Google Scholar] [CrossRef] [PubMed]
- Wekwejt, M.; Michalska-Sionkowska, M.; Bartmański, M.; Nadolska, M.; Łukowicz, K.; Pałubicka, A.; Osyczka, A.M.; Zieliński, A. Influence of Several Biodegradable Components Added to Pure and Nanosilver-Doped PMMA Bone Cements on Its Biological and Mechanical Properties. Mater. Sci. Eng. C 2020, 117, 111286. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, T.; Lassila, L.V.J.; Baba, H.; Tashiro, S.; Hamanaka, I.; Takahashi, Y.; Vallittu, P.K. Effect of Cellulose Nanofiber Content on Flexural Properties of a Model, Thermoplastic, Injection-Molded, Polymethyl Methacrylate Denture Base Material. J. Mech. Behav. Biomed. Mater. 2020, 102, 103513. [Google Scholar] [CrossRef] [PubMed]
- Mansoorianfar, M.; Shahin, K.; Mirström, M.M.; Li, D. Cellulose-Reinforced Bioglass Composite as Flexible Bioactive Bandage to Enhance Bone Healing. Ceram. Int. 2021, 47, 416–423. [Google Scholar] [CrossRef]
- Letchmanan, K.; Shen, S.-C.; Ng, W.K.; Kingshuk, P.; Shi, Z.; Wang, W.; Tan, R.B.H. Mechanical Properties and Antibiotic Release Characteristics of Poly(Methyl Methacrylate)-Based Bone Cement Formulated with Mesoporous Silica Nanoparticles. J. Mech. Behav. Biomed. Mater. 2017, 72, 163–170. [Google Scholar] [CrossRef]
- Slane, J.; Vivanco, J.; Ebenstein, D.; Squire, M.; Ploeg, H.-L. Multiscale Characterization of Acrylic Bone Cement Modified with Functionalized Mesoporous Silica Nanoparticles. J. Mech. Behav. Biomed. Mater. 2014, 37, 141–152. [Google Scholar] [CrossRef]
- He, X.; Qu, Y.; Peng, J.; Peng, T.; Qian, Z. A Novel Botryoidal Aramid Fiber Reinforcement of a PMMA Resin for a Restorative Biomaterial. Biomater. Sci. 2017, 5, 808–816. [Google Scholar] [CrossRef]
- Nasiri, F.; Ajeli, S.; Semnani, D.; Jahanshahi, M.; Emadi, R. Design, Fabrication and Structural Optimization of Tubular Carbon/Kevlar®/PMMA/Graphene Nanoplate Composite for Bone Fixation Prosthesis. Biomed. Mater. 2018, 13, 045010. [Google Scholar] [CrossRef]
- Beruto, D.T.; Mezzasalma, S.A.; Capurro, M.; Botter, R.; Cirillo, P. Use of α-Tricalcium Phosphate (TCP) as Powders and as an Aqueous Dispersion to Modify Processing, Microstructure, and Mechanical Properties of Polymethylmethacrylate (PMMA) Bone Cements and to Produce Bone-Substitute Compounds. J. Biomed. Mater. Res. 2000, 49, 498–505. [Google Scholar] [CrossRef]
- Serbetci, K.; Korkusuz, F.; Hasirci, N. Thermal and Mechanical Properties of Hydroxyapatite Impregnated Acrylic Bone Cements. Polym. Test. 2004, 23, 145–155. [Google Scholar] [CrossRef]
- Kang, I.-G.; Park, C.-I.; Lee, H.; Kim, H.-E.; Lee, S.-M. Hydroxyapatite Microspheres as an Additive to Enhance Radiopacity, Biocompatibility, and Osteoconductivity of Poly(Methyl Methacrylate) Bone Cement. Materials 2018, 11, 258. [Google Scholar] [CrossRef] [PubMed]
- Che, Y.; Min, S.; Wang, M.; Rao, M.; Quan, C. Biological Activity of Hydroxyapatite/Poly(Methylmethacrylate) Bone Cement with Different Surface Morphologies and Modifications for Induced Osteogenesis. J. Appl. Polym. Sci. 2019, 136, 48188. [Google Scholar] [CrossRef]
- Montaño, C.J.; Campos, T.P.R.; Lemos, B.R.S.; Yoshida, M.I.; Almeida, N.G.S.; Aguilar, M.T.P.; Lima, C.V. Effects of Hydroxyapatite on PMMA-HAp Cement for Biomedical Applications. Biomed. Mater. Eng. 2020, 31, 191–201. [Google Scholar] [CrossRef]
- Litak, J.; Czyzewski, W.; Szymoniuk, M.; Pastuszak, B.; Litak, J.; Litak, G.; Grochowski, C.; Rahnama-Hezavah, M.; Kamieniak, P. Hydroxyapatite Use in Spine Surgery—Molecular and Clinical Aspect. Materials 2022, 15, 2906. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Tang, Y.; Zhao, K.; Zha, X.; Liu, J.; Bai, H.; Wu, Z. Fabrication of the Antibiotic-Releasing Gelatin/PMMA Bone Cement. Colloids Surf. B Biointerfaces 2019, 183, 110448. [Google Scholar] [CrossRef]
- Cacciola, G.; De Meo, F.; Cavaliere, P. Mechanical and Elution Properties of G3 Low Viscosity Bone Cement Loaded up to Three Antibiotics. J. Orthop. 2018, 15, 1004–1007. [Google Scholar] [CrossRef] [PubMed]
- Anagnostakos, K.; Fürst, O.; Kelm, J. Antibiotic-Impregnated PMMA Hip Spacers: Current Status. Acta Orthop. 2006, 77, 628–637. [Google Scholar] [CrossRef]
- ISO 5833:2002; Implants for Surgery—Acrylic Resin Cements. ISO: Geneva, Switzerland, 2002.
- Schonhoff, M.; Bormann, T.; Knappe, K.; Reiner, T.; Stange, L.; Jaeger, S. The Effect of Cement Aging on the Stability of a Cement-in-Cement Revision Construct. Appl. Sci. 2021, 11, 2814. [Google Scholar] [CrossRef]
- Wu, M.; O’Donnell, J.; Cochrane, N.; Ryan, S.; Belay, E.; Myntti, M.; Seyler, T. Effect of Commonly Used Lavage Solutions on the Polymerization of Bone Cement. Orthop. Traumatol. Surg. Res. 2022, 103243. [Google Scholar] [CrossRef]
- Donaldson, A.J.; Thomson, H.E.; Harper, N.J.; Kenny, N.W. Bone Cement Implantation Syndrome. Br. J. Anaesth. 2009, 102, 12–22. [Google Scholar] [CrossRef]
- Rassir, R.; Schuiling, M.; Sierevelt, I.N.; van der Hoeven, C.W.P.; Nolte, P.A. What are the Frequency, Related Mortality, and Factors Associated with Bone Cement Implantation Syndrome in Arthroplasty Surgery? Clin. Orthop. 2021, 479, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.I.; Ahmed, A.B.; Baxendale, B.R.; Moran, C.G. Cardiac Output during Hemiarthroplasty of the Hip: A Prospective, Controlled Trial of Cemented and Uncemented Prostheses. J. Bone Jt. Surg. Br. 2001, 83-B, 414–418. [Google Scholar] [CrossRef]
- Orsini, E.C.; Byrick, R.J.; Mullen, J.B.; Kay, J.C.; Waddell, J.P. Cardiopulmonary Function and Pulmonary Microemboli during Arthroplasty Using Cemented or Non-Cemented Components. The Role of Intramedullary Pressure. J. Bone Jt. Surg. Am. 1987, 69, 822–832. [Google Scholar] [CrossRef]
- Bettencourt, A.; Calado, A.; Amaral, J.; Alfaia, A.; Vale, F.M.; Monteiro, J.; Montemor, M.F.; Ferreira, M.G.S.; Castro, M. Surface Studies on Acrylic Bone Cement. Int. J. Pharm. 2004, 278, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Pijls, B.G.; Valstar, E.R.; Nouta, K.-A.; Plevier, J.W.; Fiocco, M.; Middeldorp, S.; Nelissen, R.G. Early Migration of Tibial Components Is Associated with Late Revision: A Systematic Review and Meta-Analysis of 21,000 Knee Arthroplasties. Acta Orthop. 2012, 83, 614–624. [Google Scholar] [CrossRef] [PubMed]
- Jasty, M.; Bragdon, C.; Burke, D.; O’Connor, D.; Lowenstein, J.; Harris, W.H. In Vivo Skeletal Responses to Porous-Surfaced Implants Subjected to Small Induced Motions*. J. Bone Jt. Surg. Am. 1997, 79, 707–714. [Google Scholar] [CrossRef] [PubMed]
- Pahlevanzadeh, F.; Bakhsheshi-Rad, H.R.; Ismail, A.F.; Aziz, M.; Chen, X.B. Development of PMMA-Mon-CNT Bone Cement with Superior Mechanical Properties and Favorable Biological Properties for Use in Bone-Defect Treatment. Mater. Lett. 2019, 240, 9–12. [Google Scholar] [CrossRef]
- Zheng, X.; Wang, Y.; Liu, J.; Han, J.; Cui, Z.; Wu, S.; Liang, Y.; Zhu, S.; Ge, X.; Li, Z. Gelatin/Gentamicin Sulfate-Modified PMMA Bone Cement with Proper Mechanical Properties and High Antibacterial Ability. Mater. Res. Express 2022, 9, 035405. [Google Scholar] [CrossRef]
- Phakatkar, A.H.; Shirdar, M.R.; Qi, M.; Taheri, M.M.; Narayanan, S.; Foroozan, T.; Sharifi-Asl, S.; Huang, Z.; Agrawal, M.; Lu, Y.; et al. Novel PMMA Bone Cement Nanocomposites Containing Magnesium Phosphate Nanosheets and Hydroxyapatite Nanofibers. Mater. Sci. Eng. C 2020, 109, 110497. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Maeda, T.; Miyazaki, T. Effect of Calcium Acetate Content on Apatite-Forming Ability and Mechanical Property of PMMA Bone Cement Modified with Quaternary Ammonium. Materials 2020, 13, 4998. [Google Scholar] [CrossRef] [PubMed]
- Rudawska, A.; Abdel Wahab, M.; Szabelski, J.; Miturska, I.; Doluk, E. The Strength of Rigid and Flexible Adhesive Joints at Room Temperature and After Thermal Shocks. In Proceedings of 1st International Conference on Structural Damage Modelling and Assessment, SDMA 2020, Ghent University, Ghent, Belgium, 4–5 August 2020; Lecture Notes in Civil Engineering; Wahab, M.A., Ed.; Springer: Singapore, 2021; Volume 110, pp. 229–241. ISBN 9789811591204. [Google Scholar]
- Rudawska, A.; Miturska, I.; Szabelski, J.; Abdel Wahab, M.; Stančeková, D.; Čuboňová, N.; Madleňák, R. The Impact of the Selected Exploitation Factors on the Adhesive Joints Strength. In Proceedings of the 13th International Conference on Damage Assessment of Structures, DAMAS 2019, Porto, Portugal, 9–10 July 2019; Lecture Notes in Mechanical Engineering; Wahab, M.A., Ed.; Springer: Singapore, 2020; pp. 899–913. ISBN 9789811383304. [Google Scholar]
- Rudawska, A.; Miturska, I.; Szabelski, J.; Skoczylas, A.; Droździel, P.; Bociąga, E.; Madleňák, R.; Kasperek, D. Experimental Research and Statistic Analysis of Polymer Composite Adhesive Joints Strength. J. Phys. Conf. Ser. 2017, 842, 012074. [Google Scholar] [CrossRef]
- Szabelski, J. Effect of Incorrect Mix Ratio on Strength of Two Component Adhesive Butt-Joints Tested at Elevated Temperature. MATEC Web Conf. 2018, 244, 01019. [Google Scholar] [CrossRef]
- Le Coz, C.-J. Occupational Allergic Contact Dermatitis from Polyurethane/Methacrylates in Windscreen Repair Chemical: Contact Point. Contact Dermat. 2003, 48, 275–276. [Google Scholar] [CrossRef]
- Hickey, J.R.; Sansom, J.E. Allergic Contact Dermatitis Following Airborne Exposure to Methacrylates Used in the Manufacture of Artificial Skin. Contact Dermat. 2003, 49, 221. [Google Scholar] [CrossRef]
- Heinemann, L.; Kamann, S. Adhesives Used for Diabetes Medical Devices: A Neglected Risk with Serious Consequences? J. Diabetes Sci. Technol. 2016, 10, 1211–1215. [Google Scholar] [CrossRef]
- Szabelski, J.; Karpiński, R.; Machrowska, A. Application of an Artificial Neural Network in the Modelling of Heat Curing Effects on the Strength of Adhesive Joints at Elevated Temperature with Imprecise Adhesive Mix Ratios. Materials 2022, 15, 721. [Google Scholar] [CrossRef]
- Gould, G.; Goswami, T. Modelling PMMA Porosity on the Cement-Stem Interface of Hip Implants. Int. J. Biomed. Eng. Technol. 2013, 11, 107. [Google Scholar] [CrossRef]
- Kim, S.; Baril, C.; Rudraraju, S.; Ploeg, H.-L. Influence of Porosity on Fracture Toughness and Fracture Behavior of Antibiotic-Loaded PMMA Bone Cement. J. Biomech. Eng. 2022, 144, 011006. [Google Scholar] [CrossRef] [PubMed]
- Madrala, A.; Nuño, N.; Bureau, M.N. Does Stem Preheating Have a Beneficial Effect on PMMA Bulk Porosity in Cemented THA? J. Biomed. Mater. Res. B Appl. Biomater. 2010, 95, 1–8. [Google Scholar] [CrossRef] [PubMed]

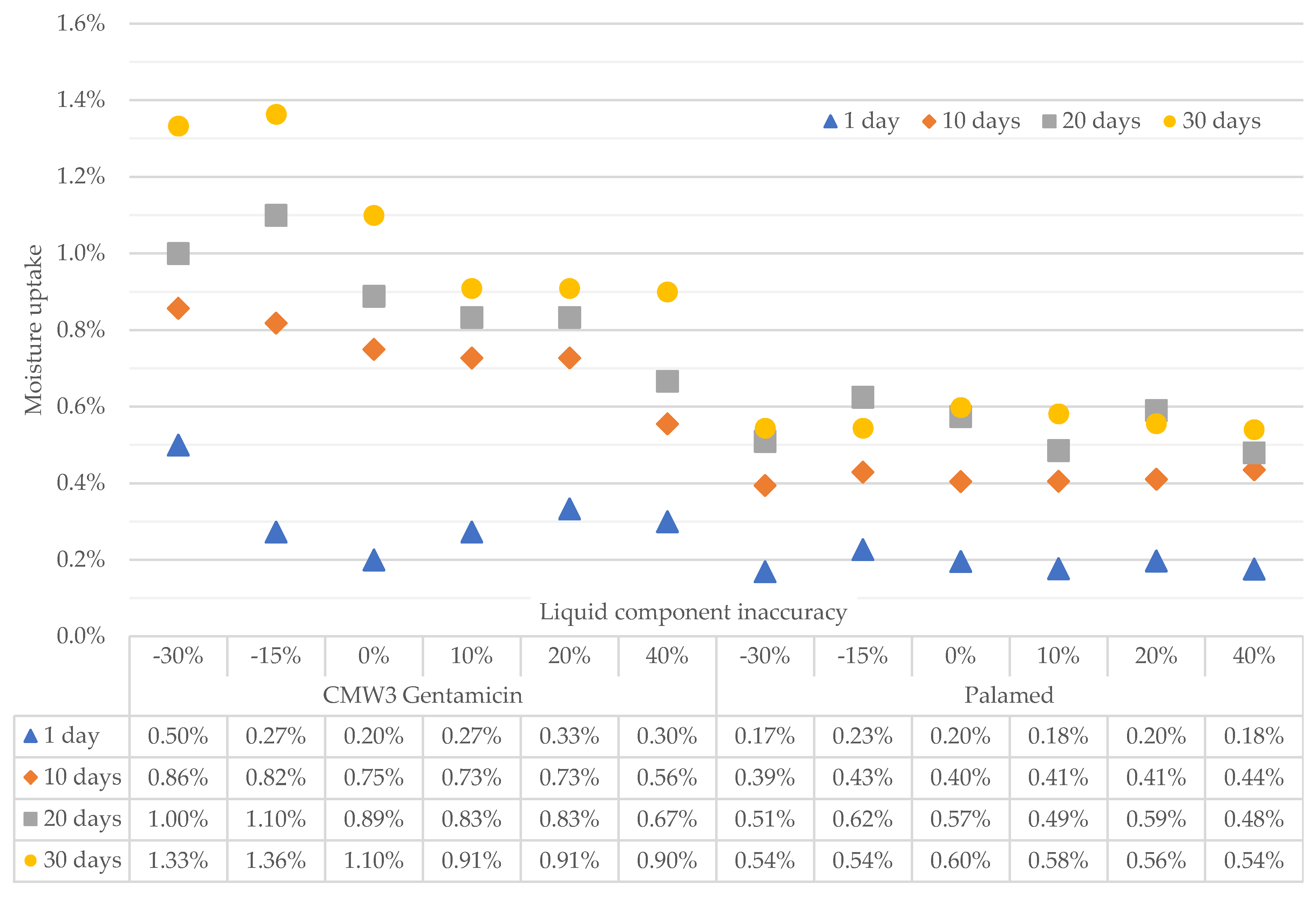

| Inaccuracy of Components Ratio (Liquid Part) | Palamed | CMW3 | ||||
|---|---|---|---|---|---|---|
| m | b | R2 | m | b | R2 | |
| −30% | 0.0035 | 0.0025 | 0.8853 | 0.0081 | 0.0063 | 0.9724 |
| −15% | 0.0033 | 0.0046 | 0.7770 | 0.0088 | 0.0013 | 0.9365 |
| 0% | 0.0036 | 0.0028 | 0.8993 | 0.0065 | 0.0031 | 0.7926 |
| +20% | 0.0035 | 0.0026 | 0.9259 | 0.0051 | 0.0059 | 0.8775 |
| +40% | 0.0034 | 0.0035 | 0.8520 | 0.0057 | 0.0037 | 0.9819 |
| +50% | 0.0031 | 0.0034 | 0.8338 | 0.0049 | 0.0053 | 0.9746 |
| Liquid Part Inaccuracy | Seasoning [Days] | CMW 3 Gentamicin | Palamed | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Strength [MPa] | 1 | 2 | 3 | Mean Strength [MPa] | 1 | 2 | 3 | ||
| −30% | 0 | 75.21 | * | 64.12 | * | ||||
| 1 | 76.30 | * | 66.23 | * | |||||
| 10 | 71.03 | * | 61.24 | * | * | ||||
| 20 | 70.81 | * | 57.02 | * | |||||
| 30 | 69.94 | * | 66.10 | * | |||||
| −15% | 0 | 78.92 | * | 69.58 | * | * | |||
| 1 | 75.36 | * | 66.22 | * | * | ||||
| 10 | 70.57 | * | 63.73 | * | |||||
| 20 | 74.49 | * | 64.58 | * | * | ||||
| 30 | 70.38 | * | 71.28 | * | |||||
| 0% | 0 | 84.81 | * | 70.79 | * | ||||
| 1 | 78.98 | * | * | 67.20 | * | ||||
| 10 | 76.53 | * | * | 68.22 | * | ||||
| 20 | 73.10 | * | 66.31 | * | |||||
| 30 | 73.73 | * | 69.89 | * | |||||
| 10% | 0 | 89.94 | * | 75.87 | * | ||||
| 1 | 80.86 | * | 71.81 | * | * | ||||
| 10 | 77.70 | * | * | 68.97 | * | * | |||
| 20 | 74.38 | * | 65.82 | * | |||||
| 30 | 73.82 | * | 72.10 | * | * | ||||
| 20% | 0 | 94.57 | * | 73.53 | * | ||||
| 1 | 82.18 | * | 69.68 | * | * | ||||
| 10 | 76.12 | * | * | 67.09 | * | ||||
| 20 | 72.97 | * | 65.14 | * | |||||
| 30 | 74.09 | * | 68.48 | * | * | ||||
| 40% | 0 | 83.15 | * | 73.17 | * | ||||
| 1 | 80.08 | * | * | 72.73 | * | ||||
| 10 | 77.42 | * | 68.85 | * | * | ||||
| 20 | 73.09 | * | 66.34 | * | |||||
| 30 | 71.00 | * | 68.34 | * | * | ||||
| b1 | b2 | b3 | b4 | b5 | b6 | |
|---|---|---|---|---|---|---|
| Palamed | 71.3464 | 0.1506 | −0.7459 | −0.0025 | −0.0029 | 0.0236 |
| CMW3 G | 82.0006 | 0.1541 | −0.722 | −0.0029 | −0.0035 | 0.0148 |
| Liquid Part Inaccuracy | Seasoning [Days] | CMW 3 Gentamicin | Palamed | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean Modulus [MPa] | 1 | 2 | 3 | 4 | Mean Modulus [MPa] | 1 | 2 | 3 | ||
| −30% | 0 | 904.48 | * | 1457.99 | * | |||||
| 1 | 806.33 | * | 1470.34 | * | ||||||
| 10 | 809.93 | * | 1276.22 | * | * | |||||
| 20 | 793.59 | * | 1134.26 | * | ||||||
| 30 | 755.62 | * | 1371.70 | * | * | |||||
| −15% | 0 | 935.71 | * | 1572.86 | * | |||||
| 1 | 806.98 | * | 1512.53 | * | ||||||
| 10 | 785.34 | * | 1407.61 | * | ||||||
| 20 | 790.46 | * | 1396.41 | * | ||||||
| 30 | 753.97 | * | 1627.89 | * | ||||||
| 0% | 0 | 964.26 | * | 1504.81 | * | |||||
| 1 | 860.35 | * | * | 1512.06 | * | |||||
| 10 | 828.00 | * | 1425.05 | * | ||||||
| 20 | 816.98 | * | 1471.68 | * | ||||||
| 30 | 803.12 | * | 1476.22 | * | ||||||
| 10% | 0 | 979.96 | * | 1529.62 | * | * | ||||
| 1 | 919.66 | * | * | 1714.86 | * | |||||
| 10 | 838.39 | * | * | 1636.84 | * | * | ||||
| 20 | 800.83 | * | 1456.18 | * | ||||||
| 30 | 793.51 | * | 1654.31 | * | * | |||||
| 20% | 0 | 926.79 | * | 1627.03 | * | |||||
| 1 | 870.62 | * | 1592.06 | * | ||||||
| 10 | 776.62 | * | 1499.11 | * | ||||||
| 20 | 788.06 | * | 1468.36 | * | ||||||
| 30 | 738.10 | * | 1511.07 | * | ||||||
| 40% | 0 | 975.34 | * | 1452.31 | * | |||||
| 1 | 901.90 | * | 1813.58 | * | ||||||
| 10 | 852.64 | * | * | 1684.67 | * | * | ||||
| 20 | 823.97 | * | * | 1638.91 | * | * | ||||
| 30 | 780.30 | * | 1662.44 | * | * | |||||
| b1 | b2 | b3 | b4 | b5 | b6 | |
|---|---|---|---|---|---|---|
| Palamed | 1570.73 | 3.564 | −15.5502 | −0.0263 | 0.048 | 0.4738 |
| CMW3 G | 897.64 | 1.1818 | −8.7537 | −0.0061 | −0.0333 | 0.1616 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szabelski, J.; Karpiński, R.; Krakowski, P.; Jojczuk, M.; Jonak, J.; Nogalski, A. Analysis of the Effect of Component Ratio Imbalances on Selected Mechanical Properties of Seasoned, Medium Viscosity Bone Cements. Materials 2022, 15, 5577. https://doi.org/10.3390/ma15165577
Szabelski J, Karpiński R, Krakowski P, Jojczuk M, Jonak J, Nogalski A. Analysis of the Effect of Component Ratio Imbalances on Selected Mechanical Properties of Seasoned, Medium Viscosity Bone Cements. Materials. 2022; 15(16):5577. https://doi.org/10.3390/ma15165577
Chicago/Turabian StyleSzabelski, Jakub, Robert Karpiński, Przemysław Krakowski, Mariusz Jojczuk, Józef Jonak, and Adam Nogalski. 2022. "Analysis of the Effect of Component Ratio Imbalances on Selected Mechanical Properties of Seasoned, Medium Viscosity Bone Cements" Materials 15, no. 16: 5577. https://doi.org/10.3390/ma15165577
APA StyleSzabelski, J., Karpiński, R., Krakowski, P., Jojczuk, M., Jonak, J., & Nogalski, A. (2022). Analysis of the Effect of Component Ratio Imbalances on Selected Mechanical Properties of Seasoned, Medium Viscosity Bone Cements. Materials, 15(16), 5577. https://doi.org/10.3390/ma15165577







