Pilot Evaluation of Sealer-Based Root Canal Obturation Using Epoxy-Resin-Based and Calcium-Silicate-Based Sealers: A Randomized Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
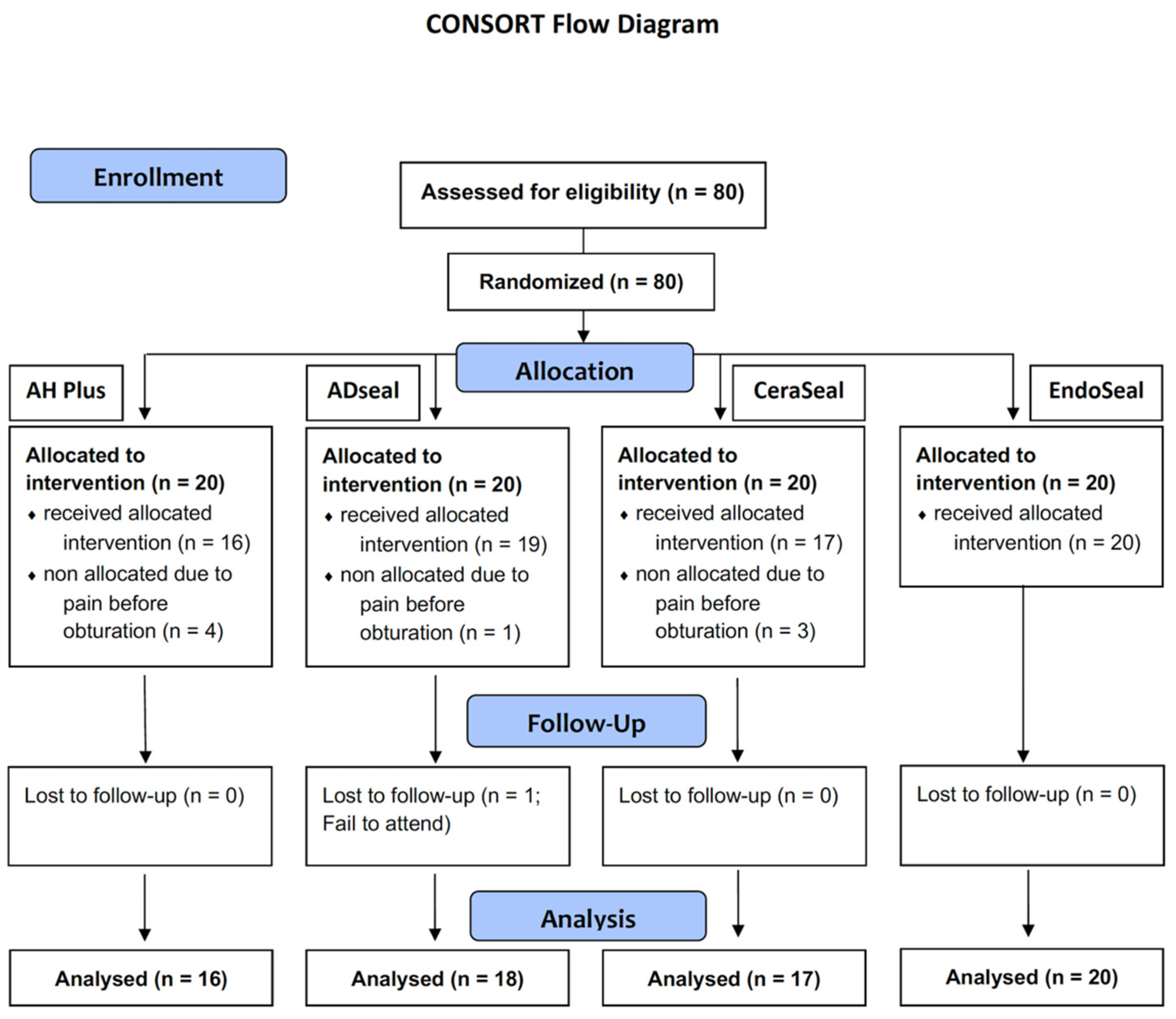
2.1. Study Design and Inclusion/Exclusion Criteria
2.2. Sample Size Calculation and Randomization
2.3. Treatment Procedure
2.4. Clinical and Radiographic Evaluation
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ørstavik, D. Endodontic filling materials. Endod. Top. 2014, 31, 53–67. [Google Scholar] [CrossRef]
- Trope, M.; Bunes, A.; Debelian, G. Root filling materials and techniques: Bioceramics a new hope? Endod. Top. 2015, 32, 86–96. [Google Scholar] [CrossRef]
- Lim, M.; Jung, C.; Shin, D.H.; Cho, Y.B.; Song, M. Calcium silicate-based root canal sealers: A literature review. Restor. Dent. Endod. 2020, 45, e35. [Google Scholar] [CrossRef]
- Al-Haddad, A.; Che Ab Aziz, Z.A. Bioceramic-based root canal sealers: A review. Int. J. Biomater. 2016, 2016, 9753210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horsted-Bindslev, P.; Andersen, M.A.; Jensen, M.F.; Nilsson, J.H.; Wenzel, A. Quality of molar root canal fillings performed with the lateral compaction and the single-cone technique. J. Endod. 2007, 33, 468–471. [Google Scholar] [CrossRef] [PubMed]
- Marciano, M.A.; Ordinola-Zapata, R.; da Cunha, T.V.; Duarte, M.A.H.; Cavenago, B.C.; Garcia, R.B.; Bramante, C.M.; Bernardineli, N.; Moraesl, I.G. Analysis of four gutta-percha techniques used to fill mesial root canals of mandibular molars. Int. Endod. J. 2011, 44, 321–329. [Google Scholar] [CrossRef]
- Somma, F.; Cretella, G.; Carotenuto, M.; Pecci, R.; Bedini, R.; De Biasi, M.; Angerame, D. Quality of thermoplasticized and single point root fillings assessed by micro-computed tomography. Int. Endod. J. 2011, 44, 362–369. [Google Scholar] [CrossRef] [PubMed]
- Poggio, C.; Arciola, C.R.; Dagna, A.; Colombo, M.; Bianchi, S.; Visai, L. Solubility of root canal sealers: A comparative study. Int. J. Artif. Organs 2010, 33, 676–681. [Google Scholar] [CrossRef] [PubMed]
- Schweikl, H.; Schmalz, G.; Federlin, M. Mutagenicity of the root canal sealer AH Plus in the Ames test. Clin. Oral Investig. 1998, 2, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Azar, N.G.; Heidari, M.; Bahrami, Z.S.; Shokri, F. In vitro cytotoxicity of a new epoxy resin root canal sealer. J. Endod. 2000, 26, 462–465. [Google Scholar] [CrossRef]
- Sousa, C.J.; Montes, C.R.; Pascon, E.A.; Loyola, A.M.; Versiani, M.A. Comparison of the intraosseous biocompatibility of AH Plus, EndoREZ, and Epiphany root canal sealers. J. Endod. 2006, 32, 656–662. [Google Scholar] [CrossRef]
- López-García, S.; Myong-Hyun, B.; Lozano, A.; García-Bernal, D.; Forner, L.; Llena, C.; Guerrero-Gironés, J.; Murcia, L.; Rodríguez-Lozano, F.J. Cytocompatibility, bioactivity potential, and ion release of three premixed calcium silicate-based sealers. Clin. Oral Investig. 2020, 24, 1749–1759. [Google Scholar] [CrossRef] [PubMed]
- Donnermeyer, D.; Burklein, S.; Dammaschke, T.; Schafer, E. Endodontic sealers based on calcium silicates: A systematic review. Odontology 2019, 107, 421–436. [Google Scholar] [CrossRef] [PubMed]
- Abedi-Amin, A.; Luzi, A.; Giovarruscio, M.; Paolone, G.; Darvizeh, A.; Agulló, V.V.; Sauro, S. Innovative root-end filling materials based on calcium-silicates and calcium-phosphates. J. Mater. Sci. Mater. Med. 2017, 28, 31. [Google Scholar] [CrossRef] [PubMed]
- Kharouf, N.; Arntz, Y.; Eid, A.; Zghal, J.; Sauro, S.; Haikel, Y.; Mancino, D. Physicochemical and antibacterial properties of novel, premixed calcium silicate-based sealer compared to powder-liquid bioceramic sealer. J. Clin. Med. 2020, 9, 3096. [Google Scholar] [CrossRef]
- Kim, S.R.; Kwak, S.W.; Lee, J.K.; Goo, H.J.; Ha, J.H.; Kim, H.C. Efficacy and retrievability of root canal filling using calcium silicate-based and epoxy resin-based root canal sealers with matched obturation techniques. Aust. Endod. J. 2019, 45, 337–345. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Fonseca, B.; Coelho, M.S.; Bueno, C.E.dS.; Fontana, C.E.; Martin, A.S.D.; Rocha, D.G.P. Assessment of extrusion and postoperative pain of a bioceramic and resin-based root canal sealer. Eur. J. Dent. 2019, 13, 343–348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferreira, N.S.; Gollo, E.K.F.; Boscato, N.; Arias, A.; Silva, E. Postoperative pain after root canal filling with different endodontic sealers: A randomized clinical trial. Braz. Oral Res. 2020, 34, e069. [Google Scholar] [CrossRef]
- Guivarc’h, M.; Jeanneau, C.; Giraud, T.; Pommel, L.; About, I.; Azim, A.A.; Bukiet, F. An international survey on the use of calcium silicate-based sealers in non-surgical endodontic treatment. Clin. Oral Investig. 2020, 24, 417–424. [Google Scholar] [CrossRef]
- Yu, Y.H.; Kushnir, L.; Kohli, M.; Karabucak, B. Comparing the incidence of postoperative pain after root canal filling with warm vertical obturation with resin-based sealer and sealer-based obturation with calcium silicate-based sealer: A prospective clinical trial. Clin. Oral Investig. 2021, 25, 5033–5042. [Google Scholar] [CrossRef]
- Alonso-Ezpeleta, L.O.; Gasco-Garcia, C.; Castellanos-Cosano, L.; Martin-Gonzalez, J.; Lopez-Frias, F.J.; Segura-Egea, J.J. Postoperative pain after one-visit root-canal treatment on teeth with vital pulps: Comparison of three different obturation techniques. Med. Oral Patol. Oral Circ. Bucal. 2012, 17, e721–e727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, H.S.G.; Lim, K.C.; Lui, J.N.; Lai, W.M.C.; Yu, V.S.H. Postobturation pain associated with tricalcium silicate and resin-based sealer techniques: A randomized clinical trial. J. Endod. 2021, 47, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Parirokh, M.; Torabinejad, M. Mineral trioxide aggregate: A comprehensive literature review—Part III: Clinical applications, drawbacks, and mechanism of action. J. Endod. 2010, 36, 400–413. [Google Scholar] [CrossRef]
- Sfeir, G.; Zogheib, C.; Patel, S.; Giraud, T.; Nagendrababu, V.; Bukiet, F. Calcium silicate-based root canal sealers: A narrative review and clinical perspectives. Materials 2021, 14, 3965. [Google Scholar] [CrossRef]
- Lim, E.S.; Park, Y.B.; Kwon, Y.S.; Shon, W.J.; Lee, K.W.; Min, K.S. Physical properties and biocompatibility of an injectable calcium-silicate-based root canal sealer: In vitro and in vivo study. BMC Oral Health 2015, 15, 129. [Google Scholar] [CrossRef] [Green Version]
- Chopra, V.; Davis, G.; Baysan, A. Physico-chemical properties of calcium-silicate vs. resin based sealers-A systematic review and meta-analysis of laboratory-based studies. Materials 2021, 15, 229. [Google Scholar] [CrossRef]
- Santos-Junior, A.O.; Tanomaru-Filho, M.; Pinto, J.C.; Tavares, K.; Torres, F.F.E.; Guerreiro-Tanomaru, J.M. Effect of obturation technique using a new bioceramic sealer on the presence of voids in flattened root canals. Braz. Oral Res. 2021, 35, e028. [Google Scholar] [CrossRef] [PubMed]
- Penha da Silva, P.J.; Marceliano-Alves, M.F.; Provenzano, J.C.; Dellazari, R.L.A.; Gonçalves, L.S.; Alves, F.R.F. Quality of root canal filling using a bioceramic sealer in oval canals: A three-dimensional analysis. Eur. J. Dent. 2021, 15, 475–480. [Google Scholar] [CrossRef]
- Al-Jadaa, A.; Attin, T.; Peltomäki, T.; Heumann, C.; Schmidlin, P.R.; Paquè, F. Influence of the internal anatomy on the leakage of root canals filled with thermoplastic technique. Clin. Oral Investig. 2018, 22, 1385–1393. [Google Scholar] [CrossRef]
- Tanomaru-Filho, M.; Pinto, J.C.; Torres, F.F.E.; de Souza, P.H.F.; Pereira, M.C.; Guerreiro-Tanomaru, J.M. Flow, filling ability and apical extrusion of new calcium silicate-based sealers: A micro-computed tomographic study. Dent. Oral Biol. Craniofac. Res. 2020, 3, 1–6. [Google Scholar]
- Ricucci, D.; Rocas, I.N.; Alves, F.R.; Loghin, S.; Siqueira, J.F., Jr. Apically extruded sealers: Fate and influence on treatment outcome. J. Endod. 2016, 42, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Sari, S.; Duruturk, L. Radiographic evaluation of periapical healing of permanent teeth with periapical lesions after extrusion of AH Plus sealer. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 104, e54–e59. [Google Scholar] [CrossRef] [PubMed]
- Scarparo, R.K.; Grecca, F.S.; Fachin, E.V. Analysis of tissue reactions to methacrylate resin-based, epoxy resin-based, and zinc oxide-eugenol endodontic sealers. J. Endod. 2009, 35, 229–232. [Google Scholar] [CrossRef]
- Ruparel, N.B.; Ruparel, S.B.; Chen, P.B.; Ishikawa, B.; Diogenes, A. Direct effect of endodontic sealers on trigeminal neuronal activity. J. Endod. 2014, 40, 683–687. [Google Scholar] [CrossRef] [PubMed]
- Gomes-Filho, J.E.; Watanabe, S.; Cintra, L.T.; Nery, M.J.; Dezan-Júnior, E.; Queiroz, I.O.; Lodi, C.S.; Basso, M.D. Effect of MTA-based sealer on the healing of periapical lesions. J. Appl. Oral Sci. 2013, 21, 235–242. [Google Scholar] [CrossRef]
- Ricucci, D.; Grande, N.M.; Plotino, G.; Tay, F.R. Histologic response of human pulp and periapical tissues to tricalcium silicate-based materials: A series of successfully treated cases. J. Endod. 2020, 46, 307–317. [Google Scholar] [CrossRef]
- Ali, A.; Olivieri, J.G.; Duran-Sindreu, F.; Abella, F.; Roig, M.; Garcia-Font, M. Influence of preoperative pain intensity on postoperative pain after root canal treatment: A prospective clinical study. J. Dent. 2016, 45, 39–42. [Google Scholar] [CrossRef]

| AH Plus (n = 16) | ADseal (n = 19) | CeraSeal (n = 17) | EndoSeal TCS (n = 20) | |
|---|---|---|---|---|
| Sex | ||||
| Male | 7 | 8 | 5 | 9 |
| Female | 9 | 11 | 12 | 11 |
| Age | ||||
| ≤30 | 2 | 2 | 3 | 1 |
| 30~60 | 5 | 7 | 7 | 13 |
| 61≤ | 9 | 10 | 7 | 6 |
| Arch | ||||
| Maxilla | 5 | 10 | 10 | 10 |
| Mandible | 11 | 9 | 7 | 10 |
| Tooth type | ||||
| Anterior | 3 | 5 | 4 | 1 |
| Premolar | 3 | 3 | 2 | 5 |
| Molar | 10 | 11 | 11 | 14 |
| Void (%) | Sealer Extrusion (%) | |||||
|---|---|---|---|---|---|---|
| Tooth | p Value | Tooth | p Value | Canal | p Value | |
| AH Plus | 56.3 (9/16) | 0.145 | 56.3 (9/16) | 0.067 | 33.3 (12/36) | 0.139 |
| ADseal | 31.6 (6/19) | 21.1 (4/19) | 12.2 (5/41) | |||
| CeraSeal | 29.4 (5/17) | 58.8 (10/17) | 29.7 (11/37) | |||
| EndoSeal | 60.0 (12/20) | 35.0 (7/20) | 17.8 (8/45) | |||
| VAS (Mean) | Percussion (+) (n) | Palpation (+) (n) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1-Week | 1-Month | 3-Month | 1-Week | 1-Month | 3-Month | 1-Week | 1-Month | 3-Month | |
| AH Plus (16) | 0.06 | 0.13 | 0.13 | 0 | 0 | 0 | 0 | 0 | 0 |
| ADseal (18) | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| CeraSeal (17) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| EndoSeal (20) | 0.05 | 0.05 | 0.05 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cases with Lesion | 1-Week | 1-Month | 3-Month | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Worse | C * | Healing | Worse | C * | Healing | Worse | C * | Healing | ||
| AH Plus | 6 | 0 | 16 | 0 | 0 | 14 | 2 | 0 | 14 | 2 |
| ADseal | 7 | 0 | 18 | 0 | 0 | 16 | 2 | 0 | 15 | 3 |
| CeraSeal | 8 | 0 | 17 | 0 | 0 | 17 | 0 | 0 | 15 | 2 |
| EndoSeal | 10 | 0 | 20 | 0 | 0 | 18 | 2 | 0 | 16 | 4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, M.; Park, M.-G.; Kwak, S.-W.; Kim, R.H.; Ha, J.-H.; Kim, H.-C. Pilot Evaluation of Sealer-Based Root Canal Obturation Using Epoxy-Resin-Based and Calcium-Silicate-Based Sealers: A Randomized Clinical Trial. Materials 2022, 15, 5146. https://doi.org/10.3390/ma15155146
Song M, Park M-G, Kwak S-W, Kim RH, Ha J-H, Kim H-C. Pilot Evaluation of Sealer-Based Root Canal Obturation Using Epoxy-Resin-Based and Calcium-Silicate-Based Sealers: A Randomized Clinical Trial. Materials. 2022; 15(15):5146. https://doi.org/10.3390/ma15155146
Chicago/Turabian StyleSong, Minju, Min-Gyu Park, Sang-Won Kwak, Ruben H. Kim, Jung-Hong Ha, and Hyeon-Cheol Kim. 2022. "Pilot Evaluation of Sealer-Based Root Canal Obturation Using Epoxy-Resin-Based and Calcium-Silicate-Based Sealers: A Randomized Clinical Trial" Materials 15, no. 15: 5146. https://doi.org/10.3390/ma15155146
APA StyleSong, M., Park, M.-G., Kwak, S.-W., Kim, R. H., Ha, J.-H., & Kim, H.-C. (2022). Pilot Evaluation of Sealer-Based Root Canal Obturation Using Epoxy-Resin-Based and Calcium-Silicate-Based Sealers: A Randomized Clinical Trial. Materials, 15(15), 5146. https://doi.org/10.3390/ma15155146








